Contents
- What is Wolff Parkinson White syndrome
What is Wolff Parkinson White syndrome
Wolff-Parkinson-White (WPW) syndrome is a heart condition that causes the heart to beat abnormally fast for periods of time.
It’s a relatively common condition, affecting between one and three in every 1,000 people.
The cause is an abnormal electrical pathways between the atria and ventricles (called accessory pathways) causing the electrical signal to arrive at the ventricles too soon and to be transmitted back into the atria. These accessory pathways can cause electrical impulses to travel in both directions rather than one direction (normal direction from the atria into the ventricles). In Wolff-Parkinson-White (WPW) syndrome, an extra electrical pathway between your heart’s upper chambers and lower chambers causes a rapid heartbeat. Some people with Wolff Parkinson White syndrome also have atrial fibrillation. Wolff Parkinson White syndrome causes the conduct of impulses to be faster than normal. Very fast heart rates may develop as the electrical signal ricochets between the atria and ventricles. Some people with WPW syndrome don’t have symptoms but they still have an increased risk for sudden death.
This problem with the heart is present at birth (congenital), although symptoms may not develop until later in life. Many cases are diagnosed in otherwise healthy adults aged between 20 and 40.
Sometimes the extra electrical connection won’t cause any symptoms and may only be picked up when an electrocardiogram (ECG) test is carried out for another reason. In these cases, further tests will be done to determine if treatment is required.
Doctors can detect WPW syndrome through a routine exam known as an electrocardiogram or ECG (see Figures 2 to 4). Electrodes placed on the chest will pick up the heart’s electrical activity and chart it on a graph. That graph will show any irregularities.
Is Wolff Parkinson White syndrome serious?
It can be scary to be told that you have a problem with your heart, but Wolff Parkinson White syndrome usually isn’t serious.
Many people will have no symptoms or only experience occasional, mild episodes of their heart racing. With treatment, the condition can normally be completely cured.
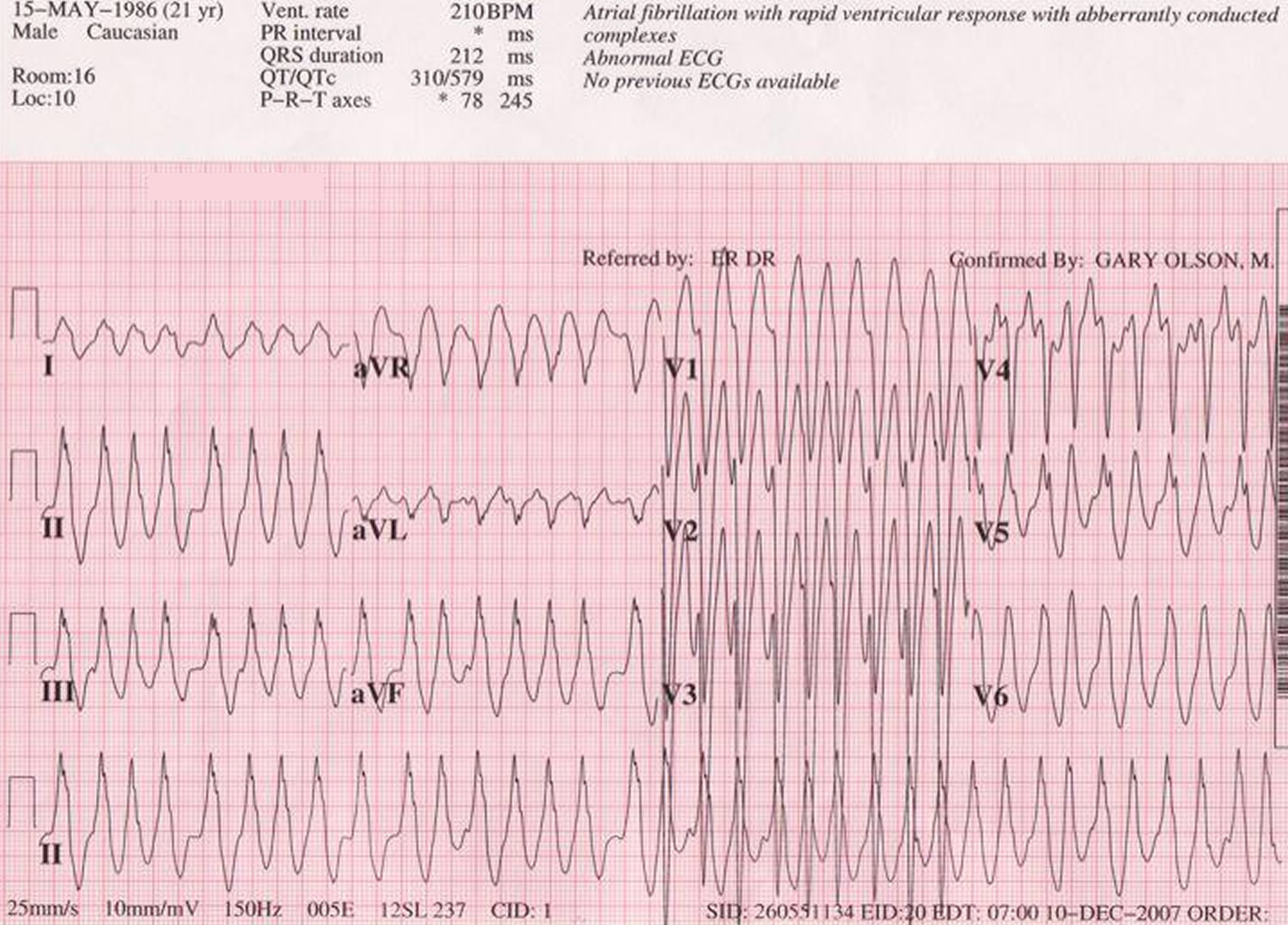
Wolff Parkinson White syndrome can sometimes be life-threatening, particularly if it occurs alongside a type of irregular heartbeat called atrial fibrillation (see Figure 6). But this is rare and treatment can eliminate this risk.
