Contents
What is Noonan syndrome
Noonan syndrome is a relatively common autosomal-dominant inherited disorder that affects many areas of the body. Noonan syndrome is characterized by mildly unusual facial features, short stature, chest deformity, congenital heart defects, bleeding problems, skeletal malformations, renal malformation, pubertal delay, webbed neck, developmental or behavioral problems, vision problems, hearing loss, and lymphedema. Noonan syndrome occurs in approximately 1 in 1,000 to 2,500 children are born with Noonan syndrome. It affects both sexes and all ethnic groups equally.
Boys frequently present with cryptorchidism (undescended testis) and manifest delayed puberty.
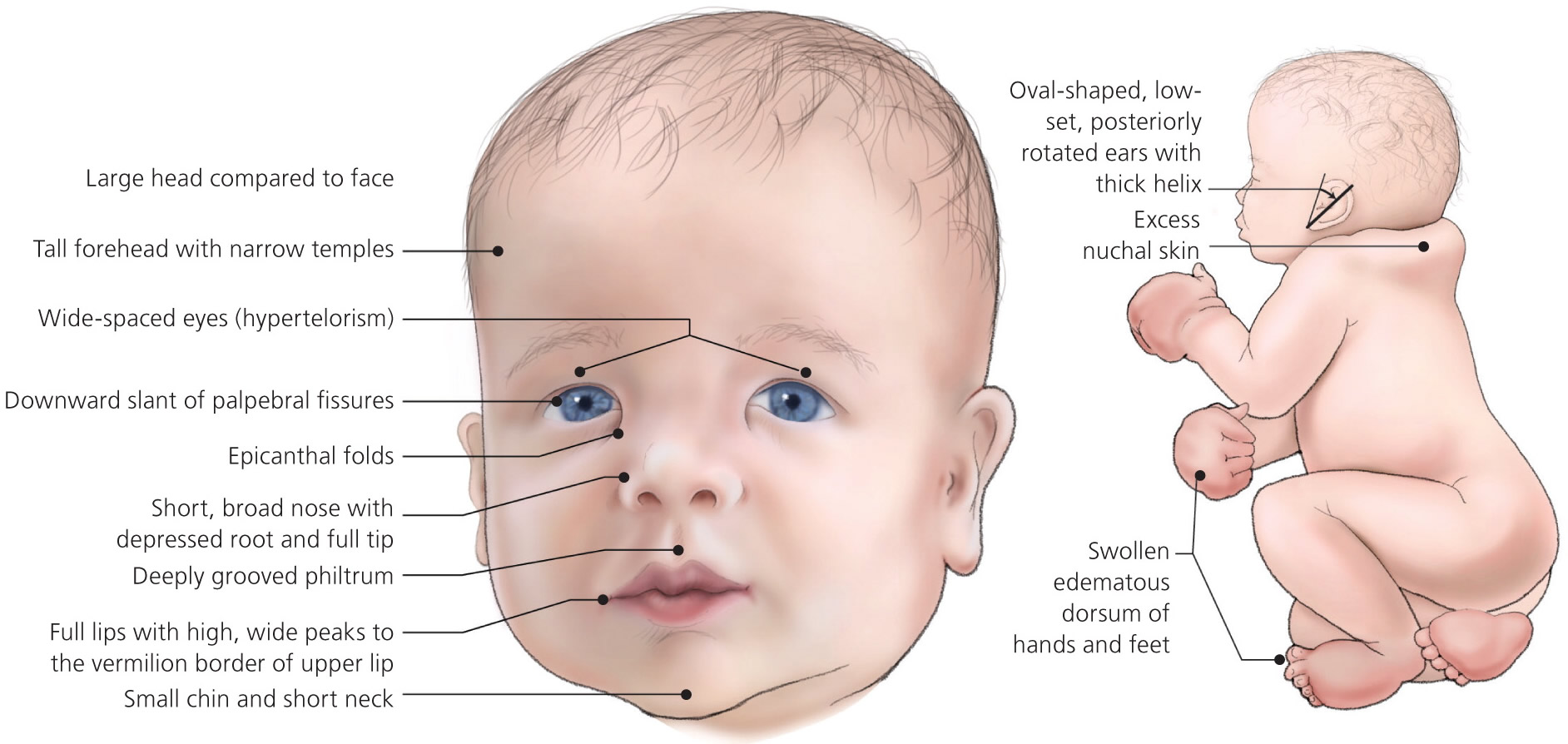
People with Noonan syndrome have distinctive facial features such as a deep groove in the area between the nose and mouth (philtrum) (Figure 1), widely spaced eyes that are usually pale blue or blue-green in color and low-set ears that are rotated backward (Figure 2). Affected individuals may have a high arch in the roof of the mouth (high-arched palate) (Figure 3), poor teeth alignment, and a small lower jaw (micrognathia). Many children with Noonan syndrome have a short neck, and both children and adults may have excess neck skin (also called webbing) and a low hairline at the back of the neck. Diagnosis can be made on the basis of clinical features, but may be missed in mildly affected patients.
