Contents
- What is psoriasis
- Psoriasis vs Eczema
- Psoriasis symptoms and signs
- Types of psoriasis
- Plaque psoriasis (also called psoriasis vulgaris)
- Nail psoriasis
- Guttate psoriasis
- Pustular psoriasis
- Inverse psoriasis (also called flexural psoriasis or intertriginous psoriasis)
- Erythrodermic psoriasis (also called exfoliative psoriasis)
- Psoriatic arthritis
- What causes psoriasis ?
- What triggers psoriasis ?
- Risk factors for psoriasis
- Complications of psoriasis
- How is psoriasis diagnosed ?
- How severe is your psoriasis ?
- Treatment of psoriasis
- Home remedies for psoriasis
- Psoriasis diet
- Psoriasis and Dietary Supplements
What is psoriasis
Psoriasis is a chronic (long-lasting) immune-mediated skin disease that causes itchy or sore patches of thick, raised, red skin with silvery scales to appear on the skin 1. You usually get the patches on your elbows, knees, scalp, back, face, palms and feet, but they can show up on other parts of your body. Some people who have psoriasis also get a form of arthritis called psoriatic arthritis.
Psoriasis develops when your immune system sends faulty signals that tell skin cells to grow too quickly. In a process called cell turnover, skin cells that grow deep in your skin rise to the surface. Normally, new skin cells take weeks to rise to the surface. In psoriasis, it happens in just days because your cells rise too fast.
The body does not shed these excess skin cells. The skin cells pile up on the surface of the skin, causing patches of psoriasis to appear.
Psoriasis may look contagious, but it’s not. You cannot get psoriasis from touching someone who has it. To get psoriasis, a person must inherit the genes that cause it.
Psoriasis typically affects the outside of the elbows, knees or scalp, though it can appear on any location. Some people report that psoriasis is itchy, burns and stings. Psoriasis is associated with other serious health conditions, such as diabetes, heart disease and depression.
If you develop a rash that doesn’t go away with an over-the-counter medication, you should consider contacting your doctor.
Psoriasis can be hard to diagnose because it can look like other skin diseases. Your doctor might need to look at a small skin sample under a microscope.
Psoriasis can last a long time, even a lifetime. Symptoms come and go. Things that make them worse include:
- Infections
- Stress
- Dry skin
- Certain medicines.
Who gets psoriasis ?
Psoriasis in the United States affects approximately 7.5 million Americans. People who get psoriasis usually have one or more person in their family who has psoriasis 2. Not everyone who has a family member with psoriasis will get psoriasis. But psoriasis is common. In the United States, about 7.5 million people have psoriasis. Most people, about 80%, have plaque psoriasis.
Psoriasis can begin at any age. Men and women develop psoriasis at equal rates.
Psoriasis also occurs in all racial groups, but at varying rates. Whites get psoriasis more often than other races. About 1.9 percent of African-Americans have psoriasis, compared to 3.6 percent of Caucasians.
Most people get psoriasis between 15 and 30 years of age, but it can develop at any age. About 10 to 15 percent of those with psoriasis get it before age 10. By age 40, most people who will get psoriasis, about 75%, have psoriasis. Another common time for psoriasis to begin is between 50 and 60 years of age.
Some infants have psoriasis, although this is considered rare.
Infants and young children are more likely to get inverse psoriasis and guttate psoriasis.
Doctors know that psoriasis is not contagious. It is not something you can “catch” or that others can catch from you. You cannot get psoriasis from swimming in the same pool or having sex. Psoriasis lesions are not infectious.
What about psoriasis in children ?
Every year, roughly 20,000 children under 10 years of age are diagnosed with psoriasis. Sometimes it is misdiagnosed because it is confused with other skin diseases. Symptoms include pitting and discoloration of the nails, severe scalp scaling, diaper dermatitis or plaques similar to that of adult psoriasis on the trunk and extremities. Psoriasis in infants is uncommon, but it does occur. Only close observation can determine if an infant has the disease.
If one parent has the disease, there is about a 10 percent chance of a child contracting it. If both parents have psoriasis, the chance increases to 50 percent. No one can predict who will get psoriasis. Scientists now believe that at least 10 percent of the general population inherits one or more of the genes that create a predisposition to psoriasis. However, only 2 to 3 percent of the population develops the disease.
Some young people report the onset of psoriasis following an infection, particularly strep throat. One-third to one-half of all young people with psoriasis may experience a flare-up two to six weeks after an earache, strep throat, bronchitis, tonsillitis or a respiratory infection. Areas of skin that have been injured or traumatized are occasionally the sites of psoriasis, know as the “Koebner [keb-ner] phenomenon.” However, not everyone who has psoriasis develops it at the site of an injury.
Psoriasis vs Eczema
Eczema is also called dermatitis, is a general term for rash-like skin conditions 3. Most types cause dry, itchy skin and rashes on the face, inside the elbows and behind the knees, and on the hands and feet 4. Scratching the skin can cause it to turn red, and to swell and itch even more.
The most common type of eczema is called atopic dermatitis 5. Eczema is often very itchy. When you scratch it, your skin becomes red and inflamed (puffy). Eczema affects adults and children. It is most common in babies.
Atopic dermatitis is a chronic skin condition. It is caused by an allergic reaction. It is the most common type of eczema. “Atopic” describes an inherited tendency to develop dermatitis, asthma, and hay fever. “Dermatitis” means that the skin is red and itchy.
Atopic dermatitis usually starts during infancy and continues into childhood. There are times when the condition gets worse (called flare-ups). Flare-ups are followed by times when the skin will heal. During these times, there may be no signs of atopic dermatitis (called remission). Remission can last for weeks, months, or even years. Some children will outgrow atopic dermatitis. Others will still have it when they are adults. Flare-ups in adults tend to be less severe.
What’s the difference between eczema and psoriasis ?
- Children get eczema. They can also get psoriasis.
- While more children develop eczema than psoriasis, almost 1% of children have psoriasis.
- It’s not always easy to tell whether a child has eczema or psoriasis. A study conducted in Australia found that most children who had psoriasis were initially diagnosed by their primary care doctor as having another disease, often eczema.
- To a dermatologist’s trained eye, psoriasis and eczema tend to look quite different.
Learning the differences between eczema and psoriasis
- Psoriasis causes well-defined, thick, red, scaly patches, commonly in areas like the elbows and knees. It is common to see psoriasis on the face, buttocks, and scalp of a child. You’ll also commonly see thick patches of skin with overlying redness.
- Eczema tends to appear in the crooks of the knees and the elbows.
- Children who have psoriasis tend to have mild itching. In eczema, the itching can be intense.
- There are many ways for a dermatologist to tell the difference between eczema and psoriasis, including what one sees on the skin, the amount of itch, and where the disease appears on the skin.
There can be overlap between eczema and psoriasis
- Still in some children, it’s hard to tell the difference. In this case, a dermatologist might diagnose the child with “psoriasiform dermatitis.”
- Sometimes, a child has both eczema and psoriasis, so there can be some overlap.
- A dermatologist, however, will generally be able to differentiate between these two relatively common skin disorders.
Symptoms of eczema and atopic dermatitis
Atopic dermatitis and eczema may start out as dry, extremely itchy skin 5. The rash may become very red, swollen, and sore. The more you scratch it, the worse it generally gets. A clear fluid may leak from the rash. Eventually, the rash will crust over and start to scale. Common places for the rash are in the elbow creases, behind the knees, on the cheeks, and on the buttocks.
What causes eczema and atopic dermatitis ?
You are more likely to have atopic dermatitis or eczema if a family member has it. These conditions aren’t contagious. This means you can’t catch them from other people. The exact cause of eczema and atopic dermatitis is unknown.
How are eczema and atopic dermatitis diagnosed ?
Your doctor will be able to diagnose eczema simply by looking. As part of your exam, he or she will also review your medical history. It is important to tell your doctor if you have allergies or asthma. He or she may order blood and skin patch tests to rule out other conditions.
Can eczema and atopic dermatitis be prevented or avoided ?
You may never know what causes your eczema or atopic dermatitis. Without knowing, you can’t avoid them. And they can’t be cured. But they can be managed. You can also learn to avoid the things that trigger them.
Limit your contact with things that can irritate your skin.
Some things that may irritate your skin include:
- household cleansers
- detergents
- aftershave lotions
- soap
- gasoline
- turpentine and other solvents.
Try to avoid contact with things that make you break out with eczema. Soaps and wetness can cause skin irritation. Wash your hands only when necessary. Use a mild unscented soap such as Dove, Basis, or Olay, especially if you have eczema on your hands. Dry your hands completely after you wash them.
Wear gloves to protect the skin on your hands.
Wear vinyl or plastic gloves for work that requires you to have your hands in water. Also, wear gloves when your hands are exposed to anything that can irritate your skin. Wear cotton gloves under plastic gloves to soak up sweat from your hands. Take occasional breaks and remove your gloves. This will prevent a buildup of sweat inside your gloves.
Wear gloves when you go outside during the winter. Cold air and low humidity can dry your skin. Dryness can make your eczema worse. Wear clothes made of cotton or a cotton blend. Wool and some synthetic fabrics can irritate your skin.
Care for your skin in the bath or shower.
Bathe only with a mild unscented soap, such as Dove, Basis, or Olay. Use a small amount of soap. Keep the water temperature cool or warm, not hot. Soaking in the tub for a short time can be good for your skin. Doing so allows your skin’s outer layer to absorb water and become less dry. Soak for 15 to 20 minutes. Then use a soft towel to pat your skin dry without rubbing. Immediately after drying, apply a moisturizer to your skin. This helps seal in the moisture.
Use a moisturizer on your skin every day.
Moisturizers help keep your skin soft and flexible. They prevent skin cracks. A plain moisturizer is best. Avoid moisturizers with fragrances (perfume) and a lot of extra ingredients. A good, cheap moisturizer is plain petroleum jelly (such as Vaseline). Use moisturizers that are more greasy than creamy because creams usually have more preservatives in them.
Regular use of a moisturizer can help prevent the dry skin that is common in winter.
Avoid getting too hot and sweaty.
Too much heat and sweat can make your skin more irritated and itchy. Try to avoid activities that make you hot and sweaty.
Eczema and atopic dermatitis treatment
Your doctor may prescribe a corticosteroid cream or ointment to apply to your rash. This will help reduce itching and calm inflammation. Use it right after bathing. Follow your doctor’s directions for using this medicine or check the label for proper use. Call your doctor if your skin does not get better after 3 weeks of using the medicine.
Antihistamines like hydroxyzine reduce itching. They can help make it easier to not scratch. A new class of drugs, called immunomodulators, works well if you have a severe rash. Two drugs in this class are tacrolimus and pimecrolimus. These drugs keep your immune system from overreacting when stimulated by an allergen. However, they can affect your immune system. So the Food and Drug Administration recommends that these drugs be used only when other treatments won’t work.
Try not to scratch the irritated area on your skin, even if it itches. Scratching can break the skin. Bacteria can enter these breaks and cause infection. Moisturizing your skin will help prevent itchiness.
Living with eczema and atopic dermatitis
Eczema can flare up when you are under stress. Learn how to recognize and cope with stress. Stress reduction techniques can help. Changing your activities to reduce daily stress can also be helpful.
The area where you had the eczema may easily get irritated again, so it needs special care. Continue to follow the tips provided here even after your skin has healed.
What does psoriasis look like ?
