Contents
What is peeling skin
Peeling skin can be caused by exfoliative keratolysis, which is a common skin condition in which there is focal peeling of the skin on your palms and less often the soles of your feet. It is also known as ‘keratolysis exfoliativa’, dyshidrosis lamellosa sicca, and ‘focal palmar peeling’ 1.
Exfoliative keratolysis is more common during the summer months in about 50% of affected individuals, and most often affects young adults. It may be more common in those with with sweaty palms, i.e. lcoalized hyperhidrosis.
The first sign is one or more superficial air-filled blisters on the fingers or palms. The blisters burst to leave expanding collarettes of scale and circular or oval, tender, peeled areas. These peeled areas lack a normal barrier function and may become red, dry and cracked. However, they are not generally itchy.
Sometimes on the ends of the fingers the split in the skin is deeper, in which case the skin feels hard and numb and takes longer to peel off.
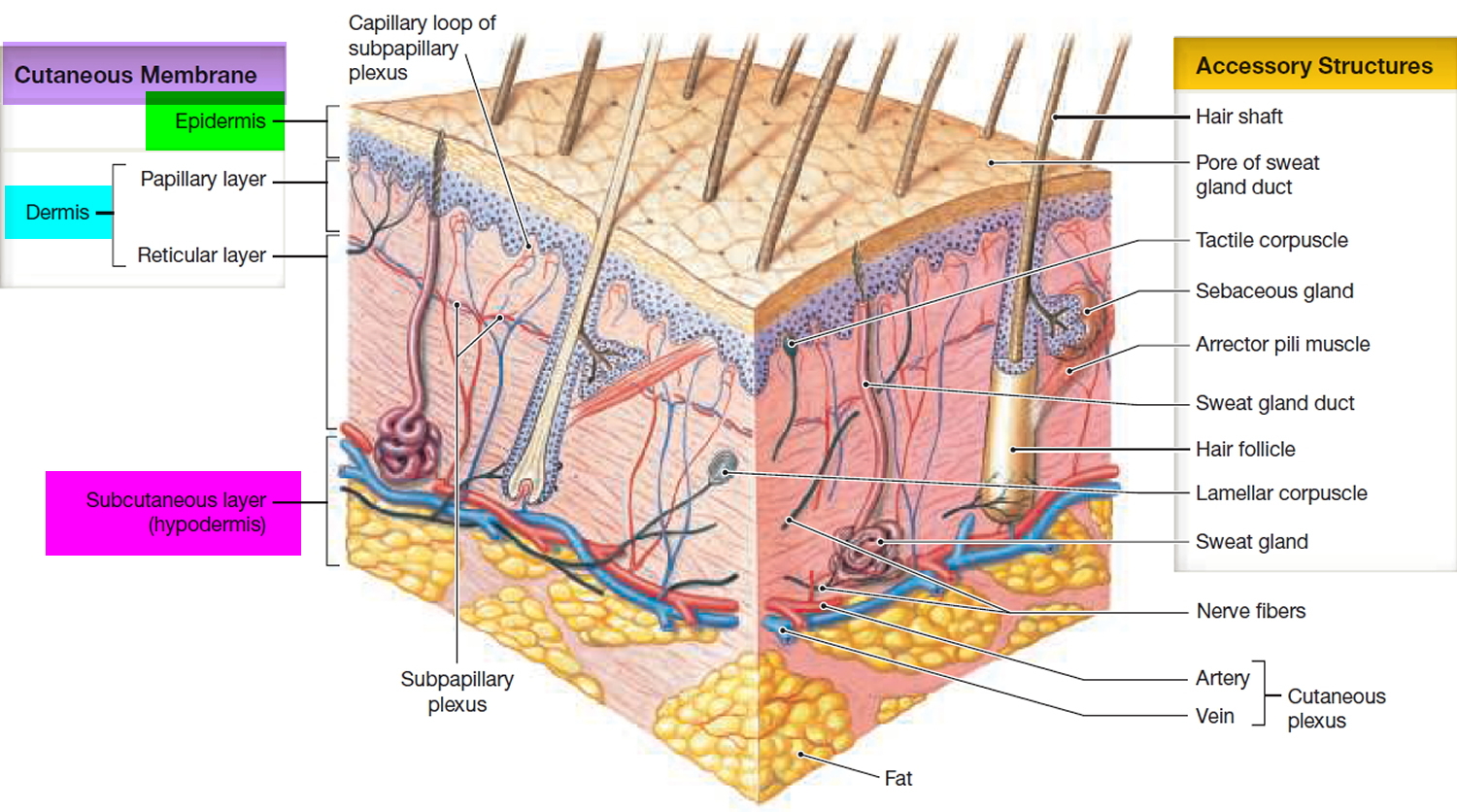
Figure 1. Skin structure
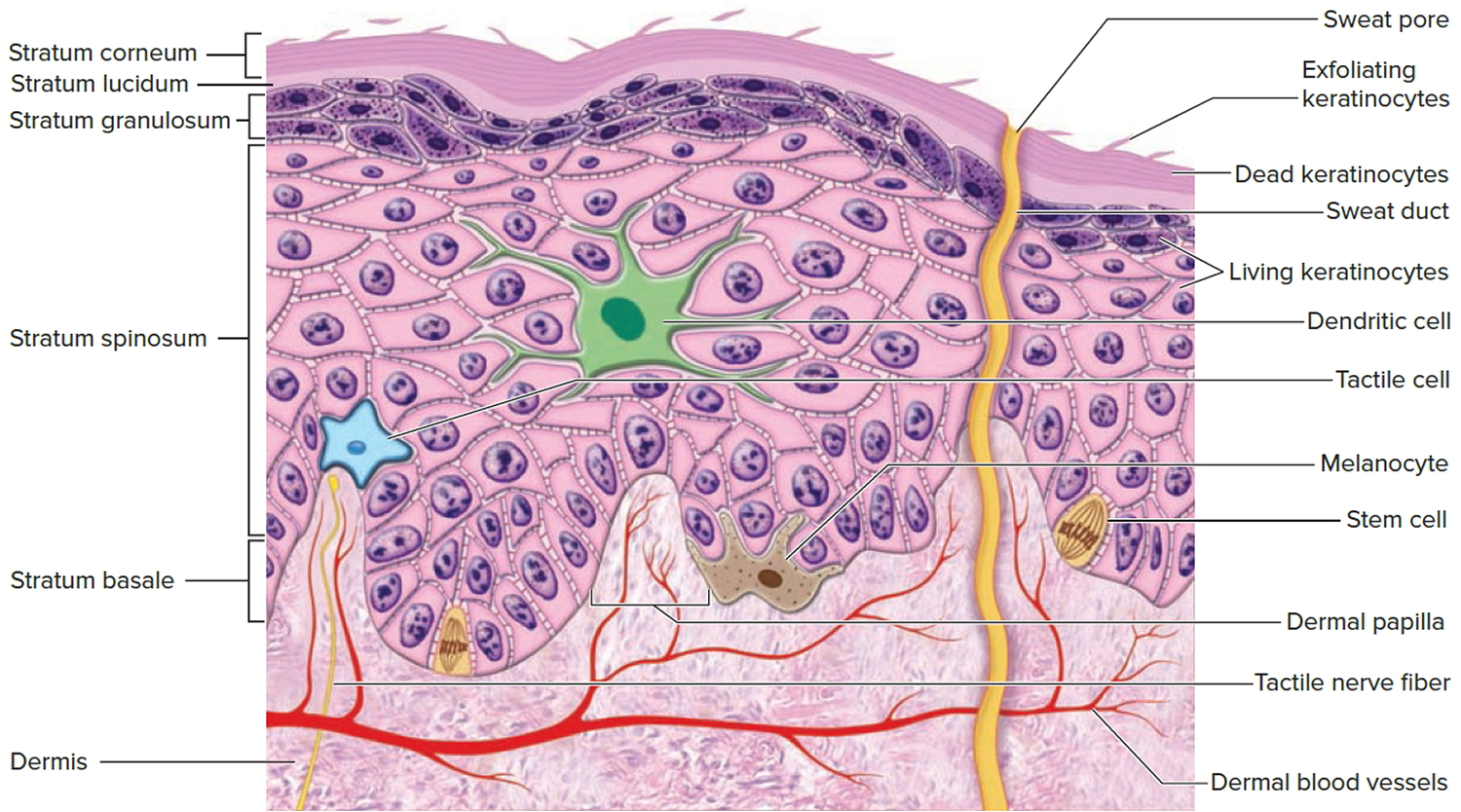
Figure 2. Structure and skin cells of the Epidermis
What is the cause of exfoliative keratolysis?
