Contents
What is a pilonidal cyst
The pilonidal cyst an abnormal pocket in the skin that usually contains hair and skin debris due to a granulomatous reaction of a hair shaft penetrating the skin. Pilonidal cysts usually occur when hair punctures the skin and then becomes embedded. Hence the name pilonidal (“pilus” meaning hair and “nidal” meaning nest). A pilonidal cyst is almost always located near the tailbone at the top of the cleft of the buttocks, but may occur in the umbilicus.
Males are preferentially affected 3-4:1 females.
If a pilonidal cyst becomes infected, the resulting pilonidal abscess is often extremely painful.
- An infected pilonidal cyst or abscess requires surgical drainage plus antibiotics. It will not heal with antibiotic medicines alone.
- The pilonidal cyst can be drained through a small incision or removed surgically. If you continue to have infections, the pilonidal cyst can be surgically removed.
- Depending on the type of pilonidal cyst surgery required, pilonidal cyst surgery recovery time may take 4 to 10 weeks to heal.
Pilonidal cysts most commonly occur in young men, and the problem has a tendency to recur. People who sit for prolonged periods of time, such as truck drivers, are at higher risk of developing a pilonidal cyst.
Who gets pilonidal disease?
Pilonidal disease affects both men and women usually between the ages of 20–40 years. It is 3–4 times more common in men than women. Other factors that increase the risk of pilonidal disease include:
- Coarse, curly or crinkly hair
- Obesity
- Family predisposition
- Poor hygiene
- Prolonged sitting or buttock friction causing increased sweating
- Repeated local injury (once known as “Jeep rider’s disease” as it hospitalized more than 80,000 US soldiers in WWII)
- Co-existing hidradenitis suppurativa.
You may help heal the infection and prevent pilonidal cyst from happening again by:
- keeping your buttock cleft clean and dry
- using a mild soap and making sure all soap is removed after cleaning
- shaving the area regularly or using a hair-removal product
- soaking in a warm tub (sitz bath) a few times a day
- taking pain relief medication
- avoiding sitting for long periods.
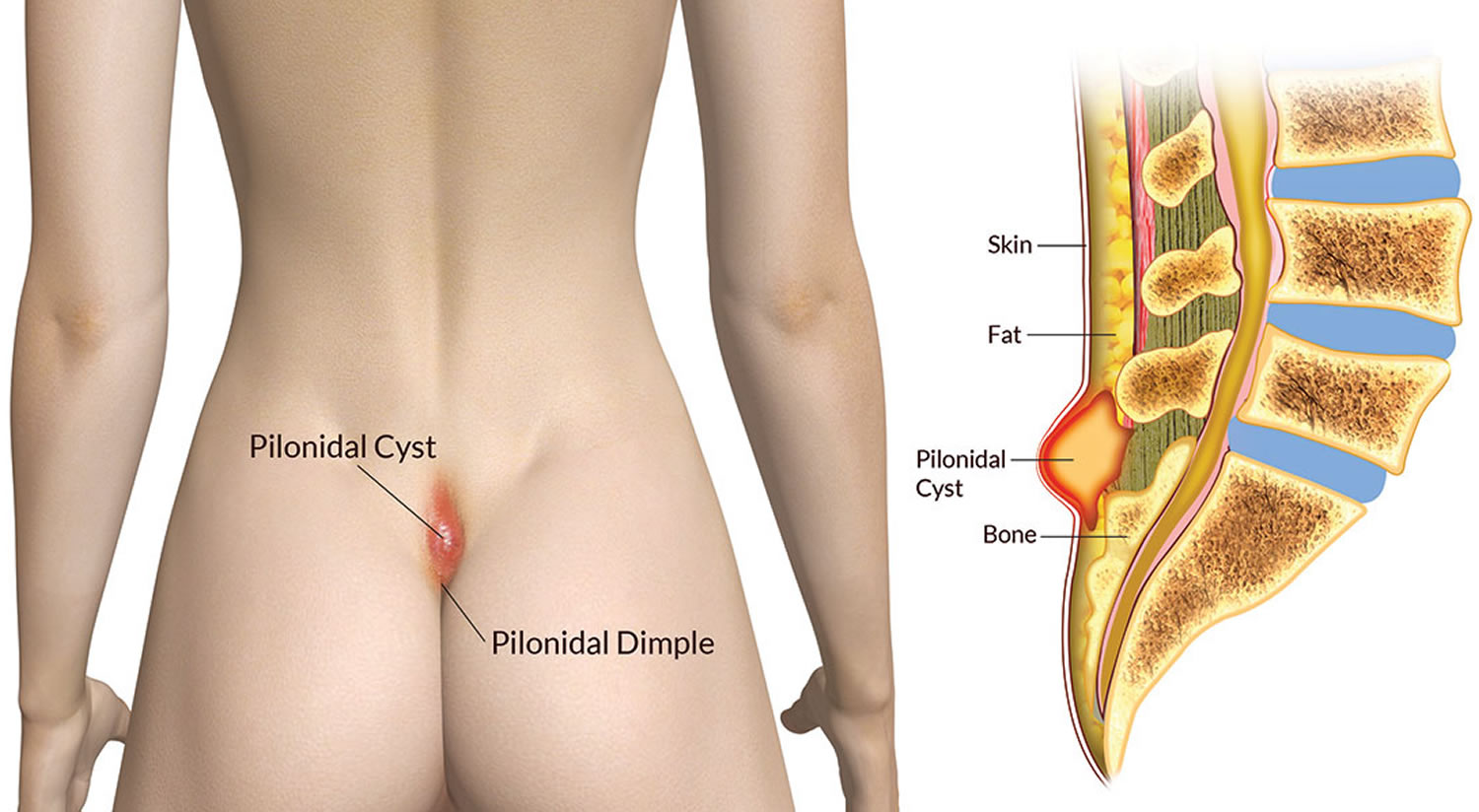
Figure 1. Pilonidal cyst
Figure 2. Pilonidal cyst
Figure 3. Pilonidal cyst with granuloma formation
Pilonidal cyst complications
