Contents
- What is mumps
- What do mumps look like
- Mumps complications
- Mumps outbreak
- Mumps causes
- Mumps prevention
- Mumps vaccine
- Who Should Get MMR Vaccine?
- Risks of a mumps vaccine reaction
- Who DON’T need the MMR vaccine?
- Who should WAIT to get the MMR vaccine
- Who should check with their doctors
- Who Should NOT Get MMR Vaccine?
- State Vaccination Requirements
- Information for Travelers 4
- I got the vaccine but still got mumps. Does this mean the vaccine doesn’t work?
- Mumps vaccine
- Mumps symptoms
- Mumps diagnosis
- Mumps treatment
What is mumps
Mumps (or “the mumps”) is a contagious viral infection (mumps virus) that is most common in children between two and 15 years of age who haven’t received the mumps vaccine, but you can catch it at any age. You can catch mumps by being with another person who has mumps. There is no treatment for mumps, but the measles-mumps-rubella (MMR) vaccine can prevent it. Before the routine vaccination program in the United States, mumps was a common illness in infants, children and young adults. These days mumps is rarely seen because of effective vaccination.
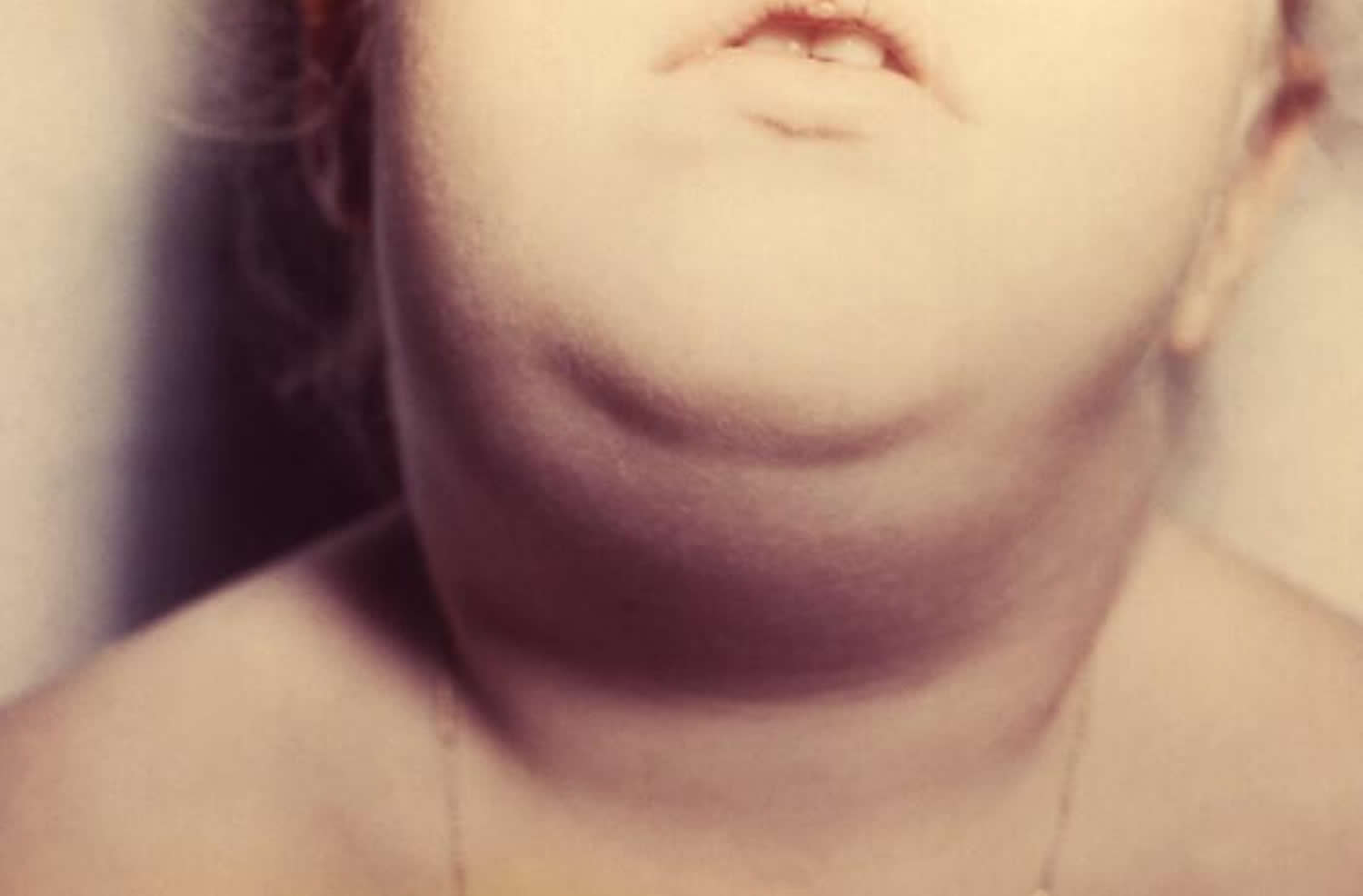
Mumps starts with infection of the salivary glands under your ears or jaw where they become swollen and tender (parotitis). Mumps is most recognizable by the painful swellings located at the side of the face under the ears (the parotid glands), giving a person with mumps a distinctive ‘hamster face’ or ‘chipmunk cheeks’ appearance. The swelling can be on one or both sides of the face. Symptoms last 7 to 10 days. This swollen parotid glands can be very painful, and is sometimes the only symptom.