Figure 1. Psoriasis

Figure 2. Plaque psoriasis

Figure 3. Guttate psoriasis

Figure 4. Intertriginous psoriasis (armpit area)
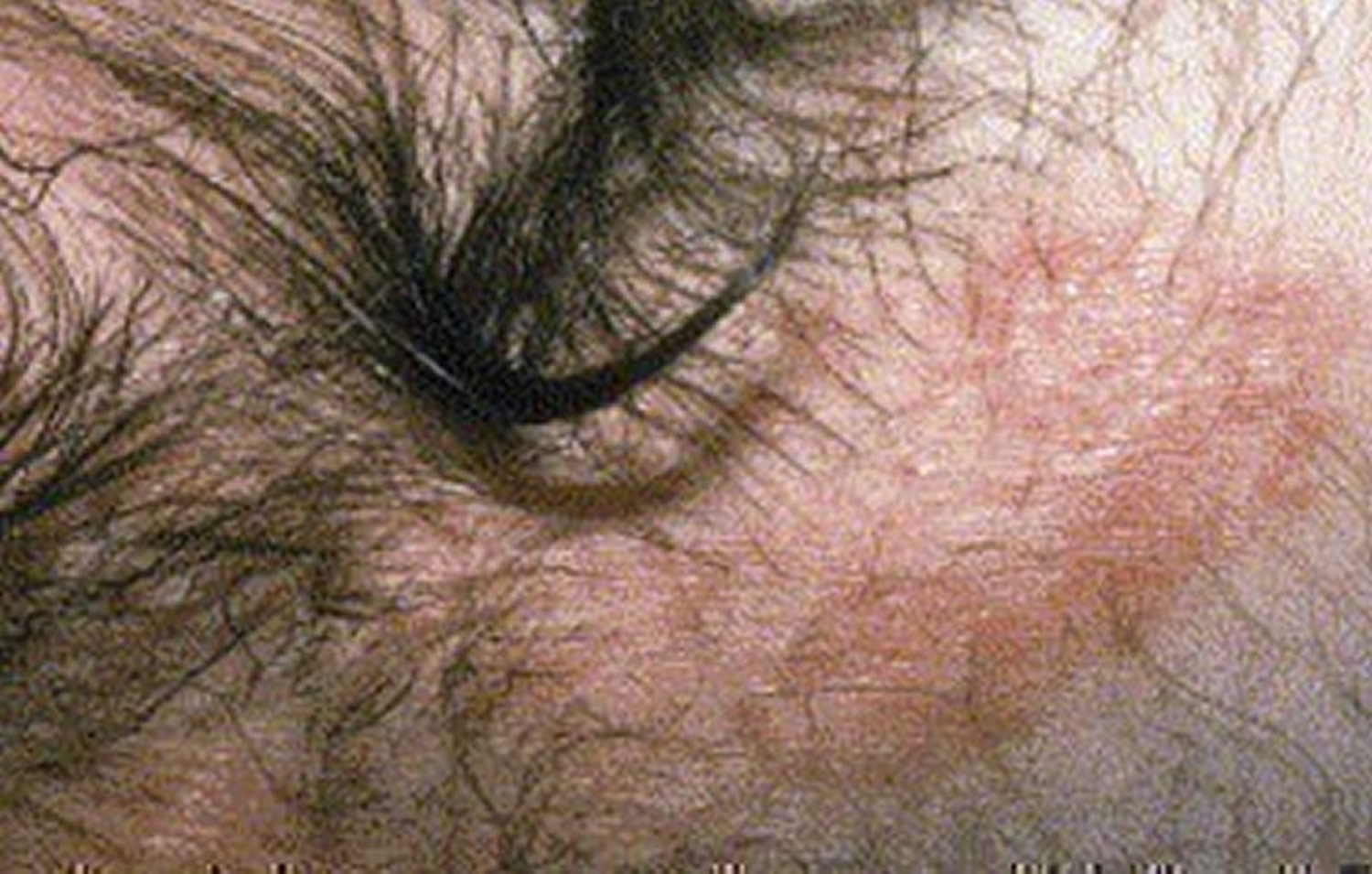
Figure 5. Pustular psoriasis

Figure 6. Erythrodermic psoriasis

Figure 7. Nail psoriasis

Figure 8. Psoriatic arthritis

Psoriasis symptoms and signs
Psoriasis signs and symptoms are different for everyone. What you see and feel depends on the type of psoriasis you have. You may have just a few of the signs and symptoms listed below, or you may have many.
Common signs and symptoms include:
- Red patches of skin covered with thick, silvery scales
- Small scaling spots (commonly seen in children)
- Dry, cracked skin that may bleed
- Itching, burning or soreness
- Thickened, pitted or ridged nails
- Swollen and stiff joints
Psoriasis patches can range from a few spots of dandruff-like scaling to major eruptions that cover large areas.
Most types of psoriasis go through cycles, flaring for a few weeks or months, then subsiding for a time or even going into complete remission.
Where does psoriasis show up ?
Psoriasis can show up anywhere—on the eyelids, ears, mouth and lips, skin folds, hands and feet, and nails. The skin at each of these sites is different and requires different treatments.
Light therapy or topical treatments are often used when psoriasis is limited to a specific part of the body. However, doctors may prescribe oral or injectable drugs if the psoriasis is widespread or greatly affects your quality of life. Effective treatments are available, no matter where your psoriasis is located.
Scalp Psoriasis
At least half of all the people who have psoriasis have it on their scalp.
Scalp psoriasis can be very mild, with slight, fine scaling. It can also be very severe with thick, crusted plaques covering the entire scalp. Psoriasis can extend beyond the hairline onto the forehead, the back of the neck and around the ears.
Other skin disorders, such as seborrheic dermatitis, may look similar to psoriasis. However, scalp psoriasis appears powdery with a silvery sheen, while seborrheic dermatitis appears yellowish and greasy.
Psoriasis on the Face
Facial psoriasis most often affects the eyebrows, the skin between the nose and upper lip, the upper forehead and the hairline. You might need a biopsy to confirm that it is psoriasis.
Psoriasis on and around the face should be treated carefully as the skin here is very sensitive. Occasional use of mild topical steroids, also called corticosteroids, may be effective. Other treatments include Dovonex, Tazorac, keratolytic products (scale removers) and ultraviolet light. Dovonex and Tazorac can be irritating, so you should work with your doctor to find a way to address this concern.
The U.S. Food and Drug Administration (FDA) has approved two drugs, Protopic and Elidel, for the treatment of eczema which many dermatologists have found work well for treating psoriasis on the face or other sensitive areas. Medication used to treat facial psoriasis should applied carefully and sparingly; creams and ointments can irritate eyes. Because facial skin is delicate, prolonged use of steroids may cause it to become thin, shiny and/or prone to enlarged capillaries. Treatment with steroids may be safe if a careful treatment schedule is followed.
Around the eyes
When psoriasis affects the eyelids, scales may cover lashes. The edges of the eyelids may become red and crusty. If inflamed for long periods, the rims of the lids may turn up or down. If the rim turns down, lashes can rub against the eyeball and cause irritation. Psoriasis of the eye is extremely rare. When it does occur, it can cause inflammation, dryness and discomfort. It may impair vision. Topical antibiotics may be used to treat infection.
In some cases, a special steroid medication made for use around the eyes may be used to treat scaling. Your doctor must carefully supervise the treatment because eyelid skin can be easily damaged. If topical steroids are overused in and around your eyes, glaucoma and/or cataracts may develop, which is the reason doctors suggest having your intraocular pressure checked regularly by an ophthalmologist.
Protopic ointment or Elidel cream won’t cause glaucoma and is effective on eyelids, but can sting the first few days of use. Using Protopic or Elidel for eyelid psoriasis may help you avoid the potential side effects of topical steroids.
In the ears
Psoriasis in the ears can cause scale buildup that blocks the ear canal. This buildup may lead to temporary hearing loss. A doctor should remove this scale. Psoriasis generally occurs in the external ear canal, not inside the ear or behind the eardrum.
Prescription steroid solutions can be dripped into the ear canal or applied to the outside portion of the ear canal. Dovonex or Tazorac may cause irritation when used alone and may be best used in combination with a topical steroid. The eardrum is easily damaged. Care should be taken when inserting anything rigid into the ear. Also, impaction of scale already present from psoriasis can occur if medication prescribed for the skin on the ear is not appropriately applied inside the ear canal.
Around the mouth and nose
For a very small number of people, psoriasis lesions appear on the gums, the tongue, inside the cheek, inside the nose or on the lips. The lesions are usually white or gray. Psoriasis in these areas can be relatively uncomfortable. It can cause difficulty in chewing and swallowing food.
For the most part, psoriasis treatments for the mouth and nose involve the use of topical steroids that have been designed to treat moist areas. Improving hygiene and rinsing frequently with a saline solution can help relieve oral discomfort. Low-potency steroids, such as hydrocortisone 1% ointment, may be useful in treating psoriasis on the lips. Protopic and Elidel may also be effective treatment options for psoriasis in and around the mouth.
Hands, Feet and Nails
Psoriasis on the hands and feet can lead to cracking, blisters and swelling. There are several treatments that can help psoriasis in these areas. A few lifestyle changes also can ease the discomfort of hand, feet and nail psoriasis.
Genital Psoriasis
The most common type of psoriasis in the genital region is inverse psoriasis. This type of psoriasis first shows up as smooth, dry, red lesions. It usually lacks the scale associated with plaque psoriasis.
There are various regions of the genital area that can be affected by psoriasis:
- Pubis: The pubis is the region on males and females above the genitals. This area can be treated similarly to psoriasis on the scalp; however, use caution. Skin in the pubic region is more sensitive than the skin on the scalp.
- Upper thighs: Psoriasis on the upper thighs often consists of many small, round patches that are red and scaly. Psoriasis in between the thighs is easily irritated, especially if the thighs rub together when you walk or run.
- Creases between thigh and groin: Psoriasis generally appears as non-scaly and reddish-white in the creases between the thigh and groin. The skin may have fissures (cracks). People who are overweight or athletic may have an infection called intertrigo, which looks similar to a yeast infection in the folds of the skin.
- Genitals: Psoriasis of the vulva often appears as a smooth, non-scaly redness. Scratching this area may cause an infection, create dryness, and result in thickening of the skin and further itching. Genital psoriasis usually affects the outer skin of the vagina because psoriasis does not normally affect mucous membranes. In general, genital psoriasis does not affect the urethra.
Psoriasis of the penis may appear as many small, red patches on the glans, or shaft. The skin may be scaly or smooth and shiny. Genital psoriasis affects both circumcised and uncircumcised males.
Anus and surrounding skin: Psoriasis on or near the anus is red, non-scaly and prone to itchiness. Psoriasis in this area may be confused with yeast, infections, hemorrhoidal itching and pinworm infestations. The presence of these conditions can complicate the treatment of psoriasis. Rectal examinations and skin cultures can confirm these conditions. Symptoms of anal psoriasis may include bleeding, pain during bowel movements, and excessive dryness and itching.
Buttocks crease: Psoriasis in the buttocks crease may be red and non-scaly or red with very heavy scales. The skin in this area is not as fragile as that of the groin.
Skin Folds
Inverse psoriasis can occur in skin folds such as the armpits and under the breasts. Friction and sweat can irritate this form of psoriasis.
Weaker corticosteroids are often used to treat inverse psoriasis in skin folds. These areas can be prone to yeast or fungal infections, so corticosteroids are sometimes used in combination with other medications.
Other topical treatments, such as calcipotriene (Dovonex), coal tar or anthralin, can be somewhat effective in treating psoriasis in skin folds. However, they may also be irritating. They should be used with caution and under the direction of a doctor. People with severe inverse psoriasis may occasionally require systemic medications to control the condition.
Your doctor may prescribe a product called Castellani’s Paint, which is used to treat inverse psoriasis. This product is compounded by a pharmacist or bought over the counter as brand name Castederm. It is a liquid that can be painted on the affected skin. It can help dry the moist lesions of psoriasis in skin folds. Powders may also help to dry the moist lesions. Some people use creams at night and powders in the morning.
Types of psoriasis
There are several types of psoriasis. If you have psoriasis, you will have one or more of these types 6:
- Plaque psoriasis (also called psoriasis vulgaris).
- Nail psoriasis.
- Guttate psoriasis.
- Inverse psoriasis (also called flexural psoriasis or intertriginous psoriasis).
- Pustular psoriasis.
