Contents
Primary aldosteronism
Primary hyperaldosteronism is a disorder caused by excess production of the hormone aldosterone by the adrenal glands 1. Aldosterone is a hormone which helps balance the levels of sodium (salt) and potassium in your body. Having too much aldosterone causes the body to hold on to sodium, resulting in salt and water build-up and a rise in blood pressure. The main symptom of primary hyperaldosteronism is high blood pressure (hypertension), but other symptoms may include headaches, weakness, swelling (edema), and muscle spasms (tetany). Uncontrolled high blood pressure can put you at risk for stroke, heart attack, heart failure, or kidney failure. The risk of heart disease and stroke may be even greater in people with primary hyperaldosteronism than in other people with high blood pressure.
When the increase of aldosterone is caused by a problem in your adrenals, the condition is called primary aldosteronism. When the problem originates outside the adrenals, it’s called secondary aldosteronism. The main causes of primary hyperaldosteronism are:
- Overactivity of both adrenal glands, which occurs in about two-thirds of cases
- A noncancerous growth or tumor in one adrenal gland (also called Conn’s syndrome), which occurs in about one-third of cases
- An inherited disorder which affects aldosterone production, which is rare
- A cancerous tumor of the adrenal gland, which is extremely rare
The cause of primary hyperaldosteronism can vary. One cause may be an adenoma, or benign tumor, on the adrenal glands, which causes them to produce too much aldosterone. If primary hyperaldosteronism is caused by an adenoma, it is known as Conn’s syndrome. The condition may also be caused by enlarged adrenal glands without adenomas (adrenal hyperplasia).
In some cases, primary hyperaldosteronism is inherited in an autosomal dominant manner, but in most cases the exact cause of the disease is unknown (idiopathic). A diagnosis is made by testing the blood for high levels of aldosterone. Treatment for Conn’s syndrome includes surgical removal of the adenomas. Medication is used to treat primary hyperaldosteronism if it is caused by adrenal hyperplasia. Other options for people with primary aldosteronism include lifestyle modifications and surgery.
Have your blood pressure checked regularly, especially if you have risk factors for high blood pressure. Ask your doctor about the possibility of having primary aldosteronism if:
- You’re age 45 or older
- You have a family history of high blood pressure
- You have high blood pressure that began at age 44 or younger
- You’re overweight
- You have a sedentary lifestyle
- You use tobacco
- You drink a lot of alcohol
- You have dietary imbalances (too much salt, not enough potassium)
Primary aldosteronism complications
Primary aldosteronism can lead to high blood pressure and low potassium levels. These complications in turn can lead to other problems.
Problems related to high blood pressure
Persistently elevated blood pressure can lead to problems with your heart and kidneys, including:
- Heart attack
- Heart failure
- Left ventricular hypertrophy — enlargement of the muscle that makes up the wall of the left ventricle, one of your heart’s pumping chambers
- Stroke
- Kidney disease or kidney failure
- Premature death
High blood pressure caused by primary aldosteronism carries a higher risk of cardiovascular complications than do other types of high blood pressure. This excess risk is due to the high aldosterone levels, which can cause heart and blood vessel damage independent of complications related to high blood pressure.
