Contents
What is amenorrhea
Amenorrhea is the term used when a woman or adolescent girl is not having menstrual periods or absence of menstruation — one or more missed menstrual periods. Women who have missed at least three menstrual periods in a row have amenorrhea, as do girls who haven’t begun menstruation by age 15. Amenorrhea is not a disease, but it can be a symptom of another condition. A normal menstrual cycle typically occurs every 21 to 35 days 1. Consult your doctor if you’ve missed at least three menstrual periods in a row, or if you’ve never had a menstrual period and you’re age 15 or older.
Amenorrhea is often a sign of another health problem rather than a disease itself, and it can happen for many reasons. It can occur as a natural part of life with the most common cause of amenorrhea is pregnancy. Other causes of amenorrhea include problems with the reproductive organs or with the glands that help regulate hormone levels.
Women naturally stop menstruating during pregnancy, long-term breastfeeding (lactational amenorrhea) and menopause. Birth control pills and injections and hormone-containing IUDs cause amenorrhea in some women. A number of other conditions can cause secondary amenorrhea.
There are two types of amenorrhea:
- Primary amenorrhea: when a girl has not started having periods by age 15 (or within five years of the first signs of puberty)
- Secondary amenorrhea: when a girl or woman has been having periods but then stops having them for at least three months
Primary amenorrhea occurs when a girl has not had her first period by age 16. Secondary amenorrhea describes women who experience an absence of more than three menstrual cycles after having regular periods.
Having regular periods is an important sign of overall health. Missing a period, when not caused by pregnancy, breastfeeding, or menopause, is generally a sign of another health problem. If you miss your period, talk to your health care provider about possible causes, including pregnancy.
Missing a period is the main sign of amenorrhea.
Depending on the cause, a woman might have other signs or symptoms as well, such as:
- Excess facial hair
- Hair loss
- Headache
- Lack of breast development
- Milky discharge from the breasts
- Vision changes
Treatment of the underlying condition often resolves amenorrhea.
Who is at risk of amenorrhea?
According to the American Society for Reproductive Medicine, amenorrhea that is not caused by pregnancy, breastfeeding, or menopause occurs in a small percentage (less than 5%) of women during their lifetime.
The risk factors for amenorrhea include 2:
- Excessive exercise
- Obesity
- Eating disorders, such as anorexia nervosa
- A family history of amenorrhea or early menopause
- Genetics, such as having a change to the FMR1 gene, which also causes Fragile X syndrome 3
Primary amenorrhea
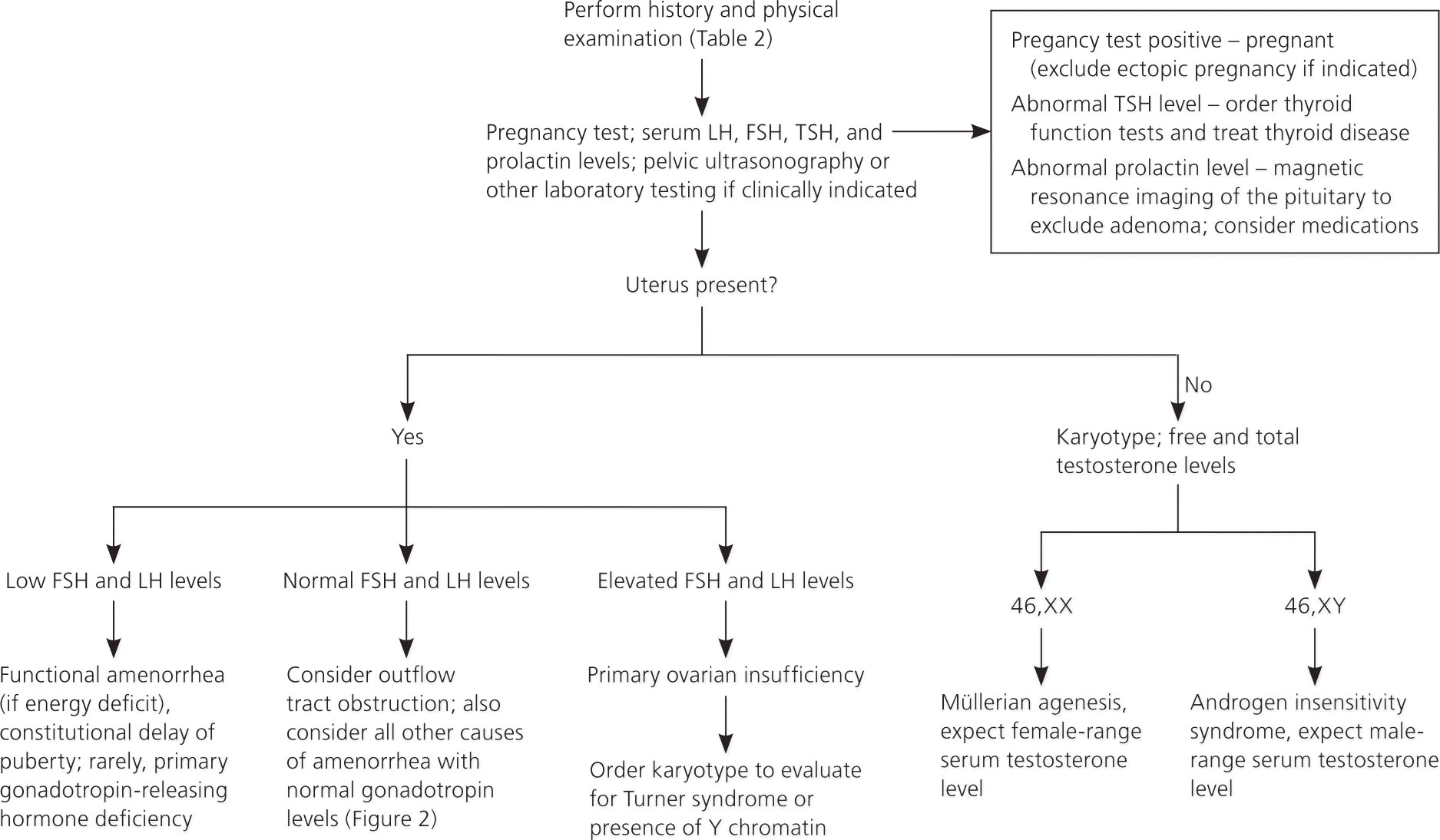
Primary amenorrhea, which by definition is failure to reach menarche (failure of menses to occur by age 16), is often the result of chromosomal irregularities leading to primary ovarian insufficiency (e.g., Turner syndrome) or anatomic abnormalities (e.g., Müllerian agenesis). Primary amenorrhea can result from two main causes:
- Chromosomal or genetic abnormalities can cause the ovaries to stop functioning normally. Turner syndrome, a condition caused by a partially or completely missing X chromosome, and androgen insensitivity syndrome, often characterized by high levels of testosterone, are two examples of genetic abnormalities that can delay or disrupt menstruation 4.
