Contents
What is Whipple disease
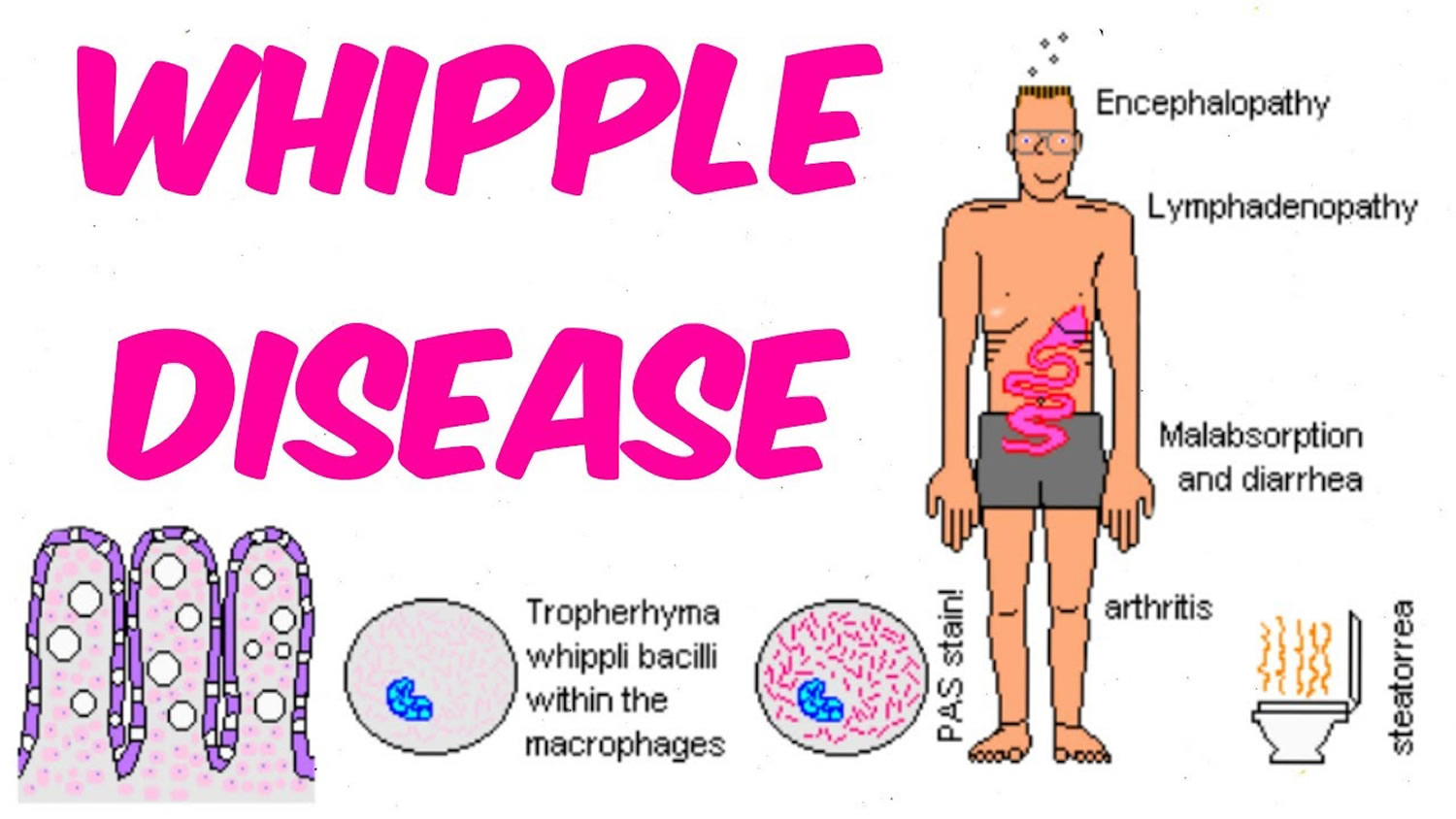
Whipple disease is a rare multi-system infectious bacterial disease that interferes with your body’s ability to metabolize fats. Whipple disease is caused by the bacterium Tropheryma whipplei, the disorder can affect any system in the body, including the brain, eyes, heart, joints, and lungs, but usually occurs in the gastrointestinal system primarily affects the small intestine.
