Contents
What is achalasia
Achalasia from the Greek for ‘does not relax’, also known as cardiospasm, is a neurodegenerative motility disorder of the esophagus resulting in deranged esophageal peristalsis and loss of lower esophageal sphincter function 1. Instead of food and drink moving normally through the esophagus when you swallow, in people with achalasia they can get stuck there, or even come back up into the mouth.
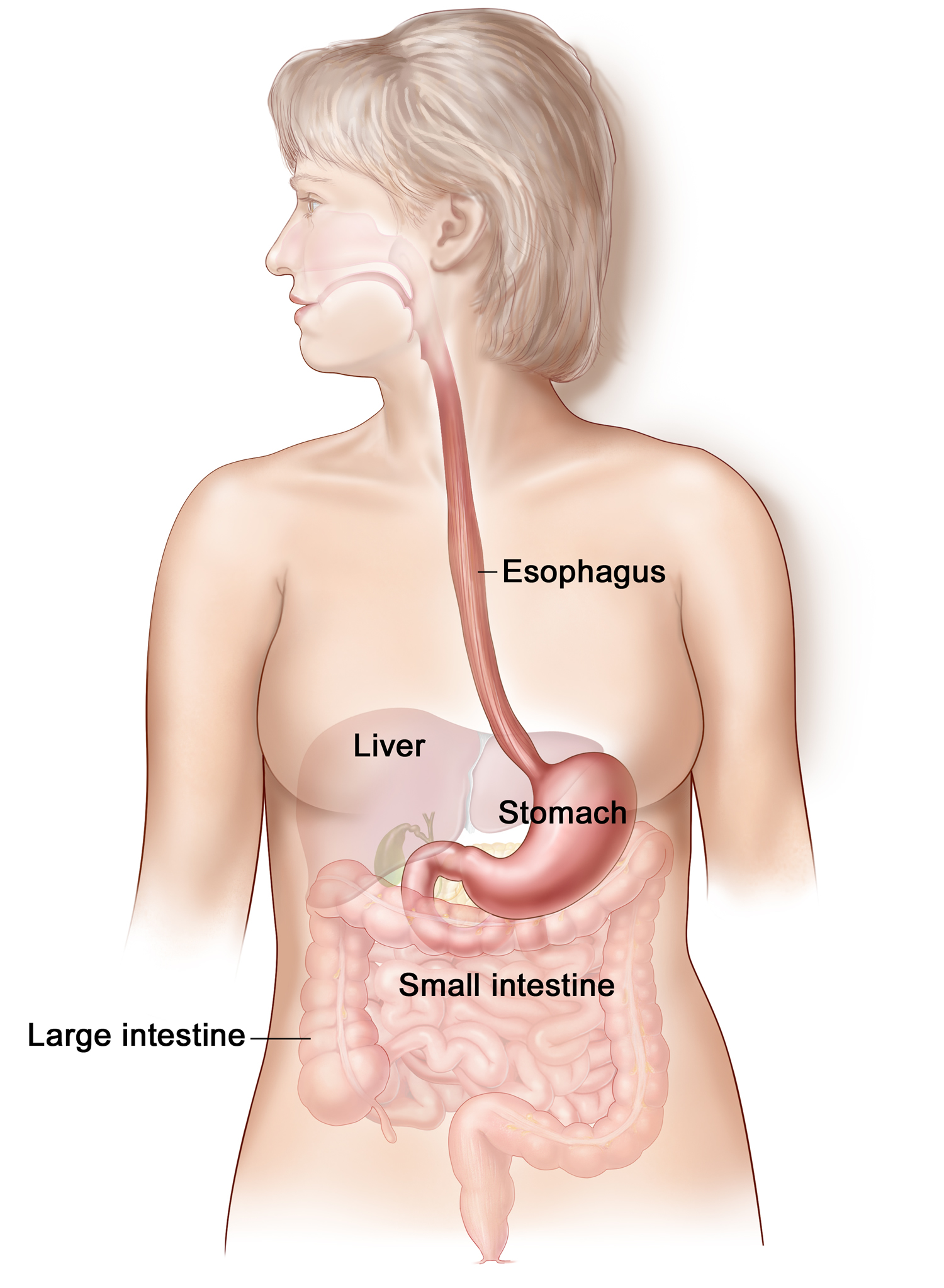
Under normal circumstances, when you swallow, food passes down the esophagus by waves of muscle contractions and through a special valve into the stomach.
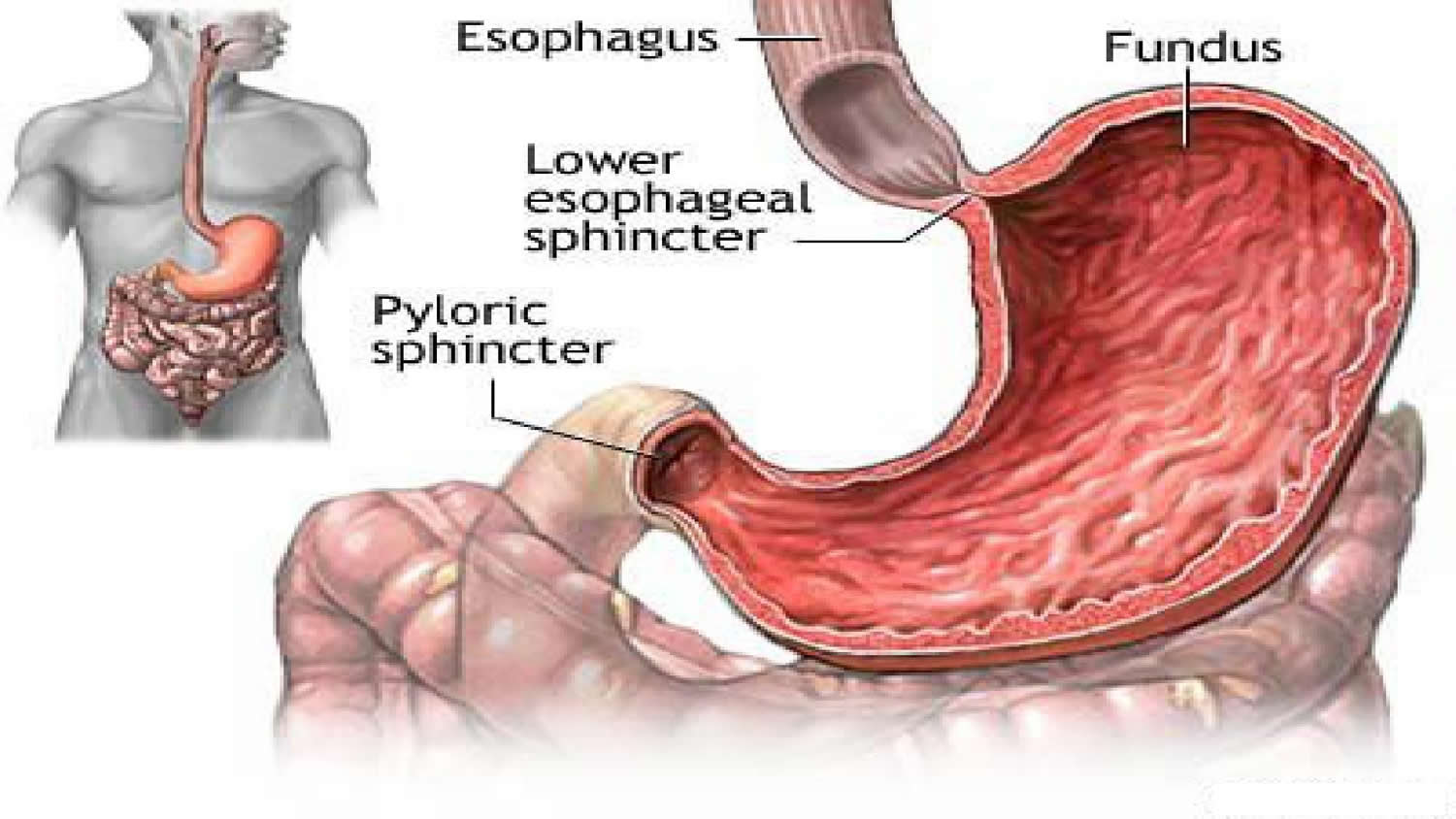
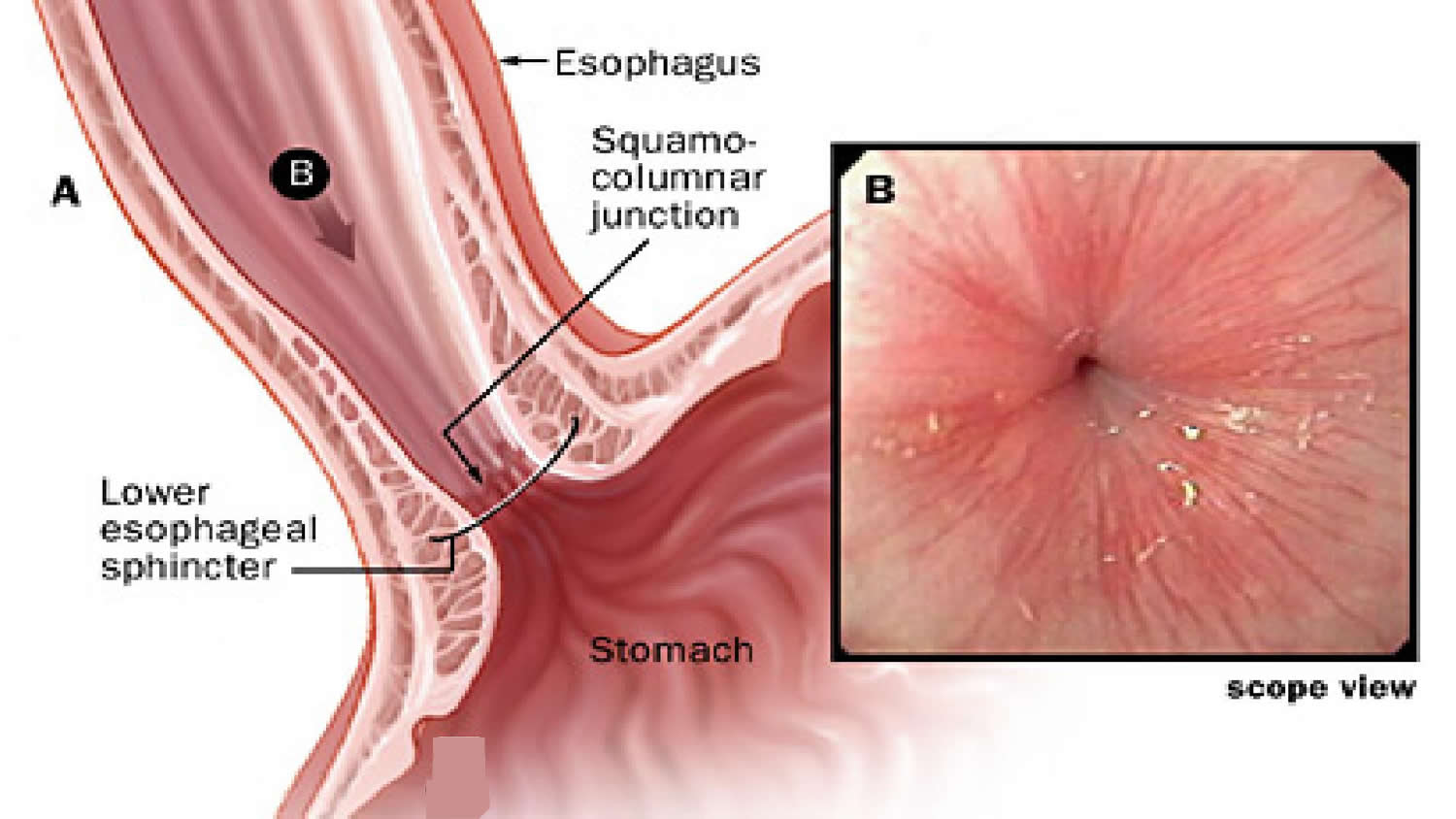
The valve – a ring of muscle called the lower esophageal sphincter (see Figures 2 and 3)– controls the entry of food from the lower end of the esophagus into the stomach. If you have achalasia, the nerves that control this sphincter are affected, preventing it from relaxing and allowing food to pass through.
Achalasia also affects the muscular contractions of the esophagus (peristalsis), which normally work to propel food down towards the stomach. This is thought to be due to a malfunction of the nerves around the esophagus.
The pathogenesis of achalasia is not well understood but it is believed to be due to an inflammatory neurodegenerative insult with possible viral involvement. The measles and herpes viruses have been suggested as candidate viruses however molecular techniques have failed to confirm these claims and therefore the causative agent remains undiscovered 2. Genetic and autoimmune components have also been suggested as origins of the neuronal damage however research to date has not found the exact cause 3. Inflammatory changes within the esophagus following the causative insult result in the loss of postganglionic inhibitory neurons in the myenteric plexus and a consequent reduction in the inhibitory transmitters, nitric oxide and vasoactive intestinal peptide. The excitatory neurons remain unaffected, with the resulting imbalance between excitatory and inhibitory neurons preventing lower esophageal sphincter relaxation 4. Lack of peristalsis and a non-relaxing lower esophageal sphincter cause progressive dysphagia. Regurgitation, particularly at night, with aspiration of undigested food and weight loss can be presenting features, particularly in established disease. Features which present in the early stages of the disease may be similar to that of gastro-esophageal reflux (GERD), including retrosternal chest pain typically after eating and heartburn 5. Due to initial non-specific symptoms in early stage disease and the low prevalence of achalasia worldwide, the condition often goes undiagnosed for many years, giving rise to features of late stage disease and their associated complications.
