Contents
What is a torn meniscus
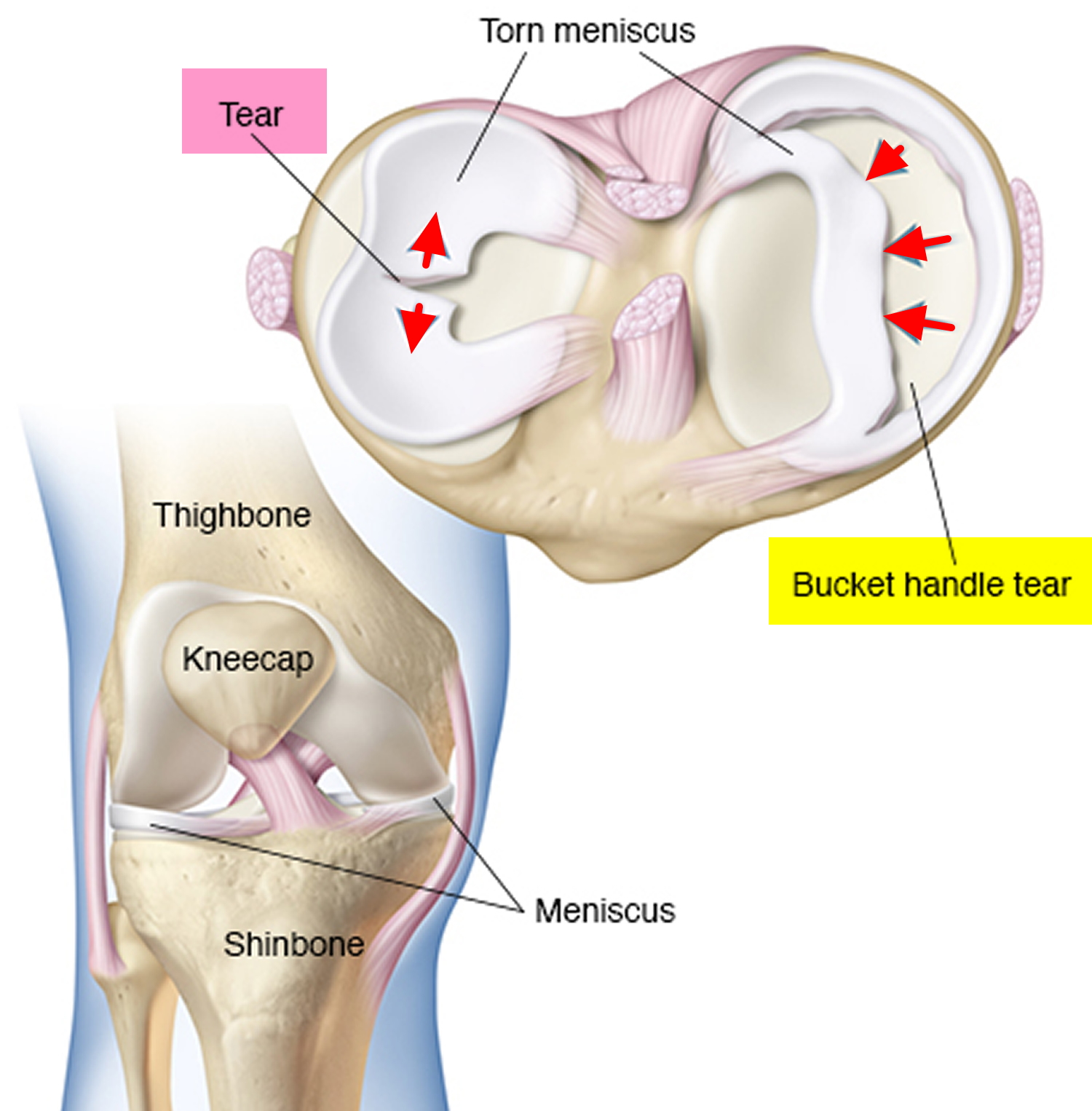
A torn meniscus is one of the most common knee injuries (see Figures 2, 4, 5 and 6 below). Any activity that causes you to forcefully twist or rotate your knee, especially when putting your full weight on it, can lead to a torn meniscus. Athletes, particularly those who play contact sports, are at risk for meniscus tears. However, anyone at any age can tear a meniscus.
A torn meniscus can result from any activity that causes you to forcefully twist or rotate your knee, such as aggressive pivoting or sudden stops and turns. Even kneeling, deep squatting or lifting something heavy can sometimes lead to a torn meniscus. Direct contact, like a tackle, is sometimes also involved.
Older people are more likely to have degenerative meniscus tears. Cartilage weakens and wears thin over time. Aged, worn tissue is more prone to tears with little or no trauma. Just an awkward twist when getting up from a chair may be enough to cause a tear, if the menisci have weakened with age.
Risk factors for torn meniscus
- Performing activities that involve aggressive twisting and pivoting of the knee puts you at risk of a torn meniscus. The risk is particularly high for athletes — especially those who participate in contact sports, such as football, or activities that involve pivoting, such as tennis or basketball.
- The risk of a torn meniscus also increases as you get older, due to wear and tear on your knees.
Each of your knees has two menisci — C-shaped (medial meniscus) and an incomplete O-shaped (lateral meniscus) pieces of cartilage that provides cushioning to distribute your body weight across your knee joint between your shinbone and your thighbone. A torn meniscus causes pain, swelling and stiffness. You also might feel a block to knee motion and have trouble extending your knee fully.
Torn meniscus of your knee are noted by how they look, as well as where the tear occurs in the meniscus. Common meniscus tears include bucket handle, flap, and radial (see Figures 4, 5 and 6). Sports-related torn meniscus often occurs along with other knee injuries, such as anterior cruciate ligament (ACL) tears.
Conservative treatment such as rest, ice and medication is sometimes enough to relieve the pain of a torn meniscus and give the injury time to heal on its own. In other cases, however, a torn meniscus requires surgical repair. Meniscal injuries are commonly associated with other knee injuries, which need to be treated in conjunction with your meniscal tear. In many cases, a surgical procedure called “arthroscopy” is used to repair or remove a torn meniscus.
