Contents
What is the plague
Plague also called bubonic plague or black plague, is a disease that affects humans and other mammals. It is caused by the bacterium, Yersinia pestis. Humans usually get plague after being bitten by a rodent flea that is carrying the plague bacterium or by handling an animal infected with plague. Plague is known as the Black Death during medieval times and plague is infamous for killing millions of people in Europe during the Middle Ages. Today plague occurs in fewer than 5,000 people a year worldwide and modern antibiotics are effective in treating plague. Without prompt treatment, plague (bubonic plague or black plague) can cause serious illness or death. Presently, human plague infections continue to occur in the western United States, but significantly more cases occur in parts of Africa and Asia.
The most common form of plague results in swollen and tender lymph nodes — called buboes — in the groin, armpits or neck. The rarest and deadliest form of plague affects the lungs, and it can be spread from person to person.
Plague in the United States
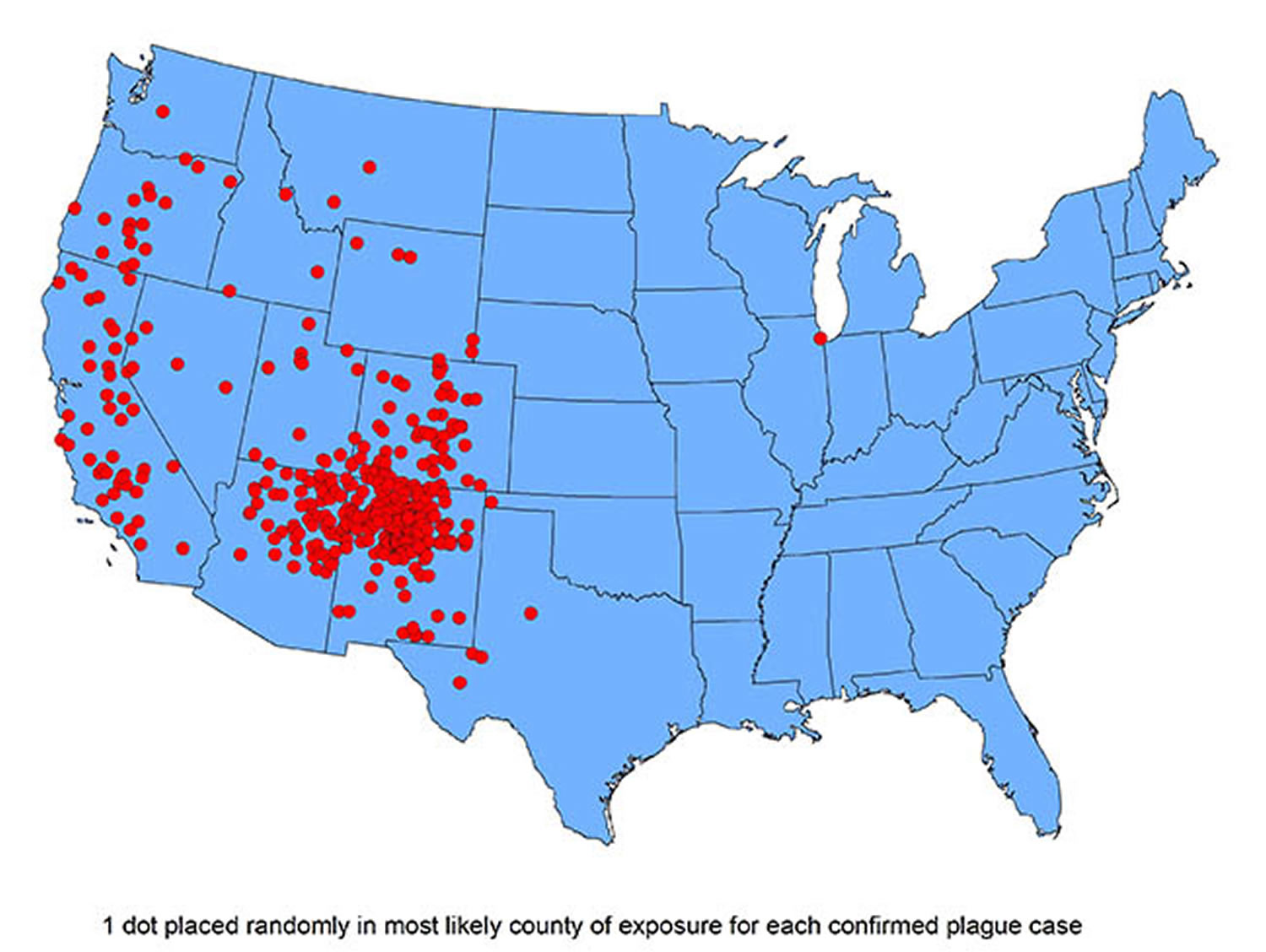