The cause of exfoliative keratolysis is unknown. Microscopy reveals cleavage within the outside horny layer of skin, the stratum corneum. It is thought that for some reason the coneocytes separate from each other prematurely. No genetic abnormality has been detected to date.
The symptoms are aggravated by exposure to irritants including water, soap, detergents and solvents. Eventually normal skin forms, but frequently exfoliative keratolysis recurs within a few weeks.
Exfoliative keratolysis is not eczema, but some cases may lead to or be confused with pompholyx, an itchy form of eczema in which there are small fluid-filled blisters.
It can also be confused with psoriasis, in which there are scaly patches, localized epidermolysis bullosa, in which blistering occurs, or with tinea (ringworm fungus), but scrapings for fungal culture are negative.
What is tinea?
Tinea manuum is the name given to ringworm fungus (dermatophyte) infection of one or both hands. It is much less common than tinea pedis (tinea affecting the foot). The diagnosis of hand tinea (tinea manuum) is confirmed by microscopy and culture of skin scrapings.
Tinea manuum is frequently misdiagnosed because it appears similar to:
- Hand dermatitis – especially the type called pompholyx.
- Psoriasis – especially palmoplantar pustulosis.
- Keratolysis exfoliativa.
Tinea manuum can occur as an acute inflammatory rash like tinea corporis. There is usually a raised border and clearing in the middle (ringworm). This is most likely when a zoophilic (animal) or geophilic (soil) fungus is responsible. The likely fungi are:
- Trichophyton erinacei – from a hedgehog
- Trichophyton verrucosum – from cattle
- Microsporum canis – from a cat or dog
- Microsporum gypseum – from soil
More frequently, hand tinea (tinea manuum) causes a slowly extending area of peeling, dryness and mild itching on the palm of one hand (hyperkeratotic tinea). Skin markings may be increased. Generally both feet appear similar (“one hand, two foot syndrome”). The usual cause is an anthropophilic (human) fungus:
- Trichophyton rubrum
- Trichophyton mentagrophytes var. interdigitale
- Epidermophyton floccosum
These fungi may also cause a blistering rash on the edges of the fingers or palm. The blisters appear in crops and contain a sticky clear fluid. They may have a peeling edge. This form of tinea manuum itches and burns.
Distinguishing features of hand tinea (tinea manuum)
Tinea manuum can be distinguished from hand dermatitis:
- In most cases of tinea manuum, only a single hand is involved.
- If both hands are affected, involvement is asymmetrical.
- Increased skin markings can be seen in dermatitis but in chronic tinea manuum they are white because of surface scale.
- Involvement of both palm and back of hand in contiguity.
- The rash may have an elevated border.
- Nearby nails may also be infected (tinea unguium). However, other skin conditions can also affect nails.
Treatment of hand tinea
Mild tinea manuum is treated with topical antifungal agents, but if the treatment is unsuccessful, oral antifungal medicines may be considered, including terbinafine and itraconazole.
Treatment of exfoliative keratolysis
Exfoliative keratolysis does not improve with topical steroids, unlike hand dermatitis.
