Contents
What is bloating ?
Bloating has been defined as a feeling of increased abdominal pressure that may or may not be accompanied by objective abdominal distension, i.e., visible enlargement of the waist 1. Conversely, abdominal distension may occur without associated bloating sensation 2. Thus, bloating is a sensation and distension a sign but either one may produce significant distress 3. Although the distinction between bloating and distension is nowadays well established, both terms have been used imprecisely.
Bloating and abdominal distension may be manifestations of organic disease and potential causes should be considered first in the differential diagnosis. Acute infectious enteritis may be associated with severe bloating and abdominal distension in the early stages, often before the onset of diarrhea. Celiac disease and other conditions associated with malabsorption often present with bloating and concomitant abdominal distension. Acute or subacute bowel ischemia resulting from left sited cardiac failure or mesenteric insufficiency may manifest with bloating before the true cause of the clinical picture becomes self-evident. In the early stages of ascites formation in patients with liver cirrhosis, bloating may be a prominent clinical feature. Of course neoplastic (cancer) conditions and any mechanical impediment to normal flow of content along the gastrointestinal tract may be associated with symptoms of bloating and abdominal distension.
In clinical practice, bloating not associated with definite organic causes is what often brings patients to request medical consultation. As such, it may present as a cardinal symptom or main complaint, constituting a broad and imprecisely defined category termed functional abdominal bloating/distension by the Rome IV committee 4, but more often as part of other functional disorders such as functional dyspepsia (indigestion) or irritable bowel syndrome (IBS) 5. Indeed, bloating is a highly prevalent manifestation in irritable bowel syndrome (IBS) patients and for many it is their most bothersome symptom 6.
In functional dyspepsia (indigestion), patients may describe a bloating sensation centered in the upper abdomen, often postprandial and sometimes associated with visible upper abdominal distension. Dyspeptic bloating may be indistinguishable from the characteristic epigastric fullness that constitutes a key symptom in the postprandial distress syndrome subgroup of functional dyspepsia. Dyspeptic patients may describe it with the even more imprecise but common term “indigestion” or “slow digestion”. By contrast, upper abdominal bloating associated to gastroparesis tends to be accompanied by nausea and vomiting, not so frequent in the postprandial distress syndrome. Chronic belchers may present bloating as a trigger of belch-aerophagia sequences (a feature often unrecognized by the patient) or as a consequence of inflating their stomachs by pumping in air. In patients with IBS bloating tends to manifest as a diffuse abdominal sensation that is frequently described by patients as “wearing tight clothes”.
The clinical relevance of bloating as a symptom is highly variable. A lot of the people get bloated but levels of concern differ. Healthy individuals may occasionally get bloated, particularly after indulging in large, heavy meals or in association with an overload of fermentable foodstuffs. This type of bloating may be annoying but rarely elicits any concern as it is usually short lasting, maximum a few hours and ends when the individual expels stool and/or gas. Furthermore, the recall of similar past events reassures the affected person by predicting prompt resolution 7. However, there are individuals with unrealistic expectations about tolerance to sporadic food binges who will consult, not out of true concern about the significance of their postprandial bloating but to obtain from their healthcare provider a preventive drug or measure that would allow them to continue overindulging as they please without experiencing the punishment of bloating.
Bloating and flatulence, defined as evacuation of large volumes of gas per anus, often coexist but are definitely not the same. Experimental evidence indicates than increasing the amount of fermentable substrate in the colon, for instance by administering a poorly absorbable oligosaccharide such as lactulose to healthy individuals, results in rapid generation of excess gas (mostly H2 and CO2) flatulence 8, and bloating 9. Interestingly, ingestion of low fermentable psyllium fiber may induce a similar bloating sensation without excess intestinal gas production and hence without increased flatulence 10. This effect of bulk, dissociated from flatulence, is often acknowledged by bloated patients who indicate that ingestion of large amounts of fiber, particularly crude, aggravates their bloating even if their stool frequency increases.
What cause bloated stomach ?
Common causes include:
- Swallowing air
- Constipation
- Gastroesophageal reflux (GERD)
- Irritable bowel syndrome
- Lactose intolerance and problems digesting other foods
- Overeating
- Small bowel bacterial overgrowth
- Weight gain
You may have bloating if you take the oral diabetes medicine acarbose. Some other medicines or foods containing lactulose or sorbitol, may cause bloating.