The most common features of Noonan syndrome are:
- Unusual facial features, such as a broad forehead, drooping eyelids and a wider-than-usual distance between the eyes
- Short stature (restricted growth)
- Heart defects (congenital heart disease)
Noonan syndrome is caused by a fault in one of several genes. At least eight different faulty genes have been linked to the condition so far.
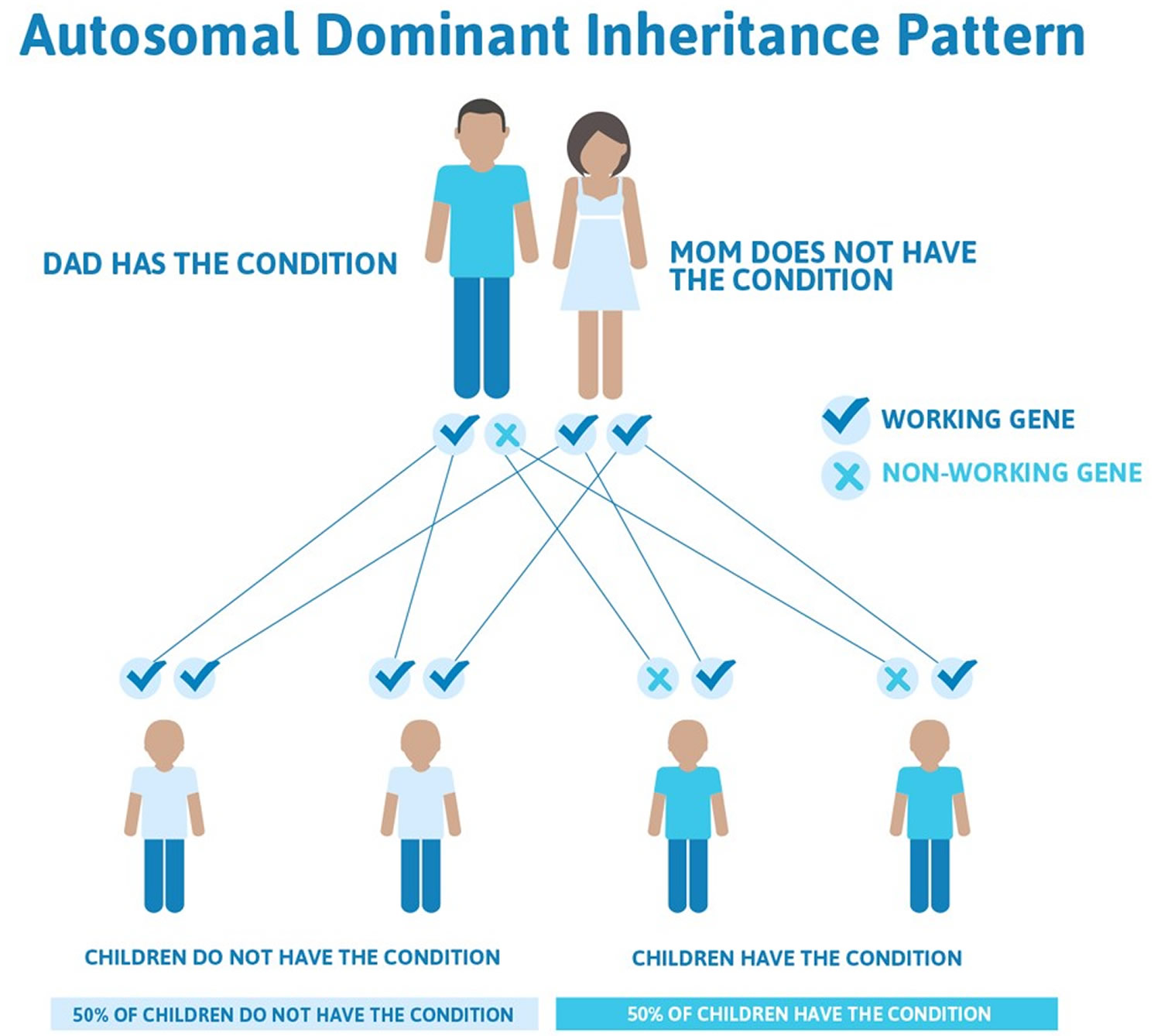
In some cases, the faulty gene associated with Noonan syndrome is inherited from one of the child’s parents. The parent with the faulty gene may or may not have obvious features of the condition themselves. Only one parent needs to carry the fault to pass it on and each child they have has a 50% chance of being born with the condition, which is consistent with an autosomal dominant mode of inheritance (see Figure 4 below).
In other cases, the disorder is caused by a new genetic fault (de novo or spontaneous mutations) that isn’t inherited from either parent. In these cases, the chance of the parents having another child with Noonan syndrome is very small (estimated to be less than 1%).
Molecular genetic testing can confirm diagnosis in 70% of cases and has important implications for genetic counseling and management. Most patients with Noonan syndrome are intellectually normal as adults, but some may require multidisciplinary evaluation and regular follow-up care.
Figure 1. Noonan syndrome deep philtrum
Figure 2. Noonan syndrome
Figure 3. Noonan syndrome high-arched palate
Between 50 and 70 percent of individuals with Noonan syndrome have short stature. At birth, they are usually a normal length and weight, but growth slows over time. Abnormal levels of growth hormone, a protein that is necessary for the normal growth of the body’s bones and tissues, may contribute to the slow growth.
Individuals with Noonan syndrome often have either a sunken chest (pectus excavatum) or a protruding chest (pectus carinatum). Some affected people may also have an abnormal side-to-side curvature of the spine (scoliosis).
