Contents
- What is rickets
What is rickets
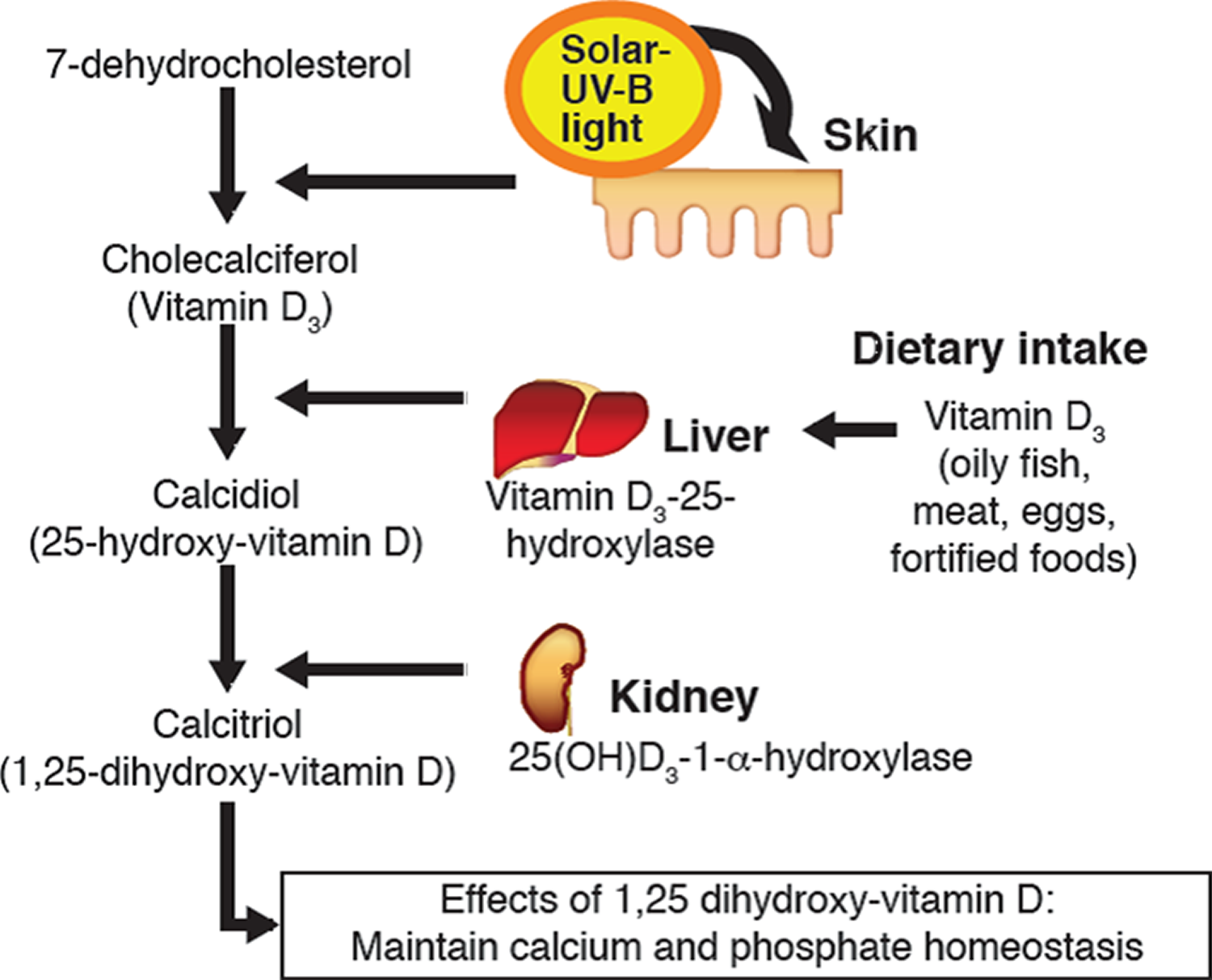
Rickets is a condition that causes children to have soft, weak bones. Rickets usually occurs when children do not get enough vitamin D, which helps growing bones absorb the minerals calcium and phosphorous. Rickets can also happen when calcium or phosphorus levels are too low. Vitamin D comes from sunlight and food. Skin produces vitamin D in response to the sun’s ultraviolet-B (UV-B) rays (see Figures 1 and 2 below). Some foods also contain vitamin D, including fortified dairy products and cereals, and some kinds of oily fish such as salmon, mackerel, herring, fresh tuna and sardines, as well as red meat and eggs 1. Vitamin D is also added to all infant formula milk, as well as some breakfast cereals, fat spreads and non-dairy milk alternatives. The amounts added to these products can vary and may only be added in small amounts. Manufacturers must by law add vitamin D to infant formula milk. Another source of vitamin D is dietary supplements. Your body can’t make vitamin D if you are sitting indoors by a sunny window because ultraviolet B (UV-B) rays (the ones your body needs to make vitamin D) can’t get through the glass.
You need vitamin D to help your body absorb calcium and phosphate from your diet (see Figures 1 and 2 below). These minerals are important for healthy bones, teeth and muscles. A lack of vitamin D – known as vitamin D deficiency – can cause your bones to become soft and weak, which can lead to bone deformities. In children, a lack of vitamin D can lead to rickets. In adults, it can lead to osteomalacia, which causes bone pain and tenderness.
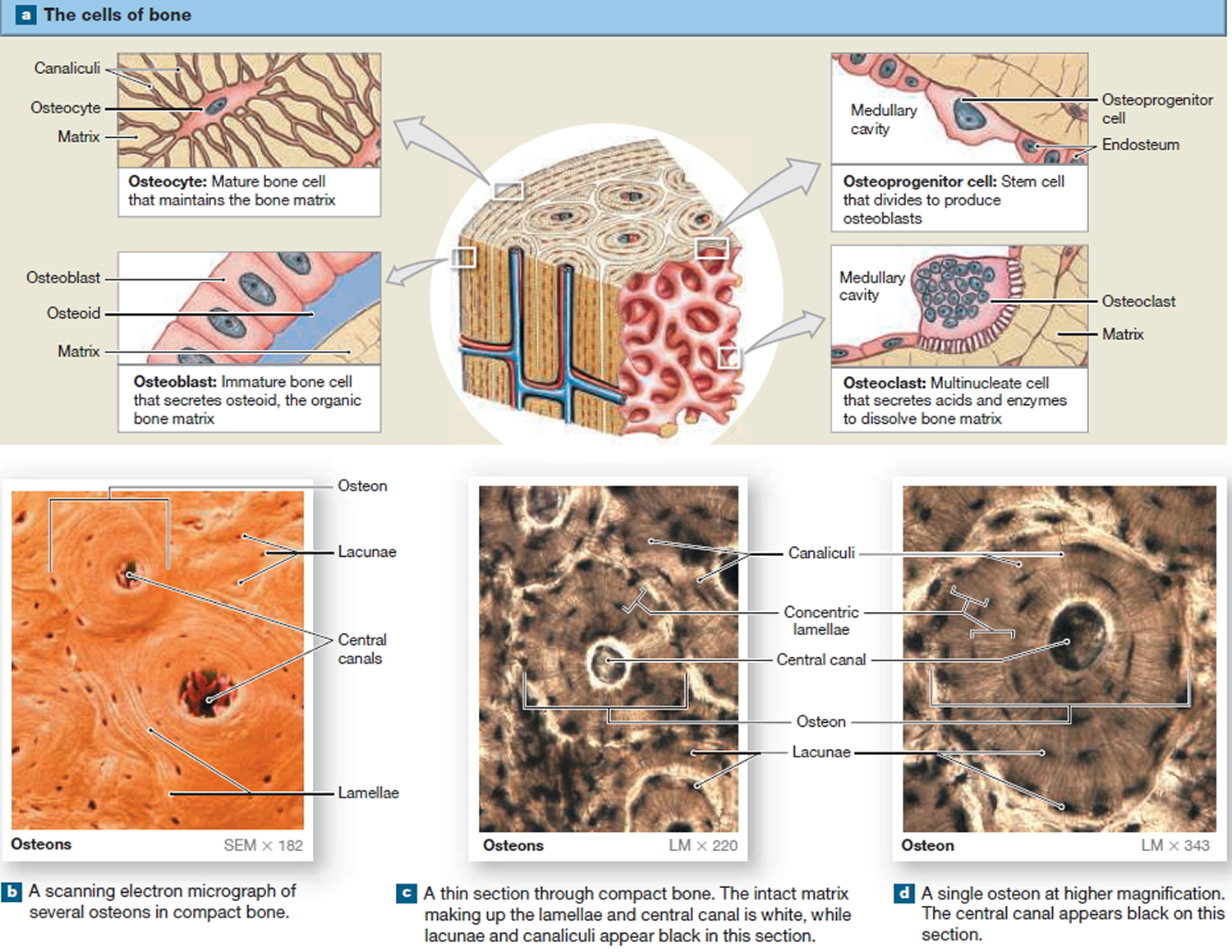
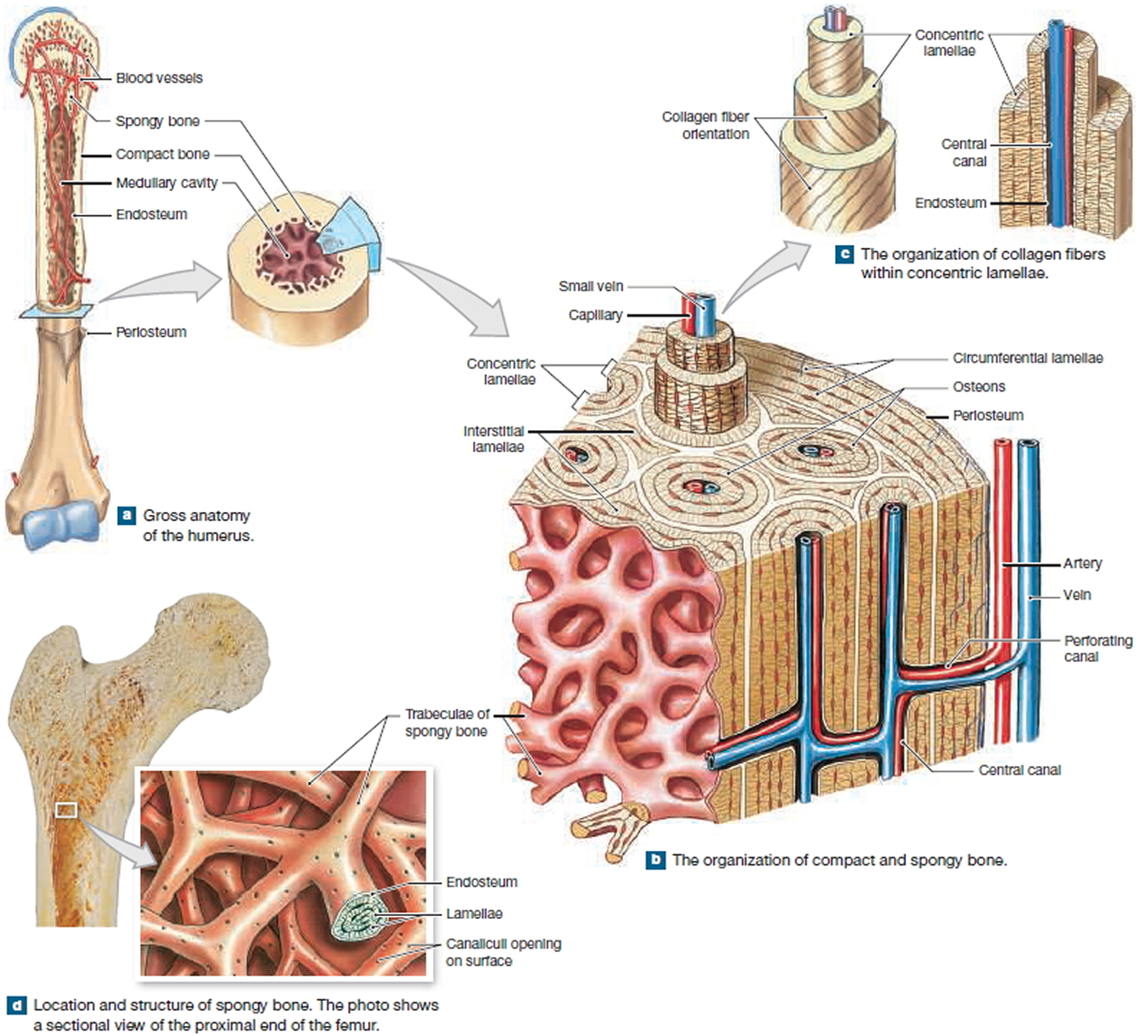
There are several types of cells constituting the bone. Osteoblasts are bone forming cells which lay down osteoid. Osteoclasts help in bone remodeling. Osteoid is subsequently mineralized by calcium salts. In rickets, the mineralization defect leads to the accumulation of osteoid in the bone tissue below the growth plate (metaphysis). This leads to weak bones and bowing over a period of time.