Historically, annual achalasia incidence rates were believed to be low, approximately 0.5-1.2 per 100000. More recent reports suggest that annual incidence rates have risen to 1.6 per 100,000 in some populations. Achalasia affects men and women equally between the ages of 30-60. It can also occur in infancy and childhood.
The cause of achalasia is still unknown (idiopathic), but is likely to be multi-factorial. Suggested causes include environmental or viral exposures resulting in inflammation of the esophageal myenteric plexus, which elicits an autoimmune response 1. However, Achalasia can also develop as a result of damage to the nerves to the esophagus. This is seen in chronic Chagas disease – a condition common in South America which is caused by the Trypanosoma cruzi parasite.
Achalasia can happen at any age, but is more common in middle-aged or older adults. While there is no cure currently available, there are treatments that can help manage the symptoms.
Achalasia is a progressive disease meaning patients will gradually develop increasing severity of difficulty when swallowing. Medical treatment may alleviate symptoms but they do not provide a long term solution.
Most patients require surgical intervention. Those who are treated early (before marked dilation) may avoid complications of esophageal ulceration, esophageal candidiasis and aspirating stomach contents into the lung. There is also a slight increase in the risk of esophageal carcinoma (cancer of the esophagus). There are limited data to support routine screening for cancer. The overall number of cancers remains low and estimates have suggested that over 400 endoscopies would be required to detect one cancer 6. These numbers are further tempered by the fact that the survival of these patients is poor once the diagnosis is made 7.
With successful myotomy (surgery dividing the abnormal muscle in the lower sphincter of the esophagus), patients are able to gain weight and lead a normal life. Some will develop gastro-esophageal reflux (GERD), especially after surgery which responds to medical treatment. Some recommend endoscopic monitoring for the increased risk of esophageal carcinoma.