Problems related to low potassium levels
Some, but not all, people with primary aldosteronism have low potassium levels (hypokalemia). Mild hypokalemia may not cause any symptoms, but very low levels of potassium can lead to:
- Weakness
- Cardiac arrhythmias
- Muscle cramps
- Excess thirst or urination
Adrenal glands
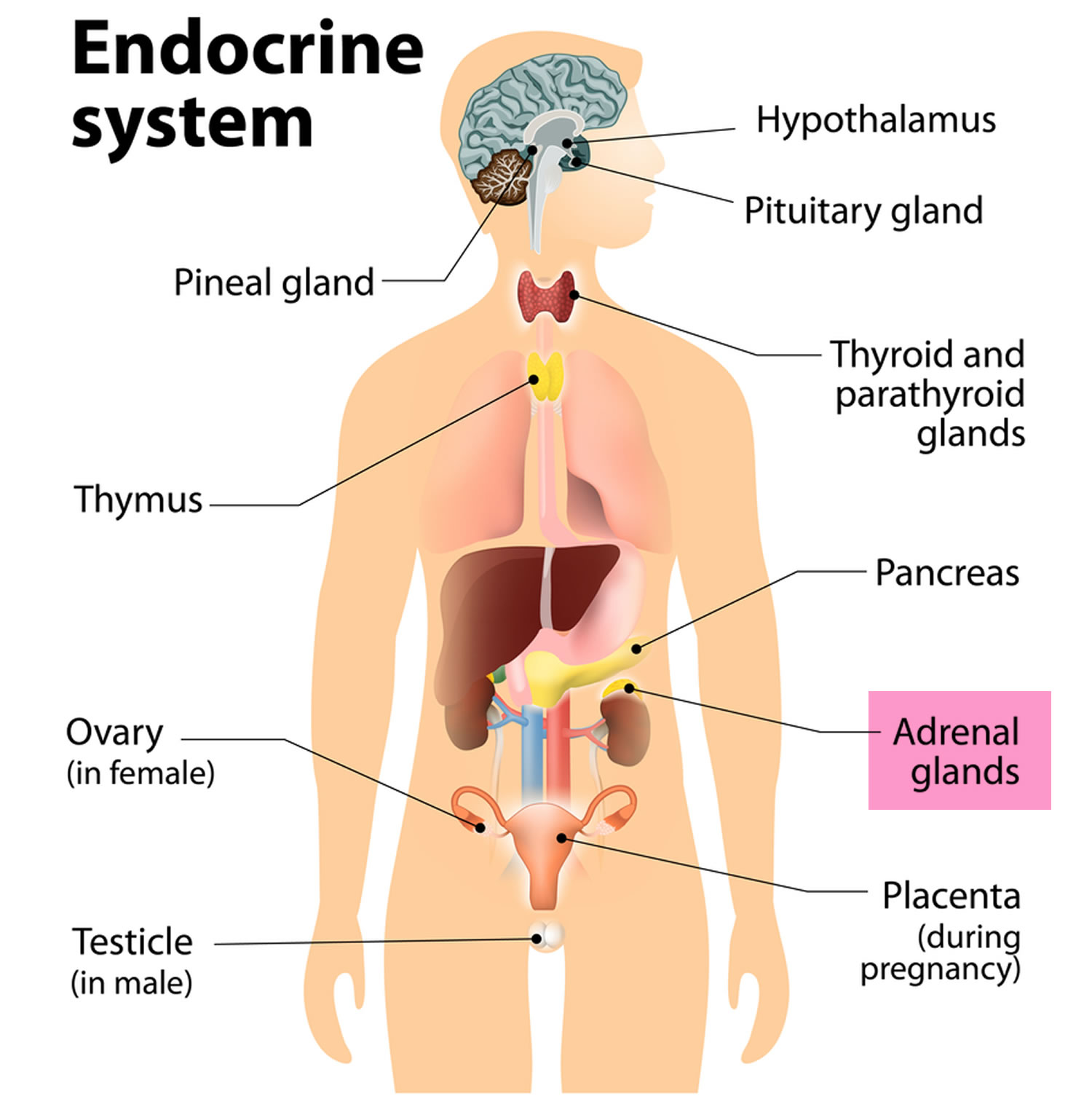
