Contents
What is aphasia
Aphasia is an impairment of language, affecting the production or comprehension of speech and the ability to read or write. Aphasia impairs the ability to speak and understand others, and most people with aphasia experience difficulty reading and writing. Aphasia is always due to injury to the brain-most commonly from a stroke, particularly in older individuals. But brain injuries resulting in aphasia may also arise from head trauma, from brain tumors, or from infections. Scientists and clinicians who study how language is stored in the brain have learned that different aspects of language are located in different parts of the left hemisphere of the brain. For example, areas in the back portions allow you to understand words. When a stroke affects this posterior or back part of the left hemisphere of the brain, people can have great difficulty understanding what they hear or read.
Aphasia affects a person’s language, but it doesn’t affect a person’s intelligence.
Aphasia affects about two million Americans and is more common than Parkinson’s Disease, cerebral palsy or muscular dystrophy. Nearly 180,000 Americans acquire the disorder each year. However, most people have never heard of it.
While aphasia is most common among older people, it can occur in people of all ages, races, nationalities and gender.
The severity of a person’s aphasia depends on the location and type of injury sustained by the brain. Aphasia typically occurs suddenly after a stroke or a head injury. But it can also come on gradually from a slow-growing brain tumor or a disease that causes progressive, permanent damage (degenerative). Where and how bad the brain damage is and what caused it determine the degree of disability.
Aphasia can occur by itself or alongside other disorders, such as visual difficulties, mobility problems, limb weakness and cognitive changes.
Aphasia can make it hard for you to read, write, and say what you mean to say. Aphasia is most common in adults who have had a stroke. Brain tumors, infections, injuries, and dementia can also cause it. The type of problem you have and how bad it is depends on which part of your brain is damaged and how much damage there is.
People with aphasia make mistakes with the words they use, sometimes using the wrong sounds in a word, choosing the wrong word, or putting words together incorrectly.
Aphasia also affects speaking and writing in the same way. Many people with the condition find it difficult to understand words and sentences they hear or read.
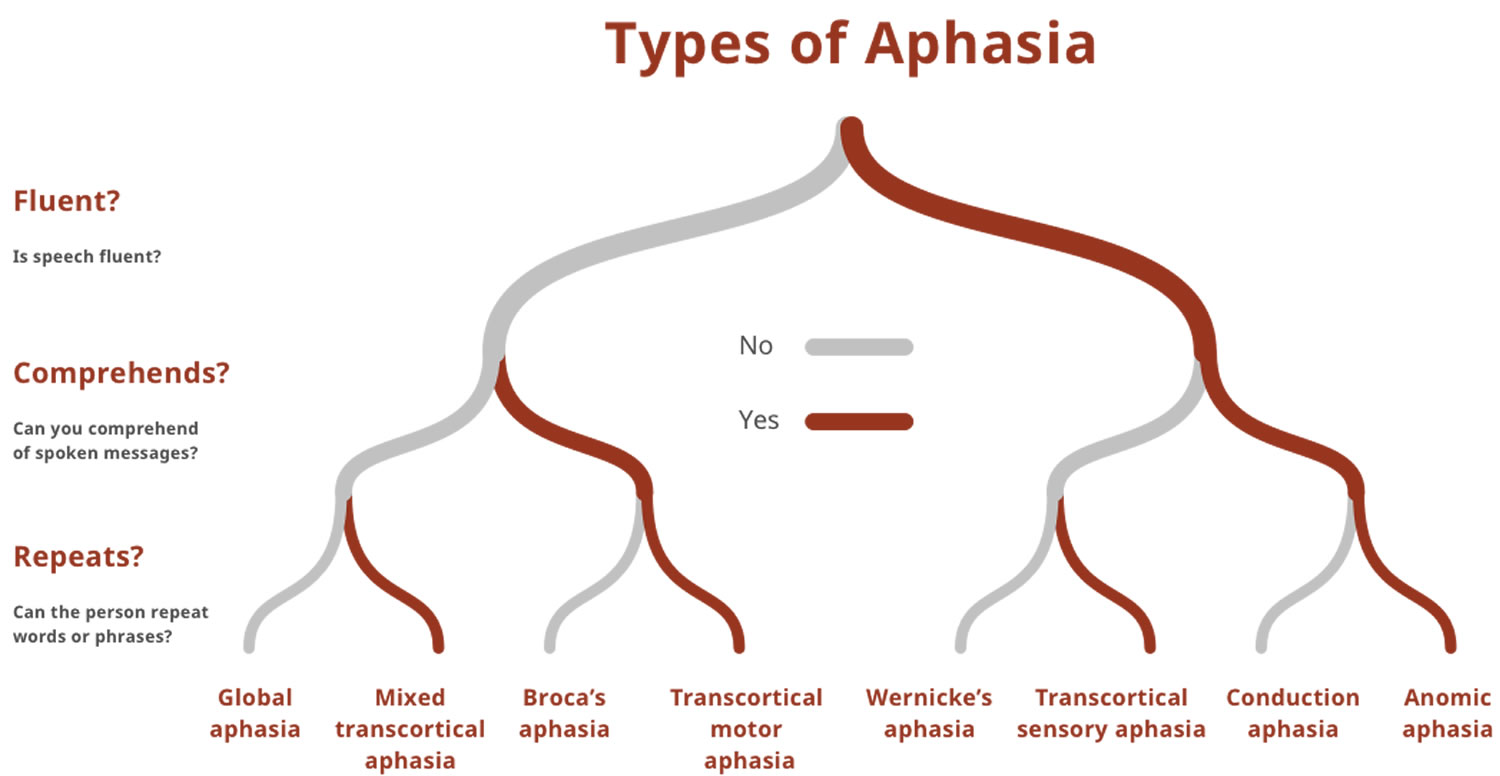
There are four main types of aphasia:
- Expressive aphasia – you know what you want to say, but you have trouble saying or writing what you mean
- Receptive aphasia – you hear the voice or see the print, but you can’t make sense of the words
- Anomic aphasia – you have trouble using the correct word for objects, places, or events.
