Contents
- What is cholecystitis
- The Gallbladder
- Acute cholecystitis
- Chronic cholecystitis
- Cholecystitis causes
- Cholecystitis prevention
- Cholecystitis signs and symptoms
- Cholecystitis complications
- Cholecystitis diagnosis
- Cholecystitis treatment
- Cholestasis of pregnancy
- What are the risks of intrahepatic cholestasis of pregnancy in pregnancy?
- Intrahepatic cholestasis of pregnancy causes
- Does intrahepatic cholestasis of pregnancy go away after giving birth?
- Intrahepatic cholestasis of pregnancy symptoms
- Intrahepatic cholestasis of pregnancy diagnosis
- Intrahepatic cholestasis of pregnancy treatment
What is cholecystitis
Cholecystitis is the inflammation of the gallbladder. It occurs mostly as a complication of gallstones.
Gallstones are very common – affecting 10-20% of the population. It is difficult to determine exactly what the incidence of cholecystitis is, but studies have shown that patients with gallstones have a 1% per year incidence of severe events (cholecystitis, obstructive jaundice or biliary pancreatitis).
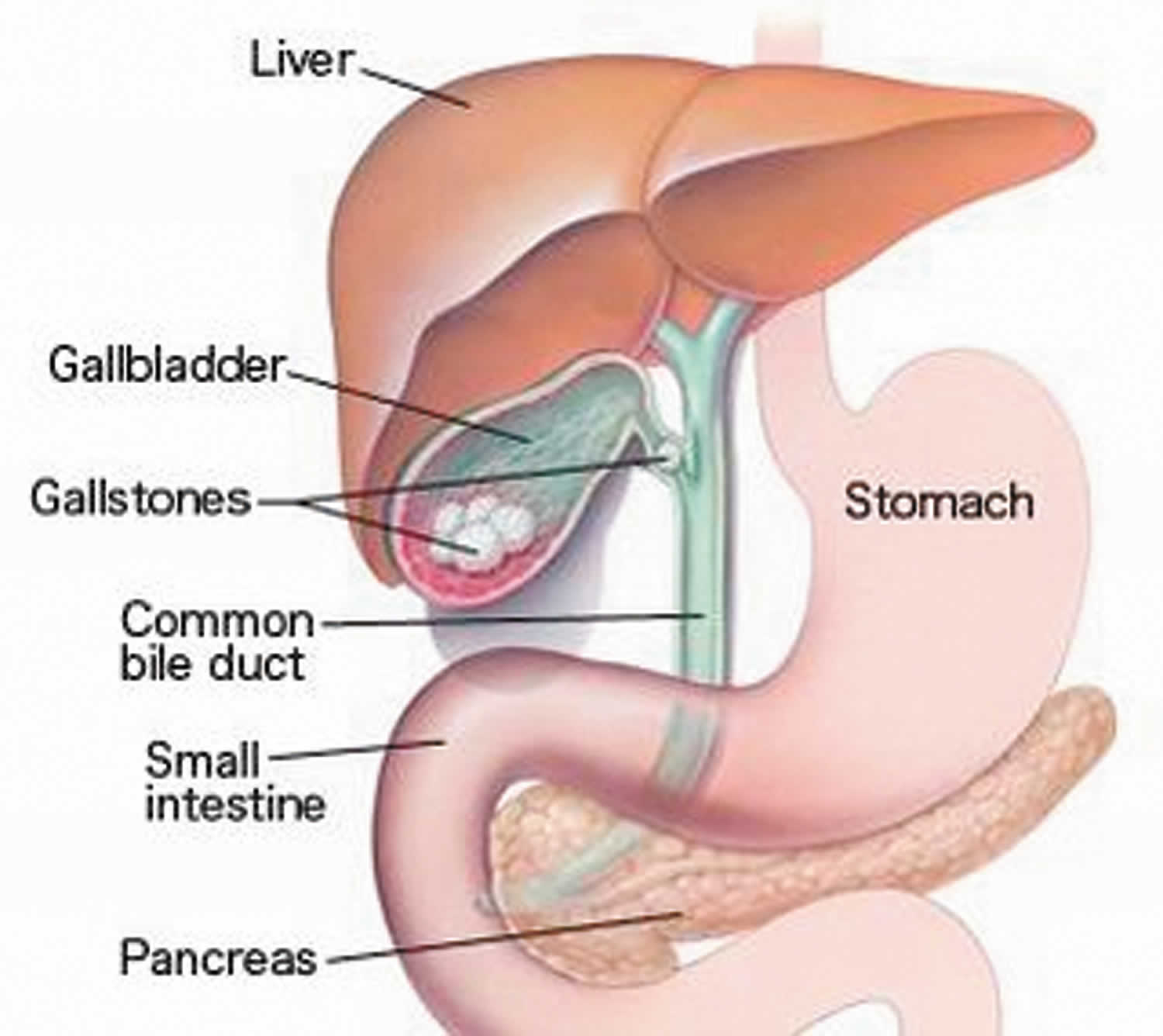
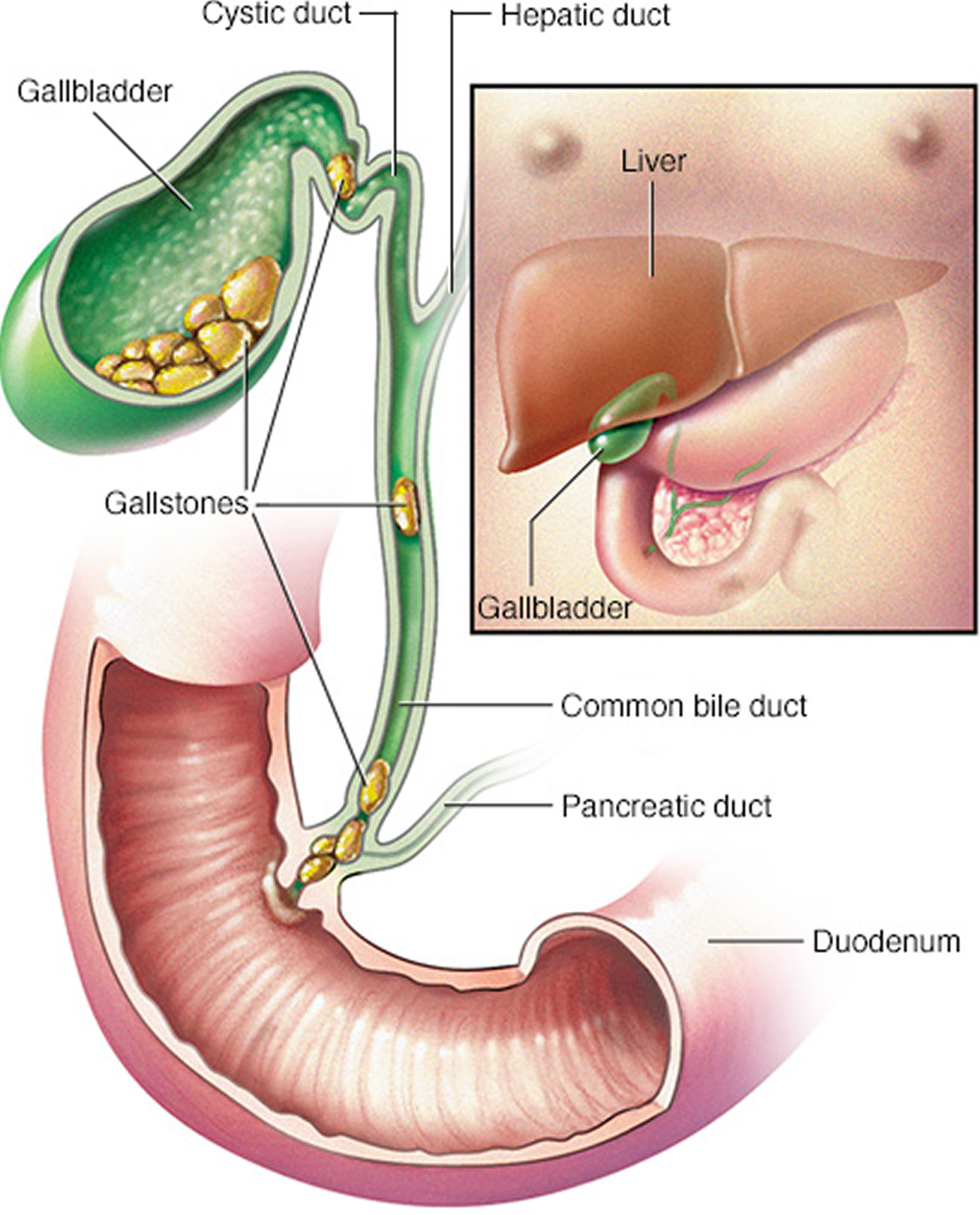
Your gallbladder is a small, pear-shaped organ on the right side of your abdomen, beneath your liver. The gallbladder holds a digestive fluid that’s released into your small intestine (bile) (see Figures 1 to 4).