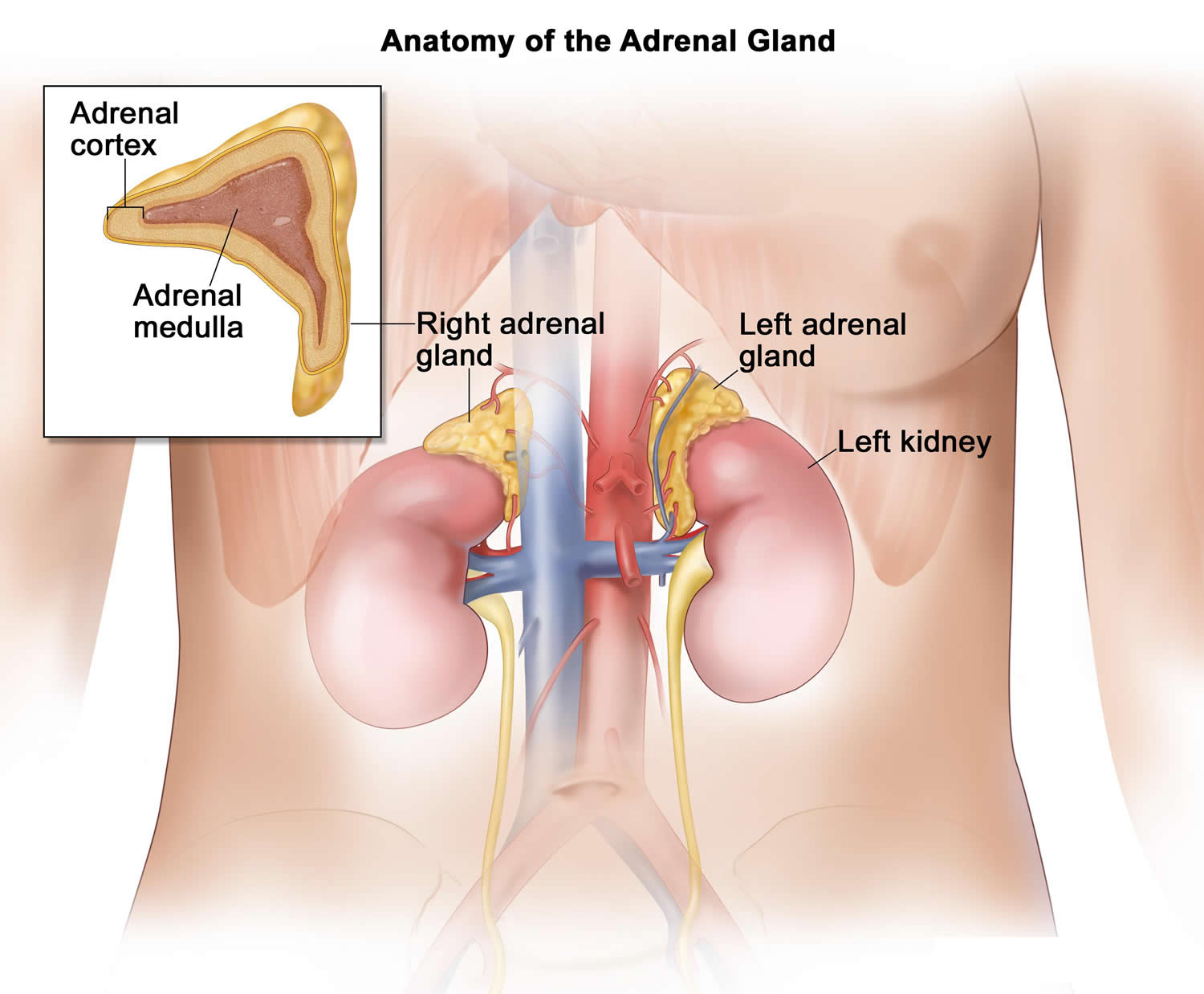
The adrenal glands are two, triangle-shaped endocrine glands that measure about 1.5 inches in height and 3 inches in length. One sits on top of each kidney (see Figures 1 and 2). They form part of the body’s hormonal system. They produce several hormones that are involved in controlling your blood pressure, metabolism and your body’s response to stress.