The following may be helpful:
- Protection from irritants
- Emollient hand creams especially those containing urea, lactic acid, or silicone
- Photochemotherapy.
Peeling skin syndrome
Peeling skin syndrome also called acral peeling skin syndrome, is a group of rare inherited skin disorders characterized by painless spontaneous skin peeling (exfoliation) of the top layer of skin due to a separation of the outermost layer of the epidermis (stratum corneum) from the underlying layers 2. The term “acral” refers to the fact that the skin peeling in this condition is most apparent on the hands and feet. Occasionally, peeling also occurs on the arms and legs. The peeling is usually evident from birth, although the condition can also begin in childhood or later in life. Skin peeling is made worse by exposure to heat, humidity and other forms of moisture, and friction. The underlying skin may be temporarily red and itchy, but it typically heals without scarring. Peeling skin syndrome (acral peeling skin syndrome) is not associated with any other health problems.
Other findings may include blistering and/or reddening of the skin (erythema) and itching (pruritus). Symptoms may be present from birth or appear in early childhood. Based on the extent of skin involvement, two forms of peeling skin syndrome are recognized: a generalized form involving the entire integument, and an acral form involving only the extremities, and mostly hands and feet. Generalized peeling skin syndrome may clinically overlap with Netherton syndrome, which is another autosomal recessive skin disorder belonging to the group of congenital ichthyoses, with onset in the neonatal period and infancy.
Affected individuals may also experience itching and reddening of the skin. The signs and symptoms of peeling skin syndrome usually appear soon after birth, but they may also develop later in life.
There are two main subtypes of this condition, called noninflammatory type A and inflammatory type B. In some families, an acral form of peeling skin syndrome has been reported, in which skin peeling is strictly limited to the hands and feet. Peeling skin syndrome has an autosomal recessive pattern of inheritance. Mutations in the TGM5 gene have been identified in several patients with the acral form of peeling skin syndrome 3.
Acral peeling skin syndrome is a rare condition, with less than 100 cases have been reported in the medical literature. However, because its signs and symptoms tend to be mild and similar to those of other skin disorders, the condition is likely underdiagnosed.
Peeling skin syndrome is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
What is ichthyosis?
Ichthyosis is a family of genetic skin disorders characterized by dry, scaling skin that may be thickened or very thin. The prefix “ichthy” is taken from the Greek root for the word fish. Each year, more than 16,000 babies are born with some form of ichthyosis. A recent study has determined that approximately 300 babies are born each year with a moderate to severe form of ichthyosis. Ichthyosis affects people of all ages, races and gender. The disease usually presents at birth, or within the first year, and continues to affect the patient throughout their lifetime.
Most forms of ichthyosis are very rare. The genetic mutation that causes the disorder is passed from parent to child. In some cases however, neither parent exhibits the disorder themselves, but they are carriers of the defective gene. When two carriers pass their mutated gene on to a new life, the child will inherit the disorder. In some very rare cases, the genetic mutation occurs spontaneously in the affected generation.
Besides the common scaling condition of the skin and depending on the severity, there may be associated psychological symptoms due to the abnormal appearance of the skin. Ichthyosis is disfiguring for most affected individuals. In addition to the numerous medical complications like dehydration, infections, chronic blistering, overheating, and rapid-calorie loss, patients with ichthyosis are subjected to psychological issues. Patients are often ostracized and concerns of isolation, low self-esteem, and depression are common due to the appearance of their visible, chronically shedding skin.
What causes peeling skin syndrome
Acral peeling skin syndrome is caused by mutations in the TGM5 gene. This gene provides instructions for making an enzyme called transglutaminase 5, which is a component of the outer layer of skin (the epidermis). Transglutaminase 5 plays a critical role in the formation of a structure called the cornified cell envelope, which surrounds epidermal cells and helps the skin form a protective barrier between the body and its environment.