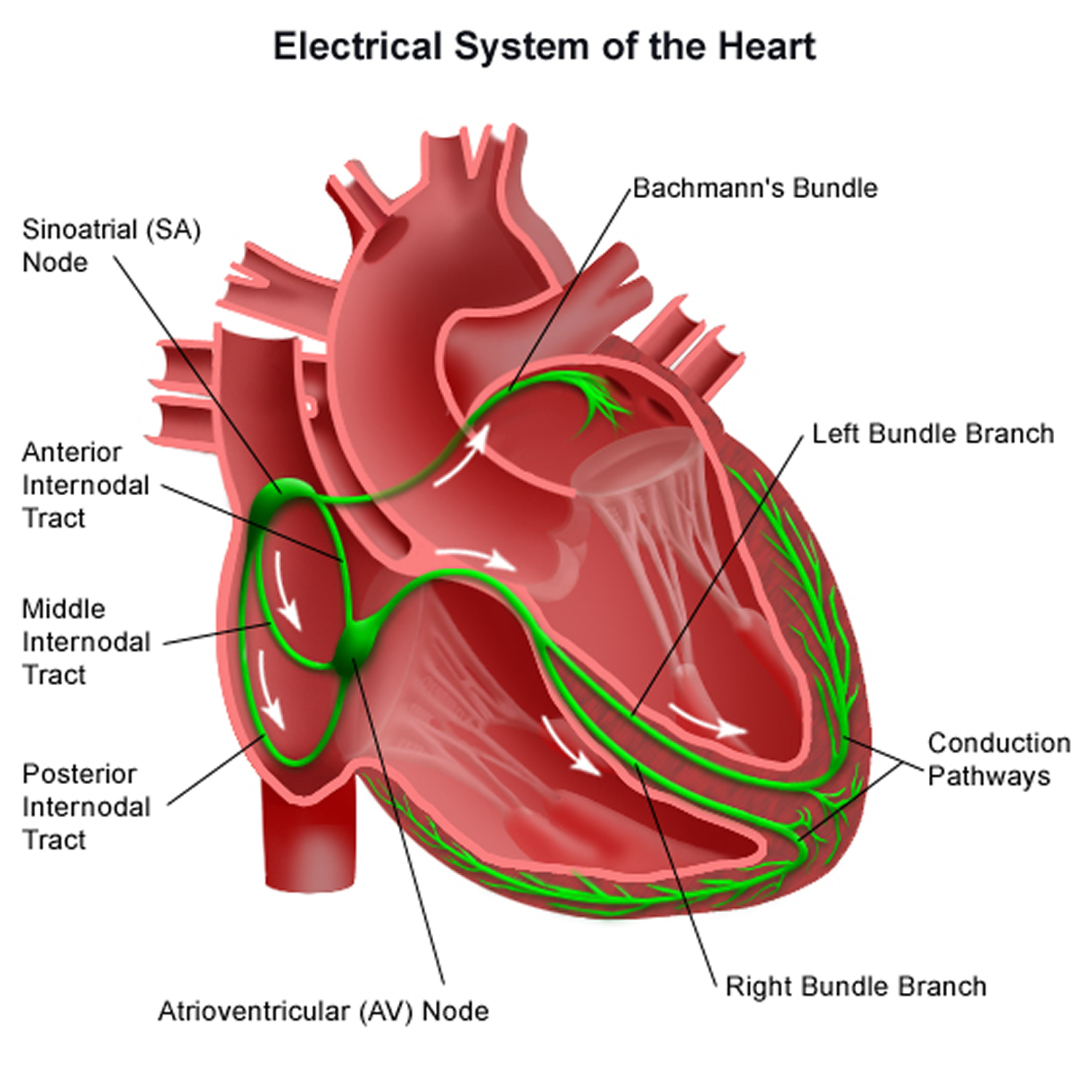
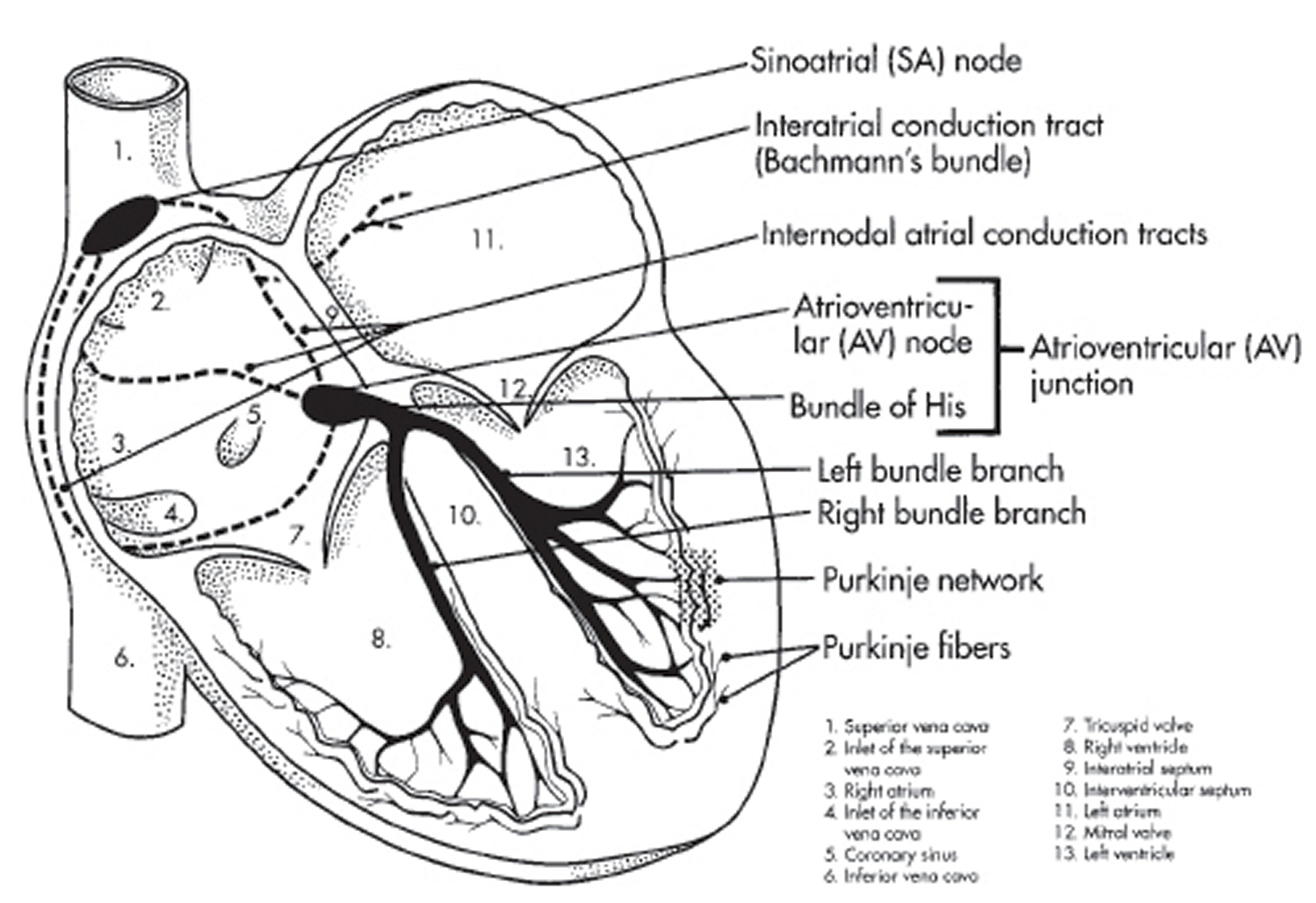
Normal heart electrical system
Your heart is made up of four chambers — two upper chambers (atria) and two lower chambers (ventricles). The rhythm of your heart is normally controlled by a mass of tissue in the right atrium (sinus node). The sinus node produces electrical impulses that generate each heartbeat.
These electrical impulses travel across the atria, causing muscle contractions that pump blood into the ventricles. The electrical impulses then arrive at a cluster of cells called the atrioventricular (AV) node — usually the only pathway for signals to travel from the atria to the ventricles. The AV node slows the electrical signal before sending it to the ventricles.
This slight delay allows the ventricles to fill with blood. When electrical impulses reach the ventricles, muscle contractions pump blood to the lungs and the rest of the body.