More serious disorders that may cause bloating are:
- Ascites and tumors
- Celiac disease
- Dumping syndrome
- Ovarian cancer
- Problems with the pancreas not producing enough digestive enzymes (pancreatic insufficiency)
Bloating and distension associated with accumulation of luminal gas and/or fluid
Aerophagia, that is excessive swallowing of air, sometimes compounded by rapid ingestion of carbonated drinks, may potentially induce bloating and distension due to the lag between gas swallowing and spontaneous gas venting. However, this is usually not the case for two reasons. First, aerophagics tend to be belchers as well and even if they fill up their stomachs with air (esophageal belchers excluded) they do not accumulate enough quantities at a given time to produce bloating and distension. The second reason is that air advancing from the stomach into the upper small bowel is promptly cleared. CO2 and O2 rapidly diffuse through the permeable intestinal wall and N2, which is poorly absorbed is rapidly propelled distally and expelled through the anus 3.
Indeed, a series of experimental studies showed that the normal gut is extremely efficient in propelling gas towards the back end. Normal people are able to propel intestinal gas and expel it rectally at about the same rate as it is infused with only a relatively small volume remaining inside the gut at a given time 11. Under these conditions only a small minority of healthy subjects retains enough gas to develop bloating and/or perceptible distension. Conversely, a much higher proportion of individuals with functional abdominal symptoms, such as irritable bowel syndrome (IBS), functional bloating or functional dyspepsia (indigestion), show impaired gas disposal. Such patients tend to retain a relatively large proportion of the infused gas and consequently develop uncomfortable abdominal distension 12. Additional studies in healthy volunteers compared the effects of pharmacological gut motor inhibition and restrained voluntary evacuation on gas dynamics 13. In the former, distension was unaccompanied by discomfort whereas the latter produced both. The results suggested that, under the experimental conditions described, abdominal distension depends on the volume of gas retention whereas symptom perception depends on gut motor activity and the mechanism of retention. The symptom bloating appears to represent the clinical expression of an imbalance between gut tone and the volume of content. Such imbalance increases bowel wall tension and the latter generates the uncomfortable sensation of bloating. Intraluminal lipids accentuate gas retention and the bloating sensation 14 an observation that probably explains the symptomatic aggravation by fatty meals observed clinically. These experimental results provide a theoretical framework for the pharmacologic treatment of bloating.
Not only gas but other physical intraluminal components may distend the intestines. The volume of water within the small bowel may be substantially increased by slowly absorbed carbohydrates such as fructose and mannitol in association with perceived bloating sensation in irritable bowel syndrome (IBS) patients 15. Direct distending effects of excess retained stool in constipated individuals are another plausible possibility. Thus, a direct cause and effect relation between intraluminal gas and bloating has not been established and it is quite possible that intraluminal substrates other than gas (fluid and/or solid) may also elicit bloating as in the previously referred experiment with psyllium overload in healthy volunteers 10.
Bloating and distension associated with increased generation of intestinal gas
As pointed out earlier, flatulence and bloating do not necessarily present simultaneously in the same individual but excess gas generation may, under the right conditions, produce any of these two manifestations.
As opposed to excessive air intake that follows the oral route and may advance towards the back end, excess gas generation takes place inside the gut itself 16. The quantitatively important gases produced endogenously are CO2, H2, and CH4. Theoretically, during the post meal period considerable quantities of CO2 are produced by bicarbonate neutralization of gastric acid entering the duodenum but CO2 rapidly diffuses through the small intestinal wall and too little would remain in the lumen to produce significant bowel distension. Intraluminal fermentation of dietary and endogenous substrates which takes place mostly in the colon is the main source of bowel gas. We have estimated in healthy individuals that ~69% of the total gas present in the gut is located in the colon. However, only 23% of the gas produced in the colon is eventually expelled by anus, the rest being eliminated by other routes such as transmural disposal or bacterial consumption or Mego et al. 17.
The permeability of the bowel wall to gas diffusion is modified by blood flow and inflammation, among other factors, and plays a modulatory role on accumulation of gas generated inside the bowel itself. Scientists know that in the colon small/frequent/fast waves that act like a squeegee may propel gas rapidly past other luminal contents, basically stool, and expel it and flatus 18. Thus, whether newly generated colonic gas remains or not inside the colon depends on wall physical permeability and the type of motor activity. Exercise is another important factor as it favours antegrade movement and evacuation of intraluminal gas 19. In addition, intraluminal gas consumption by specialized catabolizing bacteria 20 counter balances gas generation in the colon due to fermentation of food residues. Bacterial gas consumption by colonic methanogenic, sulfate reducing, and acetogenic bacteria is quantitatively substantial.
Gas production increases rapidly after each meal containing non-absorbable, fermentable substrates 21. We have recently shown that both accumulation of fermentable residues from successive meals as well as the quantity of fermentable residue present between individual meals determines total gas production rates in healthy humans 22. Thus, the total amount of fermentable residues present in the colon at a given time is quite relevant. This may explain why constipation tends to be associated with bloating and flatulence and, conversely, why clearing the colon of retained residue improves these unwanted consequences. The distribution of liquid/solid residue within the colon appears to be rather uniform and stable although it tends to displace caudally into the pelvic colon during the postprandial period 23. However, even though colonic transit has been reported to be sluggish in bloated IBS patients 24 comparison of colonic non-gaseous content and distribution between healthy individuals and patients with bloating and abdominal distension shows no significant differences 25.
