Contents
What is diabetic ketoacidosis
Diabetic ketoacidosis, sometimes called DKA, is an emergency, dangerous and serious condition in which extreme hyperglycemia (high blood sugar level), along with a severe lack of insulin. As a result, your body starts burning its stores of fat for energy instead. This process produces by-products called ketones. As the level of ketones in the body increases – an accumulation of ketones in the blood and urine, diabetic ketoacidosis can lead to dehydration and confusion. Signs of diabetic ketoacidosis are nausea, vomiting, stomach pain, fruity odor on the breath, and rapid (Kussmaul) breathing. If not treated, people with ketoacidosis can become unconscious and can die.
- Diabetic ketoacidosis is characterized by a serum glucose level greater than 250 mg per dL (13.9 mmol/L), a pH less than 7.3, a serum bicarbonate level less than 18 mEq per L, an elevated serum ketone level, and dehydration.
Diabetic ketoacidosis usually occurs in people with type 1 diabetes. It is rare in type 2 diabetes – a third of diabetic ketoacidosis cases occur in those with type 2 diabetes. Although most cases of diabetic ketoacidosis affect people over the age of 20 and the great majority of diabetic ketoacidosis cases in kids aren’t fatal, this condition is still the No. 1 killer of children and adolescents with type 1 diabetes. And in some instances, people discover that they have diabetes after they land in the hospital with diabetic ketoacidosis. So it’s important to know the signs of diabetic ketoacidosis—and how to avoid it.
Diabetic ketoacidosis can occur in persons of all ages, with 14 percent of cases occurring in persons older than 70 years, 23 percent in persons 51 to 70 years of age, 27 percent in persons 30 to 50 years of age, and 36 percent in persons younger than 30 years 1. The case fatality rate is 1 to 5 percent 2. About one-third of all cases are in persons without a history of diabetes mellitus.
In a study of 28,770 persons younger than 20 years (mean age of 14 years) with diabetes, 94 percent had no episodes of diabetic ketoacidosis, 5 percent had one episode, and 1 percent had at least two episodes 3. Additionally, diabetic ketoacidosis occurred more often in females, in persons with a migration background, and in persons 11 to 15 years of age 3. Diabetic ketoacidosis has a case fatality rate of 1 to 5 percent 2. Although the highest rate of mortality is in older adults and persons with comorbid conditions, diabetic ketoacidosis is the leading cause of death in persons younger than 24 years with diabetes, most often because of cerebral edema 4.
Although people with diabetic ketoacidosis typically have a history of diabetes, 27 to 37 percent have newly diagnosed diabetes 5. This is especially true in young children. Most persons with diabetic ketoacidosis have type 1 diabetes. There is also a subgroup of persons with type 2 diabetes who have ketosis-prone diabetes; this subgroup represents 20 to 50 percent of persons with diabetic ketoacidosis 6. Persons with ketosis-prone diabetes have impaired insulin secretion; however, with proper glucose management, beta cell function improves and the clinical course resembles that of type 2 diabetes 7. These persons are often black or Latino, male, middle-aged, overweight or obese, have a family history of diabetes, and have newly diagnosed diabetes 8.
People with type 1 diabetes and children are at greater risk for diabetic ketoacidosis than those with type 2 and adults, respectively. One reason that kids are prone to diabetic ketoacidosis is illness, which can trigger diabetic ketoacidosis. Children are sick more often, largely because they spend a lot of time in close association with other children. However, when sick, adults with diabetes, especially type 1, may also develop diabetic ketoacidosis. Illness increases the levels of stress hormones in the body, the same hormones that counteract insulin and raise blood glucose levels. Nausea and vomiting can also cause dehydration (especially dangerous in infants and toddlers), which can increase the risk for diabetic ketoacidosis. Plus, if people don’t feel like eating, they may not think to take at least some of their mealtime insulin.
Also, certain ethnic groups get ketosis-prone diabetes, such as those of West African descent. Low-income people have more diabetic ketoacidosis episodes than others, because people just stop taking insulin. A lot of them are patients who don’t have access to their medications because of cost. Another contributing factor is drug abuse. When you are busy using substances, your insulin becomes less of a need. Plus, some illicit substances, such as cocaine, can drive up levels of anti-insulin hormones, pushing the body toward diabetic ketoacidosis.