Figure 1. Rickets in children
Your child might not get enough vitamin D if he or she:
- Has dark skin
- Spends too little time outside
- Has on sunscreen all the time when out of doors
- Doesn’t eat foods containing vitamin D because of lactose intolerance or a strict vegetarian diet
- Is breastfed without receiving vitamin D supplements
- Can’t make or use vitamin D because of a medical disorder such as Celiac disease
In addition to dietary rickets, children can get an inherited form of the disease. Symptoms include bone pain or tenderness, impaired growth, and deformities of the bones and teeth. Your child’s doctor uses lab and imaging tests to make the diagnosis. Treatment is replacing the calcium, phosphorus, or vitamin D that are lacking in the diet. Rickets is rare in the United States.
Overt vitamin D deficiency, characterized by hypocalcemia or hypophosphatemia and rickets or osteomalacia, is now uncommon in most developed countries. However, subclinical vitamin D deficiency is associated with osteoporosis, increased risk of falls, and possibly fractures. The prevalence of vitamin D deficiency varies with the definition used (calcidiol [25(OH)D] <20 or <30 ng/mL). In the National Health and Nutrition Examination Survey (NHANES) 2000–2004, >30% of participants of age 12 years and older had calcidiol [25(OH)D] levels below 20 ng/mL 2. In India, there is high prevalence of vitamin D deficiency, with a study reporting 90% prevalence in adults and 84% prevalence in pregnant women 3. The prevalence of low vitamin D levels is increasing in the general population. Data from NHANES showed a decrease in mean calcidiol [25(OH)D] concentration from 30 to 24 ng/mL between 1988 and 2004. This may be due to assay changes, changes in milk intake, use of sun protection, and changes in body mass index (BMI) 4.
Rickets complications
Left untreated, rickets can lead to:
- Failure to grow
- Abnormally curved spine
- Skeletal deformities
- Dental defects
- Seizures
What is Vitamin D
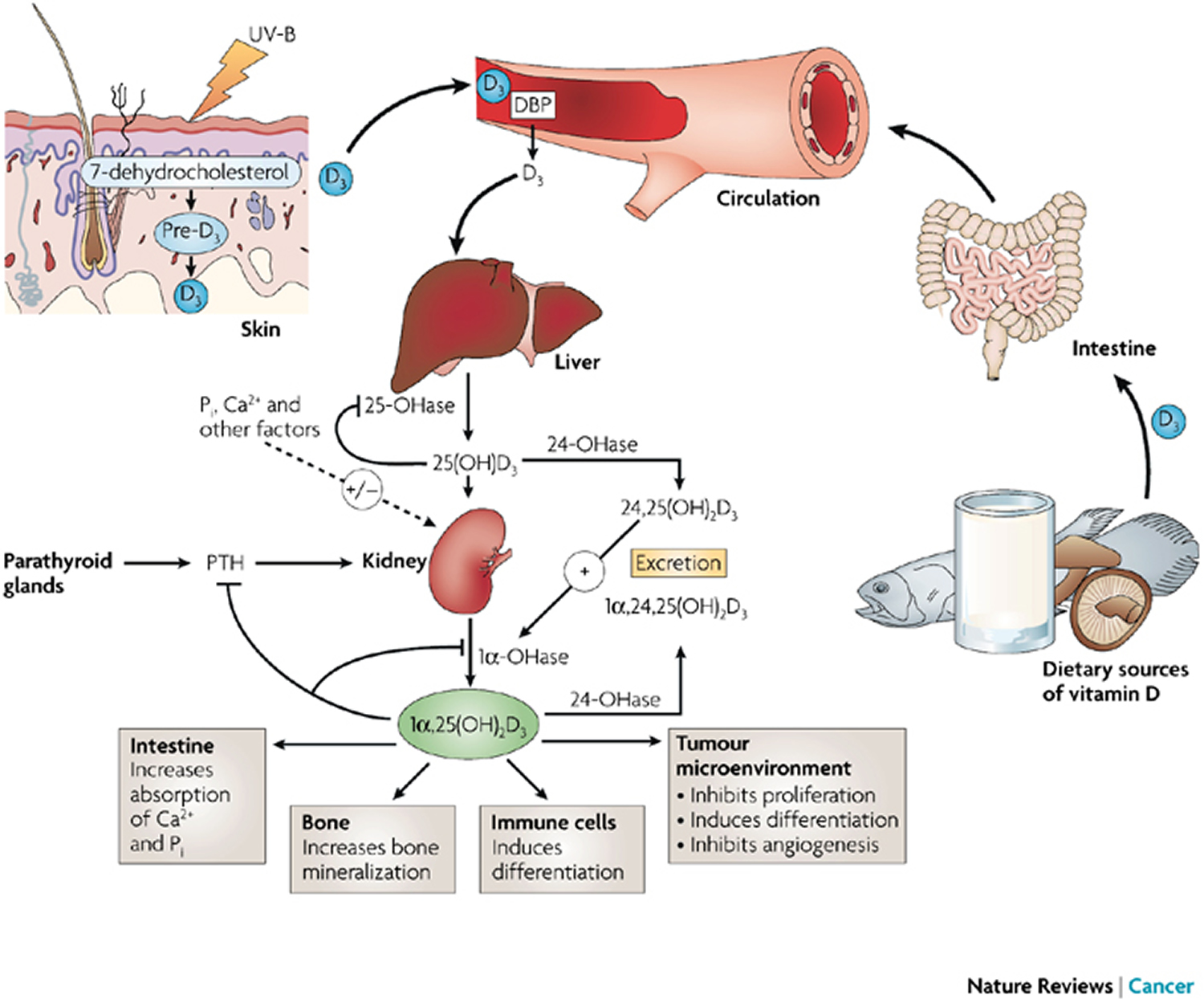
Vitamin D (calciferol) is a fat-soluble vitamin that is naturally present in very few foods, added to others, and available as a dietary supplement. Vitamin D is also produced endogenously when ultraviolet rays from sunlight strike the skin and trigger vitamin D synthesis. Vitamin D obtained from sun exposure, food, and supplements is biologically inert and must undergo two hydroxylations in the body for activation 5. The first occurs in the liver and converts vitamin D to 25-hydroxyvitamin D [25(OH)D], also known as calcidiol. The second occurs primarily in the kidney and forms the physiologically active 1,25-dihydroxyvitamin D [1,25(OH)2D], also known as calcitriol 6.
The plasma calcitriol (1,25-dihydroxyvitamin D or 1,25(OH)2D) concentration depends on the availability of calcidiol (25-hydroxyvitamin D or 25(OH)D) and the activities of the renal enzymes 1-α-hydroxylase and 24-α-hydroxylase 7. The renal 1-α-hydroxylase enzyme is primarily regulated by parathyroid hormone (PTH), serum calcium and phosphate concentrations, and fibroblast growth factor 23 (FGF23) 8. Increased parathyroid hormone (PTH), calcitonin, and hypophosphatemia (low blood phosphate) stimulate the renal enzymes 1-α-hydroxylase and enhance calcitriol [1,25(OH)2D] production, while high calcium, hyperphosphatemia (high blood phosphate) and calcitriol [1,25(OH)2D] inhibit the renal enzymes 1-α-hydroxylase 9. Calcitriol [1,25-dihydroxyvitamin D or 1,25(OH)2D] inhibits the synthesis and secretion of parathyroid hormone (PTH), providing negative feedback regulation of calcitriol production. Calcitriol [1,25-dihydroxyvitamin D or 1,25(OH)2D] synthesis may also be modulated by vitamin D receptors on the cell surface; downregulation of these receptors may play an important role in regulating vitamin D activation 10. Fibroblast growth factor 23 (FGF23), a newly described phosphaturic hormone, inhibits renal production of Calcitriol [1,25-dihydroxyvitamin D or 1,25(OH)2D] by inhibiting 1-α-hydroxylase in the renal proximal tubule and by simultaneously increasing the expression of 24-α-hydroxylase and production of 24,25(OH)2D (an inactive metabolite) 11. Calcitriol [1,25-dihydroxyvitamin D or 1,25(OH)2D] stimulates fibroblast growth factor 23 (FGF23), creating a feedback loop. Fibroblast growth factor 23 (FGF23) decreases renal reabsorption of phosphate, and thereby counteracts the increased gastrointestinal phosphate reabsorption induced by Calcitriol, maintaining phosphate homeostasis 12.
When hypocalcemia (low blood calcium) occurs, serum parathyroid hormone (PTH) concentration increases and enhances renal tubular reabsorption of calcium, as well as the activity of 1-α-hydroxylase in the kidney. This results in increased Calcitriol [1,25-dihydroxyvitamin D or 1,25(OH)2D] production, and in turn, intestinal calcium absorption. Parathyroid hormone (PTH) also stimulates bone osteoclast activity to mobilize bone calcium stores, thereby increasing serum calcium. Both Calcitriol and Calcidiol [25-hydroxyvitamin D or 25(OH)D] are degraded in part by being hydroxylated at the 24 position by a 24-hydroxylase. The activity of the 24-hydroxylase gene is increased by calcitriol (which therefore promotes its own inactivation) and reduced by parathyroid hormone (thereby allowing more active hormone to be formed) 8. Estrogen, placental growth hormone, and prolactin may also regulate vitamin D metabolism, playing a role during pregnancy to meet increased calcium demands. Calcitriol is also formed in some other tissues, but is used only within the tissues and not circulated. Parathyroid hormone (PTH)- independent extrarenal production of Calcitriol from Calcidiol is by activated macrophages in the lung and lymph nodes. The 1-α-hydroxylase enzyme is also expressed at other extrarenal sites, including the gastrointestinal tract, skin, vasculature, mammary epithelial cells, and in osteoblasts and osteoclasts 13.
