Contents
What does an enlarged liver mean
Enlarged liver refers to swelling of the liver beyond its normal size. Hepatomegaly is the medical term to describe this problem. If both your liver and spleen are enlarged, it is called hepatosplenomegaly. This condition is most often discovered by a provider. You may not be aware of the liver or spleen swelling.
An enlarged liver may be a sign of a wide range of diseases. Although diseases of the liver itself often cause an enlarged liver, there are many other possible causes, including:
- Bacteria, viruses and parasites
- Certain heart conditions
- Several genetic diseases
- Some types of leukemia and lymphoma
The lower edge of the liver normally comes just to the lower edge of the ribs on the right side. The edge of the liver is normally thin and firm. It cannot be felt with the fingertips below the edge of the ribs, except when you take a deep breath. It may be enlarged if a health care provider can feel it in this area.
It’s very unusual to have an enlarged liver without other signs and symptoms that point to an underlying disease.
The Liver
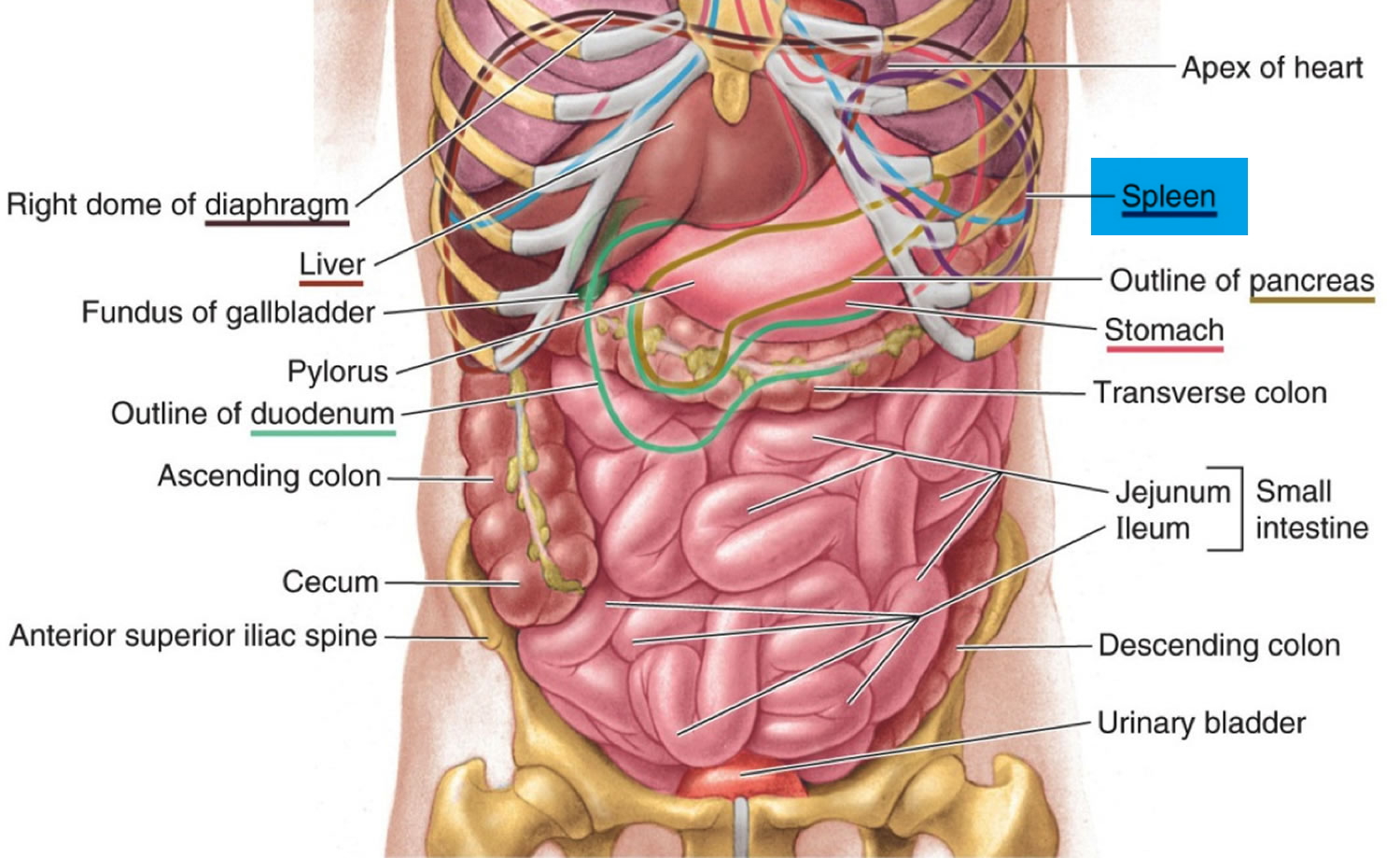
Your liver is the largest organ inside your body, weighing about 1.4 kg (3 pounds) and measuring an average of 5.9 inches (15 cm) in width in an average adult. The liver is in the right upper quadrant of the abdominal cavity, just inferior to the diaphragm in the right superior part of the abdominal cavity and under your right ribs just beneath your right lung – filling much of the right hypochondriac and epigastric regions and extending