Contents
What is aspergillosis
Aspergillosis is an infection or allergic reaction caused by the Aspergillus fungus, a common mold (a type of fungus) that lives indoors and outdoors on rotting vegetation. Aspergillus mold growth is encouraged by warm and humid conditions. Aspergillus is ubiquitous in the environment; it can be found in soil, decomposing plant matter, household dust, building materials, plants, food, and water. Outdoors they can be found in shady, damp areas or places where leaves or other vegetation is decomposing. Indoors they can be found where humidity levels are high, such as basements or showers. Most people breathe in Aspergillus fungus spores every day without getting sick. However, people with weakened immune systems or lung diseases are at a higher risk of developing health problems due to Aspergillus. Some people with asthma are allergic to Aspergillus and develop allergic bronchopulmonary aspergillosis (ABPA). The symptoms include wheezing and blood-stained sputum.
There are approximately 180 species of Aspergillus, but fewer than 40 of them are known to cause infections in humans. Aspergillus fumigatus is the most common cause of human Aspergillus infections. Other common species include Aspergillus flavus, Aspergillus terreus, Aspergillus nidulans, Aspergillus versicolor and Aspergillus niger.
Although Aspergillus fungi are commonly found in the environment, farmers are most at risk when working with composting or decaying vegetation such as rain damaged hay, silage or moldy grain.
Heavy rainfall and damp conditions increase the incidence of molds in hay and composting vegetation. Moldy hay can contain Aspergillus mold spores which are tiny at 2-3 microns and can go deep into your lungs when inhaled, causing respiratory illness.
If hay is baled at high moisture content levels it can increase the likelihood of hay becoming moldy. When purchasing hay you should also check for the presence of mold. Hay which is darker in color or has a musty smell is indicative of mold being present.
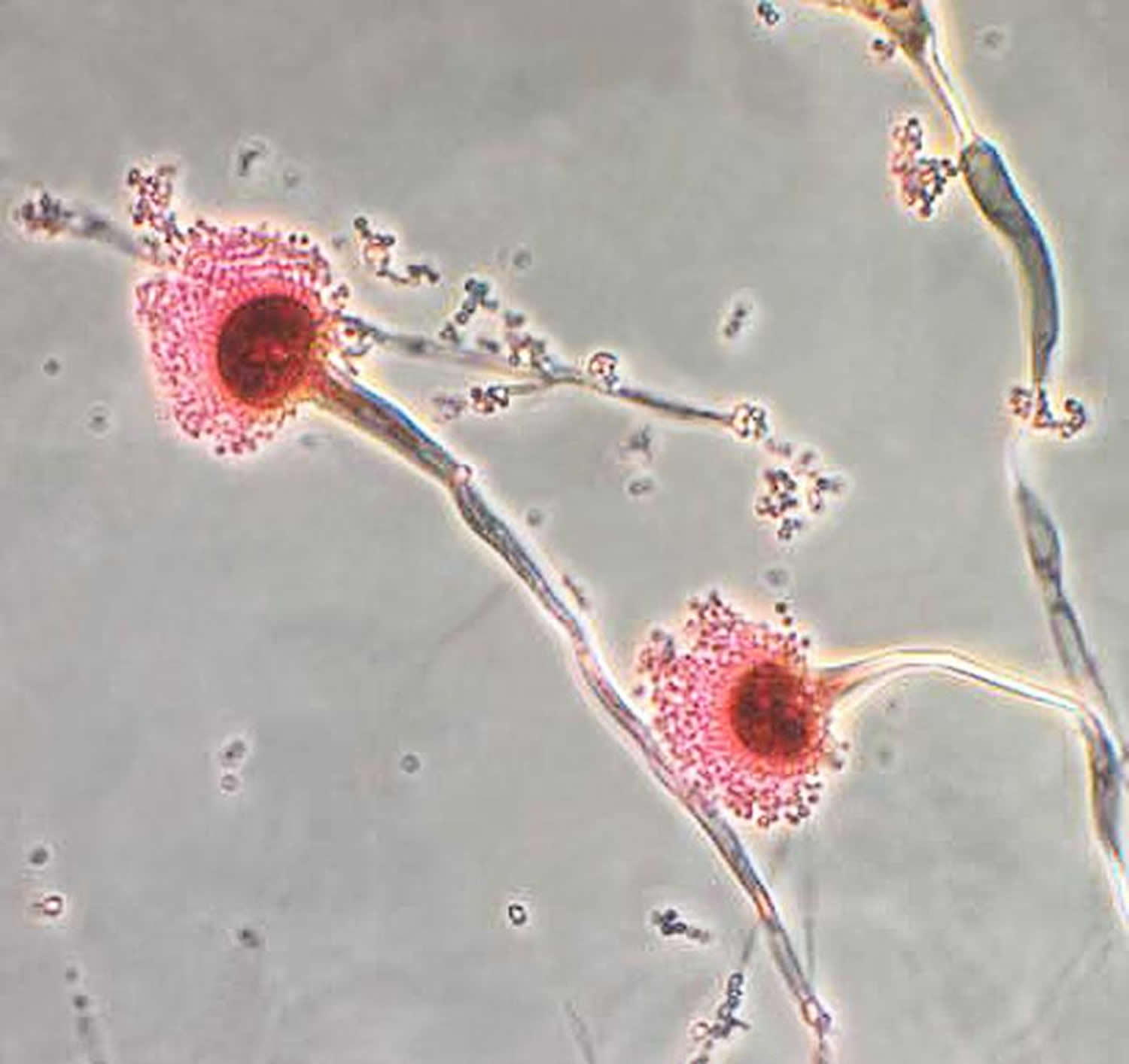
Figure 1. Aspergillus (aspergillus fumigatus)
The types of health problems caused by Aspergillus include allergic reactions, lung infections, and infections in other organs.