The symptoms of diabetic ketoacidosis include high blood glucose, high levels of ketones in the urine, and:
- quick breathing (Kussmaul)
- flushed cheeks
- abdominal pain
- breath that smells like sweet acetone (similar nail polish remover)
- vomiting
- dehydration.
Diabetic ketoacidosis is a serious condition that requires immediate assessment and treatment in the hospital. If someone you know has diabetes and becomes confused or unconscious, or has the symptoms listed above, call your local emergency number for an ambulance.
If you have diabetes and you find your blood sugar level is higher than it should be, it’s important that you follow the advice provided by your doctor or diabetes nurse or educator. You may also find it useful to read the advice provided in our other article on hyperglycaemia (high blood sugar).
If you feel ill or stressed or you’ve had a recent illness or injury, check your blood sugar level often. You might also try an over-the-counter urine ketones testing kit.
Contact your doctor immediately if:
- You’re vomiting and unable to tolerate food or liquid
- Your blood sugar level is higher than your target range and doesn’t respond to home treatment
- Your urine ketone level is moderate or high
Seek emergency care if:
- Your blood sugar level is consistently higher than 300 milligrams per deciliter (300 mg/dL), or 16.7 millimoles per liter (16.7 mmol/L)
- You have ketones in your urine and can’t reach your doctor for advice
- You have multiple signs and symptoms of diabetic ketoacidosis — excessive thirst, frequent urination, nausea and vomiting, abdominal pain, shortness of breath, fruity-scented breath, confusion
Remember, untreated diabetic ketoacidosis can be fatal.
Diabetic ketoacidosis pathophysiology
Your body runs on glucose. Glucose is the fuel that keeps your brain working and your muscles moving. But without enough insulin to transport the glucose into your cells, the body breaks down fat for fuel instead of glucose, causing ketones to form and circulate in the bloodstream.
Diabetic ketoacidosis starts with a lack of the hormone insulin. When things are working normally, insulin ushers glucose (a kind of sugar from food) into cells, where it can be converted into energy. But without enough insulin in the body, glucose accumulates in the blood, where it is of little use. Even though there is plenty of glucose around, it can’t get into the cells to feed them. The body’s response is to drive up blood glucose even more by spurring the liver to break down its glucose stores and to make additional glucose from scratch.