It has been postulated that increased gas production or decreased gas consumption in patients with bloating and flatulence may occur due to variations in colonic microbiota 26. However, when similar loads of fermentable carbohydrates are ingested by patients with IBS and healthy controls, both groups produce comparable volume of gas 27. Moreover, in a recent study comparing volume and distribution of intraluminal gas between normal and patients with functional disorders complaining of abdominal bloating and distension we observed no significant differences overall, although in some individuals aberrant gas distribution or gas accumulation, albeit in small amounts, is detectable during bloating episodes. Indeed, during symptomatic events such as bloating and distension episodes, intracolonic gas volume appears to be increased, albeit slightly 28. Therefore, although differences in colonic gas volume between asymptomatic and symptomatic periods are usually minimal, the mechanism of visceral hypersensitivity appear to be sufficient to both increase conscious perception (bloating), and activate unperceived, yet aberrant, viscero-somatic reflexes that expand the abdominal girth (distension).
In contrast to functional bloating and distension, patients with advanced intestinal neuropathy and enteric dysmotility develop symptomatic abdominal distension through a substantially different mechanism. Ineffective peristalsis resulting from disturbed enteric motility produces marked pooling of intestinal gas together with other luminal content 29 which becomes directly responsible for the observed abdominal distension.
Individual perception and focussed attention
Conscious perception of both bowel and abdominal distension probably play a determinant role in symptomatic bloating. That is, the same degree of bowel and abdominal distension may be either unperceived, produce minor discomfort or significant pain depending on the degree of conscious sensitivity. Indeed, visceral hyperalgesia, a common feature of IBS and functional bloating may largely account for the “bloating” sensation that, as noted earlier, occurs in the presence of normal or only mildly increased amounts of intraluminal gas or other bowel content. Bloating as a sensation may constitute an expression of discomfort just below the threshold for pain as suggested by physiological studies in healthy volunteers that are ramp-distended with intraluminal balloons. Conscious perception of intraluminal content is likely to be substantially increased by the physiological phenomenon of spatial summation whereby distending stimuli applied simultaneously at different sites, result in a marked increase in the perception score. Regional tolerance is another important factor. Scientists have shown, for instance, that exogenous gas infused into the colon is better tolerated that gas infused into the small bowel 30. Furthermore, the gut normally tolerates well the usual postprandial load of food, liquid, and gas, suggesting that postprandial accommodation is physiologically achieved without increasing gut wall tension 28. Normal propulsion of intraluminal content which may cause transient bowel distension ahead of the propagating contraction is also unperceived. Hence, it seems quite plausible that visceral hypersensitivity associated with functional bowel disorders converts these events, not normally sensed by healthy individuals, into bloating and other symptoms 31.
It is important to recognize that perception and reflex responses to stimuli arising from the gut are functions regulated at various levels along the brain–gut axis. Thus, both perceived and unperceived gut stimuli are modulated by complex neuro-hormonal mechanisms that act peripherally (where inflammation, sensitization, and other local factors may act as amplifiers and modifiers) but also along autonomic and medullar connecting pathways to the brain (where sympathetic arousal, descending inhibitory mechanisms and other mechanisms participate). At a central level, emotion and cognitive pain modulation are deeply interlinked, probably explaining the importance of the psychological status (stress and anxiety) on central reception and representation of nociceptive signals from the gut 32. It is also apparent that central activity may influence local gut conditions. It has been shown for instance that anxiety and depression facilitate gut inflammation 33. Furthermore, recent evidence indicates that in about 1/3 of patients with IBS, psychological distress develops after first appearance of gut symptoms suggesting that anxiety and depression may not necessarily be the primary drivers of the functional syndrome 34.
In the experience of bloating, disturbed emotional and cognitive pain modulation seem to play a facilitatory role. Individual differences in conscious perception of a given gut stimulus probably account for the wide range of bloating intensities and other features that may be observed in response to standardized bowel stimuli in experimental human studies. More to the point, an intraluminal distending stimulus may elicit symptoms in one individual (allodynia) and remain unnoticed by others.
Reflex responses to unperceived stimuli
Unperceived stimuli may be similarly modulated and upgraded by the central nervous system. Thus, abnormal viscero-somatic reflex responses that produce abdominal distension may operate, at least in theory, in the absence of pain.