Figure 1. Esophagus
Figure 2. Lower esophageal sphincter
Figure 3. lower esophageal sphincter (endoscopic view)
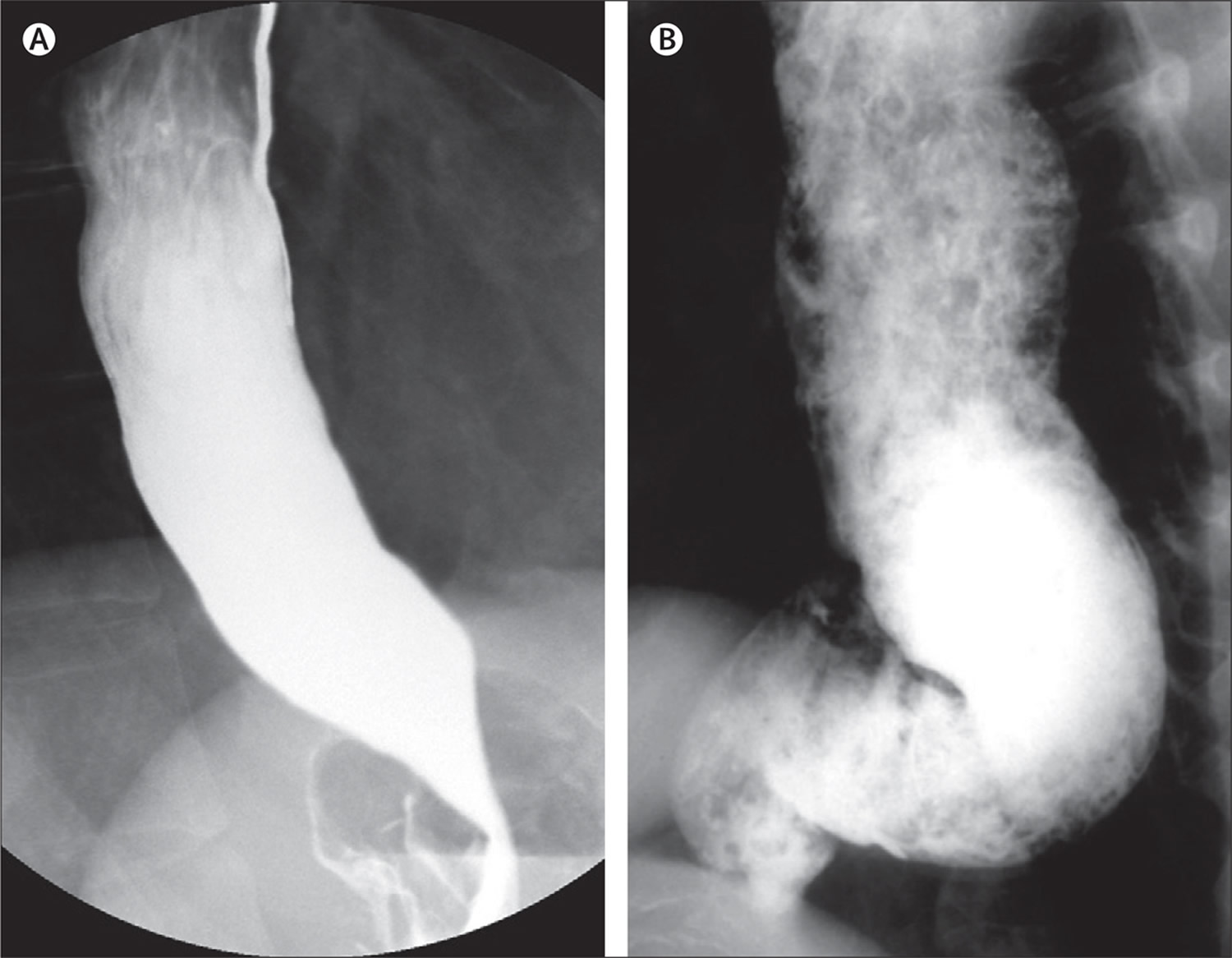
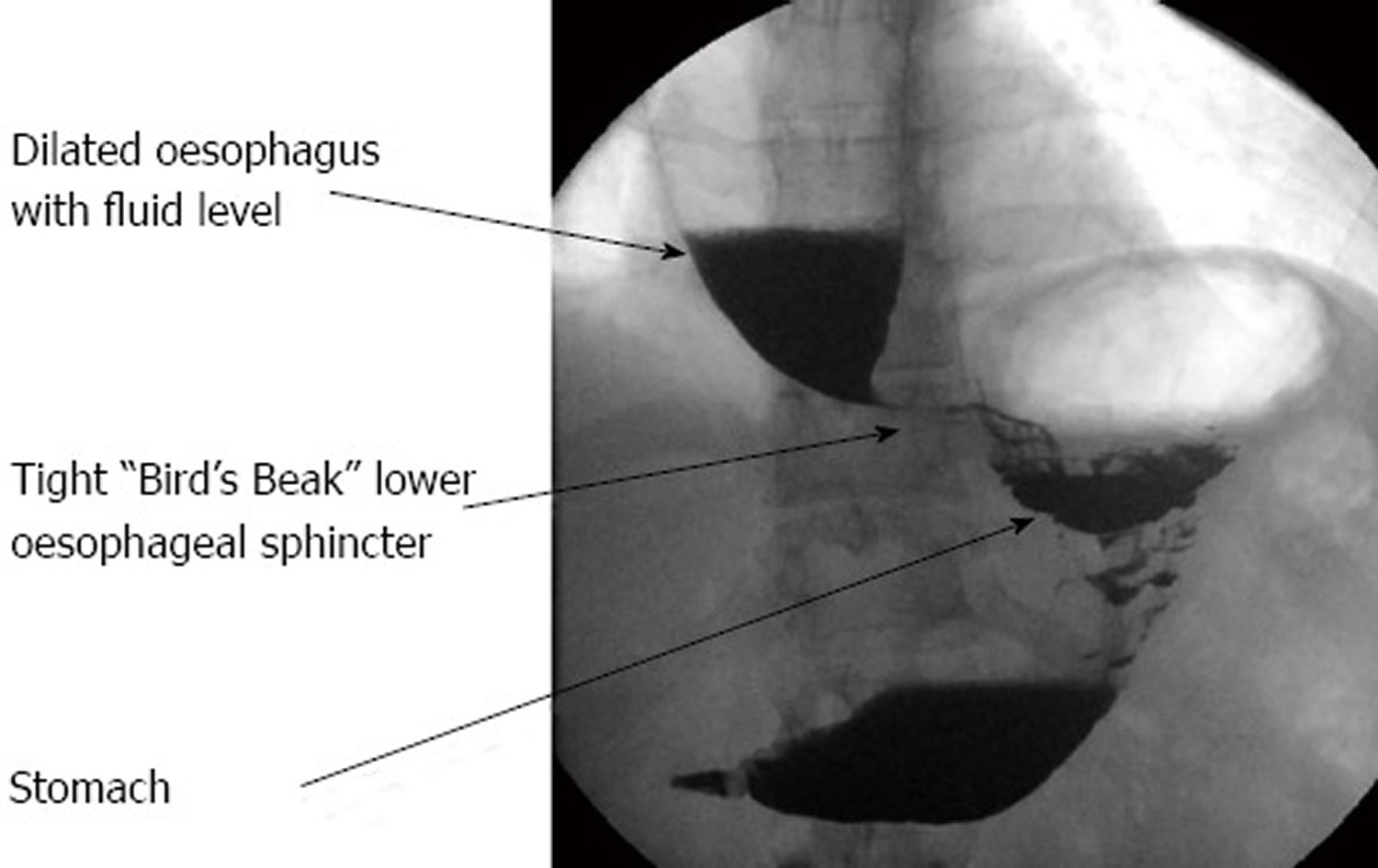
Figure 4. Esophageal achalasia (Barium swallow)
Note: Barium swallow demonstrating typical “bird’s-beak” appearance of the lower oesophageal sphincter in achalasia. The oesophagus above this is dilated.
Achalasia types
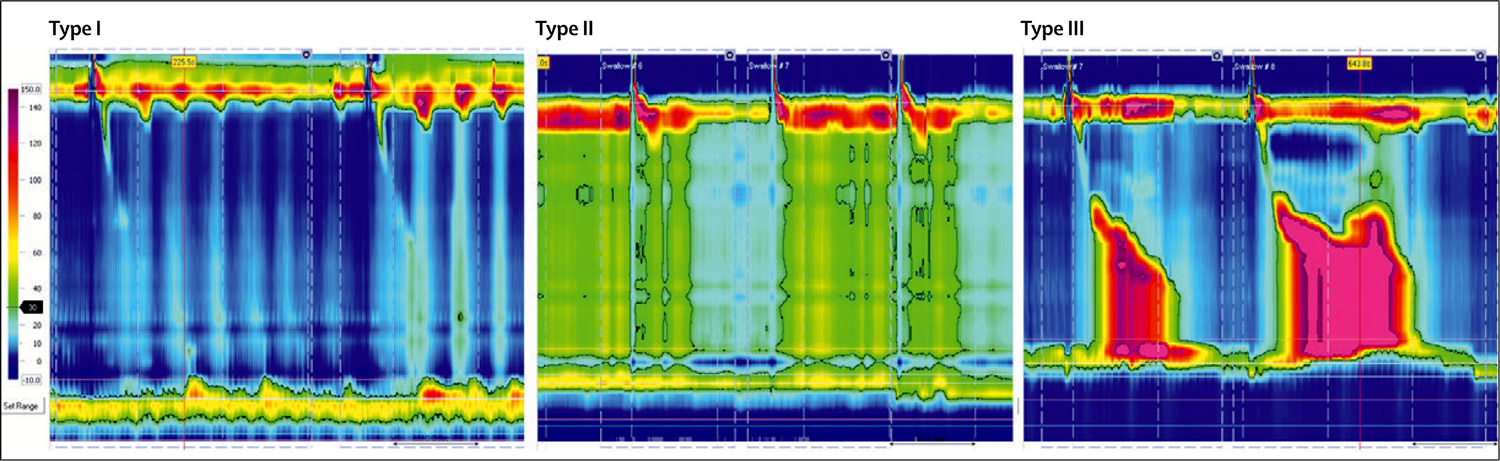
The use of high-resolution manometry has led to the subclassification of achalasia into three clinically relevant groups on the basis of the pattern of contractility in the oesophageal body 8 or variants with potential treatment outcome implications 9. To date, three separate retrospective cohort studies have shown that subtype II has the best prognosis, whereas subtype I is somewhat lower and subtype III can be difficult to treat 9. Although these subtypes can be defined with careful analysis of conventional tracings, it is easier and more reproducible with high-resolution manometry.
On the basis of the information reported to date, the evidence clearly confirms that the subtype of achalasia is an independent predictor of success, with type III having the worst outcome after therapy. To what extent the subtypes represent different phenotypes or simply reflect different stages of the disease is hard to say. Recent detailed analyses of high-resolution manometry tracings, combined with impedance and ultrasound images, seem to suggest that type III and type I achalasia, respectively, represent the feature of a compensated and decompensated esophagus to outflow obstructions caused by a dysfunctional lower esophageal sphincter 10. The pressurization pattern typical of type II achalasia, on the other hand, stems from another, novel motor response of the esophagus involving longitudinal muscle contractions of the distal esophagus.