- Global aphasia – you can’t speak, understand speech, read, or write
Your doctor may also refer to aphasia as nonfluent, fluent or global:
Nonfluent aphasia (Broca’s aphasia)
Individuals with Broca’s aphasia have trouble speaking fluently but their comprehension can be relatively preserved. This type of aphasia is also known as non-fluent or expressive aphasia. Broca’s aphasia is named after the French scientist, Paul Broca, who in 1861 first related a set of deficits associated with this type of aphasia to localized brain damage in a patient who could only say the word “tan”.
People with Broca’s aphasia struggle to get words out, speak in very short sentences and omit words. A person might say “Want food” or “Walk park today.” A listener can usually understand the meaning. People with Broca’s aphasia may understand what other people say better than they can speak. Producing the right sounds or finding the right words is often a laborious process. Some persons have more difficulty using verbs than using nouns. They’re often aware of their difficulty communicating and may get frustrated. People with Broca’s aphasia may also have right-sided paralysis or weakness.
A person with Broca’s aphasia may understand speech relatively well, particularly when the grammatical structure of the spoken language is simple. However they may have harder times understanding sentences with more complex grammatical construct. For example the sentence “Mary gave John balloons” may be easy to understand but “The balloons were given to John by Mary” may pose a challenge when interpreting the meaning of who gave the balloons to whom.
Individuals with this type of aphasia may be able to read but be limited in writing.
Broca’s aphasia results from injury to speech and language brain areas such the left hemisphere inferior frontal gyrus, among others. Such damage is often a result of stroke but may also occur due to brain trauma. Like in other types of aphasia, intellectual and cognitive capabilities not related to speech and language may be fully preserved.
Fluent aphasia (Wernicke’s aphasia)
In Wernicke’s aphasia the ability to grasp the meaning of spoken words and sentences is impaired, while the ease of producing connected speech is not very affected. Therefore Wernicke’s aphasia is also referred to as ‘fluent aphasia’ or ‘receptive aphasia’.
Wernicke’s aphasia and Wernicke’s area are named after the German neurologist Carl Wernicke who first related this specific type of speech deficit to a damage in a left posterior temporal area of the brain.
Reading and writing are often severely impaired. As in other forms of aphasia, individuals can have completely preserved intellectual and cognitive capabilities unrelated to speech and language.
Persons with Wernicke’s aphasia can produce many words and they often speak using grammatically correct sentences with normal rate and prosody. However, often what they say doesn’t make a lot of sense or they pepper their sentences with non-existent, incorrect or irrelevant words. They may fail to realize that they are using the wrong words or using a non-existent word and often they are not fully aware that what they say doesn’t make sense. They usually don’t understand spoken language well and often don’t realize that others can’t understand them.
Patients with this type of aphasia usually have profound language comprehension deficits, even for single words or simple sentences. This is because in Wernicke’s aphasia individuals have damage in brain areas that are important for processing the meaning of words and spoken language. Such damage includes left posterior temporal regions of the brain, which are part of what is knows as Wernicke’s area, hence the name of the aphasia.
Global aphasia
Global aphasia results from extensive damage to the brain’s language networks. Global Aphasia is caused by injuries to multiple language-processing areas of the brain, including those known as Wernicke’s and Broca’s areas. These brain areas are particularly important for understanding spoken language, accessing vocabulary, using grammar, and producing words and sentences. This is the most severe form of aphasia, and is applied to patients who can produce few recognizable words and understand little or no spoken language.
People with global aphasia have severe disabilities with expression and comprehension. Persons with Global Aphasia can neither read nor write. Like in other milder forms of aphasia, individuals with global aphasia can have fully preserved intellectual and cognitive capabilities unrelated to language and speech.
Global aphasia may often be seen immediately after the patient has suffered a stroke or a brain trauma. Symptoms may rapidly improve in the first few months after stroke if the damage has not been too extensive. However, with greater brain damage, severe and lasting disability may result. It is important to speak with your doctor about finding speech and language therapy as soon as possible after Global Aphasia has been diagnosed.
Mixed Non-fluent Aphasia
Mixed non-fluent aphasia applies to persons who have sparse and effortful speech, resembling severe Broca’s aphasia. However, unlike individuals with Broca’s aphasia, mixed non-fluent aphasia patients remain limited in their comprehension of speech, similar to people with Wernicke’s aphasia. Individuals with mixed non-fluent aphasia do not read or write beyond an elementary level.