- Erythrodermic psoriasis (also called exfoliative psoriasis).
Some people get more than one type. Sometimes a person gets one type of psoriasis, and then the type of psoriasis changes.
Plaque psoriasis (also called psoriasis vulgaris)
The most common form, plaque psoriasis causes dry, raised, red skin lesions (plaques) covered with silvery-white scales. The plaques might be itchy or painful and there may be few or many. They can occur anywhere on your body, including your genitals and the soft tissue inside your mouth.
Signs and symptoms (see Figure 2):
- Raised, reddish patches on the skin called plaque.
- Patches may be covered with a silvery-white coating, which dermatologists call scale.
- Patches can appear anywhere on the skin.
- Most patches appear on the knees, elbows, lower back, and scalp.
- Patches can itch.
- Scratching the itchy patches often causes the patches to thicken.
- Patches vary in size and can appear as separate patches or join together to cover a large area.
- Nail problems — pits in the nails, crumbling nail, nail falls off.
Nail psoriasis
Psoriasis can affect fingernails and toenails, causing pitting, abnormal nail growth and discoloration. Psoriatic nails might loosen and separate from the nail bed (onycholysis). Severe cases may cause the nail to crumble (see Figure 7).
Guttate psoriasis
Guttate psoriasis causes small spots that can show up all over the skin.
Guttate psoriasis primarily affects young adults and children. It’s usually triggered by a bacterial infection such as strep throat. It’s marked by small, water-drop-shaped, scaling lesions on your trunk, arms, legs and scalp.
The lesions are covered by a fine scale and aren’t as thick as typical plaques are. You may have a single outbreak that goes away on its own, or you may have repeated episodes.
Signs and symptoms (see Figure 3):
- Small, red spots (usually on the trunk, arms, and legs but can appear on the scalp, face, and ears).
- Spots can show up all over the skin.
- Spots often appear after an illness, especially strep throat.
- Spots may clear up in a few weeks or months without treatment.
- Spots may appear where the person had plaque psoriasis.
Pustular psoriasis
Pustular psoriasis causes pus-filled bumps that usually appear on the foot or hand.
This uncommon form of psoriasis can occur in widespread patches (generalized pustular psoriasis) or in smaller areas on your hands, feet or fingertips.
It generally develops quickly, with pus-filled blisters appearing just hours after your skin becomes red and tender. The blisters may come and go frequently. Generalized pustular psoriasis can also cause fever, chills, severe itching and diarrhea.
Signs and symptoms (see Figure 5):
- Skin red, swollen, and dotted with pus-filled bumps.
- Bumps usually appear only on the palms and soles.
- Soreness and pain where the bumps appear.
- Pus-filled bumps will dry, and leave behind brown dots and/or scale on the skin.
When pus-filled bumps cover the body, the person also may have:
- Bright-red skin.
- Been feeling sick and exhausted.
- Fever.
- Chills.
- Severe itching.
- Rapid pulse.
- Loss of appetite.
- Muscle weakness.
Inverse psoriasis (also called flexural psoriasis or intertriginous psoriasis)
Inverse psoriasis mainly develops in areas where skin touches skin, such as the skin in the armpits, in the groin, under the breasts and around the genitals. Inverse psoriasis causes smooth patches of red, inflamed skin that worsen with friction and sweating. Fungal infections may trigger this type of psoriasis.
Signs and symptoms (see Figure 4):
- Smooth, red patches of skin that look raw.
- Patches only develop where skin touches skin, such as the armpits, around the groin, genitals, and buttocks. Women can develop a red, raw patch under their breasts.
- Skin feels very sore where inverse psoriasis appears.
Erythrodermic psoriasis (also called exfoliative psoriasis)
Erythrodermic psoriasis is a particularly inflammatory form of psoriasis that often affects most of the body surface. Erythrodermic psoriasis can cause the skin to look like it is badly burned and can cover your entire body with a red, peeling rash that can itch or burn intensely.
This is the least common type of psoriasis.
- Individuals having an erythrodermic psoriasis flare should see a doctor immediately. This form of psoriasis can be life-threatening 7.
Erythrodermic psoriasis may occur in association with von Zumbusch pustular psoriasis. It is a rare type of psoriasis, occurring once or more during the lifetime of 3 percent of people who have psoriasis 7. It generally appears on people who have unstable plaque psoriasis. This means the lesions are not clearly defined. Widespread, fiery redness and exfoliation of the skin characterize this form. Severe itching and pain often accompanies it.
Erythrodermic psoriasis “throws off” the body’s chemistry. This causes protein and fluid loss that can lead to severe illness. Edema (swelling from fluid retention), especially around the ankles, may develop, along with infection. The body may not be able to maintain its temperature. This can produce shivering episodes. Erythrodermic psoriasis also can bring on pneumonia and congestive heart failure. People with severe cases often require hospitalization. Erythrodermic psoriasis can occur abruptly at the first signs of psoriasis or it can come on gradually in people with plaque psoriasis. The reason erythrodermic psoriasis appears is not understood. However, there are some known triggers.
Triggers of Erythrodermic psoriasis
- Abrupt withdrawal of systemic treatment
- Severe sunburn
- Allergic, drug-induced rash that brings on the Koebner phenomenon (a tendency for psoriasis to appear on the site of skin injuries)
- Use of systemic steroids (cortisone)
- Infection
- Emotional stress
- Alcoholism
Signs and symptoms (see Figure 6):
- Skin looks as if it has been burned.
- Most (or all) of the skin on the body turns bright red.
- Severe redness and shedding of skin over a large area of the body.
- Exfoliation often occurs in large “sheets” instead of smaller scales.
- Body cannot maintain its normal temperature of 98.6° F. Body temperature goes up and down, especially on very hot or cold days. Person gets very hot or very cold.
- Heart rate increases.
- Intense itching.
- Intense pain.
Psoriatic arthritis
In addition to inflamed, scaly skin, psoriatic arthritis causes swollen, stiffness and painful joints that are typical of arthritis. Sometimes the joint symptoms are the first or only manifestation of psoriasis or at times only nail changes and overall fatigue are seen. Symptoms range from mild to severe, and psoriatic arthritis can affect any joint. Although the disease usually isn’t as crippling as other forms of arthritis, it can cause stiffness and progressive joint damage that in the most serious cases may lead to permanent deformity.
Studies show that delaying treatment for psoriatic arthritis as little as six months can result in permanent joint damage. Early recognition, diagnosis and treatment of psoriatic arthritis are critical to relieve pain and inflammation and help prevent joint damage.
Up to 30 percent of people with psoriasis also develop psoriatic arthritis, which causes pain, stiffness and swelling in and around the joints.
Psoriatic arthritis can develop at any time, but it most commonly appears between the ages of 30 and 50. Genes, the immune system and environmental factors are all believed to play a role in the onset of the disease.
Psoriatic arthritis can develop slowly with mild symptoms, or it can develop quickly and be severe. Early recognition, diagnosis and treatment of psoriatic arthritis can help prevent or limit extensive joint damage that occurs in later stages of the disease. The disease can develop in a joint after an injury and may seem like a cartilage tear.
Here are common symptoms of psoriatic arthritis:
- Generalized fatigue
- Tenderness, pain and swelling over tendons
- Swollen fingers and toes that look like sausages
- Stiffness, pain, throbbing, swelling and tenderness in one or more joints
- A reduced range of motion
- Morning stiffness and tiredness
- Nail changes—for example, the nail separates from the nail bed and/or becomes pitted and mimics fungus infections
- Redness and pain of the eye, such as conjunctivitis
Psoriatic arthritis usually affects the distal joints (those closest to the nail) in fingers or toes.
You may also experience symptoms in your lower back, wrists, knees or ankle.
In 85 percent of patients, psoriasis occurs before joint disease. If you have been diagnosed with psoriasis, it is important to tell your dermatologist if you have any aches and pains.
There is little connection between your psoriasis severity and psoriatic arthritis severity. Having a severe case of psoriasis does not necessarily mean a person will have a severe case of psoriatic arthritis. A person could have few skin lesions, but have many joints affected by the arthritis.
What causes psoriasis ?
While scientists do not know what exactly causes psoriasis, they do know that the immune system (problem with T cells and other white blood cells, called neutrophils, in your body) and genetics play major roles in its development.
T cells (T lymphocytes) normally travel through the body to defend against foreign substances, such as viruses or bacteria. But if you have psoriasis, the T cells (T lymphocytes) attack healthy skin cells by mistake, as if to heal a wound or to fight an infection.
Overactive T cells also trigger increased production of healthy skin cells, more T cells and other white blood cells, especially neutrophils. These travel into the skin causing redness and sometimes pus in pustular lesions. Dilated blood vessels in psoriasis-affected areas create warmth and redness in the skin lesions.
The process becomes an ongoing cycle in which new skin cells move to the outermost layer of skin too quickly — in days rather than weeks. Skin cells build up in thick, scaly patches on the skin’s surface, continuing until treatment stops the cycle.
Just what causes T cells to malfunction in people with psoriasis isn’t entirely clear. Researchers believe both genetics and environmental factors play a role.
Moreover, scientists are still trying to learn everything that happens inside the body to cause psoriasis.
Usually, something triggers psoriasis to flare. The skin cells in people with psoriasis grow at an abnormally fast rate, which causes the buildup of psoriasis lesions.
Scientists have learned that a person’s immune system and genes play important roles. It seems that many genes must interact to cause psoriasis.
Scientists also know that not everyone who inherits the genes for psoriasis will get psoriasis. It seems that a person must inherit the “right” mix of genes. Then the person must be exposed to a trigger.
Which genes make a person more likely to develop psoriasis ?
Scientists have now identified about 25 genetic variants that make a person more likely to develop psoriatic disease. At the University of Michigan, Dr. J.T. Elder and his team of researchers have identified several areas on the human genome where more than one gene may be involved in psoriasis and psoriatic arthritis.
At the University of California-San Francisco, Dr. Wilson Liao is using new genetic sequencing technology to find rare “trigger genes” that may be the leading causes of psoriasis in certain individuals.
Working with DNA samples from a large family that includes many people with psoriasis, Anne Bowcock, Ph.D., a professor of genetics at Washington University School of Medicine in St. Louis, has identified a gene mutation known as CARD14 that when triggered leads to plaque psoriasis.
At the University of Utah, Drs. Gerald Krueger and Kristina Callis Duffin have carefully catalogued the psoriasis of more than 1,200 patients. By comparing the genes of each individual to the way psoriasis shows up on his or her body, the team hopes to understand which genes are involved in specific types of disease.
Using a NPF Discovery grant, British researcher Francesca Capon found that a mutation to the gene called IL36RN might be involved in the three forms of pustular psoriasis.
What triggers psoriasis ?
Many people say that their psoriasis began after they experienced one of these common psoriasis triggers:
- A stressful event.
- Smoking.
- Heavy alcohol consumption
- Infections, such as strep throat or skin infections.
- Certain medications — including lithium, which is prescribed for bipolar disorder, high blood pressure medications such as beta blockers, antimalarial drugs, and iodides.
- Cold, dry weather.
- Injury to the skin, such as a cut or scrape, a bug bite, or a severe sunburn.
- Vitamin D deficiency.
Certain medications are associated with triggering psoriasis, including:
- Lithium: Used to treat manic depression and other psychiatric disorders. Lithium aggravates psoriasis in about half of those with psoriasis who take it.
- Antimalarials: Plaquenil, Quinacrine, chloroquine and hydroxychloroquine may cause a flare of psoriasis, usually two to three weeks after the drug is taken.
- Hydroxychloroquine is the least likely to cause side effects.
- Inderal: This high blood pressure medication worsens psoriasis in about 25 percent to 30 percent of patients with psoriasis who take it. It is not known if all high blood pressure (beta blocker) medications worsen psoriasis, but they may have that potential.
- Quinidine: This heart medication has been reported to worsen some cases of psoriasis.