Tropheryma whipplei bacterium initially affects the mucosal lining of your small intestine, forming small lesions within the intestinal wall. The bacterium also damages the fine, hair-like projections (villi) that line the small intestine. With time, the infection can spread to other parts of your body.
Not much is known about the bacterium. Although it seems readily present in the environment, scientists don’t really know where it comes from or how it’s transmitted to humans. Not everyone who carries the bacterium develops the disease. Some researchers believe that people with the disease may have a genetic defect in their immune system response that makes them more susceptible to becoming ill when exposed to the bacterium.
Whipple disease is extremely uncommon, affecting fewer than one in 1 million people.
The infection may spread to any organ in the body; however, it more commonly affects the:
- joints
- central nervous system, which includes the brain, the spinal cord, and nerves located throughout the body
- heart
- eyes
- lungs
Left untreated, Whipple disease gets worse and is usually life threatening and fatal.
Neurological symptoms occur in up to 40 percent of individuals and may include dementia, abnormalities of eye and facial muscle movements, headaches, seizures, loss of muscle control, memory loss, weakness, and vision problems. Gastrointestinal symptoms may include diarrhea, weight loss, fatigue, weakness, and abdominal bleeding and pain. Fever, cough, anemia, heart and lung damage, darkening of the skin, and joint soreness may also be present. The disease is more common in men and neurological symptoms are more common in individuals who have severe abdominal disease, Rarely, neurological symptoms may appear without gastrointestinal symptoms and can mimic symptoms of almost any neurologic disease.
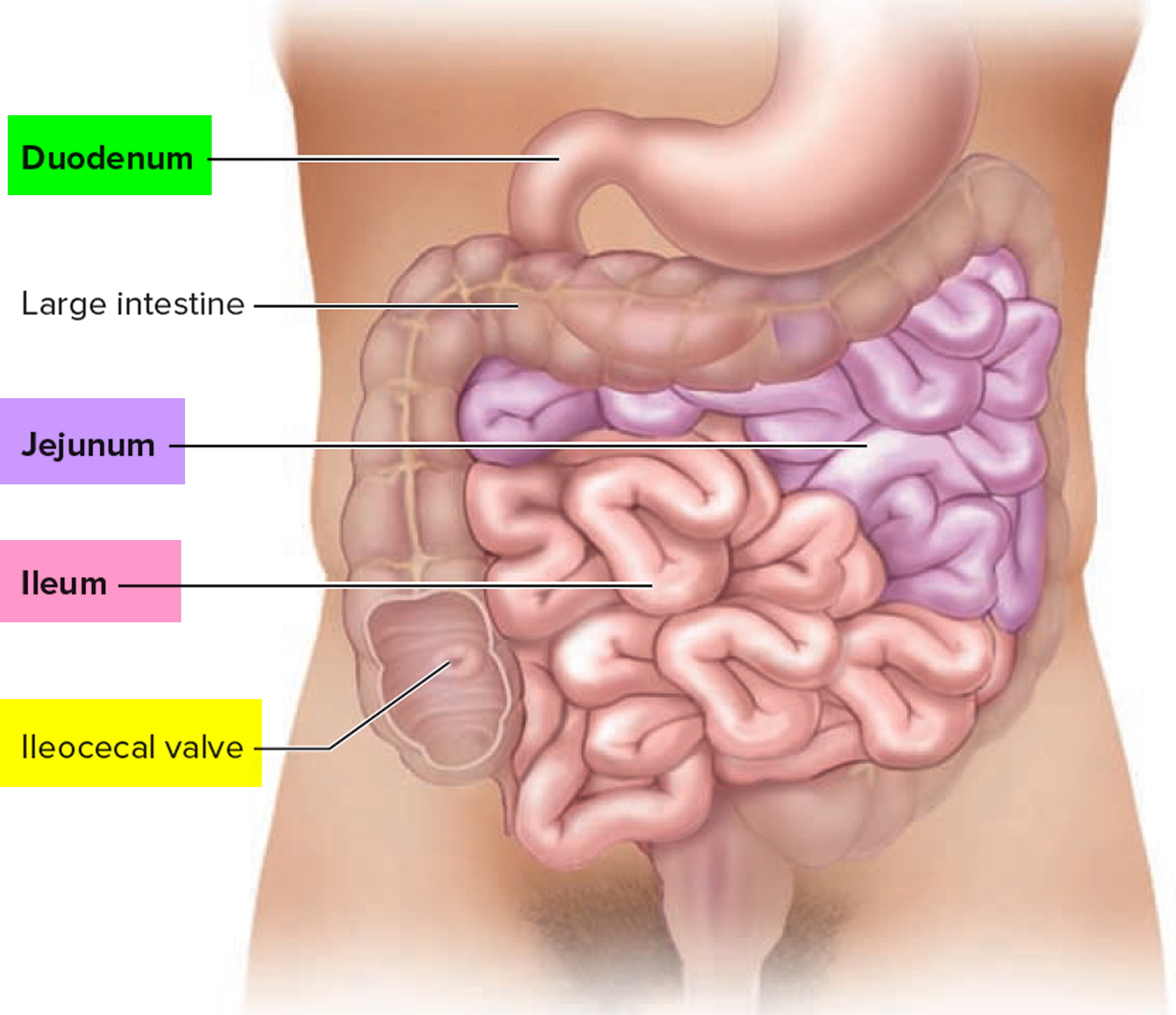
The small intestine
The small intestine is part of the upper gastrointestinal (GI) tract and is a tube-shaped organ between the stomach and large intestine. The upper GI tract also includes the mouth, esophagus, stomach, and duodenum, or the first part of the small intestine.
The small intestine is the longest part of the alimentary canal and it begins at the pyloric sphincter of the stomach, coils through the central and inferior part of the abdominal cavity, and eventually opens into the large intestine.