Plague was first introduced into the United States in 1900, by rat–infested steamships that had sailed from affected areas, mostly from Asia. Epidemics occurred in port cities. The last urban plague epidemic in the United States occurred in Los Angeles from 1924 through 1925. Plague then spread from urban rats to rural rodent species, and became entrenched in many areas of the western United States. Since that time, plague has occurred as scattered cases in rural areas. Most human cases in the United States occur in two regions:
- Northern New Mexico, northern Arizona, and southern Colorado
- California, southern Oregon, and far western Nevada
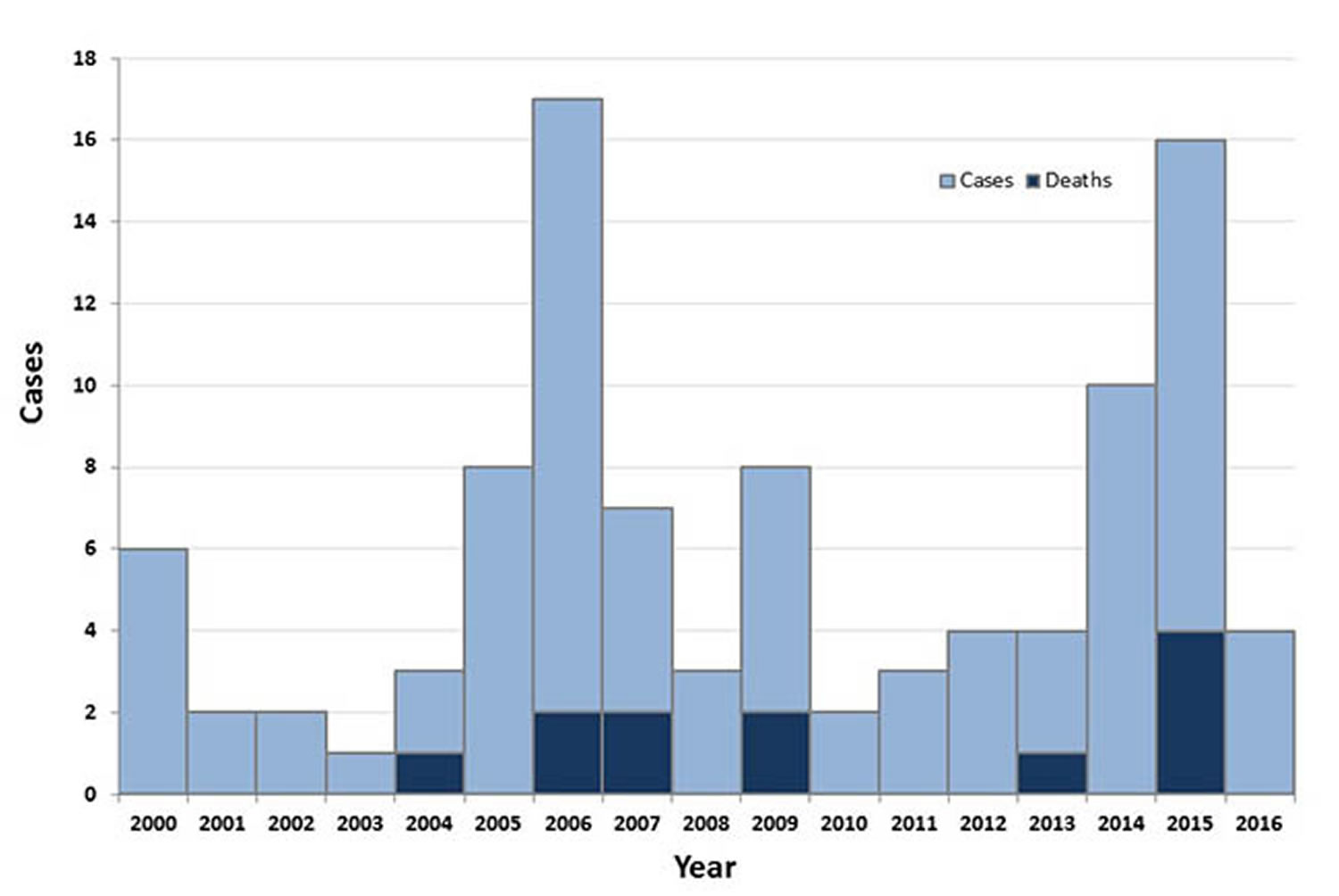
Over 80% of United States plague cases have been the bubonic form. In recent decades, an average of seven human plague cases have been reported each year (range: 1–17 cases per year). Plague has occurred in people of all ages (infants up to age 96), though 50% of cases occur in people ages 12–45. It occurs in both men and women, though historically is slightly more common among men, probably because of increased outdoor activities that put them at higher risk.