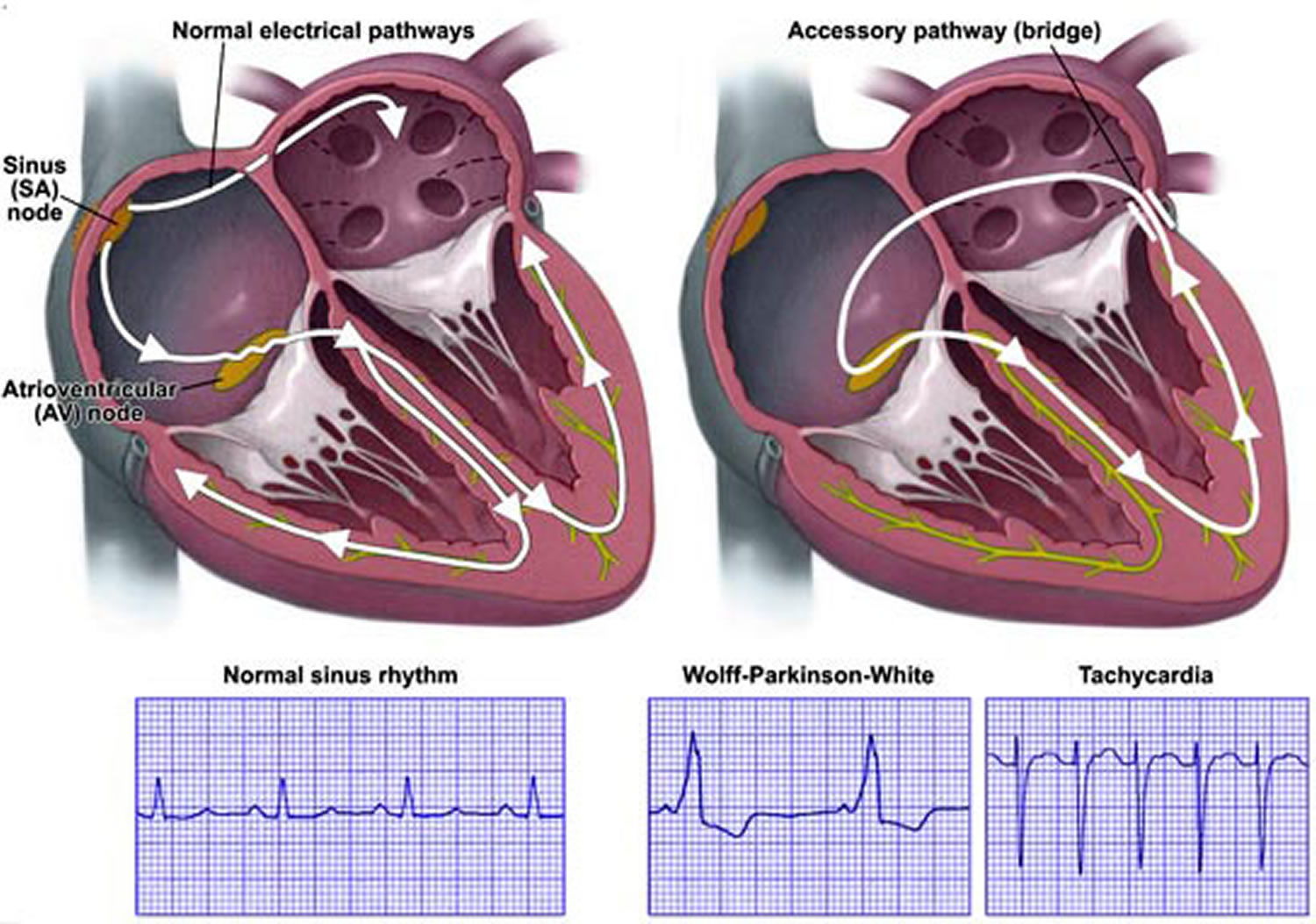
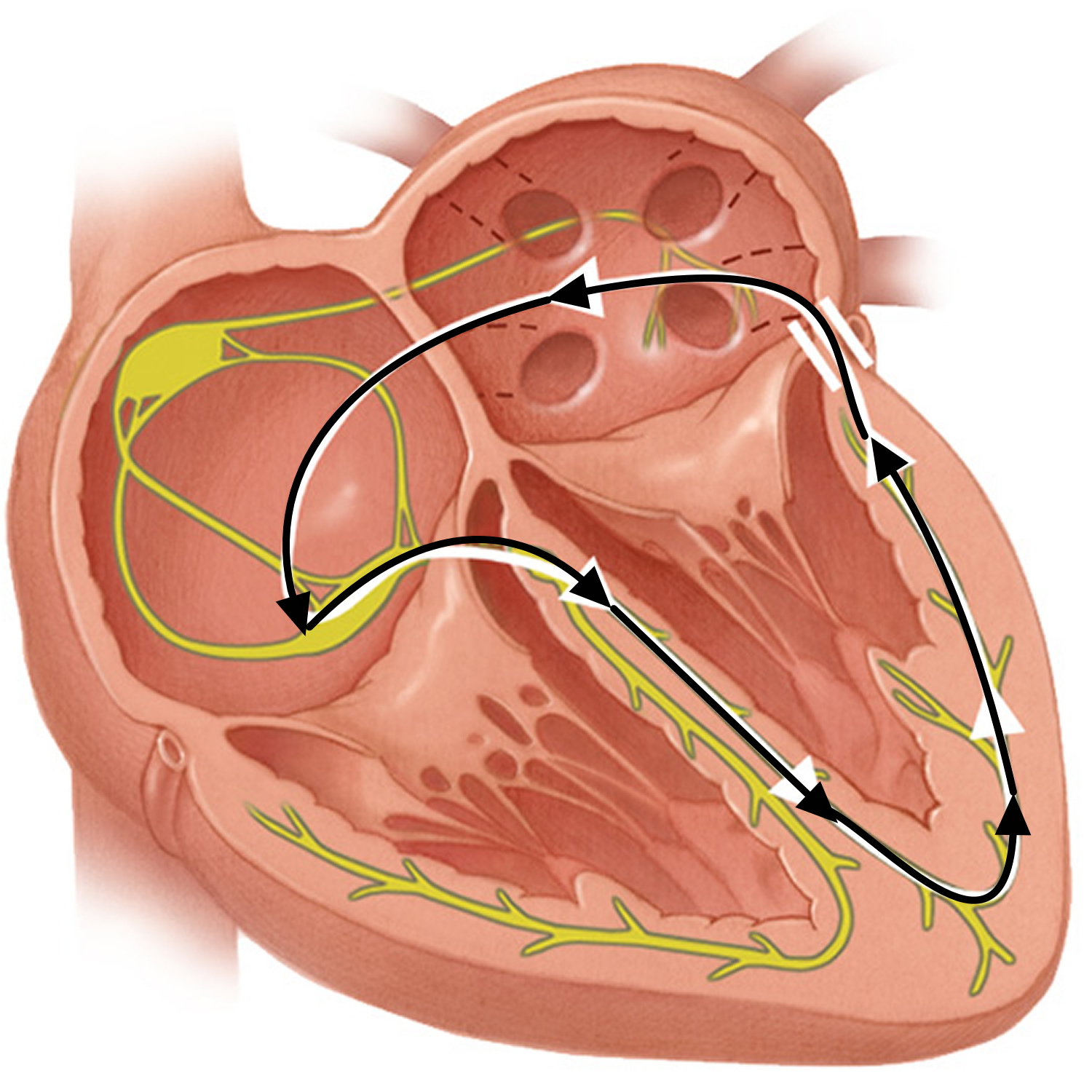
Figure 1. The heart’s electrical system
Abnormal electrical system in Wolff Parkinson White
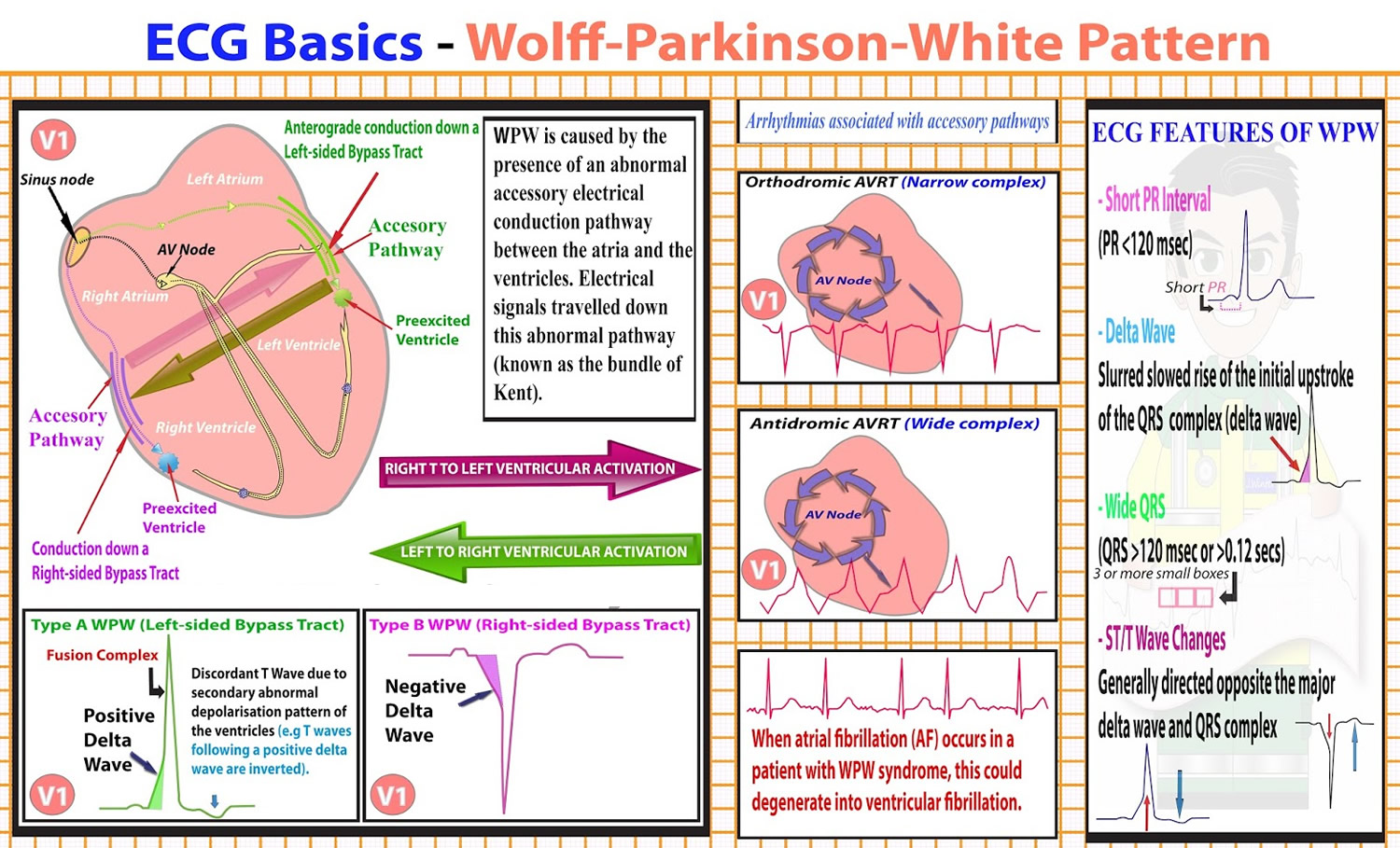
In Wolff Parkinson White syndrome, an extra electrical pathway connects the atria and ventricles, allowing electrical impulses to bypass the AV node. When the electrical impulses use this detour through the heart, the ventricles are activated too early.
The extra electrical pathway can cause two major types of rhythm disturbances:
- Looped electrical impulses. In Wolff Parkinson White, the heart’s electrical impulses travel down either the normal or the extra pathway and up the other one, creating a complete electrical loop of signals. This condition (AV reentrant tachycardia) sends impulses to the ventricles at a very rapid rate. As a result, the ventricles pump very quickly, causing rapid heartbeat.