The term small intestine refers not to its length but to its diameter—about 2.5 cm (1 in.).
The small intestine is approximately 6 to 7 m long (range 3–7 m) with a narrowing diameter from beginning to end.
The small intestine consists of the duodenum, the jejunum, and the ileum.
The small intestine receives chyme from the stomach and secretions from the pancreas, liver, and gallbladder. It completes digestion of the nutrients in chyme, absorbs the products of digestion, and transports the residue to the large intestine.
Most food digestion and nutrient absorption take place in the small intestine. The small intestine the site of most enzymatic digestion and about 90 percent of all nutrients absorption and most of the rest occurs in the proximal portion of the large intestine. Its length alone provides a large surface area for digestion and absorption, and that area is further increased by circular folds, villi, and microvilli. Villi—tiny, fingerlike protrusions—line the inside of the small intestine. Villi normally let nutrients from food be absorbed through the walls of the small intestine into the bloodstream. Most digestive enzymes that operate within the small intestine are secreted not by the intestine, but by the pancreas. During digestion, the small intestine undergoes active segmentation movements, shuffling the chyme back and forth and thereby maximizing its contact with the nutrient-absorbing mucosa.
Peristalsis propels chyme through the small intestine in about 3–6 hours.
Figure 1. Small intestine
Whipple disease causes
Bacteria called Tropheryma whipplei (T. whipplei) cause Whipple disease. Tropheryma whipplei infection can cause internal sores, also called lesions, and thickening of tissues in the small intestine. The villi take on an abnormal, clublike appearance and the damaged intestinal lining does not properly absorb nutrients, causing diarrhea and malnutrition. Diarrhea is frequent, loose, and watery bowel movements. Malnutrition is a condition that develops when the body does not get the right amount of vitamins, minerals, and other nutrients it needs to maintain healthy tissues and organ function. Over time, the infection spreads to other parts of the person’s body and will damage other organs.