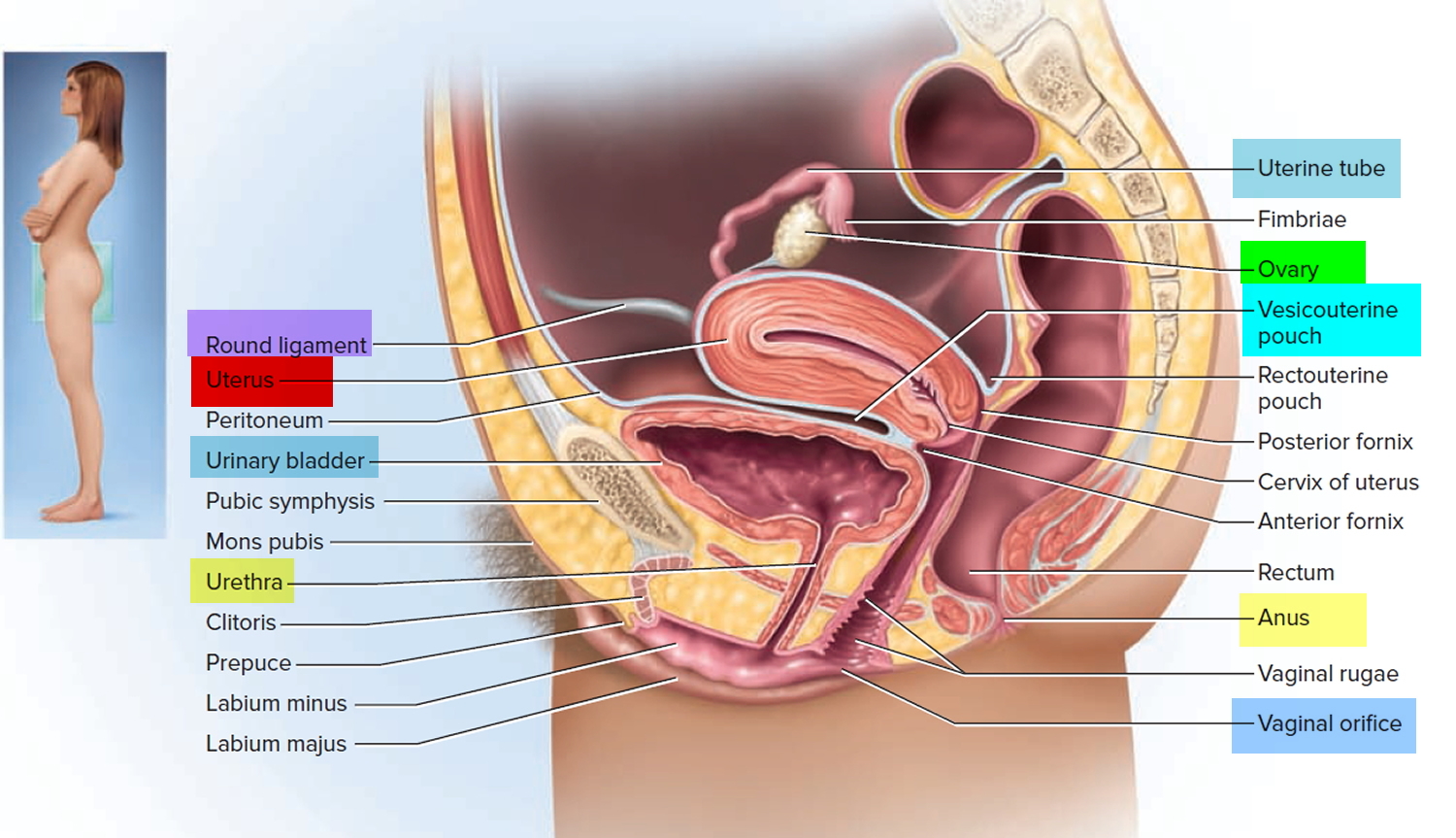
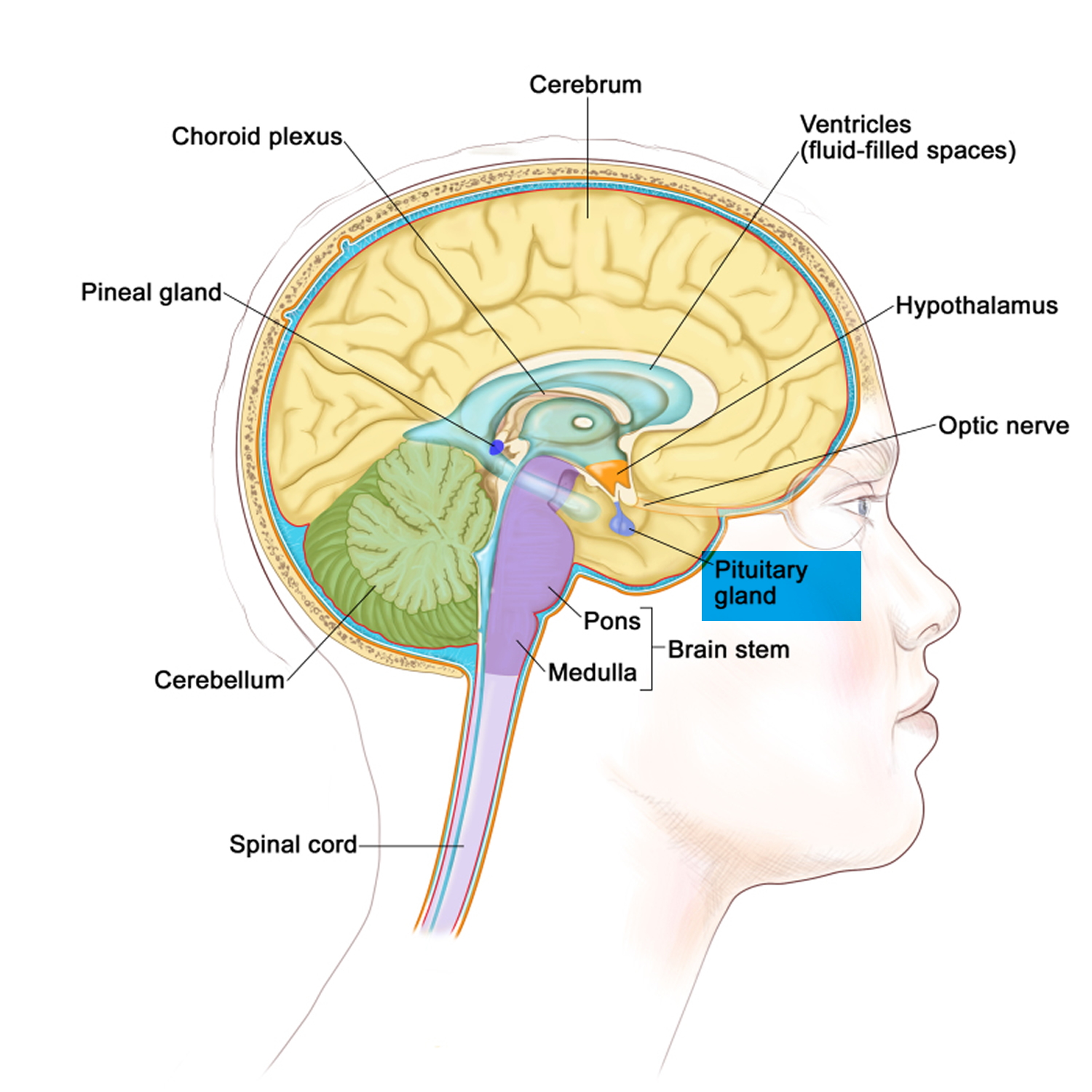
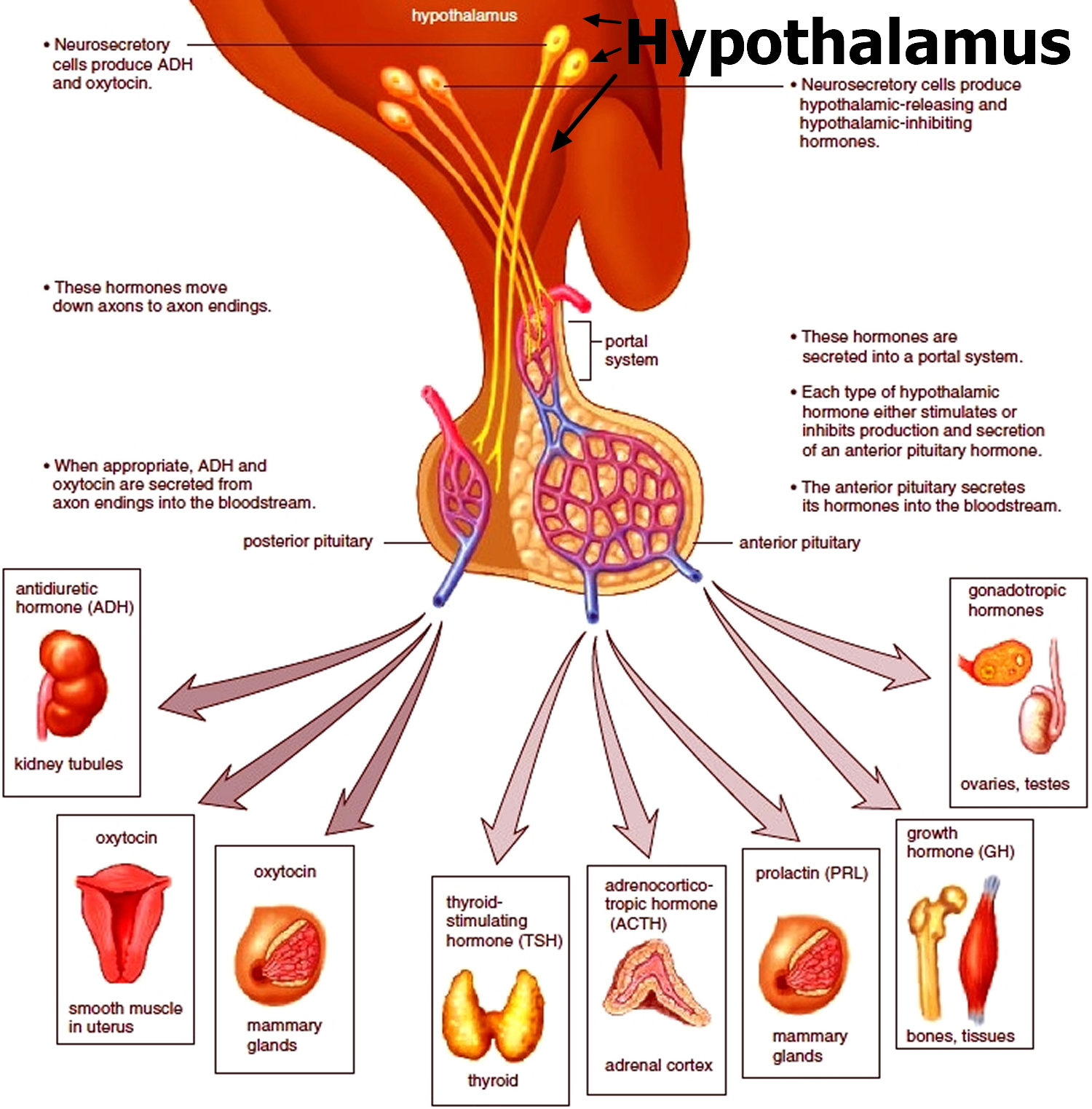
- Problems with the hypothalamus or pituitary gland in the brain can cause an imbalance of hormones that can prevent periods from starting. Conditions such as eating disorders, excessive exercise, and extreme physical or psychological stress or a combination of these factors can also disrupt the normal functioning of the hypothalamus or pituitary gland, delaying the onset of menstruation.