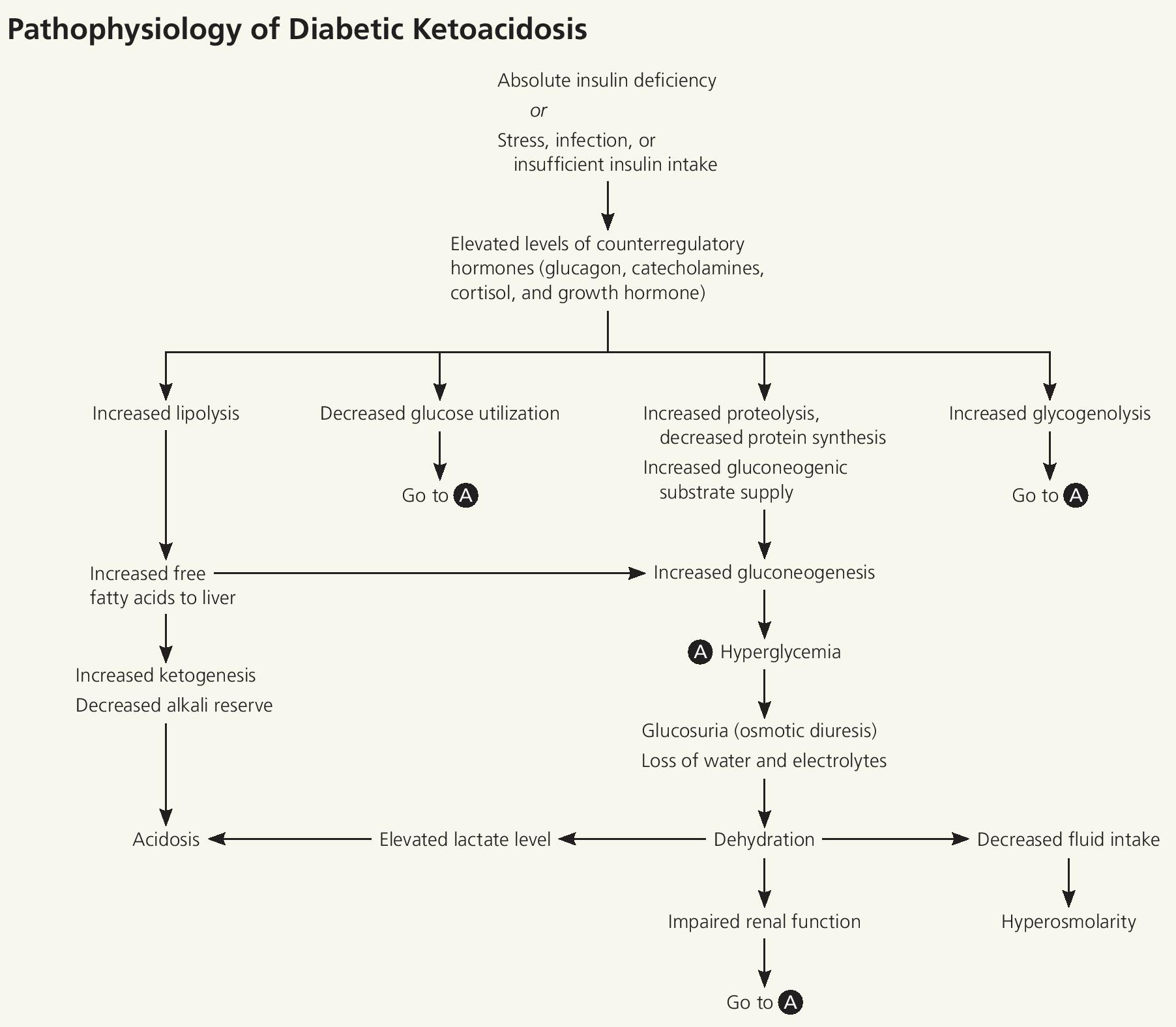
Figure 1. Diabetic ketoacidosis pathophysiology
This insulin deficiency stimulates the elevation of the counter regulatory hormones (glucagon, catecholamines, cortisol, and growth hormone). Without the ability to use glucose, the body needs alternative energy sources. Lipase activity increases, causing a breakdown of adipose tissue that yields free fatty acids. These components are converted to acetyl coenzyme A, some of which enter the Krebs cycle for energy production; the remainder are broken down into ketones (acetone, acetoacetate, and β-hydroxybutyrate). Ketones can be used for energy, but accumulate rapidly. Glycogen and proteins are catabolized to form glucose. Together, these factors promote hyperglycemia, which leads to an osmotic diuresis resulting in dehydration, metabolic acidosis, and a hyperosmolar state.
As the body tries to clear the surplus glucose out of its blood through urination, a person may become dangerously dehydrated. At the same time, the body starts to breakdown fat deposits for energy. Fat is indeed rich in energy, but breaking down these fat stockpiles produces acidic side products called ketones. In high enough concentrations, ketones become toxic by making the blood more acidic. This imbalance is the crux of diabetic ketoacidosis and gives this complication its name. This increase in blood acidity can severely disrupt the finely tuned chemical processes in your body that keep you living and healthy.
The most common triggers for diabetic ketoacidosis are illnesses or infections, which promote the production of certain hormones in the body that counteract insulin. This is why “sick-day rules” focus on taking more insulin when you’re ill. The condition may also arise from other events that place stress on the body, such as heart attack and stroke. In addition, missing insulin doses, undetected insulin pump failure, and certain medications can lead to the development of diabetic ketoacidosis.
People with type 1 diabetes are most at risk because they no longer produce insulin and are completely dependent on injected or pumped insulin to keep blood glucose and ketones in check. In fact, many people are diagnosed with type 1 following an episode of diabetic ketoacidosis. People with type 2 diabetes don’t make enough insulin to maintain normal blood glucose levels, but the insulin they do produce is usually enough to suppress ketone formation. They may develop diabetic ketoacidosis amid extreme bodily stress, such as a serious infection.