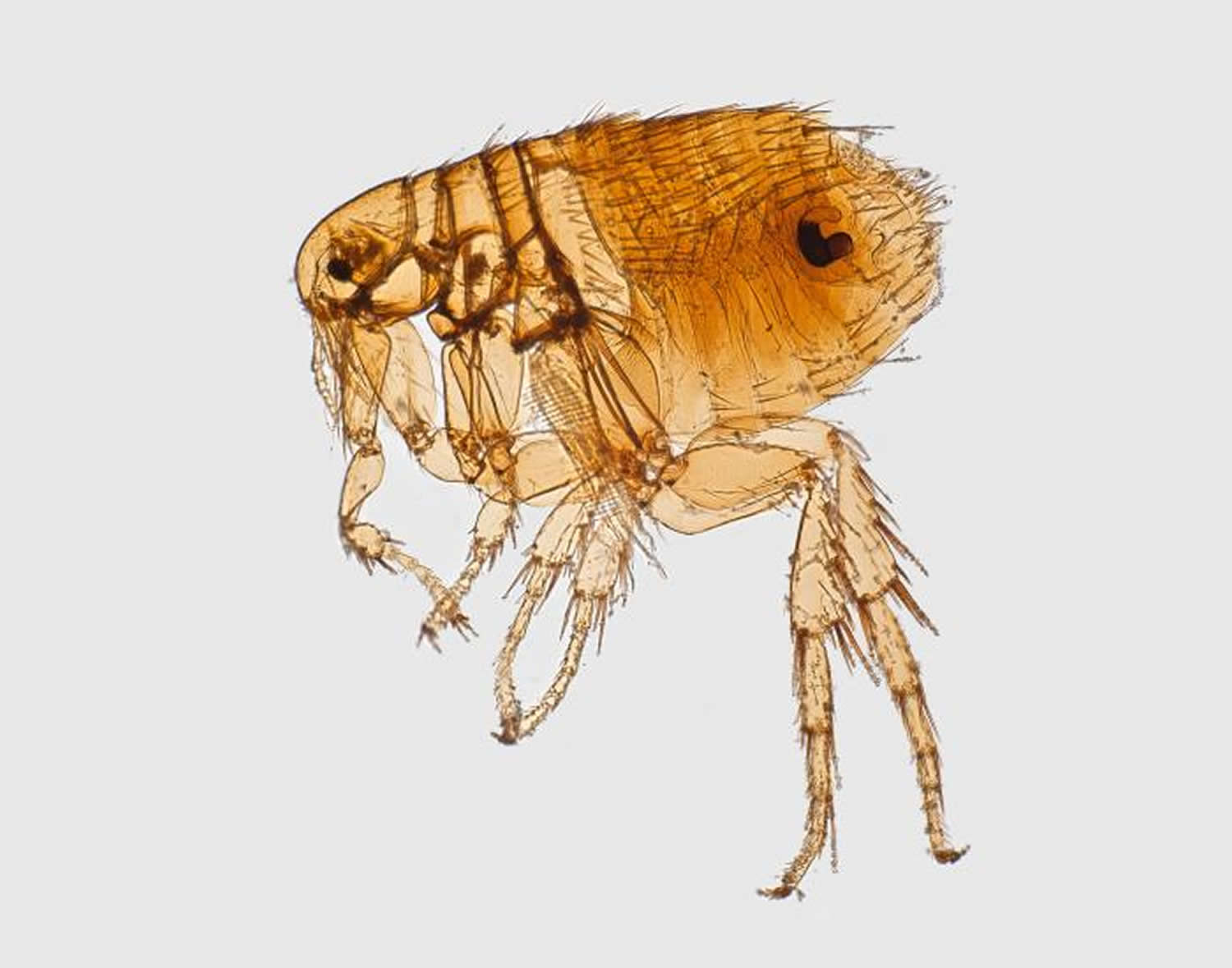
Figure 1. Oriental rat flea – bubonic plague vector (Female Oriental rat flea, Xenopsylla cheopis, a well-known bubonic plague vector)
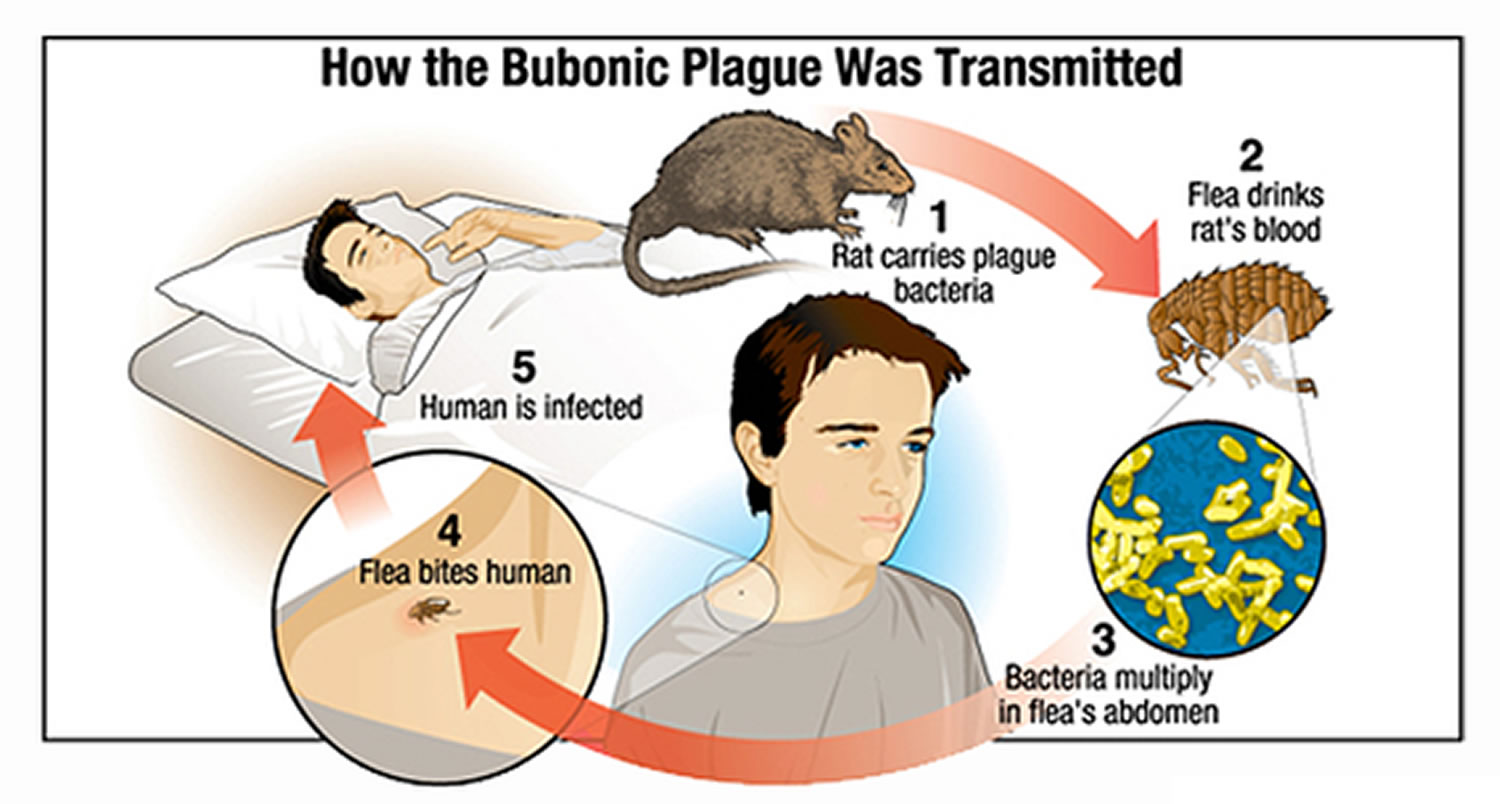
Figure 2. How bubonic plague is transmitted
Figure 3. Reported Cases of Human Plague – United States, 1970-2016
[Source 1]Figure 4. Human Plague Cases and Deaths – United States, 2000-2016 (in recent decades, an average of seven human plague cases have been reported each year, range: 1–17 cases per year).
Plague Worldwide
Plague epidemics have occurred in Africa, Asia, and South America but most human cases since the 1990s have occurred in Africa. Almost all of the cases reported in the last 20 years have occurred among people living in small towns and villages or agricultural areas rather than in larger towns and cities.
Figure 5. Reported Plague Cases by Country, 2010-2015
Three Major Plague Pandemics
There have been three plague pandemics in recorded history. The most famous was the second – the “Black Death” of the 14th to 17th centuries in Europe.
There was a smaller pandemic in the 19th and 20th centuries. However, little is currently known about the genetics of the first pandemic in recorded history – the “Plague of Justinian” of 6th–8th centuries AD. This was reported to have killed around 100 million people, and is seen by many historians as contributing to the fall of the Roman Empire and the onset of the Dark Ages.
The Justinian Plague
The first recorded pandemic, the Justinian Plague, was named after the 6th century Byzantine emperor Justinian I. The Justinian Plague began in 541 AD and was followed by frequent outbreaks over the next two hundred years that eventually killed over 25 million people 2 and affected much of the Mediterranean basin–virtually all of the known world at that time.
“Black Death” or the Great Plague
The second pandemic, widely known as the “Black Death” or the Great Plague, originated in China in 1334 and spread along the great trade routes to Constantinople and then to Europe, where it claimed an estimated 60% of the European population 3. Entire towns were wiped out. Some contemporary historians report that on occasion, there were not enough survivors remaining to bury the dead 4. Despite the vast devastation caused by this pandemic, however, massive labor shortages due to high mortality rates sped up the development of many economic, social, and technical modernizations 3. It has even been considered a factor in the emergence of the Renaissance in the late 14th century.