Many people also experience:
- Fever as high as 103°F to 104°F (39.4 °C to 40 °C) starting after the first few days and lasting for 2 to 3 days
- Headache
- Chills
- Lack of appetite
- Face pain
- Muscle aches and joint pain
- Tiredness
- Loss of appetite
- Sore throat
- Swelling of the temples or jaw
Serious complications are rare.
Mumps is caused by the mumps virus, which belongs to a family of viruses known as ‘paramyxoviruses’. Mumps virus is spread by close contact or by coughing and sneezing. Paramyxoviruses are a common source of infection, particularly in children.
If you have mumps, you can help prevent it spreading by:
- regularly washing your hands with soap
- using and disposing of tissues when you sneeze
- avoiding school or work for at least five days after your symptoms first develop
When you get mumps, the virus moves from your respiratory tract (your nose, mouth and throat) into your parotid glands (the glands that produce saliva), where it begins to reproduce. This causes inflammation and swelling of the glands.
The mumps virus can less commonly spread to other areas of your body, which may lead to other serious conditions. When the mumps virus enters your cerebrospinal fluid (CSF), which is the fluid that surrounds and protects your brain and spine, it can also lead to hearing loss and meningitis (infection of membranes that cover the brain and spinal cord). The mumps virus can spread to other parts of your body, such as your brain, pancreas, testes (in boys and men) and ovaries (in girls and women). Mumps can also cause miscarriage in pregnant women.
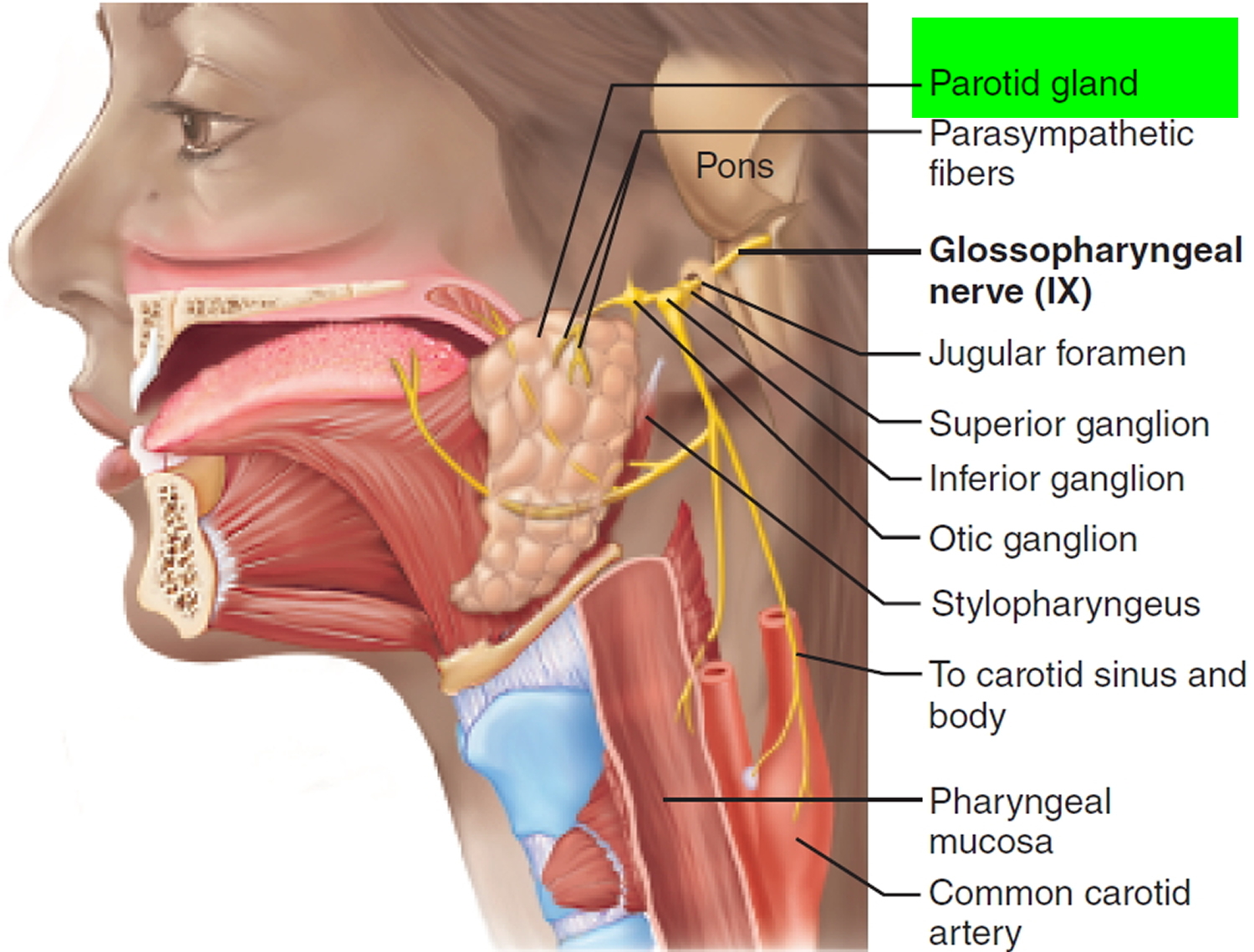
Figure 1. Parotid gland
If you suspect that you or your child has mumps, see your doctor. Let your doctor’s office know before you go in that you suspect mumps so that you won’t have to wait so long in the waiting room, possibly infecting others. Mumps has become an uncommon illness, so it’s possible that the signs and symptoms are caused by another condition. Swollen salivary glands and a fever could be an indication of inflamed tonsils (tonsillitis) or a blocked salivary gland.