Extraintestinal tissues within the abdominal cavity may also potentially influence the perception of bloating and abdominal distension. Intraabdominal adipose tissue accumulation is probably important. Several studies have shown that rapid weight gain aggravates symptomatic bloating, and conversely, weight loss tends to be associated with improvement. Several mechanisms may be at play. First, intraabdominal fat accumulation may constrain bowel expansion during luminal distension by gas or fluid, hence stimulating visceral and peritoneal sensory receptors. Second, adipose tissue accumulation in the epiplon or mesentery may have a pro-inflammatory action, on account of its capacity to release inflammatory cytokines, and thus contribute to intestinal hypersensitivity 35. Third, unwanted abdominal distension by fat may contribute to focus patient’s attention on the region and exacerbate the symptomatic response as it is known that attention or distraction substantially modify conscious perception of abdominal stimuli 36.
In females, another relevant factor to consider is the menstrual cycle. Abdominal bloating and discomfort frequently develop during the perimenstrual period (and sometimes ovulation as well) in normal otherwise asymptomatic females 37 and the aggravating influence of the menstrual cycle in females suffering from bloating and distension is frequently observed clinically. The mechanism remains unclear although enhanced visceral sensitivity in the premenstrual phase is probably a relevant factor 38.
Bloating and abdominal distension are also much influenced by meals and evacuation. Many patients acknowledge that the bloating sensation increases during the postprandial period and hence they tend to feel more comfortable during fasting. It is conceivably that a combination of gas and chyme pooling at various levels of the gastrointestinal tract enhances gut sensorial stimulation during digestion (an effect apparent in many normal individuals after binge eating) thus exceeding the threshold of conscious perception and even raising above the threshold for discomfort. These effects may be potentiated by chemical stimulation by specific food components, such as fat, that appears to intervene via CCK-dependent mechanisms 39. Bloaters may, therefore, distend more and feel more uncomfortable after meals, particularly after consumption of fatty foods. Bloaters may also acknowledge worsening of their symptomatology when they become constipated and accumulate a large quantity of stool inside their colon. Relief may follow evacuation although it is true that other patients indicate that passing stools does not necessarily relieve their bloating sensation. Pharmacological agents that relieve constipation have shown some effectivity in ameliorating bloating in constipated individuals but it is difficult to discern to what extent unloading of retained stool vs. direct neuropharmacological effects of these agents are responsible for the improvement. In patients with constipation due to functional outlet obstruction bloating tends to correlate with rectal balloon expulsion impairment 40.
Relation between bloating and flatulence
The relation between bloating and flatulence is somewhat ambiguous. Bloated patients often express the conviction that they would feel much relieved if they could expel “retained” gas per anus and/or mouth. Sometimes this may be the case but bloated patients may also acknowledge that forcefully expelling flatus does not diminish their bloating sensation or distension. It is unclear why this is the case since, intuitively, gas evacuation should reduce bowel distension. A possible explanation is the location of the retained gas stimulus that induces the bloating sensation. We have previously shown that gas accumulating inside the small bowel is more likely to induce abdominal discomfort than in the colon. Conversely, patients complaining of flatulence may not feel bloated unless they voluntarily inhibit expelling gas for social or other reasons. Scientists have previously shown that voluntary anal contraction to restrict evacuation of retained bowel gas produces, even in normal individuals, uncomfortable abdominal distension 13.
In most episodic bloaters there is a very apparent circadian rhythm 41 that modulates their bloating sensation and abdominal distension 42. Patients tend to wake up in the morning with no or minimal bloating. After breakfast and particularly during the afternoon and early evening the bloating sensation worsens and abdominal distension becomes more apparent 43. However, some bloaters do not manifest the aforementioned circadian rhythm and remain permanently bloated, and distended though long periods configuring a more severe clinical picture. In some patients, particularly women, dressing up with tight clothes aggravates their abdominal discomfort and the distension becomes more inconvenient and self-conscious, increasing patient’s uneasiness. Moreover, in some patients the unsatisfactory self-appearance produced by abdominal distension has adverse psychological consequences and may aggravate underlying anxiety/depression.
Abdominal shape
Normal individuals react to intestinal gas distension by contracting their anterior abdominal muscles and relaxing the diaphragm. By this reflex manoeuvre they increase the total capacity of the abdominal cavity without protruding their abdomen 44. Scientists have shown that patients complaining of bloating and abdominal distension activate different viscero-somatic responses that result in thoracic expansion, diaphragm contraction, and relaxation of the inferior oblique muscles. This manoeuvre reshapes their abdominal cavity and redistributes its contents resulting in anterior wall protrusion and visible distension (Figure 1). Net intraabdominal volume shows only a modest increase 45.
Thus, abdominal distension produced by reshaping of the abdomen appears to be a feature of patients with functional disorders via abnormal viscero-somatic responses rather than a direct consequence of intestinal dysmotility 46.