Most people with Noonan syndrome have some form of critical congenital heart disease. The most common heart defect in these individuals is a narrowing of the valve that controls blood flow from the heart to the lungs (pulmonary valve stenosis). Some have hypertrophic cardiomyopathy, which enlarges and weakens the heart muscle.
A variety of bleeding disorders have been associated with Noonan syndrome. Some affected individuals have excessive bruising, nosebleeds, or prolonged bleeding following injury or surgery. Rarely, women with Noonan syndrome who have a bleeding disorder have excessive bleeding during menstruation (menorrhagia) or childbirth.
Adolescent males with Noonan syndrome typically experience delayed puberty. They go through puberty starting at age 13 or 14 and have a reduced pubertal growth spurt that results in shortened stature. Most males with Noonan syndrome have undescended testes (cryptorchidism), which may contribute to infertility (inability to father a child) later in life. Females with Noonan syndrome can experience delayed puberty but most have normal puberty and fertility.
Noonan syndrome can cause a variety of other signs and symptoms. Most children diagnosed with Noonan syndrome have normal intelligence, but a few have special educational needs, and some have intellectual disability. Some affected individuals have vision or hearing problems. Affected infants may have feeding problems, which typically get better by age 1 or 2 years. Infants with Noonan syndrome may be born with puffy hands and feet caused by a buildup of fluid (lymphedema), which can go away on its own. Older individuals can also develop lymphedema, usually in the ankles and lower legs.
Some people with Noonan syndrome develop cancer, particularly those involving the blood-forming cells (leukemia). It has been estimated that children with Noonan syndrome have an eightfold increased risk of developing leukemia or other cancers over age-matched peers.