Modern Plague
The third pandemic, the Modern Plague, began in China in the 1860s and appeared in Hong Kong by 1894. Over the next 20 years, it spread to port cities around the world by rats on steamships. The pandemic caused approximately 10 million deaths 5. During this last pandemic, scientists identified the causative agent as a bacterium and determined that plague is spread by infectious flea bites. Rat-associated plague was soon brought under control in most urban areas, but the infection easily spread to local populations of ground squirrels and other small mammals in the Americas, Africa, and Asia. These new species of carriers have allowed plague to become endemic in many rural areas, including the western U.S.
However, as a bacterial disease, plague can be treated with antibiotics, and can be prevented from spreading by prompt identification, treatment and management of human cases. Applications of effective insecticides to control the flea vectors also provide assistance in controlling plague.
Recent Plague Outbreaks
The most recent plague epidemics have been reported in India during the first half of the 20th century, and in Vietnam during wartime in the 1960s and 1970s. Plague is now commonly found in sub-Saharan Africa and Madagascar, areas which now account for over 95% of reported cases 6.
What caused the black plague
The plague bacteria, Yersinia pestis, is transmitted to humans when they are bitten by fleas that have previously fed on infected animals, such as:
- Rats
- Squirrels
- Rabbits
- Prairie dogs
- Chipmunks
The bacteria can also enter your body if you have a break in your skin that comes into contact with an infected animal’s blood. Domestic cats and dogs can become infected with plague from flea bites or from eating infected rodents.
Pneumonic plague, which affects the lungs, is spread by inhaling infectious droplets coughed into the air by a sick animal or person.
Oriental rat flea – bubonic plague vector
The bacteria that cause plague, Yersinia pestis, maintain their existence in a cycle involving rodents and their fleas. Woodland rodents are the main reservoir of bubonic plague. They transmit the infection to domestic rats (Rattus rattus) by the rat flea (Xenopsylla cheopis). The fleas then transmit the infection to humans through biting.
Occasionally the infection is also transmitted to humans by infected feces being rubbed into skin wounds or though inhalation of droplets.
Risk factors for plague include a recent flea bite; and occupational or environmental exposure to rodents (especially rabbits, squirrels, or prairie dogs; or scratches or bites from infected domestic cats).
In urban areas or places with dense rat infestations, the plague bacteria can cycle between rats and their fleas. The last urban outbreak of rat-associated plague in the United States occurred in Los Angeles in 1924-1925.
Since that time, plague has occurred in rural and semi-rural areas of the western United States, primarily in semi-arid upland forests and grasslands where many types of rodent species can be involved. Many types of animals, such as rock squirrels, wood rats, ground squirrels, prairie dogs, chipmunks, mice, voles, and rabbits can be affected by plague. Wild carnivores can become infected by eating other infected animals.
Scientists think that plague bacteria circulate at low rates within populations of certain rodents without causing excessive rodent die-off. These infected animals and their fleas serve as long-term reservoirs for the bacteria. This is called the enzootic cycle.
Occasionally, other species become infected, causing an outbreak among animals, called an epizootic. Humans are usually more at risk during, or shortly after, a plague epizootic. Scientific studies have suggested that epizootics in the southwestern United States are more likely during cooler summers that follow wet winters. Epizootics are most likely in areas with multiple types of rodents living in high densities and in diverse habitats.
Transmission
The plague bacteria can be transmitted to humans in the following ways:
- Flea bites. Plague bacteria are most often transmitted by the bite of an infected flea. During plague epizootics, many rodents die, causing hungry fleas to seek other sources of blood. People and animals that visit places where rodents have recently died from plague are at risk of being infected from flea bites. Dogs and cats may also bring plague-infected fleas into the home. Flea bite exposure may result in primary bubonic plague or septicemic plague.
- Contact with contaminated fluid or tissue. Humans can become infected when handling tissue or body fluids of a plague-infected animal. For example, a hunter skinning a rabbit or other infected animal without using proper precautions could become infected with plague bacteria. This form of exposure most commonly results in bubonic plague or septicemic plague.
- Infectious droplets. When a person has plague pneumonia, they may cough droplets containing the plague bacteria into air. If these bacteria-containing droplets are breathed in by another person they can cause pneumonic plague. Typically this requires direct and close contact with the person with pneumonic plague. Transmission of these droplets is the only way that plague can spread between people. This type of spread has not been documented in the United States since 1924, but still occurs with some frequency in developing countries. Cats are particularly susceptible to plague, and can be infected by eating infected rodents. Sick cats pose a risk of transmitting infectious plague droplets to their owners or to veterinarians. Several cases of human plague have occurred in the United States in recent decades as a result of contact with infected cats.
Risk factors for developing plague
The risk of developing plague is very low. Worldwide, only a few thousand people develop plague each year. However, your risk of plague can be increased by where you live and travel, your occupation, and even by some of your hobbies.
Location
Plague outbreaks are most common in rural and semirural areas characterized by overcrowding, poor sanitation and a high rodent population. The greatest number of human plague infections occurs in Africa.
Occupation
Veterinarians and their assistants have a higher risk of coming into contact with domestic cats and dogs that may have become infected with plague. Also at higher risk are people who work outdoors in areas where plague-infected animals are common.