Be that as it may, it seems fair to conclude that type III achalasia, characterized by well-defined, lumen-obliterating spastic contractions in the distal esophagus, responds the least to therapy. In this subgroup of achalasia patients, reducing the lower esophageal sphincter pressure may not suffice to control the symptoms, especially as the segment affected by the spastic motility extends well above the lower esophageal sphincter. Chest pain, a prominent symptom in type III achalasia patients (probably associated with spastic contractions), is especially difficult to treat, explaining the lower success rates in these patients. The response to therapy in type II is rather better than that in type I, but in the European Achalasia Trial, at least there were apparently no major differences in the success rate for these subtypes between pneumatic dilation and laparoscopic Heller myotomy.
Future outcome studies are needed to determine the clinical impact of the three subtypes.
- Type I (classical achalasia; no evidence of pressurisation) achalasia is associated with absent peristalsis and minimal esophageal body pressurization.
- Type II achalasia is associated with panesophageal pressurization related to a compression effect.
- Type III achalasia has evidence of abnormal contractility (spastic).
Figure 5. Manometric types of achalasia
Note: Type I is characterised by absence of distal pressurisation to greater than 30 mm Hg. In type II, pressurisation to greater than 30 mm Hg occurs in at least two of ten test swallows, whereas patients with type III disease have spastic contractions with or without periods of compartmentalized pressurisation.
[Source 11Prognosis of achalasia
Surgery often results in longer lasting relief of symptoms, while dilation alone (done at endoscopy) often results in only temporary improvement in symptoms. There is a slightly increased risk of esophageal cancer.
Complications of achalasia
Many people with achalasia delay going to the doctor and getting a diagnosis because their symptoms are not causing major discomfort. However, if you think you may have achalasia, it’s important that you seek medical advice and treatment, because doctors believe the condition may slightly increase the risk of cancer of the esophagus.
Other complications of achalasia can arise because of undigested food being regurgitated during sleep. If the food is accidentally inhaled into the lungs, this can lead to pneumonia, an abscess of the lung, or damage to the bronchial tubes.
Achalasia can also lead to inflammation of the esophagus (esophagitis).
Achalasia causes
The causes of achalasia are not well understood. Often when someone develops the disorder, there is no obvious reason why the nerves in their oesophagus no longer work properly.
Suspected possible causes of achalasia include:
- viral infections that damage the nerves of the esophagus (this may happen earlier in life, rather than at the time of developing achalasia)
- autoimmune conditions (when the immune system attacks the body’s own cells)
- Chagas disease – an infectious disease that can destroy nerve cells 12.
Some people seem to be more susceptible to developing achalasia, including people with Parkinson’s disease.
There has been much debate over the cause of achalasia, with several potential triggers for the inflammatory destruction of inhibitory neurons in the oesophageal myenteric plexus being implicated. These include autoimmune responses, infectious agents and genetic factors.
Auto-immune conditions
One recent study observed that patients with achalasia were 3.6 times more likely to suffer an autoimmune condition, compared with the general population 13. Sjogren’s syndrome, Systemic Lupus Erythematosus and uveitis were all significantly more prevalent in achalasia patients. The study also found the presence of a T-cell (T lymphocyte) infiltrate and antibodies within the myenteric plexus of many patients with achalasia and an increased presence of human leukocyte antigen class II antigens 13. Another study noted an overall higher prevalence of neural autoantibodies in patients with achalasia in comparison with a healthy control group 14. Although no specific autoantibody was identified, this further supports the theory that achalasia has an autoimmune basis 14.
Infectious agents
The role of an infectious agent in the development of achalasia has been widely debated with several viral agents being implicated. For example, Chagas disease has a known infectious aetiology, and exhibits many similarities with achalasia 12. In addition, there are several reports of varicella zoster virus and Guillain-Barre syndrome preceding the onset of achalasia 12. Antibody studies have demonstrated increased titres to herpes and measles viruses in patients with achalasia in comparison to healthy control groups 15. One study looking specifically at the link between the herpes simplex virus (HSV) and primary achalasia indicated the presence of HSV-1 reactive immune cells in the lower oeseophageal sphincter of achalasia patients, suggesting that HSV-1 may be involved in the neuronal damage to the myenteric plexus leading to achalasia 16. A further study of peripheral blood immune cells found that patients with achalasia showed an enhanced response to HSV-1 antigens 17. In contrast, another investigation using PCR on myotomy specimens did not find any association between herpes, measles or human papilloma viruses and achalasia 18. The current evidence for a causative infectious agent is contradictory and no clear causal relationship has yet been established.
Genetic predisposition
The genetic basis for achalasia has not been widely investigated due to its low prevalence. One syndrome, known as the triple “A” syndrome, which consists of a triad of achalasia, alacrima and adrenocorticotrophic hormone resistant adrenal insufficiency is a known autosomal recessive disorder caused by gene mutations on chromosome 12. This syndrome, together with the prevalence of cases within children of consanguineous couples 19, suggests the possibility for a genetic component to the aetiology of achalasia. There have been associations with other genetic diseases including Parkinson’s disease, Downs syndrome and MEN2B syndrome 20. One recent suggested the possibility of involvement of the rearranged during transfection gene, which is a major susceptibility gene for Hirschprung’s disease (also linked with Down’s syndrome) 21. Mayberry et al 22 conducted a study of first degree relatives of achalasia patients but concluded that inheritance was unlikely to be a significant causative factor due to the rarity of familial cases and exposure to common environmental and social factors within a family group may explain the presence of familial cases of achalasia.
It has been postulated that achalasia may incorporate a multi-factorial aetiology with an initiating event such as a viral or environmental insult resulting in oesophageal myenteric plexus inflammation. This inflammatory reaction may then initiate an autoimmune response in a susceptible group of genetically predisposed people, causing destruction of inhibitory neurons 23.
Achalasia symptoms
The symptoms of achalasia often start slowly and progress gradually, sometimes taking years to fully develop. They include:
- difficulty swallowing (dysphagia), which can be painful
- a lump or feeling of fullness in the throat
- chest pain
- heartburn
- regurgitation of undigested food or liquids (including when asleep)
- coughing or choking (due to regurgitation of food), which may be worse at night
- hiccups
- difficulty burping
- weight loss.
The most frequently occurring symptoms of achalasia are dysphagia (>90%) for solids and liquids, regurgitation of undigested food (76–91%), respiratory complications (nocturnal cough [30%] and aspiration [8%]), chest pain (25–64%), heartburn (18–52%), and weight loss (35–91%) 24.