Noonan syndrome is one of a group of related conditions, collectively known as RASopathies. These conditions all have similar signs and symptoms and are caused by changes in the same cell signaling pathway. In addition to Noonan syndrome, the RASopathies include cardiofaciocutaneous syndrome, Costello syndrome, neurofibromatosis type 1, Legius syndrome, and Noonan syndrome with multiple lentigines.
Treatment focuses on the individual symptom, and may include surgery for undescended testes in boys, optimization of cardiac function, and growth hormone treatment for short stature.
What causes Noonan syndrome
Noonan syndrome is inherited in an autosomal dominant pattern in about 30-75% of cases, which means one copy of the altered gene from one of the child’s parents is sufficient to cause the disorder. This means that only one parent has to carry a copy of one of the faulty genes to pass it on, and each child they have will have a 50% chance of being born with Noonan syndrome (see Figure 4). The parent carrying the faulty gene will also have the condition themselves, although it may be very mild.
In the remaining cases, the disorder is caused by a new genetic fault that isn’t inherited from either parent.
There’s no evidence to suggest the genetic fault is caused by environmental factors, such as diet or exposure to radiation.
Faults in at least eight different genes have been linked to Noonan syndrome. The most commonly altered genes are:
- the PTPN11 gene
- the SOS1 gene
- the RIT1 gene
- the RAF1 gene
- the KRAS gene
In around 1 in 5 cases, no specific genetic fault can be found.
The symptoms of Noonan syndrome are generally similar, no matter which gene is affected.
However, the faulty PTPN11 gene is commonly associated with pulmonary stenosis (a narrowed heart valve) and the faulty RAF1 gene is more often associated with cardiomyopathy (disease of the heart muscle).
Figure 4. Noonan syndrome autosomal dominant inheritance pattern
Genetic Changes
Mutations in multiple genes can cause Noonan syndrome. Mutations in the PTPN11 gene cause about half of all cases. SOS1 gene mutations cause an additional 10 to 15 percent, and RAF1 and RIT1 genes each account for about 5 percent of cases. Mutations in other genes each account for a small number of cases. The cause of Noonan syndrome in 15 to 20 percent of people with this disorder is unknown.
The PTPN11, SOS1, RAF1, and RIT1 genes all provide instructions for making proteins that are important in the RAS/MAPK cell signaling pathway, which is needed for cell division and growth (proliferation), the process by which cells mature to carry out specific functions (differentiation), and cell movement (migration). Many of the mutations in the genes associated with Noonan syndrome cause the resulting protein to be turned on (active) longer than normal, rather than promptly switching on and off in response to cell signals. This prolonged activation alters normal RAS/MAPK signaling, which disrupts the regulation of cell growth and division, leading to the characteristic features of Noonan syndrome.
Rarely, Noonan syndrome is associated with genes that are not involved in the RAS/MAPK cell signaling pathway. Researchers are working to determine how mutations in these genes can lead to the signs and symptoms of Noonan syndrome.
What are the chances of having another child with the condition?
If you have a child with Noonan syndrome and neither you or your partner have been diagnosed with the condition yourselves, you may be able to have a genetic blood test to see if either of you carry one of the faulty genes associated with the condition.
If one of you does carry a faulty gene or has been diagnosed with Noonan syndrome, there’s a 50% risk of each further child you have being born with the condition. In this case, it may be possible during pregnancy to test for the condition in a baby before he or she is born.
If neither of you carry one of the faulty genes, the risk of having another child with the condition is very small (estimated to be less than 1%).
Noonan syndrome prognosis
Noonan syndrome can range from being very mild to severe and life-threatening. The majority of patients with Noonan syndrome lead normal lives. Prognosis is largely dependent on the type and severity of cardiac disease, which may occur in 50% to 80% of cases.
In many cases, the problems associated with the condition can be treated successfully at a young age or become less prominent over time. Almost all children with Noonan syndrome reach adulthood and most are able to lead normal, independent lives.
However, problems such as heart defects can occasionally be severe and life-threatening. Some children may need emergency surgery to correct the problem as soon as possible, and most people with Noonan syndrome will need to have their heart monitored regularly throughout their life.