- Disorganized electrical impulses. If electrical impulses don’t begin correctly in the right atrium, they may travel across the atria in a disorganized way, causing atrial fibrillation. The disorganized signals and the extra pathway of Wolff Parkinson White also can cause the ventricles to beat faster. As a result, the ventricles don’t have time to fill with blood and don’t pump enough blood to the body.
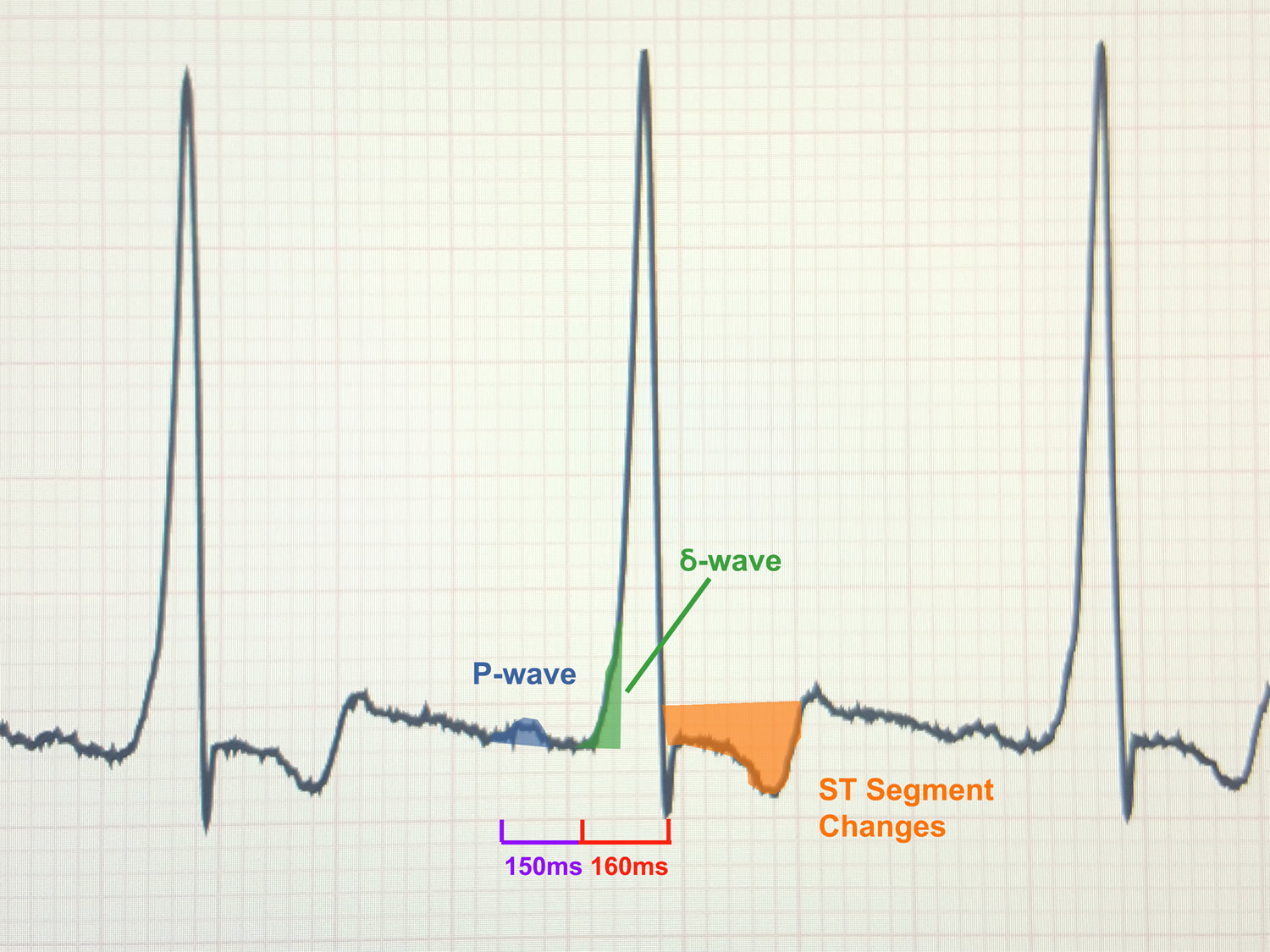
Figure 2. Wolff Parkinson White syndrome
 Note: In Wolff-Parkinson-White (WPW) syndrome, an extra electrical pathway between your heart’s upper chambers and lower chambers causes a rapid heartbeat.