Vitamin D is a nutrient found in some foods that is needed for health and to maintain strong bones. It does so by helping the body absorb calcium (one of bone’s main building blocks) from food and supplements. People who get too little vitamin D may develop soft, thin, and brittle bones, a condition known as rickets in children and osteomalacia in adults.
Vitamin D is important to the body in many other ways as well. Muscles need it to move, for example, nerves need it to carry messages between the brain and every body part, and the immune system needs vitamin D to fight off invading bacteria and viruses. Together with calcium, vitamin D also helps protect older adults from osteoporosis. Vitamin D is found in cells throughout the body.
Vitamin D promotes calcium absorption in the gut and maintains adequate serum calcium and phosphate concentrations to enable normal mineralization of bone and to prevent hypocalcemic tetany. It is also needed for bone growth and bone remodeling by osteoblasts and osteoclasts 6, 14. Without sufficient vitamin D, bones can become thin, brittle, or misshapen. Vitamin D sufficiency prevents rickets in children and osteomalacia in adults 6. Together with calcium, vitamin D also helps protect older adults from osteoporosis.
Figure 2. Vitamin D synthesis and function in your body for maintaining Calcium and Phosphate homeostasis
Figure 3. Vitamin D synthesis and function in your body including its anti-cancer effect
Figure 4. Microscopic Structure of a Typical Bone
Figure 5. Internal organization of bones
Vitamin D has other roles in the body, including modulation of cell growth, neuromuscular and immune function, and reduction of inflammation 6, 15, 16. Many genes encoding proteins that regulate cell proliferation, differentiation, and apoptosis are modulated in part by vitamin D 6. Many cells have vitamin D receptors, and some convert 25(OH)D to 1,25(OH)2D.
Serum concentration of 25(OH)D is the best indicator of vitamin D status. It reflects vitamin D produced cutaneously and that obtained from food and supplements 6 and has a fairly long circulating half-life of 15 days 17. 25(OH)D functions as a biomarker of exposure, but it is not clear to what extent 25(OH)D levels also serve as a biomarker of effect (i.e., relating to health status or outcomes) 6. Serum 25(OH)D levels do not indicate the amount of vitamin D stored in body tissues.
In contrast to 25(OH)D, circulating 1,25(OH)2D is generally not a good indicator of vitamin D status because it has a short half-life of 15 hours and serum concentrations are closely regulated by parathyroid hormone, calcium, and phosphate 17. Levels of 1,25(OH)2D do not typically decrease until vitamin D deficiency is severe 14, 18.
What happens if I take too much vitamin D?
Taking too many vitamin D supplements over a long period of time can cause too much calcium to build up in the body (hypercalcemia). This can weaken the bones and damage the kidneys and the heart.
If you choose to take vitamin D supplements, 10mcg (400 IU) a day will be enough for most people.
Don’t take more than 100mcg (4000 IU) of vitamin D a day as it could be harmful. This applies to adults, including pregnant and breastfeeding women and the elderly, and children aged 11-17 years.
Children aged 1-10 years shouldn’t have more than 50mcg (2000 IU) a day. Infants under 12 months shouldn’t have more than 25mcg (1000 IU) a day.
Some people have medical conditions that mean they may not be able to safely take as much. If in doubt, you should consult your doctor.
If your doctor has recommended you take a different amount of vitamin D, you should follow their advice.
Your body doesn’t make too much vitamin D from sun exposure, but always remember to cover up or protect your skin if you’re out in the sun for long periods to reduce the risk of skin damage and skin cancer.
Who’s at risk of rickets?
Any child who doesn’t get enough vitamin D or calcium can develop rickets, but there are certain groups of children who are more at risk.
For example, rickets is more common in children of Asian, African-Caribbean and Middle Eastern origin because their skin is darker and needs more sunlight to get enough vitamin D.
Babies born prematurely are also at risk of developing rickets because they build up stores of vitamin D while they’re in the womb. Babies who are exclusively breastfed, especially for longer than six months, may also be at risk of vitamin D deficiency.
This is why the National Institute of Health recommends that:
- pregnant and breastfeeding women should consider taking a daily supplement containing 10 micrograms (400 IU) of vitamin D
- babies from birth to one year of age, whether exclusively or partially breastfed, should be given a daily supplement containing 8.5 to 10mcg (340 to 400 IU) of vitamin D, to make sure they get enough
- babies fed infant formula do not need a vitamin D supplement until they are receiving less than 500ml (about a pint) of infant formula a day, because infant formula is fortified with vitamin D
- children aged 1 to 4 years old should be given a daily supplement containing 10mcg (400 IU) of vitamin D
Table 1 : The amount of vitamin D you need each day depends on your age. Average daily recommended amounts from the Food and Nutrition Board (a national group of experts) for different ages are listed below in International Units (IU) or microgram (mcg):
| Life Stage | Recommended Amount |
|---|---|
| Birth to 12 months | 400 IU [10 mcg] |
| Children 1–13 years | 600 IU [15 mcg] |
| Teens 14–18 years | 600 IU [15 mcg] |
| Adults 19–70 years | 600 IU [15 mcg] |
| Adults 71 years and older | 800 IU [20 mcg] |
| Pregnant and breastfeeding women | 600 IU [15 mcg] |
Note: The amount of vitamin D contained in supplements is sometimes expressed in international units (IU) where 40 IU is equal to one microgram (1 mcg) of vitamin D.
Table 2: Selected Food Sources of Vitamin D
| Food | IUs per serving* | Percent DV** |
|---|---|---|
| Cod liver oil, 1 tablespoon | 1,360 | 340 |
| Swordfish, cooked, 3 ounces | 566 | 142 |
| Salmon (sockeye), cooked, 3 ounces | 447 | 112 |
| Tuna fish, canned in water, drained, 3 ounces | 154 | 39 |
| Orange juice fortified with vitamin D, 1 cup (check product labels, as amount of added vitamin D varies) | 137 | 34 |
| Milk, nonfat, reduced fat, and whole, vitamin D-fortified, 1 cup | 115-124 | 29-31 |
| Yogurt, fortified with 20% of the DV for vitamin D, 6 ounces (more heavily fortified yogurts provide more of the DV) | 80 | 20 |
| Margarine, fortified, 1 tablespoon | 60 | 15 |
| Sardines, canned in oil, drained, 2 sardines | 46 | 12 |
| Liver, beef, cooked, 3 ounces | 42 | 11 |
| Egg, 1 large (vitamin D is found in yolk) | 41 | 10 |
| Ready-to-eat cereal, fortified with 10% of the DV for vitamin D, 0.75-1 cup (more heavily fortified cereals might provide more of the DV) | 40 | 10 |
| Cheese, Swiss, 1 ounce | 6 | 2 |
* IUs = International Units.
** DV = Daily Value. DVs were developed by the U.S. Food and Drug Administration to help consumers compare the nutrient contents among products within the context of a total daily diet. The DV for vitamin D is currently set at 400 IU for adults and children age 4 and older. Food labels, however, are not required to list vitamin D content unless a food has been fortified with this nutrient. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
Note: The amount of vitamin D contained in supplements is sometimes expressed in international units (IU) where 40 IU is equal to one microgram (1 mcg) of vitamin D.
[Source 19]How long should you spend in the sun?
Most people can make enough vitamin D from being out in the sun daily for short periods with their forearms, hands or lower legs uncovered and without sunscreen from late March or early April to the end of September, especially from 11am to 3pm.
It’s not known exactly how much time is needed in the sun to make enough vitamin D to meet your body’s requirements. This is because there are a number of factors that can affect how vitamin D is made, such as your skin color or how much skin you have exposed. But you should be careful not to burn in the sun, so take care to cover up, or protect your skin with sunscreen, before your skin starts to turn red or burn.
Your risk of sunburn depends on 2 things. How sun-sensitive your skin is, and how strong the UV rays are you’re exposed to. Different people will have a different risk of sunburn on the same day, so it’s a good idea to know when your risk is high, so you can protect your skin.
In general people who have one or more of the following are at more risk:
- skin that burns easily
- light or fair colored skin, hair, or eyes
- lots of moles or freckles
- a history of sunburn
- a personal or family history of skin cancer
People with dark skin, such as those of African, African-Caribbean or south Asian origin, will need to spend longer in the sun to produce the same amount of vitamin D as someone with lighter skin.
- Children aged under six months should be kept out of direct strong sunlight. To ensure they get enough vitamin D, babies and children aged under five years should be given vitamin D supplements even if they do get out in the sun.
How long it takes for your skin to go red or burn varies from person to person. You’re the best person to know how your skin reacts in the sun. The more easily you get sunburnt, the more careful you need to be. Remember, you don’t need to peel – if your skin’s gone red or pink in the sun, that’s sunburn, and it’s dangerous. For people with darker skin it may feel irritated, tender or itchy. The longer you stay in the sun, especially for prolonged periods without sun protection, the greater your risk of skin cancer. Using sunbeds is not a recommended way of making vitamin D.
Other things that affect the strength of UV rays are the:
- Time of year – the highest risk months in the US are April to September. Near the equator, there are strong UV rays all year round.
- Altitude – UV rays are stronger the higher you go. So skiers and mountaineers can easily get caught out.
- Cloud cover – over 90% of UV can pass through light cloud.
- Reflection – up to 80% of UV rays are reflected back from snow, 15% from sand, 10% from concrete and up to 30% from water (depending on how choppy it is).
Rickets disease
Normal bone growth and mineralization depends on the availability of adequate calcium and phosphate. Deficient mineralization can result in rickets and/or osteomalacia. In rickets, there is deficient mineralization at the growth plate, whereas osteomalacia refers to impaired mineralization of the bone matrix. Rickets and osteomalacia usually occur together as long as the growth plates are open as in children; only osteomalacia occurs after the growth plates have fused as seen in adults 20.
The mineralization defects can be classified as calcipenic (hypocalcemic) rickets caused by calcium deficiency and phosphopenic (hypophosphatemic) rickets caused by phosphate deficiency 21. Vitamin D is a prohormone that is essential for normal absorption of calcium from the gut, and deficiency of vitamin D is usually more common than either isolated calcium or phosphorus deficiency and is the commonest cause of rickets/osteomalacia.