Noonan syndrome complications
Complications can arise that may require special attention, including:
- Developmental delays. If your child is affected developmentally, he or she may have difficulty with organization and spatial sense. Sometimes the developmental challenges are significant enough to require a special plan to address your child’s learning and educational needs.
- Bleeding and bruising. Sometimes the excessive bleeding common in Noonan syndrome isn’t discovered until a person has dental work or surgery and experiences excessive bleeding.
- Lymphatic complications. These usually involve excess fluid that gets stored in various places in the body. Sometimes fluid can collect in the space around the heart and lungs.
- Urinary tract complications. Structural abnormalities in the kidneys may increase the risk of urinary tract infections.
- Fertility issues. Males may have a low sperm count and other fertility problems because of undescended testicles or testicles that don’t function properly.
- Increased risk of cancer. There may be an increased risk of developing certain types of cancer, such as leukemia or certain types of tumors.
Noonan syndrome symptoms
Noonan syndrome can affect a person in many different ways and vary greatly among individuals and may be mild to severe. Not everyone with the disorder will share the same characteristics.
The three most common characteristics of Noonan syndrome are:
- Unusual facial features
- Short stature (restricted growth)
- Heart defects present at birth (congenital heart disease)
These are discussed in more detail below.
Unusual facial features
People with Noonan syndrome may have a characteristic facial appearance, although this isn’t always the case.
The following features may become apparent soon after birth:
- Eyes are wide-set and down-slanting with drooping eyelids (ptosis). Irises are pale blue or green.
- Ears are low-set and rotated rotated towards the back of the head
- Short, broad nose that is depressed at the top, with a wide base and bulbous tip.
- Mouth has a deep groove between the nose and the mouth and wide peaks in the upper lip. The crease that runs from the edge of the nose to the corner of the mouth becomes deeply grooved with age. Teeth may be crooked, the inside roof of the mouth (palate) may be highly arched and the lower jaw may be small.
- Facial features may appear coarse, but appear sharper with age. The face may appear droopy and expressionless.
- Head may appear large with a prominent forehead and a low hairline on the back of the head.
- Skin may appear thin and transparent with age.
- A broad forehead
- A small jaw
- A short neck with excess skin folds
- A lower-than-usual hairline at the back of the head and neck
Figure 5. Noonan syndrome baby
[Source 1]Children with Noonan syndrome also have abnormalities that affect the bones of the chest. For example, their chest may stick out or sink in, or they may have an usually wide chest with a large distance between the nipples.
These features may be more obvious in early childhood, but tend to become much less noticeable in adulthood.
Short stature
Children with Noonan syndrome are usually a normal length at birth. However, at around two years old you may notice that they don’t grow as quickly as other children of the same age.
Puberty (when a child begins to mature sexually and physically) typically occurs a few years later than normal and the expected growth spurt that normally happens during puberty is either reduced or doesn’t happen at all.
Medication known as human growth hormone can sometimes help children reach a more normal height. Left untreated, the average adult height for men with Noonan syndrome is 162.5cm (5ft 3in) and for women is 153cm (5ft).
Heart defects
Most children with Noonan syndrome will have some form of congenital heart disease. This is usually one of the following:
- Pulmonary stenosis – where the pulmonary valve (the valve that helps control the flow of blood from the heart to the lungs) is unusually narrow, which means the heart has to work much harder to pump blood into the lungs
- Hypertrophic cardiomyopathy – where the muscles of the heart are much larger than they should be, which can place a strain on the heart
- Septal defects – a hole between two of the chambers of the heart (a “hole in the heart”), which can cause the heart to enlarge and/or lead to high pressure in the lungs
- Irregular heart rhythm. This can occur with or without structural heart abnormalities. Irregular heart rhythm occurs in the majority of people with Noonan syndrome.