Types of aspergillosis
- Allergic bronchopulmonary aspergillosis (ABPA): Aspergillus causes inflammation in the lungs and allergy symptoms such as coughing and wheezing, but doesn’t cause an infection 1. This happens in patients with asthma when the bronchi (large windpipe leading to the lungs) is infected with a fungus called Aspergillus. Depending of individuals, there is mounting of an immune response towards these fungi, leading to recurrent symptoms like a typical asthma attack. This is a disease of the airways, ie. the windpipe leading to the lungs. Asthma is a criterion for diagnosing allergic bronchopulmonary aspergillosis (ABPA). This disease only occurs in asthmatics. A recent study suggested that the allergic bronchopulmonary aspergillosis (ABPA) in patients with chronic bronchial asthma is as high as 16%. Otherwise, aspergillosis affects all races, gender, and age equally. There is also no geographical differences around the world. The mechanism of allergic bronchopulmonary aspergillosis (ABPA) remains incompletely understood. However it involves allergic reaction to the fungus Aspergillus sp. Chronic lung conditions such as asthma and cystic fibrosis may trap Aspergillus fumigatus in the persistent, thick secretions. The body responds by mounting an immune reaction towards Aspergillus. It is interesting to note that despite vigorous immune responses towards Aspergillus, the fungus is still able to colonise the airway and cause recurrent symptoms. Chronic colonisation by Aspergillus eventually leads to enzymes and toxin release by the fungi. Added with chronic inflammation, this can lead to airway destruction and dilatation, called bronchiectasis. This disease is characterized by remissions and relapses. This means the disease comes and goes.
- Allergic Aspergillus sinusitis: Aspergillus causes inflammation in the sinuses and symptoms of a sinus infection (drainage, stuffiness, headache) but doesn’t cause an infection 2.
- Aspergilloma: also called a “fungus ball.” As the name suggests, it is a ball of Aspergillus that grows in the lungs or sinuses, but usually does not spread to other parts of the body 3.
- Chronic pulmonary aspergillosis: a long-term (3 months or more) condition in which Aspergillus can cause cavities in the lungs. One or more fungal balls (aspergillomas) may also be present in the lungs 4.
- Invasive aspergillosis: a serious infection that usually affects people who have weakened immune systems, such as people who have had an organ transplant or a stem cell transplant. Invasive aspergillosis most commonly affects the lungs, but it can also spread to other parts of the body.
- Cutaneous (skin) aspergillosis: Aspergillus enters the body through a break in the skin (for example, after surgery or a burn wound) and causes infection, usually in people who have weakened immune systems. Cutaneous aspergillosis can also occur if invasive aspergillosis spreads to the skin from somewhere else in the body, such as the lungs 5.
Allergic forms of aspergillosis such as allergic bronchopulmonary aspergillosis (ABPA) and allergic Aspergillus sinusitis are generally not life-threatening.
In contrast, although invasive aspergillosis is uncommon, it is a serious infection and can be a major cause of mortality in immunocompromised patients. For example, a large prospective study found that the one-year survival for people who had invasive aspergillosis was 59% among solid organ transplant recipients 6 and 25% among stem cell transplant recipients 7.
Because aspergillosis is not a reportable infection in the United States, the exact number of cases is difficult to determine. Milder, allergic forms of aspergillosis are more common than the invasive form of the infection.
Allergic bronchopulmonary aspergillosis (ABPA) likely affects between 1 and 15% of cystic fibrosis patients 8. One study calculated that 2.5% of adults who have asthma also have allergic bronchopulmonary aspergillosis (ABPA), which is approximately 4.8 million people worldwide 9. Of these 4.8 million people who have allergic bronchopulmonary aspergillosis, an estimated 400,000 also have chronic pulmonary aspergillosis 9. Another 1.2 million people are estimated to have chronic pulmonary aspergillosis as a sequel to tuberculosis 10 and over 70,000 people are estimated to have chronic pulmonary aspergillosis as a complication of sarcoidosis 11.
Invasive aspergillosis is uncommon and occurs primarily in immunocompromised people. The first population-based incidence estimates for invasive aspergillosis were obtained from laboratory surveillance conducted in the San Francisco Bay Area during 1992-1993 and suggested a yearly rate of 1 to 2 cases of aspergillosis per 100,000 population 12. However, the epidemiology of invasive Aspergillus infections has likely shifted since this time due to the increasing number of solid organ and stem cell transplant recipients and newer immunosuppressive agents.