Vitamin D dependent rickets type I
Vitamin D dependent rickets type I is also known as pseudovitamin D-deficient rickets and was identified in 1961. Vitamin D dependent rickets type I is an autosomal recessive disorder. Patients with vitamin D dependent rickets type I have inactivating mutations in the CYP27B1 gene, located on 12 q13.3, which encodes the enzyme [25- (OH) D 1-α-hydroxylase or 1-α-hydroxylase], leading to 1-α-hydroxylase deficiency 22. As a result, calcidiol [25(OH)D] is not hydroxylated to calcitriol [1,25(OH)2D] and calcium is not absorbed normally. Vitamin D dependent rickets type Iis characterized by early onset of skeletal disease (within the first year of life), severe hypocalcemia (sometimes with tetany), and moderate hypophosphatemia. Patients exhibit enamel hypoplasia, muscle weakness, hypotonia, motor retardation, and stunted growth. With progression, patients develop the classic radiographic signs of vitamin D deficiency rickets and bone biopsy evidence of osteomalacia. Biochemical evaluation shows hypocalcemia, increased PTH, and increase in urinary excretion of amino acids and phosphate. The characteristic biochemical findings of vitamin D dependent rickets type I are normal serum levels of calcidiol and low levels of calcitriol. The clinical and biochemical evidence of rickets can be corrected with calcitriol [1,25(OH)2D] treatment. The dose depends upon the severity of disease and body weight. The initial dose for florid rickets is 1 mcg/day. Treatment is continued at this dose until bones are healed. Thereafter, the maintenance dose varies between 0.25 and 1 mcg/day, depending on the results of biochemical analyses. The aims of the treatment are to achieve normocalcemia, to maintain PTH levels within normal limits, and to avoid hypercalciuria.
Vitamin D dependent rickets type II
Vitamin D dependent rickets type II is also known as hereditary vitamin D resistant rickets. Hereditary vitamin D resistant rickets is a very rare autosomal recessive form of rickets, with fewer than 50 known affected kindreds. It is associated with end-organ resistance to calcitriol, usually caused by mutations in the gene encoding the vitamin D receptor. The defect in the receptor interferes with the function of the hormone–receptor complex, thereby preventing calcitriol action 23. The identified mutations or defects in the vitamin D receptor include: (a) failure of calcitriol [1,25(OH)2D] binding to available receptors, (b) reduction in calcitriol [1,25(OH)2D] receptor binding sites, (c) abnormal binding affinity of calcitriol [1,25(OH)2D] to receptor, (d) inadequate translocation of calcitriol [1,25(OH)2D]–receptor complex to the nucleus, and (e) diminished affinity of the calcitriol [1,25(OH)2D]–receptor complex for the dNA-binding domain, secondary to changes in the structure of receptor zinc-binding fingers.
The clinical spectrum of hereditary vitamin D resistant rickets varies with the type of mutation within the vitamin D receptor and residual vitamin D receptor activity. Affected children usually appear normal at birth, but develop rickets within the first 2 years of life. A unique feature of the syndrome is alopecia, which is seen in approximately two-thirds of cases and is a marker of disease severity. Alopecia results from the lack of vitamin D receptor action within keratinocytes. Additional ectodermal anomalies may also be seen, including multiple milia, epidermal cysts, and oligodontia. The treatment of hereditary vitamin D resistant rickets involves a therapeutic trial of calcitriol and calcium supplementation. The individual response varies with the severity of the receptor defect. Therapy is started at daily doses of 2 mcg of calcitriol and 1000 mg of calcium. However, administration of extremely high doses of calcitriol (up to 30–60 mcg/day) and calcium (up to 3 g/day) may be necessary. Long-term infusion of calcium into a central vein is an alternative for resistant patients and needs to be continued for many months. Oral calcium therapy may be sufficient once radiographic healing has been observed. During treatment, patients should initially be evaluated at least once per week. Serum calcium, phosphorus, ALP, creatinine, calcitriol, PTH concentrations, and the urinary calcium/creatinine ratio should be measured. If the biochemical parameters do not respond, the dose of calcitriol should be gradually increased to reach serum concentrations of up to 100 times the normal mean. Failure of therapy should be considered if no biochemical response occurs after 3–5 months of treatment.
Rickets in adults
Osteomalacia is the adult counterpart of rickets in children. Both of these conditions are caused by a defect in vitamin D availability or metabolism. Osteomalacia is characterised by poor bone formation, resulting in weakened bone. The incidence of osteomalacia is approximately 1 in 1000 people.
In adults, the vitamin D deficiency results in abnormal bone formation, which is weaker than healthy bone. There is increased risk of fractures, which tend to affect the vertebral bodies in the spine and the neck of femur. If osteomalacia persists, it may result in lower density bone and subsequently osteoporosis.
When osteomalacia is in its early stages, you might not have any symptoms, although signs of osteomalacia may be apparent on an X-ray or other diagnostic tests. As osteomalacia progresses, you might develop bone pain and muscle weakness.
The dull, aching pain associated with osteomalacia most commonly affects the lower back, pelvis, hips, legs and ribs. The pain might be worse at night, or when you put pressure on the bones, and are rarely relieved completely by rest.
Decreased muscle tone and leg weakness can cause a waddling gait and make walking slower and more difficult.
Complications of Osteomalacia
If you have osteomalacia, you’re more likely to break bones, particularly those in your ribs, spine and legs.
Causes of Osteomalacia
Osteomalacia results from a defect in the bone-maturing process. Your body uses the minerals calcium and phosphate to help build strong bones. You might develop osteomalacia if you don’t get enough of these minerals in your diet or if your body doesn’t absorb them properly. These problems can be caused by:
- Vitamin D deficiency. Sunlight produces vitamin D in your skin. People who live in areas where sunlight hours are short or eat a diet low in vitamin D can develop osteomalacia. Vitamin D deficiency is the most common cause of osteomalacia worldwide.
- Certain surgeries. Normally, the stomach breaks down food to release vitamin D and other minerals that are absorbed in the intestine. This process is disrupted if you have surgery to remove part or all of your stomach, and can result in vitamin D and calcium deficiency. Surgery to remove or bypass your small intestine also can lead to vitamin D and calcium deficiency.
- Celiac disease. In this autoimmune disorder, consuming foods containing gluten, a protein found in wheat, barley and rye, can damage the lining of your small intestine. A damaged intestinal lining doesn’t absorb nutrients well, and can lead to vitamin D and calcium deficiency.
- Kidney or liver disorders. These organs are involved in activating vitamin D in your body. Problems with your kidneys or liver can interfere with your body’s ability to make active vitamin D.
- Drugs. Some drugs used to treat seizures, including phenytoin (Dilantin, Phenytek) and phenobarbital, can cause severe vitamin D deficiency and osteomalacia.
Risk Factors for Osteomalacia
Risk of osteomalacia is increased by:
- Inadequate dietary intake of vitamin D, for instance due to lactose intolerance
- Inadequate exposure to sunlight (ultraviolet radiation), which produces vitamin D in the body (increased risk in elderly people who are housebound)
- Malabsorption of vitamin D by the intestines
- Inherited or acquired disorders of vitamin D metabolism
- Advanced renal disease
- Phosphate depletion associated with low dietary intake of phosphates
- Certain medications such as those used to treat epilepsy
Osteomalacia prevention
Osteomalacia caused by inadequate sun exposure or a diet low in vitamin D often can be prevented by getting enough vitamin D.
- Eat foods high in vitamin D. Foods naturally rich in vitamin D include oily fish (salmon, mackerel, sardines) and egg yolks. Also look for foods fortified with vitamin D, such as cereal, bread, milk and yogurt.
- Take supplements, if needed. If you don’t get enough vitamins and minerals in your diet or if you have a medical condition affecting the ability of your digestive system to absorb nutrients properly, ask your doctor about taking vitamin D and calcium supplements.
Unprotected sun exposure can increase your risk of skin cancer. There’s no consensus among experts about what amount of sun exposure is safe and enough to prevent or treat osteomalacia.
Osteomalacia diagnosis
Osteomalacia can be difficult to diagnose. To pinpoint the cause and to rule out other bone disorders, such as osteoporosis, you might undergo one or more of the following tests:
- Blood and urine tests. These help detect low levels of vitamin D and problems with calcium and phosphorus.
- X-rays. Slight cracks in your bones that are visible on X-rays are characteristic of osteomalacia.
- Bone biopsy. Using general anesthesia, a surgeon inserts a slender needle through your skin and into your pelvic bone above the hip to withdraw a small sample of bone. Although a bone biopsy is accurate in detecting osteomalacia, it’s rarely needed to make the diagnosis.
Prognosis of Osteomalacia
Prognosis is good if underlying causes of vitamin D deficiency are addressed. Patients should be encouraged to eat a balanced diet and ensure adequate sun exposure.
How is Osteomalacia Treated?
Treatment should be aimed at correcting any underlying cause where possible. Osteomalacia due to poor intake is reversed by ensuring adequate diet, sunlight exposure and vitamin D and calcium supplements if necessary (see Treatment below).
Rickets causes
What causes rickets
Rickets usually occurs because of a lack of vitamin D or calcium, although it can also be caused by a genetic defect or another health condition.
Lack of vitamin D and Calcium
The most common cause of rickets is a lack of vitamin D or calcium in a child’s diet. Both are essential for children to develop strong and healthy bones.
Vitamin D is essential for skeletal health. Vitamin D promotes differentiation of enterocytes and the intestinal absorption of calcium and phosphorus. This helps in bone mineralization. In conditions of hypocalcemia or hypophosphatemia, vitamin D stimulates bone resorption, thereby maintaining serum levels of calcium and phosphorus. vitamin D deficiency or resistance thus causes hypocalcemia and hypophosphatemia. Hypocalcemia stimulates the release of parathyroid hormone (PTH), which, through its actions on bone and kidney, partially corrects the hypocalcemia but enhances urinary phosphate excretion, leading to hypophosphatemia and osteomalacia. Calcidiol [25(OH)D] also plays an important role in extraskeletal health. vitamin D deficiency may be associated with certain immunological conditions such as multiple sclerosis, type 1 diabetes, rheumatoid arthritis, inflammatory bowel disease, mood disorders, and cancers such as breast, prostate, and colon cancer 24. In adolescents, low serum vitamin D levels are associated with increased risk of hypertension, hyperglycemia, metabolic syndrome, and higher risk of upper respiratory infections 24.
Sources of vitamin D are:
- sunlight – your skin produces vitamin D when it’s exposed to the sun, and we get most of our vitamin D this way
- food – vitamin D is also found in some foods, such as oily fish, eggs and fortified breakfast cereals
- dietary supplements
Calcium is commonly found in dairy products, such as milk, cheese and yogurt, and green vegetables, such as broccoli and cabbage.
Over time, a vitamin D or calcium deficiency will cause rickets in children and soft bones (osteomalacia) in adults.
Causes of vitamin D deficiency
Reduced cutaneous synthesis
Vitamin D deficiency can occur in people who live without sun exposure.