into the left hypochondriac region. The liver is partially surrounded by the ribs, and extends from the level of the fifth intercostal space to the lower margin of the right rib cage, which protects this highly vascular organ from blows that could rupture it. The liver is shaped like a wedge, the wide base of which faces right and the narrow apex of which lies just inferior to the level of the left nipple. The reddish-brown liver is well supplied with blood vessels.
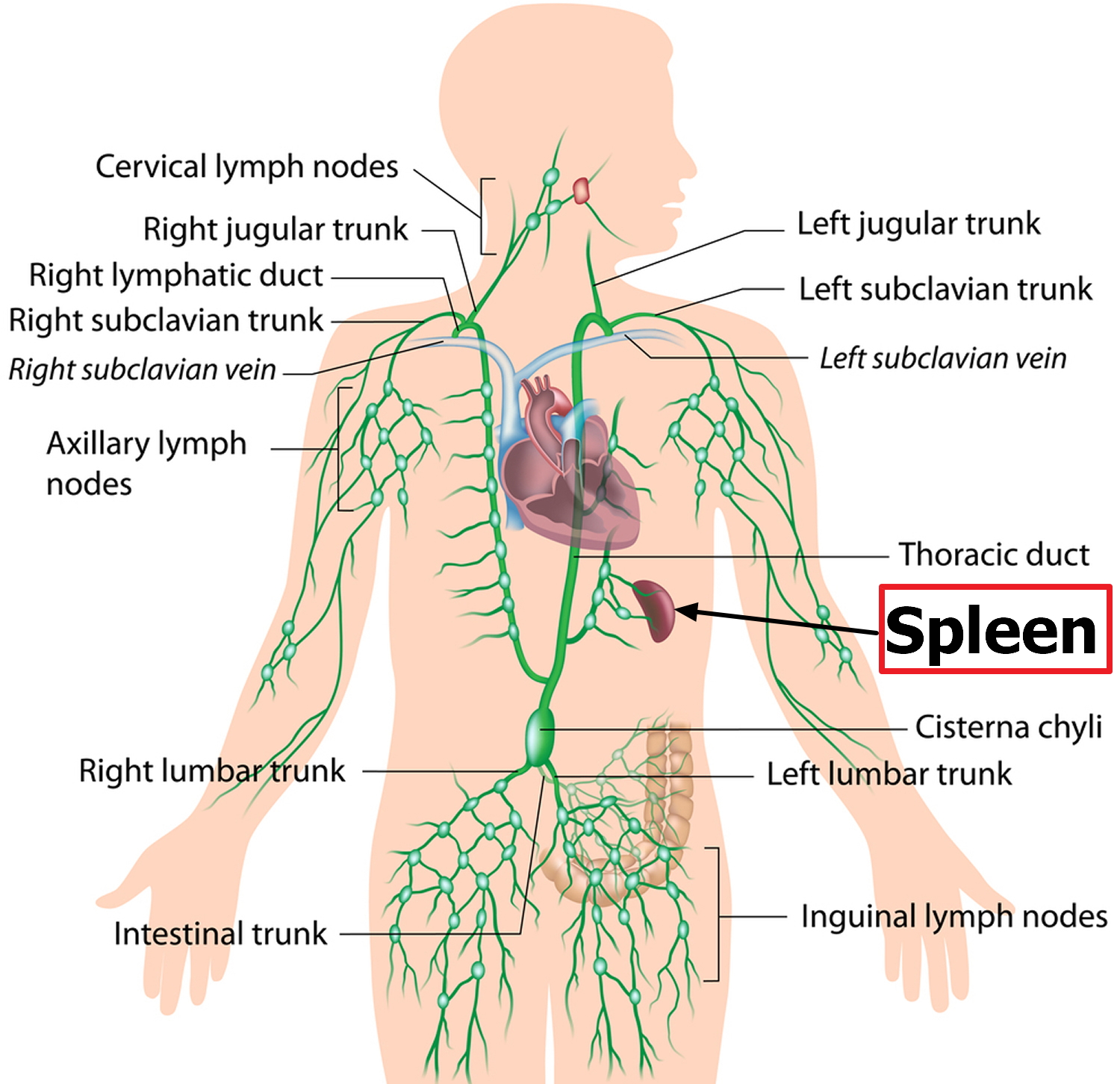
What is a spleen
The spleen, the largest lymphatic organ. The normal position of the spleen is within the peritoneal cavity in the left upper quadrant of the abdominal cavity adjacent to ribs nine through 12, just beneath the left diaphragm. The spleen lies behind and to the left side of your stomach (see Figure 1). The normal sized spleen abuts the stomach, colon, and left kidney The spleen resembles a large lymph node and is subdivided into lobules (see Figure 3). However, unlike the lymphatic sinuses of a lymph node, the spaces in the spleen, called venous sinuses, are filled with blood instead of lymph.
A normal spleen ranges in length from 6 to 13 cm and in weight from 75 to 200 g 1. The spleen is not normally palpable except in slender young adults 1. When the spleen can be felt below the left costal (rib) margin, at rest or on inspiration, spleen enlargement should be assumed and the explanation sought. Although the normal-size or even the abnormally small, spleen can be involved in pathologic processes, with the exception of rubs associated with splenic infarcts, physical examination is generally not helpful in identifying the problem. Nevertheless, the enlarged and palpable spleen is an important clue to the presence of a variety of illnesses 1.
Figure 1. Location of the human liver and spleen
Figure 2. Spleen and the lymphatic system
Liver functions
Amazingly versatile, your liver performs over 500 functions. Its digestive function is to produce bile, a green alkaline liquid that is stored in the gallbladder and secreted into the duodenum. Bile salts emulsify fats in the small intestine; that is, they break up fatty nutrients into tiny particles, just as dish detergent breaks up a pool of fat drippings in a roasting pan. These smaller particles are more accessible to digestive enzymes from the pancreas. The liver also performs many metabolic functions and you cannot live without your liver:
- Picks up glucose from nutrient-rich blood returning from the alimentary canal and stores this carbohydrate as glycogen for subsequent use by the body.
- Processes fats and amino acids and stores certain vitamins.
- Detoxifies many poisons and drugs in the blood.
- Makes the blood proteins.
- It breaks down and stores many of the nutrients absorbed from the intestine that your body needs to function. Some nutrients must be changed (metabolized) in the liver before they can be used for energy or to build and repair body tissues.
- It makes most of the clotting factors that keep you from bleeding too much when you are cut or injured.
- It secretes bile into the intestines to help absorb nutrients (especially fats).