Anomic Aphasia
Anomic aphasia is one of the milder forms of aphasia. The term is applied to persons who are left with a persistent inability to supply the words for the very things they want to talk about, particularly the significant nouns and verbs. Your speech is fluent and grammatically correct but it is full of vague words (such as ‘thing’) and circumlocutions (attempts to describe the word they are trying to find). The feeling is often that of having the word on the tip of one’s tongue, which results in their speech having lots of expressions of frustration. People with anomic aphasia understand speech well and they can repeat words and sentences. In most cases they can read adequately. Difficulty finding words is as evident in writing as it is in speech.
Other varieties
In addition to the foregoing syndromes that are seen repeatedly by speech clinicians, there are many other possible combinations of deficits that do not exactly fit into these categories.Some of the components of a complex aphasia syndrome may also occur in isolation. This may be the case for disorders of reading (alexia) or disorders affecting both reading and writing (alexia and agraphia), following a stroke. Severe impairments of calculation often accompany aphasia, yet in some instances patients retain excellent calculation in spite of the loss of language.
How Long Does it Take to Recover from Aphasia?
If the symptoms of aphasia last longer than two or three months after a stroke, a complete recovery is unlikely. However, it is important to note that some people continue to improve over a period of years and even decades. Improvement is a slow process that usually involves both helping the individual and family understand the nature of aphasia and learning compensatory strategies for communicating.
Some people recover from aphasia without treatment. Most, however, need language therapy as soon as possible.
Once the cause has been addressed, the main treatment for aphasia is speech and language therapy. The person with aphasia relearns and practices language skills and learns to use other ways to communicate. Family members often participate in the process, helping the person communicate.
Does Aphasia Affect a Person’s Intelligence?
NO. A person with aphasia may have difficulty retrieving words and names, but the person’s intelligence is basically intact. Aphasia is not like Alzheimer’s disease; for people with aphasia it is the ability to access ideas and thoughts through language – not the ideas and thoughts themselves- that is disrupted. But because people with aphasia have difficulty communicating, others often mistakenly assume they are mentally ill or have mental retardation.
Can people who have Aphasia return to their jobs?
Sometimes. Since most jobs require speech and language skills, aphasia can make some types of work difficult. Individuals with mild or even moderate aphasia are sometimes able to work, but they may have to change jobs.
Because aphasia is often a sign of a serious problem, such as a stroke, seek emergency medical care if you suddenly develop:
- Difficulty speaking
- Trouble understanding speech
- Difficulty with word recall
- Problems with reading or writing
Primary Progressive Aphasia
The syndrome of primary progressive aphasia has been defined by Mesulam and colleagues 1 as a progressive disorder of language, with preservation of other mental functions and of activities of daily living, for at least two years. Primary progressive aphasia is not Alzheimer’s disease. Most people with primary progressive aphasia maintain ability to take care of themselves, pursue hobbies, and, in some instances, remain employed. The problem is a disorder of language; and signs and symptoms of other clinical syndromes are not found through tests routinely used to determine the presence of other conditions.
Primary Progressive Aphasia also called progressive aphasia without dementia, is a rare neurological syndrome in which language capabilities become slowly and progressively impaired. Unlike other forms of aphasia that result from stroke or brain injury, primary progressive aphasia is caused by neurodegenerative diseases, such as Alzheimer’s Disease or Frontotemporal Lobar Degeneration. Primary Progressive Aphasia results from deterioration of brain tissue important for speech and language. Although the first symptoms are problems with speech and language, other problems associated with the underlying disease, such as memory loss, often occur later.
Primary Progressive Aphasia is a disorder of language; and signs and symptoms of other clinical syndromes are not found through tests routinely used to determine the presence of other conditions.
The type or pattern of the language disorder may differ from patient to patient. As with aphasia secondary to stroke, the manifestations of primary progressive aphasia depend on what parts of the left hemisphere are relatively more damaged at any given point in the illness. The initial language disturbance may be fluent aphasia (i.e., the person may have normal or even increased rate of word production) or non-fluent (it is an effort for the person to speak and he or she produces fewer words). The person with primary progressive aphasia may or may not have difficulty understanding speech. Eventually, almost all patients become mute
and unable to understand spoken or written language, even if their behavior seems otherwise normal.
The average age of onset is 60; most people with primary progressive aphasia are between the ages of about 40 to 80. Men are affected twice as often as women. About half of primary progressive aphasia patients have a family history of dementia in a parent or sibling, indicating the existence of a genetic component. Half of all people with primary progressive aphasia will eventually develop cognitive or behavioral problems consistent with a more pervasive dementia syndrome, such as Alzheimer’s disease or Fronto-Temporal-Limbic Dementia, after an average of five years. In other people, primary progressive aphasia may remain relatively isolated or even be the sole manifestation for as long as 15 years. In general, the longer the duration of aphasia as an isolated symptom, the less likely that other signs of dementia will develop.