The success of the meniscus repair, however, depended on whether the tear type was simple, complex or a “displaced bucket-handle.” In the study, 99 patients (18 or younger) had a meniscus repair at the time of an anterior cruciate ligament (ACL) reconstruction between 1990 and 2005. Overall, patients had a 74 percent success rate of their meniscus tear. Patients with simple tears (one major tear) had an 84 percent successful repair rate. The success rate decreased to 59 percent for displaced bucket-handle tears (a tear around the rim of the meniscus, causing the central portion to displace into the joint) and 57 percent for complex tears (a tear that occurred in multiple planes). Two years after surgery, these patients had a freedom from failure rate of 90.9 percent; however, after 8 years, the rate decreased to 76.8 percent. In evaluating knee function (limp, locking, instability, pain, swelling and trouble climbing stairs), the patients improved from a median score of 48 (in a range of 38-70) before surgery to 90 (range 52-100) after surgery. Rating the sporting activity level of patients on a scale of 0–10, with 10 being national elite competitive sports, and 0 being inability to perform daily activities, patients improved their activity level significantly to 6.2 from a 1.9.
Can you walk with a torn meniscus?
Most people can still walk on their injured knee with the torn meniscus. Many athletes keep playing with a torn meniscus. However, over 2 to 3 days, your knee will gradually become more stiff and swollen. And if a piece of meniscus come loose and drift into the knee joint, your knee may become locked in a flexed position or you can’t fully straighten your knee. The torn meniscus can also cause your knee to slip, pop, or lock.
Torn meniscus recovery
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
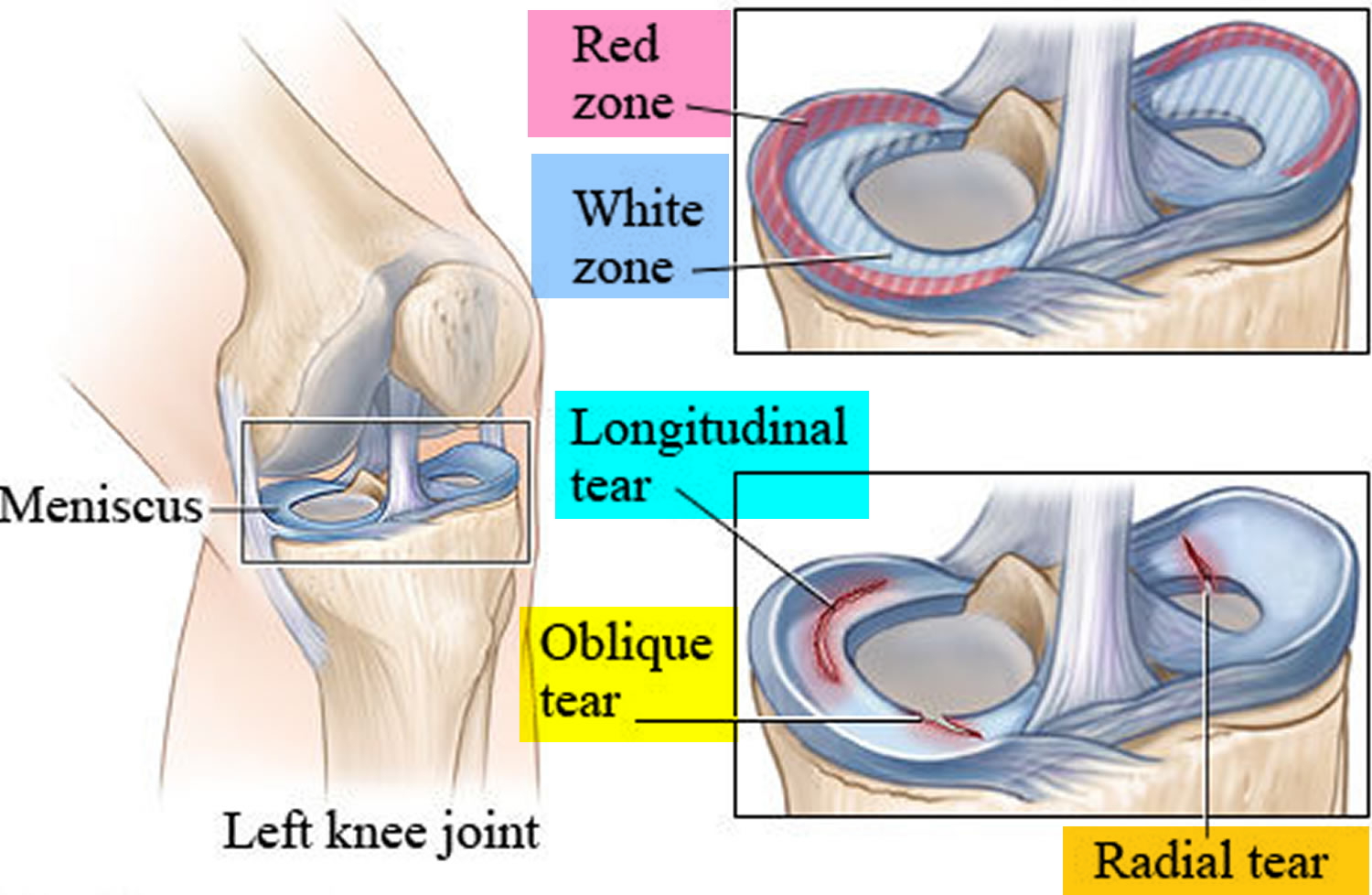
Meniscal blood supply is limited: your meniscus receives its nutrition from blood and synovial fluid within the joint capsule. Your meniscus has two distinct regions that affect their ability to heal. Doctors call these the Red Zone and the White Zone (see Figure 6 below).
Red Zone
The red zone has blood supply, whereas the the white zone doesn’t have a blood supply and won’t heal naturally. The outside of the meniscus has a blood supply from the synovial capsule. Lateral meniscal tears may heal without the need for surgery.
A small meniscus tear, or a tear in the red zone, will usually respond quickly to physiotherapy treatment.
White Zone
The inside of the meniscus gets its nutrition from the synovial fluid. Due to this, tears of the inner meniscus do not usually heal due to a lack of blood supply to trigger an inflammatory response. These injuries often require surgery.