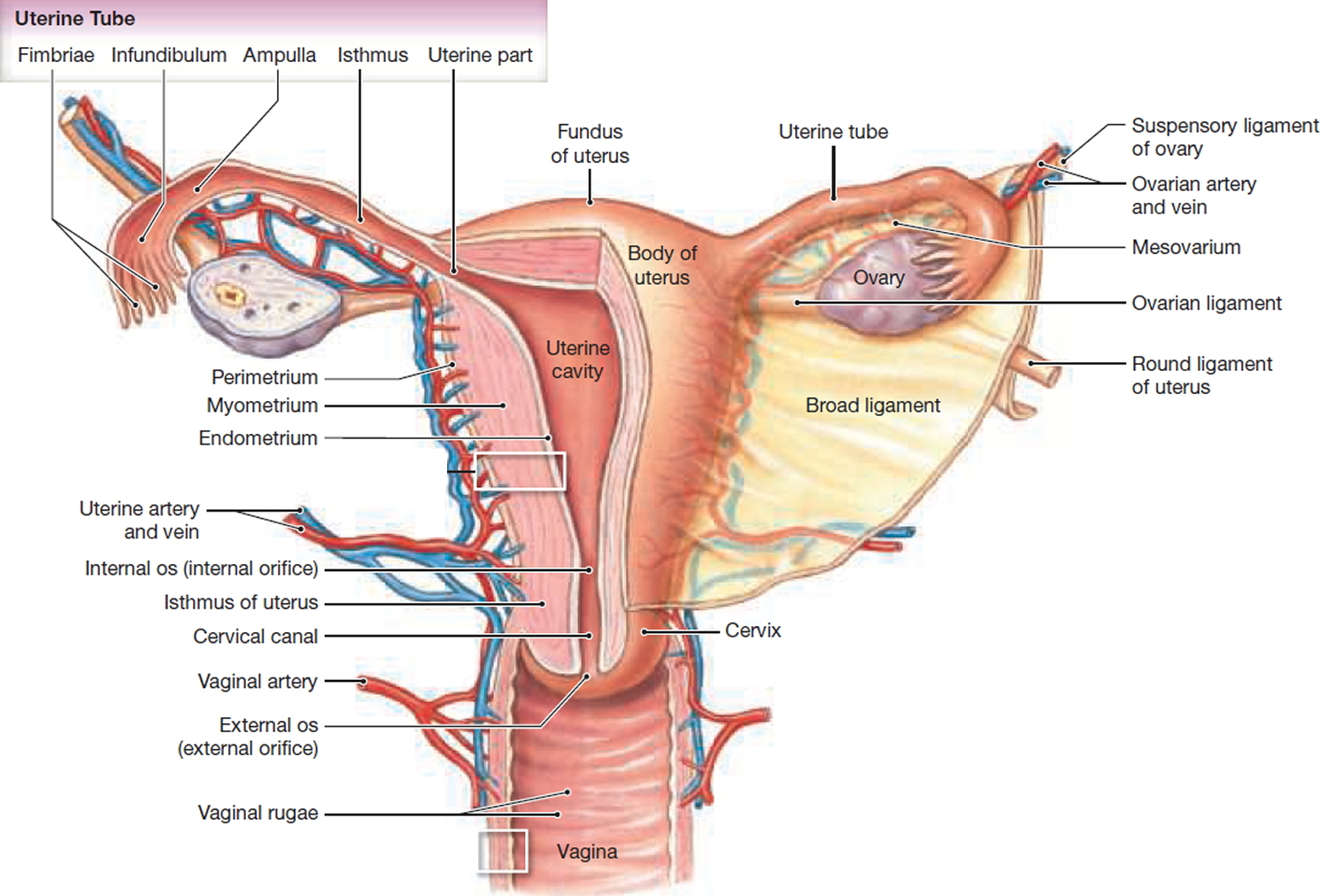
In rare cases, physical problems—such as missing reproductive organs or blockage of reproductive passageways—can also lead to primary amenorrhea. Missing portions of the reproductive tract can cause endocrine disruptions and may combine with hypothalamic or pituitary problems to prevent menstruation. Blockages may also prevent menstrual bleeding, making it seem like a girl has primary amenorrhea, even if her menstrual cycles are actually normal 5.
