Contents
What is a molar pregnancy
A molar pregnancy also known as hydatidiform mole, is an uncommon complication of pregnancy where a fetus doesn’t form properly in the womb and a baby doesn’t develop. A lump of abnormal cells grows in the womb instead of a healthy fetus. There are two types of molar pregnancies, complete and partial.
- A complete molar pregnancy is an androgenetic pregnancy (i.e. a pregnancy which contains only paternal and non maternal chromosomes). These pregnancies occur when a single sperm fertilizes an “empty” egg (i.e. an egg containing no DNA) and then duplicates its own chromosomes (rather than joining with the maternal chromosome, as is the case in a normal pregnancy). The pregnancy that results contains no fetal tissue and resembles grape-like cysts that fill the uterine cavity.
- A partial molar pregnancy occurs when more than one sperm fertilizes a normal egg, resulting in a pregnancy where both the fetus and placenta are abnormal. The term “partial” is used because the placenta contains both normal tissue and grape-like cysts similar to that seen in complete moles. Partial molar pregnancy is known as triploid gestation (i.e. pregnancy that have two paternal and one maternal chromosomes). They occur when two sperm fertilize a single egg. As a result, the embryo has 69 chromosomes instead of 46.
- Some 10% of all hydatidiform moles will become malignant. The risk of developing a malignancy after a complete mole is approximately 20% and after a partial mole is approximately 1-4%. Malignant gestational trophoblastic disease spreads locally within the muscular wall of the uterus (called invasive mole) or spreads (called metastasis) more widely to other parts of the body, most commonly the lungs, liver or brain, which requires treatment.
A molar pregnancy (hydatidiform mole) is a type of gestational trophoblastic disease that arises when fertilization of an egg cell results in an abnormal pregnancy. Eighty percent of molar pregnancies are benign, in that they cause no further trouble after they are removed from the uterus.
An estimated 1-3 in 1000 pregnancies are affected by benign hydatidiform moles, however incidence varies internationally and is highest in the Asian region. Around 8% of women with a previous molar pregnancy will develop persistent trophoblastic disease (i.e. recurring hydatidiform moles). Molar pregnancy occurs in only one of every 1,000–1,200 pregnancies in the United States.
Although a hydatidiform mole is not cancer and rarely even becomes cancerous, it can behave in similar ways. Most of the treatment is aimed at stopping the disease process long before any of these things happen.
A molar pregnancy can usually be treated with a simple procedure to remove the growth of cells from the womb, but cells are sometimes left over and further treatment is needed to remove them.
The risk that a mole will develop in a future pregnancy is only one to two percent. The vast majority of couples go on to have healthy babies.
You may be especially concerned about becoming pregnant again in the future. However, it is highly unlikely that you will suffer another molar pregnancy. In fact, the chance of experiencing a second molar pregnancy is only about 1 in 80 to 1 in 100. The vast majority of couples go on to have healthy babies.
It is usually recommended that those who have had treatment wait at least one year from the point of treatment finishing before becoming pregnant again. This is because your human chorionic gonadotropin (hCG) levels need to be continuously monitored at regular intervals for signs of the mole returning and also to allow the chemotherapy to leave your body – chemotherapy can cause devastating results in pregnancies. After the mandatory one-year wait, you should receive the all clear from your treatment center/consultant and can start trying again. This is the standard remission time but each individual is different.
What is gestational trophoblastic disease?
Gestational trophoblastic disease is a a rare group of interrelated tumors in which tumors grow inside a woman’s uterus (womb) 1. The abnormal cells start in the tissue that would normally become the placenta. The placenta is the organ that develops during pregnancy to feed the fetus.
A baby may or may not develop during these types of pregnancies.
More than 80% of gestational trophoblastic disease cases are noncancerous. All forms of gestational trophoblastic disease can be treated, and in the great majority of cases the treatment results in a cure. Most women who have had a single incidence of gestational trophoblastic disease can go on to have normal pregnancies.
There are three main types of gestational trophoblastic disease:
- Choriocarcinoma (a type of cancer). Choriocarcinoma is a highly malignant form of gestational trophoblastic disease that spreads rapidly throughout the body and requires vigorous treatment. It may have begun as a molar pregnancy or from tissue that remains in the uterus following a miscarriage or childbirth. Choriocarcinoma is rare, arising in only one of every 20,000–40,000 pregnancies.