Sun exposure
Dietary vitamin D deficiency can also occur in children, with differences among ethnic groups depending on skin pigmentation and varied ingestion of supplements 25. A Caucasian infant’s vitamin D requirements are met by exposure to sunlight for 30 minutes per week, clothed only in a diaper, or for 2 hours per week fully clothed with no hat. Asians require approximately threefold longer periods of sunlight exposure because of the protective pigmentation in their skin and Africans need six times the same exposure 26. Current American Academy of Pediatrics recommendations include keeping infants <6 months old out of direct sunlight, selecting children’s activities that minimize sunlight exposure, and using protective clothing and sunscreen. These recommendations are acceptable for light-skinned children in lower latitudes, particularly in the summer months. However, the effects of UV-B exposure on dark-skinned children who live in higher latitudes need to be explored. Above 37° north latitude, in the winter months, the number of UV-B photons reaching the earth’s atmosphere is decreased by 80–100%, and as a consequence, little cholecalciferol (vitamin D3) is produced in the skin. Cholecalciferol (vitamin D3) is formed by the action of ultraviolet-B (UV-B) radiation (wavelength 290–315 nm) on skin, which converts 7-dehydrocholesterol in epidermal keratinocytes and dermal fibroblasts to pre-vitamin D, which subsequently isomerizes to vitamin D3 in a nonenzymatic manner 27. This is the form of vitamin D found in animal products (fortified milk, fatty fish, cod-liver oil, eggs) and some vitamin D supplements. Sunscreen absorbs UV-B and some UV-A light and prevents it from reaching and entering the skin. A sunscreen with a sun protection factor (SPF) of 8 can decrease vitamin D3 (cholecalciferol) synthetic capacity by 95%, and SPF 15 can decrease it by 98%. For adequate vitamin D synthesis, exposure to the midday sun (between 1000 and 1500 hours) for 10–15 minutes in the spring, summer, and fall is considered sufficient for light-skinned people. After this extent of exposure, application of a sunscreen with an SPF of 15 is recommended to prevent the damaging effects of chronic excessive exposure to sunlight. Whole body clothing as noted in some cultures prevents adequate sun exposure, i.e. purdah system in Muslim community. Cloud cover, increasing water vapor, and industrial pollution can reduce the amount of UV-B that reaches the earth’s surface, and industrial pollution has been associated with a greater prevalence of vitamin D deficiency rickets. This is because after prolonged UV-B radiation exposure, the vitamin D made in the skin is further degraded to the inactive vitamin D metabolites, tachysterol and lumisterol.
Cold climates
Vitamin D deficiency is also common at the end of the winter due to less sun exposure 28. Vitamin D deficiency has been reported in dark-skinned immigrants from warm climates to cold climates. Asian Indian immigrants to the United States may have vitamin D deficiency, even with adequate sun exposure 29.
Extensive burns
In patients with a history of extensive burn injuries, vitamin D synthesis in skin is below normal, even with sun exposure 30.
Nutritional deficiency
Vitamin D deficiency can occur even with adequate sun exposure 31. It can occur in people who consume foods that are not fortified with vitamin D or if there is intestinal malabsorption of vitamin D. There are few foods that naturally contain vitamin D and because most of these are meat or fish based, they may not be acceptable to cultures that favor a vegetarian diet. Currently, few foods are fortified with vitamin D. Routine vitamin D fortification should be considered for milk and other food products.
Elderly people
Cutaneous vitamin D production and vitamin D stores decline with age. vitamin D intake is often low in older subjects. Achlorhydria, which is common in the elderly, limits calcium absorption. Older persons, in addition, may also be confined indoors 32.
Maternal vitamin D deficiency
Vitamin D is transferred from the mother to the fetus across the placenta, and reduced vitamin D stores in the mother are associated with lower vitamin D levels in the infant 33. Low vitamin D levels during pregnancy have been associated with intrauterine growth retardation, premature labor, and hypertension, all of which increase the risk of low birth weight.
Prematurity
Vitamin D levels are low in premature infants, who have less time to accumulate vitamin D from the mother through transplacental transfer. The third trimester is a critical time for vitamin D transfer because this is when the fetal skeleton becomes calcified, requiring increased activation of calcidiol [25(OH)D] to calcitriol [1,25(OH)2D] in the maternal kidneys and placenta. Vitamin D deficiency in the mother during this period can cause fetal vitamin D deficiency, and in severe cases, fetal rickets 34. The premature infants are more likely to have enamel defects in both primary and permanent teeth because vitamin D sufficiency is necessary for normal fetal tooth development.
Exclusive breast feeding
The vitamin D content of breast milk is low (15–50 IU/L) even in a vitamin D replete mother 35. Exclusively breastfed infants consuming an average of 750 mL of breast milk daily thus ingest only 10–40 IU/day of vitamin D. Most breastfed infants need to be exposed to sunlight for at least 30 minutes/ week while wearing only a diaper in order to maintain calcidiol [25(OH)D] levels at >20 ng/mL. Vitamin D deficiency is uncommon in formula-fed infants because of the fortification of infant formulas (400 IU/L). However, it can still occur if the infant had low vitamin D stores at birth because of maternal vitamin D deficiency and if the vitamin D content of the formula is insufficient 36.
Obesity
Calcidiol [25(OH)D] levels are low in obese individuals as vitamin D is sequestrated in fat. vitamin D requirements are thus higher in obese individuals 37.
Hospitalized patients
Inadequate intake and lack of sun exposure cause vitamin D deficiency in this group of patients 38.
Women treated for osteoporosis
Subclinical vitamin D deficiency is common in postmenopausal women on therapy for osteoporosis (bisphosphonates, raloxifene, calcitonin, or PTH) 39.
Renal diseases
Chronic renal disease
In patients with chronic kidney disease, calcitriol [1,25(OH)2D] production is low due to diminished glomerular filtration, loss of the 1-α-hydroxylase enzyme secondary to structural renal damage, and suppression of enzyme activity secondary to hyperphosphatemia. This results in hypocalcemia, hyperparathyroidism, and bone disease 40. In addition to the deficiency of calcitriol [1,25(OH)2D], recent studies have shown co-existence of calcidiol [25(OH)D] deficiency in pre-dialysis and dialysis patients, especially in female diabetics and patients on peritoneal dialysis 41. Whether improving calcidiol [25(OH)D] concentrations benefits these patients is controversial, but Kidney Dialysis Outcome Initiative guidelines have recommended supplementation.
Nephrotic syndrome
Most of the calcidiol in serum is bound to vitamin D binding protein. Patients with nephrotic syndrome lose vitamin D binding protein and may develop vitamin D deficiency 42.
Distal renal tubular acidosis
Hypocalcemia can occur in distal renal tubular acidosis, along with acidosis, which causes rickets. The presence of distal renal tubular acidosis is suspected in conditions of hypokalemia, hyperchloremia, and nomal anion gap metabolic acidosis 43.
Gastrointestinal disease
Malabsorption associated with diseases of the small intestine, hepatobiliary tree with cholestatic liver disease, extrahepatic biliary obstruction, and diseases of pancreas may result in decreased absorption of vitamin D and/or depletion of endogenous calcidiol [25(OH)D] stores due to abnormal enterohepatic circulation. Malabsorption of vitamin D occurs as a consequence of steatorrhea, which disturbs fat emulsification and chylomicron-mediated absorption. Patients may have rickets or osteomalacia or only low bone density. Common examples are celiac disease, inflammatory bowel disease, food allergies, cholestasis, and exocrine pancreatic insufficiency (as in cystic fibrosis) 44.
Gastric bypass
Patients with short-limb bypass have secondary hyperparathyroidism in spite of normal calcidiol [25(OH)D] concentrations, due to calcium malabsorption. vitamin D deficiency also occurs in patients with partial or total gastrectomy for peptic ulcer disease or bariatric surgery due to the loss of gastrointestinal acidity, malfunction of the proximal small bowel which leads to vitamin D malabsorption, absence of adequate absorbing surface, or failure of intestinal mucosal cells to respond to vitamin D 45.
Liver disease
Vitamin D is hydroxylated in the liver to produce calcidiol [25(OH)D]. Hence, patients with significant parenchymal or obstructive liver disease have reduced calcidiol [25(OH)D]. These patients manifest biochemical or histological evidence of osteomalacia only in the presence of concomitant nutritional deficiency or interruption of the enterohepatic circulation 45.
Medications
Certain anticonvulsants and antiretroviral drugs used to treat HIV infection can precipitate vitamin D deficiency by enhancing catabolism of calcidiol [25(OH)D] and calcitriol [1,25(OH)2D] 46 decreased circulating levels of calcidiol occur in patients on phenytoin, phenobarbitone, carbamazepine, isoniazid, rifampicin, and theophylline due to induction of P-450 enzyme activity, which metabolizes calcidiol to inactive vitamin D metabolites. Tenofovir can cause rickets. Abnormalities in calcium concentration are seen with medications used in the treatment of the complications of HIV, such as foscarnet, pentamidine, and recombinant growth hormone. vitamin D requirements are higher in patients on glucocorticoids because they inhibit intestinal vitamin D dependent calcium absorption. Ketoconazole and some other antifungal agents increase vitamin D requirements because they block 1-hydroxylation. Supplementation with vitamin D (400–4000 IU/day) may be needed for these patients 47.
Calcipenic rickets
Calcipenic (hypocalcemic) rickets is characterized by deficiency of calcium or more commonly vitamin D. The calcium requirements and content of common foodstuffs is given in Tables 3 and 4. The amount of calcium you need each day depends on your age. Rickets can occur despite adequate vitamin D levels if the calcium intake is very low. This problem generally does not occur unless calcium intake is very low because vitamin D increases intestinal calcium absorption. Most children with calcium deficiency rickets have normal serum 25-hydroxyVitamin D [calcidiol] and high serum 1,25-dihydroxyVitamin D [calcitriol] concentrations, indicating adequate intake of vitamin D. These children may have an increased vitamin D requirement when measured by their response to vitamin D replacement. Thus, vitamin D requirements may be higher than expected in children who are calcium deficient 48. In addition to this, low dietary calcium intake even without coexisting vitamin D deficiency increases serum 1,25(OH)2D concentrations, which in turn decrease the half-life of 25(OH)D, probably by increasing the catabolism of 25(OH)D. In the majority of South Asian children with rickets, 25(OH)D concentrations are also in the vitamin D deficient range 49.
Table 3: Average calcium daily recommended amounts are listed below in milligrams (mg):
| Life Stage | Recommended Dietary Allowances (RDAs) for Calcium Amount |
|---|---|
| Birth to 6 months | 200 mg |
| Infants 7–12 months | 260 mg |
| Children 1–3 years | 700 mg |
| Children 4–8 years | 1,000 mg |
| Children 9–13 years | 1,300 mg |
| Teens 14–18 years | 1,300 mg |
| Adults 19–50 years | 1,000 mg |
| Adult men 51–70 years | 1,000 mg |
| Adult women 51–70 years | 1,200 mg |
| Adults 71 years and older | 1,200 mg |
| Pregnant and breastfeeding teens | 1,300 mg |
| Pregnant and breastfeeding adults | 1,000 mg |
Many people don’t get recommended amounts of calcium from the foods they eat. When total intakes from both food and supplements are considered, many people—particularly adolescent girls—still fall short of getting enough calcium, while some older women likely get more than the upper limit.
People should get most of their nutrients from food, advises the federal government’s Dietary Guidelines for Americans. Foods contain vitamins, minerals, dietary fiber and other substances that benefit health. In some cases, fortified foods and dietary supplements may provide nutrients that otherwise may be consumed in less-than-recommended amounts. For more information about building a healthy diet, refer to the Dietary Guidelines for Americans 50 and the U.S. Department of Agriculture’s MyPlate 51.