Other viruses can infect the parotid glands, causing a mumps-like illness.
See your doctor if you notice:
- Severe headache
- Stiff neck
- Eye redness
- Drowsiness
- Abdominal pain
- Vomiting
- Testicle pain or lump
Women who are pregnant and may have been exposed to mumps should call the doctor, even if they don’t show any symptoms.
If seizures occur, seek emergency medical care.
Is mumps a serious disease?
Mumps can be serious, but most people with mumps recover completely in a few weeks. While infected with mumps, many people feel tired and achy, have a fever, and swollen salivary glands on the side of the face. Others may feel extremely ill and be unable to eat because of jaw pain, and a few will develop serious complications. Men and adolescent boys can develop pain or swelling in their testicles, which rarely results in sterility. Inflammation of the protective membranes covering the brain and spinal cord (meningitis) and loss of hearing can also occur, and in rare cases, this hearing loss can be permanent. The most serious complication is inflammation of the brain (encephalitis), which can lead to death or permanent disability.
What do mumps look like
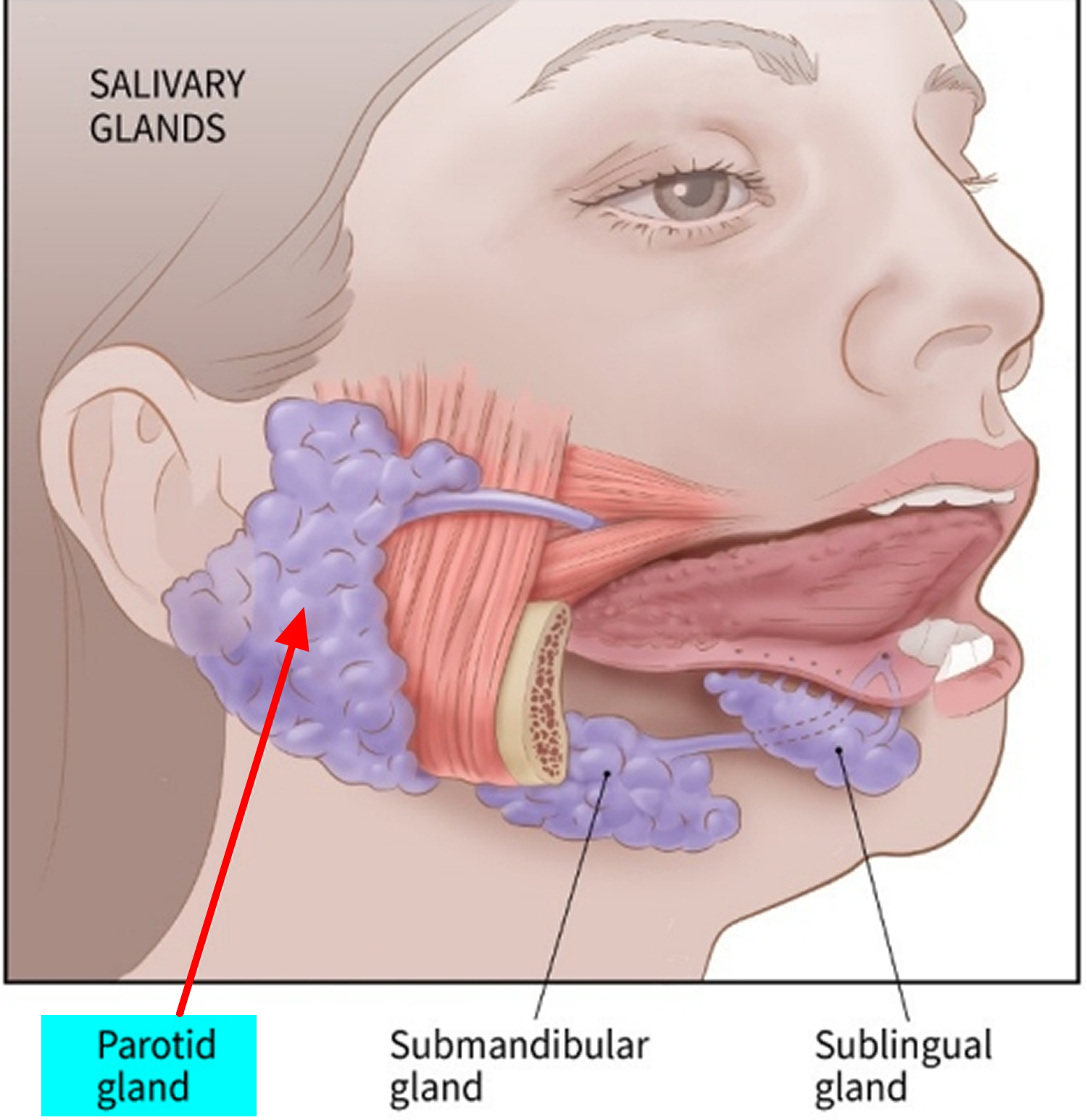
Figure 2. Mumps
Mumps complications
Some complications of mumps are known to occur more frequently among adults than children. Death from mumps is exceedingly rare.