Hobbies
Camping, hunting or hiking in areas where plague-infected animals reside can increase your risk of being bitten by an infected flea.
Plague Prevention
- Reduce rodent habitat around your home, work place, and recreational areas. Remove brush, rock piles, junk, cluttered firewood, and possible rodent food supplies, such as pet and wild animal food. Make your home and outbuildings rodent-proof.
- Wear gloves if you are handling or skinning potentially infected animals to prevent contact between your skin and the plague bacteria. Contact your local health department if you have questions about disposal of dead animals.
- Use repellent if you think you could be exposed to rodent fleas during activities such as camping, hiking, or working outdoors. Products containing DEET can be applied to the skin as well as clothing and products containing permethrin can be applied to clothing (always follow instructions on the label).
- Keep fleas off of your pets by applying flea control products. Animals that roam freely are more likely to come in contact with plague infected animals or fleas and could bring them into homes. If your pet becomes sick, seek care from a veterinarian as soon as possible.
- Do not allow dogs or cats that roam free in endemic areas to sleep on your bed.
Note: A plague vaccine is no longer available in the United States. New plague vaccines are in development but are not expected to be commercially available in the immediate future.
Bubonic plague symptoms
Plague symptoms depend on how the patient was exposed to the plague bacteria. Plague can take different clinical forms, but the most common are bubonic, pneumonic, and septicemic.
Patients develop sudden onset of fever, headache, chills, and weakness and one or more swollen, tender and painful lymph nodes (called buboes). This form usually results from the bite of an infected flea. The bacteria multiply in the lymph node closest to where the bacteria entered the human body. If the patient is not treated with the appropriate antibiotics, the bacteria can spread to other parts of the body.
Bubonic plague
Bubonic plague is the most common variety of the disease. It’s named after the buboes — swollen lymph nodes — which typically develop within a week after an infected flea bites you. Buboes may be:
- Situated in the groin, armpit or neck
- About the size of a chicken egg
- Tender and warm to the touch
Other signs and symptoms may include:
- Sudden onset of fever and chills
- Headache
- Fatigue or malaise
- Muscle aches
Septicemic plague
Patients develop fever, chills, extreme weakness, abdominal pain, shock, and possibly bleeding into the skin and other organs. Skin and other tissues may turn black and die, especially on fingers, toes, and the nose. Septicemic plague can occur as the first symptom of plague, or may develop from untreated bubonic plague. This form results from bites of infected fleas or from handling an infected animal.
Pneumonic plague
Pneumonic plague affects the lungs. It’s the least common variety of plague but the most dangerous, because it can be spread from person to person via cough nfectious droplets. Patients develop fever, headache, weakness, and a rapidly developing pneumonia with shortness of breath, chest pain, cough, and sometimes bloody or watery mucous. Pneumonic plague may develop from inhaling infectious droplets or may develop from untreated bubonic or septicemic plague after the bacteria spread to the lungs. The pneumonia may cause respiratory failure and shock.
Signs and symptoms can begin within a few hours after infection, and may include:
- Cough, with bloody sputum
- Difficulty breathing
- Nausea and vomiting
- High fever
- Headache
- Weakness
Pneumonic plague progresses rapidly and may cause respiratory failure and shock within two days of infection. If antibiotic treatment isn’t initiated within a day after signs and symptoms first appear, the infection is likely to be fatal.
Plague complications
Complications of plague may include:
- Death. Most people who receive prompt antibiotic treatment survive bubonic plague. Untreated plague has a high fatality rate.
- Gangrene. Blood clots in the tiny blood vessels of your fingers and toes can disrupt the flow of blood and cause that tissue to die. The portions of your fingers and toes that have died may need to be amputated.
- Meningitis. Rarely, plague may cause inflammation of the membranes surrounding your brain and spinal cord (meningitis).
Bubonic plague diagnosis
Plague should be considered in any patient with clinical signs of plague and a recent history of travel to the western United States or any other plague endemic area. Bubonic plague is the most common primary manifestation, with a bubo usually occurring in the groin, axilla or cervical nodes. Buboes are often so painful that patients are generally guarded and have restricted movement in the affected region. The incubation period for bubonic plague is usually 2 to 6 days.
If bubonic plague is untreated, plague bacteria invade the bloodstream and spread rapidly, causing septicemic plague, and if the lungs are seeded, secondary pneumonic plague. Septicemic and pneumonic plague may also be primary manifestations. A person with pneumonic plague may experience high fever, chills, cough, and breathing difficulty and may expel bloody sputum. If pneumonic plague patients are not given specific antibiotic therapy, the disease can progress rapidly to death.
Although the majority of patients with plague present with a bubo, some may have nonspecific symptoms. For example, septicemic plague can present with prominent gastrointestinal symptoms such as nausea, vomiting, diarrhea, and abdominal pain 7. Additional rare forms of plague include pharyngeal, meningeal, and cutaneous.