Heartburn can lead to an erroneous diagnosis of gastro-esophageal reflux disease (GERD), which might culminate in antireflux surgery. Nocturnal coughing mainly occurs in patients with substantial stasis of large amounts of food and secretions. Chest pain is predominantly present in patients with type III disease 25 and responds less well to treatment than do dysphagia and regurgitation, which probably explains the less favourable therapeutic results obtained in patients with type III disease compared with those with type I or II disease 26. However, symptoms of achalasia are not specific, which explains the long delay between onset of symptoms and the final diagnosis (up to 5 years in some studies) 27. Although some patients lose a lot of weight (more than 20 kg), achalasia should also be considered in obese patients 28.
Achalasia diagnosis
Achalasia can be diagnosed in a number of ways. If your doctor thinks you may have achalasia, you will be referred to a hospital where a specialist called a gastroenterologist may do one or more of the following diagnostic tests.
Barium swallow
The ‘barium swallow’ is a common test for achalasia. This involves drinking a thick liquid containing the chemical barium, which coats the inside of your esophagus and stomach, making them show up on an X-ray. In people with achalasia, the test often shows that the lower part of the esophagus has narrowed, while an area above this has become stretched or enlarged. The specialist will also be able to see whether the muscle contractions of the esophagus (peristalsis) are working normally or not.
Gastrografin swallow
A Gastrografin swallow is similar to a barium swallow – you have to swallow a liquid which contains an X-ray contrast medium – this shows up on X-ray and shows the esophagus, including the outline of the inside of the esophagus. Gastrografin is often used when a barium meal can’t be used. Gastrografin is less irritating to the body if there is a leak from the esophagus, such as from a tear.
Esophageal Manometry
Another investigation that can be used in the diagnosis of achalasia is esophageal manometry. In this test, a thin tube with pressure gauges along its surface is inserted through the mouth or nose into the esophagus. As you swallow small sips of water, the instrument measures the pressure along your esophagus.
In a person with achalasia, the test usually shows that the muscular contractions needed to pass food along the esophagus are weak or missing, and that the lower esophageal sphincter is not relaxing as it should after you swallow. The sphincter may also have higher than normal pressure.
Endoscopy (gastroscopy)
An endoscope (a flexible tube with a light and camera on the end) can be used to examine the esophagus.
If you have achalasia, this may show that the esophagus is wider than normal. It would also show if there were any obstructions in the esophagus or stomach.
During the test, the specialist may take a sample of tissue (a biopsy) from your esophagus or stomach to examine in the laboratory for any abnormalities.
Achalasia treatment
Achalasia is treated by a gastroenterologist, who deals with problems of the digestive tract.
While treatments can’t repair damaged nerves or restore normal contractions in the esophagus, they can often improve the symptoms of achalasia. They do this by weakening the sphincter at the base of the esophagus, so that food is able to pass through to the stomach.
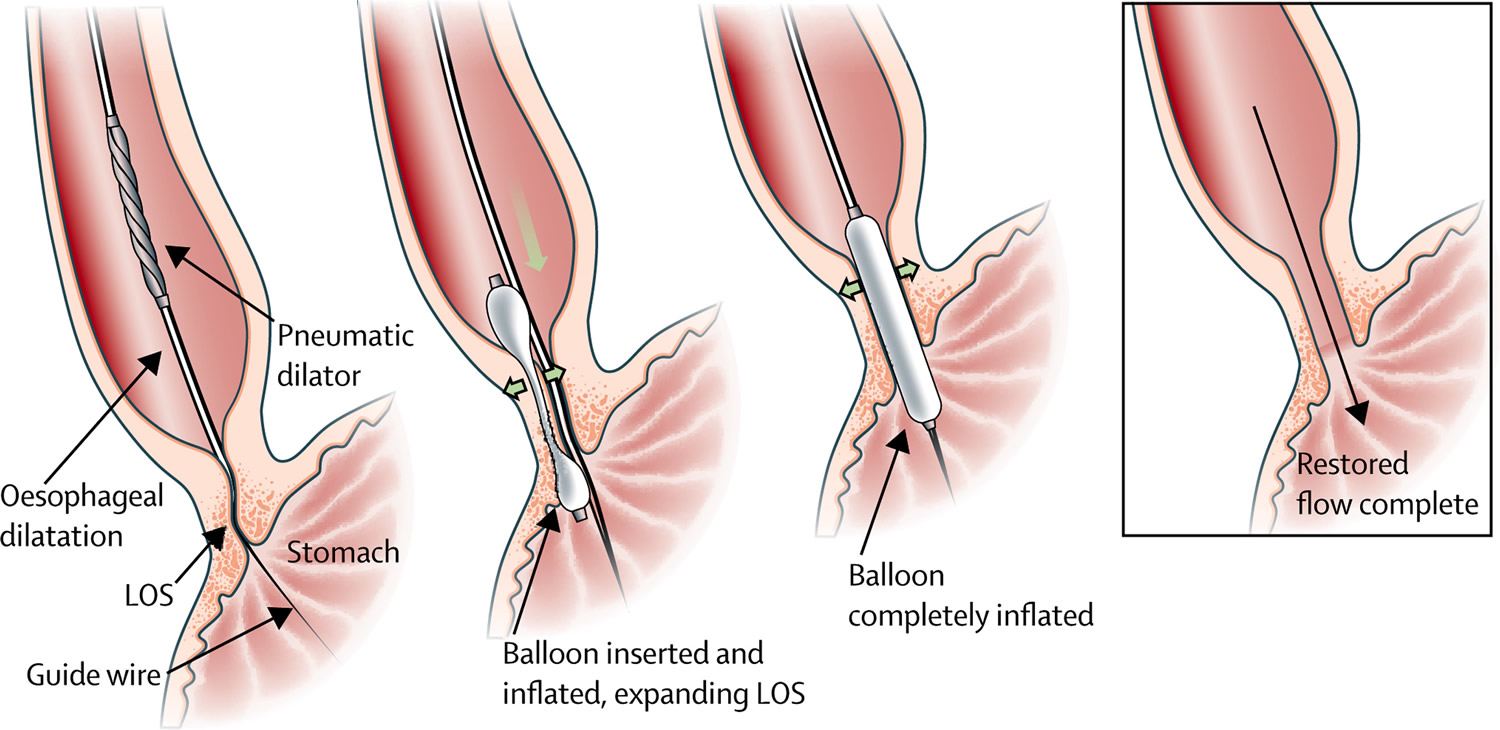
Balloon dilation
Often one of the first approaches used to treat achalasia is dilation or stretching of the sphincter at the base of the esophagus. This is done by putting a small balloon inside the sphincter and inflating it.
Unfortunately, there is a risk during this procedure that the esophagus can rupture or tear. The dilation process may also need to be repeated, as it can stop having the desired effect after a while, and this further increases the risk of rupture.
This outpatient procedure may need to be repeated if the esophageal sphincter doesn’t stay open. Nearly one-third of people treated with balloon dilation need repeat treatment within six years.