In recent U.S. mumps outbreaks, orchitis occurred in 3.3 to 10% of adolescent and adult males. In 60% to 83% of males with orchitis caused by mumps, only one testis is affected. Such orchitis, even bilaterally, very rarely causes sterility. Among adolescent and adult females in recent outbreaks, mastitis rates have been ≤1% and oophoritis rates have been ≤1%. Other rare complications of mumps include pancreatitis, deafness, meningitis, and encephalitis, which have occurred in less than 1% of cases in recent U.S. outbreaks. There have been no mumps related deaths reported in the United States during recent mumps outbreaks.
Inflammation
Most mumps complications involve inflammation and swelling in some part of the body, such as:
- Testicles. This condition, known as orchitis, causes one or both testicles to swell in males who’ve reached puberty. Orchitis is painful, but it rarely leads to sterility — the inability to father a child.
- Pancreas. The signs and symptoms of this condition, known as pancreatitis, include pain in the upper abdomen, nausea and vomiting.
- Pancreatitis: About 1 in 20 cases of mumps lead to short-term inflammation of the pancreas (acute pancreatitis). The most common symptom is sudden pain in the centre of your belly. Other symptoms of acute pancreatitis can include:
- feeling or being sick
- diarrhea
- loss of appetite
- high temperature
- tenderness of the belly
- less commonly, yellowing of the skin and the whites of the eyes (jaundice)
- Although pancreatitis associated with mumps is usually mild, you may be admitted to hospital so your body functions can be supported until your pancreas recovers.
- Pancreatitis: About 1 in 20 cases of mumps lead to short-term inflammation of the pancreas (acute pancreatitis). The most common symptom is sudden pain in the centre of your belly. Other symptoms of acute pancreatitis can include:
- Ovaries and breasts. Females who’ve reached puberty may have inflammation in the ovaries (oophoritis) or breasts (mastitis). Fertility is rarely affected.
- Swollen ovaries:
- One in 20 females who get mumps after puberty experience swelling of the ovaries (oophoritis), which can cause:
- lower abdominal pain
- high temperature
- being sick
- The symptoms of oophoritis usually pass once the body has fought off the underlying mumps infection.
- One in 20 females who get mumps after puberty experience swelling of the ovaries (oophoritis), which can cause:
- Swollen ovaries:
- Brain. A viral infection, such as mumps, can lead to inflammation of the brain (encephalitis). Encephalitis can lead to neurological problems and become life-threatening.
- Viral meningitis
- Viral meningitis can occur if the mumps virus spreads into the outer protective layer of the brain (the meninges). It occurs in about one in seven cases of mumps.
- Unlike bacterial meningitis, which is regarded as a potentially life-threatening medical emergency, viral meningitis causes milder, flu-like symptoms, and the risk of serious complications is low.
- Sensitivity to light, neck stiffness and headaches are common symptoms of viral meningitis. These usually pass within 14 days.
- Viral meningitis
- Membranes and fluid around the brain and spinal cord. This condition, known as meningitis, can occur if the mumps virus spreads through your bloodstream to infect your central nervous system.
Rare complications of mumps
Rare but potentially serious complications of mumps include an infection of the brain itself, known as encephalitis. This is thought to occur in around 1 in 1,000 people who develop viral meningitis from mumps. Encephalitis is a potentially fatal condition that requires admission to a hospital intensive care unit.
About 1 in 20 people with mumps experience some temporary hearing loss, but permanent loss of hearing is rare. It’s estimated this occurs in around 1 in 20,000 cases of mumps.
- Hearing loss. In rare cases, mumps can cause hearing loss, usually permanent, in one or both ears.
Mumps and pregnancy
In the past it was thought developing mumps during pregnancy increased the risk of miscarriage, but there’s little evidence to support this. But, as a general precaution it’s recommended pregnant women avoid close contact with people known to have an active mumps infection (or any other type of infection).
If you’re pregnant and you think you’ve come into contact with someone with mumps but you haven’t been vaccinated, contact your doctor for advice.
There’s no cure for mumps but a doctor will be able to suggest treatment to relieve your symptoms.
Mumps outbreak
Mumps outbreaks can occur any time of year. A major factor contributing to mumps outbreaks is being in a crowded environment, such as attending the same class, playing on the same sports team, or living in a dormitory with a person who has mumps. Also, certain behaviors that result in exchanging saliva, such as kissing or sharing utensils, cups, lip balm or cigarettes, might increase spread of the virus. In some years, there are more cases of mumps than usual because of outbreaks.
Mumps outbreaks can still occur in highly vaccinated U.S. communities, particularly in close-contact settings. In recent years, outbreaks have occurred in schools, colleges, and camps. However, high vaccination coverage helps limit the size, duration, and spread of mumps outbreaks. Measles, mumps and rubella (MMR) vaccine prevents most, but not all, cases of mumps and complications caused by the disease. Two doses of the vaccine are 88% (range: 66 to 95%) effective at protecting against mumps; one dose is 78% (range: 49% to 92%) effective. Studies have shown that the measles, mumps and rubella (MMR) vaccine protects against currently circulating mumps strains.