- Indomethacin: This is a nonsteroidal anti-inflammatory drug used to treat arthritis. It has worsened some cases of psoriasis. Other anti-inflammatories usually can be substituted. Indomethacin’s negative effects are usually minimal when it is taken properly. Its side effects are usually outweighed by its benefits in psoriatic arthritis.
Risk factors for psoriasis
Anyone can develop psoriasis, but these factors can increase your risk of developing the disease:
- Family history. This is one of the most significant risk factors. Having one parent with psoriasis increases your risk of getting the disease, and having two parents with psoriasis increases your risk even more.
- Viral and bacterial infections. People with HIV are more likely to develop psoriasis than people with healthy immune systems are. Children and young adults with recurring infections, particularly strep throat, also may be at increased risk.
- Stress. Because stress can impact your immune system, high stress levels may increase your risk of psoriasis.
- Obesity. Excess weight increases the risk of psoriasis. Lesions (plaques) associated with all types of psoriasis often develop in skin creases and folds.
- Smoking. Smoking tobacco not only increases your risk of psoriasis but also may increase the severity of the disease. Smoking may also play a role in the initial development of the disease.
Complications of psoriasis
If you have psoriasis, you’re at greater risk of developing certain diseases. These include 8:
- Psoriatic arthritis. This complication of psoriasis can cause joint damage and a loss of function in some joints, which can be debilitating.
- Eye conditions. Certain eye disorders — such as conjunctivitis, blepharitis and uveitis — are more common in people with psoriasis.
- Obesity. People with psoriasis, especially those with more severe disease, are more likely to be obese. It’s not clear how these diseases are linked, however. The inflammation linked to obesity may play a role in the development of psoriasis. Or it may be that people with psoriasis are more likely to gain weight, possibly because they’re less active because of their psoriasis.
- Type 2 diabetes. The risk of type 2 diabetes rises in people with psoriasis. The more severe the psoriasis, the greater the likelihood of type 2 diabetes.
- High blood pressure. The odds of having high blood pressure are higher for people with psoriasis.
- Cardiovascular disease. For people with psoriasis, the risk of cardiovascular disease is twice as high as it is for those without the disease. Psoriasis and some treatments also increase the risk of irregular heartbeat, stroke, high cholesterol and atherosclerosis.
- Metabolic syndrome. This cluster of conditions — including high blood pressure, elevated insulin levels and abnormal cholesterol levels — increases your risk of heart disease.
- Other autoimmune diseases. Celiac disease, sclerosis and the inflammatory bowel disease called Crohn’s disease are more likely to strike people with psoriasis.
- Parkinson’s disease. This chronic neurological condition is more likely to occur in people with psoriasis.
- Kidney disease. Moderate to severe psoriasis has been linked to a higher risk of kidney disease.
- Emotional problems. Psoriasis can also affect your quality of life. Psoriasis is associated with low self-esteem and depression. You may also withdraw socially.
How is psoriasis diagnosed ?
There are no special blood tests or tools to diagnose psoriasis. A dermatologist (doctor who specializes in skin diseases) or other health care provider usually examines the affected skin and determines if it is psoriasis.
To diagnose psoriasis, a dermatologist:
- Examines a patient’s skin, nails, and scalp for signs of psoriasis.
- Asks whether family members have psoriasis.
- Learns about what has been happening in the patient’s life. A dermatologist may want to know whether a patient has been under a lot of stress, had a recent illness, or just started taking a medicine.
Sometimes a dermatologist also take a piece of the affected skin (a biopsy) and examine it under the microscope. A dermatologist may call this confirming the diagnosis. By looking at the removed skin under a microscope, a dermatologist can confirm whether a person has psoriasis.
When biopsied, psoriasis skin looks thicker and inflamed when compared to skin with eczema.
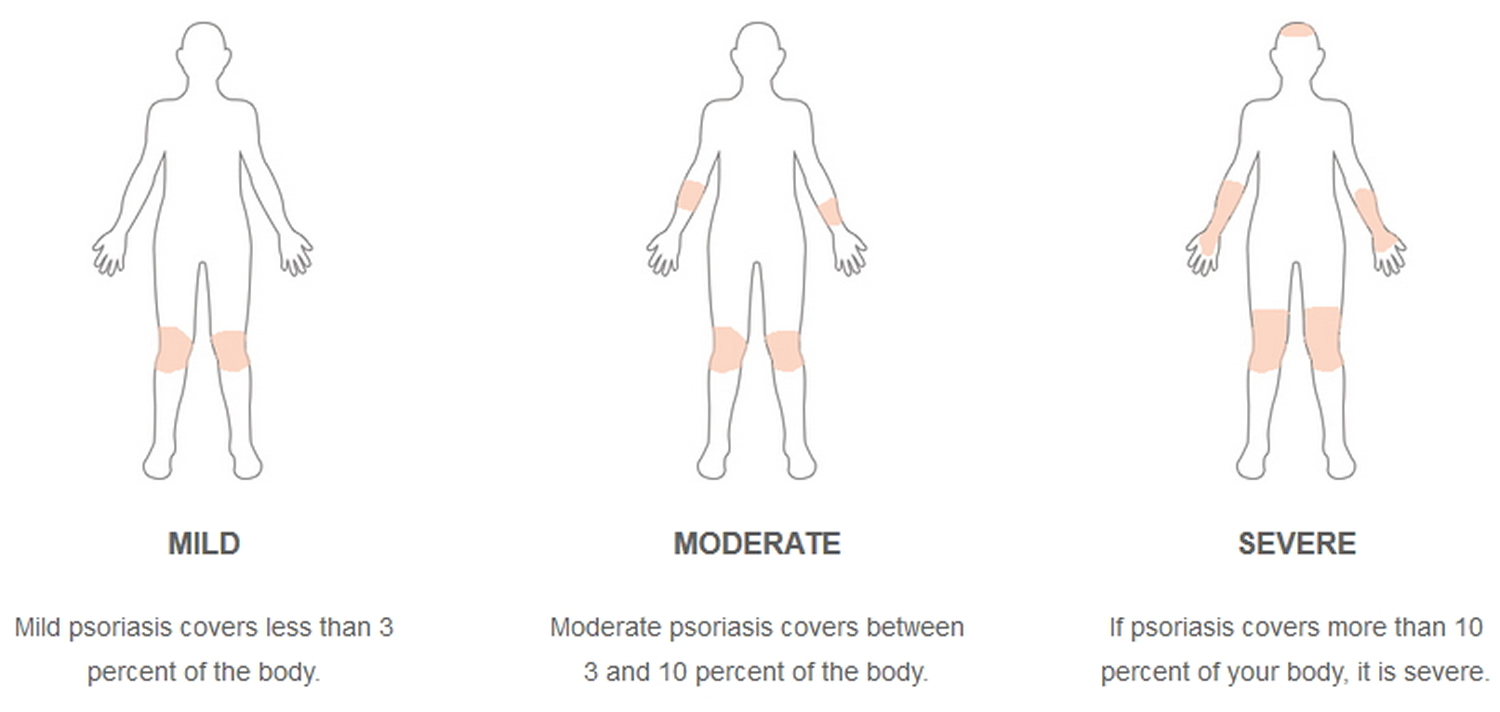
How severe is your psoriasis ?
Psoriasis can be mild, moderate or severe. Your treatment options may depend on how severe your psoriasis is. Severity is based on how much of your body is affected by psoriasis. The entire hand (the palm, fingers and thumb) is equal to about 1 percent of your body surface area.
However, the severity of psoriasis is also measured by how psoriasis affects a person’s quality of life. For example, psoriasis can have a serious impact on one’s daily activities even if it involves a small area, such as the palms of the hands or soles of the feet.
- Mild psoriasis: Topical treatments, such as moisturizers, over-the-counter and prescriptions creams and shampoos, typically are used for mild psoriasis.
- Moderate to severe psoriasis: Treating moderate to severe psoriasis usually involves a combination of treatment strategies. Besides topical treatments, your doctor your doctor may prescribe phototherapy (also known as light therapy). Your doctor may also prescribe systemic medications, including biologic drugs, especially if your psoriasis is significantly impacting your quality of life.
Figure 9. Psoriasis severity
 [Source 1]
[Source 1]
Treatment of psoriasis
Psoriasis is a chronic (long-lasting) disease of the immune system. It cannot be cured. This means that most people have psoriasis for life. By teaming up with a dermatologist who treats psoriasis, you can find a treatment plan that works for you.
Dermatologists encourage their patients who have psoriasis to take an active role in managing this disease. By taking an active role, you can reduce the effects that psoriasis has on your quality of life.
Psoriasis treatments reduce inflammation and clear the skin. Treatments can be divided into three main types: topical treatments, light therapy and systemic medications.
Topical treatments
Used alone, creams and ointments that you apply to your skin can effectively treat mild to moderate psoriasis. When the disease is more severe, creams are likely to be combined with oral medications or light therapy. Topical psoriasis treatments include:
- Topical corticosteroids. These drugs are the most frequently prescribed medications for treating mild to moderate psoriasis. They reduce inflammation and relieve itching and may be used with other treatments. Mild corticosteroid ointments are usually recommended for sensitive areas, such as your face or skin folds, and for treating widespread patches of damaged skin. Your doctor may prescribe stronger corticosteroid ointment for smaller, less sensitive or tougher-to-treat areas.
Long-term use or overuse of strong corticosteroids can cause thinning of the skin. Topical corticosteroids may stop working over time. It’s usually best to use topical corticosteroids as a short-term treatment during flares.
- Vitamin D analogues. These synthetic forms of vitamin D slow skin cell growth. Calcipotriene (Dovonex) is a prescription cream or solution containing a vitamin D analogue that treats mild to moderate psoriasis along with other treatments. Calcipotriene might irritate your skin. Calcitriol (Vectical) is expensive but may be equally effective and possibly less irritating than calcipotriene.
- Anthralin. This medication helps slow skin cell growth. Anthralin (Dritho-Scalp) can also remove scales and make skin smoother. But anthralin can irritate skin, and it stains almost anything it touches. It’s usually applied for a short time and then washed off.
- Topical retinoids. These are vitamin A derivatives that may decrease inflammation. The most common side effect is skin irritation. These medications may also increase sensitivity to sunlight, so while using the medication apply sunscreen before going outdoors. The risk of birth defects is far lower for topical retinoids than for oral retinoids. But tazarotene (Tazorac, Avage) isn’t recommended when you’re pregnant or breast-feeding or if you intend to become pregnant.
- Calcineurin inhibitors. Calcineurin inhibitors — tacrolimus (Prograf) and pimecrolimus (Elidel) — reduce inflammation and plaque buildup. Calcineurin inhibitors are not recommended for long-term or continuous use because of a potential increased risk of skin cancer and lymphoma. They may be especially helpful in areas of thin skin, such as around the eyes, where steroid creams or retinoids are too irritating or may cause harmful effects.
- Salicylic acid. Available over-the-counter (nonprescription) and by prescription, salicylic acid promotes sloughing of dead skin cells and reduces scaling. Sometimes it’s combined with other medications, such as topical corticosteroids or coal tar, to increase its effectiveness. Salicylic acid is available in medicated shampoos and scalp solutions to treat scalp psoriasis.
Salicylic Acid
Salicylic acid is classified as a keratolytic, or peeling agent, and works by causing the outer layer of skin to shed. It is a common and effective treatment for a wide variety of skin problems. As a psoriasis treatment, it acts as a scale lifter, helping to soften and remove psoriasis scales.
Strong salicylic acid preparations can cause irritation if left in contact with the skin for too long. The body may absorb too much salicylic acid if used over large areas of the skin. Salicylic acid may also weaken hair shafts and make them more likely to break, leading to temporary hair loss.
- Coal tar. Derived from coal, coal tar reduces scaling, itching and inflammation. Coal tar can irritate the skin. It’s also messy, stains clothing and bedding, and has a strong odor. Coal tar is available in over-the-counter shampoos, creams and oils. It’s also available in higher concentrations by prescription. This treatment isn’t recommended for women who are pregnant or breast-feeding.