Torn meniscus recovery time
Your torn meniscus will commonly take up to six or eight weeks to fully heal. As mentioned previously, some meniscal tears will require surgery.
Your orthopedic surgeon will guide you as to what is most likely for your knee injury.
It is important to avoid activities and exercises that place excessive stress through your meniscus and further delay your healing. In some cases, your orthopedic surgeon may advise you to keep weight off your knee. In this instances, crutches may be recommended.
Everyone is different, so be guided by your orthopedic surgeon advice.
Torn meniscus complications
A torn meniscus can lead to knee instability, inability to move your knee normally or persistent knee pain. You might be more likely to develop osteoarthritis in the injured knee.
The Knee Joint
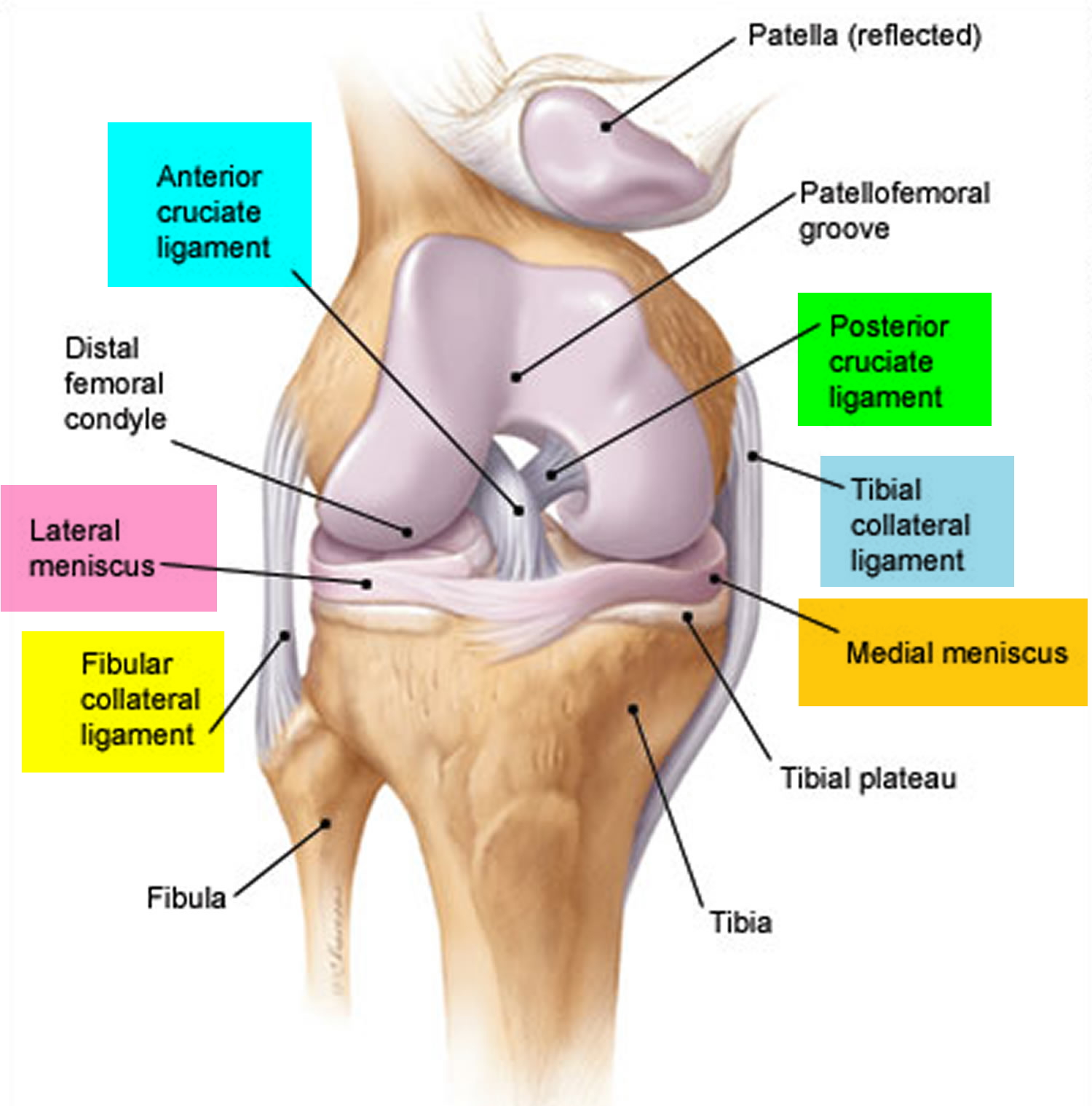
Three bones meet to form your knee joint: your thighbone (femur), shinbone (tibia), and kneecap (patella). Your kneecap sits in front of the joint to provide some protection.
The knee joint (tibiofemoral joint) is the largest and most complex joint of the body (Figures 1) and its evaluation can present a challenge. It is a modified hinge joint (because its primary movement is a uniaxial hinge movement) that consists of three joints within a single synovial cavity:
- Laterally is a tibiofemoral joint, between the lateral condyle of the femur, lateral meniscus, and lateral condyle of the tibia, which is the weight-bearing bone of the leg.
- Medially is another tibiofemoral joint, between the medial condyle of the femur, medial meniscus, and medial condyle of the tibia.
- An intermediate patellofemoral joint is between the patella and the patellar surface of the femur.