Although it is not mandatory to report mumps outbreaks to Centers for Disease Prevention and Control (CDC), many health departments will contact CDC when they experience an unusually high number of cases. In 2016 and 2017, a number of cases and outbreaks have been reported to CDC, primarily associated with college settings. These outbreaks have ranged in size from a few to several hundred cases, have mostly affected young adults, and are likely due to a combination of factors. These factors include the known effectiveness of the vaccine, waning immunity following vaccination, and the intensity of exposure to the virus in close-contact settings (such as a college campus) coupled with behaviors that increase the risk of transmission.
Past Mumps Outbreaks 1
- In 2016-17, a large outbreak in a close-knit community in northwest Arkansas, resulted in nearly 3,000 cases.
- In 2015-16*, outbreaks were reported from several university campuses, including a number of smaller outbreaks with limited spread. The two largest outbreaks were from Iowa and Illinois, each involving several hundred university students; both held wide-scale vaccination campaigns.
- In 2014, several outbreaks affiliated with universities were reported from multiple states, including one community outbreak in Ohio linked to a university that involved over 400 people, and an outbreak affecting the National Hockey League.
- In 2011-2013, there were several smaller mumps outbreaks reported on college campuses in California, Virginia, and Maryland. However, these all had limited spread, and national case counts for these years were at several hundred cases per year.
- In 2009 to 2010, two large outbreaks occurred.
- One multi-year outbreak involved over 3,000 people and mostly affected high school-aged students who were part of a close-knit religious community in New York City and attended schools in which they had very close contact. The outbreak started when an infected student in this religious community returned from the United Kingdom where a large mumps outbreak was occurring.
- The second outbreak involved about 500 people, mostly school-aged children, in the U.S. Territory of Guam.
- In 2006, the United States experienced a multi-state mumps outbreak involving more than 6,500 reported cases. This resurgence predominantly affected college-aged students living in the Midwest, with outbreaks occurring on many different Midwestern college campuses.
What should I do during a mumps outbreak?
Make sure you are up to date on your MMR vaccine. Visit the Mumps Vaccination page to see recommendations for different groups. Let your doctor know right away if you think that you or someone in your family may have mumps.
In any situation, including when there is a mumps outbreak, washing hands often with soap and water and having good health practices are the most important steps you can take to avoid getting sick and spreading germs to others.
Mumps causes
Mumps is caused by mumps virus that is spread by infected saliva or mucus from the mouth, nose, or throat. This means the virus can spread very much like the common cold. For example, if an infected person sneezes near you or you touch something that an infected person has touched, and you have not been vaccinated, you may get the mumps. Mumps likely spreads before the salivary glands begin to swell and up to five days after the swelling begins.
An infected person can spread the virus by:
- coughing, sneezing, or talking,
- sharing items, such as cups or eating utensils, with others, and
- touching objects or surfaces with unwashed hands that are then touched by others.
Normally, you won’t get sick until 12 to 24 days after being exposed to the virus. These 12 to 24 days are called the incubation period.
I’ve been told that I need to stay away from people while I’m sick with mumps. What does that mean and why does it matter?
When you have mumps, you should avoid prolonged, close contact with other people until at least five days after your salivary glands begin to swell because you are contagious during this time. You should not go to work or school. You should stay home when you are sick with mumps and limit contact with the people you live with; for example, sleep in a separate room by yourself if you can. Staying home while sick with mumps is an important way to avoid spreading the virus to other people. People who are infected with mumps don’t get sick right away—it can take 2 to 4 weeks for them to show signs of infection
What else should I do to prevent mumps from spreading?
In addition to staying away from others when you have mumps, you can help prevent the virus from spreading by:
- Covering your mouth and nose with a tissue when you cough or sneeze, and put your used tissue in the trash can. If you don’t have a tissue, cough or sneeze into your upper sleeve or elbow, not your hands.
- Washing your hands often with soap and water.
- Avoiding sharing drinks or eating utensils.
- Disinfecting frequently touched surfaces, such as toys, doorknobs, tables, counters.
Mumps prevention
The measles, mumps and rubella (MMR) vaccine prevents the mumps in 80% to 90% of people. Two doses are more effective than one. Before the U.S. mumps vaccination program started in 1967, about 186,000 cases were reported each year, but the actual number of cases was likely much higher due to underreporting. Since the pre-vaccine era, there has been a more than 99% decrease in mumps cases in the United States. Since the two-dose vaccination program was introduced in 1989, mumps cases have ranged year to year from a couple of hundred to several thousand. However, in recent years, there has been an increase in the number of reported cases, from 229 cases in 2012 to 6,366 cases in 2016. The recent increase has been mainly due to multiple mumps outbreaks reported across the country in settings where people often have close contact with one another, like college campuses.
Mumps outbreaks can still occur in highly vaccinated U.S. communities, particularly in close-contact settings such as schools, colleges, and camps. However, high vaccination coverage helps to limit the size, duration, and spread of mumps outbreaks. Outbreaks can still occur in locations where vaccination rates are low.
Mumps vaccine
The measles, mumps and rubella (MMR) vaccine is usually given to infants 12 to 15 months of age. Children often are given the vaccine between ages 4 to 6 or between ages 11 to 12 if they haven’t yet received it. However, it is never too late to be vaccinated. If you work in a public setting or in the health care field, you should get vaccinated if you haven’t already. Talk to your doctor if you think you may need to be vaccinated.