Figure 1. Uterus anatomy
Figure 2. Uterus location
Figure 3. Primary amenorrhea diagnosis
Secondary amenorrhea
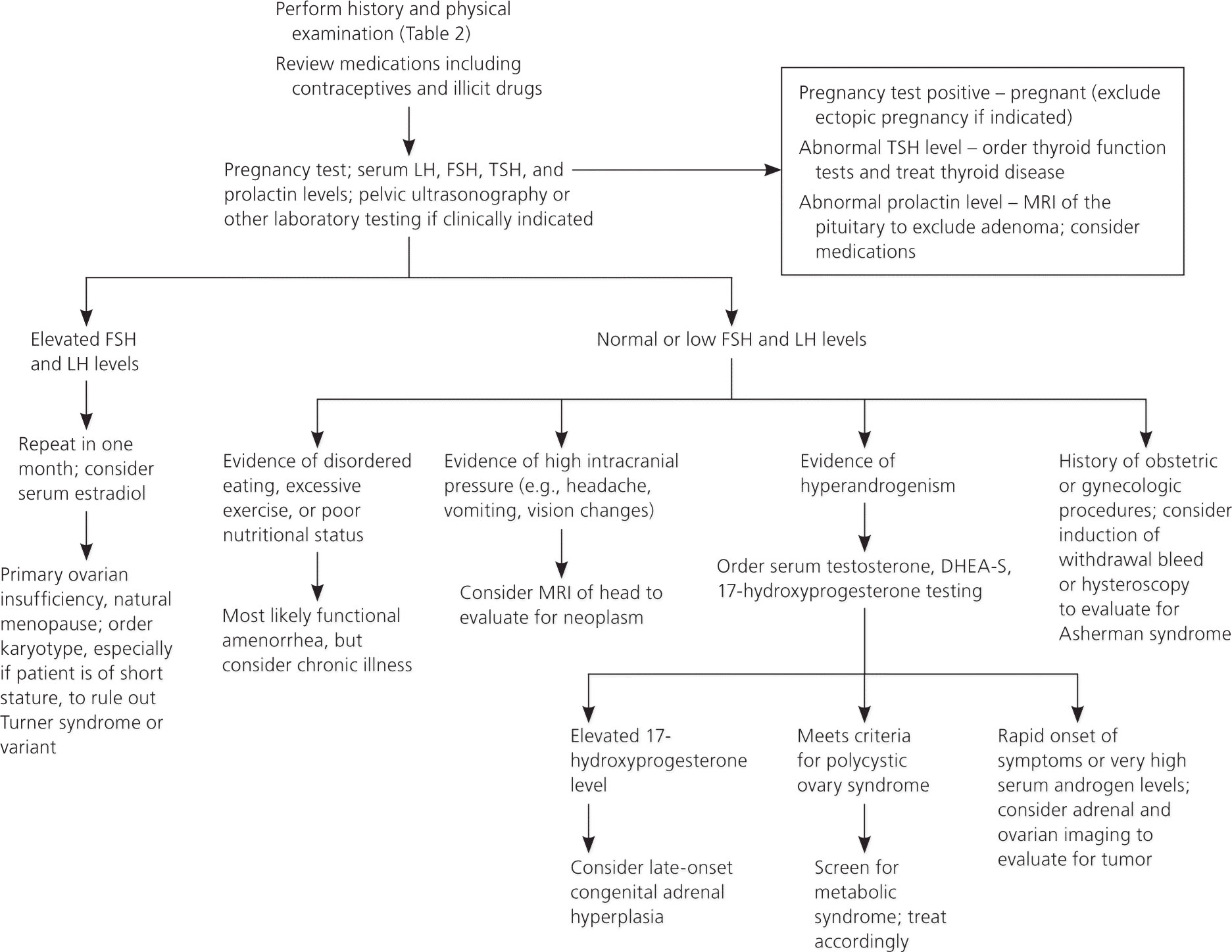
Secondary amenorrhea (missing three menstrual periods in a row or not having periods for at least 6 months after menstruating normally) can result from various causes.
Secondary amenorrhea causes
- Natural causes
- Pregnancy is the most common natural cause of secondary amenorrhea.
- Other physiologic causes include breastfeeding and menopause.
- Medications and therapies
- Certain birth control pills, injectable contraceptives, and hormonal intrauterine devices (IUDs) can cause amenorrhea. It can take a few months after stopping one of these types of birth control for the menstrual cycle to restart and become regular.
- Some medications, including certain antidepressants and blood pressure medications, can increase the levels of a hormone that prevents ovulation and the menstrual cycle 6.
- Chemotherapy and radiation treatments for hematologic cancer (including blood, bone marrow, and lymph nodes) and breast or gynecologic cancer can destroy estrogen-producing cells and eggs in the ovaries, leading to amenorrhea. The resulting amenorrhea may be short-term, especially in younger women 7.
- Sometimes scar tissue can build up in the lining of the uterus, preventing the normal shedding of the uterine lining in the menstrual cycle. This scarring sometimes occurs after a dilation and curettage (D&C), a procedure in which tissue is removed from the uterus to diagnose or treat heavy bleeding or to clear the uterine lining after a miscarriage 8, a cesarean section, or treatment for uterine fibroids.
- Hypothalamic amenorrhea. This condition occurs when the hypothalamus, a gland in the brain that regulates body processes, slows or stops releasing gonadotropin-releasing hormone (GnRH), the hormone that starts the menstrual cycle.7 Common characteristics of women with hypothalamic amenorrhea include 9:
- Low body weight
- Rapid weight loss (any cause)
- Low percentage of body fat
- Very low intake of calories or fat
- Eating disorders such as anorexia
- Malabsorption
- Emotional stress
- Strenuous exercise that burns more calories than are taken in through food
- Deficiency of leptin, a protein hormone that regulates appetite and metabolism
- Tumor of the hypothalamus
- Traumatic brain injury
- Infection (e.g., meningitis, tuberculosis, syphilis)
- Some medical conditions or illnesses
- Gonadotropin deficiency (e.g., Kallmann syndrome)
- Gynecological conditions, specifically those that lead to or result from hormone imbalances, may also have secondary amenorrhea as a main symptom.
- Polycystic ovary syndrome (PCOS). PCOS occurs when a woman’s body produces more androgens (a type of hormone) than normal. High levels of androgens can cause fluid-filled sacs or cysts to grow in the ovaries, interfering with the release of eggs (ovulation). Most women with polycystic ovary syndrome either have amenorrhea or experience irregular periods, called oligomenorrhea.
- Fragile X-associated primary ovarian insufficiency. The term fragile X-associated primary ovarian insufficiency describes a condition in which a woman’s ovaries stop functioning before normal menopause, sometimes around age 40. Fragile X-associated primary ovarian insufficiency results from certain changes to a gene on the X chromosome. Fragile X-associated primary ovarian insufficiency is fairly common among women who seek treatment for amenorrhea 7.
- Anatomic abnormalities / Outflow tract conditions
- Congenital
- Complete androgen resistance
- Imperforate hymen
- Müllerian agenesis
- Transverse vaginal septum
- Acquired
- Asherman syndrome (intrauterine synechiae)
- Cervical stenosis
- Congenital
- Thyroid problems. The thyroid is a small butterfly-shaped gland at the base of the neck, just below the Adam’s apple. The thyroid produces hormones that control metabolism and play a role in puberty and menstruation 10. A thyroid gland that is overactive (called hyperthyroidism) or underactive (hypothyroidism) can cause menstrual irregularities, including amenorrhea 11.
- Pituitary tumors. The pituitary gland in the brain regulates the production of hormones that affect many body functions, including metabolism and the reproductive cycle. Tumors on the pituitary gland – increased prolactin by a small benign tumor (prolactinoma) are usually noncancerous (benign) but can interfere with the body’s hormonal regulation of menstruation 11.