Who is more likely to develop Whipple disease?
Anyone can get Whipple disease. However, it is more common in Caucasian men between 40 and 60 years old 1. Whipple disease is rare, and fewer than one in 1 million people get this disease each year 2. The condition appears to be more common in farmers and other people who work outdoors and have frequent contact with soil and sewage wastewater 3.
Experts are not sure how Tropheryma whipplei infects people; however, scientists have noted:
- the bacteria are found in soil and sewage wastewater
- the bacteria are also found in people who are carriers of the disease—healthy individuals who have the bacteria, yet do not get sick
- Whipple disease is not transmitted from person to person
Some people may be more likely to develop Whipple disease because of genetic factors—related to genes, or traits passed from parent to child—that influence the body’s immune system. The immune system normally protects people from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances.
Risk factors for Whipple disease
Because so little is known about the bacterium that causes Whipple disease, risk factors for the disease haven’t been clearly identified. Based on available reports, it appears more likely to affect:
- Men
- People ages 40 to 60
- Whites in North America and Europe
- Farmers and other people who work outdoors and have frequent contact with sewage and wastewater.
Whipple disease prevention
Experts have not yet found a way to prevent Whipple disease.
Whipple disease prognosis
Generally, long-term antibiotic treatment to destroy the bacteria can relieve symptoms and cure the disease. If left untreated, the disease is progressive and fatal. Individuals with involvement of the central nervous system generally have a worse prognosis and may be left with permanent neurologic disability. Deficits may persist and relapses may still occur in individuals who receive appropriate treatment in a timely fashion. Prognosis may improve with earlier recognition, diagnosis, and treatment of the disorder.
Whipple disease complications
People with Whipple disease may have complications caused by malnutrition, which is due to damaged villi in the small intestine. As a result of delayed diagnosis or treatment, people may experience the following complications in other areas of the body:
- long-lasting nutritional deficiencies
- heart and heart valve damage
- brain damage
A person with Whipple disease may experience a relapse—a return of symptoms. Relapse can happen years after treatment and requires repeat treatments.
Whipple disease is a progressive and potentially fatal disease. Although the infection is rare, associated deaths continue to be reported, due in large part to late diagnoses and delayed treatment. Death often is caused by the spread of the infection to the central nervous system, which can cause irreversible damage.
Whipple disease symptoms
Signs and symptoms of Whipple disease can vary widely from person to person.
The most common symptoms of Whipple disease are:
- diarrhea
- weight loss caused by malabsorption
A person may not have diarrhea. Instead, other signs and symptoms of Whipple disease may appear, such as:
- abnormal yellow and white patches on the lining of the small intestine
- joint pain, with or without inflammation, that may appear off and on for years before other symptoms
- fatty or bloody stools
- abdominal cramps or bloating felt between the chest and groin
- enlarged lymph nodes—the small glands that make infection-fighting white blood cells
- loss of appetite
- fever
- fatigue, or feeling tired
- weakness
- anemia
- darkening of the skin
People with a more advanced stage of Whipple disease may have neurologic symptoms—those related to the central nervous system—such as:
- vision problems.
- memory problems or personality changes.
- facial numbness.
- headaches.
- muscle weakness or twitching.
- difficulty walking.
- hearing loss or ringing in the ears.
- dementia—the name for a group of symptoms caused by disorders that affect the brain. People with dementia may not be able to think well enough to do normal activities such as getting dressed or eating.
Less common symptoms of Whipple disease may include:
- chronic cough.
- chest pain.
- pericarditis—inflammation of the membrane surrounding the heart.
- heart failure—a long-lasting condition in which the heart cannot pump enough blood to meet the body’s needs. Heart failure does not mean the heart suddenly stops working.
Whipple disease diagnosis
A health care provider may use several tests and exams to diagnose Whipple disease, including the following:
- medical and family history
- physical exam
- blood tests
- upper GI endoscopy and enteroscopy
A patient may be referred to a gastroenterologist—a doctor who specializes in digestive diseases.