In most cases, gallstones blocking the tube leading out of your gallbladder cause cholecystitis (see Figure 5). This results in a bile buildup that can cause inflammation. Other causes of cholecystitis include bile duct problems, tumors, serious illness and certain infections.
If left untreated, cholecystitis can lead to serious, sometimes life-threatening complications, such as a gallbladder rupture. Treatment for cholecystitis often involves gallbladder removal.
See your health care provider if:
- Severe belly pain does not go away
- Symptoms of cholecystitis return
Make an appointment with your doctor if you have worrisome signs or symptoms. If your abdominal pain is so severe that you can’t sit still or get comfortable, have someone drive you to the emergency room.
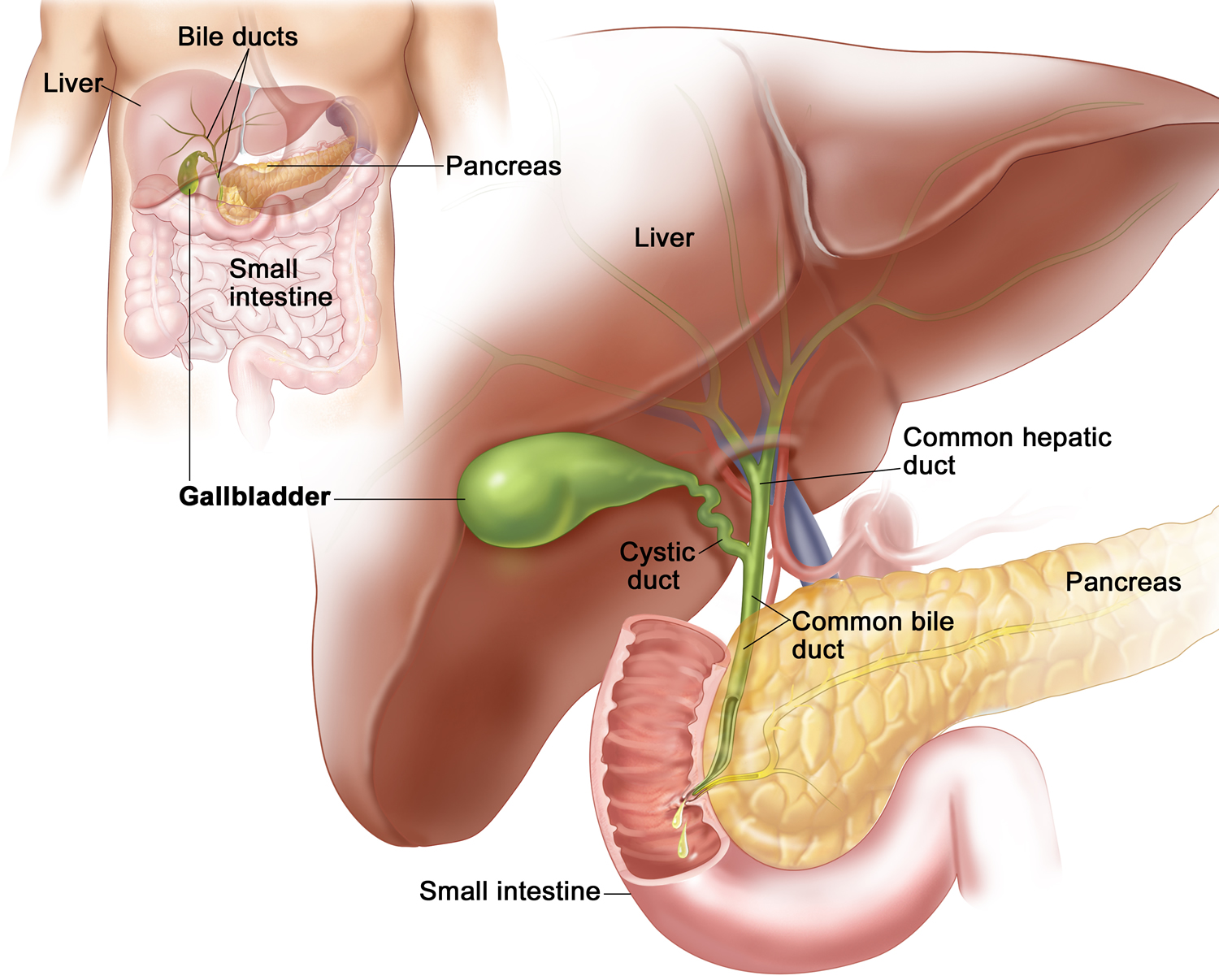
The Gallbladder