Although primary progressive aphasia may take a number of forms, it commonly appears initially as a disorder of speaking (an articulatory problem), progressing to nearly total inability to speak in its most severe stage, while comprehension remains relatively preserved. A less common variety begins with impaired word finding and progressive deterioration of naming and comprehension, with relatively preserved articulation. However, other neurological disorders exist in which progressive deterioration of language is only one component of a broad, progressive decline of mental functions, including memory, attention, visuospatial skills, reasoning, and the carrying out of complex motor activities. These diseases, such as Alzheimer’s disease, Pick’s disease, and Creutzfeld Jakob disease, should be excluded by appropriate neurologic examinations, when a person experiences progressive language decline.
Primary Progressive Aphasia commonly begins as a subtle disorder of language, progressing to a nearly total inability to speak, in its most severe stage. The type or pattern of the language deficit may differ from patient to patient. The initial language disturbance may be fluent aphasia (i.e., the person may have normal or even increased rate of word production) or non-fluent aphasia (speech becomes effortful and the person produces fewer words). A less common variety begins with impaired word-finding and progressive deterioration of naming and comprehension, with relatively preserved articulation.
As with aphasia that results from stroke or brain trauma, the manifestations of primary progressive aphasia depend on what parts of the left hemisphere are relatively more damaged at any given point in the illness. The person may or may not have difficulty understanding speech. Eventually, almost all patients become mute and unable to understand spoken or written language, even if their behavior seems otherwise normal.
Signs and symptoms of other clinical syndromes are not found through tests used to determine the presence of other conditions. Primary Progressive Aphasia is not Alzheimer’s disease. Most people with primary progressive aphasia maintain ability to take care of themselves, pursue hobbies, and, in some instances, remain employed.
Is there any treatment or assistance for people with primary progressive aphasia?
People with primary progressive aphasia are fighting against a condition in which they will continue to lose their ability to speak, read, write, and/or understand what they hear. Usually people with aphasia that results from stroke or head injury will experience improvement over time, often aided by speech therapy. This is not the case for people with primary progressive aphasia. However, individuals with primary progressive aphasia may benefit during the course of their illness by acquiring new communication strategies from speech-language pathologists. Some families have also learned new strategies through participation in Aphasia Community Groups.
Many people with aphasia find it helpful to carry identification cards and other materials that can help explain the person’s condition to others. ID cards are available from the the National Aphasia Association website 2. Some communication-assistive devices may also be helpful. Non-verbal techniques for communicating, such as gesturing and pointing to pictures, may help people with primary progressive aphasia express themselves.
Primary progressive aphasia diagnosis
As with other “degenerative” brain diseases, including Alzheimer’s disease, there are no totally reliable non-invasive diagnostic tests for primary progressive aphasia. Whether or not the aphasia is “pure”, that is, unaccompanied by other cognitive impairments, may in some cases be difficult to establish through psychological assessments because aphasia can affect performance on “non-language “ (e.g., memory) portions of the test. CT scans, MRI, EEG (electroencephalography) often suggest left hemispheric damage, but these tests may also be normal even though the person has primary progressive aphasia. “Metabolic” imaging studies such as single photon emission computed tomography (SPECT), positron emission tomography (PET), and Functional MRI indicate left hemispheric dysfunction when a person has primary progressive aphasia, but other disorders with different symptoms may also cause the same radiologic
abnormalities.
The cause of primary progressive aphasia and other degenerative brain disorders is unknown. A variety of brain abnormalities in people with primary progressive aphasia have been seen during autopsies. These abnormalities have involved the left hemisphere either exclusively or to a much greater extent than the right hemisphere. Most often, brain abnormalities are consistent with Fronto-Temporal-Limbic Dementia, itself a syndrome — not a single disease — with variable symptoms and microscopic abnormalities. Although Fronto-Temporal-Limbic Dementia is usually associated initially with progressive changes in personality, sometimes it presents as primary progressive aphasia, personality deterioration occurring years later. Alzheimer’s disease has been proven the cause of primary progressive aphasia in a minority of patients. People with primary progressive aphasia due to Alzheimer’s disease usually have fluent aphasia.
Primary Progressive Aphasia Treatment
There is currently no cure for primary progressive aphasia.
The primary approaches to managing primary progressive aphasia at this time are behavioral. That is, there are things that the person with primary progressive aphasia can do that may lessen the impact of the disease. Behavioral approaches emphasize practice, drill, and counseling to (1) enhance the ability to communicate, or (2) compensate for the inability to communicate in conventional ways.
Some behavioral approaches for primary progressive aphasia are directed at improving or maintaining (in the short term) impaired language abilities. The decision to pursue this type of therapy should take into account the following considerations. First, the person with primary progressive aphasia must still have some capacity for insight, motivation and learning. Without them the possibility of meaningful improvement is greatly reduced. Also, the individual’s significant others must be motivated and involved as well. They play an important role in working on practice activities beyond formal therapy sessions and in providing cues for using effective communication strategies.
Finally, everyone involved must understand that therapy will not eliminate difficulties with communication. Even if there is improvement in communication ability, it will not reverse the progression of the disease.
The skills targeted for therapy are generally based on three factors: those abilities that are declining, those that may be relatively preserved, and those that are most important to the affected person. In all instances, therapy requires work that might be called “focused exercise of the brain’s language system.”