The measles, mumps and rubella (MMR) vaccine protects against three diseases: Measles, Mumps, and Rubella. Centers for Disease Prevention and Control (CDC) recommends children get two doses of MMR vaccine, starting with the first dose at 12 through 15 months of age, and the second dose at 4 through 6 years of age. Teens and adults also should also be up to date on their MMR vaccination.
Children should get 2 doses of MMR vaccine, usually:
- First dose: 12 through 15 months of age
- Second dose: 4 through 6 years of age
Infants who will be traveling outside the United States when they are between 6 and 11 months of age should get a dose of MMR vaccine before travel. This can provide temporary protection from measles infection, but will not give permanent immunity. The child should still get 2 doses at the recommended ages for long-lasting protection.
Adults might also need MMR vaccine. Many adults 18 years of age and older might be susceptible to measles, mumps, and rubella without knowing it.
A third dose of MMR might be recommended in certain mumps outbreak situations.
There are no known risks to getting MMR vaccine at the same time as other vaccines.
MMR vaccine is very safe and effective. The mumps component of the MMR vaccine is about 88% (range: 66-95%) effective when a person gets two doses; one dose is about 78% (range: 49%−92%) effective.
Children may also get MMRV vaccine, which protects against measles, mumps, rubella, and varicella (chickenpox). This vaccine is only licensed for use in children who are 12 months through 12 years of age.
Who Should Get MMR Vaccine?
Children
CDC recommends all children get two doses of MMR (measles-mumps-rubella) vaccine, starting with the first dose at 12 through 15 months of age, and the second dose at 4 through 6 years of age. Children can receive the second dose earlier as long as it is at least 28 days after the first dose.
MMR vaccine is given later than some other childhood vaccines because antibodies transferred from the mother to the baby can provide some protection from disease and make the MMR vaccine less effective until about 1 year of age.
MMRV (measles, mumps, rubella, and varicella) vaccine protects against four diseases: measles, mumps, rubella, and varicella (chickenpox). This vaccine is only licensed for use in children 12 months through 12 years of age. CDC recommends that children get one dose of MMRV vaccine at 12 through 15 months of age, and the second dose at 4 through 6 years of age. A doctor can help parents decide whether to use this vaccine or MMR vaccine. MMRV is given by shot and may be given at the same time as other vaccines.
Students at post-high school educational institutions
Students at post-high school educational institutions who do not have evidence of immunity need two doses of MMR vaccine, separated by at least 28 days.
Adults
Adults who do not have evidence of immunity should get at least one dose of MMR vaccine.
International travelers
People 6 months of age and older who will be traveling internationally should be protected against measles. Before any international travel:
- Infants 6 through 11 months of age should receive one dose of MMR vaccine. Infants who get one dose of MMR vaccine before their first birthday should get two more doses (one dose at 12 through 15 months of age and another dose separated by at least 28 days).
- Children 12 months of age and older should receive two doses of MMR vaccine, separated by at least 28 days.
- Teenagers and adults who do not have evidence of immunity against measles should get two doses of MMR vaccine separated by at least 28 days.
Women of Childbearing Age
Women of childbearing age should check with their doctor to make sure they are vaccinated before they get pregnant. Women of childbearing age who do not have evidence of immunity should get at least one dose of MMR vaccine.
It is safe for breastfeeding women to receive MMR vaccination. Breastfeeding does not interfere with the response to MMR vaccine, and the baby will not be affected by the vaccine through breast milk.
Risks of a mumps vaccine reaction
You can’t get mumps from the MMR vaccine, and most people experience no side effects from the vaccine. A few may experience a mild fever or rash, and some people (mostly adults) have achy joints afterward for a short time. Less than one out of 1 million doses causes a serious allergic reaction.
Although concerns have been raised about a connection between the MMR vaccine and autism, extensive reports from the American Academy of Pediatrics, the Institute of Medicine and the Centers for Disease Control and Prevention conclude that there’s no scientifically proven link between the MMR vaccine and autism.
However, with any medicine, including vaccines, there is a chance of reactions. These are usually mild and go away on their own, but serious reactions are also possible.
Getting MMR vaccine is much safer than getting measles, mumps, or rubella disease. Most people who get MMR vaccine do not have any problems with it.
After MMR vaccination, a person might experience:
Minor events:
- Sore arm from the injection
- Fever
- Redness or rash at the injection site
- Swelling of glands in the cheeks or neck
If these events happen, they usually begin within 2 weeks after the shot. They occur less often after the second dose.
Moderate events:
- Seizure (jerking or staring) often associated with fever
- Temporary pain and stiffness in the joints, mostly in teenage or adult women
- Temporary low platelet count, which can cause unusual bleeding or bruising
- Rash all over body
Severe events occur very rarely:
- Deafness
- Long-term seizures, coma, or lowered consciousness
- Brain damage
Other things that could happen after this vaccine:
- People sometimes faint after medical procedures, including vaccination. Sitting or lying down for about 15 minutes can help prevent fainting and injuries caused by a fall. Tell your provider if you feel dizzy or have vision changes or ringing in the ears.
- Some people get shoulder pain that can be more severe and longer-lasting than routine soreness that can follow injections. This happens very rarely.
- Any medication can cause a severe allergic reaction. Such reactions to a vaccine are estimated at about 1 in a million doses, and would happen within a few minutes to a few hours after the vaccination.
As with any medicine, there is a very remote chance of a vaccine causing a serious injury or death.
Should You Get Vaccinated After Being Exposed to Measles, Mumps, or Rubella?