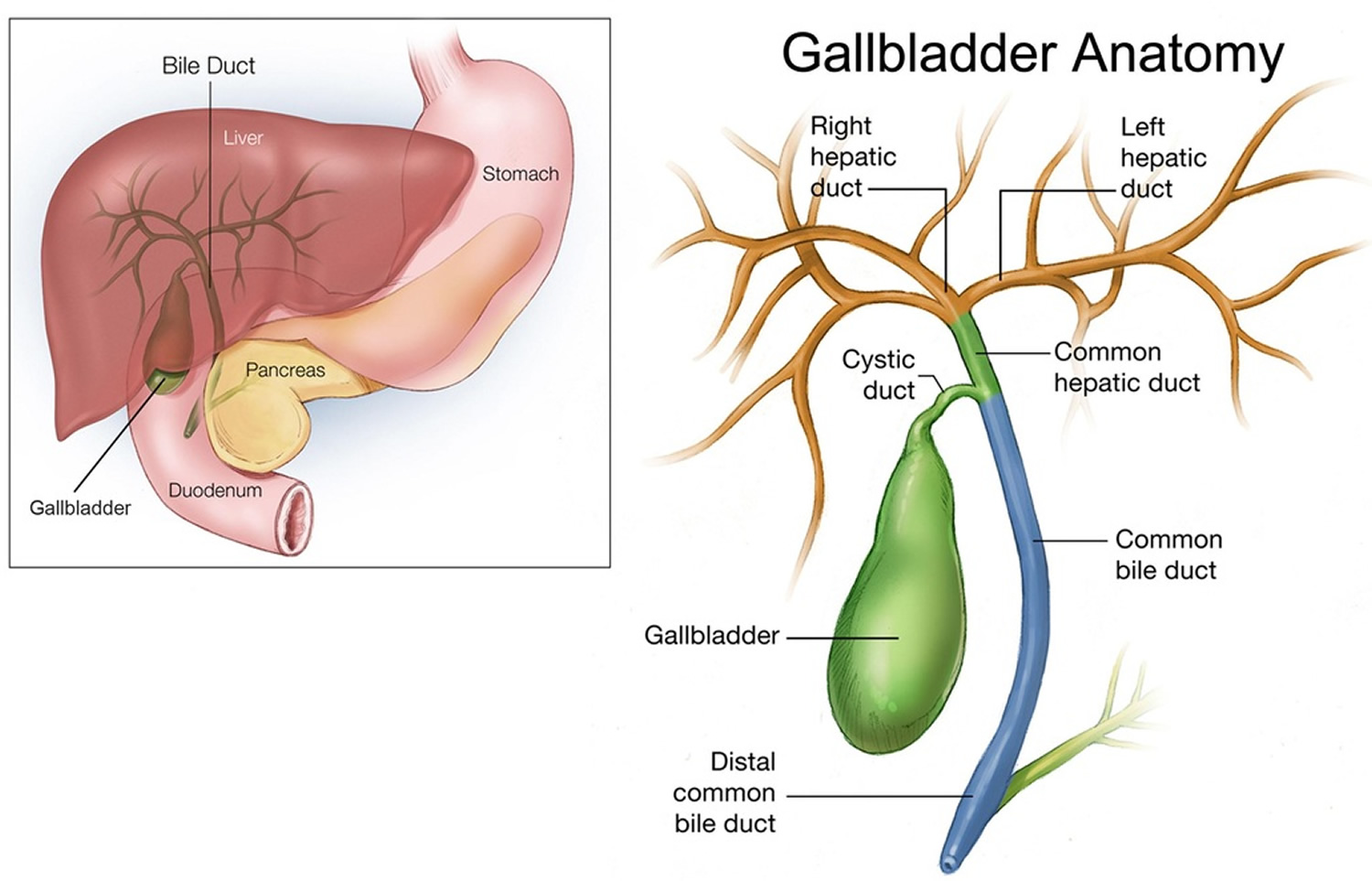
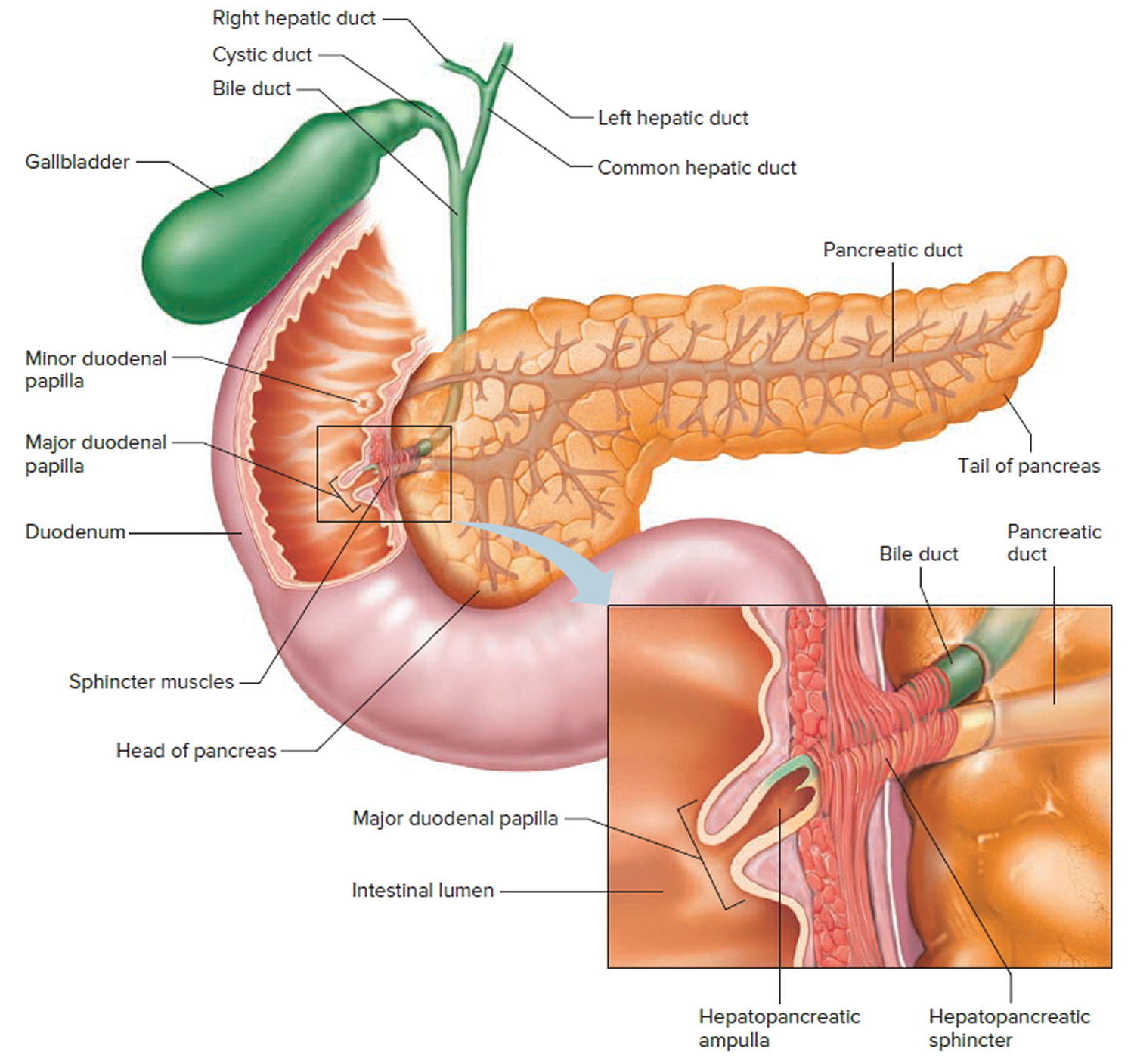
The gallbladder is a pear-shaped sac in a depression on the liver’s under surface. The gallbladder is lined with epithelial cells and has a strong layer of smooth muscle in its wall. The gallbladder stores bile between meals, reabsorbs water to concentrate bile, and contracts to release bile into the small intestine. It connects to the cystic duct, which in turn joins the common hepatic duct (Figure 2).
The common hepatic duct and cystic duct join to form the bile duct (common bile duct). It leads to the duodenum where the hepatopancreatic sphincter guards its exit (Figure 3). Because this sphincter normally remains contracted, bile collects in the bile duct. It backs up into the cystic duct and flows into the gallbladder, where it is stored.