At this time a small number of reports all of which are based on only one person or a few carefully selected people with primary progressive aphasia – have documented improvements in abilities targeted by therapy. Skills that have improved include comprehension of spoken instructions and questions, production of sentences, retrieval of words, and number reading. It is premature to conclude that such treatments are likely to be effective for many people with primary progressive aphasia. However, these reports do suggest that for some affected individuals, and for some deficits, therapy may be beneficial. Whether these benefits continue beyond the period of formal therapy is not known.
Compensatory Strategies for both Patients and Families
Other behavioral approaches emphasize compensatory strategies that can improve communication, although not necessarily in conventional ways. Compensatory strategies can be “patient-oriented” or “other-oriented,” or a combination of both. Patient-oriented strategies reflect things that the person with primary progressive aphasia can do to enhance communication, such as establishing the topic at the outset of a conversation, using gestures, and using pictures, writing or drawing. “Other-oriented” strategies include paying full attention to the affected person, giving feedback about the need for clarification, providing more time for communication, confirming information, keeping statements relatively brief, and supplementing speech with gestures. Joint efforts on the part of both the person with primary progressive aphasia and others include speaking in environments that are conducive to effective communication (such as face-to-face conversations with minimal noise and other distractions). People with primary progressive aphasia and their significant others often benefit from following the rule that communicating requires everyone’s full attention. The notion that people with primary progressive aphasia require all the fuel in their “language tank” when communicating is a useful analogy and one to keep in mind when engaged in speaking, listening, reading or writing activities.
It can be very helpful to consult with a speech-language pathologist to identify important communication needs, learn how and when compensatory strategies can best be used, and practice their use. The speech-language pathologist can help to identify specific strategies and investigate whether augmentative strategies (for example, gesture, pantomime, and drawing) may supplement or sometimes replace verbal communication. Such strategies have been reported as helpful in some people with primary progressive aphasia.
Electronic/computer devices may be able to supplement or replace speech in some people with primary progressive aphasia. Because they require a person to use conventional language or other symbols, they may not be helpful for those whose language skills are already severely impaired. Some people with primary progressive aphasia also have an apraxia of speech a problem with the programming of movements for speech rather than a language problem). They may have speech that is far more impaired than their language comprehension or ability to read and write. As long as their ability to control movements of body parts needed to use the devices is relatively intact, those with apraxia of speech and relatively mild primary progressive aphasia may be good candidates for electronic/computer alternatives to speech. Generally, the development, practice and learning of augmentative or alternative means of communication should occur well before there is an actual need to use them, so they are readily available and more easily used when and if the need emerges.
Finally, there can be little doubt that simply learning about primary progressive aphasia is beneficial, both psychologically and practically. As discussed above, speech-language pathologists who have experience working with people with aphasia and degenerative neurological diseases can address questions about aphasia in general, and primary progressive aphasia in particular, and can help plan for future communication needs. Free or low-cost evaluations and therapy may be available from university speech language clinics. Some primary progressive aphasia patients and/or spouses benefit from joining an Aphasia Community Group or Stroke Support Group 3 that has others with aphasia in it. This is true even if the others do not have aphasia that is progressive. The National Aphasia Association 2 provides information about primary progressive aphasia and listings of support groups. The American Heart Association resources can make referrals to stroke support groups 4.
Viewed in the most positive sense, the diagnosis of primary progressive aphasia does not mean the end of communication. It can be the first step to identifying ways to maintain communication abilities for as long as possible.
Medications
From the medical perspective, there are currently no drugs or other interventions specifically designed for primary progressive aphasia. This partly reflects doctors limited understanding of what causes primary progressive aphasia and the likelihood that it has more than a single cause. Neurologists sometimes prescribe drugs that are used for people with Alzheimer’s disease under the assumption that primary progressive aphasia and Alzheimer’s disease may share a common cause. This assumption is unlikely to be true in the majority of cases. Currently, there are only anecdotal reports that the same drugs that target Alzheimer’s disease are helpful in relieving the signs and symptoms of primary progressive aphasia.
Aphasia prognosis
The outcome of aphasia is difficult to predict given the wide range of variability of the condition. Generally, people who are younger or have less extensive brain damage fare better. The location of the injury is also important and is another clue to prognosis. In general, people tend to recover skills in language comprehension more completely than those skills involving expression.
Aphasia complications
Aphasia can create numerous quality-of-life problems because communication is so much a part of your life. Communication difficulty may affect your:
- Job
- Relationships
- Day-to-day function
Language barriers may lead to embarrassment, depression, anxiety and relationship problems.
If you’re concerned about someone with aphasia, encourage them to discuss any problems with their doctor or a member of their care team to access the relevant support.
If the person is unable to do this themselves, they may require someone to communicate on their behalf.
Aphasia causes
Aphasia is the result of damage to the parts of the brain involved in speaking, reading, writing and understanding others.
Any damage to the language areas of the brain can result in loss of function, leading to aphasia.
The severity of a person’s aphasia depends on the location and type of injury sustained by the brain.
Aphasia can occur by itself or alongside other disorders, such as visual difficulties, mobility problems, limb weakness and cognitive changes.
Aphasia affects a person’s language, but it doesn’t affect a person’s intelligence.