While rare, it is possible to develop diabetic ketoacidosis without high blood glucose—what’s known as euglycemic diabetic ketoacidosis (ediabetic ketoacidosis). The main cause of ediabetic ketoacidosis is an illness that involves vomiting and very little food intake for prolonged periods of time. Drugs in the Sodium-glucose Cotransporter-2 (SGLT2) inhibitor class (e.g. Gliflozin) can also increase the risk of ediabetic ketoacidosis. In both cases, glucose levels may be in the 100 to 200 mg/dl (5.6 to 11.1 mmol/L) range, rather than the 250 mg/dl (13.9 mmol/L) or higher typical of diabetic ketoacidosis. SGLT-2 inhibitors lower blood glucose by causing you to excrete excess glucose through the urine. Because doctors expect blood glucose to be higher with diabetic ketoacidosis, this can lead to a missed diabetic ketoacidosis diagnosis. The FDA 9 recently issued a warning regarding this potential side effect of SGLT-2 inhibitors. Because the problem is more common with type 1 diabetes, these drugs shouldn’t be used by people with type 1. Euglycemic diabetic ketoacidosis can sometimes occur in people with type 2.
Diabetic ketoacidosis can develop rapidly, typically in less than 24 hours. It brings on a range of symptoms. Frequent urination from hyperglycemia results in dehydration and tremendous thirst. Other symptoms include nausea, vomiting, abdominal pain, loss of appetite, and confusion.
Shortness of breath is another diabetic ketoacidosis symptom. As the body’s natural buffering system is overwhelmed by the acidic ketones, this imbalance causes hyperventilation as the body attempts to regulate blood acid levels by getting rid of carbon dioxide in expired air. As the severity of ketoacidosis increases, the smell of a person’s breath may take on the fruity tinge of nail polish remover.
High blood glucose levels that don’t respond to medication are also a sign of diabetic ketoacidosis, particularly levels greater than 300 mg/dl (16.7 mmol/L). But elevated blood glucose isn’t always present with diabetic ketoacidosis. Some people get what is called “euglycemic diabetic ketoacidosis,” meaning that although their blood glucose is not elevated, they are still producing ketones.
- The key to diagnosing diabetic ketoacidosis is checking ketone levels in the urine. Over-the-counter ketone test kits are available at pharmacies, or a test for ketones can be done at the doctor’s office. If you have diabetic ketoacidosis symptoms, consistently high blood glucose, or persistently high urinary ketones, you should immediately seek emergency care. This is especially true if you have or recently had an illness or infection.
What are the Warning Signs of diabetic ketoacidosis?
Diabetic ketoacidosis usually develops slowly. But when vomiting occurs, this life-threatening condition can develop in a few hours.
Early symptoms include the following:
- Thirst or a very dry mouth
- Frequent urination
- High blood glucose (blood sugar) levels
- High levels of ketones in the urine
Then, other symptoms appear:
- Constantly feeling tired
- Dry or flushed skin
- Nausea, vomiting, or abdominal pain
- Vomiting can be caused by many illnesses, not just ketoacidosis. If vomiting continues for more than 2 hours, contact your health care provider.
- Difficulty breathing
- Fruity odor on breath
- A hard time paying attention, or confusion
Checking your blood sugar and ketone levels
Ketone testing is a key part of type 1 diabetes management as it helps to prevent a dangerous short term complication, ketoacidosis, from occurring.
If you have type 1 diabetes, it is recommended that you have ketone testing supplies on your prescription.
Ketone testing may also be useful in people with other types of diabetes that are dependent upon insulin.
Check your blood sugar level if you have symptoms of diabetic ketoacidosis.
You can detect ketones with a simple urine test using a test strip, similar to a blood testing strip. Ask your health care provider when and how you should test for ketones. If your blood sugar is 11 mmol/L or over and you have a blood or urine ketone testing kit, check your ketone level. Many experts advise to check your urine for ketones when your blood glucose is more than 250 mg/dL (13.9 mmol/L).
When you are ill (when you have a cold or the flu, for example), check for ketones every 4 to 6 hours. And check every 4 to 6 hours when your blood glucose is more than 250 mg/dL (13.9 mmol/L).
The presence of high levels of ketones in the bloodstream is a common complication of diabetes, which if left untreated can lead to ketoacidosis.
Ketones build up when there is insufficient insulin to help fuel the body’s cells.