A health care provider may first try to rule out more common conditions with similar symptoms, including:
- Inflammatory rheumatic disease—characterized by inflammation and loss of function in one or more connecting or supporting structures of the body.
- Celiac disease—a digestive disease that damages the small intestine and interferes with the absorption of nutrients from food. People who have celiac disease cannot tolerate gluten, a protein in wheat, rye, and barley.
- Neurologic diseases—disorders of the central nervous system.
- Intra-abdominal lymphoma—abdominal cancer in part of the immune system called the lymphatic system.
- Mycobacterium avium complex—an infection that affects people with AIDS.
Medical and Family History
Taking a family and medical history can help a health care provider diagnose Whipple disease.
Physical Exam
A physical exam may help diagnose Whipple disease. During a physical exam, a health care provider usually:
- examines a patient’s body
- uses a stethoscope to listen to sounds related to the abdomen
- taps on specific areas of the patient’s body checking for pain or tenderness
Blood Tests
A technician or nurse draws a blood sample during an office visit or at a commercial facility and sends the sample to a lab for analysis. The health care provider may use blood tests to check for:
- Malabsorption. When the damaged villi do not absorb certain nutrients from food, the body has a shortage of protein, calories, and vitamins. Blood tests can show shortages of protein, calories, and vitamins in the body.
- Abnormal levels of electrolytes. Electrolytes—chemicals in body fluids, including sodium, potassium, magnesium, and chloride—regulate a person’s nerve and muscle function. A patient who has malabsorption or a lot of diarrhea may lose fluids and electrolytes, causing an imbalance in the body.
- Anemia. Anemia is a condition in which the body has fewer red blood cells than normal. A patient with Whipple disease does not absorb the proper nutrients to make enough red blood cells in the body, leading to anemia.
- T. whipplei DNA. Although not yet approved, rapid polymerase chain reaction diagnostic tests have been developed to detect T. whipplei DNA and may be useful in diagnosis.
Upper Gastrointestinal Endoscopy and Enteroscopy
An upper GI endoscopy and enteroscopy are procedures that use an endoscope—a small, flexible tube with a light—to see the upper GI tract. A health care provider performs these tests at a hospital or an outpatient center. The health care provider carefully feeds the endoscope down the esophagus and into the stomach and duodenum.
Once the endoscope is in the duodenum, the health care provider will use smaller tools and a smaller scope to see more of the small intestine. These additional procedures may include:
- Push enteroscopy, which uses a long endoscope to examine the upper portion of the small intestine.
- Double-balloon enteroscopy, which uses balloons to help move the endoscope through the entire small intestine.
- Capsule enteroscopy, during which the patient swallows a capsule containing a tiny camera. As the capsule passes through the GI tract, the camera will transmit images to a video monitor. Using this procedure, the health care provider can examine the entire digestive tract.
A small camera mounted on the endoscope transmits a video image to a monitor, allowing close examination of the intestinal lining. A health care provider may give a patient a liquid anesthetic to gargle or may spray anesthetic on the back of the patient’s throat. A health care provider will place an intravenous (IV) needle in a vein in the arm or hand to administer sedation. Sedatives help patients stay relaxed and comfortable. The test can show changes in the lining of the small intestine that can occur with Whipple disease.
The health care provider can use tiny tools passed through the endoscope to perform biopsies. A biopsy is a procedure that involves taking a piece of tissue for examination with a microscope. A pathologist—a doctor who specializes in examining tissues to diagnose diseases—examines the tissue from the stomach lining in a lab. The pathologist applies a special stain to the tissue and examines it for T. whipplei-infected cells with a microscope. Once the pathologist completes the examination of the tissue, he or she sends a report to the gastroenterologist for review.