Cholesterol in bile may precipitate under certain conditions and form crystals called gallstones. Gallstones in the bile duct may block bile flow into the small intestine and cause considerable pain. A surgical procedure called a cholecystectomy can remove the gallbladder when gallstones are obstructive. The surgery can often be done with a laparoscope (small, lit probe) on an outpatient basis.
Figure 1. Gallbladder location
Figure 2. Gallbladder anatomy
Figure 3. The common bile duct is closely associated with the pancreatic duct and the duodenum
 Gallbladder function
Gallbladder function
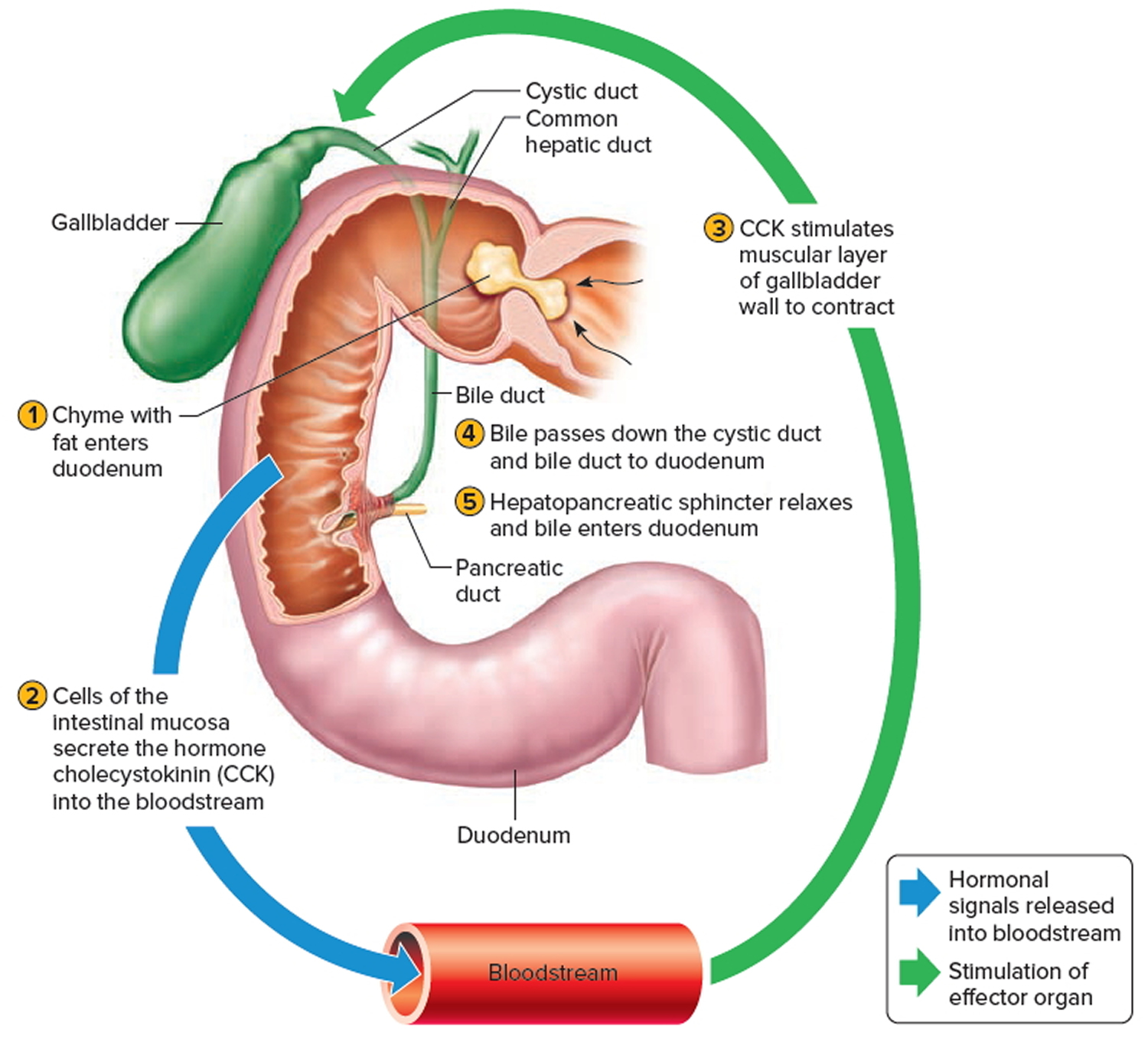
Following a meal, the mixing movements of the stomach wall aid in producing a semifluid paste of food particles and gastric juice called chyme.
As chyme enters the duodenum (the proximal portion of the small intestine), accessory organs—the pancreas, liver, and gallbladder—add their secretions.
Bile is a yellowish-green liquid continuously secreted from hepatic (liver) cells. In addition to water, bile contains bile salts, bile pigments (bilirubin and biliverdin), cholesterol, and electrolytes. Of these, bile salts are the most abundant and are the only bile components that have a digestive function.
Bile pigments are breakdown products of hemoglobin from red blood cells and are normally secreted in the bile.
Normally bile does not enter the duodenum until cholecystokinin stimulates the gallbladder to contract. Proteins and fats in chyme in the duodenum stimulate
the intestinal wall to release cholecystokinin. Cholecystokinin travels via the bloodstream to the pancreas also, where it stimulate the pancreas to release its pancreatic juice that has a high concentration of digestive enzymes.
The hepatopancreatic sphincter usually remains contracted until a peristaltic wave in the duodenal wall approaches it. Then the sphincter relaxes, and bile is squirted into the duodenum (see Figure 4).
Note: Cholecystokinin produced by the intestinal wall cells, in response to proteins and fats in the small intestine, decreases secretory activity of gastric glands and inhibits gastric motility; stimulates pancreas to secrete fluid with a high digestive enzyme concentration and stimulates gallbladder to contract and release bile.
Figure 4. Fatty chyme entering the duodenum stimulates the gallbladder to release bile
Acute cholecystitis
Acute cholecystitis is sudden swelling and irritation of the gallbladder. It causes severe belly pain.
In 90% of cases, acute cholecystitis is caused by gallstones in the gallbladder. Other causes include severe illness and (rarely) tumors of the gallbladder.
Gallstones occur more often in women than men. Gallstones become more common with age in both sexes. Native Americans and Hispanics have a higher rate of gallstones than most other people.
Acute cholecystitis causes
The gallbladder is an organ that sits below the liver. It stores bile, which your body uses to digest fats in the small intestine.
Acute cholecystitis occurs when bile becomes trapped in the gallbladder. This often happens because a gallstone blocks the cystic duct, the tube through which bile travels into and out of the gallbladder. When a stone blocks this duct, bile builds up, causing irritation and pressure in the gallbladder. This can lead to swelling, infection and a hole (perforation) in the organ.
Other causes include:
- Serious illnesses, such as HIV or diabetes
- Tumors of the gallbladder (rare)
Some people are more at risk for gallstones. Risk factors include:
- Being female
- Pregnancy
- Hormone therapy
- Older age
- Being Native American or Hispanic
- Obesity
- Losing or gaining weight rapidly
- Diabetes
Sometimes the bile duct becomes blocked temporarily. When this occurs repeatedly, it can lead to chronic cholecystitis. This is swelling and irritation that continues over time. Eventually, the gallbladder becomes thick and hard. It does not store and release bile as well as it did.