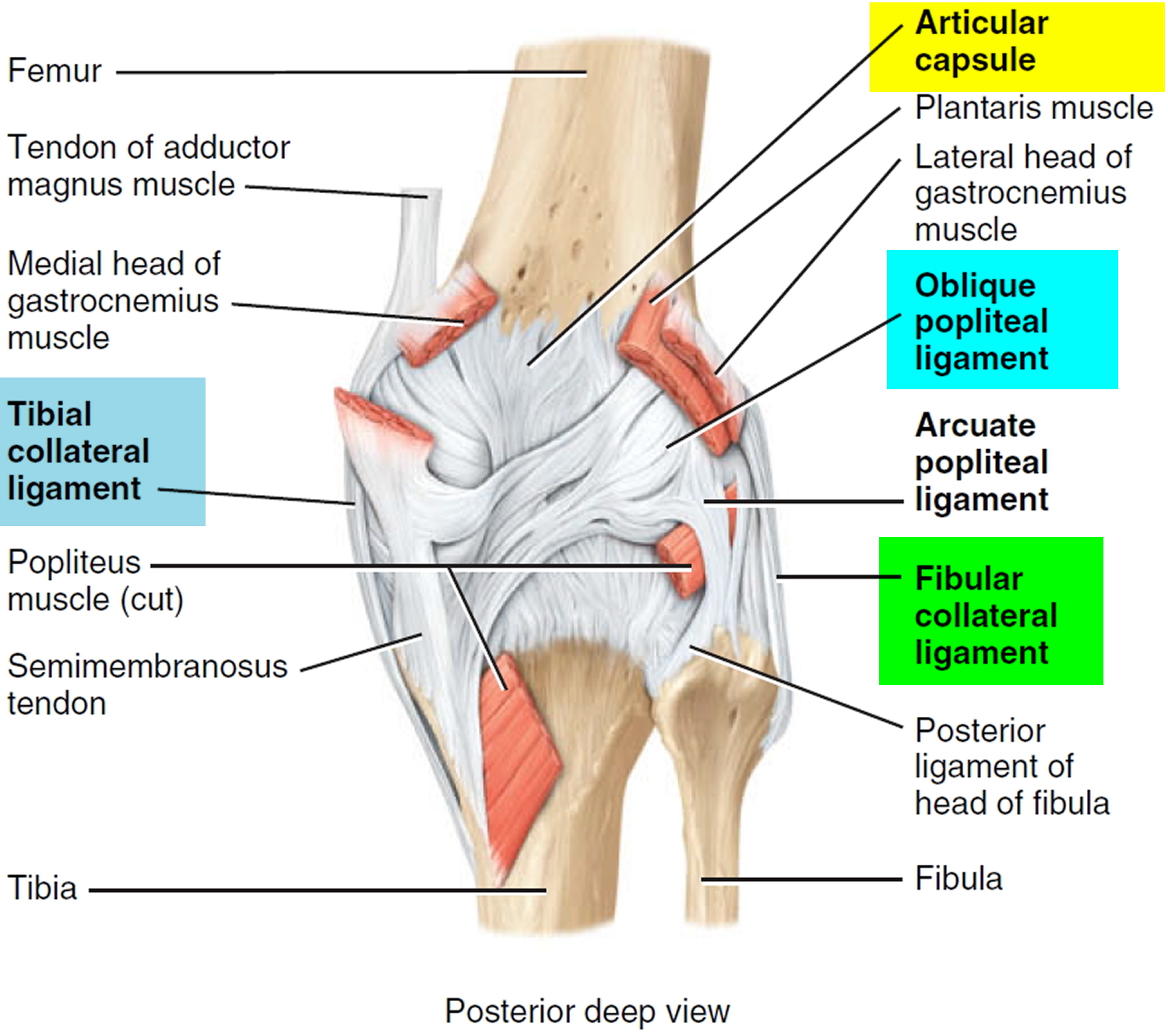
Bones are connected to other bones by ligaments. There are four primary ligaments in your knee. They act like strong ropes to hold the bones together and keep your knee stable.
- The lateral collateral ligament strengthens the knee joint on the outer side of the knee. It runs between your femur (thigh bone) and the top of your fibula — the long, thin bone adjacent to the tibia.
- The medial collateral ligament strengthens the knee joint on the inner side of the knee. It runs between your femur and the upper inside edge of your tibia (shin bone).
Together the collateral ligaments resist side-to-side movement of the knee joint and help prevent rotation between your thigh bone and your shin and brace it against unusual movement.
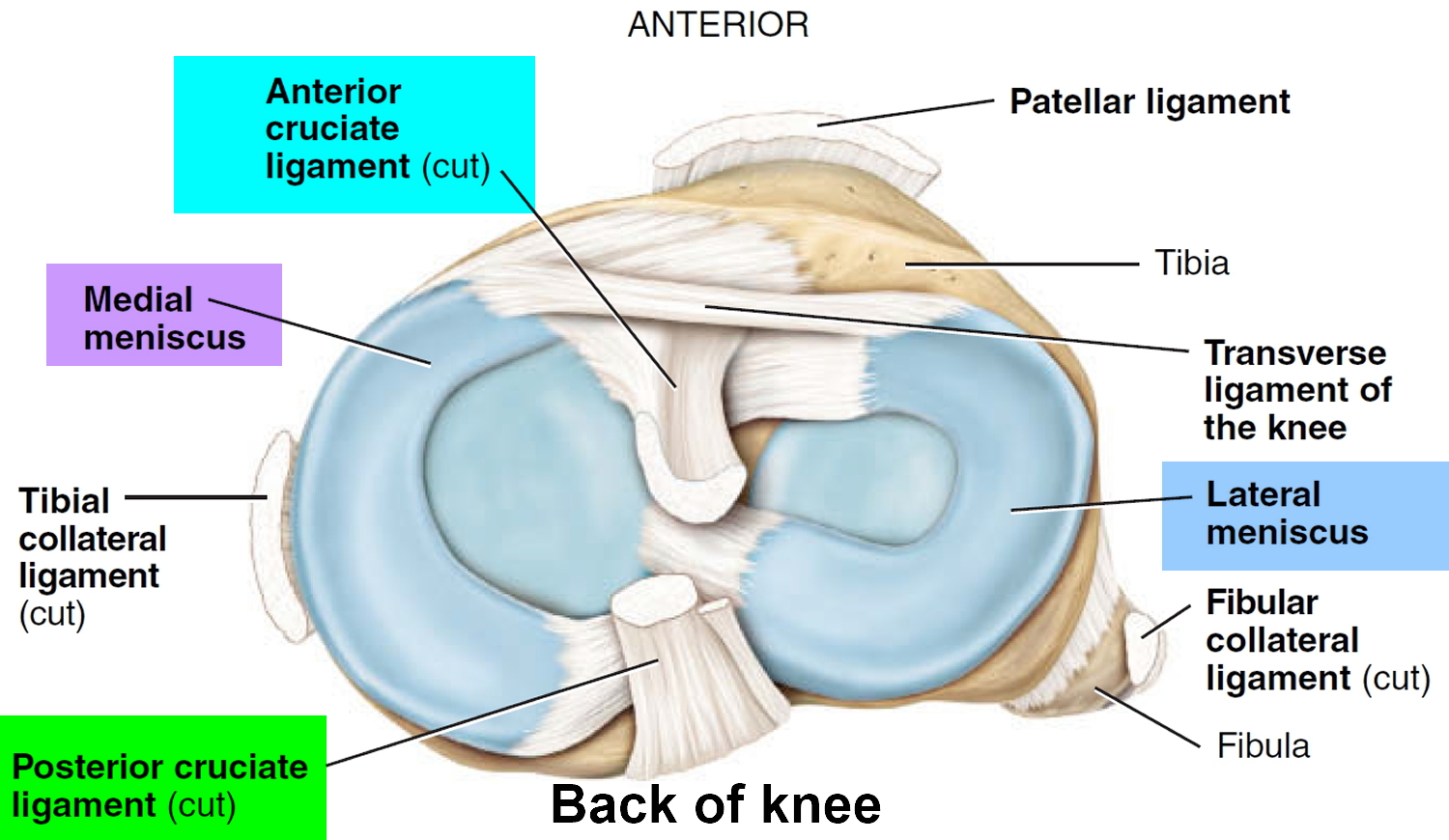
Articular discs (menisci). The meniscus is a C-shaped piece of tough, rubbery fibrocartilage discs that acts as a shock absorber between your tibial and femoral condyles help compensate for the irregular shapes of the bones and circulate synovial fluid. The meniscus can be torn if you suddenly twist your knee while bearing weight on it.