- Pituitary disorders
- Pituitary damage / radiation to the head
- Autoimmune disease
- Cocaine
- Cushing syndrome
- Empty sella syndrome
- Hyperprolactinemia
- Infiltrative disease (e.g., sarcoidosis)
- Medications:
- Antidepressants
- Antihistamines
- Antihypertensives
- Antipsychotics
- Opiates
- Other pituitary or central nervous system tumor
- Sheehan syndrome
- Primary ovarian insufficiency/premature ovarian failure. Primary ovarian insufficiency, also called premature ovarian failure (menopause before age 40) can be caused by:
- Congenital
- Gonadal dysgenesis (other than Turner syndrome)
- Turner syndrome or variant
- Acquired
- Damage to the ovaries from chemotherapy or radiation
- Autoimmune destruction
- Congenital
- Other endocrine gland disorders
- Adrenal disease
- Adult-onset adrenal hyperplasia
- Androgen-secreting tumor
- Chronic disease
- Constitutional delay of puberty
- Cushing syndrome
- Ovarian tumors (androgen producing)
- Polycystic ovary syndrome (multifactorial)
- Thyroid disease
Figure 4. The pituitary gland location
Figure 5. The hypothalamus and pituitary gland (anterior and posterior) endocrine pathways and target organs
Figure 6. Secondary amenorrhea diagnosis
Amenorrhea causes
What causes amenorrhea
There are a number of reasons why your periods can stop.
The most common reasons for amenorrhea are:
Natural amenorrhea
During the normal course of your life, you may experience amenorrhea for natural reasons, such as:
- Pregnancy
- Breast-feeding
- Menopause
Contraceptives
Some women who take birth control pills may not have periods. Even after stopping oral contraceptives, it may take some time before regular ovulation and menstruation return. Contraceptives that are injected or implanted also may cause amenorrhea, as can some types of intrauterine devices.
Medications
Certain medications can cause menstrual periods to stop, including some types of:
- Antipsychotics
- Cancer chemotherapy
- Antidepressants
- Blood pressure drugs
- Allergy medications
Lifestyle factors
Sometimes lifestyle factors contribute to amenorrhea, for instance:
- Low body weight. Excessively low body weight — about 10 percent under normal weight — interrupts many hormonal functions in your body, potentially halting ovulation. Women who have an eating disorder, such as anorexia or bulimia, often stop having periods because of these abnormal hormonal changes.
- Excessive exercise. Women who participate in activities that require rigorous training, such as ballet, may find their menstrual cycles interrupted. Several factors combine to contribute to the loss of periods in athletes, including low body fat, stress and high energy expenditure.
- Stress. Mental stress can temporarily alter the functioning of your hypothalamus — an area of your brain that controls the hormones that regulate your menstrual cycle. Ovulation and menstruation may stop as a result. Regular menstrual periods usually resume after your stress decreases.
Hormonal imbalance
Many types of medical problems can cause hormonal imbalance, including:
- Polycystic ovary syndrome (PCOS). PCOS causes relatively high and sustained levels of hormones, rather than the fluctuating levels seen in the normal menstrual cycle.
- Thyroid malfunction. An overactive thyroid gland (hyperthyroidism) or underactive thyroid gland (hypothyroidism) can cause menstrual irregularities, including amenorrhea.
- Pituitary tumor. A noncancerous (benign) tumor in your pituitary gland can interfere with the hormonal regulation of menstruation.
- Premature menopause. Menopause usually begins around age 50. But, for some women, the ovarian supply of eggs diminishes before age 40, and menstruation stops.
Structural problems
Problems with the sexual organs themselves also can cause amenorrhea. Examples include:
- Uterine scarring. Asherman’s syndrome, a condition in which scar tissue builds up in the lining of the uterus, can sometimes occur after a dilation and curettage (D&C), cesarean section or treatment for uterine fibroids. Uterine scarring prevents the normal buildup and shedding of the uterine lining.
- Lack of reproductive organs. Sometimes problems arise during fetal development that lead to a girl being born without some major part of her reproductive system, such as her uterus, cervix or vagina. Because her reproductive system didn’t develop normally, she can’t have menstrual cycles.
- Structural abnormality of the vagina. An obstruction of the vagina may prevent visible menstrual bleeding. A membrane or wall may be present in the vagina that blocks the outflow of blood from the uterus and cervix.
Periods can also sometimes stop as a result of a long-term medical condition, such as heart disease, uncontrolled diabetes, an overactive thyroid, or premature ovarian failure.
Anatomic abnormalities
Müllerian agenesis, a condition characterized by a congenital malformation of the genital tract, may present with normal breast development without menarche, and may be associated with urinary tract defects and fused vertebrae 12. Other congenital abnormalities that may cause amenorrhea include imperforate hymen and transverse vaginal septum. In these conditions, products of menstruation accumulate behind the defect and can lead to cyclic or acute pelvic pain. Physical examination, as well as ultrasonography or MRI, is key to diagnosis, and surgical correction is usually warranted 12.
Rare causes of amenorrhea include complete androgen insensitivity syndrome, which is characterized by normal breast development, sparse or absent pubic and axillary hair, and a blind vaginal pouch; and 5-alpha reductase deficiency, which is characterized by partially virilized genitalia.1 In these conditions, serum testosterone levels will be in the same range as those found in males of the same age 13. The karyotype will be 46,XY, and testicular tissue should be removed to avoid malignant transformation 14.
A structural cause of secondary amenorrhea is Asherman syndrome: intrauterine synechiae caused by uterine instrumentation during gynecologic or obstetric procedures, which can be evaluated and treated with hysteroscopy 15.
Hypothalamic and pituitary causes
The ovaries require physiologic stimulation by pituitary gonadotropins for appropriate follicular development and estrogen production. Functional hypothalamic amenorrhea occurs when the hypothalamic-pituitary-ovarian axis is suppressed due to an energy deficit stemming from stress, weight loss (independent of original weight), excessive exercise, or disordered eating 16. It is characterized by a low estrogen state without other organic or structural disease. Laboratory tests usually reveal low or low-normal levels of serum follicle-stimulating hormone, luteinizing hormone, and estradiol; however, these levels can fluctuate, and the clinical context is the discriminating factor 16. Patients with functional amenorrhea may demonstrate the features of the female athlete triad, which consists of insufficient caloric intake with or without an eating disorder, amenorrhea, and low bone density or osteoporosis 17. These patients should be screened for eating disorders, diets, and malabsorption syndromes (e.g., celiac disease) 18.
Treatment of functional hypothalamic amenorrhea involves nutritional rehabilitation as well as reductions in stress and exercise levels 16. Menses typically return after correction of the underlying nutritional deficit 19. Bone loss is best treated by reversal of the underlying process, and the patient should undergo bone density evaluation and take calcium and vitamin D supplements 16. Although the bone loss is partly secondary to estrogen deficiency, estrogen replacement without nutritional rehabilitation does not reverse the bone loss. Combined OCs will restore menses, but will not correct bone density 16. Leptin administration has been reported to restore pulsatility of gonadotropin-releasing hormone and ovulation in these patients, but its effect on bone health is unknown 16. The effect of bisphosphonates on long-term bone health in premenopausal women is unclear, as is their teratogenic potential 16.
Pregnancy
You might be pregnant if you’re sexually active and your period is late. Pregnancy is a common reason why periods unexpectedly stop. It can sometimes happen if the contraception you’re using fails.
It might be that your period is simply late, so you could wait a few days to see if it arrives. If it doesn’t arrive, you can do a pregnancy test to confirm whether or not you’re pregnant.
It’s important to be aware that you can get pregnant in the days after your period is normally due. This can happen if the release of an egg (ovulation) is delayed – for example, as a result of illness or stress.
Stress
If you’re stressed, your menstrual cycle can become longer or shorter, your periods may stop altogether, or they might become more painful.
Try to avoid becoming stressed by making sure you have time to relax. Regular exercise, such as running, swimming and yoga, can help you relax. Breathing exercises can also help.
If you’re finding it hard to cope with stress, cognitive behavioral therapy (CBT) may be recommended. Cognitive behavioral therapy is a talking therapy that can help you manage your problems by changing the way you think and act.
Sudden weight loss
Excessive or sudden weight loss can cause your periods to stop. Severely restricting the amount of calories you eat stops the production of hormones needed for ovulation.
Your doctor may refer you to a dietitian if you’re underweight, where you have a body mass index (BMI) of less than 18.5. The dietitian will be able to advise you about how to regain weight safely.