Coal Tar
Tar derived from both coal and wood (e.g., juniper, pine) are both used for medicinal purposes. However, coal tar is the type used most commonly to treat psoriasis. Tar can help slow the rapid growth of skin cells and restore the skin’s appearance. In addition, it can help reduce the inflammation, itching and scaling of psoriasis. Tar products can vary dramatically from brand to brand. Generally, the higher the concentration of tar, the more potent the product.
Tar can irritate, redden and dry the skin. Test a tar product on a small area of the skin first. If reddening occurs, try applying the tar on top of a moisturizer. Tar can stain clothing, bed linen, and light-colored hair. Tar makes skin more sensitive to sunlight, so be sure to wash it off thoroughly, use sunscreen and monitor your sun exposure. Tar remains active on the skin for at least 24 hours, and you are at increased risk of sunburn during this period.
Studies show some of the chemicals in coal tar may cause cancer, but only in very high concentrations, such as in what is used in industrial paving. Anyone using tar regularly should follow a regular skin cancer checkup schedule. California requires over-the-counter (OTC) coal tar shampoos, lotions and creams that contain more than 0.5 percent coal tar to be labeled with cancer warnings. However, the FDA maintains that over-the-counter (OTC) products with coal tar concentrations between 0.5 percent and 5 percent are safe and effective for psoriasis, and there is no scientific evidence that the tar in over-the-counter (OTC) products is carcinogenic.
- Moisturizers. Moisturizing creams alone won’t heal psoriasis, but they can reduce itching, scaling and dryness. Moisturizers in an ointment base are usually more effective than are lighter creams and lotions. Apply immediately after a bath or shower to lock in moisture.
Moisturizers
Keeping the skin lubricated on a daily basis is an important part of psoriasis care because it reduces redness and itching and helps the skin heal. Dermatologists recommend heavy creams and ointments to lock water into the skin. Cooking oils and even shortening can be effective as economical substitutes for commercial moisturizers. Here are some quick tips for keeping your skin moisturized:
- use fragrance-free products
- apply moisturizers after showering and after washing your hands
- wash with moisturizing soaps
- limit your lukewarm showers to 10 minutes or less
Light therapy (phototherapy)
This treatment uses natural or artificial ultraviolet light. The simplest and easiest form of phototherapy involves exposing your skin to controlled amounts of natural sunlight.
Other forms of light therapy include the use of artificial ultraviolet A (UVA) or ultraviolet B (UVB) light, either alone or in combination with medications.
- Sunlight. Exposure to ultraviolet (UV) rays in sunlight or artificial light slows skin cell turnover and reduces scaling and inflammation. Brief, daily exposures to small amounts of sunlight may improve psoriasis, but intense sun exposure can worsen symptoms and cause skin damage. Before beginning a sunlight regimen, ask your doctor about the safest way to use natural sunlight for psoriasis treatment.
- UVB phototherapy. Controlled doses of UVB light from an artificial light source may improve mild to moderate psoriasis symptoms. UVB phototherapy, also called broadband UVB, can be used to treat single patches, widespread psoriasis and psoriasis that resists topical treatments. Short-term side effects may include redness, itching and dry skin. Using a moisturizer may help decrease these side effects.
- Narrow band UVB phototherapy. A newer type of psoriasis treatment, narrow band UVB phototherapy may be more effective than broadband UVB treatment. It’s usually administered two or three times a week until the skin improves, and then maintenance may require only weekly sessions. Narrow band UVB phototherapy may cause more-severe and longer lasting burns, however.
- Goeckerman therapy. Some doctors combine UVB treatment and coal tar treatment, which is known as Goeckerman treatment. The two therapies together are more effective than either alone because coal tar makes skin more receptive to UVB light.
- Psoralen plus ultraviolet A (PUVA). This form of photochemotherapy involves taking a light-sensitizing medication (psoralen) before exposure to UVA light. UVA light penetrates deeper into the skin than does UVB light, and psoralen makes the skin more responsive to UVA exposure. This more aggressive treatment consistently improves skin and is often used for more-severe cases of psoriasis. Short-term side effects include nausea, headache, burning and itching. Long-term side effects include dry and wrinkled skin, freckles, increased sun sensitivity, and increased risk of skin cancer, including melanoma.
- Excimer laser. This form of light therapy, used for mild to moderate psoriasis, treats only the involved skin without harming healthy skin. A controlled beam of UVB light is directed to the psoriasis plaques to control scaling and inflammation. Excimer laser therapy requires fewer sessions than does traditional phototherapy because more powerful UVB light is used. Side effects can include redness and blistering.
Oral or injected medications
If you have severe psoriasis or it’s resistant to other types of treatment, your doctor may prescribe oral or injected drugs. This is known as systemic treatment. Because of severe side effects, some of these medications are used for only brief periods and may be alternated with other forms of treatment.
- Retinoids. Related to vitamin A, this group of drugs may help if you have severe psoriasis that doesn’t respond to other therapies. Side effects may include lip inflammation and hair loss. And because retinoids such as acitretin (Soriatane) can cause severe birth defects, women must avoid pregnancy for at least three years after taking the medication.
- Methotrexate. Taken orally, methotrexate (Rheumatrex) helps psoriasis by decreasing the production of skin cells and suppressing inflammation. It may also slow the progression of psoriatic arthritis in some people. Methotrexate is generally well-tolerated in low doses but may cause upset stomach, loss of appetite and fatigue. When used for long periods, it can cause a number of serious side effects, including severe liver damage and decreased production of red and white blood cells and platelets.
- Cyclosporine. Cyclosporine (Gengraf, Neoral) suppresses the immune system and is similar to methotrexate in effectiveness, but can only be taken short-term. Like other immunosuppressant drugs, cyclosporine increases your risk of infection and other health problems, including cancer. Cyclosporine also makes you more susceptible to kidney problems and high blood pressure — the risk increases with higher dosages and long-term therapy.
- Drugs that alter the immune system (biologics). Several of these drugs are approved for the treatment of moderate to severe psoriasis. They include etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira), ustekinumab (Stelara), golimumab (Simponi), apremilast (Otezla), secukinumab (Cosentyx) and ixekizumab (Taltz). Most of these drugs are given by injection (apremilast is oral) and are usually used for people who have failed to respond to traditional therapy or who have associated psoriatic arthritis. Biologics must be used with caution because they have strong effects on the immune system and may permit life-threatening infections. In particular, people taking these treatments must be screened for tuberculosis.
- Other medications. Thioguanine (Tabloid) and hydroxyurea (Droxia, Hydrea) are medications that can be used when other drugs can’t be given.
Treatment considerations
Although doctors choose treatments based on the type and severity of psoriasis and the areas of skin affected, the traditional approach is to start with the mildest treatments — topical creams and ultraviolet light therapy (phototherapy) — in those patients with typical skin lesions (plaques) and then progress to stronger ones only if necessary. Patients with pustular or erythrodermic psoriasis or associated arthritis usually need systemic therapy from the beginning of treatment. The goal is to find the most effective way to slow cell turnover with the fewest possible side effects.
Potential future treatments
There are a number of new medications currently being researched that have the potential to improve psoriasis treatment. These treatments target different proteins that work with the immune system.
Alternative medicine
A number of alternative therapies claim to ease the symptoms of psoriasis, including special diets, creams, dietary supplements and herbs. None have definitively been proved effective. But some alternative therapies are deemed generally safe, and they may be helpful to some people in reducing signs and symptoms, such as itching and scaling. These treatments would be most appropriate for those with milder, plaque disease and not for those with pustules, erythroderma or arthritis.
- Aloe vera. Taken from the leaves of the aloe vera plant, aloe extract cream may reduce redness, scaling, itching and inflammation. You may need to use the cream several times a day for a month or more to see any improvements in your skin.
- Fish oil. Omega-3 fatty acids found in fish oil supplements may reduce inflammation associated with psoriasis, although results from studies are mixed. Taking 3 grams or less of fish oil daily is generally recognized as safe, and you may find it beneficial.
- Oregon grape. Also known as barberry, topical applications of Oregon grape may reduce inflammation and ease psoriasis symptoms.
If you’re considering dietary supplements or other alternative therapy to ease the symptoms of psoriasis, consult your doctor. He or she can help you weigh the pros and cons of specific alternative therapies.
Home remedies for psoriasis
There are other products which don’t contain salicylic acid or coal tar that are beneficial for treating psoriasis. Ingredients such as aloe vera, jojoba, zinc pyrithione, capsaicin and others, are frequently used to moisturize, soothe, remove scale or relieve itching.
The effectiveness of some of these products is not known. Be aware that “natural” ingredients can also cause side effects or allergic reactions. If irritation occurs, discontinue use.
Inverse psoriasis can be treated with Castederm, a liquid that is painted on the affected skin to help to dry moist lesions of psoriasis in folds of the body. The use of powders may also help to dry the moist lesions associated with inverse psoriasis.
Although self-help measures won’t cure psoriasis, they may help improve the appearance and feel of damaged skin. These measures may benefit you:
- Take daily baths. Bathing daily helps remove scales and calm inflamed skin. Add bath oil, colloidal oatmeal, Epsom salts or Dead Sea salts to the water and soak – can help remove psoriasis scale and soothe itching. Soak for around 15 minutes and apply a moisturizer or oil to the skin immediately after getting out of the bath. Avoid hot water and harsh soaps, which can worsen symptoms; use lukewarm water and mild soaps that have added oils and fats. Soak about 10 minutes then gently pat dry skin.
- Use moisturizer. After bathing, apply a heavy, ointment-based moisturizer while your skin is still moist. For very dry skin, oils may be preferable — they have more staying power than creams or lotions do and are more effective at preventing water from evaporating from your skin. During cold, dry weather, you may need to apply a moisturizer several times a day.
- Anti-itch. There are several ingredients that have been approved by the U.S. Food and Drug Administration (FDA) for treating itch. Some of these include calamine, hydrocortisone (a weak steroid), camphor, diphenhydramine hydrochloride (HCl), benzocaine and menthol. Beware that these ingredients may increase irritation and dryness.
- Scale lifters (keratolytics). Scale lifters help loosen and remove scale allowing medications to reach the psoriasis lesions. There are scale-lifting products designed for the scalp, body or both. Note that scalp products are usually stronger and may be too harsh for other skin sites. Over-the-counter (OTC) products that contain an active ingredient of salicylic acid, lactic acid, urea or phenol can be used as scale lifters.
- Occlusion. Some topical medications or moisturizers can be occluded (or covered) to increase their effectiveness and the amount absorbed into the skin. With occlusion, the topical is applied to psoriasis lesions and the area is covered with plastic wrap, cellophane, waterproof dressing, cotton socks or a nylon suit. Always check with your doctor before occluding a steroid or other prescription medication.
- Expose your skin to small amounts of sunlight. A controlled amount of sunlight can improve psoriasis, but too much sun can trigger or worsen outbreaks and increase the risk of skin cancer. First ask your doctor about the best way to use natural sunlight to treat your skin. Log your time in the sun, and protect skin that isn’t affected by psoriasis with sunscreen.
- Avoid psoriasis triggers, if possible. Find out what triggers, if any, worsen your psoriasis and take steps to prevent or avoid them. Infections, injuries to your skin, stress, smoking and intense sun exposure can all worsen psoriasis.
- Avoid drinking alcohol. Alcohol consumption may decrease the effectiveness of some psoriasis treatments. If you have psoriasis, avoid alcohol. If you do drink, keep it moderate.