- It breaks down alcohol, drugs, and toxic wastes in the blood, which then pass from the body through urine and stool.
Almost all of these functions are carried out by a type of cell called a hepatocyte or simply a liver cell.
The liver carries on many important metabolic activities. The liver plays a key role in carbohydrate metabolism by helping maintain concentration of blood glucose within the normal range. Liver cells responding to the hormone insulin lower the blood glucose level by polymerizing glucose to glycogen. Liver cells responding to the hormone glucagon raise the blood glucose level by breaking down glycogen to glucose or by converting noncarbohydrates into glucose.
The liver’s effects on lipid metabolism include oxidizing (breaking down) fatty acids at an especially high rate; synthesizing lipoproteins, phospholipids, and cholesterol; and converting excess portions of carbohydrate molecules into fat molecules. The blood transports fats synthesized in the liver to adipose tissue for storage.
Other liver functions concern protein metabolism. They include deaminating amino acids; forming urea; synthesizing plasma proteins such as clotting factors; and converting certain amino acids into other amino acids.
The liver also stores many substances, including glycogen, iron, and vitamins A, D, and B12. In addition, macrophages in the liver help destroy damaged red blood cells and phagocytize foreign antigens. The liver also removes toxic substances such as alcohol and certain drugs from blood (detoxification).
The Bile
Bile is a yellowish-green liquid continuously secreted from hepatic cells. In addition to water, bile contains bile salts, bile pigments (bilirubin and biliverdin), cholesterol, and electrolytes. Of these, bile salts are the most abundant and are the only bile components that have a digestive function.
Bile pigments are breakdown products of hemoglobin from red blood cells and are normally secreted in the bile.
Jaundice, a yellowing of the skin and mucous membranes due to accumulation of bile pigment, has several causes. In obstructive jaundice bile ducts are blocked, perhaps by gallstones or tumors. In hepatocellular jaundice the liver is diseased, as in cirrhosis or hepatitis. In hemolytic jaundice red blood cells are destroyed too rapidly, as happens with an incompatible blood transfusion or a blood infection.
Functions of Bile Salts
Bile salts aid digestive enzymes. Bile salts affect fat globules (clumped molecules of fats) much like a soap or detergent would affect them. That is, bile salts break fat globules into smaller droplets that are more soluble in water. This action, called emulsification, greatly increases the total surface area of the fatty substance. The resulting fat droplets disperse in water. Fat-splitting enzymes (lipases) can then digest the fat molecules more effectively. Bile salts also enhance absorption of fatty acids, cholesterol, and the fat-soluble vitamins A, D, E, and K.
Low levels of bile salts result in poor lipid absorption and vitamin deficiencies.
What does the spleen do ?
The spleen plays a significant role in hematopoiesis and immunosurveillance. The major functions of the spleen include clearance of abnormal red blood cells, removal of microorganisms and antigens as well as the synthesis of immunoglobulin G (IgG). The spleen also synthesizes the immune system peptides properdin and tuftsin 2. Also, approximately one-third of circulating platelets are stored in the spleen.
The tissues within splenic lobules are of two types. The white pulp is distributed throughout the spleen in tiny islands. This tissue is composed of splenic nodules, which are similar to the lymphatic nodules in lymph nodes and are packed with lymphocytes (T lymphocyte cells and B lymphocyte cells). The red pulp, which fills the remaining spaces of the lobules, surrounds the venous sinuses. This pulp contains numerous red blood cells, which impart its color, plus many lymphocytes and macrophages.
Without an immune system, a human being would be just as exposed to the harmful influences of pathogens or other substances from the outside environment as to changes harmful to health happening inside of the body. The main tasks of the body’s immune system are:
- Neutralizing pathogens like bacteria, viruses, parasites or fungi that have entered the body, and removing them from the body
- Recognizing and neutralizing harmful substances from the environment
- Fighting against the body’s own cells that have changed due to an illness, for example cancerous cells.