Table 4: Selected Food Sources of Calcium
| Food | Milligrams (mg) per serving | Percent DV* |
|---|---|---|
| Yogurt, plain, low fat, 8 ounces | 415 | 42 |
| Mozzarella, part skim, 1.5 ounces | 333 | 33 |
| Sardines, canned in oil, with bones, 3 ounces | 325 | 33 |
| Yogurt, fruit, low fat, 8 ounces | 313–384 | 31–38 |
| Cheddar cheese, 1.5 ounces | 307 | 31 |
| Milk, nonfat, 8 ounces** | 299 | 30 |
| Soymilk, calcium-fortified, 8 ounces | 299 | 30 |
| Milk, reduced-fat (2% milk fat), 8 ounces | 293 | 29 |
| Milk, buttermilk, lowfat, 8 ounces | 284 | 28 |
| Milk, whole (3.25% milk fat), 8 ounces | 276 | 28 |
| Orange juice, calcium-fortified, 6 ounces | 261 | 26 |
| Tofu, firm, made with calcium sulfate, ½ cup*** | 253 | 25 |
| Salmon, pink, canned, solids with bone, 3 ounces | 181 | 18 |
| Cottage cheese, 1% milk fat, 1 cup | 138 | 14 |
| Tofu, soft, made with calcium sulfate, ½ cup*** | 138 | 14 |
| Ready-to-eat cereal, calcium-fortified, 1 cup | 100–1,000 | 10–100 |
| Frozen yogurt, vanilla, soft serve, ½ cup | 103 | 10 |
| Turnip greens, fresh, boiled, ½ cup | 99 | 10 |
| Kale, fresh, cooked, 1 cup | 94 | 9 |
| Ice cream, vanilla, ½ cup | 84 | 8 |
| Chinese cabbage, bok choi, raw, shredded, 1 cup | 74 | 7 |
| Bread, white, 1 slice | 73 | 7 |
| Pudding, chocolate, ready to eat, refrigerated, 4 ounces | 55 | 6 |
| Tortilla, corn, ready-to-bake/fry, one 6” diameter | 46 | 5 |
| Tortilla, flour, ready-to-bake/fry, one 6” diameter | 32 | 3 |
| Sour cream, reduced fat, cultured, 2 tablespoons | 31 | 3 |
| Bread, whole-wheat, 1 slice | 30 | 3 |
| Kale, raw, chopped, 1 cup | 24 | 2 |
| Broccoli, raw, ½ cup | 21 | 2 |
| Cheese, cream, regular, 1 tablespoon | 14 | 1 |
* DV = Daily Value. DVs were developed by the U.S. Food and Drug Administration to help consumers compare the nutrient contents among products within the context of a total daily diet. The DV for calcium is 1,000 mg for adults and children aged 4 years and older. Foods providing 20% of more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
[Source 52]In its food guidance system, MyPlate, the U.S. Department of Agriculture recommends that persons aged 9 years and older eat 3 cups of foods from the milk group per day 53. A cup is equal to 1 cup (8 ounces) of milk, 1 cup of yogurt, 1.5 ounces of natural cheese (such as Cheddar), or 2 ounces of processed cheese (such as American).
Genetic defect
Rare forms of rickets can also occur in some inherited (genetic) disorders. For example, hypophosphatemic rickets is a genetic disorder where the kidneys and bones deal abnormally with phosphate.
Phosphate binds to calcium and is what makes bones and teeth hard. This leaves too little phosphate in the blood and bones, leading to weak and soft bones.
Other types of genetic rickets affect certain proteins in the body that are used by vitamin D.
Phosphopenic rickets
Phosphopenic rickets is commonly caused by renal phosphate wasting. This may be isolated or part of a generalized renal tubular disorder such as Fanconi syndrome or Dent disease 54. Isolated phosphate loss is seen in X-linked hypophosphatemic rickets (XLH), autosomal dominant hypophosphatemic rickets, tumor-induced osteomalacia, and hypophosphatemic rickets with hypercalciuria (autosomal recessive) disease. Nutritional deficiency is uncommon. These causes can be distinguished by measuring urinary amino acids, bicarbonate, glucose, calcium, and vitamin D concentrations 55.
Another way to classify rickets is as nutritional and non-nutritional. Of the 126 children with non-nutritional (refractory) rickets, 64.3% had distal renal tubular acidosis, 20.6% had renal failure,7.1% had proximal renal tubular acidosis, while 6.4% had hypophosphatemic rickets and 1.6% had vitamin D dependent rickets 55.
Underlying conditions
Occasionally, rickets develops in children with rare forms of kidney, liver and intestinal conditions. These can affect the absorption of vitamins and minerals.
Risk factors for rickets
Factors that can increase a child’s risk of rickets include:
- Dark skin. Dark skin doesn’t react as strongly to sunshine as does lighter skin, so it produces less vitamin D.
- Mother’s vitamin D deficiency during pregnancy. A baby born to a mother with severe vitamin D deficiency can be born with signs of rickets or develop them within a few months after birth.
- Northern latitudes. Children who live in geographical locations where there is less sunshine are at higher risk of rickets.
- Premature birth. Babies born before their due dates are more likely to develop rickets.
- Medications. Certain types of anti-seizure medications and antiretroviral medications, used to treat HIV infections, appear to interfere with the body’s ability to use vitamin D.
- Exclusive breast-feeding. Breast milk doesn’t contain enough vitamin D to prevent rickets. Babies who are exclusively breast-fed should receive vitamin D drops.
Rickets prevention
There are several steps you can take to help prevent rickets.
These include ensuring your child:
- has a healthy, balanced diet, eats foods that contain vitamin D naturally — fatty fish, fish oil and egg yolks — or that have been fortified with vitamin D (check labels to determine the vitamin D content of fortified foods), such as:
- Infant formula
- Cereal
- Bread
- Milk, but not foods made from milk, such as yogurt and cheese
- Orange juice
- spends some time outside in the sun
- takes a vitamin D supplement
Exposure to sunlight provides the best source of vitamin D. During most seasons, 10 to 15 minutes of exposure to the sun near midday is enough. However, if you’re dark-skinned, if it’s winter or if you live in northern latitudes, you might not be able to get enough vitamin D from sun exposure. In addition, because of skin cancer concerns, infants and young children, especially, are warned to avoid direct sun or to always wear sunscreen and protective clothing.
Because human milk contains only a small amount of vitamin D, all breast-fed infants should receive 400 international units (IU) of oral vitamin D daily. The American Academy of Pediatricians recommends that breast-fed infants or those who drink less than 33.8 ounces (1 liter) of infant formula a day to take an oral vitamin D supplement.
Children from the age of one year and adults need 15mcg (600 IU) of vitamin D a day.
The Department of Health recommends that:
- pregnant and breastfeeding women should consider taking a daily supplement containing 10 mcg (400 IU) of vitamin D
- babies from birth to one year of age, whether exclusively or partially breastfed, should be given a daily supplement containing 8.5 to 10mcg (340 to 400 IU) of vitamin D, to make sure they get enough
- babies fed infant formula do not need a vitamin D supplement until they are receiving less than 500ml (about a pint) of infant formula a day, because infant formula is fortified with vitamin D
- children aged 1 to 4 years old should be given a daily supplement containing 10 mcg (400 IU) of vitamin D
Vitamin D
Vitamin D helps regulate the amount of calcium and phosphate in the body.
These nutrients are needed to keep bones, teeth and muscles healthy.
A lack of vitamin D can lead to bone deformities such as rickets in children, and bone pain caused by a condition called osteomalacia in adults.
Good sources of vitamin D
From about late March/early April to the end of September, most people should be able to get all the vitamin D they need from sunlight. The body creates vitamin D from direct sunlight on the skin when outdoors. But between October and early March you don’t get enough vitamin D from sunlight.
Rickets symptoms
Rickets causes a child’s bones to become soft and weak, which can lead to bone deformities.
The signs and symptoms of rickets can include:
- Pain – the bones affected by rickets can be sore and painful, so the child may be reluctant to walk or may tire easily; the child’s walk may look different (waddling)
- Skeletal deformities – thickening of the ankles, wrists and knees, bowed legs, soft skull bones and, rarely, bending of the spine
- Dental problems – including weak tooth enamel, delay in teeth coming through and increased risk of cavities
- Poor growth and development – if the skeleton doesn’t grow and develop properly, the child will be shorter than average
- Fragile bones – in severe cases, the bones become weaker and more prone to fractures
Because rickets softens the growth plates at the ends of a child’s bones, it can cause skeletal deformities such as:
- Bowed legs or knock knees
- Thickened wrists and ankles
- Breastbone projection
These symptoms can also affect adults who have soft bones (osteomalacia).
Some children with rickets may also have low levels of calcium in their blood (hypocalcaemia). This can make the symptoms of rickets worse and can also cause muscle cramps, twitching, tingling in the hands and feet, and fits.
Rickets diagnosis
During the exam, the doctor will gently press on your child’s bones, checking for abnormalities. He or she will pay particular attention to your child’s:
- Skull. Babies who have rickets often have softer skull bones and might have a delay in the closure of the soft spots (fontanels).
- Legs. While even healthy toddlers are a little bowlegged, an exaggerated bowing of the legs is common with rickets.
- Chest. Some children with rickets develop abnormalities in their rib cages, which can flatten and cause their breastbones to protrude.
- Wrists and ankles. Children who have rickets often have wrists and ankles that are larger or thicker than normal.
X-rays of the affected bones can reveal bone deformities. Blood and urine tests can confirm a diagnosis of rickets and also monitor the progress of treatment.
Vitamin D levels
The best way to assess vitamin D status is to measure calcidiol [25(OH)D] levels. As calcidiol [25(OH)D] levels fall, intestinal absorption of calcium falls, leading to a decrease in serum calcium. This causes a rise in serum parathyroid hormone (PTH), which stimulates conversion of calcidiol [25(OH)D] to calcitriol [1,25(OH)2D] and thereby maintains absorption of calcium 56. Thus, optimal level of calcidiol [25(OH)D] is defined as the level which causes maximal suppression of parathyroid hormone (PTH) and maximum calcium absorption. The optimal calcidiol [25(OH)D] concentration may also be defined clinically, such as level needed for fracture reduction. There is no consensus on the optimal calcidiol [25(OH)D] concentration for skeletal health. The Institute of Medicine (IOM) supports calcidiol [25(OH)D] concentrations above 20 ng/mL. National Osteoporosis Foundation, International Osteoporosis Foundation, and American Geriatric Society suggest that a minimum level of 30 ng/mL is necessary in older adults to minimize the risk of falls and fracture. All agree that levels lower than 20 ng/mL are suboptimal for skeletal health 57. The optimal serum calcidiol [25(OH)D] level for extraskeletal health is not established. A safe upper serum level has also not been determined. There is an increased risk for fractures and some cancers (e.g. pancreatic, prostate) and mortality with levels above 30–48 ng/mL 58. The Institute of Medicine systematic review favors maintaining the serum calcidiol [25(OH)D] concentration between 20 and 40 ng/mL, whereas others favor maintaining calcidiol [25(OH)D] levels between 30 and 50 ng/mL.
Currently accepted standards for defining vitamin D status in children and adolescents are:
- Vitamin D sufficiency: calcidiol [25(OH)D] ≥ 20 ng/mL;
- Vitamin D insufficiency: calcidiol [25(OH)D] between 15 and 20 ng/mL; and
- Vitamin D deficiency: calcidiol [25(OH)D] ≤ 15 ng/mL.