Figure 1. Bloating (CT image)
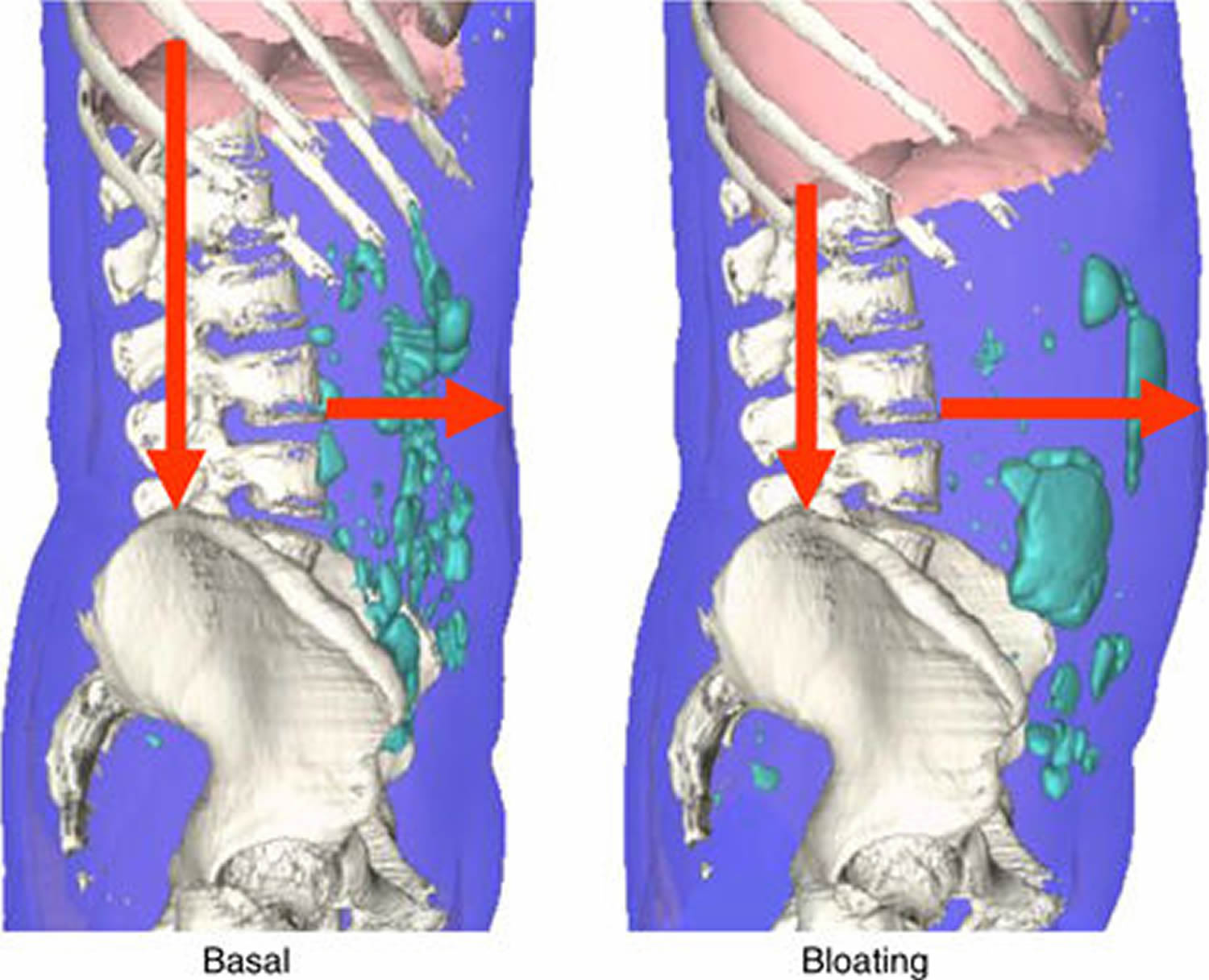
Note: Abdominal imaging in a patient with functional bloating. The left panel CT image shows a non-distended period with a mild bloating sensation. The right panel shows the same patient during a bloating and distension episode. Note the abdominal protrusion with elongated spine-navel axis and the marked descent of the diaphragm. Intrabowel gas volume increased by only 22 ml during the bloating episode.
When to see your doctor
Excessive belching, passing gas and bloating often resolve on their own or with simple changes. If these are the only symptoms you have, they rarely represent any serious underlying condition.
Consult your doctor if your symptoms don’t improve with simple changes, particularly if you also notice:
- Diarrhea
- Persistent or severe abdominal pain
- Bloody stools
- Changes in the color or frequency of stools
- Unintended weight loss
- Chest discomfort
- Loss of appetite or feeling full quickly
These signs and symptoms could signal an underlying digestive condition. Intestinal symptoms can be embarrassing — but don’t let embarrassment keep you from seeking help.