The normal adult spleen contributes to the homeostasis of the body by removing from the blood useless or potentially injurious materials (e.g., abnormal or “wornout” red blood cells and microorganisms) and by synthesizing immunoglobulins and properdin 1.
Enlarged liver causes
What causes an enlarged liver
The liver is involved in many of the body’s functions. It is affected by many conditions that can cause hepatomegaly, including:
- Alcohol use (especially alcohol abuse)
- Nonalcoholic fatty liver disease
- Cancer metastases (spread of cancer to the liver)
- Congestive heart failure
- Glycogen storage disease
- Hepatitis A
- Hepatitis B
- Hepatitis C
- Hepatitis D
- Hepatitis E
- Hepatocellular carcinoma (liver cancer)
- Hereditary fructose intolerance
- Infectious mononucleosis
- Some types of leukemia
- Some types of lymphoma
- Multiple myeloma
- Niemann-Pick disease
- Primary biliary cholangitis
- Reye syndrome
- Sarcoidosis
- Sclerosing cholangitis
- Steatosis (fat in the liver from metabolic problems such as diabetes, obesity, and high triglycerides, also called nonalcoholic steatohepatitis, or NASH)
Among the list, the most common causes of liver enlargement are:
- Alcoholic liver disease, which includes alcoholic fatty liver disease, alcoholic hepatitis and cirrhosis
- Nonalcoholic fatty liver disease, a lifestyle-related metabolic disease or other (e.g., jejunoileal bypass and total parenteral nutrition)
- Viral hepatitis (hepatitis A, B, C, D or E )
- Liver cancer, or cancer that has spread to the liver from a different organ (metastatic cancer)
- Congestive heart failure
Many less-common liver diseases may also cause liver enlargement, as do some diseases that primarily affect other organs but involve the liver indirectly. A partial list includes:
Cancers
- Some types of leukemia
- Some types of lymphoma
- Multiple myeloma
Genetic diseases
- Hemochromatosis
- Wilson’s disease
- Glycogen storage diseases
- Gaucher’s disease
Heart and blood vessel problems
- Blockage of the veins that drain the liver (Budd-Chiari syndrome)
- Congestive heart failure
- Narrowing (stenosis) of the heart’s tricuspid or mitral valves
Infections
- Liver abscess, caused by parasites (amebiasis) or bacteria
- Other parasitic infections (schistosomiasis, fascioliasis)
- Relapsing fever, which humans catch from body lice or ticks
Damage from toxins
- Drug-induced liver injury from such medications as acetaminophen (Tylenol, others) and amoxicillin-clavulanate (Augmentin, Amoclans)
- Toxic hepatitis from exposure to poisons, such as the industrial chemicals carbon tetrachloride and chloroform
Complex liver and systemic diseases
- Amyloidosis
- Autoimmune hepatitis
- Primary biliary cirrhosis
- Primary sclerosing cholangitis
Risk factors for developing enlarged liver
Factors that may increase your risk of liver problems include:
- Excessive alcohol use. Drinking large amounts of alcohol can be damaging to your liver.
- Large doses of medicines, vitamins or supplements. Taking larger than recommended doses of vitamins, supplements, or over-the-counter or prescription medicines may increase your risk of liver damage.
- Medicinal herbs. Certain herbs, including comfrey, ma huang and mistletoe, can increase your risk of liver damage.
Enlarged liver prevention
To reduce your risk of liver disease, you can:
- Choose a healthy diet. Choose a diet full of fruits, vegetables and whole grains.
- Drink alcohol in moderation, if at all. Check with your doctor to find out what’s the right amount of alcohol for you, if any.
- Follow directions when taking medications, vitamins or supplements. Limit yourself to the recommended doses when taking vitamins, supplements, and over-the-counter or prescription medications.
- Limit contact with chemicals. Use aerosol cleaners, insecticides and other toxic chemicals only in well-ventilated areas. In addition, wear gloves, long sleeves and a mask.