Figure 6. Balloon (pneumatic) dilation
Note: Schematic representation of the pneumodilatation procedure. The deflated balloon is inserted over a guide wire, after which the slightly inflated balloon is positioned at the oesophagogastric junction with the indentation still visible. Finally, the balloon is fully inflated and the indentation disappears. After removal of the balloon, the LOS is distended, allowing adequate passage. LOS=lower oesophageal splinter.
Medications
There are no medicines in US to specifically treat achalasia, although sometimes medicines may be prescribed to help relax the lower esophageal sphincter. These include nitrates (such as glyceryl trinitrate) and calcium channel blockers (such as nifedipine), which are also used to treat high blood pressure and angina.
Medications are generally considered only if you’re not a candidate for pneumatic dilation or surgery, and Botox hasn’t helped.
While these medications may help relieve some of the symptoms of achalasia temporarily, they are not effective in all cases, and tend to stop working over time. They can also cause unwanted side effects such as headaches and low blood pressure. For these reasons, they are often only used for people who are unable to have other forms of treatment.
Botulinum toxin
Botulinum toxin (Botox) is a nerve toxin that is well-known for its ability to relax muscles, including those causing facial frown lines and wrinkles. When used in the treatment of achalasia, Botulinum toxin is injected directly into the lower esophageal sphincter via an endoscope. Although the procedure is relatively safe, it only provides temporary relief (usually for 3 to 12 months) and its long-term effects are not yet known.
Repeat Botulinum toxin injections may make it more difficult to perform surgery later if needed. Botox is generally recommended only for people who aren’t good candidates for pneumatic dilation or surgery due to age or overall health.
Achalasia surgery
Surgery may be recommended for younger people because nonsurgical treatment tends to be less effective in this group.
Surgical options include:
- Heller myotomy
Surgery can be done to decrease the pressure in the lower sphincter of the esophagus, using a procedure called myotomy (or Heller myotomy). This type of surgery is generally reserved for cases where achalasia does not respond to treatment using balloon dilation. During the myotomy, the surgeon cuts the lower esophageal sphincter muscle to release the tension. The surgery is done laparoscopically (using small abdominal incisions to pass a camera and surgical instruments through) and under a general anesthetic.
Although the operation is successful in about 85 per cent of cases, up to 20 per cent of people develop a condition called gastro-esophageal reflux disease (GERD) after surgery, which causes acid in the stomach to rise into the esophagus and can cause heartburn.
- Fundoplication
The surgeon wraps the top of your stomach around the lower esophageal sphincter, to tighten the muscle and prevent acid reflux. Fundoplication might be performed at the same time as Heller myotomy, to avoid future problems with acid reflux. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure.
- Peroral endoscopic myotomy (POEM)
A new operation known as peroral endoscopic myotomy (POEM) has recently been developed, but is still being tested for its effectiveness compared to standard treatments.
The surgeon uses an endoscope inserted through your mouth and down your throat to create an incision in the inside lining of your esophagus. Then, as in a Heller myotomy, the surgeon cuts the muscle at the lower end of the esophageal sphincter. POEM doesn’t include an anti-reflux procedure.
- Oesophagectomy for end-stage achalasia
Despite the efficacy of pneumodilatation and laparoscopic Heller myotomy, 2–5% of patients will develop end-stage disease 29, defined as a massive dilatation of the esophagus with retention of food, unresponsive reflux disease, or the presence of preneoplastic lesions 30. In these cases, esophageal resection might be necessary to improve the patient’s quality of life and avoid the risk of invasive carcinoma. The risk of needing esophagectomy is higher if the esophagus is already markedly dilated at the first intervention than if it is mildly dilated (<4 cm) 31.
The ideal reconstruction method after esophagectomy has not yet been established. Gastric interposition has the advantage of needing only one anastomosis, but gastro-esophageal reflux can cause severe damage if the anastomosis is intrathoracic. If a total esophagectomy is done and the anastomosis is in the neck, the critical vascular supply to the gastric tube can be compromised, resulting in anastomotic leakage and stricture 31. Alternatively, a long colonic interposition can be constructed, but anastomotic failure or stricture due to ischemia might occur. Short-segment colon interposition with an intrathoracic anastomosis might be a valid option in such patients. In a recent review that included 295 patients,119 an optimum outcome (defined as unrestricted or regular diet) was present in 65–100% of patients at a medium follow-up of 44 months (range 25–72), irrespective of the technique used.
Achalasia diet
The management of a person with achalasia and nutritional problems is very similar to that of patients with dysphagia (difficulty swallowing) due to neurologic disease or esophagogastric cancer 32. Oral feeding has relevant psychosocial significance to patients and their families, and should be continued whenever possible. In some patients, oral intake is often not adequate even in the absence of significant swallowing difficulties. In mild to moderate achalasia, nutrition is generally mildly affected and if the family encourages the patient to follow dietary modifications, loss of weight and malnutrition rarely occurs.
Dysphagia diets should be highly individualized, including modification of food texture or fluid viscosity. Food may be chopped, minced, or puréed, and fluids may be thickened 33.
If a person is unable to eat or drink or to consume sufficient quantities of food, or the risk of pulmonary aspiration is high, tube feeding should be provided. If there is a possibility for surgical myotomy, enteral nutrition via a nasal feeding tube will be adequate as a provisional measure, considering that a malnourished patient is always at major risk for postoperative complications. In very rare and selected cases of end-stage achalasia, in which there is any further possibility of surgery or pneumatic dilation, the insertion of the feeding tube through a percutaneous radiologic gastrostomy rather than a surgical gastrostomy would be the treatment of choice. Percutaneous gastric tube feeding is effective and usually acceptable to patients and their carers. Long-term complications include tube obstruction and wound infection. In some patients who are fed via a gastric tube, pulmonary aspiration may occur and routine intrajejunal feeding has been suggested for these cases 34.