In many cases, particularly in septicemic and pneumonic plague, there are no obvious signs that indicate plague. Diagnosis is made by taking samples from the patient, especially blood or part of a swollen lymph gland, and submitting them for laboratory testing. Once plague has been identified as a possible cause of the illness, appropriate treatment should begin immediately.
Appropriate diagnostic samples include blood cultures, lymph node aspirates if possible, and/or sputum, if indicated. Drug therapy should begin as soon as possible after the laboratory specimens are taken. If plague is suspected, local and state health departments should be notified immediately. If the patient has pneumonic signs, he/she should also be isolated and placed on droplet precautions.
If your doctor suspects plague, he or she may look for the Yersinia pestis bacteria in samples taken from your:
- Buboes. If you have the swollen lymph nodes (buboes) characteristic of bubonic plague, a fluid sample can be taken from them with a needle.
- Blood. Yersinia pestis bacteria generally are present in your bloodstream only if you have septicemic plague.
- Lungs. To check for pneumonic plague, your doctor will take sputum or fluid from your airways using endoscopy — a thin, flexible tube inserted through your nose or mouth and down your throat.
Diagnostic Testing
If plague is suspected, pre-treatment specimens should be taken if possible, but treatment should not be delayed. Specimens should be obtained from appropriate sites for isolating the bacteria, and depend on the clinical presentation:
- Lymph node aspirate: An affected bubo should contain numerous organisms that can be evaluated microscopically and by culture.
- Blood cultures: Organisms may be seen in blood smears if the patient is septicemic. Blood smears taken from suspected bubonic plague patients early in the course of illness are usually negative for bacteria by microscopic examination but may be positive by culture.
- Sputum: Culture is possible from sputum of very ill pneumonic patients; however, blood is usually culture-positive at this time as well.
- Bronchial/tracheal washing may be taken from suspected pneumonic plague patients; throat specimens are not ideal for isolation of plague since they often contain many other bacteria that can mask the presence of plague.
- In cases where live organisms are unculturable (such as postmortem), lymphoid, spleen, lung, and liver tissue or bone marrow samples may yield evidence of plague infection by direct detection methods such as direct fluorescent antibody or PCR.
Yersinia pestis may be identified microscopically by examination of Gram, Wright, Giemsa, or Wayson’s stained smears of peripheral blood, sputum, or lymph node specimen.Visualization of bipolar-staining, ovoid, Gram-negative organisms with a “safety pin” appearance permits a rapid presumptive diagnosis of plague.
If cultures yield negative results, and plague is still suspected, serologic testing is possible to confirm the diagnosis. One serum specimen should be taken as early in the illness as possible, followed by a convalescent sample 4-6 weeks or more after disease onset.
Bubonic plague treatment
Begin appropriate IV (intravenous) therapy as soon as plague is suspected. Gentamicin and fluoroquinolones are typically first-line treatments in the United States. Duration of treatment is 10 to 14 days, or until 2 days after fever subsides. Oral therapy may be substituted once the patient improves.
The regimens listed below are guidelines only and may need to be adjusted depending on a patient’s age, medical history, underlying health conditions, or allergies. Please use clinical judgment.
Table 1. Recommended antibiotic treatment of adults for plague
| Antibiotic | Dose | Route of administration | Notes |
|---|---|---|---|
| Streptomycin | 1 g twice daily | IM | Not widely available in the US |
| Gentamicin | 5 mg/kg once daily, or 2 mg/kg loading dose followed by 1.7 mg/kg every 8 hours | IM or IV | Not FDA approved but considered an effective alternative to streptomycin 8. Due to poor abscess penetration, consider alternative or dual therapy for patients with bubonic disease. |
| Levofloxacin | 500 mg once daily | IV or po | Bactericidal. FDA approved based on animal studies but limited clinical experience treating human plague. A higher dose (750 mg) may be used if clinically indicated. |
| Ciprofloxacin | 400 mg every 8-12 hours | IV | Bactericidal. FDA approved based on animal studies but limited clinical experience treating human plague. |
| 500-750 mg twice daily | po | ||
| Doxycycline | 100 mg twice daily or 200 mg once daily | IV or po | Bacteriostatic, but effective in a randomized trial when compared to gentamicin 9. |
| Moxifloxacin | 400 mg once daily | IV or po | |
| Chloramphenicol | 25 mg/kg every 6 hours | IV | Not widely available in the United States. |