Prospective surveillance among transplant recipients performed during 2001-2006 found that invasive aspergillosis was the most common type of fungal infection among stem cell transplant recipients 7 and was the second-most common type of fungal infection among solid organ transplant recipients 6.
Although most cases of aspergillosis are sporadic (not part of an outbreak), outbreaks of invasive aspergillosis occasionally occur in hospitalized patients. Invasive aspergillosis outbreaks are often found to be associated with hospital construction or renovation, which can increase the amount of airborne Aspergillus, resulting in respiratory infections or surgical site infections in high-risk patients 13. Outbreaks of primary cutaneous aspergillosis and central nervous system aspergillosis in association with the use of contaminated medical devices have also been described 14. The incubation period for aspergillosis is unclear and likely varies depending on the dose of Aspergillus and the host immune response.
Is aspergillosis contagious?
No. Aspergillosis can’t spread between people or between people and animals from the lungs.
Who gets aspergillosis
The different types of aspergillosis affect different groups of people 15.
- Allergic bronchopulmonary aspergillosis (ABPA) most often occurs in people who have cystic fibrosis or asthma.
- Aspergillomas usually affect people who have other lung diseases like tuberculosis.
- Chronic pulmonary aspergillosis typically occurs in people who have other lung diseases, including tuberculosis, chronic obstructive pulmonary disease (COPD), or sarcoidosis 16.
- Invasive aspergillosis affects people who have weakened immune systems, such as people who have had a stem cell transplant or organ transplant, are getting chemotherapy for cancer, or are taking high doses of corticosteroids.
Aspergillus causes
Aspergillus mold is unavoidable. Outdoors, it’s found in decaying leaves and compost and on plants, trees and grain crops. Inside, the spores — the reproductive parts of mold — thrive in air conditioning and heating ducts, insulation, and some food and spices.
Everyday exposure to aspergillus is rarely a problem for people with healthy immune systems. When mold spores are inhaled, immune system cells surround and destroy them. But people who have a weakened immune system from illness or immunosuppressant medications have fewer infection-fighting cells. This allows aspergillus to take hold, invading the lungs and, in the most serious cases, other parts of the body.
Aspergillosis is not contagious from person to person.
Risk factors for developing aspergillosis
Your risk of developing aspergillosis depends on your overall health and the extent of your exposure to mold. In general, these factors make you more vulnerable to infection:
- Weakened immune system. People taking immune-suppressing drugs after undergoing transplant surgery — especially bone marrow or stem cell transplants — or people who have certain cancers of the blood are at highest risk of invasive aspergillosis. People in the later stages of AIDS also may be at increased risk.
- Low white blood cell level. Having chemotherapy, an organ transplant or leukemia lowers your white cell level, making you more susceptible to invasive aspergillosis. So does having chronic granulomatous disease — an inherited disorder that affects immune system cells.
- Lung cavities. People who have healed air spaces (cavities) in their lungs are at higher risk of developing a mass of tangled fungus fibers (aspergilloma). Cavities are areas that have been damaged by radiation to the lung or by lung diseases such as tuberculosis or sarcoidosis — a noncancerous, inflammatory illness.
- Asthma or cystic fibrosis. People with asthma and cystic fibrosis, especially those whose lung problems are long-standing or hard to control, are more likely to have an allergic response to aspergillus mold.
- Long-term corticosteroid therapy. Long-term use of corticosteroids may increase the risk of opportunistic infections, depending on the underlying disease being treated and what other drugs are being used.
Aspergillus prevention
It’s difficult to avoid breathing in Aspergillus spores because the fungus is common in the environment. For people who have weakened immune systems, there may be some ways to lower the chances of developing a severe Aspergillus infection.
- Protect yourself from the environment 17. It’s important to note that although these actions are recommended, they haven’t been proven to prevent aspergillosis.
- Try to avoid areas with a lot of dust like construction or excavation sites. If you can’t avoid these areas, wear an N95 respirator (a type of face mask) while you’re there.
- Avoid activities that involve close contact to soil or dust, such as yard work or gardening. If this isn’t possible,
- Wear shoes, long pants, and a long-sleeved shirt when doing outdoor activities such as gardening, yard work, or visiting wooded areas.
- Wear gloves when handling materials such as soil, moss, or manure.
- To reduce the chances of developing a skin infection, clean skin injuries well with soap and water, especially if they have been exposed to soil or dust.