Acute cholecystitis prevention
Removing the gallbladder and gallstones will prevent further attacks.
Acute cholecystitis outlook (prognosis)
Most people who have surgery to remove their gallbladder recover completely.
Acute cholecystitis possible complications
Untreated, cholecystitis may lead to any of the following health problems:
- Empyema (pus in the gallbladder)
- Gangrene
- Injury to the bile ducts draining the liver (may occur after gallbladder surgery)
- Pancreatitis
- Perforation
- Peritonitis (inflammation of the lining of the abdomen)
Acute cholecystitis symptoms
The main symptom is pain in the upper right side or upper middle of your belly that usually lasts at least 30 minutes. You may feel:
- Sharp, cramping, or dull pain
- Steady pain
- Pain that spreads to your back or below your right shoulder blade
Other symptoms that may occur include:
- Clay-colored stools
- Fever
- Nausea and vomiting
- Yellowing of skin and whites of the eyes (jaundice)
Acute cholecystitis diagnosis
Your health care provider will perform a physical exam and ask about your symptoms. During the physical exam, you will likely have pain when the provider touches your belly.
Your health care provider may order the following blood tests:
- Amylase and lipase
- Bilirubin
- Complete blood count (CBC)
- Liver function tests
Imaging tests can show gallstones or inflammation. You may have one of these tests:
- Abdominal ultrasound
- Abdominal CT scan
- Abdominal x-ray
- Oral cholecystogram
- Gallbladder radionuclide scan
Acute cholecystitis treatment
If you have severe belly pain, seek medical attention right away.
If you’re diagnosed with acute cholecystitis, you’ll probably need to be admitted to hospital for treatment.
In the emergency room, you’ll be given fluids through a vein. You also may be given antibiotics to fight infection.
Cholecystitis may clear up on its own. However, if you have gallstones, you will probably need surgery to remove your gallbladder.
Initial treatment for acute cholecystitis will usually involve:
- Not eating or drinking (fasting) to take the strain off your gallbladder
- Receiving fluids through a drip directly into a vein (intravenously) to prevent dehydration
- Taking medication to relieve your pain
You’ll also be given antibiotics if it’s thought you have an infection. These often need to be continued for up to a week, during which time you may need to stay in hospital, or you may be able to go home.
After initial treatment, any gallstones that may have caused acute cholecystitis usually fall back into the gallbladder and the inflammation will often settle down.
Nonsurgical treatment includes:
- Antibiotics you take at home to fight infection
- Low-fat diet (if you are able to eat)
- Pain medicines
You may need emergency surgery if you have complications such as:
- Gangrene (tissue death)
- Perforation (a hole that forms in the wall of the gallbladder)
- Pancreatitis (inflamed pancreas)
- Persistent bile duct blockage
- Inflammation of the common bile duct
If you are very ill, a tube may be placed through your belly into your gallbladder to drain it. Once you feel better, you may have surgery.
Gallbladder Surgery
Removing your gallbladder may be recommended at some point after initial treatment to prevent acute cholecystitis recurring and reduce your risk of developing potentially serious complications. This type of surgery is known as a cholecystectomy.
Although uncommon, an alternative procedure called a percutaneous cholecystostomy may be carried out if you’re too unwell to have surgery. This is where a needle is inserted through your abdomen to drain away the fluid that’s built up in the gallbladder.
If you’re fit enough to have surgery, your doctors will decide when the best time to remove your gallbladder is. In some cases you may need to have surgery immediately or in the next day or two, or it may be necessary to wait a few weeks until the inflammation has settled down.
Surgery can be carried out in three ways:
- Laparoscopic cholecystectomy – a type of keyhole surgery where the gallbladder is removed using special surgical instruments inserted through a number of small cuts (incisions) in your abdomen
- Single-incision laparoscopic cholecystectomy – where the gallbladder is removed through a single incision, which is usually made near the bellybutton
- Open cholecystectomy – where the gallbladder is removed through a single larger incision in the abdomen
Although some people who’ve had their gallbladder removed have reported symptoms of bloating and diarrhea after eating certain foods, it’s possible to lead a perfectly normal life without a gallbladder. The organ can be useful, but it’s not essential as your liver will still produce bile to digest food.
Possible side effects of surgery
You can live perfectly normally without a gallbladder, so there aren’t usually any long-term effects from gallbladder removal surgery.
However, it’s common to experience some temporary side effects while you recover, including:
- swollen, bruised and painful wounds – this should start to improve within a few days; regular painkillers such as paracetamol may help reduce the discomfort
- feeling sick – you may feel sick as a result of the anesthetic or painkillers you’ve been given, but this should pass quickly
- pain in your tummy and shoulders – this is a result of the gas used to inflate your tummy and should pass after a couple of days; painkillers can be taken to relieve the discomfort
- bloating, flatulence and diarrhea – this can last a few weeks; eating high-fiber food such as fruit, vegetables, brown rice and wholemeal bread can help to
- firm up your stools, and your doctor may also be able to prescribe medication to help
- fatigue, mood swings and irritability – these feelings should improve as you recover
Recovery after gallbladder surgery
How long it takes to recover from gallbladder removal surgery (cholecystectomy) depends on whether you had a laparoscopic (keyhole) or open procedure.
Most people who have keyhole surgery are able to leave hospital on the same day as the operation. It will usually take around two weeks to return to your normal activities.
In many cases, dissolvable stitches will be used to close your wounds. These should start to disappear by themselves within a week or two.
If non-dissolvable stitches were used, you’ll usually need to have them removed by a nurse at your doctor surgery after 7-10 days. You’ll be given an appointment for this before you leave hospital.
After open surgery, you’ll usually have to stay in hospital for three to five days and your recovery time will be longer. It can take around six to eight weeks to return to your normal activities.
In either case, you’ll need to arrange for someone to take you home from hospital. Someone should also stay with you for at least 24 hours if you go home the same day as your operation, as you may still be feeling the effects of the anesthetic.
Generally speaking, after keyhole surgery you can:
- Eat a normal diet straight away – you can return to a normal diet even if you were advised to avoid certain foods before your operation, although you should try to have a generally healthy and balanced diet (read more about diet after gallbladder surgery)
- Do gentle exercises, such as walking – but be careful not to push yourself too hard too soon and ask your surgeon or GP for advice about returning to more strenuous exercise
- Drive again after a week or so – but first make sure you can wear a seatbelt and practice an emergency stop without feeling any discomfort
- Have sex as soon as you feel up to it – but try not to place weight on your wounds until they’ve healed
- Return to work after 10-14 days, depending on what your job involves
It can take a bit longer to return to these activities after open gallbladder removal surgery. For example, you may not be able to drive or return to work for around four to eight weeks.
Chronic cholecystitis
Chronic cholecystitis is swelling and irritation of the gallbladder that continues over time.
The gallbladder is a sac located under the liver. It stores bile that is made in the liver. Bile helps the intestines digest fats.
Chronic cholecystitis causes
Most of the time, chronic cholecystitis is caused by repeated attacks of acute (sudden) cholecystitis. Most of these attacks are caused by gallstones in the gallbladder.