If your weight loss is caused by an eating disorder, such as anorexia, you’ll be referred to a psychiatrist.
Being overweight or obese
Being overweight or obese can also affect your menstrual cycle. If you’re overweight, your body may produce an excess amount of estrogen, one of the hormones that regulate the reproductive system in women.
The excess estrogen can affect how often you have periods, and can also cause your periods to stop.
Your doctor may refer you to a dietitian if you’re overweight or obese, with a BMI of 30 or more, and it’s affecting your periods. The dietitian will be able to advise you about losing weight safely.
Extreme overexercising
The stress that intense physical activity places on your body can affect the hormones responsible for your periods. Losing too much body fat through intense exercise can also stop you ovulating.
You’ll be advised to reduce your level of activity if excessive exercise has caused your periods to stop.
If you’re a professional athlete, you may benefit from seeing a doctor who specializes in sports medicine. They’ll be able to give you advice about how to maintain your performance without disrupting your periods.
Contraceptive pill
You might miss a period every so often if you’re taking the contraceptive pill. This isn’t usually a cause for concern.
Some types of contraception, such as the progestogen-only pill, contraceptive injection and intrauterine system (IUS), particularly Mirena, can cause periods to stop altogether.
However, your periods should return when you stop using these types of contraception.
Menopause
You may start missing periods as you approach the menopause. This is because estrogen levels will start to decrease, and ovulation will become less regular. After the menopause, your periods will stop completely.
The menopause is a natural part of the ageing process in women, which usually occurs between the ages of 45 and 55. The average age for a woman to reach the menopause is 50 in the US.
However, around 1 in 100 women experience the menopause before the age of 40. This is known as premature menopause or premature ovarian failure.
Polycystic ovary syndrome (PCOS)
Polycystic ovaries contain a large number of harmless follicles, which are underdeveloped sacs in which eggs develop. If you have PCOS, these sacs are often unable to release an egg, which means ovulation doesn’t take place. Polycystic ovary syndrome (PCOS) is a multifactorial endocrine disorder, usually involving peripheral insulin resistance. It is characterized by hyperandrogenism found on clinical or laboratory examination, polycystic ovaries as suggested by ultrasonography, and ovulatory dysfunction.
PCOS is thought to be very common, affecting about 1 in every 10 women in the US. The condition is responsible for as many as one in three cases of stopped periods.
The Rotterdam Consensus Criteria published in 2003 require the presence of two of the three above conditions for diagnosis, whereas the Androgen Excess Society’s 2006 guidelines require hyperandrogenism and either of the remaining two conditions 20. In polycystic ovary syndrome (PCOS), serum androgen levels are typically no greater than twice the upper limit of normal. Thus, higher levels suggest other causes of hyperandrogenism 21.
With insulin resistance contributing to the underlying pathology of PCOS, patients should be screened for dyslipidemia and overall cardiovascular risk. Glucose intolerance should be assessed with a fasting glucose and two-hour glucose tolerance test, because patients may have insulin resistance and beta-cell dysfunction 18. In patients with PCOS who are overweight, weight loss combined with exercise is the first-line treatment 22. Chronic anovulation with resultant unopposed estrogen secretion is a risk factor for endometrial cancer, and low-dose combined oral contraceptives are more frequently prescribed to reduce this risk than higher-dose pills or progestin-only methods 22. Many combined OCs suppress the secretion of ovarian androgen and may be useful in decreasing hirsutism and acne, although data are limited 22. Metformin (Glucophage) can increase insulin sensitivity, thereby improving glucose tolerance. It may also improve ovulation rate, reduce the incidence of menstrual abnormalities, and improve serum androgen concentrations 22.
Primary ovarian insufficiency/premature ovarian failure
Primary ovarian insufficiency, also called premature ovarian failure (menopause before age 40) can be caused by:
- Abnormal chromosomes
- Immune disorders
- Damage to the ovaries from chemotherapy or radiation
Primary ovarian insufficiency, a condition characterized by follicle depletion or dysfunction leading to a continuum of impaired ovarian function, is suggested by a concentration of follicle-stimulating hormone in the menopausal range (per reference laboratory), confirmed on two occasions separated by one month, and diagnosed in patients younger than 40 years with amenorrhea or oligomenorrhea.6 Other terms, including premature ovarian failure, are used synonymously with primary ovarian insufficiency 23. Up to 1% of women may experience primary ovarian insufficiency. This condition differs from menopause, in which the average age is 50 years, because of age and less long-term predictability in ovarian function 23. More than 90% of cases unrelated to a syndrome are idiopathic, but they can be attributed to radiation, chemotherapeutic agents, infection, tumor, empty sella syndrome, or an autoimmune or infiltrative process 23.
Patients with primary ovarian insufficiency should be counseled about possible fertility, because up to 10% of such patients may achieve temporary and unpredictable remission 24. Hormone therapy (e.g., 100 mcg of daily transdermal estradiol or 0.625 mg of daily conjugated equine estrogen [Premarin] on days 1 through 26 of the menstrual cycle, and 10 mg of cyclic medroxyprogesterone acetate for 12 days [e.g., days 14 through 26] of the menstrual cycle 24 until the average age of natural menopause is usually recommended to decrease the likelihood of osteoporosis, ischemic heart disease, and vasomotor symptoms 25. Combined oral contraceptives deliver higher concentrations of estrogen and progesterone than necessary for hormone therapy, may confer thromboembolic risk, and may theoretically be ineffective at suppressing follicle-stimulating hormone for contraceptive purposes in this population; thus, a barrier method or intrauterine device is appropriate in sexually active patients. For optimal bone health, patients with primary ovarian insufficiency should be advised to perform weightbearing exercises and supplement calcium (e.g., 1,200 mg daily) and vitamin D3 (e.g., 800 IU daily) intake 23.
There is evidence of genetic predisposition to primary ovarian insufficiency, and patients without evidence of a syndrome should be tested for FMR1 gene premutation (confers risk of fragile X syndrome in their offspring) and thyroid and adrenal autoantibodies 23.
Turner syndrome, a condition characterized by a chromosomal pattern of 45,X or a variant, can present with a classic phenotype including a webbed neck, a low hairline, cardiac defects, and lymphedema 26. Some patients who have Turner syndrome have only short stature and variable defects in ovarian function (even with possible fertility) 23. Thus, all patients with short stature and amenorrhea should have a karyotype analysis 26. Because patients require screening for a number of systemic problems, including coarctation of the aorta, other cardiac lesions, renal abnormalities, hearing problems, and hypothyroidism, and because they may require human growth hormone treatment and hormone replacement therapy, physicians inexperienced with Turner syndrome should consult an endocrinologist 26.
Elevations in serum prolactin
Prolactin levels can be elevated because of medications, pituitary adenoma, hypothyroidism, or mass lesion compromising normal hypothalamic inhibition 27. Elevated prolactin levels, whatever the cause, inhibit the secretion and effect of gonadotropins, and warrant MRI of the pituitary. Exceptions may occur in cases with a clear pharmacologic trigger and relatively low levels of serum prolactin (i.e., < 100 ng per mL [< 100 mcg per L]) 27. Treatment of prolactinomas may involve dopamine agonists or surgical resection 27.
Risk factors for amenorrhea
Factors that may increase your risk of amenorrhea may include:
- Family history. If other women in your family have experienced amenorrhea, you may have inherited a predisposition for the problem.
- Eating disorders. If you have an eating disorder, such as anorexia or bulimia, you are at higher risk of developing amenorrhea.
- Athletic training. Rigorous athletic training can increase your risk of amenorrhea.
Amenorrhea symptoms
Symptoms vary according to the cause. Women can have hot flashes, discharge of milk from the nipples, vaginal dryness, headaches, and vision changes. Some women develop acne and grow hair on the face and body. Many women have no symptoms other than the lack of periods.