If you do not have immunity against measles, mumps, or rubella and are exposed to someone with one of these diseases, talk with your doctor about getting MMR vaccine. It is not harmful to get MMR vaccine after being exposed to measles, mumps, or rubella, and doing so may possibly prevent later disease.
During outbreaks, everyone without evidence of immunity should be brought up to date on their MMR vaccination. Sometimes during measles and mumps outbreaks, an additional dose of MMR may be given.
If you get MMR vaccine within 72 hours of initially being exposed to measles, you may get some protection against the disease, or have milder illness. Also, if you are given a medicine called immunoglobulin (IG) within six days of being exposed to measles, you may get some protection against the disease, or have milder illness. Except in healthcare settings, unvaccinated people who get their first dose of MMR vaccine within 72 hours after being exposed to measles may return to childcare, school, or work.
Who DON’T need the MMR vaccine?
You don’t need a MMR vaccine if you:
- Had two doses of the MMR vaccine after 12 months of age or one dose of the MMR vaccine plus a second dose of the measles vaccine
- Had one dose of MMR and you’re not at high risk of measles or mumps exposure
- Have blood tests that demonstrate you’re immune to measles, mumps and rubella
- Are a man who was born before 1957
- Are a woman who was born before 1957 and you don’t plan to have any more children
Also, the vaccine isn’t recommended for:
- Pregnant women or women who plan to get pregnant within the next four weeks
- People who have had a life-threatening allergic reaction to gelatin or the antibiotic neomycin
- People with severely compromised immune systems, or people who take oral steroids, unless the benefits of the vaccine exceed the risks.
Who should WAIT to get the MMR vaccine
Consider waiting if:
- You’re moderately or severely ill. Wait until you recover.
- You’re pregnant. Wait until after you give birth.
Who should check with their doctors
Check with your doctor before getting vaccinated for mumps if:
- You have cancer
- You have a blood disorder
- You have a disease that affects your immune system, such as HIV/AIDS
- You’re being treated with drugs, such as steroids, that affect your immune system
- You’ve received another vaccine within the past four weeks
Who Should NOT Get MMR Vaccine?
Measles, Mumps, and Rubella (MMR) vaccine
Some people should not get MMR vaccine or should wait.
- Anyone who has ever had a life-threatening allergic reaction to the antibiotic neomycin, or any other component of MMR vaccine, should not get the vaccine. Tell your doctor if you have any severe allergies.
- Anyone who had a life-threatening allergic reaction to a previous dose of MMR or MMRV vaccine should not get another dose.
- Some people who are sick at the time the shot is scheduled may be advised to wait until they recover before getting MMR vaccine.
- Pregnant women should not get MMR vaccine. Pregnant women who need the vaccine should wait until after giving birth. Women should avoid getting pregnant for 4 weeks after vaccination with MMR vaccine.
- Tell your doctor if the person getting the vaccine:
- Has HIV/AIDS, or another disease that affects the immune system
- Is being treated with drugs that affect the immune system, such as steroids
- Has any kind of cancer
- Is being treated for cancer with radiation or drugs
- Has ever had a low platelet count (a blood disorder)
- Has gotten another vaccine within the past 4 weeks
- Has recently had a transfusion or received other blood products
- Any of these might be a reason to not get the vaccine, or delay vaccination until later.
A minor illness, such as a cold or chickenpox, should not delay anyone from receiving the benefits of MMR or any other vaccine. In addition, it is safe for people around a pregnant woman to be vaccinated. Measles, mumps, and rubella vaccine viruses are not transmitted from the vaccinated person, so a recently vaccinated person would not pose a risk to a pregnant woman.
State Vaccination Requirements
All 50 states and the District of Columbia (DC) have state laws that require children entering childcare or public schools to have certain vaccinations 2. State laws establish vaccination requirements for school children. These laws often apply not only to children attending public schools but also to those attending private schools and day care facilities. All states provide medical exemptions, and some state laws also offer exemptions for religious and/or philosophical reasons. State laws also establish mechanisms for enforcement of school vaccination requirements and exemptions.
The Advisory Committee on Immunization Practices 3 recommends that all states require children entering childcare, and students starting school, college, and other postsecondary educational institutions to be up to date on MMR vaccination:
- 1 dose is recommended for preschool-aged children 12 months or older
- 2 doses are recommended for school-aged children in kindergarten through grade 12 as well as students attending colleges or other post-high school educational institutions.
Information for Travelers 4
Mumps remains a common disease in many parts of the world, including areas in Europe, Asia, the Pacific, and Africa. Anyone who is not protected against mumps is at risk of getting infected when they travel internationally.
Before traveling internationally, people should be protected against mumps.
- Children 12 months of age or older should have two doses of MMR vaccine, separated by at least 28 days.
- Teenagers and adults without evidence of immunity (protection) to mumps should have two doses of MMR vaccine, separated by at least 28 days.
I got the vaccine but still got mumps. Does this mean the vaccine doesn’t work?
MMR vaccine prevents most, but not all, cases of mumps and complications caused by the disease. People who have received two doses of the MMR vaccine are about nine times less likely to get mumps than unvaccinated people who have the same exposure to mumps virus. However, some people who receive two doses of MMR can still get mumps, especially if they have prolonged, close contact with someone who has the disease. If a vaccinated person does get mumps, they will likely have less severe illness than an unvaccinated person.