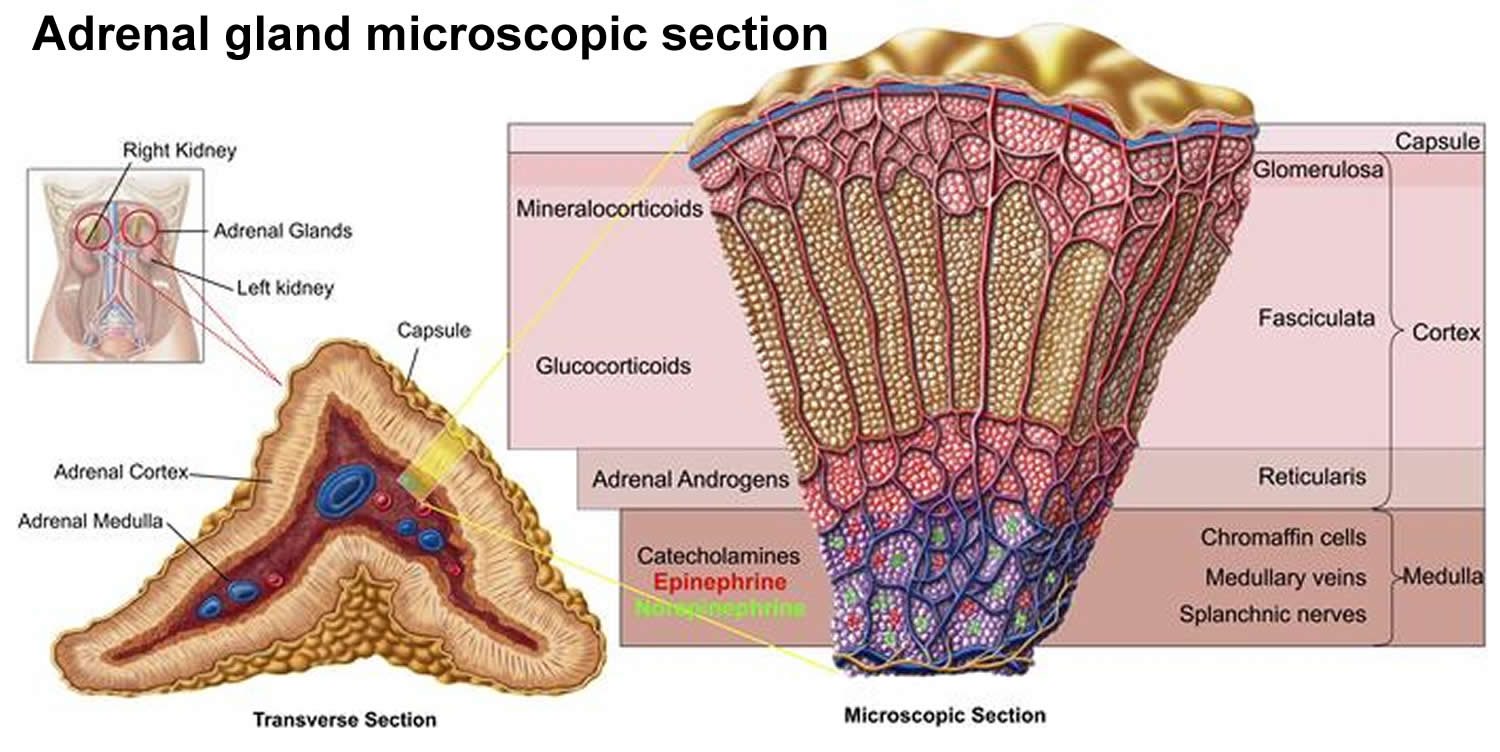
The outer part of the adrenal gland, called the adrenal cortex, produces the hormones cortisol, aldosterone, and hormones that can be changed into testosterone 2. The inner part of the gland, called the adrenal medulla, produces the hormones adrenaline and noradrenaline. These hormones are also called epinephrine and norepinephrine 2.
These hormones—cortisol, aldosterone, adrenaline, and noradrenaline—control many important functions in the body, including:
- Maintaining metabolic processes, such as managing blood sugar levels and regulating inflammation.