Diagnosis of bloated stomach
There are individuals who have heartburn and stomach disorders that may swallow air for relief. The diagnosis of esophageal reflux or gastric inflammation should be excluded by x-rays or endoscopy (examining the esophagus and stomach with a flexible tube while the patient is sedated). Abdominal distension when erect but not when recumbent is an indication of weak abdominal muscles. If lactose intolerance is suspected, milk can be withdrawn from the diet and symptoms observed. However, lactose can be administered orally and the hydrogen gas which is generated in susceptible people can be measured in the breath. Postnasal discharge from sinus problems can cause air swallowing and should be considered. If bacterial overgrowth is suspected, your physician may administer a hydrogen breath test.
Blood tests are not usually helpful for gaseous problems but testing for celiac disease may prove useful since failure to absorb wheat, barley, and rye can lead to excess flatulence.
Patients complaining of excessive gas passages may benefit from keeping a “flatus” diary for three days. The time of each gas passage and food for each meal can be noted. The gas passages can be compared to published “normal” flatus frequency.
Treatment of bloated stomach
Patients should eliminate carbonated beverages such as soda and beer. Foods such as cauliflower, broccoli, cabbage, beans, and bran should be avoided. Milk and other dairy foods should be avoided. Lactaid milk or non-dairy milk such as soy or almond milk can be used. Chewing gum and sucking on hard candies should be avoided. Sugar free gum and hard candies should be avoided as they may have mannitol or sorbitol as sweeteners which can cause flatulence. To ensure that only potentially symptom causing foods are eliminated without resulting in marked dietary restrictions, patients should eliminate food items one by one and keep a symptom diary.
Simethicone products have been promoted as treatment for gaseousness but their efficacy has not been convincing. Charcoal tablets have also been used to reduce flatulence without convincing benefit. Bismuth subsalicylate has been used to reduce the noxious odor of some sulfa-containing rectal gasses. Alpha-d-galactosidase, an over the counter product, has been used to help in the digestion of complex carbohydrates. Some patients may benefit from this strategy.
Individuals with IBS may benefit from symptomatic therapy for “gas pains” by using antispasmodic therapy such as dicyclomine or hyoscyamine under the tongue.
Some patients with bacterial overgrowth may see improvement from the occasional use of antibiotics to reduce the number of bacteria in the small bowel, thereby reducing gas production.
If weak abdominal muscles are suspected as a cause for abdominal distension, abdominal-tensing exercises may be helpful, although very difficult to achieve when patients are middle aged and older.
If symptoms fail to respond to the dietary strategies noted above, medical help should be sought to be confident that no other underlying abnormalities are present.
Home Remedies of bloated stomach
You may take the following steps:
- Eat and drink slowly. Taking your time can help you swallow less air. Try to make meals relaxed occasions; eating when you’re stressed or on the run increases the air you swallow.
- Avoid carbonated drinks and beer. They release carbon dioxide gas.
- Stay away from foods with high levels of fructose or sorbitol.
- Skip the gum and hard candy. When you chew gum or suck on hard candy, you swallow more often than normal. Part of what you’re swallowing is air.
- Don’t smoke. When you inhale smoke, you also inhale and swallow air.
- Check your dentures. Poorly fitting dentures can cause you to swallow excess air when you eat and drink.
- Get moving. It may help to take a short walk after eating.
- Treat heartburn. For occasional, mild heartburn, over-the-counter antacids or other remedies may be helpful. Gastroesophageal reflux disease (GERD) may require prescription-strength medication or other treatments.
- void foods that can produce gas, such as Brussels sprouts, turnips, cabbage, beans, and lentils.
- Eat fewer fatty foods. Fat slows digestion, giving food more time to ferment.
- Try an over-the-counter remedy. Some products such as Lactaid or Dairy Ease can help digest lactose. Products containing simethicone (Gas-X, Mylanta Gas) haven’t been proved to be helpful, but many people feel that these products work. Products such as Beano may decrease the gas produced during the breakdown of certain types of beans.
Get treatment for constipation if you have it. However, fiber supplements such as psyllium or 100% bran can make your symptoms worse.
You may try simethicone and other medicines you buy at the drugstore to help with gas. Charcoal caps can also help.
Watch for foods that trigger your bloating so you can start to avoid those foods. These may include:
- Milk and other dairy products that contain lactose
- Certain carbohydrates that contain fructose, known as FODMAPs
Summary
- Belching and flatulence are normal body processes.
- Swallowed air is “gas” in the body and contributes significantly to symptoms.
- Unabsorbed dietary carbohydrates can cause gas production by colon bacteria.
- Carbonated beverages, sucking on hard candy, and chewing gum should be avoided.