High levels of ketones are therefore more common in people with type 1 diabetes or people with advanced type 2 diabetes.
Whats the difference between mmol/L and mg/dL?
Both sets of units are used to measure blood sugar levels and both give a measurement of the concentration of glucose in the blood, albeit in slightly different ways.
mmol/L gives the molarity, which is the number of molecules of a substance within a specified volume, in this case within 1 litre. mg/dL gives the concentration by the ratio of weight to volume, in this case milligrams per decilitre.
mmol/L is the most common measurement used in the UK with mg/dL predominantly used in the USA and continental Europe.
- mmol/L : International standard unit for measuring the concentration of glucose in the blood – also known as millimolar (mM). This unit is used in the UK.: Millimoles per litre
- mg/dL : Unit for measuring concentration of glucose in the blood in the USA – milligrams per decilitre.: Milligrams per 100 millilitres
Blood glucose typically varies from 72 mg/dL (4 mmol/L) to 108 mg/dL (6 mmol/L) for people without diabetes.
Blood sugar (also called blood glucose) needs to be tightly controlled in the human body to minimize the risk of complications developing.
- Formula to calculate mmol/l from mg/dl: mmol/l = mg/dl /18
- Formula to calculate mg/dl from mmol/l: mg/dl = 18 × mmol/l
Why test for ketones?
Ketones are produced by the body as an alternative source of energy to sugar (see Diabetic ketoacidosis pathophysiology section above). The body produces ketones by breaking down fats, this process is known as ketosis.
Ketones may be produced as part of weight loss, however, it’s important for people with diabetes on insulin to note that ketones can be produced when the body has insufficient insulin.
When the body has too little insulin, it means that cells of the body cannot take in enough sugar from the blood. To compensate for this, the body will start to break down fat to provide ketones.
However, if a high level of ketones is produced, this can cause the blood to become acidic which can lead to illness and even potential danger to organs if not treated in time.
This state is referred to as diabetic ketoacidosis.
When to test for ketones?
People with insulin dependent diabetes should take a ketone test:
- Any time your blood sugar is over 17 mmol/l (300 mg/dl)
- If sugar levels have repeatedly been over 13 mmol/l (230 mg/dl)
- If you are unwell and have any of the symptoms of ketoacidosis
How do I test for ketones?
Ketone testing can be carried out at home.
The most accurate way of testing for ketones is to use a blood glucose meter which can test for ketones as well as blood glucose levels.
You can also test urine for ketone levels, however, the testing of urine means that the level you get is representative of your ketone levels up to a few hours ago.
What should the ketone test results be?
- lower than 10.8 mg/dL (0.6 mmol/L) is a normal reading
- 10.8 to 27 mg/dL (0.6 to 1.5 mmol/L) means you’re at a slightly increased risk of diabetic ketoacidosis and should test again in a couple of hours
- 28.8 to 52.2 mg/dL (1.6 to 2.9 mmol/L) means you’re at an increased risk of diabetic ketoacidosis and should contact your diabetes team or doctor as soon as possible
- 54 mg/dL (3 mmol/L) or over means you have a very high risk of diabetic ketoacidosis and should get medical help immediately
If you do a urine ketone test, a result of more than 2+ means there’s a high chance you have diabetic ketoacidosis.
- For people with diabetes on insulin, having high ketone levels should be regarded as potentially dangerous.
What If I Find Higher-than-normal Levels of Ketones?
If your health care provider has not told you what levels of ketones are dangerous, then call when you find moderate amounts after more than one test. Often, your health care provider can tell you what to do over the phone.
Call your health care provider at once if you experience the following conditions:
- Your urine tests show high levels of ketones.
- Your urine tests show high levels of ketones and your blood glucose level is high.
- Your urine tests show high levels of ketones and you have vomited more than twice in four hours.
Do NOT exercise when your urine tests show ketones and your blood glucose is high. High levels of ketones and high blood glucose levels can mean your diabetes is out of control. Check with your health care provider about how to handle this situation.
Diabetic ketoacidosis complications
Diabetic ketoacidosis is treated with fluids, electrolytes — such as sodium, potassium and chloride — and insulin. Perhaps surprisingly, the most common complications of diabetic ketoacidosis are related to this lifesaving treatment.