- Antifungal medication. If you are at high risk for developing invasive aspergillosis (for example, if you’ve had an organ transplant or a stem cell transplant), your healthcare provider may prescribe medication to prevent aspergillosis 18. Scientists are still learning about which transplant patients are at highest risk and how to best prevent fungal infections. The Infectious Diseases Society of America 19 recommends prophylaxis with posaconazole (strong recommendation; high-quality evidence), voriconazole (strong recommendation; moderate-quality evidence), and/or micafungin (weak recommendation; low-quality evidence) during prolonged neutropenia for those who are at high risk for invasive aspergillosis (strong recommendation; high-quality evidence). Prophylaxis with caspofungin is also probably effective (weak recommendation; low-quality evidence). Prophylaxis with itraconazole is effective, but therapy may be limited by absorption and tolerability (strong recommendation; moderate-quality evidence). Triazoles should not be coadministered with other agents known to have potentially toxic levels with concurrent triazole coadministration (eg, vinca alkaloids, and others) (strong recommendation; moderate-quality evidence).
- For Patients With Graft-Versus-Host Disease: The Infectious Diseases Society of America 19 recommends prophylaxis with posaconazole for allogeneic allogeneic hematopoietic stem cell transplant recipients with Graft-Versus-Host Disease who are at high risk for invasive aspergillosis (strong recommendation; high-quality evidence). Prophylaxis with other mold-active azoles is also effective. Voriconazole is commonly used for prophylaxis against IA in high-risk patients but did not show improved survival in clinical trials (strong recommendation; moderate-quality evidence). Prophylaxis with itraconazole is limited by tolerability and absorption (strong recommendation; high-quality evidence).The Infectious Diseases Society of America 19 recommends continuation of antifungal prophylaxis throughout the duration of immunosuppression in patients with chronic immunosuppression associated with Graft-Versus-Host Disease (corticosteroid equivalent of >1 mg/kg/day of prednisone for >2 weeks and/or the use of other anti-Graft-Versus-Host Disease therapies, such as lymphocyte-depleting agents, or tumor necrosis factor α (TNF-α) inhibition, for refractory Graft-Versus-Host Disease) (strong recommendation; high-quality evidence).
- For Lung Transplant Patients: The Infectious Diseases Society of America 19 recommends antifungal prophylaxis with either a systemic triazole such as voriconazole or itraconazole or an inhaled AmB product for 3 to 4 months after lung transplant (strong recommendation; moderate-quality evidence).Systemic voriconazole or itraconazole is suggested over inhaled AmB for lung transplant recipients with mold colonization pre- or post–lung transplant, mold infections found in explanted lungs, fungal infections of the sinus, and single-lung transplant recipients (weak recommendation; low-quality evidence).The Infectious Diseases Society of America 19 recommends reinitiating antifungal prophylaxis for lung transplant recipients receiving immunosuppression augmentation with either thymoglobulin, alemtuzumab, or high-dose corticosteroids (strong recommendation; moderate-quality evidence).
- For Nonlung Solid Organ Transplant Recipients: The Infectious Diseases Society of America 19 recommends prophylactic strategies in Solid Organ Transplant recipients based on the institutional epidemiology of infection and assessment of individual risk factors (strong recommendation; low-quality evidence). Prospective trials are lacking to address the need for routine anti-Aspergillus prophylaxis other than for lung transplant recipients. Individual risk factors have been identified in cardiac (pretransplant colonization, reoperation, cytomegalovirus [CMV] infection, renal dysfunction, institutional outbreak), liver (fulminant hepatic failure, reoperation, retransplantation, or renal failure), and others with institutional outbreaks or prolonged or high-dose corticosteroid use. In such patients, the optimal duration of prophylaxis is not known.
- Testing for early infection. Some high-risk patients may benefit from blood tests to detect invasive aspergillosis 20. Talk to your doctor to determine if this type of test is right for you.
How people can decrease mold exposure
Sensitive individuals should avoid areas that are likely to have mold, such as compost piles, cut grass, and wooded areas. Inside homes, mold growth can be slowed by controlling humidity levels and ventilating showers and cooking areas. If there is mold growth in your home, you should clean up the mold and fix the water problem. Mold growth can be removed from hard surfaces with commercial products, soap and water, or a bleach solution of no more than 1 cup of household laundry bleach in 1 gallon of water. Follow the manufacturers’ instructions for use (see product label).
If you choose to use bleach to clean up mold:
- Never mix bleach with ammonia or other household cleaners. Mixing bleach with ammonia or other cleaning products will produce dangerous, toxic fumes.
- Open windows and doors to provide fresh air.
- Wear rubber boots, rubber gloves, and goggles during cleanup of affected area.
- If the area to be cleaned is more than 10 square feet, consult the U.S. Environmental Protection Agency (EPA) guide titled Mold Remediation in Schools and Commercial Buildings. Although focused on schools and commercial buildings, this document also applies to other building types. You can get it by going to the EPA web site at https://www.epa.gov/mold/mold-remediation-schools-and-commercial-buildings-guide.
- Always follow the manufacturer’s instructions when using bleach or any other cleaning product.
Specific Recommendations:
- Keep humidity levels as low as you can—no higher than 50%–all day long. An air conditioner or dehumidifier will help you keep the level low. Bear in mind that humidity levels change over the course of a day with changes in the moisture in the air and the air temperature, so you will need to check the humidity levels more than once a day.
- Use an air conditioner or a dehumidifier during humid months.