Psoriasis diet
Psoriasis is a chronic, immune-mediated inflammatory skin disease. Beyond the skin, psoriasis is associated with a systemic inflammatory state that has been linked to obesity, cardiovascular diseases, and type 2 diabetes 9. In line with the current literature, BMI (body mass index) and abdominal obesity, as measured by waist circumference, were associated with psoriasis 10. In addition, as also very recently reported 11 in a series of psoriatic patients (treated and untreated) compared with normal weight controls, it was found that psoriatic patients exhibited statistically significant differences in body composition evaluated by BIA (the measurement of body fat in relation to lean body mass) also compared with BMI-matched control group. In particular, we found that psoriatic patients have lower values of the ratio of total body water to body weight, greater amounts of adiposity and lower muscle mass compared with the obese counterpart without psoriasis. A case-control study of 373 psoriasis patients and matched healthy controls showed that there was a two-fold increased risk for psoriasis development in the setting of obesity as compared to normal body weight. In addition, for each unit increment increase in BMI, there was a 9% higher risk for psoriasis onset and a 7% higher risk for increased Psoriasis Area and Severity Index 12.
Although a correlative relationship between obesity and psoriasis has been well recognized, the mechanistic link between these conditions is not fully understood. Adipocytes produce a variety of pro-inflammatory cytokines including TNF-alpha, MCP-1, and IL-6 13. Moreover, they key psoriasis cytokines IL-17 and IL-23 have been found to be elevated in obese women compared to lean women 14. Weight loss in overweight or obese subjects, through decreased caloric intake, appears to have an added beneficial effect on psoriasis or psoriatic arthritis when used in conjunction with other prescription medications. Interestingly, studies have shown that caloric restriction in obese subjects lowers the level of circulating inflammatory cytokines 15, 16. These cytokines may potentially serve to worsen existing psoriasis or trigger the development of new psoriasis.
Limited data exist regarding the role of specific diet regimens in psoriasis, mainly with the aim to reduce cardiac risk factors and obesity-related comorbidities. Previous studies or single case reports reported the positive effects of low-energy diets and vegetarian diets 17, formula diet weight loss programmes 18, gluten-free diet 19, very low-calorie carbohydrate-free (ketogenic) 20. Fasting periods or vegetarian diets and diets rich in omega-3 polyunsaturated fatty acids (ω-3 PUFA) from fish oil have been associated with improvement of psoriasis in clinical trials. In this, the reduced amounts of arachidonic acid and the increased eicosapentaenoic acid (EPA) intake might result in an anti-inflammatory environment 21. Some psoriatic patients are gluten-sensitive and may benefit from a gluten-free diet. It is believed that some vitamins (A, E and C), and oligoelements (iron, copper, manganese, zinc, and selenium) have anti-oxidants ability, which decrease oxidative stress and the production of reactive oxygen species. In addition, along with improving glucose, insulin and lipid control, food fibres also play an important role in systemic inflammation, by decreasing the oxidative stress produced by the elevated intake of high-simple carbohydrate foods. Finally, due to its role in proliferation and maturation of keratinocytes, vitamin D has become an important therapeutic option in the treatment of psoriasis.
Monounsaturated fatty acids (MUFA) are considered a healthy dietary fat, as opposed to saturated fatty acid. The most frequently consumed MUFA rich dietary oils is extra virgin olive oil (EVOO). Traditionally, the beneficial effects of EVOO have been attributed to its high MUFA content (oleic acid), as it protects lipoproteins and cellular membranes from oxidative damage. Very recently, we have demonstrated that psoriatic patients, compared to the control group, have a higher consumption of simple carbohydrates, total fat and ω-6/ω-3 PUFA ratio, with a lower intake of protein, complex carbohydrates, MUFA, ω-3 PUFA, and fibres 22. In particular, in that study it was found that the lowest intake of MUFA was associated with the highest clinical severity of psoriasis. The association between low MUFA intake and progression of psoriasis is in line with the same observation reported in other chronic inflammatory diseases. Additionally, the relationship of psoriasis with either individual nutrients or individual food groups, it should be kept in mind that diet is a complex combination of foods from various groups and nutrients, and some nutrients are highly correlated. Thus, it is challenging to separate the effect of a single nutrient or food group from that of others in free-living populations.
Rucevic et al. 23 performed a randomized, controlled trial comparing a low calorie diet (LCD) to a routine diet for psoriasis patients with plaque psoriasis and BMI>27. During the trial, patients were allowed to continue their baseline anti-psoriatic treatment which had been unchanged for 3 months prior, with approximately 20% of the patients on systemic psoriasis treatments. The low calorie diet (LCD) group lost significantly more weight than the routine diet group. Moreover, the LED group achieved a greater reduction in Psoriasis Area and Severity Index and greater improvement in the Dermatology Life Quality Index than the control group.
Another study 24 looked into the dietary habits of sixty two psoriatic subjects found that the psoriatic patients consumed less extra virgin olive oil, fruit, fish and nuts, while consumed more red meat compared to the control group. That study also suggested perhaps the Mediterranean diet characterized by a high intake of fruit and vegetables, legumes, grains and cereals, fish and seafood and nuts; a low intake of dairy products, meat and meat products; and a moderate ethanol intake mainly in the form of wine and during meals – might be considered an adjunctive tool for the treatment of psoriasis 24 .
Vegetarian diets has been shown to improve psoriasis symptoms in some studies 25. Beneficial effects of these diets are believed by others to be a result of better eicosanoid profile 26, so that inflammatory processes are suppressed. However, the relation of a potassium deficiency to psoriasis is much less well documented; specially considering the fact that increased potassium is a key consequence of vegetarian diets 27.
Higher potassium intake leads to higher cortisol biosynthesis 28. There are no qualitative differences between the effects of endogenous cortisol and exogenously applied synthetic glucocorticoids, which are used to treat psoriasis. The beauty of this is that all effects are transmitted via the same receptor 29. Results of a recent clinical trial showed that the elevated serum cortisol followed potassium supplementation 30. Briefly, thirty two hypokalaemic patients (48.6 ± 6 y) with active rheumatoid arthritis were investigated in a parallel randomized design for 28 days. In addition to their usual medication, the control group received placebo, and the intervention group received 6000 mg potassium chloride dissolved in grape juice on 28 consecutive days. The total potassium intakes, including dietary potassium and taking compliance into account, were 1540 ± 260 mg/day in placebo and 6495 ± 285 mg/day in intervention group. In the intervention group, mean serum potassium and serum cortisol were significantly raised by 1.51–1.75 mmol/L and 81.00–115.20 nmoles/L respectively, at the end of supplementation 30.
Psoriasis and Dietary Supplements
A number of single food components have been suggested to play a role in psoriasis. The ability of dietary of antioxidants, such as omega-3 polyunsaturated fatty acids from fish oil, some vitamins (A, B, E and C), and oligoelements (iron, copper, manganese, zinc and selenium), which decrease oxidative stress and the production of reactive oxygen species, might be of particular relevance mainly in a chronic systemic inflammatory diseases, like psoriasis 31.
Fish Oil
An elevated arachidonic acid (a product of omega-6 fatty acid) level has been implicated in psoriasis, and its metabolite, leukotriene B4, is a known inflammatory mediator in this condition 32. Consumption of omega-3 fatty acids from fish oil forms leukotrienes and prostaglandins that are of odd-number, such as prostaglandin E3 and leukotriene B5 33, which oppose the even-numbered inflammatory mediators, decreasing overall inflammation 34. A high consumption of omega-3 fatty acids is found in the populations of the West African countries, and this dietary intake of omega-3 has been linked to a low incidence of psoriasis in this region 35.
Oils of cold water fish rich in omega-3 polyunsaturated fatty acids, eicosapentaenoic acid (EPA) and docosahexanoic acid (DHA) have been considered for use in psoriasis treatment. A review 31 of fifteen trials evaluating fish oil for the treatment of psoriasis, despite the populations studied and the outcomes assessed were heterogeneous, overall there was moderate evidence of benefit for the use of fish oil supplements in psoriasis, with 12 trials (6 controlled, 6 uncontrolled) showing clinical benefit in psoriasis and 3 trials (2 controlled, 1 uncontrolled) showing no benefit.
Mayser et al. 36 and Grimminger et al. 37 each conducted double-blind, randomized, controlled studies comparing the effect of intravenous omega-3 fatty acids (Omegaven) to omega-6 fatty acids (Lipoven) for the treatment of psoriasis. In the Mayser et al. study 36, 75 subjects with chronic plaque psoriasis subjects were randomized to a 14-day treatment with either intravenous omega-3 or omega-6. The omega-3 group showed significantly better improvement for the erythema, scale, and induration. In Grimminger et al. 37, 20 subjects with acute guttate psoriasis received either intravenous omega-3 or omega-6 for 10 days. The omega-3 group demonstrated greater improvement in erythema, scale, and induration compared to the omega-6 group. This corresponded to a greater than ten-fold increase in favorable neutrophil leukotriene products seen in the omega-3 group but not in the omega-6 group.
In another double-blind placebo-controlled trial of 24 patients with chronic stable plaque psoriasis, the group that received 10 capsules of MaxEPA (1.8 g EPA, 1.2 g DHA) daily for 12 weeks showed more improvement in itching, erythema, scaling, and affected body surface area than the control group receiving 10 capsules of olive oil a day; however, only the improvement in erythema was statistically significant at 12 weeks5. Several uncontrolled, open studies have also shown that supplementation of fish oil, ranging from 0.54 to 13.5 grams EPA and 0 to 9.0 grams DHA daily for 6 weeks to 6 months, resulted in clinical improvement, measured by erythema, induration, and scaling 38, 39. These studies have also demonstrated clinical improvement associated with inhibition of leukotriene B4 production in peripheral leukocytes in vitro, decreases in platelet malondialdehyde production, changes in abnormalities of erythrocyte lipid membrane pattern, and increase in leukotriene B5 to leukotriene B4 ratio in peripheral blood neutrophils 40, 41.
Fish oil appears has also been studied in combination with other therapies. A double-blind, placebo-controlled study of 18 patients with severe stable plaque psoriasis demonstrated a statistically significant improvement of psoriasis on a regimen of fish oil with UVB therapy versus placebo olive oil with UVB 42. An open investigation of 30 patients with mild-to-moderate plaque psoriasis who were given either tacalcitol, a synthetic vitamin D3 analog, or combined tacalcitol and Oravex (2.8 g EPA, 0.4mg DHA), showed highly significant improvement in the Psoriasis Area and Severity Index score in the Oravex group compared to control after 8 weeks 43. Another study of 40 patients with chronic stable plaque psoriasis reported better clinical improvement of psoriasis with fish oil in combination with oral etretinate compared to etretinate monotherapy16.
There have also been several trials that have not shown significant improvement in psoriasis with fish oil. These studies utilized 1.8 to 3.2 g daily EPA and 1.2 to 2.2 g daily DHA11, 17, 18. In one randomized, double-blinded, controlled trial of 27 patients with psoriasis, there was no significant clinical difference between experimental fish oil group, which received 1.8 g EPA and 1.2 g DHA daily for eight weeks, and the control olive oil group 44. Another randomized, double-blinded, controlled study of 145 patients with moderate to severe psoriasis showed no significant difference in Psoriasis Area and Severity Index or patient reported subjective score between the group receiving fish oil and the placebo group receiving corn oil 45. A third open study that included 21 patients with plaque psoriasis also showed no clinically significant improvement following fish oil supplementation for six to eight weeks, although a single patient with pustular psoriasis showed significant improvement 46.
The most common side effects of fish oil include nausea, which may be dose dependent, indigestion, diarrhea, and fishy taste in the mouth.
Vitamin D
Vitamin D deficiency associated with psoriasis has been reported 47. Seven prospective trials of vitamin D3 supplementation in psoriasis and two trials in psoriatic arthritis- all were open-label uncontrolled studies except for one randomized, placebo-controlled trial. The forms of vitamin D3 used in these trials varied from 1,25-dihydroxyvitamin D3 (calcitriol, the physiologically active form of vitamin D) to 1-alpha-hydroxyvitamin D3 (alfacalcidol, requiring only liver metabolism to be converted to the active form) to vitamin D3 (cholecalciferol, requiring both liver and kidney metabolism to become active).