Common causes include:
- Stroke – thought to be the most common cause, around one in three people experience some degree of aphasia after having a stroke
- Severe head injury
- Brain tumor
- Progressive neurological conditions – conditions that, over time, cause progressive brain and nervous system damage e.g. dementia, progressive supranuclear palsy or corticobasal degeneration
- Infections that affect the brain – such as meningitis (an infection of the outer layer of the brain) and encephalitis (an infection of the brain itself), although this is a much rarer cause of aphasia
The most common cause of aphasia is brain damage resulting from a stroke (about 25-40% of stroke survivors acquire aphasia) — the blockage or rupture of a blood vessel in the brain. Loss of blood to the brain leads to brain cell death or damage in areas that control language.
Brain damage caused by a severe head injury, a tumor, an infection or a degenerative process also can cause aphasia. In these cases, the aphasia usually occurs with other types of cognitive problems, such as memory problems or confusion.
Primary progressive aphasia is the term used for language difficulty that develops gradually. This is due to the gradual degeneration of brain cells located in the language networks. Sometimes this type of aphasia will progress to a more generalized dementia.
Sometimes temporary episodes of aphasia can occur. These can be due to migraines, seizures or a transient ischemic attack (TIA). A TIA occurs when blood flow is temporarily blocked to an area of the brain. People who’ve had a transient ischemic attack (TIA) are at an increased risk of having a stroke in the near future.
Aphasia symptoms
Aphasia is a sign of some other condition, such as a stroke or a brain tumor.
In cases where aphasia has been caused by a sudden brain injury, such as a stroke or a severe head injury, symptoms will usually develop straight after the injury.
In cases where there is gradual damage to the brain as a result of a condition that gets worse over time, such as dementia or a brain tumour, the symptoms may develop gradually.
A person with aphasia may:
- Speak in short or incomplete sentences
- Speak in sentences that don’t make sense
- Substitute one word for another or one sound for another
- Speak unrecognizable words
- Not understand other people’s conversation
- Write sentences that don’t make sense
The severity and scope of the problems depend on the extent of damage and the area of the brain affected.
Expressive aphasia
Someone with expressive aphasia experiences difficulty communicating their thoughts, ideas and messages to others.
This may affect speech, writing, gestures or drawing, and causes problems with everyday tasks such as using the telephone, writing an email, or speaking to family and friends.
People with expressive aphasia may have some of the following signs and symptoms:
- slow and halting speech
- they may struggle to get certain words out, such as the names of objects, places or people
- the content of their speech is stripped down to simple elements and only contains basic nouns and verbs – for example, “want drink” or “go town today”
- spelling or grammatical errors
- using the wrong word, such as saying “chair” instead of “table”
- difficulty constructing a sentence
- being able to write or speak fluently, using long sentences, but often including nonsense words or their speech lacks meaning
Receptive aphasia
A person with receptive aphasia experiences difficulty understanding things they hear or read. They may also have difficulty interpreting gestures, drawings, numbers and pictures.
This can affect everyday activities such as reading an email, managing finances, having conversations, listening to the radio, or following TV programmes.
People with receptive aphasia may have some of the following signs and symptoms:
- difficulty understanding what people say
- difficulty understanding written words
- misinterpreting the meaning of words, gestures, pictures or drawings
- giving responses that may not make sense if they’ve misunderstood questions or comments
- not being aware of their difficulties with understanding
Primary progressive aphasia
This type of aphasia occurs in people with a specific type of dementia. As it’s a primary progressive condition, the symptoms get worse over time.
Usually, the first problem people with primary progressive aphasia (primary progressive aphasia) notice is difficulty finding the right word or remembering somebody’s name.
The problems gradually get worse and can include:
- speech becoming hesitant and difficult, and making mistakes with the sounds of words or grammar
- speech becomes slow with short, simple sentences
- forgetting the meaning of complicated words, and later also simple ones, making it more difficult for them to understand other people
- speech becomes more vague, and the person has difficulty being specific or clarifying what they’re saying
- becoming less and less likely to join in with or start conversations
A person with primary progressive aphasia may also experience other symptoms later in their illness, including changes in their personality and behaviour, difficulties with memory and thinking similar to Alzheimer’s disease, or difficulties with movement similar to Parkinson’s disease.
Can a person have Aphasia without having a physical disability?
Yes, but many people with aphasia also have weakness or paralysis of their right leg and right arm. When a person acquires aphasia it is usually due to damage on the left side of the brain, which controls movements on the right side of the body.
Aphasia diagnosis
Your speech and language therapist will likely give you a physical and a neurological exam, test your strength, feeling and reflexes, and listen to your heart and the vessels in your neck. He or she will likely request an imaging test, usually an MRI scan, to quickly identify what’s causing the aphasia.
You’ll also likely undergo tests and informal observations to assess your language skills, such as the ability to:
- Name common objects
- Engage in a conversation
- Understand and use words correctly
- Answer questions about something read or heard
- Repeat words and sentences
- Follow instructions
- Answer yes-no questions and respond to open-ended questions about common subjects
- Read and write.