- Medial meniscus. Semicircular piece of fibrocartilage (C-shaped). Its anterior end is attached to the anterior intercondylar fossa of the tibia, anterior to the anterior cruciate ligament. Its posterior end is attached to the posterior intercondylar fossa of the tibia between the attachments of the posterior cruciate ligament and lateral meniscus.
- Lateral meniscus. Nearly circular piece of fibrocartilage (approaches an incomplete O in shape). Its anterior end is attached anteriorly to the intercondylar eminence of the tibia, and laterally and posteriorly to the anterior cruciate ligament. Its posterior end is attached posteriorly to the intercondylar eminence of the tibia, and anteriorly to the posterior end of the medial meniscus. The anterior surfaces of the medial and lateral menisci are connected to each other by the transverse ligament of the knee and to the margins of the head of the tibia by the coronary ligaments.
Figure 1. Knee joint
Figure 2. Knee joint meniscus
Figure 3. Knee joint ligaments (posterior view)
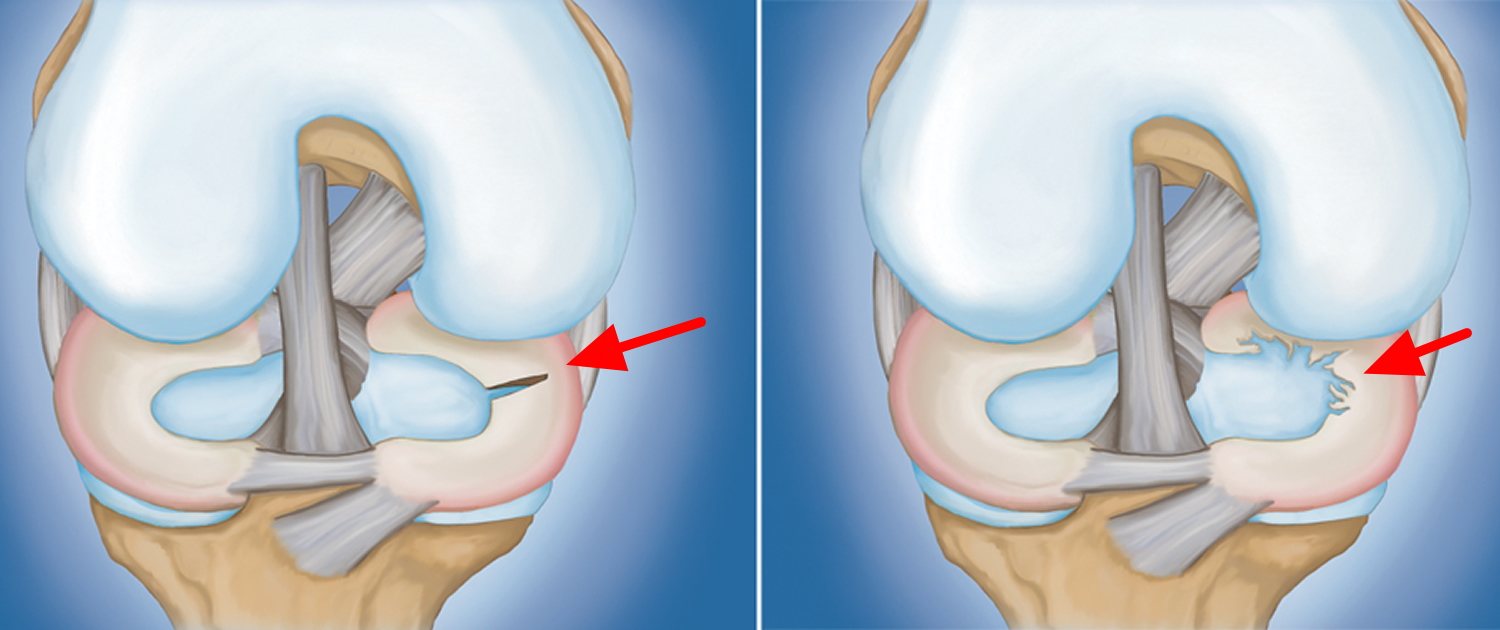
Figure 4. Torn meniscus – (Left) Flap tear. (Right) Bucket handle tear.
Figure 5. Torn meniscus – (Left) Radial tear. (Right) Degenerative tear.