Other characteristics
Musculoskeletal issues
Some common issues can include:
- An unusually shaped chest often with a sunken sternum (pectus excavatum) or raised sternum (pectus carinatum)
- Wide-set nipples
- Short neck, often with extra folds of skin (webbed neck) or prominent neck muscles (trapezius)
- Deformities of the spine
Other less common characteristics of Noonan syndrome can include:
- Learning disability – children with Noonan syndrome tend to have a slightly lower-than-average IQ and a small number have learning disabilities, though these are often mild
- Feeding problems – babies with Noonan syndrome may have problems sucking and chewing, and may vomit soon after eating
- Behavioral problems – some children with Noonan syndrome may be fussy eaters, behave immaturely compared to children of a similar age, have problems with attention and have difficulty recognising or describing their or other people’s emotions
- Increased bruising or bleeding – sometimes the blood doesn’t clot properly, which can make children with Noonan syndrome more vulnerable to bruising and heavy bleeding from cuts or medical procedures
- Eye conditions – including a squint or cross-eye (strabismus – where the eyes point in different directions), a lazy eye (where one eye is less able to focus) and/or astigmatism (slightly blurred vision caused by the front of the eye being an irregular shape), nearsightedness (myopia) or farsightedness (hyperopia), rapid movement of the eyeballs (nystagmus) and cataracts
- Hearing problems – Noonan syndrome can cause hearing deficits due to nerve issues or to structural abnormalities in the inner ear bones
- Hypotonia – decreased muscle tone, which can mean it takes your child a bit longer to reach early developmental milestones
- Undescended testicles – in boys with Noonan syndrome, one or both testicles may fail to drop into the scrotum (sack of skin that holds the testicles)
- Infertility – especially if undescended testicles aren’t corrected at an early age, there’s a risk of boys with Noonan syndrome having reduced fertility; fertility in girls is usually unaffected
- Genital and kidney conditions – Many people, especially males, with Noonan syndrome can have problems with the genitals and kidneys.
- Testicles. Undescended testicles (cryptorchidism) are common in males.
- Puberty. Puberty may be delayed in both boys and girls.
- Fertility. Most females develop normal fertility. In males, however, fertility may not develop normally, often because of undescended testicles.
- Kidneys. Kidney problems are generally mild and occur in a fairly small number of people with Noonan syndrome.
- Lymphoedema – a build-up of fluid in the lymphatic system (a network of vessels and glands distributed throughout the body).These problems:
- May show up before or after birth or develop in the teenage years or adulthood
- Can be focused in a particular area of the body or widespread
- Most commonly cause excess fluid (lymphedema) on the back of the hands or top of the feet
- Bleeding – Noonan syndrome can cause excessive bleeding and bruising due to clotting defects or having too few platelets.
- Skin conditions – People with Noonan syndrome may have skin conditions, which most commonly are:
- Various problems that affect the color and texture of the skin
- Curly, coarse hair or sparse hair
- Bone marrow problems – a small number of people can develop an abnormal white blood cell count; this can sometimes get better on its own, but can occasionally turn into leukaemia
A variety of different tumors (cancerous growths) have also been found in people with Noonan syndrome, but it’s often not clear if these are caused by the condition or occur by chance.
Overall, the risk of developing cancer doesn’t appear to be much higher than for people without Noonan syndrome, although there may be a very small increased risk of some rare childhood cancers.
Noonan syndrome diagnosis
Noonan syndrome may be suspected if your child has some of the signs and symptoms associated with the condition.
These include:
- distinctive facial features
- short stature (restricted growth)
- a mild learning disability
- undescended testicles
- lymphoedema
However, these symptoms can have a number of different causes, so it’s difficult to make a diagnosis based on them alone.
You may be referred to a genetics specialist for genetic testing. In most cases, Noonan syndrome can be confirmed by a blood test for the various genetic mutations. However, in about 1 in 5 cases no specific mutation can be found, so a negative blood test will not rule out Noonan syndrome.
Further testing
If Noonan syndrome has been confirmed or is strongly suspected, further tests are needed to establish the extent of the symptoms. These tests may include:
- an electrocardiogram (ECG) – where electrodes (small, metallic discs placed on the skin) measure the electrical activity of the heart
- an echocardiogram – an ultrasound scan of the heart
- an educational assessment
- blood tests to check how well the blood clots
- eye tests – to check for problems such as squints or blurred vision
- hearing tests – to check for problems such as hearing loss caused by otitis media or damage to the cells or nerves inside the ear
Some of these tests may need to be repeated regularly after the diagnosis, to monitor the condition.