Depending on the cause of amenorrhea, you might experience other signs or symptoms along with the absence of periods, such as:
- Milky nipple discharge
- Hair loss
- Headache
- Vision changes
- Excess facial hair
- Pelvic pain
- Acne
Amenorrhea complications
Complications of amenorrhea may include:
- Infertility. If you don’t ovulate and have menstrual periods, you can’t become pregnant.
- Osteoporosis. If your amenorrhea is caused by low estrogen levels, you may also be at risk of osteoporosis — a weakening of your bones.
Amenorrhea diagnosis
During your appointment, your doctor will perform a pelvic exam to check for any problems with your reproductive organs. If you’ve never had a period, your doctor may examine your breasts and genitals to see if you’re experiencing the normal changes of puberty.
Amenorrhea can be a sign of a complex set of hormonal problems. Finding the underlying cause can take time and may require more than one kind of testing.
Lab tests
A variety of blood tests may be necessary, including:
- Pregnancy test. This will probably be the first test your doctor suggests, to rule out or confirm a possible pregnancy.
- Thyroid function test. This test measures the amount of thyroid-stimulating hormone (TSH) in your blood, which can help determine if your thyroid is working properly. A thyroid gland that is overactive (hyperthyroidism) or underactive (hypothyroidism) can cause menstrual irregularities, including amenorrhea.
- Prolactin test. Low levels of the hormone prolactin may be a sign of a pituitary gland tumor.
- Ovary function test. This test measures the amount of follicle-stimulating hormone (FSH) or luteinizing hormone (LH)—hormones made by the pituitary gland—in your blood to determine if your ovaries are working properly. Your health care provider may also evaluate the level of anti-Mullerian hormone (AMH), which is produced by the ovarian follicles. Higher levels of anti-Mullerian hormone may be associated with polycystic ovary syndrome (PCOS) 28. Low or undetectable amounts of anti-Mullerian hormone may be associated with menopause or primary ovarian insufficiency.
- Androgen test / Male hormone test. Androgens are sometimes called “male hormones” because men need higher levels of these hormones than woman do for overall health. However, both men and women need androgens to stay healthy. If you’re experiencing increased facial hair and a lowered voice, your doctor may want to check the level of male hormones in your blood. High levels of androgens may indicate a woman has PCOS.
- Hormone challenge test. With this test, you will take a hormonal medication for seven to 10 days in an effort to trigger a menstrual cycle. Results from the test can tell your health care provider whether your periods have stopped because of a lack of estrogen.
- Screening for a premutation of the FMR1 gene. Changes in this gene can cause the ovaries to stop functioning properly, leading to amenorrhea 29.
- Chromosome evaluation. This test, also known as a karyotype, involves counting and evaluating the chromosomes from cells in the body to identify any missing, extra, or rearranged cells. Results from this evaluation can help determine the cause of the chromosomal abnormality causing primary or secondary amenorrhea.
- Ultrasound. This painless test uses sound waves to produce images of internal organs. This test can help determine if your reproductive organs are all present and shaped normally.
- Computerized tomography (CT). CT scans combine many X-ray images taken from different directions to create cross-sectional views of internal structures. A CT scan can indicate whether your uterus, ovaries, and kidneys look normal.
- Magnetic resonance imaging (MRI). MRI uses radio waves with a strong magnetic field to produce detailed images of soft tissues within the body. Your health care provider may order an MRI to check for a pituitary tumor or to examine your reproductive organs.
- Hysteroscopy. In this procedure a thin, lighted camera is passed through your vagina and cervix to allow your health care provider to look at the inside of your vagina, cervix and uterus.
Your health care provider might use several of these tests to attempt to diagnose the cause of amenorrhea. In some cases, no specific cause for the amenorrhea can be found. This situation is called idiopathic amenorrhea 30.
Amenorrhea treatment
Treatment depends on the underlying cause of your amenorrhea. In some cases, contraceptive pills or other hormone therapies can restart your menstrual cycles. For example, if the cause is PCOS, you may be advised to take the contraceptive pill or tablets containing a hormone called progesterone. Amenorrhea caused by thyroid or pituitary disorders may be treated with medications. If you have an overactive thyroid gland, you may be given medication to stop your thyroid gland producing too many hormones. If a tumor or structural blockage is causing the problem, surgery may be necessary.
If the cause is early menopause (premature ovarian failure), this means the ovaries no longer function normally. Hormone medication is usually recommended. Treatments to try include the contraceptive pill or hormone replacement therapy (HRT).
If primary or secondary amenorrhea is caused by lifestyle factors, your health care provider may suggest changes in the areas below:
- Weight. Being overweight or severely underweight can affect your menstrual cycle. Attaining and maintaining a healthy weight often helps balance hormone levels and restore your menstrual cycle.
- Stress. Assess the areas of stress in your life and reduce the things that are causing stress. If you can’t decrease stress on your own, ask for help from family, friends, your health care provider, or a professional listener such as a counselor.
- Level of physical activity. You may need to change or adjust your physical activity level to help restart your menstrual cycle. Talk to your health care provider and your coach or trainer about how to train in a way that maintains your health and menstrual cycles.
Be aware of changes in your menstrual cycle and check with your health care provider if you have concerns. Keep a record of when your periods occur. Note the date your period starts, how long it lasts, and any problems you experience. The first day of bleeding is considered the first day of your menstrual cycle.
Treatments for Primary Amenorrhea
For primary amenorrhea, depending on your age and the results of the ovary function test, health care providers may recommend watchful waiting. If an ovary function test shows low follicle-stimulating hormone (FSH) or luteinizing hormone (LH) levels, menstruation may just be delayed. In females with a family history of delayed menstruation, this kind of delay is common 2.
Primary amenorrhea caused by chromosomal or genetic problems may require surgery. Women with a genetic condition called 46, XY gonadal dysgenesis have one X and one Y chromosome, but their ovaries do not develop normally. This condition increases the risk for cancer developing in the ovaries. The gonads (ovaries) are often removed through laparoscopic surgery to prevent or reduce the risk of cancer 31.
Medical Treatments for Secondary Amenorrhea
Common medical treatments for secondary amenorrhea include 5:
- Birth control pills or other types of hormonal medication. Certain oral contraceptives may help restart the menstrual cycle.
- Medications to help relieve the symptoms of PCOS. Clomiphene citrate therapy is often prescribed to help trigger ovulation 32.
- Estrogen replacement therapy. Estrogen replacement therapy may help balance hormonal levels and restart the menstrual cycle in women with primary ovarian insufficiency or Fragile X-associated primary ovarian insufficiency 33. Women with Fragile X-associated primary ovarian insufficiency often experience symptoms of menopause, such as hot flashes and night sweats. Estrogen replacement therapy replaces the estrogen a woman’s body should be making naturally for a normal menstrual cycle. In addition, estrogen replacement therapy may help women with Fragile X-associated primary ovarian insufficiency lower their risk for the bone disease osteoporosis 34. Estrogen replacement therapy can increase the risk for uterine cancer, so your health care provider may also prescribe progestin or progesterone to reduce this risk.
In general, medications are safe, but they can have side effects, some of which may be serious. You should discuss side effects and risks with your health care provider before deciding on any specific medical treatment.
Surgical Treatments for Secondary Amenorrhea
Surgical treatment for amenorrhea is not common, but may be recommended in certain conditions. These include:
- Uterine scarring. This scarring sometimes occurs after removal of uterine fibroids, a cesarean section, or a dilation and curettage (D&C), a procedure in which tissue is removed from the uterus to diagnose or treat heavy bleeding or to clear the uterine lining after a miscarriage 8. Removal of the scar tissue during a procedure called a hysteroscopic resection can help restore the menstrual cycle 35.