- Severe deficiency is defined as a calcidiol [25(OH)D] <5 ng/mL. These cut-offs may need to be revised if future pediatric studies demonstrate efficacy of higher calcidiol [25(OH)D] level. Individuals with calcidiol [25(OH)D] levels of 100 ng/mL have been arbitrarily designated as having vitamin D excess and above 150 ng/mL is considered to be intoxication.
Rickets treatment
Most cases of rickets can be treated with vitamin D and calcium supplements. Follow your child’s doctor’s directions as to dosage. Too much vitamin D can be harmful.
Your child’s doctor will monitor your child’s progress with X-rays and blood tests.
What kinds of vitamin D dietary supplements are available ?
Vitamin D is found in supplements (and fortified foods) in two different forms: D2 (ergocalciferol) and D3 (cholecalciferol). Both increase vitamin D in the blood.
In supplements and fortified foods, vitamin D is available in two forms, D2 (ergocalciferol) and D3 (cholecalciferol) that differ chemically only in their side-chain structure. Vitamin D2 is manufactured by the UV irradiation of ergosterol in yeast, and vitamin D3 is manufactured by the irradiation of 7-dehydrocholesterol from lanolin and the chemical conversion of cholesterol 18. The two forms have traditionally been regarded as equivalent based on their ability to cure rickets and, indeed, most steps involved in the metabolism and actions of vitamin D2 and vitamin D3 are identical. Both forms (as well as vitamin D in foods and from cutaneous synthesis) effectively raise serum Calcidiol [25-hydroxyvitamin D or 25(OH)D] levels 14. Firm conclusions about any different effects of these two forms of vitamin D cannot be drawn. However, it appears that at nutritional doses vitamins D2 and D3 are equivalent, but at high doses vitamin D2 is less potent. Some studies suggest that cholecalciferol (Vitamin D3) increases serum Calcidiol [25(OH) D] more efficiently than does ergocalciferol (Vitamin D2) 7.
- Vitamin D3 (cholecalciferol) is available in 400, 800, 1000, 2000, 5000, 10,000, and 60,000 IU capsules. It is available in some countries as an intramuscular injection (Arachital 600,000 IU, which maintains vitamin D levels for 1 year). However, it can be extremely painful 7.
- Vitamin D2 (ergocalciferol) is available for oral use in 400 and 50,000 unit capsules or in a liquid form (8000 IU/mL) 7.
Adults Vitamin D Deficiency Treatment
Dosing of vitamin D depends upon the nature and severity of the deficiency. In patients with normal absorptive capacity, for every 100 units of added vitamin D3 (cholecalciferol), serum calcidiol [25(OH)D] concentrations increase by approximately 1.0 ng/mL. Multiple dosing regimens have been shown to treat vitamin D deficiency effectively. In a 2-month trial of oral vitamin D3 (cholecalciferol) repletion in elderly women with hip fracture, the same cumulative dose given daily (1500 units), weekly (10,500 units), or monthly (45,000 units) resulted in similar increments in serum calcidiol [25(OH)D] levels. Although large annual doses of vitamin D3 (cholecalciferol) increase serum calcidiol [25(OH)D] levels, they are not recommended as undesirable effects of increasing falls and fractures in older adults are seen.
Various regimes which can be used are as follows 7:
- High-risk individuals with serum calcidiol [25(OH)D] concentrations <20 ng/mL should be treated with 50,000 IU of vitamin D2 (ergocalciferol) or D3 (cholecalciferol) orally once per week for 6–8 weeks, followed by 800 units of vitamin D daily thereafter.
- For high-risk individuals with serum calcidiol [25(OH)D] levels of 20–30 ng/mL, initial supplementation with 600–800 units of vitamin D3 (cholecalciferol) daily may be sufficient to maintain levels in the target range.
- In pregnant women, weekly doses of 50,000 units for 6–8 weeks are not recommended and 600–800 units of vitamin D3 (cholecalciferol) daily are thought to be safer. Urinary calcium excretion increases in pregnancy, and it should be monitored when treating vitamin D deficiency, especially in women with a history of renal stones.
- In malabsorption or patients with gastrectomy, generally high doses of vitamin D of 10,000–50,000 units daily are needed to correct the deficiency. Hydroxylated vitamin D metabolites are good options because they are more readily absorbed.
The above recommendations are in agreement with Endocrine Society practice guidelines on the treatment of vitamin D deficiency. In adults with vitamin D deficiency, however, the Endocrine Society guidelines suggest a maintenance dose of vitamin D2 or D3 (1500–2000 IU daily) to maintain a serum 25(OH)D concentration above 30 ng/mL 59.
All patients should consume total calcium of at least 1000 mg (for ages 19–70 years) to 1200 mg (for women of ages 51 through 70 years and for all adults 71 years and older) per day. The upper level (UL) of intake for calcium in most adults is 2000–2500 mg daily. However, a higher calcium dose (up to 4 g/day) may be necessary in patients with malabsorption. Parenteral calcium as calcium gluconate (10–20 mg of elemental calcium per kg intravenously slowly over 5–10 minutes, usually given as 1–2 mL/kg of 10% calcium gluconate) becomes necessary in case of manifest tetany or convulsions. Repeat boluses may also be necessary. In addition, calcitriol may be necessary in doses of 20–100ng/ kg/day in two to three divided doses until calcium levels normalize. High doses of calcium are necessary early in the course of therapy, after which doses are reduced by half for the next 1–2 weeks. Once vitamin D supplementation has been reduced to 400 IU/day with normal PTH and calcidiol [25(OH)D] levels, calcium supplementation is usually not necessary.
Children Vitamin D Deficiency Treatment
The most widely used treatment for vitamin D deficiency consists of vitamin D2 (ergocalciferol) or vitamin D3 (cholecalciferol). The dosing scheme recommended for treatment of vitamin D deficient rickets is 1000 IU daily for newborns <1 month, 1000–5000 IU daily for infants 1–12 months old, and 5000–10,000 IU daily for children 1 year and older. Treatment is continued until there is radiographic evidence of healing; subsequently, the dose of vitamin D is reduced to 400 IU daily. Calcium intake should be maintained at approximately 1000 mg/day (30–75 mg/ kg of elemental calcium per day in three divided doses) to avoid “hungry bone” syndrome (worsening hypocalcemia after the start of vitamin D therapy). This leads to resolution of the biochemical and radiological abnormalities within 3 months. Skeletal deformities regress completely after medical therapy. However, orthopedic intervention can be done if deformities do not improve even after radiologic appearance of the growth plates has normalized. An alternative protocol is “stoss therapy,” which consists of a high dose of oral vitamin D (600,000 IU) given on a single day, then maintained at 400–1000 IU of vitamin D per day, or 50,000 IU of vitamin D2 (ergocalciferol) weekly for 8 weeks orally (teenagers) followed by 400 IU/day. This amount of vitamin D approximately corresponds to a 3-month course of 5000 IU/day and should be sufficient to induce healing within 3 months. High-dose vitamin D may need to be intermittently repeated (usually every 3 months) if poor compliance persists. Stoss therapy is useful when compliance is a problem. However, such high doses of vitamin D can lead to hypercalcemia. Doses of 150,000 or 300,000 IU are equally effective with lesser side effects.
Vitamin D Side Effects
Side effects of calcitriol therapy include hypercalcemia, hypercalciuria, nephrocalcinosis, and intraocular calcifications. There may be polyuria, pruritis, and azotemia. The first measurable consequences of vitamin D toxicity are hypercalciuria and hypercalcemia, which have been observed only at calcidiol [25(OH)D] levels above 88 ng/mL. Many patients take vitamin and mineral supplements that contain vitamin D without being aware of these. It is important to inquire about additional dietary supplements that patients may be taking before prescribing extra vitamin D 60. Exposure to sunlight for extended periods of time does not normally cause vitamin D toxicity. Within about 20 minutes of UV exposure in light-skinned individuals, the concentrations of vitamin D precursors produced in the skin reach an equilibrium and any further vitamin D that is produced is degraded. According to some sources, endogenous production with full body exposure to sunlight is approximately 10,000 IU/day.
Some patients with vitamin D deficiency have coexisting primary hyperparathyroidism that is not recognized until vitamin D is repleted. Vitamin D replacement in these individuals should be provided cautiously as hypercalcemia and hypercalciuria may develop. In contrast, in individuals with clinically significant vitamin D deficiency and secondary hyperparathyroidism, calcium concentrations are generally normal or at the lower end of normal (rarely below normal) and PTH concentrations are mildly elevated. The PTH level should return to normal upon vitamin D repletion. Urinary calcium is extremely low in patients with vitamin D deficiency and secondary hyperparathyroidism and takes months to normalize, whereas in primary hyperparathyroidism it normalizes very rapidly with vitamin D replacement.