Perez et al. 48 performed a single center open trial to assess the safety and efficacy of oral 1,25-dihydroxyvitamin D3 for the treatment of psoriasis. Patients (n=85) were given 0.5 μg daily oral calcitriol, which was increased by 0.5 μg every 2 weeks as long as lab values were normal, for a period of six months to 36 months. Overall, 88% had some level of clinical improvement of psoriasis during the study period. 26.5% had complete improvement, 36.2% had moderate improvement, 25.3% had slight improvement of psoriasis, and 12% had no improvement. Additionally, the mean Psoriasis Area and Severity Index scores decreased from 18.4 at baseline to 9.7 at 6 months to 7.8 at 24 months of treatment.
Five additional open-label uncontrolled studies investigated the role of oral vitamin D supplementation in a smaller numbers of psoriasis patients ranging from seven to seventeen. In three of those trials, moderate or greater improvement in psoriasis was reported in at least 50% of subjects 49, 50, 51. For the other two trials, one showed statistically significant improvement in mean Psoriasis Area and Severity Index from baseline but results for individual subjects were not given 52, while in the other trial only 25% of patients showed moderate or better improvement 53. Additionally, two small trials have shown benefit of oral vitamin D on psoriatic arthritis as measured by the Disease Activity Score 54 or tender joint count 55.
In the only randomized, placebo-controlled trial of vitamin D supplementation reported to date, 9/20 (45%) receiving 1 μg daily of 1-hydroxyvitamin D3 showed slight improvement versus 8/21 (38%) in the placebo group, which was not statistically significant30.
Possible side effects of oral vitamin D supplementation include hypercalcemia, hypercalciuria, and kidney stones. Long-term vitamin D overdose can also lead to bone demineralization. Some studies reported an increase in blood levels of calcium and vitamin D or an increase of calcium in urine after starting oral supplementation 55, but no patient experienced adverse clinical side effects 56.
Vitamin B12
Vitamin B12 deficiency associated with psoriasis has been reported 57. A retrospective observational study of 98 patients with plaque psoriasis and 98 healthy controls demonstrated lower vitamin B12 levels in psoriasis patients compared to healthy controls 57. However, few studies have investigated the role of intramuscular administration of vitamin B12 in the treatment of psoriasis. Ruedemann 58 found favorable results with the administration of 1,000 g per cubic centimeter of vitamin B12 intramuscularly for 10 consecutive days, followed by a maintenance dose. Thirty-two percent (11/34) of patients cleared their psoriasis lesions and 29% (10/34) reached Psoriasis Area and Severity Index 75. Six of 34 patients initially reported severe pruritus, which resolved after two to three treatments. However, no baseline levels were taken prior to administering vitamin B12 to these subjects.
In contrast to these positive results, a double-blinded controlled study by Baker and Comaish 56 showed no difference with the use of intramuscular vitamin B12 injections for psoriasis. In this study involving 73 patients, intramuscular injections of 1,000 ug vitamin B12 or placebo were administered five days weekly for three weeks. No statistically significant benefit in vitamin B12 group was observed compared to placebo.
Vitamin B12 has no common side effects reported. Rare side effects include hypersensitivity reaction, nausea, vomiting, myalgia and swelling.
Selenium
Selenium is an essential element with anti-proliferative and immunoregulatory properties. A prospective study by Serwin et al. found that a decline in serum selenium was related to increased psoriasis disease severity in patients with psoriasis for more than three years 59. Several trials have assessed the role of selenium supplementation in psoriasis. Kharaeva et al. 60 enrolled 58 subjects in a double-blind placebo-controlled clinical study to compare the effects of combined selenium aspartate, coenzyme Q10, and Vitamin E versus placebo for the treatment of severe erythrodermic and arthropathic forms of psoriasis. They found that supplementation with the combination of antioxidants showed statistically significant clinical improvement of psoriasis by Psoriasis Area and Severity Index and Severity Score, the latter which included symptom scoring for desquamation of plaques, plaque hyperemia, plaque inflammation, nail dystrophy, and joint pain. The study also showed decline in oxidative stress, measured through activity level of enzymes such as catalase and superoxide dismutase, with the antioxidant supplementation.
In contrast, a double-blind, parallel group study of 37 patients by Serwin, Wasowicz, and Chodynicka demonstrated that selenium supplementation plus narrowband UVB was not superior to placebo plus narrowband UVB for psoriasis treatment 61. In another case-control study by Serwin et al. 62, 22 patients received topical 5% salicylic acid ointment, 0.1% to 0.3% dithranol ointment, and 200 μg daily selenomethionine versus placebo for 4 weeks. Both groups achieved almost complete remission, but the Psoriasis Area and Severity Index score was higher in the selenium group and the TNF level was also higher in the selenium group. Another small prospective study involving 7 patients showed that 6 weeks of 400 μg daily selenium increased the number of dermal CD4+ cells, but did not result in any clinical improvement in the patients 63.
Side effects with selenium are quite uncommon and are observed at doses above 400 mcg/day. They include nausea, vomiting, nail changes, loss of energy, and irritability. Long-term selenium toxicity can mimic arsenic poisoning and can include nail changes, nausea, vomiting, garlic breath, metallic taste, and hair loss.
Summary
Of the nutritional supplements reviewed, fish oil appears to be the most promising. Several studies suggest that omega-3 fatty acids may be beneficial as monotherapy or in combination with other therapeutic regimens in doses ranging from 0.45 to 13.5 g EPA and 0 to 9.0 g DHA daily for 6 weeks to 6 months.
- About Psoriasis. National Psoriasis Foundation. https://www.psoriasis.org/about-psoriasis[↩][↩]
- Psoriasis causes.American Academy of Dermatology. https://www.aad.org/public/diseases/scaly-skin/psoriasis#causes[↩]
- Eczema and Atopic Dermatitis. American Academy of Family Physicians. https://familydoctor.org/condition/eczema-and-atopic-dermatitis[↩]
- Eczema. Medline Plus. https://medlineplus.gov/eczema.html[↩]
- Atopic Dermatitis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/atopic-dermatitis[↩][↩]
- Psoriasis. American Academy of Dermatology. https://www.aad.org/public/diseases/scaly-skin/psoriasis[↩]
- Erythrodermic Psoriasis. National Psoriasis Foundation. https://www.psoriasis.org/about-psoriasis/types/erythrodermic[↩][↩]
- Psoriasis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/psoriasis/symptoms-causes/syc-20355840[↩]
- Grozdev I, Korman N, Tsankov N. Psoriasis as a systemic disease. Clin Dermatol. 2014;32:343–50. doi: 10.1016/j.clindermatol.2013.11.001. https://www.ncbi.nlm.nih.gov/pubmed/24767182[↩]
- Body mass index, waist circumference and HOMA-IR correlate with the Psoriasis Area and Severity Index in patients with psoriasis receiving phototherapy. Tobin AM, Hackett CB, Rogers S, Collins P, Richards HL, O’Shea D, Kirby B. Br J Dermatol. 2014 Aug; 171(2):436-8. https://www.ncbi.nlm.nih.gov/pubmed/24641699/[↩]
- Evaluation of body composition parameters in patients with psoriasis. Engin B, Kutlubay Z, Yardımcı G, Vehid HE, Ambarcıoğlu P, Serdaroğlu S, Tüzün Y. Int J Dermatol. 2014 Dec; 53(12):1468-73. https://www.ncbi.nlm.nih.gov/pubmed/25267412/[↩]
- Excessive body weight and smoking associates with a high risk of onset of plaque psoriasis. Wolk K, Mallbris L, Larsson P, Rosenblad A, Vingård E, Ståhle M. Acta Derm Venereol. 2009; 89(5):492-7. https://www.ncbi.nlm.nih.gov/pubmed/19734975/[↩]
- Psoriasis and systemic inflammatory diseases: potential mechanistic links between skin disease and co-morbid conditions. Davidovici BB, Sattar N, Prinz J, Puig L, Emery P, Barker JN, van de Kerkhof P, Ståhle M, Nestle FO, Girolomoni G, Krueger JG. J Invest Dermatol. 2010 Jul; 130(7):1785-96. https://www.ncbi.nlm.nih.gov/pubmed/20445552/[↩]
- Increased activity of interleukin-23/interleukin-17 proinflammatory axis in obese women. Sumarac-Dumanovic M, Stevanovic D, Ljubic A, Jorga J, Simic M, Stamenkovic-Pejkovic D, Starcevic V, Trajkovic V, Micic D. Int J Obes (Lond). 2009 Jan; 33(1):151-6. https://www.ncbi.nlm.nih.gov/pubmed/18982006/[↩]
- Hermsdorff HH, Zulet MA, Abete I, Martinez JA. Discriminated benefits of a Mediterranean dietary pattern within a hypocaloric diet program on plasma RBP4 concentrations and other inflammatory markers in obese subjects. Endocrine. 2009;36:445–51. https://www.ncbi.nlm.nih.gov/pubmed/19816812[↩]
- Nicklas BJ, Ambrosius W, Messier SP, Miller GD, Penninx BW, Loeser RF, et al. Diet-induced weight loss, exercise, and chronic inflammation in older, obese adults: a randomized controlled clinical trial. Am J Clin Nutr. 2004;79:544–51. http://ajcn.nutrition.org/content/79/4/544.long[↩]
- Upala S., Sanguankeo A. Effect of lifestyle weight loss intervention on disease severity in patients with psoriasis: A systematic review and meta-analysis. Int. J. Obes. (Lond.) 2015;39:1197–1202. doi: 10.1038/ijo.2015.64. https://www.ncbi.nlm.nih.gov/pubmed/25920774[↩]
- Leeds AR. Formula food-reducing diets:A new evidence-based addition to the weight management tool box. Nutrition Bulletin / Bnf. 2014;39(3):238-246. doi:10.1111/nbu.12098. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4314695/[↩]
- Bhatia BK, Millsop JW, Debbaneh M, Koo J, Linos E, Liao W. Diet and Psoriasis: Part 2. Celiac Disease and Role of a Gluten-Free Diet. Journal of the American Academy of Dermatology. 2014;71(2):350-358. doi:10.1016/j.jaad.2014.03.017. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4104239/[↩]
- Castaldo G., Galdo G., Rotondi Aufiero F., Cereda E. Very low-calorie ketogenic diet may allow restoring response to systemic therapy in relapsing plaque psoriasis. Obes. Res. Clin. Pract. 2015 doi: 10.1016/j.orcp.2015.10.008. https://www.ncbi.nlm.nih.gov/pubmed/26559897[↩]
- Johnson G.H., Fritsche K. Effect of dietary linoleic acid on markers of inflammation in healthy persons: A systematic review of randomized controlled trials. J. Acad. Nutr. Diet. 2012;112:1029–1041. doi: 10.1016/j.jand.2012.03.029. https://www.ncbi.nlm.nih.gov/pubmed/22889633[↩]