- Maintain a healthy weight. If your weight is healthy, work to maintain it. If you need to lose weight, cut back on the number of calories you eat each day and increase the amount of daily exercise. Ask your doctor about healthy ways to lose weight.
- Use supplements with caution. Talk with your doctor about the risks and benefits of dietary supplements and herbal remedies before you take them. Many of these products can be harmful to your liver, particularly those containing combinations of ingredients and marketed for body-building or weight loss. Specific herbs to avoid include germander, chaparral, senna, mistletoe, comfrey, ma huang, valerian root, kava, celandine and green tea extracts.
Enlarged liver signs and symptoms
In itself, an enlarged liver typically has no symptoms.
Signs and symptoms of conditions that commonly cause liver enlargement include:
- Pain in the upper right belly
- Fatigue
- Muscle aches (myalgia)
- Nausea
- Poor appetite and weight loss
- Yellowing of the skin and the whites of the eyes (jaundice).
Enlarged liver diagnosis
An enlarged liver may go unnoticed for a long time. Frequently, liver enlargement isn’t discovered until you see a doctor for more-obvious signs and symptoms of the condition responsible for your enlarged liver.
As part of the physical examination for possible liver disease, doctors use their fingertips to press on the right side of your belly just below your rib cage and feel (palpate) the lower edge of your liver, noting its size, texture, and tenderness. Depending on the underlying cause, an enlarged liver may feel soft, firm or irregular. Well-defined lumps may be present as well.
Table 1. Examination Findings Associated with Specific Liver Diseases
| Liver disease | Palpation | Size |
|---|---|---|
| Acute hepatitis | Smooth; surface tender | Enlarged |
| Chronic hepatitis | Firm liver edge | Enlarged, especially left lobe |
| Nodules rare; tender | ||
| Fulminant hepatitis | Tender surface | Shrinking size |
| Cirrhosis | Nontender, firm | Variable; late stages, liver decreases in size |
| Hepatocellular carcinoma (hepatoma) | Nodules, if present, large and hard | Moderate to massive enlargement |
| Nontender | ||
| Metastatic carcinoma | Large nodules | Enlarged |
| Nontender | ||
| Fatty liver | Smooth surface | Enlarged |
| Right heart failure | Firm, smooth, tender | Mild to massive enlargement |
This exam provides only a very rough estimate of liver size, though. For a precise measurement, you’ll need imaging, typically starting with an abdominal ultrasound. If there’s a need for more-detailed images, you may also have a computerized tomography (CT) scan or magnetic resonance imaging (MRI).
Tests to determine the cause of hepatomegaly vary, depending on the suspected cause, but may include:
- Abdominal x-ray
- Abdominal ultrasound (may be done to confirm the condition if the provider thinks your liver feels enlarged during a physical exam)
- CT scan of the abdomen
- Blood tests. A blood sample is tested to determine liver enzyme levels and blood clotting test. This can give clues about the health of your liver. Blood tests can also identify viruses that can cause enlarged liver, such as the hepatitis viruses.
- MRI scan of the abdomen. Magnetic resonance elastography uses shear waves to create a visual map (elastogram) of the stiffness of liver tissue. This test is noninvasive and can be an alternative to a liver biopsy.
- Liver biopsy. Your doctor may recommend a biopsy to collect a sample of liver tissue for laboratory testing. A liver biopsy is often done using a long, thin needle that’s inserted through your skin and into your liver. The needle draws out a core of tissue that is then sent to a laboratory for testing. Your doctor may use ultrasound to help guide the biopsy.
Enlarged liver treatment
Treatment for an enlarged liver varies, depending on condition that’s causing it. Some of the most common causes, including alcoholic hepatitis and nonalcoholic fatty liver disease, improve dramatically with alcohol abstinence, a healthy diet, regular exercise and weight loss.