These attacks cause the walls of the gallbladder to thicken. The gallbladder begins to shrink. Over time, the gallbladder is less able to concentrate, store, and release bile.
The disease occurs more often in women than in men. It is more common after age 40.
Chronic cholecystitis prevention
The condition is not always preventable. Eating less fatty foods may relieve symptoms in people. However, the benefit of a low-fat diet has not been proven.
Chronic cholecystitis outlook (prognosis)
Cholecystectomy is a common procedure with a low risk.
Chronic cholecystitis possible complications
Complications may include:
- Cancer of the gallbladder (rarely)
- Jaundice
- Pancreatitis
- Worsening of the condition
Chronic cholecystitis symptoms
Acute cholecystitis is a painful condition that leads to chronic cholecystitis. It is not clear whether chronic cholecystitis causes any symptoms.
Symptoms of acute cholecystis can include:
- Sharp, cramping, or dull pain in upper right or upper middle of your belly
- Steady pain lasting about 30 minutes
- Pain that spreads to your back or below your right shoulder blade
- Clay-colored stools
- Fever
- Nausea and vomiting
- Yellowing of skin and whites of the eyes (jaundice)
Chronic cholecystitis diagnosis
Your health care provider may order the following blood tests:
- Amylase and lipase. To diagnose diseases of the pancreas.
- Complete blood count (CBC)
- Liver function tests. To evaluate how well the liver is working.
Tests that reveal gallstones or inflammation in the gallbladder include:
- Abdominal CT scan
- Abdominal ultrasound
- Gallbladder scan (HIDA scan)
- Oral cholecystogram
Chronic cholecystitis treatment
Surgery is the most common treatment. Surgery to remove the gallbladder is called cholecystectomy.
- Laparoscopic cholecystectomy is most often done. This surgery uses smaller surgical cuts, which result in a faster recovery. Many people are able to go home from the hospital on the same day as surgery, or the next morning.
- Open cholecystectomy requires a larger cut in the upper-right part of the abdomen.
If you are too ill to have surgery because of other diseases or conditions, the gallstones may be dissolved with medicine you take by mouth. However, this may take 2 years or longer to work. The stones may return after treatment.
Cholecystitis causes
Cholecystitis occurs when your gallbladder becomes inflamed. Gallbladder inflammation can be caused by:
- Gallstones. Most often, cholecystitis is the result of hard particles that develop in your gallbladder (gallstones). Gallstones can block the tube (cystic duct) through which bile flows when it leaves the gallbladder. Bile builds up, causing inflammation.
- Tumor. A tumor may prevent bile from draining out of your gallbladder properly, causing bile buildup that can lead to cholecystitis.
- Bile duct blockage. Kinking or scarring of the bile ducts can cause blockages that lead to cholecystitis.
- Infection. AIDS and certain viral infections can trigger gallbladder inflammation.
- Blood vessel problems. A very severe illness can damage blood vessels and decrease blood flow to the gallbladder, leading to cholecystitis.
Calculous cholecystitis
Calculous cholecystitis is the most common, and usually less serious, type of acute cholecystitis. It accounts for around 95% of all cases.
Calculous cholecystitis develops when the main opening to the gallbladder, called the cystic duct, gets blocked by a gallstone or a substance known as biliary sludge.
Biliary sludge is a mixture of bile, a liquid produced by the liver that helps digest fats, and small cholesterol and salt crystals.
The blockage in the cystic duct causes bile to build up in the gallbladder, increasing the pressure inside it and causing it to become inflamed. In around one in every five cases, the inflamed gallbladder also becomes infected by bacteria.
Acalculous cholecystitis
Acalculous cholecystitis is a less common, but usually more serious, type of acute cholecystitis. It usually develops as a complication of a serious illness, infection or injury that damages the gallbladder.
Acalculous cholecystitis can be caused by accidental damage to the gallbladder during major surgery, serious injuries or burns, blood poisoning (sepsis), severe malnutrition or AIDS.
Risk factors for developing cholecystitis
Having gallstones is the main risk factor for developing cholecystitis.
Figure 5. Gallstones in gallbladder
Cholecystitis prevention
It isn’t always possible to prevent acute cholecystitis, but you can lower your risk of developing it by reducing your risk of getting gallstones.
One of the main things you can do to lower your chances of getting gallstones is to adopt a healthy, balanced diet and reduce the number of high-cholesterol foods you eat, as cholesterol is thought to contribute to the formation of gallstones.
Being overweight, particularly being obese, also increases your risk of developing gallstones. You should therefore control your weight by eating a healthy diet and exercising regularly.
However, low-calorie rapid weight loss diets should be avoided because there’s evidence they can disrupt your bile chemistry and actually increase your risk of developing gallstones. A more gradual weight loss plan is best.
You can reduce your risk of cholecystitis by taking the following steps to prevent gallstones:
- Lose weight slowly. Rapid weight loss can increase the risk of gallstones. If you need to lose weight, aim to lose 1 or 2 pounds (0.5 to about 1 kilogram) a week.
- Maintain a healthy weight. Being overweight makes you more likely to develop gallstones. To achieve a healthy weight, reduce calories and increase your physical activity. Maintain a healthy weight by continuing to eat well and exercise.
- Choose a healthy diet. Diets high in fat and low in fiber may increase the risk of gallstones. To lower your risk, choose a diet high in fruits, vegetables and whole grains.
From the limited evidence available, changes to your diet and losing weight (if you’re overweight) may help prevent gallstones.
Cholecystitis diet
Because of the role cholesterol appears to play in the formation of gallstones, it is advisable to avoid eating too many foods with a high saturated fat content.
Foods high in saturated fat include:
- meat pies
- sausages and fatty cuts of meat
- butter, ghee and lard
- cream
- hard cheeses
- cakes and biscuits
- food containing coconut or palm oil
A healthy, balanced diet is recommended. This includes plenty of fresh fruit and vegetables (at least five portions a day) and wholegrains.
There’s also evidence that regularly eating nuts, such as peanuts or cashews, can help reduce your risk of developing gallstones.
Drinking small amounts of alcohol may also help reduce your risk of gallstones. However, you shouldn’t regularly drink more than 14 units of alcohol a week as this can lead to liver problems and other health conditions. Regularly drinking any amount of alcohol can increase the risk to your health.
Losing weight
Being overweight, particularly being obese, increases the amount of cholesterol in your bile, which increases your risk of developing gallstones. You should control your weight by eating a healthy diet and taking plenty of regular exercise.
However, avoid low-calorie, rapid-weight-loss diets. There’s evidence they can disrupt your bile chemistry and increase your risk of developing gallstones. A more gradual weight loss plan is recommended.
Cholecystitis signs and symptoms
Signs and symptoms of cholecystitis may include:
- Severe pain in your upper right or center abdomen
- Pain that spreads to your right shoulder or back
- Tenderness over your abdomen when it’s touched
- Nausea
- Vomiting
- Fever
Cholecystitis signs and symptoms often occur after a meal, particularly a large or fatty one.
Cholecystitis complications
Without appropriate treatment, acute cholecystitis can sometimes lead to potentially life-threatening complications.
Cholecystitis can lead to a number of serious complications, including:
- Infection within the gallbladder. If bile builds up within your gallbladder, causing cholecystitis, the bile may become infected.