- O’Neill OM, Johnston BT, Coleman HG. Achalasia: A review of clinical diagnosis, epidemiology, treatment and outcomes. World Journal of Gastroenterology : WJG. 2013;19(35):5806-5812. doi:10.3748/wjg.v19.i35.5806. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3793135/[↩][↩]
- Boeckxstaens GE. Achalasia: virus-induced euthanasia of neurons. Am J Gastroenterol. 2008;103:1610–1612. https://www.nature.com/articles/ajg2008334[↩]
- Gockel I, Müller M, Schumacher J. Achalasia–a disease of unknown cause that is often diagnosed too late. Dtsch Arztebl Int. 2012;109:209–214. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3329145[↩]
- Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005;100:1404–1414. https://www.nature.com/articles/ajg2005241[↩]
- Francis DL, Katzka DA. Achalasia: update on the disease and its treatment. Gastroenterology. 2010;139:369–374. https://www.ncbi.nlm.nih.gov/pubmed/20600038[↩]
- Sandler RS, Nyrén O, Ekbom A, Eisen GM, Yuen J, Josefsson S. The risk of esophageal cancer in patients with achalasia: a population-based study. JAMA. 1995;274:1359–1362. doi: 10.1001/jama.1995.03530170039029. https://www.ncbi.nlm.nih.gov/pubmed/7563560[↩]
- Leeuwenburgh I, Scholten P, Alderliesten J, et al. Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol. 2010;105:2144–2149. doi: 10.1038/ajg.2010.263. https://www.ncbi.nlm.nih.gov/pubmed/20588263[↩]
- Pandolfino, JE, Kwiatek, MA, Nealis, T et al. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008; 135: 1526–1533 http://www.gastrojournal.org/article/S0016-5085(08)01332-2/fulltext[↩]
- AGA technical review on the clinical use of esophageal manometry. Pandolfino JE, Kahrilas PJ, American Gastroenterological Association. Gastroenterology. 2005 Jan; 128(1):209-24. http://www.gastrojournal.org/article/S0016-5085(04)02004-9/fulltext[↩][↩]
- Hong SJ, Bhargava V, Jiang Y, DeBoer D, Mittal RK. A unique esophagealmotor pattern that involves longitudinal is responsible for emptying in achalasia esophagus. Gastroenterology 2010; 139: 102–11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2950263[↩]
- Boeckxstaens, G and Zaninotto, G. Achalasia and esophago-gastric junction outflow obstruction: focus on the subtypes. Neurogastroenterol Motil. 2012; 24: 27–31 http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2982.2011.01833.x/full[↩]
- Ghoshal UC, Daschakraborty SB, Singh R. Pathogenesis of achalasia cardia. World J Gastroenterol. 2012;18:3050–3057. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3386318/[↩][↩][↩]
- Booy JD, Takata J, Tomlinson G, Urbach DR. The prevalence of autoimmune disease in patients with esophageal achalasia. Dis Esophagus. 2012;25:209–213. https://www.ncbi.nlm.nih.gov/pubmed/21899655[↩][↩]
- Kraichely RE, Farrugia G, Pittock SJ, Castell DO, Lennon VA. Neural autoantibody profile of primary achalasia. Dig Dis Sci. 2010;55:307–311. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2819289/[↩][↩]
- Aetiology of achalasia. http://bestpractice.bmj.com/topics/en-gb/872[↩]
- Castagliuolo I, Brun P, Costantini M, Rizzetto C, Palù G, Costantino M, Baldan N, Zaninotto G. Esophageal achalasia: is the herpes simplex virus really innocent. J Gastrointest Surg. 2004;8:24–30; discussion 30. https://www.ncbi.nlm.nih.gov/pubmed/14746832[↩]
- Lau KW, McCaughey C, Coyle PV, Murray LJ, Johnston BT. Enhanced reactivity of peripheral blood immune cells to HSV-1 in primary achalasia. Scand J Gastroenterol. 2010;45:806–813. https://www.ncbi.nlm.nih.gov/pubmed/20438398[↩]
- Birgisson S, Galinski MS, Goldblum JR, Rice TW, Richter JE. Achalasia is not associated with measles or known herpes and human papilloma viruses. Dig Dis Sci. 1997;42:300–306. https://www.ncbi.nlm.nih.gov/pubmed/9052510[↩]
- Kaar TK, Waldron R, Ashraf MS, Watson JB, O’Neill M, Kirwan WO. Familial infantile oesophageal achalasia. Arch Dis Child. 1991;66:1353–1354. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1793307/pdf/archdisch00644-0093.pdf[↩]
- Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005;100:1404–1414. https://www.ncbi.nlm.nih.gov/pubmed/15929777[↩]
- Gockel I, Müller M, Schumacher J. Achalasia–a disease of unknown cause that is often diagnosed too late. Dtsch Arztebl Int. 2012;109:209–214. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3329145/[↩]
- Mayberry JF, Atkinson M. A study of swallowing difficulties in first degree relatives of patients with achalasia. Thorax. 1985;40:391–393. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC460073/pdf/thorax00233-0071.pdf[↩]
- Chuah SK, Hsu PI, Wu KL, Wu DC, Tai WC, Changchien CS. 2011 update on esophageal achalasia. World J Gastroenterol. 2012;18:1573–1578. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3325522[↩]
- Achalasia. Boeckxstaens, Guy E et al. The Lancet 4 January 2014, Volume 383 , Issue 9911 , 83 – 93[↩]
- Rohof, WO, Salvador, R, Annese, V et al. Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology. 2013; 144: 718–725 https://www.ncbi.nlm.nih.gov/pubmed/23277105[↩]
- Eckardt, VF, Stauf, B, and Bernhard, G. Chest pain in achalasia: patient characteristics and clinical course. Gastroenterology. 1999; 116: 1300–1304 http://www.gastrojournal.org/article/S0016-5085(99)70493-2/fulltext[↩]
- Eckardt, VF. Clinical presentations and complications of achalasia. (vi.)Gastrointest Endosc Clin N Am. 2001; 11: 281–292 https://www.ncbi.nlm.nih.gov/pubmed/11319062[↩]
- Vantrappen, G, Hellemans, J, Deloof, W et al. Treatment of achalasia with pneumatic dilatations. Gut. 1971; 12: 268–275 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1411631/pdf/gut00653-0044.pdf[↩]
- Duranceau, A, Liberman, M, Martin, J et al. End-stage achalasia. Dis Esophagus. 2012; 25: 319–330 https://www.ncbi.nlm.nih.gov/pubmed/21166740[↩]
- Triadafilopoulos, G, Boeckxstaens, GE, Gullo, R et al. The Kagoshima consensus on esophageal achalasia. Dis Esophagus. 2012; 25: 337–348 https://www.ncbi.nlm.nih.gov/pubmed/21595779[↩]
- Eldaif, SM, Mutrie, CJ, Rutledge, WC et al. The risk of esophageal resection after esophagomyotomy for achalasia. (discussion 62–63.)Ann Thorac Surg. 2009; 87: 1558–1562 http://www.annalsthoracicsurgery.org/article/S0003-4975(09)00359-2/fulltext[↩][↩]
- Bower MR, Martin RC., 2nd Nutritional management during neoadjuvant therapy for esophageal cancer. J Surg Oncol. 2009;100:82–87. https://www.ncbi.nlm.nih.gov/pubmed/19373870[↩]
- Given MF, Hanson JJ, Lee MJ. Interventional radiology techniques for provision of enteral feeding. Cardiovasc Intervent Radiol. 2005;28:692–703. https://www.ncbi.nlm.nih.gov/pubmed/16184329[↩]
- Zhao JG, Li YD, Cheng YS, et al. Long-term safety and outcome of a temporary self-expanding metallic stent for achalasia: A prospective study with a 13-year single-center experience. Eur Radiol. 2009;19:1973–1980. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2705705/[↩]