- Be sure the home has adequate ventilation, including exhaust fans.
- Add mold inhibitors to paints before application.
- Clean bathrooms with mold killing products.
- Do not carpet bathrooms and basements.
- Remove or replace previously soaked carpets and upholstery.
I’m worried that the mold in my home is Aspergillus. Should someone test the mold to find out what it is?
No. Generally, it’s not necessary to identify the species of mold growing in a home, and CDC doesn’t recommend routine sampling for molds. Current evidence indicates that allergies are the type of diseases most often associated with molds. Since the susceptibility of individuals can vary greatly either because of the amount or type of mold, sampling and culturing are not reliable in determining your health risk. If you are susceptible to mold and mold is seen or smelled, there is a potential health risk; therefore, no matter what type of mold is present, you should arrange for its removal. Furthermore, reliable sampling for mold can be expensive, and standards for judging what is and what is not an acceptable or tolerable quantity of mold have not been established.
Aspergillus complications
Depending on the type of infection, aspergillosis can cause a variety of serious complications:
- Bleeding. Both aspergillomas and invasive aspergillosis can cause severe, and sometimes fatal, bleeding in your lungs.
- Systemic infection. The most serious complication of invasive aspergillosis is the spread of the infection to other parts of your body, especially your brain, heart and kidneys. Invasive aspergillosis spreads rapidly and is often fatal in spite of early treatment.
Aspergillosis symptoms
The different types of aspergillosis can cause different symptoms 15.
The symptoms of allergic bronchopulmonary aspergillosis (ABPA) are similar to asthma symptoms, including:
- Wheezing
- Shortness of breath
- Cough that may bring up blood or plugs of mucus
- Fever (in rare cases)
Some people with asthma or cystic fibrosis have an allergic reaction to aspergillus mold.
Symptoms of allergic Aspergillus sinusitis include 21:
- Stuffiness
- Runny nose
- Headache
- Reduced ability to smell
Symptoms of an aspergilloma (“fungus ball”) include 3
A growth of tangled fungus fibers (fungus ball) may develop in air spaces (cavities) in the lung as part of chronic pulmonary aspergillosis. This type of aspergillosis is called simple aspergilloma. Lung cavities may develop in people with pre-existing lung conditions, such as emphysema, tuberculosis or advanced sarcoidosis.
Aspergilloma is a benign condition that may not produce symptoms or may produce a mild cough only, but over time, the underlying condition can worsen and possibly cause:
- Cough
- Coughing up blood, sometimes large amounts
- Shortness of breath
- Wheezing
- Unintentional weight loss
- Fatigue
Symptoms of chronic pulmonary aspergillosis include 16:
- Weight loss
- Cough
- Coughing up blood
- Fatigue
- Shortness of breath
Invasive aspergillosis 15 usually occurs in people who are already sick from other medical conditions, so it can be difficult to know which symptoms are related to an Aspergillus infection. Invasive pulmonary aspergillosis — the most severe form — occurs when the infection spreads rapidly from the lungs to your brain, heart, kidneys or skin. This occurs only in people whose immune system is weakened, commonly from chemotherapy. Untreated, this form of aspergillus disease is usually fatal. Symptoms of invasive aspergillosis in the lungs include:
- Fever
- Chest pain
- Cough
- Coughing up blood or blood-streaked sputum (hemoptysis)
- Shortness of breath
- Fever and chills
- Severe bleeding from your lungs
- Joint pain
- Headaches or eye symptoms
- Nosebleed
- Facial swelling on one side
- Skin lesions
- Other symptoms can develop if the infection spreads from the lungs to other parts of the body.
Contact your healthcare provider if you have symptoms that you think are related to any form of aspergillosis.
Aspergillosis diagnosis
Diagnosing an infection caused by aspergillus mold can be difficult and depends on the type of aspergillus infection. Aspergillus is common in the environment and is sometimes found in the saliva and sputum of healthy people. What’s more, it’s hard to distinguish aspergillus from certain other molds under the microscope, and symptoms of the infection are similar to those of conditions such as tuberculosis.
Your doctor is likely to use one or more of the following tests:
- Imaging test. A chest X-ray or computerized tomography (CT) scan — a type of X-ray that produces more-detailed images than conventional X-rays do — can usually reveal a fungal mass (aspergilloma), as well as characteristic signs of invasive and allergic bronchopulmonary aspergillosis.
- Respiratory secretion (sputum) test. In this test, a sample of your sputum is stained with a dye and checked for the presence of aspergillus filaments. The specimen is then placed in a culture that encourages the mold to grow to help confirm the diagnosis.
- Tissue and blood tests. Skin, sputum and blood tests may be helpful in confirming allergic bronchopulmonary aspergillosis. For the skin test, a small amount of aspergillus antigen is injected into the skin of your forearm. If your blood has antibodies to the mold, you’ll develop a hard, red bump at the injection site. Blood tests look for high levels of certain antibodies, indicating an allergic response.
- Biopsy. In some cases, examining a sample of tissue from your lungs or sinuses under a microscope may be necessary to confirm a diagnosis of invasive aspergillosis.