- Hydatiform mole (also called a molar pregnancy)
- Placental-Site Trophoblastic Tumor. Placental-site gestational trophoblastic disease is a very rare form of the disease that arises in the uterus at the site where the placenta was attached. These tumors penetrate the muscle layer of the uterus and usually do not spread to other parts of the body. Placental site trophoblastic tumors, unlike choriocarcinoma, are not very sensitive to chemotherapy. Since in most cases the tumor is localized to the uterus, hysterectomy is generally curative. When the disease spreads outside the uterus, high-dose chemotherapy is used with some success.
Different types/stages of molar pregnancy
Hydatidiform mole
Hydatidiform moles are benign and confined to the uterine cavity, however in about 10% of cases they develop into malignant tumors. Malignant gestational trophoblastic disease tumors are either:
- Invasive hydatidiform moles: previously benign hydatidiform moles which have transformed;
- Choriocarcinoma: a very aggressive form of GTD, which can occur up to 15 years following the previous pregnancy;
- Placental site trophoblastic tumors: a tumor of the placental site which typically occurs many years after the last pregnancy and is often resistant to chemotherapy; or
- Epitheliod trophoblastic tumor: similar to placental site trophoblastic tumors.
These malignant forms of gestational trophoblastic disease most commonly occur after a previous benign molar pregnancy, however they can also occur after an apparently normal pregnancy (either carried to term or terminated through spontaneous or induced abortion) or an ectopic pregnancy. The extent and sites of metastasis vary depending on the type of tumor:
Invasive hydatidiform moles typically metastasize locally (i.e. the tumor progressively grows into the uterus walls), however in rare instances metastasis to the vagina, lungs and brain have been documented.
Choriocarcinomas is a very rare but curable form of cancer where the placenta becomes malignant. This can arise from a molar pregnancy or an otherwise normal pregnancy or miscarriage. Choriocarcinoma can also spread throughout the body, usually to organs like the lungs, liver and brain and less commonly to the vagina, kidneys and bowel.
Molar pregnancy causes
A molar pregnancy is caused by an abnormally fertilized egg. Human cells normally contain 23 pairs of chromosomes. One chromosome in each pair comes from the father, the other from the mother.
- In a complete molar pregnancy, an empty egg is fertilized by one or two sperm, and all of the genetic material is from the father. In this situation, the chromosomes from the mother’s egg are lost or inactivated and the father’s chromosomes are duplicated.
- In a partial or incomplete molar pregnancy, the mother’s chromosomes remain but the father provides two sets of chromosomes. As a result, the embryo has 69 chromosomes instead of 46. This most often occurs when two sperm fertilize an egg, resulting in an extra copy of the father’s genetic material.
Molar pregnancy is thought to be caused by a problem with the genetic information of an egg or sperm.
Factors that may increase your risk of having a molar pregnancy include:
- Age. Are younger than 20 or older than 35. The risk is higher if you’re older than 40.
- History of molar pregnancy, particularly if you’ve had two or more
- Possible ovulatory disorders
- History of miscarriage
- A diet low in carotene (a form of vitamin A). Women with low carotene or vitamin A intake have a higher rate of complete molar pregnancy
- Living in certain geographic locales (especially Southeast Asia and Mexico)
It is however, worthwhile noting, that the number of times a women has been pregnant doesn’t influence her risk.
Risk Factors for molar pregnancy
Although doctors cannot always explain why a woman develops gestational trophoblastic disease, there are a number of factors that may increase a woman’s risk of developing the disease:
- Age: Since gestational trophoblastic disease develops from pregnancy, this disease only occurs in women in the childbearing age group. The risk of developing gestational trophoblastic disease increases with age, particularly after age 40.
- Prior gestational trophoblastic disease: Women who have had a previous molar pregnancy or choriocarcinoma are at increased risk of another. For example, a second molar pregnancy occurs ten times more frequently than the first mole.
- Diet: Women whose diets are low in beta carotene or vitamin A appear to have a higher risk of developing complete molar pregnancy.
- Use of Oral Contraceptives: Long-term use of contraceptives appear to increase the risk of partial molar pregnancy.
- Irregular periods: Women who have irregular periods appear to have an increased risk of partial molar pregnancy.
- Fertility problems: Women who have had spontaneous abortions appear to have an increased risk of complete and partial molar pregnancy.
Molar pregnancy prevention
As so little is understood about how and why hydatidiform moles occur, they’re difficult to prevent. However, good healthy nutrition may decrease the risk of one developing and any other common pregnancy complications.
If you’ve had a molar pregnancy, your doctor may recommend waiting for six months to one year before trying to become pregnant. The risk of recurrence is low, but higher than the risk for women with no previous history of molar pregnancy.