Figure 6. Torn meniscus – Red Zone and White Zone – Radial tear, Oblique tear and Longitudinal tear.
Torn meniscus signs and symptoms
You might feel a “pop” when you tear a meniscus. Most people can still walk on their injured knee. Many athletes keep playing with a tear. Over 2 to 3 days, your knee will gradually become more stiff and swollen.
The most common symptoms of meniscus tear are:
- Pain
- Stiffness and swelling
- Catching or locking of your knee
- The sensation of your knee “giving way”
- You are not able to move your knee through its full range of motion
Without treatment, a piece of meniscus may come loose and drift into the joint. This can cause your knee to slip, pop, or lock.
Torn meniscus diagnosis
A torn meniscus often can be identified during a physical exam. Your doctor might move your knee and leg into different positions, watch you walk and ask you to squat to help pinpoint the cause of your signs and symptoms.
Torn meniscus symptoms test
After discussing your symptoms and medical history, your doctor will examine your knee. He or she will check for tenderness along the joint line where the meniscus sits. This often signals a tear.
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement will cause a clicking sound. Your knee will click each time your doctor does the test.
The Apley grind test is used to evaluate individuals for problems in the meniscus of the knee.
Imaging Tests
Because other knee problems cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
- X-rays. Although x-rays do not show meniscus tears, they may show other causes of knee pain, such as osteoarthritis.
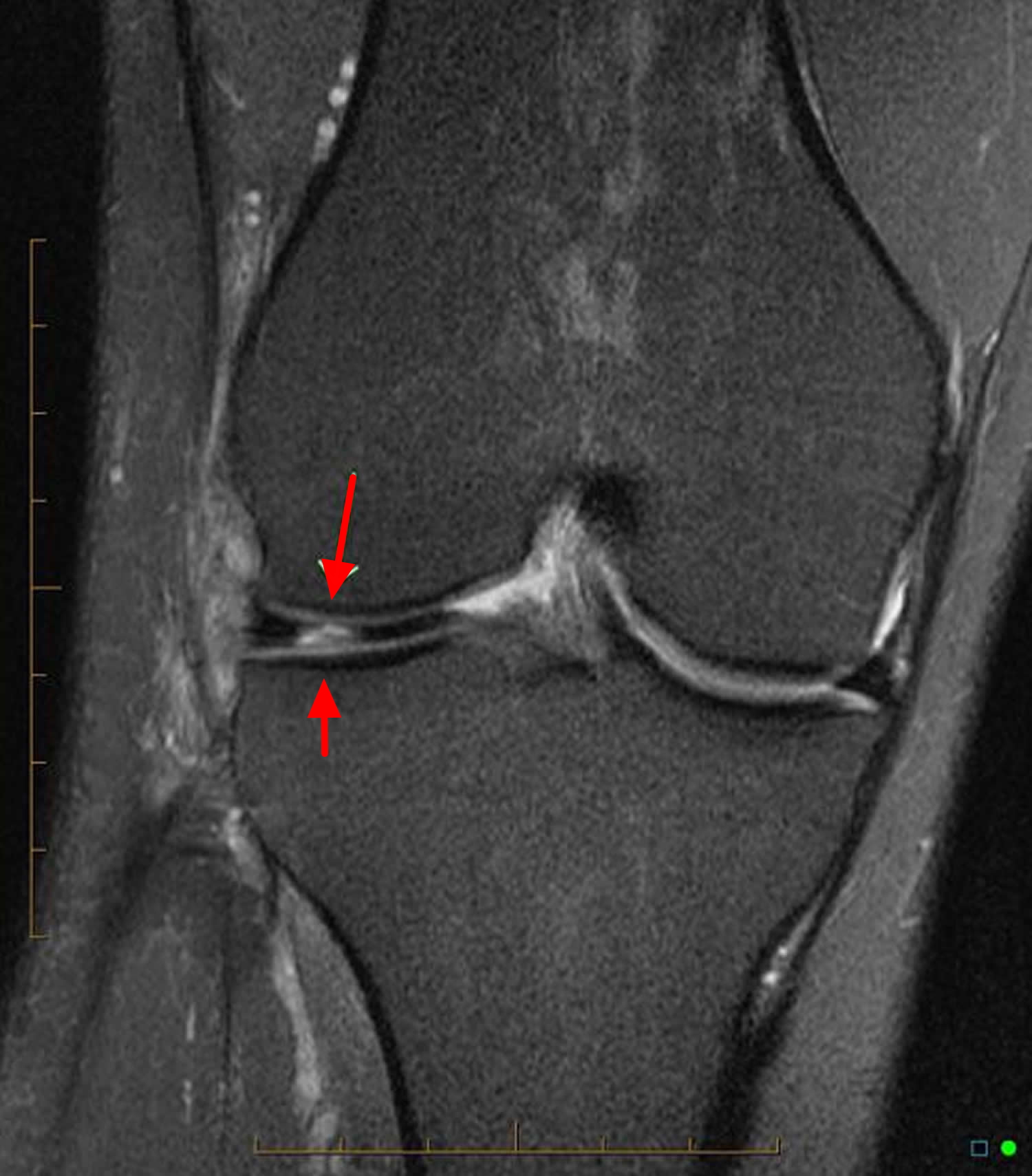
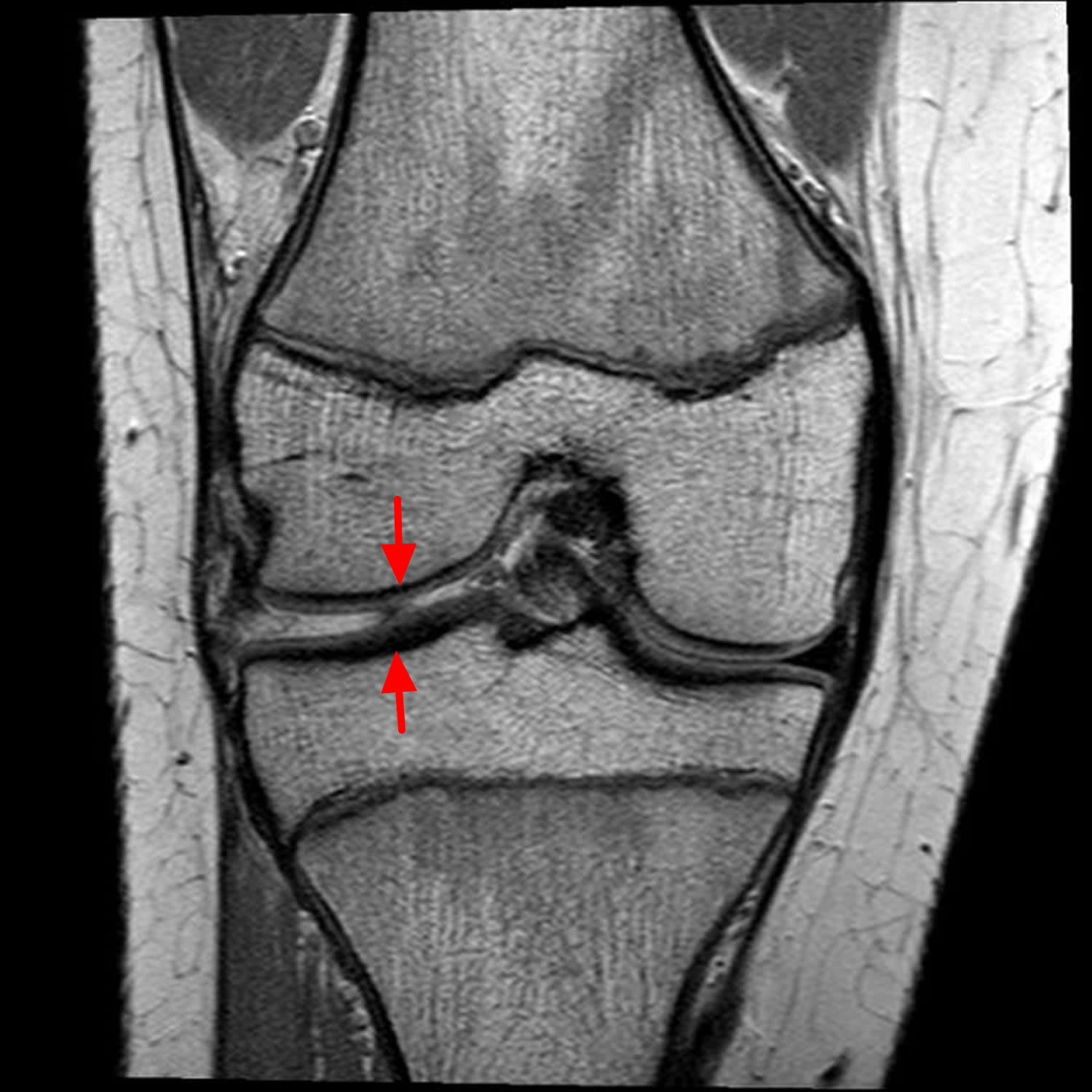
- Magnetic resonance imaging (MRI). This study can create better images of the soft tissues of your knee joint, like a meniscus.
Figure 7. Torn meniscus MRI – torn lateral meniscus lacks the normal “bow-tie” appearance of the meniscus with a radial tear at the junction of the anterior horn and body