- Microscopy: Evaluation of respiratory specimens after the application of special stains can allow for visualization of Aspergillus elements. They appear as septated hyphae with acute angle branching. However, definitive identification is difficult to make by this method alone as it is insensitive and even when positive, several filamentous fungi have a similar microscopic appearance.
- Histopathology: Important for documentation of invasive disease. Similar to microscopy, Aspergillus appears as septated hyphae with acute angle branching and can be mistaken for other filamentous molds.
- Culture: Can be done on a variety of sterile specimens and Aspergillus spp. present as rapidly growing molds that are visible 1-3 days after incubation. Culture allows for the microscopic identification down to the species level; however, this method is relatively insensitive, so patients with invasive aspergillosis may have negative cultures.
- Galactomannan antigen test: This test detects a polysaccharide that makes up part of the cell wall of Aspergillus spp. and other fungi. The Platelia (Bio-Rad Laboratories) assay is approved by the US Food and Drug Administration (FDA) for serum and bronchoalveolar lavage fluid. False positive tests have been reported in association with administration of certain antibiotics and cross reactivity exists with other fungal infections, such as those due to Fusarium spp. or Histoplasma capsulatum.
- Beta-d-glucan assay: This test also detects a component in the cell wall of Aspergillus spp, as well as other fungi. The Fungitell® assay has been approved by the FDA for diagnosis of invasive fungal infections, including those due to Aspergillus, Candida, and Pneumocystis. Similar to galactomannan testing, the specificity of this assay is reduced in a variety of clinical settings, including exposure to certain antibiotics, hemodialysis, and co-infection with certain bacteria.
- Polymerase Chain Reaction (PCR): PCR for detection of Aspergillus spp. from clinical specimens, including tissue and bronchoalveolar lavage fluid, is offered by some laboratories.
Aspergillosis treatment
Aspergillosis treatments vary with the type of disease. Possible treatments include:
- Observation. Simple, single aspergillomas often don’t need treatment, and medications aren’t usually effective in treating these fungal masses. Instead, aspergillomas that don’t cause symptoms may simply be closely monitored by chest X-ray. If the condition progresses, then antifungal medications may be recommended.
- Oral corticosteroids. The goal in treating allergic bronchopulmonary aspergillosis is to prevent existing asthma or cystic fibrosis from worsening. The best way to do this is with oral corticosteroids. Antifungal medications by themselves aren’t helpful for allergic bronchopulmonary aspergillosis, but they may be combined with corticosteroids to reduce the dose of steroids and improve lung function.
- Antifungal medications. These drugs are the standard treatment for invasive pulmonary aspergillosis. Historically, the drug of choice has been amphotericin B, but the newer medication voriconazole (Vfend) is now preferred because it appears to be more effective and may have fewer side effects. All antifungals can cause serious problems, including kidney and liver damage, and they frequently interact with other medications given to people who have weakened immune systems.
- Surgery. Because antifungal medications don’t penetrate aspergillomas very well, surgery to remove the fungal mass is the first-choice treatment when bleeding from the mass in the lungs occurs. But the surgery is risky, and your doctor may instead suggest embolization. In this procedure, a radiologist threads a small catheter into the artery that supplies blood to the cavity containing the fungus ball and injects a material that clogs the artery. Though this procedure can stop massive bleeding, it doesn’t prevent it from recurring, so it’s generally considered a temporary treatment.
Allergic aspergillosis
For allergic forms of aspergillosis such as allergic bronchopulmonary aspergillosis (ABPA) or allergic Aspergillus sinusitis, the recommended treatment is itraconazole, a prescription antifungal medication. Corticosteroids may also be helpful.
Itraconazole is currently the first-line agent for symptomatic patients, cystic fibrosis patients with low FEV1, or those with complications such as bronchiectasis, mucoid impaction, or chronic pulmonary aspergillosis. Itraconazole solution is preferred in cystic fibrosis patients because of poor absorption of capsules. Patients who fail itraconazole, or are intolerant to itraconazole, may respond to voriconazole, posaconazole, or inhaled Amphotericin B 22. Relapse after improvement during antifungal therapy is common; long-term suppressive therapy may be necessary. Interactions of itraconazole with some inhaled corticosteroids can precipitate Cushing’s syndrome, so that reduction in inhaled steroid dose or a switch to ciclesonide may be useful for those patients. Triazole antifungal resistance has been documented in some geographic regions, so susceptibility testing may be valuable in areas where epidemiologic data indicate environmental resistance or isolates are cultured from patients on antifungal therapy.