- Abdominal distension when erect but not recumbent may be due to weak abdominal muscles.
- Increasing frequency or severity of symptoms should prompt medical attention.
- Abdominal bloating. Medline Plus. https://medlineplus.gov/ency/article/003123.htm[↩]
- Bloating and Abdominal Distension: Old Misconceptions and Current Knowledge. Am J Gastroenterol 2017; 112: 1221–1231; doi:10.1038/ajg.2017.129; published online 16 May 2017. http://www.nature.com/ajg/journal/v112/n8/full/ajg2017129a.html[↩]
- Azpiroz F. Intestinal gas. In: Feldman M, Friedman LS, Brand LJ (eds). Pathophysiology, Diagnosis, Management 10th edn. Elsevier: Philadelphia, USA. 2015 pp 242–250.[↩][↩]
- Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features, and rome IV. Gastroenterology 2016;150:1262–1279.[↩]
- Tuteja AK, Talley NJ, Joos SK et al. Abdominal bloating in employed adults: prevalence, risk factors, and association with other bowel disorders. Am J Gastroenterol 2008;103:1241–1248. https://www.ncbi.nlm.nih.gov/pubmed/18422817[↩]
- Lembo T, Naliboff B, Munakata J et al. Symptoms and visceral perception in patients with pain-predominant irritable bowel syndrome. Am J Gastroenterol 1999;94:1320–1326. https://www.ncbi.nlm.nih.gov/pubmed/10235213[↩]
- Maxton DG, Martin DF, Whorwell P et al. Abdominal distension in female patients with irritable bowel syndrome: exploration of possible mechanisms. Gut 1991;32:662–664. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1378884/[↩]
- Furne JK, Levitt MD. Factors influencing frequency of flatus emission by healthy subjects. Dig Dis Sci 1996;41:1631–1635. https://www.ncbi.nlm.nih.gov/pubmed/8769291[↩]
- Longstreth GF, Thompson WG, Chey WD et al. Functional bowel disorders. Gastroenterology 2006;130:1480–1491. https://www.ncbi.nlm.nih.gov/pubmed/16678561[↩]
- McRorie J. Clinical data support that psyllium is not fermented in the gut. Am J Gastroenterol 2013;108:1541. https://www.ncbi.nlm.nih.gov/pubmed/24005363[↩][↩]
- Serra J, Azpiroz F, Malagelada J-R. Intestinal gas dynamics and tolerance in humans. Gastroenterology 1998;115:542–550. https://www.ncbi.nlm.nih.gov/pubmed/9721151[↩]
- Serra J, Azpiroz F, Malagelada J-R. Impaired transit and tolerance of intestinal gas in the irritable bowel syndrome. Gut 2001;48:14–19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1728167/pdf/v048p00014.pdf[↩]
- Serra J, Azpiroz F, Malagelada J-R. Mechanisms of intestinal gas retention in humans:impaired propulsion versus obstructed evacuation. Am J Physiol 2001;281:G138–G143.[↩][↩]
- Serra J, Salvioli B, Azpiroz F et al. Lipid-induced intestinal gas retention in the irritable bowel syndrome. Gastroenterology 2002;123:700–706. https://www.ncbi.nlm.nih.gov/pubmed/12198695[↩]
- Murray K, Wilkinson-Smith V, Hoad C et al. Differential effects of FODMAPs (fermentable oligo-, di-, mono-saccharides and polyols) on small and large intestinal contents in healthy subjects shown by MRI. Am J Gastroenterol 2014;109:110–119. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3887576/[↩]
- Guarner F, Malagelada JR. Gut flora in health and disease. Lancet 2003;361:512–519. https://www.ncbi.nlm.nih.gov/pubmed/12583961[↩]
- Mego M, Bendezu A, Accarino A et al. Intestinal gas homeostasis: disposal pathways. Neurogastroenterol Motil 2015;27:363–369.[↩]
- Mc Rorie J, Fahey G. Invited review article: a review of gastrointestinal physiology and the mechanisms underlying the health benefits of dietary fiber: matching an effective fiber with specific patients needs. Clin Nurs Stud 2017;1:82–92.[↩]
- Dainese R, Serra J, Azpiroz F et al. Effect of physical activity on intestinal gas transit and evacuation in healthy subjects. Am J Med 2004;116:536–539. https://www.ncbi.nlm.nih.gov/pubmed/15063815[↩]
- Azpiroz F. Functional abdominal bloating and gas. In: Talley NJ, Kane SV, Wallace M (eds). Practical Gastroenterology and Hepatology: Small and Large Intestine and Pancreas. Wiley-Blackwell: NJ, USA. 2010 pp 470–473.[↩]
- Azpiroz F, Hernandez C, Guyonnet D et al. Effect of a low-flatulogenic diet in patients with flatulence and functional digestive symptoms. Neurogastroenterol Motil 2014;26:779–785.[↩]