- Pituitary tumor. Medications may be recommended to shrink the tumor. If this does not work, surgery may be necessary to remove the tumor. Pituitary tumors are not cancerous, but they can cause problems as they grow. Pituitary tumors can put pressure on surrounding blood vessels and nerves such as the optic nerve and may result in loss of vision. Most of the time, pituitary tumors are removed through the nose and sinuses. Radiation therapy may be used to shrink the tumor, either in combination with surgery or, for those who cannot have surgery, by itself.
- Speroff L, Fritz MA. Clinical Gynecologic Endocrinology and Infertility. 7th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins: 2005:401–464.[↩]
- Master-Hunter, T., & Heiman, D. L. (2006). Amenorrhea: Evaluation and treatment. American Family Physician, 73, 1374–1382. https://www.aafp.org/afp/2006/0415/p1374.html[↩][↩]
- Practice Committee of the American Society for Reproductive Medicine (PC-ASRM). (2008). Current evaluation of amenorrhea. Fertility and Sterility, 90, S219–225. https://www.asrm.org/globalassets/asrm/asrm-content/news-and-publications/practice-guidelines/for-non-members/current_evaluation_of_amenorrhea-pdfnoprint.pdf[↩]
- Pascal, P., Leprieur, E., Zenaty, D., Thibaud, E., Polak, M., Frances, A. M., et al. (2010). Steroidogenic factor-1 (SF-1) gene mutation as a frequent cause of primary amenorrhea in 46,XY female adolescents with low testosterone concentration. Reproductive Biology and Endocrinology, 8, 28.[↩]
- American College of Obstetricians and Gynecologists (ACOG) Committee on Practice Bulletins—Gynecology. (2013). Practice bulletin no. 136: Management of abnormal uterine bleeding associated with ovulatory dysfunction. Obstetrics and Gynecology, 122(1), 176–185.[↩][↩]
- La Torre, D., & Falorni, A. (2007). Pharmacological causes of hyperprolactinemia. Therapeutic and Clinical Risk Management, 3, 929–951. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2376090/[↩]
- ACOG. (2014). ACOG Committee Opinion: Primary ovarian insufficiency in the adolescent. https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Adolescent-Health-Care/Primary-Ovarian-Insufficiency-in-Adolescents-and-Young-Women[↩][↩]
- ACOG. (2016). Dilation and curettage. https://www.acog.org/~/media/For Patients/faq062.pdf[↩][↩]
- Hormone Health Network. (2017). Amenorrhea. https://www.hormone.org/diseases-and-conditions/womens-health/amenorrhea[↩]
- U.S. Department of Health and Human Services Office of Women’s Health. (2015). Thyroid disease fact sheet. https://www.womenshealth.gov/a-z-topics/thyroid-disease[↩]
- Master-Hunter, T., & Heiman, D. L. (2006). Amenorrhea: Evaluation and treatment. American Family Physician,73, 1374–1382. http://www.aafp.org/afp/2006/0415/p1374.html[↩][↩]
- Folch M, Pigem I, Konje JC. Müllerian agenesis: etiology, diagnosis, and management. Obstet Gynecol Surv. 2000;55(10):644–649.[↩][↩]
- Maimoun L, Philibert P, Bouchard P, et al. Primary amenorrhea in four adolescents revealed 5α-reductase deficiency confirmed by molecular analysis. Fertil Steril. 2011;95(2):804.e1–e5.[↩]
- Capito C, Leclair MD, Arnaud A, et al. 46,XY pure gonadal dysgenesis: clinical presentations and management of the tumor risk. J Pediatr Urol. 2011;7(1):72–75[↩]
- Yu D, Wong YM, Cheong Y, Xia E, Li TC. Asherman syndrome—one century later. Fertil Steril. 2008;89(4):759–779.[↩]
- Gordon CM. Clinical practice. Functional hypothalamic amenorrhea. N Engl J Med. 2010;363(4):365–371.[↩][↩][↩][↩][↩][↩][↩]
- Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP; American College of Sports Medicine. American College of Sports Medicine position stand. The female athlete triad. Med Sci Sports Exerc. 2007;39(10):1867–1882.[↩]
- Practice Committee of American Society for Reproductive Medicine. Current evaluation of amenorrhea. Fertil Steril. 2008;90(5 suppl):S219–S225.[↩][↩]
- Falsetti L, Gambera A, Barbetti L, Specchia C. Long-term follow-up of functional hypothalamic amenorrhea and prognostic factors. J Clin Endocrinol Metab. 2002;87(2):500–505.[↩]
- Azziz R, Carmina E, Dewailly D, et al.; Androgen Excess Society. Positions statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. J Clin Endocrinol Metab. 2006;91(11):4237–4245.[↩]
- d’Alva CB, Abiven-Lepage G, Viallon V, et al. Sex steroids in androgen-secreting adrenocortical tumors: clinical and hormonal features in comparison with nontumoral causes of androgen excess. Eur J Endocrinol. 2008;159(5):641–647.[↩]
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 108: polycystic ovary syndrome. Obstet Gynecol. 2009;114(4):936–949.[↩][↩][↩][↩]
- Nelson LM. Clinical practice. Primary ovarian insufficiency. N Engl J Med. 2009;360(6):606–614.[↩][↩][↩][↩][↩][↩]
- van Kasteren YM, Schoemaker J. Premature ovarian failure: a systematic review on therapeutic interventions to restore ovarian function and achieve pregnancy. Hum Reprod Update. 1999;5(5):483–492.[↩][↩]
- Welt CK. Primary ovarian insufficiency: a more accurate term for premature ovarian failure. Clin Endocrinol (Oxf). 2008;68(4):499–509.[↩]
- Sybert VP, McCauley E. Turner’s syndrome. N Engl J Med. 2004;351(12):1227–1238.[↩][↩][↩]
- Pickett CA. Diagnosis and management of pituitary tumors: recent advances. Prim Care. 2003;30(4):765–789.[↩][↩][↩]
- Visser, J., de Jong, F. H., Laven, J., & Themmen, A. (2006). Anti-Mullerian hormone: A new marker for ovarian function. Reproduction, 139, 1–9. http://www.reproduction-online.org/content/131/1/1.long[↩]
- NIH. (2008). NIH research plan on Fragile X syndrome and associated disorders. https://www1.nichd.nih.gov/publications/pubs/Documents/nih_fragilex_research_plan_2009.pdf[↩]
- Warren, M. P., & Fried, J. L. (2001). Hypothalamic amenorrhea. The effects of environmental stresses on the reproductive system: A central effect of the central nervous system. Endocrinology & Metabolism Clinics of North America, 30, 611−629. https://www.ncbi.nlm.nih.gov/pubmed/11571933[↩]
- Verkauskas, G., Macianskyte, D., Janciauskas, D., Preiksa, R. T., Verkauskiene, R., & Jaubert, F. (2009). Diagnosis and management of 46,XY mixed gonadal dysgenesis and disorder of sexual differentiation. Medicina,45(5), 357–364. https://www.ncbi.nlm.nih.gov/pubmed/19535881[↩]
- Practice Committee of the American Society for Reproductive Medicine (PC-ASRM). (2006). Effectiveness and treatment for unexplained infertility. Fertility and Sterility, 86(suppl 4), S111–S114. https://www.asrm.org/globalassets/asrm/asrm-content/news-and-publications/practice-guidelines/for-non-members/current_evaluation_of_amenorrhea-pdfnoprint.pdf[↩]
- NIH. (2010, April). Most young women with menopause-like condition retain store of eggs. https://www.nih.gov/news-events/news-releases/most-young-women-menopause-condition-retain-store-eggs[↩]
- Rebar, R. W. (2009). Premature ovarian failure. Obstetrics and Gynecology, 113(6), 1355–1363.[↩]
- Gambadauro, P., Gudmundsson, J., & Torrejon, R. (2012). Intrauterine adhesions following conservative treatment of uterine fibroids. Obstetrics and Gynecology International,2012, 1–6. https://www.hindawi.com/journals/ogi/2012/853269/[↩]