Allergic Fungal Rhinosinusitis is a small subset (<10%) of chronic rhinosinusitis occurring in adults and children 23. allergic fungal rhinosinusitis is characterized by eosinophilic mucin and fungal hyphae in the paranasal sinuses, often associated with immediate hypersensitivity to various fungi. Fungal culture of nasal secretions is usually unhelpful as it reflects airborne fungi, so clarity about the specific fungus involved is usually inferential or unclear. The disease is commonly associated with nasal polyposis, and sometimes with amphotericin B lipid complex 24. Local complications of allergic fungal rhinosinusitis include ophthalmic involvement with oculomotor palsy, bony erosion, and cavernous venous thrombosis 25. The disease course is long, with many patients having extended periods of remission with exacerbations often following viral and/or bacterial infections. Short courses of modest doses of oral corticosteroids may shrink polyps and allow drainage, but relapse is common, and not usually prevented by topical steroids. Surgical removal of polyps and mucus is the most important aspect of management, with postoperative systemic or topical nasal steroids recommended to reduce the time to relapse 26. Saline washes are often helpful. Omaluzimab has been reported to be helpful in studies of severe asthma with associated chronic rhinitis 27. Oral antifungal therapy for allergic fungal rhinosinusitis, usually itraconazole, is helpful for refractory disease and to prevent relapse in patients with frequent recurrences 28.
Invasive aspergillosis
Invasive aspergillosis needs to be treated with prescription antifungal medication, usually voriconazole 29. Other antifungal medications used to treat aspergillosis include lipid amphotericin formulations, posaconazole, isavuconazole, itraconazole, caspofungin, and micafungin. Whenever possible, immunosuppressive medications should be discontinued or decreased. People who have severe cases of aspergillosis may need surgery.
Duration of antifungal therapy for invasive pulmonary aspergillosis is not well defined 29. The Infectious Diseases Society of America generally recommend that treatment of invasive pulmonary aspergillosis be continued for a minimum of 6–12 weeks, depending on the severity and continuation of immunosuppression, as well as the extent of resolution of clinical disease. Therapeutic monitoring of invasive pulmonary aspergillosis includes serial clinical evaluation of all symptoms and signs, as well as performance of radiographic imaging, usually with CT, at regular intervals. The frequency with which CT should be performed cannot be universally defined and should be individualized on the basis of the rapidity of evolution of pulmonary infiltrates and the acuity of illness in the individual patient. The volume of pulmonary infiltrates may increase for the first 7–10 days of therapy, especially in the context of granulocyte recovery 30. The use of serial serum galactomannan assays for therapeutic monitoring is promising but remains investigational. Progressive increases in Aspergillus antigen levels over time signify a poor prognosis. However, resolution of galactomannan antigenemia to a normal level is not sufficient as a sole criterion for discontinuation of antifungal therapy. Long-term therapy of invasive aspergillosis is facilitated by the availability of oral azole drugs in stable patients. For patients with successfully treated invasive aspergillosis who will require subsequent immunosuppression, resumption of antifungal therapy can prevent recurrent infection 31.
Surgical resection of Aspergillus-infected tissue may be useful in patients who have lesions that are contiguous with the great vessels or other critical organs, lesions causing recalcitrant hemoptysis from a single focus, and in lesions eroding into bone. This decision should be mindful of the probability of structural adhesion eliciting spillage of organism into the pleural space.
- Agarwal R, Chakrabarti A, Shah A, Gupta D, Meis JF, Guleria R, et al. Allergic bronchopulmonary aspergillosis: review of literature and proposal of new diagnostic and classification criteria. Clin Exp Allergy. 2013 Aug;43(8):850-73.[↩]
- Glass D, Amedee RG. Allergic fungal rhinosinusitis: a review. Ochsner J. 2011 Fall;11(3):271-5.[↩]
- Lee SH, Lee BJ, Jung DY, Kim JH, Sohn DS, Shin JW, et al. Clinical manifestations and treatment outcomes of pulmonary aspergilloma. Korean J Intern Med. 2004 Mar;19(1):38-42.[↩][↩]
- Denning DW, Riniotis K, Dobrashian R, Sambatakou H. Chronic cavitary and fibrosing pulmonary and pleural aspergillosis: case series, proposed nomenclature change, and review. Clin Infect Dis. 2003 Oct 1;37 Suppl 3:S265-80.[↩]
- Van Burik JA, Colven R, Spach DH. Cutaneous aspergillosis. J Clin Microbiol. 1998 Nov;36(11):3115-21.[↩]