- Rickets. MedlinePlus. https://medlineplus.gov/rickets.html[↩]
- Yetley EA. Assessing the vitamin D status of the US population. Am J Clin Nutr. 2008;88:558S. https://www.ncbi.nlm.nih.gov/pubmed/18689402[↩]
- Goswami R, Mishra SK, Kochupillai N. Prevalence and potential significance of vitamin D deficiency in Asian Indians. Indian J Med Res. 2008;127:229–38. https://www.ncbi.nlm.nih.gov/pubmed/18497436[↩]
- Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988-1994 compared with 2000-2004. Am J Clin Nutr. 2008;88:1519. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2745830/[↩]
- National Institute of Health. Vitamin D. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/[↩]
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010[↩][↩][↩][↩][↩][↩][↩]
- Sahay M, Sahay R. Rickets–vitamin D deficiency and dependency. Indian Journal of Endocrinology and Metabolism. 2012;16(2):164-176. doi:10.4103/2230-8210.93732. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3313732/[↩][↩][↩][↩][↩]
- Christakos S, Ajibade dV, dhawan P, Fechner AJ, Mady LJ. vitamin D: Metabolism. Endocrinol Metab Clin North Am. 2010;39:243. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2879391/[↩][↩]
- Portale AA, Halloran BP, Morris RC., Jr Physiologic regulation of the serum concentration of 1,25-dihydroxyvitamin D by phosphorus in normal men. J Clin Invest. 1989;83:1494. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC303852/[↩]
- Iida K, Shinki T, Yamaguchi A, DeLuca HF, Kurokawa K, Suda T. A possible role of vitamin D receptors in regulating vitamin D activation in the kidney. Proc Natl Acad Sci U S A. 1995;92:6112. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC41652/[↩]
- Prié D, Friedlander G. Reciprocal control of 1,25-dihydroxyvitamin D and FGF23 formation involving the FGF23/Klotho system. Clin J Am Soc Nephrol. 2010;5:1717. http://cjasn.asnjournals.org/content/5/9/1717.long[↩]
- Liu S, Tang W, Zhou J, Stubbs JR, Luo Q, Pi M, et al. Fibroblast growth factor 23 is a counter-regulatory phosphaturic hormone for vitamin D. J Am Soc Nephrol. 2006;17:1305–15. http://jasn.asnjournals.org/content/17/5/1305.long[↩]
- Bikle D. Nonclassic actions of vitamin D. J Clin Endocrinol Metab. 2009;94:26. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2630868/[↩]
- Cranney C, Horsely T, O’Donnell S, Weiler H, Ooi D, Atkinson S, et al. Effectiveness and safety of vitamin D. Evidence Report/Technology Assessment No. 158 prepared by the University of Ottawa Evidence-based Practice Center under Contract No. 290-02.0021. AHRQ Publication No. 07-E013. Rockville, MD: Agency for Healthcare Research and Quality, 2007. https://www.ncbi.nlm.nih.gov/pubmed/18088161?dopt=Abstract[↩][↩][↩]
- Holick MF. Vitamin D. In: Shils ME, Shike M, Ross AC, Caballero B, Cousins RJ, eds. Modern Nutrition in Health and Disease, 10th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.[↩]
- Norman AW, Henry HH. Vitamin D. In: Bowman BA, Russell RM, eds. Present Knowledge in Nutrition, 9th ed. Washington DC: ILSI Press, 2006.[↩]
- Jones G. Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr 2008;88:582S-6S. https://www.ncbi.nlm.nih.gov/pubmed/18689406?dopt=Abstract[↩][↩]
- Holick MF. Vitamin D deficiency. N Engl J Med 2007;357:266-81. https://www.ncbi.nlm.nih.gov/pubmed/17634462?dopt=Abstract[↩][↩]
- U.S. Department of Agriculture, Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 27. Nutrient Data Laboratory home page, 2014. https://ndb.nal.usda.gov/ndb/[↩]
- Pitt MJ. Rickets and osteomalacia are still around. Radiol Clin North Am. 1991;29:97–118. https://www.ncbi.nlm.nih.gov/pubmed/1985332[↩]
- Rauch F. The rachitic bone. Endocr Dev. 2003;6:69. https://www.ncbi.nlm.nih.gov/pubmed/12964426[↩]
- Kim CJ, Kaplan LE, Perwad F, Huang N, Sharma A, Choi Y, et al. vitamin D 1alpha-hydroxylase gene mutations in patients with 1alpha-hydroxylase deficiency. J Clin Endocrinol Metab. 2007;92:3177–82. https://www.ncbi.nlm.nih.gov/pubmed/17488797[↩]
- Brooks MH, Bell NH, Love L, Stern PH, Orfei E, Queener SF, et al. Vitamin-D-dependent rickets type II.Resistance of target organs to 1,25-dihydroxyvitamin D. N Engl J Med. 1978;298:996–9. https://www.ncbi.nlm.nih.gov/pubmed/205789[↩]
- Sahay M, Sahay R. Rickets–vitamin D deficiency and dependency. Indian Journal of Endocrinology and Metabolism. 2012;16(2):164-176. doi:10.4103/2230-8210.93732. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3313732[↩][↩]
- Haddad JG. vitamin D–solar rays, the Milky Way, or both? N Engl J Med. 1992;326:1213. http://www.nejm.org/doi/full/10.1056/NEJM199204303261808[↩]
- Binkley N, Novotny R, Krueger d, Kawahara T, Daida YG, Lensmeyer G, et al. Low vitamin D status despite abundant sun exposure. J Clin Endocrinol Metab. 2007;92:2130–5. https://www.ncbi.nlm.nih.gov/pubmed/17426097[↩]
- Terushkin V, Bender A, Psaty EL, Engelsen O, Wang SQ, Halpern AC. Estimated equivalency of vitamin D production from natural sun exposure versus oral vitamin D supplementation across seasons at two US latitudes. J Am Acad Dermatol. 2010;62:929.e1. https://www.ncbi.nlm.nih.gov/pubmed/20363523[↩]
- Chatfield SM, Brand C, Ebeling PR, Russell dM. vitamin D deficiency in general medical inpatients in summer and winter. Intern Med J. 2007;37:377–82. https://www.ncbi.nlm.nih.gov/pubmed/17535381[↩]
- Awumey EM, Mitra DA, Hollis BW, Kumar R, Bell NH. vitamin D metabolism is altered in Asian Indians in the southern United States: A clinical research center study. J Clin Endocrinol Metab. 1998;83:169–73. https://www.ncbi.nlm.nih.gov/pubmed/9435436[↩]
- Klein GL, Chen TC, Holick MF, Langman CB, Price H, Celis MM, et al. Synthesis of vitamin D in skin after burns. Lancet. 2004;363:291–2. https://www.ncbi.nlm.nih.gov/pubmed/14751703[↩]
- Carvalho NF, Kenney RD, Carrington PH, Hall DE. Severe nutritional deficiencies in toddlers resulting from health food milk alternatives. Pediatrics. 2001;107:E46. https://www.ncbi.nlm.nih.gov/pubmed/11335767[↩]
- Gloth FM, 3rd, Gundberg CM, Hollis BW, Haddad JG, Jr, Tobin JD. vitamin D deficiency in homebound elderly persons. JAMA. 1995;274:1683–6. https://www.ncbi.nlm.nih.gov/pubmed/7474272[↩]
- Hollis BW, Wagner CL. vitamin D requirements during lactation: High-dose maternal supplementation as therapy to prevent hypovitaminosis D for both the mother and the nursing infant. Am J Clin Nutr. 2004;80:1752S. https://www.ncbi.nlm.nih.gov/pubmed/15585800[↩]
- Thandrayen K, Pettifor JM. Maternal vitamin D status: Implications for the development of infantile nutritional rickets. Endocrinol Metab Clin North Am. 2010;39:303. https://www.ncbi.nlm.nih.gov/pubmed/20511053[↩]
- Specker BL, Valanis B, Hertzberg V, Edwards N, Tsang RC. Sunshine exposure and serum 25-hydroxyvitamin D concentrations in exclusively breast-fed infants. J Pediatr. 1985;107:372. https://www.ncbi.nlm.nih.gov/pubmed/3839846[↩]
- Tsang RC, Zlotkin SH, Nichols BL, Hansen JW, editors. 2nd ed. Cincinnati, OH: Digital Education Publishing; 1997. Formula fed nutrition during infancy: Principles and Practice; p. 467.[↩]
- Parikh SJ, Edelman M, Uwaifo GI, Freedman RJ, Semega-Janneh M, Reynolds J, et al. The relationship between obesity and serum 1, 25-dihydroxy vitamin D concentrations in healthy adults. J Clin Endocrinol Metab. 2004;89:1196–9. https://www.ncbi.nlm.nih.gov/pubmed/15001609[↩]
- Thomas MK, Lloyd-Jones DM, Thadhani RI, Shaw AC, Deraska DJ, Kitch BT, et al. Hypovitaminosis d in medical inpatients. N Engl J Med. 1998;338:777–83. http://www.nejm.org/doi/10.1056/NEJM199803193381201[↩]
- Holick MF, Siris ES, Binkley N, Beard MK, Khan A, Katzer JT, et al. Prevalence of vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab. 2005;90:3215–24. https://www.ncbi.nlm.nih.gov/pubmed/15797954[↩]
- Elder GJ, Mackun K. 25-Hydroxyvitamin D deficiency and diabetes predict reduced BMD in patients with chronic kidney disease. J Bone Miner Res. 2006;21:1778. https://www.ncbi.nlm.nih.gov/pubmed/17002574[↩]
- Taskapan H, Ersoy FF, Passadakis PS, Tam P, Memmos dE, Katopodis KP, et al. Severe vitamin D deficiency in chronic renal failure patients on peritoneal dialysis. Clin Nephrol. 2006;66:247–55. https://www.ncbi.nlm.nih.gov/pubmed/17063991[↩]
- Vaziri ND. Endocrinological consequences of the nephrotic syndrome. Am J Nephrol. 1993;13:360. https://www.ncbi.nlm.nih.gov/pubmed/8116688[↩]
- Oduwole AO, Giwa OS, Arogundade RA. Relationship between rickets and incomplete distal renal tubular acidosis in children. Ital J Pediatr. 2010;36:54. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2925332/[↩]
- Dibble JB, Sheridan P, Losowsky MS. A survey of vitamin D deficiency in gastrointestinal and liver disorders. Q J Med. 1984;53:119. https://www.ncbi.nlm.nih.gov/pubmed/6546800[↩]
- American Gastroenterological Association medical position statement: Guidelines on osteoporosis in gastrointestinal diseases. Gastroenterology. 2003;124:791. https://www.ncbi.nlm.nih.gov/pubmed/12612916[↩][↩]
- Sotaniemi EA, Hakkarainen HK, Puranen JA, Lahti RO. Radiologic bone changes and hypocalcemia with anticonvulsant therapy in epilepsy. Ann Intern Med. 1972;77:389. https://www.ncbi.nlm.nih.gov/pubmed/4262314[↩]
- Hahn TJ. Drug-induced disorders of vitamin D and mineral metabolism. Clin Endocrinol Metab. 1980;9:107. https://www.ncbi.nlm.nih.gov/pubmed/6998606[↩]
- Ric John M. Pettifor vitamin D and/or calcium deficiency rickets in infants and children: Anglobal perspective. Indian J Med Res. 2008;127:245–9. https://www.ncbi.nlm.nih.gov/pubmed/18497438[↩]
- De Lucia MC, Mitnick ME. Carpenter Nutritional rickets with normal circulating 25-hydroxyvitamin D: A call for reexamining the role of dietary calcium intake in North American infants. J Clin Endocrinol Metab. 2003;88:3539. https://www.ncbi.nlm.nih.gov/pubmed/12915633[↩]
- https://health.gov/dietaryguidelines/2015/guidelines/[↩]
- https://www.choosemyplate.gov/[↩]
- The USDA Food Composition Databases. https://ndb.nal.usda.gov/ndb/[↩]
- U.S. Department of Agriculture, Center for Nutrition Policy and Promotion. ChooseMyPlate.gov 2011. https://www.choosemyplate.gov/[↩]
- Sahay M, Vali SP, Ramesh VD. The Case. A child with metabolic acidosis and growth retardation. Kidney Int. 2009;75:1121–2. http://www.kidney-international.theisn.org/article/S0085-2538(15)53555-2/fulltext[↩]
- Sahay M, Sahay R. Rickets in tropics. Int J Endocrinol Metab. 2010;23:1–5.[↩][↩]
- Durazo-Arvizu RA, Dawson-Hughes B, Sempos CT, Yetley EA, Looker AC, Cao G, et al. Three-phase model harmonizes estimates of the maximal suppression of parathyroid hormone by 25-hydroxyvitamin D in persons 65 years of age and older. J Nutr. 2010;140:595–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2821888/[↩]
- Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R. Estimates of optimal vitamin D status. Osteoporos Int. 2005;16:713–6. https://www.ncbi.nlm.nih.gov/pubmed/15776217[↩]
- Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, et al. Annual high-dose oral vitamin D and falls and fractures in older women: A randomized controlled trial. JAMA. 2010;303:1815–22. https://www.ncbi.nlm.nih.gov/pubmed/20460620[↩]
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley dA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30. https://www.ncbi.nlm.nih.gov/pubmed/21646368[↩]
- Vieth R. vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. Am J Clin Nutr. 1999;69:842–56. https://www.ncbi.nlm.nih.gov/pubmed/10232622[↩]