Aphasia treatment
If the brain damage is mild, a person may recover language skills without treatment. However, most people undergo speech and language therapy to rehabilitate their language skills and supplement their communication experiences. Researchers are currently investigating the use of medications, alone or in combination with speech therapy, to help people with aphasia.
A speech and language therapist usually diagnoses the condition by testing your language capabilities. They can also help arrange treatment.
Speech and language therapy is the main type of treatment for people with aphasia. This aims to help restore some of your ability to communicate, as well as help you develop alternative ways of communicating, if necessary.
You may receive speech and language therapy on an individual basis or in a group, depending on your needs and the service provided.
An increasing number of computer-based applications are available to support people with aphasia. However, it’s important to start using these with the assistance of a speech and language therapist.
How successful treatment is differs from person to person, but most people with aphasia make some degree of recovery, and some recover fully. Even if aphasia persists, it does not mean a person is unable to live an independent and meaningful life.
However, the chances of recovery for people with aphasia related to progressive neurological conditions is poor. This is because there is no way of repairing or preventing the ongoing injury to the brain.
When aphasia is caused by a progressive condition, treatment focuses on making the most of what people can still do and developing other ways of communicating to prepare for a time when speaking will be more difficult.
Speech and language rehabilitation
Recovery of language skills is usually a relatively slow process. Although most people make significant progress, few people regain full pre-injury communication levels.
For aphasia, speech and language therapy tries to improve the person’s ability to communicate by restoring as much language as possible, teaching how to compensate for lost language skills and finding other methods of communicating.
Evidence suggests speech and language therapy is more effective if it’s started as soon as possible.
For many people, the most obvious recovery happens in the first six months. However, improvements can continue to be seen for much longer after this, even many years later.
How the therapy is carried out will depend on your circumstances. An intensive course of speech and language therapy may be recommended for some people. This involves a number of sessions spread out over a shorter period of time.
However, speech and language therapy can be exhausting, and an intensive course of treatment will not be suitable for everyone. For some people, shorter and less intensive sessions may be recommended.
Therapy may be individual sessions, groups, or using technology such as computer programmes or apps.
Therapy:
- Starts early. Some studies have found that therapy is most effective when it begins soon after the brain injury.
- Often works in groups. In a group setting, people with aphasia can try out their communication skills in a safe environment. Participants can practice initiating conversations, speaking in turn, clarifying misunderstandings and fixing conversations that have completely broken down.
- May include use of computers. Using computer-assisted therapy can be especially helpful for relearning verbs and word sounds (phonemes).
Speech and language therapy techniques
The specific techniques used and the aims of the treatment will depend on each person’s circumstances. Some examples are described below.
If you have difficulty understanding words, your speech and language therapist may ask you to carry out tasks such as matching words to pictures or sorting words by their meaning.
The aim of these tasks is to improve your ability to remember meanings and link them with other words.
If you have difficulty expressing yourself, your speech and language therapist may ask you to practise naming pictures or judge whether certain words rhyme. They may also ask you to repeat words that they say, with prompting if necessary.
If you are able to complete tasks with single words, your therapist will work on your ability to construct sentences.
Some techniques may involve working with a computer. Other methods may include group therapy with other people with aphasia, or working with family members.
This will allow you to practise conversational skills or rehearse common situations, such as making a telephone call.
An increasing number of computer-based programmes and apps are available to help people with aphasia improve their language abilities.
However, it’s important to start using these alongside a speech and language therapist.
Alternative methods of communication
An important part of speech therapy is finding different ways for you to communicate. Your therapist will help you develop alternatives to talking, such as using gesture, writing, drawing or communication charts.
Communication charts are large grids containing letters, words or pictures. They allow someone with aphasia to communicate by pointing at the word or letter to indicate what they want to say.
For some people, specially designed electronic devices, such as voice output communication aids (VOCAs), may be useful. Voice output communication aids use a computer-generated voice to play messages aloud.
This can help if you have difficulty speaking but are able to write or type. There are also apps available on smartphones and computer tablets that can do this.
If a communication device is felt to be beneficial, funding for the purchase of an individual device can be discussed with a speech and language therapist.
Constraint-induced therapies (CIT) have received a good deal of attention in the popular press recently.
An early researcher, Dr. Edward Taub, examined the notion that much of the long-term disability of stroke survivors resulted from a learned tendency to avoid using the impaired arm and hand, instead of focusing on compensating by using the remaining good limb. Taub proposed the term “learned non-use” to describe this process by which the survivor increasingly avoids using the impaired limb and is thus unable to capitalize on the value this limb might offer.
Principles of constraint-induced therapies (CIT)
Based on this theory, Dr. Taub developed a set of treatment principles designed to counteract learned non-use and enhance the underlying residual abilities of the impaired limb. There were three treatment principles:
- Constraint – avoid the compensation, in this case, by tying down the good limb (paw) of the animals he studied;
- Forced use – require use of the impaired limb by placing the animals in circumstances where they needed to use it to achieve a meaningful goal (for example, acquiring food pellets); and
- Massed practice – require the constraint and forced use every day and all day long.
In the last decade, Dr. Taub and many others have applied these three principles to humans. Results of these experiments suggest constraint-induced therapies (CIT) is helpful in some cases. Emerging results of a randomized controlled trial by Dr. Steve Wolf of Emory University and others endorse the value of this approach at least with regard to arm rehabilitation.