Diagnosis during pregnancy
If you’re pregnant, it may be possible to test your unborn baby for Noonan syndrome if:
- you, your partner or a close family member has been found to carry one of the faulty genes associated with the condition
- routine ultrasound scans detect possible signs of the condition in your baby, such as polyhydramnios (an excessive amount of amniotic fluid), pleural effusion (fluid in the space around the lungs) or a build-up of fluid in certain other parts of the body
Testing for Noonan syndrome during pregnancy involves collecting a sample of your baby’s DNA and checking it for any of the faulty genes associated with the condition.
This can be done using either chorionic villus sampling (where a sample of cells is removed from the placenta) or amniocentesis (where a sample of amniotic fluid is removed). Both of these tests carry around a 1% chance of causing a miscarriage.
If your baby is found to have one of the faulty genes, a genetic counselor will talk to you about what the test result means and what your options are.
Noonan syndrome treatment
There is no single treatment for Noonan syndrome, but it’s possible to treat many aspects of the disorder.
Your child may initially need quite a lot of treatment and support to help manage the various problems they have. However, they’ll typically need much less care as they get older.
Although they’ll probably need to have some routine tests and checks to monitor their condition, most adults with Noonan syndrome can lead a normal life.
Heart defects
A full assessment of your child’s heart function should be carried out when Noonan syndrome is diagnosed. This will help to determine if they have any type of congenital heart disease.
The treatment your child needs will depend on the type of heart defect they have and how severe it is.
- Pulmonary stenosis may not need any treatment if it’s mild, but more severe cases may require an operation to widen the narrowed heart valve or replace it with a new valve.
- Hypertrophic cardiomyopathy may need to be treated with medication such as beta-blockers or surgery to remove or destroy some of the excess heart muscle.
- Septal defects may not need any treatment if they’re small because they may get better with age, but more severe cases may require an operation to seal the hole in the heart.
Regular tests to check heart function will normally be carried out into adulthood.
Restricted growth
Your child’s size and growth rate will be regularly assessed throughout their childhood. If your child’s growth rate is thought to be seriously reduced, treatment with human growth hormone may be suggested.
Treatment usually starts at around four or five years of age and continues until your child stops growing. A medication called somatropin is most often used. This is given as a single daily injection.
Side effects of somatropin are uncommon, although your child is likely to experience some temporary soreness, itchiness and redness at the site of the injection.
Feeding and speech problems
In children with Noonan syndrome, weak muscles in the mouth can sometimes cause speech and feeding problems. They may be referred to a speech therapist for help and support.
The speech therapist will help your child develop the muscles in their mouth and try to teach them how to use their muscles more effectively.
In particularly severe cases of poor feeding, your baby may need a feeding tube for a few months.
Undescended testicles
If you have a baby boy with an undescended testicle or testicles that don’t descend naturally within a few months of birth, corrective surgery is usually recommended.
This is normally carried out before two years of age, because treating the problem early on should increase the chances of fertility being unaffected.
A surgical procedure known as an orchidopexy is the usual treatment for undescended testicles. It involves making a small cut in your child’s tummy or groin and moving the testicle(s) into the correct position.
Learning disabilities
If your child is diagnosed with a learning disability, it doesn’t necessarily mean they can’t be taught in a mainstream school. However, children with more severe disabilities may benefit from attending a specialist school.
To ensure your child gets the support they need, an Education, Health and Care plan may need to be drawn up. This is a type of care plan designed to meet the child’s health and educational requirements.
Other health conditions
Click on the links below to find out about treatment for some of the other problems that can affect people with Noonan syndrome:
- treating astigmatism
- treating hypotonia
- treating lazy eye
- treating lymphoedema
- treating a squint
Coping and support
A number of support groups are available for people with Noonan syndrome and their families. Talk to your doctor about finding a support group in your area. Also ask about trustworthy resources on the internet that can direct you to local support groups and sources of information about Noonan syndrome.
- Noonan Syndrome. Am Fam Physician. 2014 Jan 1;89(1):37-43. https://www.aafp.org/afp/2014/0101/p37.html[↩]