An important step in diagnosing Whipple disease is taking a tissue sample (biopsy), usually from the lining of the small intestine. To do this, your doctor typically performs an upper endoscopy. The procedure uses a thin, flexible scope that passes through your mouth, throat, esophagus and stomach to your small intestine. The scope allows your doctor to view your digestive passages and obtain biopsies.
During the procedure, tissue samples are removed from several intestinal sites. This tissue is microscopically examined for the presence of disease-causing bacteria and their lesions, and specifically for Tropheryma whipplei bacteria. If biopsies of the small intestine don’t confirm the diagnosis, your doctor might biopsy an enlarged lymph node or perform other tests.
A DNA-based test known as polymerase chain reaction, which is available at some medical centers, can detect Tropheryma whipplei bacteria in biopsy specimens or spinal fluid samples.
Whipple disease treatment
The health care provider prescribes antibiotics to destroy the T. whipplei bacteria and treat Whipple disease. Health care providers choose antibiotics that treat the infection in the small intestine and cross the blood-brain barrier—a layer of tissue around the brain. Using antibiotics that cross the blood-brain barrier ensures destruction of any bacteria that may have entered the patient’s brain and central nervous system.
The health care provider usually prescribes IV antibiotics for the first 2 weeks of treatment. Most patients feel relief from symptoms within the first week or two. A nurse or technician places an IV in the patient’s arm to give the antibiotics.
IV antibiotics used to treat Whipple disease may include:
- ceftriaxone (Rocephin)
- meropenem (Merrem I.V.)
- penicillin G (Pfizerpen)
- streptomycin (Streptomycin)
After a patient completes the IV antibiotics, the health care provider will prescribe long-term oral antibiotics. Patients receive long-term treatment—at least 1 to 2 years—to cure the infection anywhere in the body.
Oral antibiotics may include:
- trimethoprim with sulfamethoxazole (Septra, Bactrim)—a combination antibiotic
- doxycycline (Vibramycin)
Patients should finish the prescribed course of antibiotics to ensure the medication destroyed all T. whipplei bacteria in the body. Patients who feel better may still have the bacteria in the small intestine or other areas of the body for 1 to 2 years. A health care provider will monitor the patient closely, repeat the blood tests, and repeat the upper GI endoscopy with biopsy during and after treatment to determine whether T. whipplei is still present.
People may relapse during or after treatment. A health care provider will prescribe additional or new antibiotics if a relapse occurs. Some people will relapse years after treatment, so it is important for patients to schedule routine follow-ups with the health care provider. Most patients have good outcomes with an early diagnosis and complete treatment.
Relapsing neurologic Whipple’s disease. (marked by bouts of worsening of symptoms) is sometimes treated with a combination of antibiotics and weekly injections of interfron gamma, a substance made by the body that activates the immune system.
Health care providers treat patients with neurologic symptoms at diagnosis or during relapse more aggressively. Treatment may include:
- a combination of antibiotics
- hydroxychloroquine (Plaquenil)—an antimalarial medication
- weekly injections of interferon gamma—a substance made by the body that activates the immune system
- corticosteroids—medications that decrease inflammation
Eating, Diet, and Nutrition
A person with Whipple disease and malabsorption may need:
- a diet high in calories and protein
- vitamins
- nutritional supplements
People with Whipple disease should discuss their nutritional needs with a dietitian or other health care professional and meet regularly with him or her to monitor changing nutritional needs.
Taking supplements
Because of the nutrient-absorption difficulties associated with Whipple disease, your doctor may recommend taking vitamin and mineral supplements to ensure adequate nutrition. Your body may require additional vitamin D, folic acid, calcium, iron and magnesium.
- Patil S, Fantry GT. Connecting the dots: the many systemic manifestations of Whipple disease. Gastroenterology & Hepatology. 2012:8(1);63–66.[↩]
- Whipple Disease. https://www.niddk.nih.gov/health-information/digestive-diseases/whipple-disease[↩]
- Maiwald M, von Herbay A, Relman DA. Whipple’s disease. In: Feldman M, ed. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 9th ed. Philadelphia: Saunders; 2010: 1833–1842.[↩]