Enlarged spleen
Splenomegaly is defined as enlargement of the spleen measured by size or weight 2. The normal sized spleen measures up to 11 cm in length. A length of 11 cm-20 cm indicates splenomegaly and a length greater than 20cm is definitive of massive splenomegaly 2. The normal weight of the adult spleen is 70 g-200 g, spleen weight of 400 g-500 g indicates splenomegaly and spleen weight greater than 1000 g is definitive of massive splenomegaly 2. The normal sized spleen is usually not palpable in adults. However, it may be palpable due to variations in body habitus and chest wall anatomy. Splenomegaly may be diagnosed clinically or radiographically using ultrasound, CT imaging, or MRI. Splenomegaly may be a transient condition due to acute illness or may be due to serious underlying acute or chronic pathology.
Splenomegaly is a rare disease, with estimated prevalence approximately 2% of total US population 2. In adults, there has been no reported predominance in prevalence based on ethnicity, sex, or age.
Spleen enlargement can be associated with decreased or increased function, depending on the cause of the enlarged spleen.
Table 2. Causes of Splenomegaly (enlarged spleen)
| Vascular congestion |
| Cirrhosis |
| Splenic vein thrombosis |
| Portal vein thrombosis |
| Reticuloendothelial hyperplasia |
| Acute infections (e.g., typhoid fever, cytomegalovirus, Epstein-Barr virus infection) |
| Subacute or chronic infections (e.g., bacterial endocarditis, brucellosis, tuberculosis, histoplasmosis, malaria) |
| Collagen-vascular diseases and abnormal immune responses (e.g., systemic lupus erythematosus, serum sickness, sarcoidosis) |
| Work hypertrophy |
| Hemolytic anemias (e.g., spherocytosis) |
| Infiltrative or replacement processes |
| Nonmalignant hematologic disorders (e.g., polycythemia vera, myelofibrosis) |
| Leukemias |
| Lymphomas |
| Metastatic solid tumors |
| Storage diseases (e.g., Gaucher’s disease) |
| Amyloidosis |
| Benign tumor and cysts |
| Abscess |
| Subcapsular hemorrhage |
When spleen enlargement is associated with a change in splenic function, it is most frequently associated with splenic hyperfunction. This is reflected in the peripheral blood by thrombocytopenia, leukopenia, rapid red blood cell destruction, or a combination of these findings. This clinical syndrome of an enlarged spleen and peripheral cytopenias is often referred to as hypersplenism. When splenic enlargement is secondary to an infiltrative process (i.e., tumors or amyloidosis), splenic hypofunction can result. This is reflected in the peripheral blood by Howell–Jolly bodies and abnormal red blood cell forms. The presence of an enlarged spleen should lead to examination of the peripheral blood by the physician.
It is extremely important to correlate the presence of an enlarged spleen with the clinical history findings, other physical findings, laboratory results, and x-ray findings to identify the cause of splenic enlargement in a particular patient. For example, vascular spiders, red palms, and small testes in a patient with splenic enlargement would strongly suggest liver disease as the etiology. Roth spots and a new heart murmur would suggest endocarditis. Extensive lymphadenopathy, weight loss, night sweats, and an enlarged spleen would suggest a malignant lymphoproliferative disease. By making these correlations, it is possible to utilize the presence of an enlarged spleen to plan a patient’s subsequent evaluation and quickly and efficiently reach the correct diagnosis.
The mechanism underlying splenic enlargement varies based on the etiology. In the case of acute infectious illness, the spleen performs increased work in clearing antigens and producing antibodies and increases the number of reticuloendothelial cells contained within the spleen. These increased immune functions may result in splenic hypertrophy. In the case of liver disease and congestion, underlying illness causes increased venous pressure causing congestive splenomegaly. Extramedullary hematopoiesis exhibited in myeloproliferative disorders can lead to splenic hyperplasia.