Constraint-induced therapies (CIT) and aphasia
Recently these same constraint-induced therapies (CIT) principles have been applied to aphasia rehabilitation. In speech therapy, constraint means avoiding the use of compensatory strategies such as gesturing, drawing, writing, etc. Forced use means communicating only by talking; and massed practice refers to therapy occurring 2–4 hours per day.
The activities used in applying CIT principles to aphasia rehabilitation don’t differ substantially from what might be found in more traditional treatment approaches. However, what does differ are the demands placed on the speaker in the context of relevant, communicative exchange.
Preliminary investigations suggest that constraint-induced therapies (CIT) principles may be effective in aphasia rehabilitation. However, this investigation is only beginning, and scientists are not able to say any more about its efficacy than that in some cases it appears to be helpful. Not only will further study be needed to confirm that CIT is effective with aphasia, these same studies are needed to confirm its safety. For example, some of the animal work by Dr. Tim Shallart and colleagues suggested that intensive CIT may be harmful when performed too early after a stroke. Thus the application of CIT to aphasia rehabilitation must be pursued with both enthusiasm and caution.
Evaluating new treatment approaches
Whenever a new intervention or approach to rehabilitation is considered, it is best to gather as much information as possible. Before beginning any rehabilitation program, you should determine that the provider is qualified, informed and experienced. However, when considering a product or program that is new or experimental, such as CIT applied to aphasia rehabilitation, it is equally important to evaluate how the program is portrayed and the evidence that supports it. Testimonials on promotional materials and uncontrolled case reports are considered the lowest level of evidence and should be supported by research published in professional journals.
Research is currently being carried out to study whether other treatments can benefit people with aphasia.
These include:
- medication – such as piracetam, bifemelane, piribedil, bromocriptine and idebenone
- transcranial magnetic stimulation – where an electromagnet placed on the scalp is stimulated for a short time using an electric current to stimulate parts of the brain affected by aphasia
Although some studies have suggested these treatments may benefit some people with aphasia, further research is necessary.
Medications
Certain drugs are currently being studied for the treatment of aphasia. These include drugs that may improve blood flow to the brain, enhance the brain’s recovery ability or help replace depleted chemicals in the brain (neurotransmitters). Several medications, such as memantine (Namenda) and piracetam, have shown promise in small studies. But more research is needed before these treatments can be recommended.
Coping and support
People with aphasia
If you have aphasia, the following tips may help you communicate with others:
- Carry a card explaining that you have aphasia and what aphasia is.
- Carry identification and information on how to contact significant others.
- Carry a pencil and a small pad of paper with you at all times.
- Use drawings, diagrams or photos as shortcuts.
- Use gestures or point to objects.
Family and friends
Family members and friends can use the following tips when communicating with a person with aphasia:
- Simplify your sentences and slow your pace.
- Ask yes/no questions.
- Paraphrase periodically during conversation.
- Modify the length and complexity of conversations.
- Use gestures to emphasize important points.
- Establish a topic before beginning conversation.
- Keep conversations one-on-one initially.
- Allow the person time to talk.
- Don’t finish sentences or correct errors.
- Reduce distracting noise in the environment. Practice conversation in a quiet, distraction-free environment.
- Keep paper and pencils or pens available.
- Write a key word or a short sentence to help explain something.
- Help the person with aphasia create a book of words, pictures and photos to assist with conversations.
- Use drawings or gestures when you aren’t understood.
- Involve the person with aphasia in conversations as much as possible.
- Check for comprehension or summarize what you’ve discussed.
Communication Strategies: Some Dos and Don’ts
The impact of aphasia on relationships may be profound, or only slight. No two people with aphasia are alike with respect to severity, former speech and language skills, or personality. But in all cases it is essential for the person to communicate as successfully as possible from the very beginning of the recovery process.
Here are some suggestions to help communicate with a person with aphasia:
- Make sure you have the person’s attention before you start.
- Minimize or eliminate background noise (TV, radio, other people).
- Keep your own voice at a normal level, unless the person has indicated otherwise.
- Keep communication simple, but adult. Simplify your own sentence structure and reduce your rate of speech. Emphasize key words. Don’t “talk down” to the person with aphasia.
- Give them time to speak. Resist the urge to finish sentences or offer words.
- Communicate with drawings, gestures, writing and facial expressions in addition to speech.
- Confirm that you are communicating successfully with “yes” and “no” questions.
- Praise all attempts to speak and downplay any errors. Avoid insisting that that each word be produced perfectly.
- Engage in normal activities whenever possible. Do not shield people with aphasia from family or ignore them in a group conversation. Rather, try to involve them in family decision-making as much as possible. Keep them informed of events but avoid burdening them with day to day details.
- Encourage independence and avoid being overprotective.
Support groups
Local chapters of such organizations as the National Aphasia Association 2, the American Stroke Association, the American Heart Association and some medical centers may offer support groups for people with aphasia and others affected by the disorder. These groups provide people with a sense of community, a place to air frustrations and learn coping strategies. Ask your doctor or speech-language pathologist if he or she knows of any local support groups.