Note: In Wolff-Parkinson-White (WPW) syndrome, an extra electrical pathway between your heart’s upper chambers and lower chambers causes a rapid heartbeat.Figure 3. Wolff Parkinson White syndrome ECG
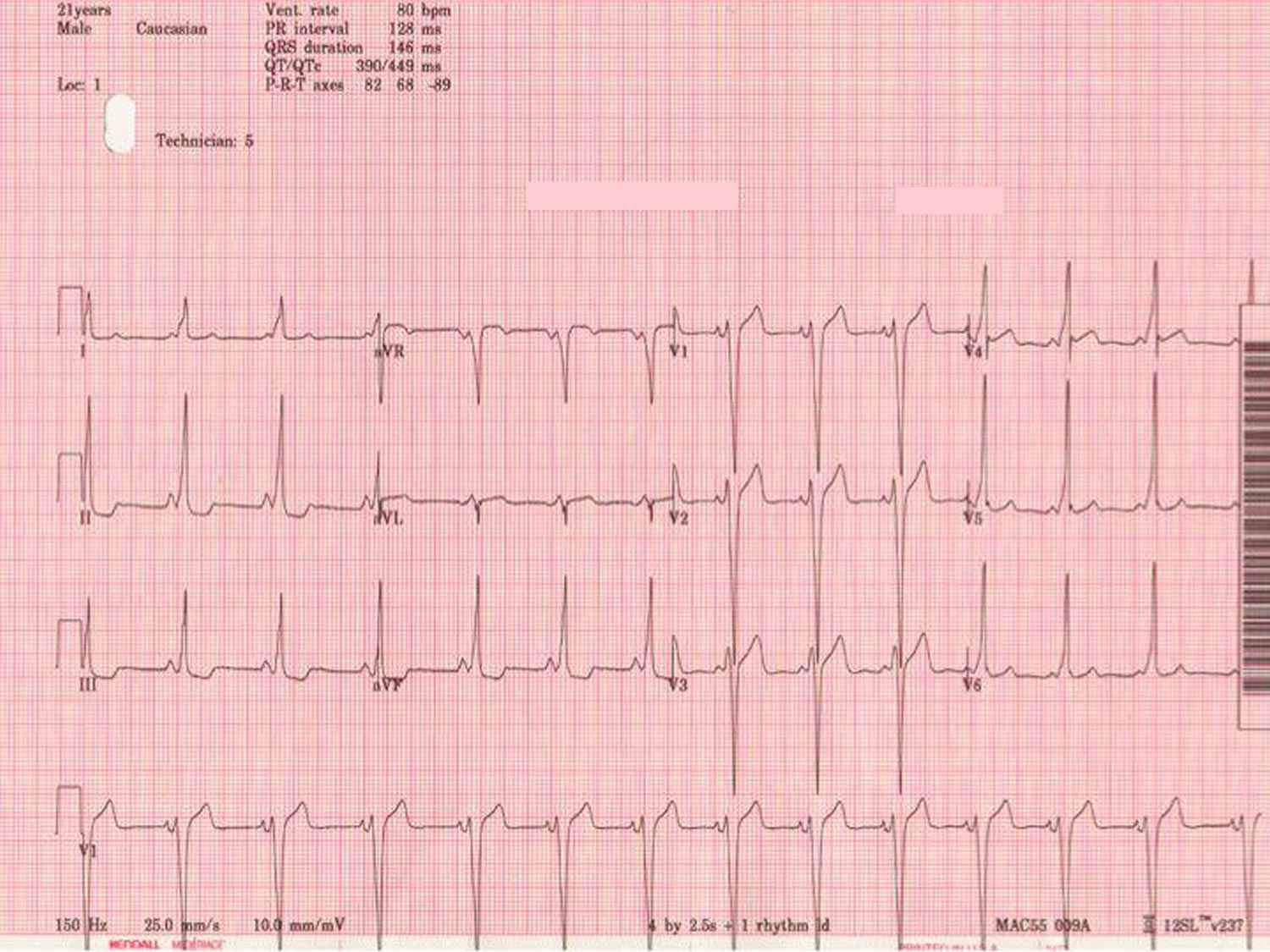
Figure 4. Wolff Parkinson White syndrome ECG (Classic Wolff-Parkinson-White electrocardiogram with short PR, QRS >120 ms, and delta wave.)
Figure 5. WPW syndrome ECG
Note: 12-lead electrocardiogram from asymptomatic 7-year-old boy with Wolff-Parkinson-White pattern. Delta waves are positive in I and aVL; negative in II, III, and aVF; isoelectric in V1; and positive in rest of precordial leads. This predicts posteroseptal location for accessory pathway.
Figure 6. Preexcited atrial fribrillation
Wolff Parkinson White syndrome causes
When the heart beats, its muscular walls contract (tighten and squeeze) to force blood out and around the body. They then relax, allowing the heart to fill with blood again. This is controlled by electrical signals.
In Wolff Parkinson White syndrome, there’s an extra electrical connection in the heart, which allows electrical signals to bypass the usual route and form a short circuit. This means the signals travel round and round in a loop, causing episodes where the heart beats very fast.
The extra electrical connection is caused by a strand of heart muscle that grows while the unborn baby is developing in the womb.
It’s not clear exactly why this happens. It just seems to occur randomly in some babies, although rare cases have been found to run in families.
Wolff Parkinson White is more common in males than in females.
Wolff Parkinson White syndrome complications
For many people, WPW syndrome doesn’t cause significant problems. But complications can occur, and it’s not always possible to know your risk of serious heart-related events. If the disorder is untreated, and particularly if you have other heart conditions, you may experience:
- Fainting spells
- Fast heartbeats
- Rarely, sudden death
Wolff Parkinson White syndrome symptoms
People of all ages, including infants, can experience the symptoms related to Wolff Parkinson White syndrome.
If you have Wolff Parkinson White syndrome, you’ll experience episodes where your heart suddenly starts racing, before stopping or slowing down abruptly. This rapid heart rate is called supraventricular tachycardia (SVT).