Note: IV = intravenous; IM = intramuscular; po = oral
Table 2. Recommended antibiotic treatment of children for plague
| ntibiotic | Dose | Route of administration | Notes |
|---|---|---|---|
| Streptomycin | 15 mg/kg twice daily (maximum 2 g/day) | IM | Not widely available in the United States. |
| Gentamicin | 2.5 mg/kg/dose every 8 hours | IM or IV | Not FDA approved but considered an effective alternative to streptomycin 8. Due to poor abscess penetration, consider alternative or dual therapy for patients with bubonic disease. |
| Levofloxacin | 8 mg/kg/dose every 12 hours (max 250 mg per dose) | IV or po | Bactericidal. This dosing regimen is based on the levofloxacin package insert and is recommended for pediatric patients <50 kg and ≥6 months of age. FDA approved based on animal studies but limited clinical experience treating human plague. |
| Ciprofloxacin | 15 mg/kg/dose every 12 hours (maximum 400 mg/dose) | IV | Bactericidal. FDA approved based on animal studies but limited clinical experience treating human plague. |
| 20 mg/kg/dose every 12 hours (maximum 500 mg/dose) | po | ||
| Doxycycline | Weight < 45 kg: 2.2 mg/kg twice daily (maximum 100 mg/dose) Weight ≥ 45 kg: same as adult dose | IV or po | Bacteriostatic, but FDA approved and effective in a randomized trial when compared to gentamicin 9. No tooth staining after multiple short courses 10. |
| Chloramphenicol (for children > 2 years) | 25 mg/kg every 6 h (maximum daily dose, 4 g) | IV | Not widely available in the United States |
Table 3. Recommended antibiotic treatment of pregnant women for plague
| Antibiotic | Dose | Route of administration | Notes |
|---|---|---|---|
| Gentamicin | Same as adult dose | IM or IV | See notes above |
| Doxycycline | Same as adult dose | IV | See notes above |
| Ciprofloxacin | Same as adult dose | IV | See notes above |
Note: All recommended antibiotics for plague have relative contraindications for use in children and pregnant women; however, use is justified in life-threatening situations.
Post-exposure prophylaxis
Post-exposure prophylaxis is indicated in persons with known exposure to plague, such as close contact with a pneumonic plague patient or direct contact with infected body fluids or tissues. Duration of post-exposure prophylaxis to prevent plague is 7 days. The recommended antibiotic regimens for post-exposure prophylaxis are as follows:
Table 4. Post-exposure prophylaxis
| Preferred agents | Dose | Route of administration | |
|---|---|---|---|
| Adults | Doxycycline | 100 mg twice daily | PO |
| Ciprofloxacin | 500 mg twice daily | PO | |
| Children | Doxycycline (for children ≥ 8 years) | Weight < 45 kg: 2.2 mg/kg twice daily (maximum daily dose, 200 mg) Weight ≥ 45 kg: same as adult dose | PO |
| Ciprofloxacin | 20 mg/kg twice daily (maximum daily dose, 1 g) | PO | |
| Pregnant women | Doxycycline1 | 100 mg twice daily | PO |
| Ciprofloxacin1 | 500 mg twice daily | PO |
- Plague Maps and Statistics. https://www.cdc.gov/plague/maps/index.html[↩]
- Rosen, William (2007), Justinian’s Flea: Plague, Empire, and the Birth of Europe. Viking Adult; pg 3; ISBN 978-0-670-03855-8.[↩]
- Benedictow, Ole J. 2004. The Black Death 1346-1353: The Complete History. Woodbridge: Boydell Press.[↩][↩]
- Gross, L. How the plague bacillus and its transmission through fleas were discovered: reminiscences from my years at the Pasteur Institute in Paris.Proc Natl Acad Sci U S A. 1995 August 15; 92(17):7609–7611.[↩]
- Khan, IA. Plague: the dreadful visitation occupying the human mind for centuries. Trans R Soc Trop Med Hyg. 2004 May;98(5):270-7. https://www.sciencedirect.com/science/article/pii/S0035920303000592[↩]
- Stenseth NC, Atshabar BB, Begon M, Belmain SR, Bertherat E, et al. Plague: Past, present, and future. PLoS Med. 2008 5(1): e3.[↩]
- Human plague–four states, 2006. MMWR Morb Mortal Wkly Rep. 2006 Sep 1;55(34):940-3. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5534a4.htm[↩]
- Boulanger LL, Ettestad P, Fogarty JD, Dennis DT, Romig D, Mertz G. Gentamicin and tetracyclines for the treatment of human plague: Review of 75 cases in New Mexico, 1985–1999. Clin Infect Dis. 2004 38(5):663-669. https://academic.oup.com/cid/article/38/5/663/280302[↩][↩]
- Mwengee W, Butler T, Mgema S, Mhina G, Almasi Y, Bradley C, Formanik JB, Rochester CG. Treatment of plague with gentamicin or doxycycline in a randomized clinical trial in Tanzania. Clin Infect Dis. 2006 42(5):614-21. https://academic.oup.com/cid/article/38/5/663/280302[↩][↩]
- Todd SR, Dahlgren FS, Traeger MS, Beltrán-Aguilar ED, Marianos DW, Hamilton C, McQuiston JH, Regan JJ. No visible dental staining in children treated with doxycycline for suspected Rocky Mountain spotted fever. J Pediatr. 2015 May;166(5):1246-51. https://www.sciencedirect.com/science/article/pii/S0022347615001353[↩]