During any subsequent pregnancies, your doctor may do early ultrasounds to monitor your condition and offer reassurance of normal development. Your doctor may also discuss prenatal genetic testing, which can be used to diagnose a molar pregnancy.
Molar pregnancy complications
After a molar pregnancy has been removed, molar tissue may remain and continue to grow. This is called persistent gestational trophoblastic neoplasia. This occurs in approximately 15 to 20 percent of complete molar pregnancies, and up to 5 percent of partial molar pregnancies.
One sign of persistent gestational trophoblastic neoplasia is a high level of human chorionic gonadotropin (HCG) — a pregnancy hormone — after the molar pregnancy has been removed. In some cases, an invasive hydatidiform mole penetrates deep into the middle layer of the uterine wall, which causes vaginal bleeding.
Persistent gestational trophoblastic neoplasia can nearly always be successfully treated, most often with chemotherapy. Another treatment option is removal of the uterus (hysterectomy).
Rarely, a cancerous form of gestational trophoblastic neoplasia known as choriocarcinoma develops and spreads to other organs. Choriocarcinoma is usually successfully treated with multiple cancer drugs. A complete molar pregnancy is more likely to have this complication than a partial molar pregnancy.
If metastatic (disease in other parts of the body) trophoblastic disease is vigorously treated, the cure rate is also 100%.
Widely metastatic disease if recognized promptly and treated aggressively with multi-agent chemotherapy (cocktail) and surgery, the cure rate is about 98%.
Molar pregnancy signs and symptoms
There are often no signs that a pregnancy is a molar pregnancy.
It may only be spotted during a routine ultrasound scan at 8-14 weeks or found during tests carried out after a miscarriage.
Some women with a molar pregnancy have:
- vaginal bleeding or a dark discharge from the vagina in early pregnancy (usually in the first three months) – this may contain small, grape-like lumps
- severe morning sickness (nausea and vomiting)
- an unusually swollen tummy
- pelvic pressure or pain
But some of these symptoms are fairly common in pregnancy and aren’t necessarily a sign that anything is wrong with your baby.
Signs of a molar pregnancy
- Rapid uterine growth — the uterus is too large for the stage of pregnancy
- High blood pressure
- Preeclampsia — a condition that causes high blood pressure and protein in the urine after 20 weeks of pregnancy
- Ovarian cysts
- Anemia
- Overactive thyroid (hyperthyroidism)
Women who develop choriocarcinoma may be symptom free or experience symptoms based on which organ(s) are involved:
- Uterus: Vaginal bleeding, discharge
- Lung: Coughing up blood, shortness of breath, chest pain