Figure 8. Torn meniscus MRI – a horizontal tear of the posterior part of the meniscus of the knee
Torn meniscus treatment
How your orthopedic surgeon treats your torn meniscus will depend on the type of tear you have, its size, and location.
The outside one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a blood supply. Without nutrients from blood, tears in this “white” zone cannot heal. These complex tears are often in thin, worn cartilage. Because the pieces cannot grow back together, tears in this zone are usually surgically trimmed away.
Along with the type of tear you have, your age, activity level, and any related injuries will factor into your treatment plan.
Nonsurgical Treatment
If your tear is small and on the outer edge of the meniscus, it may not require surgical repair. As long as your symptoms do not persist and your knee is stable, nonsurgical treatment may be all you need.
RICE. The RICE protocol is effective for most sports-related injuries. RICE stands for Rest, Ice, Compression, and Elevation.
- Rest. Take a break from the activity that caused the injury. Your doctor may recommend that you use crutches to avoid putting weight on your leg.
- Ice. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly to the skin.
- Compression. To prevent additional swelling and blood loss, wear an elastic compression bandage.
- Elevation. To reduce swelling, recline when you rest, and put your leg up higher than your heart.
Non-steroidal anti-inflammatory medicines. Drugs like aspirin and ibuprofen reduce pain and swelling.
Torn meniscus surgery
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
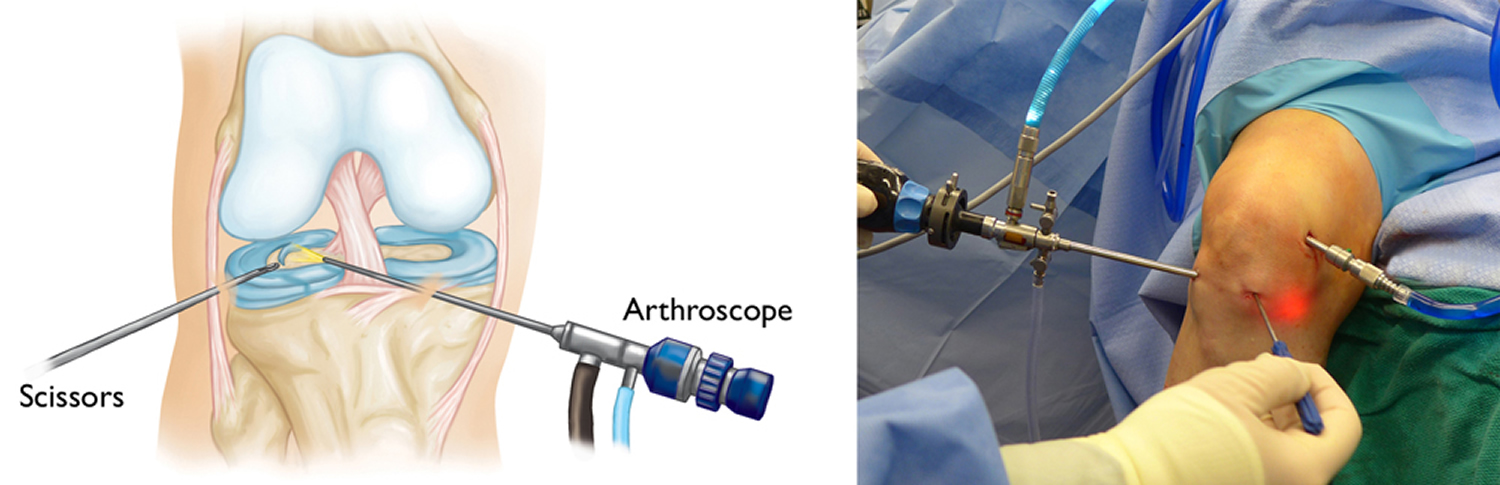
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures (see Figure 8). In it, a miniature camera is inserted through a small incision (portal). This provides a clear view of the inside of the knee. Your orthopaedic surgeon inserts miniature surgical instruments through other portals to trim or repair the tear.