If a chronically infected pilonidal cyst isn’t treated properly, you may be at slightly increased risk of developing a type of skin cancer called squamous cell carcinoma (SCC).
Pilonidal cyst causes
The exact cause of pilonidal cysts isn’t clear. But most pilonidal cysts appear to be caused by loose hairs that penetrate the skin. Friction and pressure — skin rubbing against skin, tight clothing, bicycling, long periods of sitting or similar factors — force the hair down into skin. Responding to the hair as a foreign substance, the body creates a cyst around the hair.
This explanation accounts for rare cases of pilonidal cysts that occur in parts of the body other than near the tailbone. For example, barbers, dog groomers and sheep shearers have developed pilonidal cysts in the skin between fingers.
Risk factors for developing pilonidal cysts
Certain factors can make you more susceptible to developing pilonidal cysts, such as:
- Male sex
- Younger age (pilonidal cysts are most common in people in their 20s)
- Obesity
- Inactive lifestyle
- Occupation requiring prolonged sitting
- Excess body hair
- Stiff or coarse hair
Pilonidal cyst prevention
To help prevent pilonidal cysts, try to:
- Keep the area clean
- Lose weight if needed
- Avoid prolonged sitting
If you’ve had pilonidal cysts in the past, you might want to regularly shave the area or use hair removal products to reduce the risk of recurrence.
Pilonidal cyst symptoms
Signs and symptoms can vary from a small painless pit or dimple at the base of the spine to a large painful abscess. Most patients have progressive tenderness, particularly after prolonged periods of sitting, such as during a long drive.
When it’s infected, a pilonidal cyst becomes a swollen mass (abscess). Signs and symptoms of an infected pilonidal cyst include:
- Pain, redness and swelling
- Reddening of the skin
- Small hole or holes draining fluid that may be clear, cloudy (pus) or bloody
- If infected, the draining pus may have a foul odor
- Fever, malaise or nausea
- Visible or lumpy tracts 2–5 cm long in chronic or recurrent pilonidal disease.
How pilonidal cyst diagnosis made?
The clinical features of pilonidal sinus is usually straightforward. If necessary, skin biopsy can be undertaken. The histopathological features of pilonidal sinus characteristically show foreign body reaction.