- Liver: Abdominal pain
- Brain: Headache, trouble with vision, weakness or loss of function, convulsion
- Kidney: Blood in urine
- Bowel: Blood in stool
Molar pregnancy diagnosis
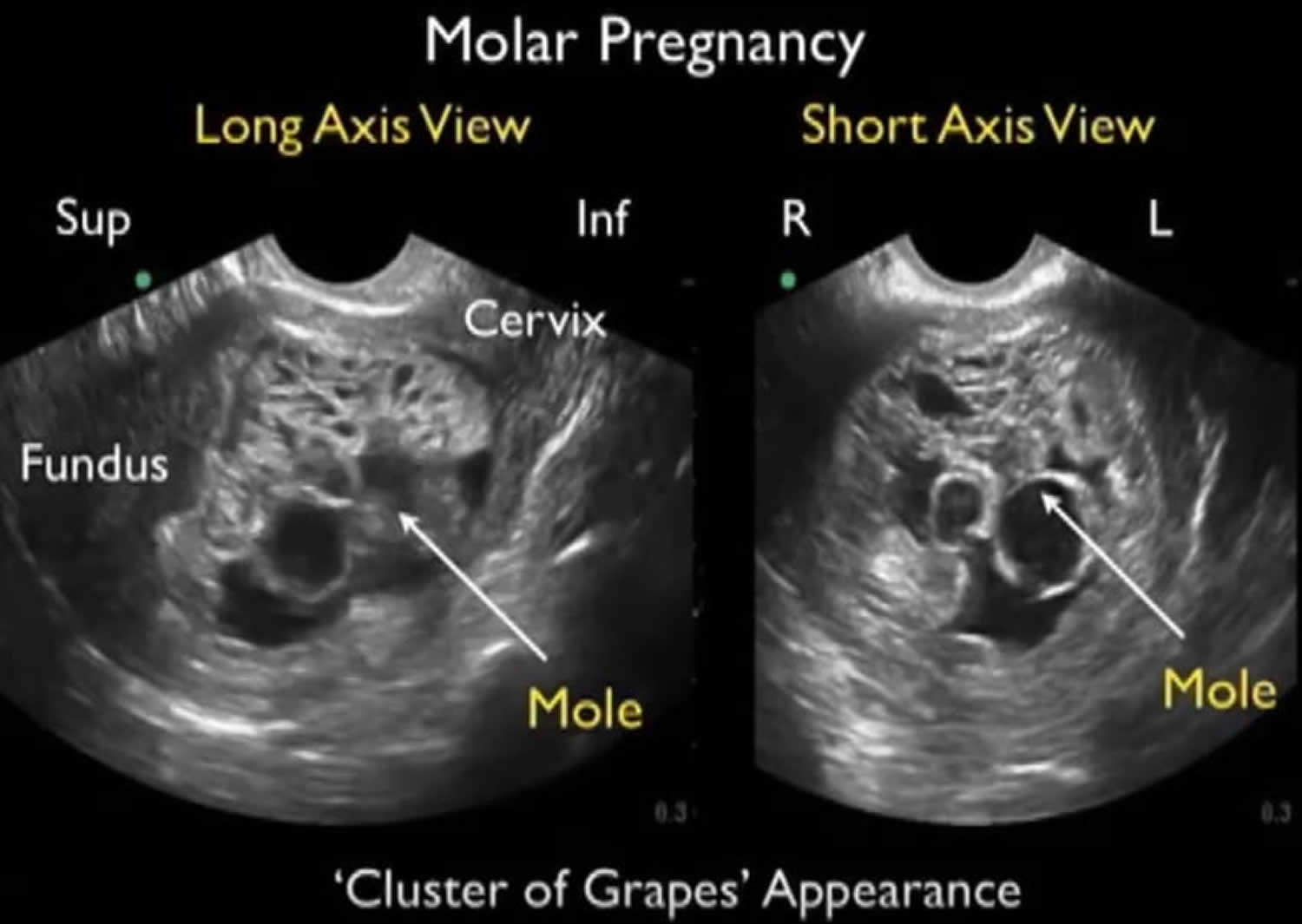
The diagnosis of hydatidiform mole is most commonly made by an ultrasound, a test that uses sound waves to show the contents of the uterus. The ultrasound picture of a complete hydatidiform mole will show the uterus filled with cysts. There is no evidence of a fetus.
An ultrasound of a complete molar pregnancy — which can be detected as early as eight or nine weeks of pregnancy — may show:
- No embryo or fetus
- No amniotic fluid
- A thick cystic placenta nearly filling the uterus
- Ovarian cysts
An ultrasound of a partial molar pregnancy may show:
- A growth-restricted fetus
- Low amniotic fluid
- A thick cystic placenta
Molar pregnancy ultrasound
If your health care provider detects a molar pregnancy, he or she may check for other medical problems, including:
- Preeclampsia
- Hyperthyroidism
- Anemia
The early diagnosis of a partial hydatidiform mole will look like a miscarriage or show an abnormal fetus with an abnormal placenta depending upon the number of weeks pregnant. In most cases of partial mole the diagnosis is made by the pathologist when he/she looks at the placenta under a microscope. This may be done after a miscarriage, termination of pregnancy or ectopic pregnancy. A mole may be suspected for several reasons in an ongoing pregnancy, for example if the womb is larger or smaller than it should be for the stage of the pregnancy, or if you are being sick more than in a normal pregnancy.
Complete hydatidiform moles also have a characteristic appearance on an ultrasound scan so this, and the fact that no developing fetus is seen when you have a scan at the ante-natal clinic, can allow the diagnosis to be suspected.
In a normal pregnancy the placenta makes many hormones to support itself, the baby and the mother. One of these hormones is called human chorionic gonadotrophin (hCG), and in a molar pregnancy, where there is overgrowth of the placenta, there is a large amount of this hormone produced.
Human chorionic gonadotrophin (hCG) circulates in the mother’s blood and hCG is excreted in her urine. These can be readily measured in the laboratory from blood or urine samples. This is useful in helping with the diagnosis of the condition, but even more useful in helping decide when a patient is cured. When there is no disease in the body, the level of hCG in the blood and hCG in the urine is low. When there is a lot of disease the level is high. As the disease resolves the levels fall gradually. These tests are important because it is possible to monitor how your disease is progressing.