Possible complications of the treatments
Treatment complications include:
- Low blood sugar (hypoglycemia). Insulin allows sugar to enter your cells, causing your blood sugar level to drop. If your blood sugar level drops too quickly, you can develop low blood sugar.
- Low potassium (hypokalemia). The fluids and insulin used to treat diabetic ketoacidosis can cause your potassium level to drop too low. A low potassium level can impair the activities of your heart, muscles and nerves.
- Swelling in the brain (cerebral edema). Adjusting your blood sugar level too quickly can produce swelling in your brain. This complication appears to be more common in children, especially those with newly diagnosed diabetes.
Left untreated, the risks are much greater. Diabetic ketoacidosis can lead to loss of consciousness and, eventually, it can be fatal.
What causes diabetic ketoacidosis
Here are three basic reasons for moderate or large amounts of ketones:
- Not enough insulin
- Maybe you did not inject enough insulin. Or your body could need more insulin than usual because of illness.
- Not enough food
- When you’re sick, you often don’t feel like eating, sometimes resulting in high ketone levels. High levels may also occur when you miss a meal.
- Insulin reaction (low blood glucose)
- If testing shows high ketone levels in the morning, you may have had an insulin reaction while asleep.
The two main causes of diabetic ketoacidosis are interruption of insulin treatment (missing insulin injections or failure of an insulin pump system) and severe illness, such as the flu with fever or even a heart attack or stroke.
Insulin controls the production of ketones, the substances that build up in the bloodstream and cause diabetic ketoacidosis, so if someone with type 1 diabetes stops taking insulin, diabetic ketoacidosis can result. During an illness, the body produces stress hormones, which counteract insulin action to such an extent that diabetic ketoacidosis can develop. High blood glucose levels result, leading to excessive urination and dehydration, which in turn push blood glucose and ketones to even higher levels. Some people incorrectly assume that if they’re sick and not eating, they shouldn’t take insulin, but this will result in rapid development of diabetic ketoacidosis. That’s why it’s important to work with your care provider early during an illness to determine the best way to avoid interruption of insulin treatment. Dehydration that occurs due to vomiting, inability to eat and drink, and high glucose and ketone levels can also contribute to rapid worsening of diabetic ketoacidosis.
The symptoms of diabetic ketoacidosis include nausea, vomiting, abdominal pain, dry mouth, thirst, and excessive urination. In advanced stages of diabetic ketoacidosis, a rapid, deep breathing pattern develops, and the breath takes on a fruity odor. A decreased level of consciousness is particularly ominous and should prompt a call for emergency medical services.
The best way to prevent diabetic ketoacidosis is to check your blood ketones when your blood glucose is persistently high (greater than 250 mg/dl or 13.9 mmol/L) and not responding normally to additional insulin, especially if you’re sick. Ketone test kits are available at pharmacies. diabetic ketoacidosis can develop rapidly, so it’s very important to check ketones early, to seek professional medical advice, and to go for emergency care promptly if your blood glucose and ketone levels are not responding to treatment. If you’re persistently nauseated or vomiting and can’t drink fluids to stay hydrated, you should call your care provider immediately.
All people with type 1 diabetes should have a reliable means for measuring blood ketones on hand. When in doubt, check your ketones—it’s easy and inexpensive, and it provides the critical information needed to prevent diabetic ketoacidosis.
- The most accurate way of testing for ketones is to use a blood glucose meter which can test for ketones as well as blood glucose levels.
- You can also test urine for ketone levels, however, the testing of urine means that the level you get is representative of your ketone levels up to a few hours ago.
Urine ketone measures only acetone and acetoacetate, not β-hydroxybutyrate, which is the primary ketone in diabetic ketoacidosis. In one study, the urine dipstick test was negative for ketones in six of 18 persons. Ketonemia was defined as a ketone level greater than 0.42 mmol per L 10. In a second study of point-of-care testing in the emergency department, urine dipstick testing for ketones had a sensitivity of 98 percent, specificity of 35 percent, and a positive predictive value of 15 percent. Serum testing for β-hydroxybutyrate had a sensitivity of 98 percent, a specificity of 79 percent, and a positive predictive value of 34 percent (using a cutoff of greater than 1.5 mmol per L), allowing for more accurate diagnosis of diabetic ketoacidosis 11. The American Diabetes Association has revised its position on ketone analysis in favor of serum testing, and has concluded that capillary measurement is equivalent to venous measurement 12.