- Regulating the balance of salt and water.
- Controlling the “fight or flight” response to stress.
- Maintaining pregnancy.
- Initiating and controlling sexual maturation during childhood and puberty.
The adrenal glands are also an important source of sex steroids, such as estrogen and testosterone.
When the adrenal glands produce more or less hormones than normal, you can become sick. This might happen at birth or later in life 3.
The adrenal glands can be affected by many diseases, such as autoimmune disorders, infections, tumors, and bleeding 3.
Conditions related to adrenal gland problems include:
- Addison disease (also called adrenal insufficiency)
- Congenital adrenal hyperplasia
- Cushing syndrome
- Diabetes – caused by another medical problem
- Glucocorticoid medicines
- Excessive or unwanted hair in women (hirsutism)
- Hump behind shoulders (dorsocervical fat pad)
- Hypoglycemia
- Primary aldosteronism (Conn syndrome)
- Waterhouse-Friderichsen syndrome
Figure 1. Location of the adrenal glands on top of each kidneys
Figure 2. Adrenal gland anatomy
Structure of the adrenal glands
Each adrenal gland is about the size of the top part of the thumb. Each adrenal gland is very vascular and consists of two parts:
- The outer part is the adrenal cortex.
- The central portion is the adrenal medulla.
These regions are not sharply divided, but they are functionally distinct structures that secrete different hormones.
The adrenal cortex and the adrenal medulla have very different functions. One of the main distinctions between them is that the hormones released by the adrenal cortex are necessary for life; those secreted by the adrenal medulla are not.
The adrenal medulla consists of irregularly shaped cells organized in groups around blood vessels. These cells are intimately connected with the sympathetic division of the autonomic nervous system. Adrenal medullary cells are actually modified postganglionic neurons. Preganglionic autonomic nerve fibers control their secretions. The adrenal medulla produces adrenaline (epinephrine) and noradrenaline (norepinephrine). These hormones are also called adrenaline and noradrenaline.
The adrenal cortex, which makes up the bulk of the adrenal gland, is composed of closely packed masses of epithelial cells, organized in layers. These layers form the outer (glomerulosa), middle (fasciculata), and inner (reticularis) zones of the cortex (Figure 3). As in the adrenal medulla, the cells of the adrenal cortex are well supplied with blood vessels. The adrenal cortex produces steroid hormones such as cortisol, aldosterone, and hormones that can be changed into testosterone.
Figure 3. Adrenal gland microscopic section
What hormones do the adrenal glands make?
The adrenal glands mainly make adrenaline, noradrenaline, cortisol and aldosterone.
Adrenaline and noradrenaline are involved in your body’s stress (or ‘fight or flight’) response. They make your heart beat faster, send more blood to your muscles and more.
Cortisol does many things, including influencing your metabolism (how your body uses energy), changing blood sugar levels and slowing down the immune system.
Aldosterone plays a part in controlling your blood pressure.
The adrenal glands also make weak sex hormones that travel to the testes or ovaries where they are converted into testosterone or oestrogen.
Medical conditions related to the adrenal glands
Adrenal gland disorders are rare.
Cushing’s syndrome is a condition where you have too much cortisol. This causes a variety of problems, such as weight gain, a flushed face, bruising and diabetes. Cushing’s syndrome is usually caused by taking steroid medication for a long time, but it can sometimes be caused by a tumor of the adrenal gland.
Addison’s disease is caused by the adrenal glands failing to make enough of the hormones cortisol and aldosterone. If you have Addison’s disease, you’ll have a poor appetite and lose weight, and you might also have abdominal pain, nausea, vomiting and dizziness.
Congenital adrenal hyperplasia is a condition in which the adrenal glands produce excess male sex hormones. Symptoms can include early puberty in boys and male features in girls.
Conn’s syndrome occurs where there is a tumor that makes excess aldosterone, leading to high blood pressure.