- Pappas PG, Alexander BD, Andes DR, Hadley S, Kauffman CA, Freifeld A, et al. Invasive fungal infections among organ transplant recipients: results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clin Infect Dis. 2010 Apr 15;50(8):1101-11.[↩][↩]
- Kontoyiannis DP, Marr KA, Park BJ, Alexander BD, Anaissie EJ, Walsh TJ, et al. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001-2006: overview of the Transplant-Associated Infection Surveillance Network (TRANSNET) Database. Clin Infect Dis. 2010 Apr 15;50(8):1091-100.[↩][↩]
- Stevens DA, Moss RB, Kurup VP, Knutsen AP, Greenberger P, Judson MA, et al. Allergic bronchopulmonary aspergillosis in cystic fibrosis–state of the art: Cystic Fibrosis Foundation Consensus Conference. Clin Infect Dis. 2003 Oct 1;37 Suppl 3:S225-64.[↩]
- Denning DW, Pleuvry A, Cole DC. Global burden of allergic bronchopulmonary aspergillosis with asthma and its complication chronic pulmonary aspergillosis in adults. Med Mycol. 2013 May;51(4):361-70.[↩][↩]
- Denning DW, Pleuvry A, Cole DC. Global burden of chronic pulmonary aspergillosis as a sequel to pulmonary tuberculosis. Bull World Health Organ. 2011 Dec 1;89(12):864-72.[↩]
- Denning DW, Pleuvry A, Cole DC. Global burden of chronic pulmonary aspergillosis complicating sarcoidosis. Eur Respir J. 2013 Mar;41(3):621-6.[↩]
- Rees JR, Pinner RW, Hajjeh RA, Brandt ME, Reingold AL. The epidemiological features of invasive mycotic infections in the San Francisco Bay area, 1992-1993: results of population-based laboratory active surveillance. Clin Infect Dis. 1998 Nov;27(5):1138-47.[↩]
- Weber DJ et al. Preventing healthcare-associated Aspergillus infections: a review of recent CDC/HICPAC recommendations. Med Mycol 2009; 47S1: S199-209[↩]
- Gunaratne PS, Wijeyaratne CN, Seneviratne HR. Aspergillus meningitis in Sri Lanka–a post-tsunami effect? N Engl J Med. 2007 Feb 15;356(7):754-6.[↩]
- Barnes PD, Marr KA. Aspergillosis: spectrum of disease, diagnosis, and treatment. Infect Dis Clin North Am. 2006 Sep;20(3):545-61, vi.[↩][↩][↩]
- Schweer KE, Bangard C, Hekmat K, Cornely OA. Chronic pulmonary aspergillosis. Mycoses. 2014 May;57(5):257-70.[↩][↩]
- Avery RK, Michaels MG. Strategies for safe living after solid organ transplantation. Am J Transplant. 2013 Mar;13 Suppl 4:304-10.[↩]
- Brizendine KD, Vishin S, Baddley JW. Antifungal prophylaxis in solid organ transplant recipients. Expert Rev Anti Infect Ther. 2011 May;9(5):571-81.[↩]
- Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America, Clinical Infectious Diseases, Volume 63, Issue 4, 15 August 2016, Pages e1–e60 https://academic.oup.com/cid/article/63/4/e1/2595039[↩][↩][↩][↩][↩][↩]
- Lackner M1, Lass-Flörl C. Up-date on diagnostic strategies of invasive aspergillosis. Curr Pharm Design 2013;19(20):3595-614.[↩]
- Singh N, Bhalodiya NH. Allergic fungal sinusitis (AFS)–earlier diagnosis and management. J Laryngol Otol. 2005 Nov;119(11):875-81.[↩]
- Chishimba L , Langridge P, Powell G, Niven RM, Denning DW. Efficacy and safety of nebulised amphotericin B (NAB) in severe asthma with fungal sensitisation (SAFS) and allergic bronchopulmonary aspergillosis (ABPA). J Asthma 2015; 52:289–95.[↩]
- Chang C , Gershwin ME, Thompson GR3rd. Fungal disease of the nose and sinuses: an updated overview. Curr Allergy Asthma Rep 2013; 13:152–61.[↩]
- Thompson GR 3rd , Patterson TF. Fungal disease of the nose and paranasal sinuses. J Allergy Clin Immunol 2012; 129:321–6.[↩]
- Bozeman S , deShazo R, Stringer S, Wright L. Complications of allergic fungal sinusitis. Am J Med 2011; 124:359–68.[↩]
- Gan EC , Thamboo A, Rudmik L, Hwang PH, Ferguson BJ, Javer AR. Medical management of allergic fungal rhinosinusitis following endoscopic sinus surgery: an evidence-based review and recommendations. Int Forum Allergy Rhinol 2014; 4:702–15.[↩]
- Tsabouri S , Tseretopoulou X, Priftis K, Ntzani EE. Omalizumab for the treatment of inadequately controlled allergic rhinitis: a systematic review and meta-analysis of randomized clinical trials. J Allergy Clin Immunol Pract 2014; 2:332–40e1.[↩]
- Thanasumpun T , Batra PS. Oral antifungal therapy for chronic rhinosinusitis and its subtypes: a systematic review. Int Forum Allergy Rhinol 2011; 1:382–9.[↩]
- Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America, Clinical Infectious Diseases, Volume 63, Issue 4, 15 August 2016, Pages e1–e60, https://academic.oup.com/cid/article/63/4/e1/2595039[↩][↩]
- Caillot D , Couaillier JF, Bernard Aet al. . Increasing volume and changing characteristics of invasive pulmonary aspergillosis on sequential thoracic computed tomography scans in patients with neutropenia. J Clin Oncol 2001; 19:253–9.[↩]
- Liu Q , Lin R, Sun Jet al. . Antifungal agents for secondary prophylaxis based on response to initial antifungal therapy in allogeneic hematopoietic stem cell transplant recipients with prior pulmonary aspergillosis. Biol Blood Marrow Transplant 2014; 20:1198–203.[↩]