TGM5 gene mutations reduce the production of transglutaminase 5 or prevent cells from making any of this protein. A shortage of transglutaminase 5 weakens the cornified cell envelope, which allows the outermost cells of the epidermis to separate easily from the underlying skin and peel off. This peeling is most noticeable on the hands and feet probably because those areas tend to be heavily exposed to moisture and friction.
Related Disorders
Exfoliative dermatitis refers to a scaling skin disorder accompanied by distinct reddening (erythematous dermatitis) involving 90% or more of the skin surface. It is characterized by erythema and scaling involving the skin’s surface that often obscures the primary lesions. It is frequently difficult for clinicians to find the cause of exfoliative dermatitis even though the history of illness prior to erythema and scaling is obtained. Often, biopsies and blood studies are required. The term red man syndrome is reserved for idiopathic exfoliative dermatitis in which no primary cause can be found, notwithstanding a variety of examinations and tests. This form of the disorder is characterized by marked hardening of the skin of the palms and soles, swelling (lymphadenopathy), and raised levels of immunoglobulin E.
Keratolysis exfoliativa congenital (also known as dyshidrosis lamellosa sicca) is limited to palms and soles with small, air-filled blisters and collarette-like scaling. It has been debated to be a subtype of dyshidrotic eczema, due to fungal infection, or drug reaction. Although this disorder shows microscopic evidence for premature falling-apart of the components of the outer horny layer of the epidermis (corneodesmolysis), no mutations were identified in TGM5 and other candidate genes, indicating that it is a distinct disorder from acral peeling skin syndrome.
Netherton syndrome is a rare type of autosomal recessive congenital ichthyosis characterized either by scaly plaques with a peculiar, double-edged border (so-called “ichthyosis linearis circumflexa”) or by persistent, generalized redness, scaling, or, sometimes, peeling. The hair is often fragile and sparse due to a structural defect of the hair shafts that results in a ball-in-socket or bamboo stick-like appearance (trichorrhexis invaginata, “bamboo hair”). Another characteristic of Netherton syndrome is a predisposition to allergies such as asthma, or food allergies that cause skin eruptions.
Peeling skin syndrome signs and symptoms
Peeling skin syndrome is a form of congenital ichthyosis with autosomal recessive inheritance. The ichthyoses comprise a group of dermatological disorders characterized by dry, thickened, scaly skin involving all or most of the body. Individuals with peeling skin syndrome exhibit lifelong spontaneous, painless, shedding or peeling of the outermost layer of the skin (horny layer, aka stratum corneum). Often, affected individuals and/or their caregivers can remove sheets of skin manually, comparable to skin peeling after a severe sunburn. Other findings associated with this disorder may include itching, short stature, and/or newly formed hairs that can be plucked out more easily than normal. The disorder is caused by a superficial detachment of the outermost horny layers of the skin. The generalized form of peeling skin syndrome has been further sub-classified into a non-inflammatory type (A) and an inflammatory type (B).
In some people, the condition is limited to the arms and legs (acral extremities), diagnosed as “acral peeling skin syndrome”. In the acral types, most patients develop blisters and erosions on hands and feet at birth or during infancy, which is reminiscent of another blistering skin disorder, epidermolysis bullosa simplex.
Peeling skin syndrome diagnosis
A good history and physical exam are often sufficient to make the diagnosis, although specialized tests including surgical removal and microscopic evaluation (biopsy) of affected tissue may be necessary at times. The continual shedding of large sheets of skin distinguishes peeling skin syndrome from Netherton syndrome and from other types of autosomal recessive congenital ichthyosis, such as congenital ichthyosiform erythroderma. The skin of so-called “collodion babies” peels off after a few weeks and does not return, in contrast to patients with peeling skin syndrome whose symptoms return time after time.
Peeling skin syndrome treatment
Treating peeling skin syndrome by applying skin softening (emollient) ointments, especially after a bath while the skin is moist, may offer some relief. Plain petroleum jelly or Vaseline is preferred. None of the corticosteroids or systemic retinoids (vitamin A derivatives) is indicated or effective and all may have serious side effects or adverse reactions.