Before there was a vaccine, mumps was a common childhood disease in the United States. In some cases, the disease caused complications, such as permanent deafness in children and, occasionally, swelling of the brain (encephalitis), which in rare cases resulted in death. From year to year, the number of mumps cases can range from roughly a couple hundred to a couple thousand. In some years, there are more cases of mumps than usual because of outbreaks.
Mumps symptoms
The symptoms of mumps usually develop 12 to 24 days after a person is infected with the mumps virus (the incubation period). The average incubation period is around 17 days.
Mumps typically starts with fever, headache, muscle aches, tiredness, and loss of appetite. Then, most people will have swelling of their salivary glands. This is what causes the puffy cheeks and a tender, swollen jaw.
Swelling of the parotid glands is the most common symptom of mumps. The parotid glands are a pair of glands responsible for producing saliva. They are located on either side of your face, just below your ears.
Both parotid glands are usually affected by the swelling, although only one gland can be affected. The swelling can cause pain, tenderness and difficulty with swallowing. It then extends downward and forward as fluid builds up in the skin and soft tissue of the face and neck. Swelling usually peaks in 1 to 3 days and then subsides during the next week. The swollen tissue pushes the angle of the ear up and out. As swelling worsens, the angle of the jawbone below the ear is no longer visible. Often, the jawbone cannot be felt because of swelling of the parotid. One parotid may swell before the other, and in 25% of patients, only one side swells. Other salivary glands (submandibular and sublingual) under the floor of the mouth also may swell but do so less frequently (10%).
Other symptoms may precede parotitis by several days, including:
- a general feeling of being unwell
- high temperature
- discomfort when chewing.
- headache
- joint pain
- feeling sick
- dry mouth
- mild pain in the tummy
- feeling tired
- loss of appetite.
In about a third of cases of mumps there are no noticeable symptoms.
Fever may persist for 3 to 4 days. Parotitis, lasts at least 2 days, but may persist longer than 10 days. Mumps infection may also present only with nonspecific or primarily respiratory symptoms, or may be asymptomatic. Vaccinated cases are less likely to present severe symptoms or complications than under- or unvaccinated cases.
Mumps infection is most often confused with swelling of the lymph nodes of the neck. Lymph node swelling can be differentiated by the well-defined borders of the lymph nodes, their location behind the angle of the jawbone, and lack of the ear protrusion or obscuring of the angle of the jaw, which are characteristics of mumps. People with mumps are usually considered most infectious for several days before and after onset of parotitis.
Your child’s face will be back to normal size in about a week. It’s rare for mumps to affect boys’ testes. This happens more often in adult men with mumps. If you think your child’s testes are swollen or painful, see your doctor.
Mumps diagnosis
If your doctor suspects that you or your child has mumps, a virus culture or a blood test may be needed. Your immune system normally makes antibodies to help you fight an infection. So if you have mumps, the blood test can detect the antibodies in your system that are fighting the mumps virus.
Mumps treatment
There are currently no anti-viral medications that can be used to treat mumps. If you or your child has mumps, the only thing to do is let the infection run its course. Most children and adults recover from an uncomplicated case of mumps within about two weeks.
As a general rule, you’re no longer considered contagious and may safely return to work or school one week after a diagnosis of mumps.
Treatment is focused on relieving symptoms until your body’s immune system manages to fight off the infection.
These self-care techniques can help:
- Get plenty of bed rest until your symptoms have passed.
- Over-the-counter painkillers, such as ibuprofen or paracetamol, can relieve pain (children aged 16 or under should not be given aspirin because of the risk of Reye’s syndrome. Reye’s syndrome is a serious illness that can lead to death.)
- Drink plenty of fluids, but avoid acidic drinks such as fruit juice as these can irritate your parotid glands, water is usually the best fluid to drink
- Applying a cold compress to your swollen glands can help to reduce the pain.
- Avoid acidic foods or foods that make your mouth water, such as citrus fruits.
- Eat foods that don’t require a lot of chewing, such as soup, mashed potatoes and scrambled eggs.
- Gargle with warm salt water several times a day.
- Try popsicles to soothe your throat.
- If the testicles are swollen, support the scrotum with an athletic supporter. Ice packs may help reduce pain. Long-term problems, such as sterility (not being able to have children), are very rare.
- Try to avoid public places and close contact for at least 5 days after symptoms appear. This is the period of time during which you are the most contagious.
Usually, people who have the mumps once become immune to it for life and can’t get it again.
You should see your doctor, or take your child to the doctor, if you suspect mumps. It’s very important to see a doctor if, in addition to swollen glands, you or your child:
- Has a stomach ache and is being sick
- If male, there is evidence of swollen, tender testes
- Complains of a severe headache
- Becomes drowsy
- Starts vomiting and can’t stand bright light
- Has a rash of small purple or red spots or bruises.
If your symptoms don’t improve after seven days, or they suddenly worsen, contact your doctor for further advice.
- Mumps Outbreak Articles. https://www.cdc.gov/mumps/pubs-resources/outbreak-articles.html[↩]
- State Vaccination Requirements. https://www.cdc.gov/vaccines/imz-managers/laws/state-reqs.html[↩]
- Advisory Committee on Immunization Practices. https://www.cdc.gov/vaccines/acip/index.html[↩]
- Infectious Diseases Related to Travel. https://wwwnc.cdc.gov/travel/yellowbook/2018/infectious-diseases-related-to-travel/mumps[↩]