- Death of gallbladder tissue (gangrenous cholecystitis). Untreated cholecystitis can cause tissue in the gallbladder to die (gangrene). It’s the most common complication, especially among older people, those who wait to get treatment, and those with diabetes. This can lead to a tear in the gallbladder, or it may cause your gallbladder to burst.
- Torn gallbladder (perforated gallbladder). A tear (perforation) in your gallbladder may result from gallbladder swelling, infection or death of tissue.
Emergency surgery to remove the gallbladder is needed to treat these complications in about one in every five cases of acute cholecystitis.
Cholecystitis diagnosis
If you have severe abdominal pain, your doctor will probably carry out a simple test called Murphy’s sign. You’ll be asked to breathe in deeply with your doctor’s hand pressed on your tummy, just below your rib cage.
Your gallbladder will move downwards as you breathe in. If you have cholecystitis, you’ll experience sudden pain as your gallbladder reaches your doctor’s hand.
If your symptoms suggest you have acute cholecystitis, your doctor will refer you to hospital immediately for further tests and treatment.
Tests and procedures used to diagnose cholecystitis include:
- Blood tests. Your doctor may order blood tests to look for signs of an infection or signs of gallbladder problems.
- Imaging tests that show your gallbladder. Abdominal ultrasound, endoscopic ultrasound, or a computerized tomography (CT) scan can be used to create pictures of your gallbladder that may reveal signs of cholecystitis or stones in the bile ducts and gallbladder.
- A scan that shows the movement of bile through your body. A hepatobiliary iminodiacetic acid (HIDA) scan tracks the production and flow of bile from your liver to your small intestine and shows blockage. A HIDA scan involves injecting a radioactive dye into your body, which attaches to bile-producing cells so that it can be seen as it travels with the bile through the bile ducts.
Cholecystitis treatment
Treatment for cholecystitis usually involves a hospital stay to control the inflammation in your gallbladder. Sometimes, surgery is needed.
At the hospital, your doctor will work to control your signs and symptoms. Treatments may include:
- Fasting. You may not be allowed to eat or drink at first in order to take stress off your inflamed gallbladder.
- Fluids through a vein in your arm. This treatment helps prevent dehydration.
- Antibiotics to fight infection. If your gallbladder is infected, your doctor likely will recommend antibiotics.
- Pain medications. These can help control pain until the inflammation in your gallbladder is relieved.
- Procedure to remove stones. Your doctor may perform a procedure called endoscopic retrograde cholangiopancreatography (ERCP) to remove any stones blocking the bile ducts or cystic duct.
Your symptoms are likely to decrease in two or three days. However, gallbladder inflammation often returns. Most people with the condition eventually need surgery to remove the gallbladder.
Gallbladder removal surgery is called a cholecystectomy. Usually, this is a minimally invasive procedure, involving a few tiny incisions in your abdomen (laparoscopic cholecystectomy). An open procedure, in which a long incision is made in your abdomen, is rarely required.
The timing of surgery depends on the severity of your symptoms and your overall risk of problems during and after surgery. If you’re at low surgical risk, surgery may be performed within 48 hours or during your hospital stay.
Once your gallbladder is removed, bile flows directly from your liver into your small intestine, rather than being stored in your gallbladder. You don’t need your gallbladder to live normally.
Cholestasis of pregnancy
Intrahepatic cholestasis of pregnancy is a liver disorder that occurs in pregnant women 1. Cholestasis is a condition that impairs the release of a digestive fluid called bile from liver cells. As a result, bile builds up in the liver, impairing liver function. Because the problems with bile release occur within the liver (intrahepatic), the condition is described as intrahepatic cholestasis. Intrahepatic cholestasis of pregnancy usually becomes apparent in the third trimester of pregnancy. Bile flow returns to normal after delivery of the baby, and the signs and symptoms of the condition disappear. However, they can return during later pregnancies.
This condition causes severe itchiness (pruritus) in the expectant mother. The itchiness usually begins on the palms of the hands and the soles of the feet and then spreads to other parts of the body. Occasionally, affected women have yellowing of the skin and whites of the eyes (jaundice). Some studies have shown that women with intrahepatic cholestasis of pregnancy are more likely to develop gallstones sometime in their life than women who do not have the condition.
Intrahepatic cholestasis of pregnancy can cause problems for the unborn baby. This condition is associated with an increased risk of premature delivery and stillbirth. Additionally, some infants born to mothers with intrahepatic cholestasis of pregnancy have a slow heart rate and a lack of oxygen during delivery (fetal distress).
In the United States, intrahepatic cholestasis of pregnancy affects less than 1 percent of women of Northern European ancestry 2. Intrahepatic cholestasis of pregnancy is more common in certain populations, such as women of Araucanian Indian ancestry in Chile or women of Scandinavian ancestry. This condition is found less frequently in other populations.
What are the risks of intrahepatic cholestasis of pregnancy in pregnancy?
Intrahepatic cholestasis of pregnancy can be very uncomfortable for the pregnant woman. It also can hurt the baby. Up to 60 percent of women with intrahepatic cholestasis of pregnancy deliver prematurely (before 37 weeks of pregnancy) 3. Premature babies are at increased risk for health problems during the newborn period and for lasting disabilities and death. intrahepatic cholestasis of pregnancy also increases the risk for stillbirth, though the risk is small (1 to 2 percent) 2. It is important to diagnose and treat intrahepatic cholestasis of pregnancy to help prevent these potential problems.
Intrahepatic cholestasis of pregnancy causes
The cause of intrahepatic cholestasis of pregnancy is not well understood. Pregnancy hormones and heredity appear to play a role. intrahepatic cholestasis of pregnancy appears to be more common in twin (or other multiple) pregnancies, possibly due to increased hormone levels 2. About half of women with intrahepatic cholestasis of pregnancy have a family history of related liver disorders 4.
Genetic changes in the ABCB11 or the ABCB4 gene can increase a woman’s likelihood of developing intrahepatic cholestasis of pregnancy.
The ABCB11 gene provides instructions for making a protein called the bile salt export pump (BSEP). This protein is found in the liver, and its main role is to move bile salts (a component of bile) out of liver cells, which is important for the normal release of bile. Changes in the ABCB11 gene associated with intrahepatic cholestasis of pregnancy reduce the amount or function of the BSEP protein, although enough function remains for sufficient bile secretion under most circumstances. Studies show that the hormones estrogen and progesterone (and products formed during their breakdown), which are elevated during pregnancy, further reduce the function of BSEP, resulting in impaired bile secretion and the features of intrahepatic cholestasis of pregnancy.
The ABCB4 gene provides instructions for making a protein that helps move certain fats called phospholipids across cell membranes and release them into bile. Phospholipids attach (bind) to bile acids (another component of bile). Large amounts of bile acids can be toxic when they are not bound to phospholipids. A mutation in one copy of the ABCB4 gene mildly reduces the production of ABCB4 protein. Under most circumstances, though, enough protein is available to move an adequate amount of phospholipids out of liver cells to bind to bile acids. Although the mechanism is unclear, the function of the remaining ABCB4 protein appears to be impaired during pregnancy, which may further reduce the movement of phospholipids into bile. The lack of phospholipids available to bind to bile acids leads to a buildup of toxic bile acids that can impair liver function, including the regulation of bile flow.
Most women with intrahepatic cholestasis of pregnancy do not have a genetic change in the ABCB11 or ABCB4 gene. Other genetic and environmental factors likely play a role in increasing susceptibility to this condition.