Once the diagnosis of trophoblastic disease is made, you will be registered with the regional center which specializes in the monitoring of the disease. All being well, your hCG level will quickly become low and remain so. Please refer to your regional center for specifics as follow up procedures between centers may differ slightly.
However, as mentioned earlier, even a tiny amount of mole tissue left in the body can grow and spread via your blood stream and this can happen up to many months after apparent cure. Thus your disease will probably be monitored by urine samples for a period of around six months.
In some cases drug treatment in the form of chemotherapy is required to eliminate any remaining disease. Up to 10% of women require further treatment in the form of chemotherapy if their hCG hormone levels do not reduce on their own or remain the same.
Molar pregnancy treatment
If an ultrasound scan shows that you have a molar pregnancy, treatment to remove it will be recommended.
Three main treatments can be used:
- Dilation and curettage (D&C) with suction removal – To treat a molar pregnancy, your doctor will remove the molar tissue from your uterus with a procedure called dilation and curettage (D&C). A D&C is usually done as an outpatient procedure in a hospital. During the procedure, you’ll receive a local or general anesthetic and be positioned on the operating room table on your back with your legs in stirrups. Your doctor will insert a speculum into your vagina, as in a pelvic exam, to see your cervix. He or she will then dilate your cervix and the abnormal cells are sucked out using a thin tube passed into your womb through your vagina.
- Medication – if the growth is too large to be sucked out, you may be given medication to make it pass out of your vagina.
- Surgery to remove the uterus (hysterectomy) – Rarely, if there is increased risk of gestational trophoblastic neoplasia (GTN) and there’s no desire for future pregnancies, the uterus may be removed (hysterectomy).
Most women are successfully treated with suction removal and can go home later the same day.
Speak to your doctor about the benefits and risks of the different options.
Monitoring after treatment for a molar pregnancy
Some abnormal cells may be left in your womb after treatment. These usually go away on their own within a few months, but further treatment may sometimes be needed to remove them.
To see if you might need further treatment, you’ll be asked to have regular blood or urine tests to measure the level of the hormone hCG (human chorionic gonadotrophin).
The amount of this hormone in your body increases during pregnancy. If it doesn’t go down after treatment for a molar pregnancy, it might mean some abnormal cells are left in your womb.
- After the uterus is emptied, testing for hCG should be performed weekly tests until a negative (<5) value is reached. Once a negative value is reached, follow with two additional consecutive weekly beta hCG tests. If all three weekly tests are negative, follow with three consecutive monthly beta hCG tests. If all hCG tests remain negative, followup is complete and pregnancy may be attempted, if appropriate. If the beta hCG level plateaus over three consecutive weeks, or re-elevates over two consecutive weeks, evaluation for persistent gestational trophoblastic disease is mandatory. Birth control pills or other forms of hormonal contraceptives are safe and effective. IUDs should not be inserted until the hCG is undetectable.
Most women need to have regular blood or urine tests for around six months to one year after treatment to make sure there’s no remaining molar tissue. Because pregnancy hCG (human chorionic gonadotrophin) levels also increase during a normal pregnancy, your doctor may recommend you wait six to 12 months before trying to become pregnant again. Your provider will recommend a reliable form of birth control during this time.
Sex, pregnancy and contraception after a molar pregnancy
You can have sex as soon as you feel physically and emotionally ready. If you have any bleeding after your treatment, don’t have sex until this stops.
Having a molar pregnancy doesn’t affect your chances of getting pregnant again. Pregnancy following too soon after trophoblastic disease may also increase the risk of recurrence or re-activation of the mole, however, the risk of having another molar pregnancy is small (about 1 in 80).
You are advised to avoid pregnancy while you are being monitored.
It’s best not to try for a baby until your after-treatment monitoring has finished, in case you need further treatment to remove any cells left in your womb.
Use contraception until your doctors say it’s safe to get pregnant again. You can use any type except implants that go in the womb, which should only be used once your hCG level has returned to normal.
Further treatment after a molar pregnancy
In a few cases, abnormal cells left in the womb after treatment don’t go away on their own. This is called persistent trophoblastic disease.
The chances of this happening are about 1 in 7 (15%) if you had a complete mole and about 1 in 200 (0.5%) if you had a partial mole.
Persistent trophoblastic disease can be serious because the abnormal cells can regrow or spread to other parts of the body, similar to cancer, if it’s not treated.
Treatment involves taking medication to kill the abnormal cells (chemotherapy) for a few months. Most women have a combination of:
- injections of a medicine called methotrexate
- tablets of a medicine called folinic acid
With treatment, almost 100% of women are cured.