Pilonidal cyst treatment
A pilonidal cyst that isn’t causing any problems doesn’t require any treatment. The patient should be advised to keep the area clean and free of hair by shaving or using a hair removal agent every 2–3 weeks. The cyst may resolve itself. Persistent and inflamed cysts (acute pilonidal abscess) are incised (cut into) and drained out to reduce inflammation and pain. Occasionally the abscess cavity may be cut out completely to remove hair nests and skin debris; this reduces the rate of recurrence to about 15%.
Persistent, complex or recurrent pilonidal sinus disease must be treated surgically. Procedures vary from taking the roof off the sinuses to wide and deep excision (i.e. all affected areas are completely cut out). In all cases, the cavity is scrubbed and scraped out to remove hair and abnormally healing granulation tissue.
Several techniques are available for wound healing and closure; these include:
- Dressing or packing open wounds
- Marsupialisation (forming a pouch), which results in a smaller wound compared to wounds that are left open to granulate
- Closure using skin flaps for wide excisions.
How to get rid of a pilonidal cyst
The initial treatment for an infected pilonidal cyst is usually a procedure that can be performed in your doctor’s office. After numbing the area with an injection, your doctor makes a small incision to drain the cyst. If the cyst recurs, which often happens, you may need a more extensive surgical procedure that removes the cyst entirely.
After surgery, your doctor may choose to:
- Leave the wound open. In this option, the surgical wound is left open and packed with dressing to allow it to heal from the inside out. This process results in a longer healing time but usually a lower risk of a recurring pilonidal cyst infection.
- Close the wound with stitches. While the healing time is shorter with this option, there’s a greater risk of recurrence. Some surgeons make the incision to the side of the cleft of the buttocks, where healing is particularly difficult.
Wound care is extremely important after surgery. Your doctor or nurse will give you detailed instructions on how to change dressings, what to expect of a normal healing process and when to call the doctor. You may also need to shave around the surgical site to prevent hairs from entering the wound.
Pilonidal cyst removal surgery
There are several types of pilonidal cyst surgery.
Incision and drainage: This is the most common treatment for an infected pilonidal cyst. It is a simple procedure done in the doctor’s office.
- Local anesthesia is used to numb the skin.
- A cut is made in the cyst to drain fluid and pus. The hole is packed with gauze and left open.
- Afterward, it can take up to 4 weeks for the cyst to heal. The gauze has to be changed often during this time.
Pilonidal cystectomy: If you keep having problems with a pilonidal cyst, it can be removed surgically. This procedure is done as an outpatient procedure, so you will not need to spend the night in the hospital.
- You may be given medicine (general anesthesia) that keeps you asleep and pain-free. Or, you may be given medicine (regional anesthesia) that numbs you from the waist down. In rare cases, you may only be given local numbing medicine.
- A cut is made to remove the skin with the pores and the underlying tissue with the hair follicles.
- Depending on how much tissue is removed, the area may or may not be packed with gauze. Sometimes a tube is placed to drain fluid that collects after surgery. The tube is removed at a later time when the fluid stops draining.
It may be hard to remove the entire cyst, so there is a chance that it will come back.
- Pilonidal cysts come back in about half of the people who have surgery the first time. Even after a second surgery, it may come back.
After the pilonidal cyst surgery:
- You can go home after the pilonidal cyst surgery on the same day
- The wound will be covered with a bandage
- You will get pain medicines
- It is very important to keep the area around the wound clean
- Your provider will show you how to care for your wound
- After it heals, shaving the hair in the wound area may help prevent pilonidal disease from coming back
Why is the pilonidal cyst surgery performed?
Surgery is needed to drain and remove a pilonidal cyst that does not heal.
- Your doctor may recommend this procedure if you have pilonidal disease that is causing pain or infection.
- A pilonidal cyst that is not causing symptoms does not need treatment.
Non-surgical treatment may be used if the area is not infected:
- Shaving or laser removal of hair around the pilonidal cyst
- Injection of surgical glue into the pilonidal cyst
Risks for pilonidal cyst surgery
Pilonidal cyst resection is generally safe. Ask your doctor about these complications:
- Bleeding
- Infection
- Taking a long time for the area to heal
- Having the pilonidal cyst come back
Pilonidal cysts come back in about half of the people who have surgery the first time. Even after a second surgery, it may come back.