- Mego M, Accarino A, Malagelada JR et al. Accumulative effect of food residues on intestinal gas production. Neurogastroenterol Motil 2015;27:1621–1628.[↩]
- Bendezu RA, Barba E, Burri E et al. Colonic content in health and its relation to functional gut symptoms. Neurogastroenterol Motil 2016;28:849–854.[↩]
- Agrawal A, Houghton LA, Reilly B et al. Bloating and distension in irritable bowel syndrome: the role of gastrointestinal transit. Am J Gastroenterol 2009;104:1998–2004.[↩]
- Pritchard SE, Marciani L, Garsed KC et al. Fasting and postprandial volumes of the undisturbed colon: normal values and changes in diarrhea-predominant irritable bowel syndrome measured using serial MRI. Neurogastroenterol Motil 2014;26:124–130.[↩]
- Simren M, Barbara G, Flint HJ et al. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut 2013;62:159–176.[↩]
- Yao CK, Tan HL, van Langenberg DR et al. Dietary sorbitol and mannitol: food content and distinct absorption patterns between healthy individuals and patients with irritable bowel syndrome. J Hum Nutr Diet 2014;27 (Suppl 2): 263–275.[↩]
- Perez F, Accarino A, Azpiroz F et al. Gas distribution within the human gut: effect of meals. Am J Gastroenterol 2007;102:842–849.[↩][↩]
- Barba E, Quiroga S, Accarino A et al. Mechanisms of abdominal distension in severe intestinal dysmotility: abdomino-thoracic response to gut retention. Neurogastroenterol Motil 2013;25:e389-94.[↩]
- Hernando-Harder AC, Serra J, Azpiroz F et al. Colonic responses to gas loads in subgroups of patients with abdominal bloating. Am J Gastroenterol 2010;105:876–882.[↩]
- Houghton LA, Calvert EL, Jackson NA et al. Visceral sensation and emotion: a study using hypnosis. Gut 2002;51:701–704.[↩]
- Murray CD, Flynn J, Ratcliffe L et al. Effect of acute physical and psychological stress on gut autonomic innervation in irritable bowel syndrome. Gastroenterology 2004;127:1695–1703.[↩]
- Ghia JE, Blennerhassett P, Collins SM. Impaired parasympathetic function increases susceptibility to inflammatory bowel disease in a mouse model of depression. J Clin Invest 2008;118:2209–2218.[↩]
- Koloski NA, Jones M, Talley NJ. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Aliment Pharmacol Ther 2016;44:592–600.[↩]
- Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 2006;444:840–846.[↩]
- Accarino AM, Azpiroz F, Malagelada JR. Attention and distraction: effects on gut perception. Gastroenterology 1997;113:415–422.[↩]
- Altman G, Cain KC, Motzer S et al. Increased symptoms in female IBS patients with dysmenorrhea and PMS. Gastroenterol Nurs 2006;29:4–11.[↩]
- Houghton LA, Lea R, Jackson N et al. The menstrual cycle affects rectal sensitivity in patients with irritable bowel syndrome but not healthy volunteers. Gut 2002;50:471–474.[↩]
- Lobo B, Serra J, D’Amato M et al. Selective CCK receptor antagonism enhances accommodation and tolerance of intestinal gas in functional gut disorders. J Gastroenterol Hepatol 2015;31:288–293.[↩]
- Shim L, Prott G, Hansen RD et al. Prolonged balloon expulsion is predictive of abdominal distension in bloating. Am J Gastroenterol 2010;105:883–887.[↩]
- Bishehsari F, Levi F, Turek FW et al. Circadian rhythms in gastrointestinal health and diseases. Gastroenterology 2016;151:e1–e5.[↩]
- Maxton DG, Martin DF, Whorwell P et al. Abdominal distension in female patients with irritable bowel syndrome: exploration of possible mechanisms. Gut 1991;32:662–664.[↩]
- Lewis M, Reilly B, Houghton L et al. Ambulatory abdominal inductance plethysmography: towards objective assessment of abdominal distension in irritable bowel syndrome. Gut 2001;48:216–220.[↩]
- Villoria A, Azpiroz F, Soldevilla A et al. Abdominal accommodation: a coordinated adaptation of the abdominal walls to its content. Am J Gastroenterol 2008;103:2807–2815.[↩]
- Villoria A, Azpiroz F, Burri E et al. Abdomino-phrenic dyssynergia in patients with abdominal bloating and distension. Am J Gastroenterol 2011;106:815–819.[↩]
- Burri E, Barba E, Huaman JW et al. Mechanisms of postprandial abdominal bloating and distension in functional dyspepsia. Gut 2014;63:395–400.[↩]