Figure 8. Torn meniscus surgery
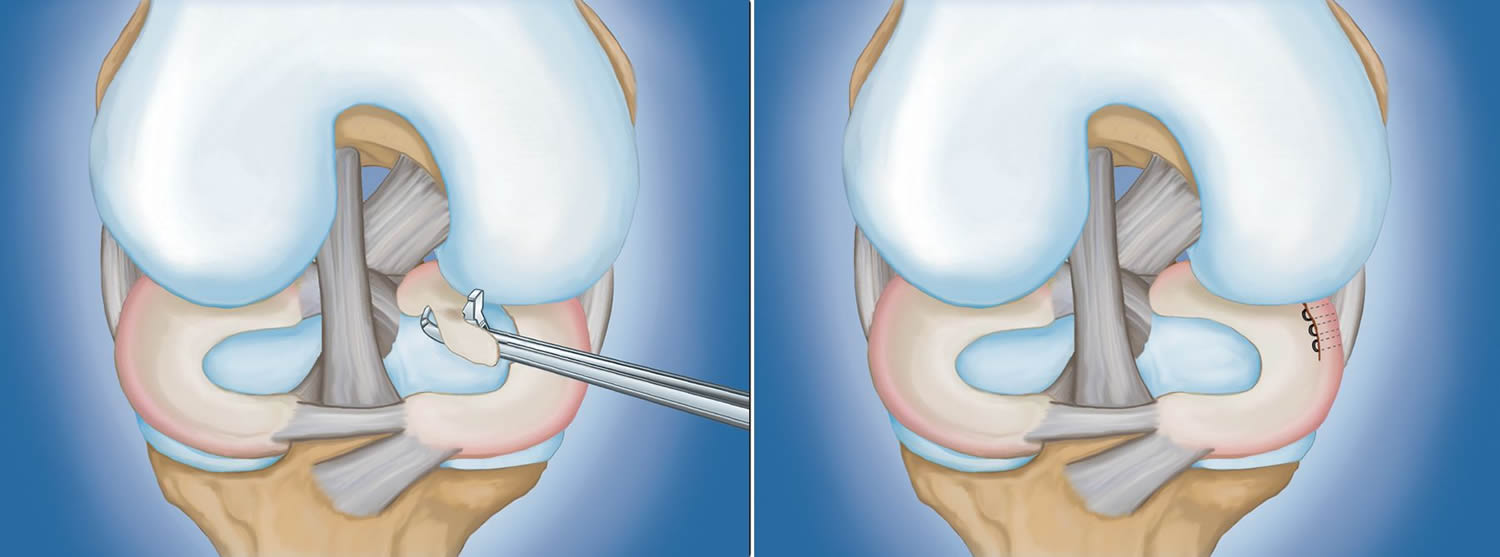
- Partial meniscectomy. In this procedure, the damaged meniscus tissue is trimmed away.
- Meniscus repair. Some meniscus tears can be repaired by suturing (stitching) the torn pieces together. Whether a tear can be successfully treated with repair depends upon the type of tear, as well as the overall condition of the injured meniscus. Because the meniscus must heal back together, recovery time for a repair is much longer than from a meniscectomy.
Figure 9. Torn meniscus surgery (Left) partial meniscectomy and Right (meniscus repair)
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
For the most part, rehabilitation can be carried out at home, although your doctor may recommend physical therapy. Rehabilitation time for a meniscus repair is about 3 months. A meniscectomy requires less time for healing — approximately 3 to 4 weeks.
Torn meniscus exercises
One of the major roles of your meniscus is shock-absorption. Luckily, the other vital shock absorbers around your knee are your muscles. Researchers have discovered that if you strengthening your leg muscles, your bone stresses will reduce as your muscle strength improves and your knee becomes more dynamically stable.
Your physiotherapy treatment will aim to:
- Reduce pain and inflammation.
- Normalise joint range of motion.
- Strengthen your knee: especially quadriceps and hamstrings.
- Strengthen your lower limb: calves, hip and pelvis muscles.
- Improve patello-femoral (knee cap) alignment.
- Normalize your muscle lengths improve your proprioception and balance Improve your technique and function e.g., walking, running, squatting, hopping and landing.
- Minimize your chance of re-injury.
Rehabilitation after a meniscus repair is usually different than a meniscus resection due to healing time require where a meniscus has been stitched. Most surgeons will have you non-weight bearing for 4 to 8 weeks to allow the meniscus to heal before commencing weight-bearing exercises.
Physiotherapy rehabilitation should focus on early mobilization of the knee (tibiofemoral) and kneecap (patellofemoral) joints, plus strengthening of your quadriceps, hamstrings and leg muscles.
Your treatment guidelines will be similar to the nonoperative approach taking into consideration the findings and operative procedures performed. For more specific information, please ask your physiotherapist.
Your physiotherapist is an expert in the assessment and correction of muscle strength deficits, timing and individually prescribed strengthening exercises appropriate for your injury, sport or lifestyle. It is important to remember that individual injuries, your stage of rehabilitation, age, gender and your sport or level of activity will dictate the best exercises suitable for you.
Seek the professional advice of your physiotherapist if you require more specific strengthening advice.