- Barrea L, Macchia PE, Tarantino G, et al. Nutrition: a key environmental dietary factor in clinical severity and cardio-metabolic risk in psoriatic male patients evaluated by 7-day food-frequency questionnaire. Journal of Translational Medicine. 2015;13:303. doi:10.1186/s12967-015-0658-y. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4571062/[↩]
- Rucević I, Perl A, Barisić-Drusko V, Adam-Perl M. The role of the low energy diet in psoriasis vulgaris treatment. Coll Antropol. 2003;27 (Suppl 1):41–8. https://www.ncbi.nlm.nih.gov/pubmed/12955890[↩]
- Barrea L, Balato N, Di Somma C, et al. Nutrition and psoriasis: is there any association between the severity of the disease and adherence to the Mediterranean diet? Journal of Translational Medicine. 2015;13:18. doi:10.1186/s12967-014-0372-1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4316654/[↩][↩]
- Lithell, H., Bruce, A., Gustafsson, I.B., Hoglund, N.J., Karlstrom, B., Ljunghall, K. et al. A fasting and vegetarian diet treatment trial on chronic inflammatory disorders. Acta Derm Venereol. 1983; 63: 397–403. https://www.ncbi.nlm.nih.gov/pubmed/6197838[↩]
- Wolters, M. Diet and psoriasis: experimental data and clinical evidence. Br J Dermatol. 2005; 153: 706–714. https://www.ncbi.nlm.nih.gov/pubmed/16181450[↩]
- Larsson, C.L. and Johansson, G.K. Dietary intake and nutritional status of young vegans and omnivores in Sweden. Am J Clin Nutr. 2002; 76: 100–106. http://ajcn.nutrition.org/content/76/1/100.long[↩]
- Li, L.A. and Lin, T.C. Interacting influence of potassium and polychlorinated biphenyl on cortisol and aldosterone biosynthesis. Toxicol Appl Pharmacol. 2007; 220: 252–261. https://www.ncbi.nlm.nih.gov/pubmed/17350062[↩]
- Buckbinder, L. and Robinson, R.P. The glucocorticoid receptor: molecular mechanism and new therapeutic opportunities. Curr Drug Targets Inflamm Allergy. 2002; 1: 127–136. https://www.ncbi.nlm.nih.gov/pubmed/14561195[↩]
- Rastmanesh, R., Abargouei, A.S., Shadman, Z., Ebrahimi, A.A., and Weber, C.E. A pilot study of potassium supplementation in the treatment of hypokalemic patients with rheumatoid arthritis: a randomized, double-blinded, placebo-controlled trial. J Pain. 2008; 9: 722–731. http://www.jpain.org/article/S1526-5900(08)00497-5/fulltext[↩][↩]
- Millsop JW, Bhatia BK, Debbaneh M, Koo J, Liao W. Diet and Psoriasis: Part 3. Role of Nutritional Supplements. Journal of the American Academy of Dermatology. 2014;71(3):561-569. doi:10.1016/j.jaad.2014.03.016. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4134971/[↩][↩]
- Stüning M, Schultz-Ehrenburg U, Altmeyer P, Raulf M, König W. Metabolism of [14C]arachidonic acid by polymorphonuclear leukocytes in patients with psoriasis. Br J Dermatol. 1987;116:153–9. https://www.ncbi.nlm.nih.gov/pubmed/3030388[↩]
- Treloar V. Integrative dermatology for psoriasis: facts and controversies. Clin Dermatol. 2010;28:93–9. https://www.ncbi.nlm.nih.gov/pubmed/20082958[↩]
- Kaimal S, Thappa DM. Diet in dermatology: revisited. Indian J Dermatol Venereol Leprol. 2010;76:103–15. https://www.ncbi.nlm.nih.gov/pubmed/20228538[↩]
- Logan AC. Omega-3, omega-6 and psoriasis: a different view. Int J Dermatol. 2005;44:527–8. author reply 8-9. https://www.ncbi.nlm.nih.gov/pubmed/15941451[↩]
- Mayser P, Mrowietz U, Arenberger P, Bartak P, Buchvald J, Christophers E, et al. Omega-3 fatty acid-based lipid infusion in patients with chronic plaque psoriasis: results of a double-blind, randomized, placebo-controlled, multicenter trial. J Am Acad Dermatol. 1998;38:539–47. https://www.ncbi.nlm.nih.gov/pubmed/9555791[↩][↩]
- Grimminger F, Mayser P, Papavassilis C, Thomas M, Schlotzer E, Heuer KU, et al. A double-blind, randomized, placebo-controlled trial of n-3 fatty acid based lipid infusion in acute, extended guttate psoriasis. Rapid improvement of clinical manifestations and changes in neutrophil leukotriene profile. Clin Investig. 1993;71:634–43. https://www.ncbi.nlm.nih.gov/pubmed/8219661[↩][↩]
- Maurice PD, Allen BR, Barkley AS, Cockbill SR, Stammers J, Bather PC. The effects of dietary supplementation with fish oil in patients with psoriasis. Br J Dermatol. 1987;117:599–606. https://www.ncbi.nlm.nih.gov/pubmed/3689678[↩]
- Kragballe K. Dietary supplementation with a combination of n-3 and n-6 fatty acids (super gamma-oil marine) improves psoriasis. Acta Derm Venereol. 1989;69:265–8. https://www.ncbi.nlm.nih.gov/pubmed/2566241[↩]
- Kojima T, Terano T, Tanabe E, Okamoto S, Tamura Y, Yoshida S. Effect of highly purified eicosapentaenoic acid on psoriasis. J Am Acad Dermatol. 1989;21:150–1. https://www.ncbi.nlm.nih.gov/pubmed/2545748[↩]
- Schena D, Chieregato GC, de Gironcoli M, Girelli D, Olivieri O, Stanzial AM, et al. Increased erythrocyte membrane arachidonate and platelet malondialdehyde (MDA) production in psoriasis: normalization after fish-oil. Acta dermato-venereologica Supplementum. 1989;146:42–4. https://www.ncbi.nlm.nih.gov/pubmed/2609880[↩]
- Gupta AK, Ellis CN, Tellner DC, Anderson TF, Voorhees JJ. Double-blind, placebo-controlled study to evaluate the efficacy of fish oil and low-dose UVB in the treatment of psoriasis. Br J Dermatol. 1989;120:801–7. https://www.ncbi.nlm.nih.gov/pubmed/2667615[↩]
- Balbás GM, Regaña MS, Millet PU. Study on the use of omega-3 fatty acids as a therapeutic supplement in treatment of psoriasis. Clinical, Cosmetic and Investigational Dermatology. 2011;4:73-77. doi:10.2147/CCID.S17220. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3133503/[↩]
- Bjørneboe A, Smith AK, Bjørneboe GE, Thune PO, Drevon CA. Effect of dietary supplementation with n-3 fatty acids on clinical manifestations of psoriasis. Br J Dermatol. 1988;118:77–83. https://www.ncbi.nlm.nih.gov/pubmed/2829958[↩]
- Søyland E, Funk J, Rajka G, Sandberg M, Thune P, Rustad L, et al. Effect of dietary supplementation with very-long-chain n-3 fatty acids in patients with psoriasis. N Engl J Med. 1993;328:1812–6. https://www.ncbi.nlm.nih.gov/pubmed/8502270[↩]
- Kettler AH, Baughn RE, Orengo IF, Black H, Wolf JE., Jr The effect of dietary fish oil supplementation on psoriasis. Improvement in a patient with pustular psoriasis. Journal of the American Academy of Dermatology. 1988;18:1267–73. https://www.ncbi.nlm.nih.gov/pubmed/2838536[↩]
- Gisondi P, Rossini M, Di Cesare A, Idolazzi L, Farina S, Beltrami G, et al. Vitamin D status in patients with chronic plaque psoriasis. Br J Dermatol. 2012;166:505–10. https://www.ncbi.nlm.nih.gov/pubmed/22013980[↩]
- Perez A, Raab R, Chen TC, Turner A, Holick MF. Safety and efficacy of oral calcitriol (1,25-dihydroxyvitamin D3) for the treatment of psoriasis. Br J Dermatol. 1996;134:1070–8. https://www.ncbi.nlm.nih.gov/pubmed/8763427[↩]
- Morimoto S, Yoshikawa K, Kozuka T, Kitano Y, Imanaka S, Fukuo K, et al. Treatment of psoriasis vulgaris by oral administration of 1 alpha-hydroxyvitamin D3–open-design study. Calcif Tissue Int. 1986;39:209–12. https://www.ncbi.nlm.nih.gov/pubmed/3093033[↩]
- Smith EL, Pincus SH, Donovan L, Holick MF. A novel approach for the evaluation and treatment of psoriasis. Oral or topical use of 1,25-dihydroxyvitamin D3 can be a safe and effective therapy for psoriasis. J Am Acad Dermatol. 1988;19:516–28. https://www.ncbi.nlm.nih.gov/pubmed/2459166[↩]
- Takamoto S, Onishi T, Morimoto S, Imanaka S, Yukawa S, Kozuka T, et al. Effect of 1 alpha-hydroxycholecalciferol on psoriasis vulgaris: a pilot study. Calcif Tissue Int. 1986;39:360–4. https://www.ncbi.nlm.nih.gov/pubmed/3100000[↩]
- Finamor DC, Sinigaglia-Coimbra R, Neves LCM, et al. A pilot study assessing the effect of prolonged administration of high daily doses of vitamin D on the clinical course of vitiligo and psoriasis. Dermato-endocrinology. 2013;5(1):222-234. doi:10.4161/derm.24808. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3897595/[↩]
- el-Azhary RA, Peters MS, Pittelkow MR, Kao PC, Muller SA. Efficacy of vitamin D3 derivatives in the treatment of psoriasis vulgaris: a preliminary report. Mayo Clinic proceedings. 1993;68:835–41. https://www.ncbi.nlm.nih.gov/pubmed/8396699[↩]
- Gaál J, Lakos G, Szodoray P, Kiss J, Horváth I, Horkay E, et al. Immunological and clinical effects of alphacalcidol in patients with psoriatic arthropathy: results of an open, follow-up pilot study. Acta Derm Venereol. 2009;89:140–4. https://www.ncbi.nlm.nih.gov/pubmed/19325997[↩]
- Huckins D, Felson DT, Holick M. Treatment of psoriatic arthritis with oral 1,25-dihydroxyvitamin D3: a pilot study. Arthritis Rheum. 1990;33:1723–7. https://www.ncbi.nlm.nih.gov/pubmed/2242069[↩][↩]
- Baker H, Comaish JS. Is Vitamin B12 of Value in Psoriasis? British Medical Journal. 1962;2(5321):1729-1730. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1926971/pdf/brmedj03003-0043.pdf[↩][↩]
- Brazzelli V, Grasso V, Fornara L, Moggio E, Gamba G, Villani S, et al. Homocysteine, vitamin B12 and folic acid levels in psoriatic patients and correlation with disease severity. Int J Immunopathol Pharmacol. 2010;23:911–6. https://www.ncbi.nlm.nih.gov/pubmed/20943063[↩][↩]
- Ruedemann R., Jr Treatment of psoriasis with large doses of vitamin B12, 1,100 micrograms per cubic centimeter; preliminary clinical report. AMA archives of dermatology and syphilology. 1954;69:738–9. https://www.ncbi.nlm.nih.gov/pubmed/13157646[↩]
- Serwin AB, Wasowicz W, Gromadzińska J, Chodynicka B. Selenium status in psoriasis and its relationship with alcohol consumption. Biol Trace Elem Res. 2002;89:127–37. https://www.ncbi.nlm.nih.gov/pubmed/12449236[↩]
- Kharaeva Z, Gostova E, De Luca C, Raskovic D, Korkina L. Clinical and biochemical effects of coenzyme Q(10), vitamin E, and selenium supplementation to psoriasis patients. Nutrition. 2009;25:295–302. https://www.ncbi.nlm.nih.gov/pubmed/19041224[↩]
- Serwin AB, Wasowicz W, Chodynicka B. Selenium supplementation, soluble tumor necrosis factor-alpha receptor type 1, and C-reactive protein during psoriasis therapy with narrowband ultraviolet B. Nutrition. 2006;22:860–4. https://www.ncbi.nlm.nih.gov/pubmed/16829029[↩]
- Serwin AB, Mysliwiec H, Hukalowicz K, Porebski P, Borawska M, Chodynicka B. Soluble tumor necrosis factor-alpha receptor type 1 during selenium supplementation in psoriasis patients. Nutrition. 2003;19:847–50. https://www.ncbi.nlm.nih.gov/pubmed/14559319[↩]
- Harvima RJ, Jagerroos H, Kajander EO, Harvima IT, Aalto ML, Neittaanmaki H, et al. Screening of effects of selenomethionine-enriched yeast supplementation on various immunological and chemical parameters of skin and blood in psoriatic patients. Acta dermato-venereologica. 1993;73:88–91. https://www.ncbi.nlm.nih.gov/pubmed/8103273[↩]