Splenic sequestration crisis is a life-threatening illness common in pediatric patients with homozygous sickle cell disease and beta thalassemia 2. Up to 30% of these children may develop splenic sequestration crisis with a mortality rate of up to 15%. This crisis occurs when splenic vaso-occlusion causes a large percentage of total blood volume to become trapped within the spleen. Clinical signs include severe, rapid drop in hemoglobin leading to hypovolemic shock and death 2. Pediatric patients with sickle cell disease and beta thalassemia experience multiple splenic infarcts, resulting in splenic fibrosis and scarring. Over time, this leads to a small, auto infarcted spleen typically by the time patients reach adulthood. Splenic sequestration crisis can only occur in functioning spleens which may be why this crisis is rarely seen in adults. However, late adolescent or adult patients in this group who maintain splenic function may develop splenic sequestration crisis.
Symptoms of enlarged spleen
The most common physical symptom associated with splenomegaly is vague abdominal discomfort 2. Patients may complain of pain in the left upper abdomen or referred pain in the left shoulder.
- Abdominal bloating, distended abdomen, anorexia, and/or early satiety may also occur.
Commonly, patients will present with symptoms due to the underlying illness causing splenomegaly 2. Constitutional symptoms such as weakness, weight loss, and night sweats suggest malignant illness. Patients with splenomegaly due to acute infection may present with fever, rigors, generalized malaise, or focal infectious symptoms. Patients with underlying liver disease may present with symptoms related to alcohol abuse or hepatitis. Symptoms of anemia (lightheadedness, dyspnea, or exertion), easy bruising, bleeding, or petechiae may indicate splenomegaly due to underlying hemolytic process.
Diagnosis of enlarged spleen
A combination of serum testing and imaging studies may definitively diagnose splenomegaly and the underlying cause. Derangement in complete blood (cell) counts and morphology including white blood cell, red blood cell and platelets will vary based on underlying disease state. Abnormalities in liver function tests, lipase, rheumatologic panels, and disease-specific infectious testing aid in the diagnosis of causative disease.
Imaging may be used to diagnose splenomegaly and elucidate its underlying cause. The spleen has a similar attenuation as the liver when measured on CT imaging. In addition to diagnosing splenomegaly (splenic measurement of greater than 10 cm in craniocaudal length), abdominal CT may detect splenic abscess, mass lesions, vascular abnormalities, cysts, inflammatory changes, traumatic injury, intra-abdominal lymphadenopathy, or liver abnormalities.
Ultrasound is a useful imaging modality in measuring the spleen and spares the patient radiation from CT imaging. Normal spleen size measured via ultrasound is less than 13 cm superior to the inferior axis, 6 cm-7 cm in medial to lateral axis and 5 cm-6 cm in anterior to posterior plane.
MRI, PET scans, liver-spleen colloid scanning, and splenectomy and splenic biopsy may be indicated in certain cases.
Treatment and Management of enlarged spleen
Treatment of splenomegaly is targeted at treating the underlying disease and protecting the patient from complications of splenomegaly itself. Patients with splenomegaly from any cause are at increased risk of splenic rupture, and increased attention must be made to protect the patient from abdominal trauma. Treatment ranges from abdominal injury avoidance in the young healthy patient with splenomegaly due to infectious mononucleosis, to splenectomy of a massively enlarged spleen in a patient with Hairy cell leukemia. Likewise, the prognosis is largely dependent on underlying disease state.
Patients who undergo splenectomy are at increased risk of overwhelming infection due to encapsulated organisms such as Hemophilus Influenzae, Streptococcus pneumoniae, and Neisseria meningitidis should receive vaccinations against these organisms. Careful attention must be paid to post-splenectomy patients presenting with febrile illnesses as they may require more aggressive, empiric antibiotic therapy.
- Armitage JO. Spleen. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 150. Available from: https://www.ncbi.nlm.nih.gov/books/NBK258/[↩][↩][↩][↩][↩]
- Chapman J, Bhimji SS. Splenomegaly. [Updated 2017 May 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2017 Jun-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430907/[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Wolf DC. Evaluation of the Size, Shape, and Consistency of the Liver. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 94. Available from: https://www.ncbi.nlm.nih.gov/books/NBK421/[↩]