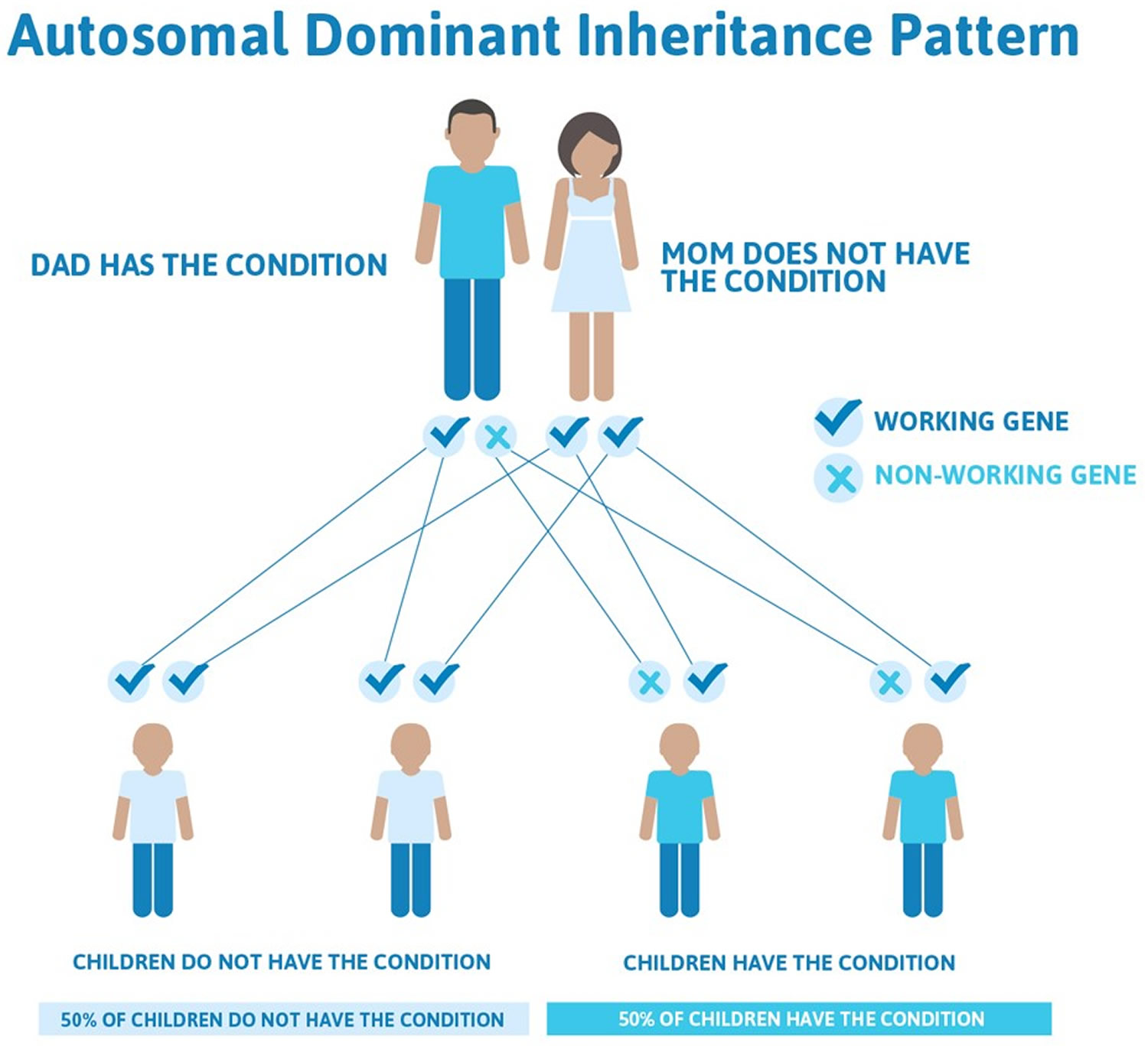
Susceptibility to intrahepatic cholestasis of pregnancy is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to increase the risk of developing the disorder. Some women with an altered gene do not develop intrahepatic cholestasis of pregnancy. Many other factors likely contribute to the risk of developing this complex disorder.
Figure 6. Intrahepatic cholestasis of pregnancy autosomal dominant inheritance pattern
Does intrahepatic cholestasis of pregnancy go away after giving birth?
Symptoms of intrahepatic cholestasis of pregnancy generally clear up on their own by about 2 days after a woman gives birth. However, about 60 to 70 percent of affected women develop intrahepatic cholestasis of pregnancy again in another pregnancy 2.
Intrahepatic cholestasis of pregnancy symptoms
The symptoms of intrahepatic cholestasis of pregnancy can range from mild to severe. Symptoms usually start in the second or third trimester of pregnancy. The most common symptoms include:
- Skin itching: Itching often is most severe on the palms of the hands and soles of the feet, but many affected women itch all over their bodies. It often gets progressively worse and may interfere with sleep and daily activities.
- Jaundice: This yellowing of the skin and whites of the eyes occurs in 10 to 20 percent of women with intrahepatic cholestasis of pregnancy 2. Jaundice is caused by a build-up of a chemical called bilirubin in the blood, resulting from the liver disorder and decreased bile flow.
A pregnant woman should see her health care provider if she has these symptoms.
Intrahepatic cholestasis of pregnancy diagnosis
There are a number of skin disorders of pregnancy that can cause itching; most do not harm the mother or baby. Blood tests can tell if a woman’s itching is due to intrahepatic cholestasis of pregnancy. These often include a blood test that measures various chemicals that show how well a woman’s liver is functioning and the amount of bile acids in her blood.
Intrahepatic cholestasis of pregnancy treatment
Intrahepatic cholestasis of pregnancy often is treated with a medication called ursodeoxycholic acid (Actigall). This medication relieves skin itching, helps correct liver function abnormalities and may help prevent stillbirth.
The health care provider monitors the baby closely (with ultrasound and tests that measure heart rate) to see if the baby appears to be developing any difficulties, such as heart rate abnormalities, due to intrahepatic cholestasis of pregnancy. If the baby is having difficulties, the provider may recommend early delivery to help reduce the risk of stillbirth. The provider also may do a test called amniocentesis when the baby is at about 36 weeks gestation to see if the lungs are mature. If the baby’s lungs are mature enough for the baby to breathe on his own, the provider may induce labor at 36 to 38 weeks to help prevent stillbirth 2.
- Intrahepatic cholestasis of pregnancy. https://www.marchofdimes.org/pregnancy/liver-disorders.aspx[↩]
- Riely, C.A., Bacq, Y. Intrahepatic Cholestasis of Pregnancy. Clinics in Liver Disease, volume 8, 2004, pages 167-176.[↩][↩][↩][↩][↩][↩]
- Lammert, F., et al. Intrahepatic Cholestasis of Pregnancy: Molecular Pathogenesis, Diagnosis and Management. Journal of Hepatology, volume 33, 2000, pages 1012-1021.[↩]
- Kroumpouzos, G. and Cohen, L.M. Specific Dermatoses of Pregnancy: An Evidence-Based Systematic Review. American Journal of Obstetrics and Gynecology, volume 188, number 4, April 2003, pages 1083-1092.[↩]