You can usually get pregnant after treatment if you wish, but you will be advised not to try for at least a year because there’s a chance (about 1 in 30) persistent trophoblastic disease could come back during this time.
Malignant gestational trophoblastic disease
A rise in the hCG (human chorionic gonadotrophin) level indicates that the molar pregnancy is malignant gestational trophoblastic disease (also called gestational trophoblastic neoplasia). More tests will be done to find out if the cancer has spread from the uterus to other parts of the body (called staging). Even if gestational trophoblastic disease has spread to other parts of the body it is still highly curable. The stages of malignant gestational trophoblastic disease are:
- Stage I. The cancer has not spread from the uterus
- Stage II. The cancer has spread from the uterus to other structures in the pelvis
- Stage III. The cancer has spread to the lungs
- Stage IV. The cancer has spread to other organs
The treatment of malignant gestational trophoblastic disease depends on the stage and number of risk factors which determine the type of drugs that will most likely cure the disease.
The factors that are characteristic of women who are likely to be cured by one or more single chemotherapy drugs (called low-risk malignant gestational trophoblastic disease) are:
- The last pregnancy was less than four months ago
- The level of hCG in the blood is low
- The cancer has not spread to the liver, brain, and/or other distant organs
- The patient has not received chemotherapy treatments earlier
The risk factors of women who develop malignant gestational trophoblastic disease who are NOT likely to be cured by one or more single chemotherapy drugs and who require treatments containing multiple agents to effect cure (called high-risk malignant gestational trophoblastic disease) are:
- The last pregnancy was more than four months ago
- The level of hCG in the blood is high
- The cancer has spread to the liver, brain, and/or other distant organs
- The patient received chemotherapy earlier and the cancer did not go away
- The tumor began after completion of a normal pregnancy
Three kinds of treatment are used for malignant gestational trophoblastic disease:
- surgery (removing the cancer),
- chemotherapy (using drugs to kill the cancer), and
- radiation therapy (uses high energy x-rays to kill cancer cells and shrink tumors).
The most common operation used for malignant gestational trophoblastic disease is hysterectomy, an operation to take out the uterus. Surgery may also be used to remove cancer involving the lungs and other organs which have not gone away with drug therapy.
Chemotherapy is the main treatment for malignant gestational trophoblastic disease and is generally highly effective. Chemotherapy uses drugs to kill cancer cells. It may be taken by pill, or by a needle in vein or muscle. It is called systemic treatment because the drugs enter the bloodstream, travel through the body, and can kill cancer cells outside the uterus. Chemotherapy may be given before or after surgery or alone. Patients can preserve fertility and still be cured with chemotherapy even in the presence of widespread disease.
Radiation may infrequently be used in certain cases to treat cancer that has spread to other parts of the body, particularly the brain. Radiation may come from a machine outside the body (external-beam radiation therapy) or from putting materials that produce radiation (radioisotopes) through thin plastic tubes into the area where the cancer cells are found (internal radiation).
Recurrent Disease
Gestational trophoblastic neoplasia (malignant gestational trophoblastic disease) is a highly curable disease. Women with hydatidiform mole have an excellent prognosis and women with malignant gestational trophoblastic disease (called gestational trophoblastic neoplasia) usually have a very good prognosis. Choriocarcinoma, for example, is an uncommon yet almost always curable cancer. Although choriocarcinoma is a highly malignant tumor and life-threatening disease, it is very sensitive to chemotherapy; 85%–90% of women with low-risk malignant gestational trophoblastic neoplasia are cured by the initial chemotherapy and the remaining are cured by the use of stronger combinations of drugs, or surgery. Similarly, 85%–90% of women who develop high-risk malignant gestational trophoblastic neoplasia are cured by chemotherapy used together with the selective use of surgery and radiation. Approximately 10%–15% of women with high-risk malignant gestational trophoblastic neoplasia will develop drug resistance after prolonged chemotherapy. This group is made up of patients with Stage IV disease that involves distant organs such as the brain, liver, and bowel. Specially designed chemotherapy treatments using drugs that have been shown to be effective against other cancers are being employed to salvage many of these women.
- Salani R, Copeland LJ. Malignant diseases and pregnancy. In: Gabbe SG, Niebyl JR, Simpson JL, et al, eds. Obstetrics: Normal and Problem Pregnancies. 7th ed. Philadelphia, PA: Elsevier; 2017:chap 50.[↩]