Symptoms of Wolff Parkinson White syndrome are the result of a fast heart rate. They most often appear for the first time in people in their teens or 20s.
Common symptoms of Wolff Parkinson White syndrome include:
- Sensation of rapid, fluttering or pounding heartbeats (palpitations)
- Dizziness or lightheadedness
- Shortness of breath
- Chest pain
- Sweating
- Feeling anxious
- Finding physical activity exhausting
- Passing out (fainting)
- Fatigue
- Anxiety
Symptoms in more-serious cases
About 10 to 30 percent of people with WPW syndrome occasionally experience a type of irregular heartbeat known as atrial fibrillation. In these people WPW signs and symptoms may include:
- Chest pain
- Chest tightness
- Difficulty breathing
- Fainting
Symptoms in infants
Signs and symptoms in infants with WPW syndrome may include:
- Ashen color
- Restlessness or irritability
- Rapid breathing
- Poor eating
An episode of a very fast heartbeat can begin suddenly and last for a few seconds, minutes or several hours. Rarely, they can last for days. Episodes can occur during exercise or while at rest. Caffeine or other stimulants and alcohol may be a trigger for some people.
How often they occur varies from person to person. Some people may have episodes on a daily basis, while others may only experience them a few times a year.
They normally occur randomly, without any identifiable cause, but they can sometimes be triggered by strenuous exercise or drinking a lot of alcohol or caffeine.
- Call your local emergency number for an ambulance if your symptoms are particularly severe or long-lasting.
If you’ve already been diagnosed with WPW syndrome and you experience an episode, first try the techniques you’ve been taught or take any medication you’ve been given (see below).
Over time, symptoms of Wolff Parkinson White may disappear in as many as 25 percent of people who experience them.
Wolff Parkinson White syndrome diagnosis
If your doctor thinks you might have Wolff Parkinson White syndrome after assessing your symptoms, they’ll probably recommend having an electrocardiogram (ECG) and will refer you to a cardiologist (heart specialist).
An ECG is a test that records your heart’s rhythm and electrical activity. Small discs called electrodes are stuck onto your arms, legs and chest and connected by wires to an ECG machine. The machine records the tiny electrical signals produced by your heart each time it beats.
If you have Wolff Parkinson White syndrome, the ECG will record an unusual pattern that isn’t usually present in people who don’t have the condition.
To confirm the diagnosis, you may be asked to wear a small portable ECG recorder so your heart rhythm can be recorded during an episode. A Holter monitor records your heart activity for 24 hours. An event recorder monitors heart activity when you experience symptoms of a fast heart rate. The recorder will trace your heart rate continuously over a few days, or when you switch it on at the start of an episode.
Electrophysiological testing. Thin, flexible tubes (catheters) tipped with electrodes are threaded through your blood vessels to various spots in your heart. The electrodes can precisely map the spread of electrical impulses during each heartbeat and identify an extra electrical pathway.
Wolff Parkinson White syndrome treatment
In many cases, episodes of abnormal heart activity associated with Wolff Parkinson White syndrome are harmless, don’t last long and settle down on their own without treatment.
You may therefore not need any treatment if your symptoms are mild or occur very occasionally, although you should still have regular check-ups so your heart can be monitored.
If your cardiologist recommends treatment, there are a number of options available. You can have treatment to either stop episodes when they occur, or prevent them occurring in the future.
Stopping an episode
There are three main techniques and treatments that can help stop episodes as they occur. These are:
- Vagal manoeuvers – techniques designed to stimulate the nerve that slows down the electrical signals in your heart. An example is the ‘Valsalva manoeuver’, where you hold your nose, close your mouth and exhale hard while straining as if you’re on the toilet.
- Medication – an injection of medicine such as adenosine can be given in hospital if vagal manoeuvers don’t help. It can block the abnormal electrical signals in your heart.
- Cardioversion – a type of electric shock therapy that jolts the heart back into a normal rhythm. This may be carried out in hospital if the above treatments don’t work.
Preventing further episodes
Techniques and treatments that can help prevent episodes include:
- Lifestyle changes – if your episodes are triggered by things such as strenuous exercise or alcohol, avoiding these may help. Your cardiologist can advise you about this.
- Medication – daily tablets of medication such as amiodarone can help prevent episodes by slowing down the electrical impulses in your heart.
- Radiofrequency catheter ablation – this procedure is commonly used nowadays to destroy the extra part of the heart causing the problems in the heart’s electrical system. Thin, flexible tubes (catheters) are threaded through blood vessels to your heart. Electrodes at the catheter tips are heated to destroy (ablate) the extra electrical pathway causing your condition. Radiofrequency ablation permanently corrects the heart-rhythm problems in most people with Wolff Parkinson White syndrome. It’s effective in around 95% of cases.Catheter ablation is very effective at preventing future episodes of Wolff Parkinson White syndrome (19 out of every 20 people treated will never have the problem again), but like all operations it carries a risk of complications. These include bruising and bleeding where the catheter was inserted. Any bruising will usually be small, but even if you have a large bruise it won’t require any treatment and will disappear within two weeks.There’s also a small risk (less than 1 in 100) of the heart’s normal electrical system being damaged. This is known as heart block, and if it happens you may need a permanent pacemaker to control your heart rhythm.You should discuss potential benefits and risks of catheter ablation with your surgeon (the electrophysiologist) before the procedure.