Diabetic ketoacidosis occurs when
- you have an infection, such as flu or a urinary tract infection (UTI)
- not following your treatment plan, such as missing doses of insulin
- an injury or surgery
- taking certain medicines, such as steroid medication
- binge drinking
- using illegal drugs
- pregnancy
- you have your period
In some cases there’s no obvious trigger.
Preventing diabetic ketoacidosis
The following tips can help reduce your chances of getting diabetic ketoacidosis:
- Check your blood sugar regularly so you can spot and treat an increase quickly
- Stick to your treatment plan – don’t stop taking insulin unless told to by a healthcare professional
- Adjust your insulin dosage as needed. Talk to your doctor or diabetes educator about how to adjust your insulin dosage in relation to your blood sugar level, what you eat, how active you are, whether you’re ill and other factors. If your blood sugar level begins to rise, follow your diabetes treatment plan to return your blood sugar level to your target range.
- Check your ketone level. When you’re ill or under stress, test your urine for excess ketones with an over-the-counter urine ketones test kit. If your ketone level is moderate or high, contact your doctor right away or seek emergency care. If you have low levels of ketones, you may need to take more insulin.
- Take extra care when you’re ill – your diabetes team can give you some “sick day rules” to follow, which include things like checking your blood sugar more often and checking your ketone level
- Be careful taking new medicines – check with a doctor or pharmacist first, as some medicines can increase the risk of diabetic ketoacidosis.
- Be prepared to act quickly. If you suspect that you have diabetic ketoacidosis — your blood sugar level is high, and you have excess ketones in your urine — seek emergency care.
Diabetes complications are scary. But don’t let fear keep you from taking good care of yourself. Follow your diabetes treatment plan carefully, and ask your diabetes treatment team for help when you need it.
Contact your diabetes team or doctor for advice if you find it hard to keep your blood sugar level down.
Diabetic ketoacidosis signs and symptoms
The presentation of diabetic ketoacidosis varies with severity and comorbid conditions. Polyuria with polydipsia is the most common presenting symptom and was found in 98 percent of persons in one study of childhood type 1 diabetes. Other common symptoms included weight loss (81 percent), fatigue (62 percent), dyspnea (57 percent), vomiting (46 percent), preceding febrile illness (40 percent), abdominal pain (32 percent), and polyphagia (23 percent) 13. Dehydration causes tachycardia, poor skin turgor, dry mucous membranes, and orthostatic hypotension. The metabolic acidosis may lead to compensatory deep (Kussmaul) respirations, whereas increased acetone can be sensed as a fruity smell on the patient’s breath. Mental status can vary from somnolence to lethargy and coma. A detailed evaluation may reveal precipitating factors, especially nonadherence to medical regimens and infection, which are common causes of diabetic ketoacidosis.
Signs of diabetic ketoacidosis include:
- needing to urinate more than usual
- feeling very thirsty
- being sick
- nausea and vomiting
- tummy pain
- breath that smells fruity (like pear drop sweets or nail varnish)
- deep or fast breathing
- feeling very tired or sleepy
- confusion
- passing out
Diabetic ketoacidosis can also cause high blood sugar (hyperglycaemia) and a high level of ketones in your blood or urine, which you can check for using home-testing kits.
Symptoms usually develop over 24 hours, but can come on faster.
Diabetic ketoacidosis diagnosis
If your doctor suspects diabetic ketoacidosis, he or she will do a physical exam and various blood tests. In some cases, additional tests may be needed to help determine what triggered the diabetic ketoacidosis.
Blood tests
Blood tests used in the diagnosis of diabetic ketoacidosis will measure:
- Blood sugar level. If there isn’t enough insulin in your body to allow sugar to enter your cells, your blood sugar level will rise (hyperglycemia). As your body breaks down fat and protein for energy, your blood sugar level will continue to rise.
- Ketone level. When your body breaks down fat and protein for energy, acids known as ketones enter your bloodstream.
- Blood acidity. If you have excess ketones in your blood, your blood will become acidic (acidosis). This can alter the normal function of organs throughout your body.
Additional tests
Your doctor may order tests to identify underlying health problems that might have contributed to diabetic ketoacidosis and to check for complications. Tests might include:
- Blood electrolyte tests
- Urinalysis
- Chest X-ray
- A recording of the electrical activity of the heart (electrocardiogram)
Diabetic ketoacidosis treatment
Diabetic ketoacidosis is typically treated in the hospital using a three-pronged approach.
Diabetic ketoacidosis treatments include:
- insulin, usually given into a vein
- fluids given into a vein to rehydrate your body
- nutrients given into a vein to replace any you’ve lost
Intravenous fluid replacement is necessary to combat dehydration. Electrolytes—which affect the heart, muscles, and nerve cells—are reduced in diabetic ketoacidosis, so treatment also focuses on bringing them back to healthy levels. Finally, since a lack of insulin brings on diabetic ketoacidosis, insulin treatment reverses the process. Insulin will bring down blood glucose and halt the acidification of blood by ketones.
You’ll also be closely monitored for any life-threatening problems that can occur, such as problems with the brain, kidneys or lungs.
You can leave hospital when you’re well enough to eat and drink and tests show a safe level of ketones in your body. It’s normal to stay in hospital for a couple of days.
Before leaving hospital, ask to speak to a diabetes nurse about why diabetic ketoacidosis occurred and what you can do to stop it happening again.
- Henriksen OM, Røder ME, Prahl JB, Svendsen OL. Diabetic ketoacidosis in Denmark incidence and mortality estimated from public health registries. Diabetes Res Clin Pract. 2007;76(1):51–56.[↩]
- Wang J, Williams DE, Narayan KM, Geiss LS. Declining death rates from hyperglycemic crisis among adults with diabetes, U.S., 1985–2002. Diabetes Care. 2006;29(9):2018–2022.[↩][↩]
- Fritsch M, Rosenbauer J, Schober E, Neu A, Placzek K, Holl RW. German Competence Network Diabetes Mellitus and the DPV Initiative. Predictors of diabetic ketoacidosis in children and adolescents with type 1 diabetes. Experience from a large multicentre database. Pediatr Diabetes. 2011;12(4 pt 1):307–312.[↩][↩]
- Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crisis in adult patients with diabetes. Diabetes Care. 2009;32(7):1335–1343.[↩]
- Schober E, Rami B, Waldhoer T; Austrian Diabetes Incidence Study Group. Diabetic ketoacidosis at diagnosis in Austrian children in 1989–2008: a population-based analysis. Diabetologia. 2010;53(6):1057–1061.[↩]
- Kim MK, Lee SH, Kim JH, et al. Clinical characteristics of Korean patients with new-onset diabetes presenting with diabetic ketoacidosis. Diabetes Res Clin Pract. 2009;85(1):e8–e11.[↩]
- Balasubramanyam A, Nalini R, Hampe CS, Maldonado M. Syndromes of ketosis-prone diabetes mellitus. Endocr Rev. 2008;29(3):292–302.[↩]
- Umpierrez GE, Smiley D, Kitabchi AE. Narrative review: ketosis-prone type 2 diabetes mellitus. Ann Intern Med. 2006;144(5):350–357.[↩]
- Sodium-glucose Cotransporter-2 (SGLT2) Inhibitors. https://www.fda.gov/Drugs/DrugSafety/ucm446852.htm[↩]
- Bektas F, Eray O, Sari R, Akbas H. Point of care blood ketone testing of diabetic patients in the emergency department. Endocr Res. 2004;30(3):395–402.[↩]
- Arora S, Henderson SO, Long T, Menchine M. Diagnostic accuracy of point-of-care testing for diabetic ketoacidosis at emergency department triage: beta-hydroxbutyrate versus the urine dipstick. Diabetes Care. 2011;34(4):852–854.[↩]
- Kitabchi AE, Umpierrez GE, Murphy MB, et al.; American Diabetes Association. Hyperglycemic crises in diabetes. Diabetes Care. 2004;27(suppl 1):S94–S102.[↩]
- Xin Y, Yang M, Chen XJ, Tong YJ, Zhang LH. Clinical features at the onset of childhood type 1 diabetes mellitus in Shenyang, China. J Paediatr Child Health. 2010;46(4):171–175.[↩]