Causes of aldosteronism
Common conditions causing the overproduction of aldosterone include:
- A benign growth in an adrenal gland (aldosterone-producing adenoma) — a condition also known as Conn’s syndrome
- Overactivity of both adrenal glands (idiopathic hyperaldosteronism)
In rare cases, primary aldosteronism may be caused by:
- A cancerous (malignant) growth of the outer layer (cortex) of the adrenal gland (adrenal cortical carcinoma)
- A rare type of primary aldosteronism called glucocorticoid-remediable aldosteronism that runs in families and causes high blood pressure in children and young adults
What are the risk factors for primary aldosteronism?
- High blood pressure that requires more than three medications to manage
- High blood pressure that started at a young age (less than age 30)
- Family history of stroke at a young age
- Low potassium level in your blood (called hypokalemia)
Aldosteronism symptoms
The main signs of primary aldosteronism are:
- Moderate to severe high blood pressure
- High blood pressure that takes several medications to control (resistant hypertension)
- High blood pressure along with a low potassium level (hypokalemia)
High aldosterone levels can lead to low potassium levels. Low potassium levels often cause no symptoms but may lead to weakness, tingling, muscle spasms, and periods of temporary paralysis. Some people become extremely thirsty and urinate frequently.
Primary aldosteronism diagnosis
A variety of tests are available to help diagnose primary aldosteronism.
Screening test
Doctors who suspect hyperaldosteronism first test the levels of sodium and potassium in the blood. Doctors then also measure renin and aldosterone levels in your blood. Renin is an enzyme released by your kidneys that helps regulate blood pressure. The combination of a very low renin level with a high aldosterone level suggests that primary aldosteronism may be the cause of your high blood pressure.
- Measurement of sodium, potassium, and hormone levels in the blood
- Imaging tests of the adrenal glands
If the aldosterone level is high, spironolactone or eplerenone, drugs that block the action of aldosterone, may be given to see if the levels of sodium and potassium return to normal. Doctors also measure the levels of renin. In Conn syndrome, the levels of renin are also very low.
Confirmation tests
If the aldosterone-renin test suggests that you might have primary aldosteronism, you’ll need another test to confirm the diagnosis, such as one of the following:
- Oral salt loading. You’ll follow a high-sodium diet for three days before your doctor measures aldosterone and sodium levels in your urine.
- Saline infusion test. Your aldosterone levels are tested after sodium mixed with water (saline) is infused into your bloodstream for several hours.
- Fludrocortisone suppression test. After you’ve followed a high-sodium diet and taken fludrocortisone — which mimics the action of aldosterone — for several days, aldosterone levels in your blood are measured.
Additional tests
When too much aldosterone is being produced, doctors examine the adrenal glands for a noncancerous tumor (adenoma). Computed tomography (CT) or magnetic resonance imaging (MRI) can be helpful, but sometimes blood samples from each of the adrenal glands must be tested to determine whether the underlying cause is an aldosterone-producing adenoma or overactivity of both adrenal glands. Tests may include:
- Abdominal computerized tomography (CT) scan. A CT scan can help identify a tumor on your adrenal gland or an enlargement that suggests overactivity. You may still need additional testing after a CT scan because this imaging test may miss small but important abnormalities or find tumors that don’t produce aldosterone.
- Adrenal vein sampling. A radiologist draws blood from both your right and left adrenal veins and compares the two samples. Aldosterone levels that are significantly higher on one side indicate the presence of an aldosteronoma on that side. Similar aldosterone levels on both sides point to overactivity in both glands.
This test involves placing a tube in a vein in your groin and threading it up to the adrenal veins. Though essential for determining the appropriate treatment, this test carries the risk of bleeding or a blood clot in the vein.
Primary aldosteronism treatment
Treatment for primary aldosteronism depends on the underlying cause and can include medication, lifestyle changes or surgery, but its basic goal is to normalize or block the effect of high aldosterone levels and prevent the potential complications of high blood pressure and low potassium levels.
If you desire surgery, many times your doctor will order a test called adrenal vein sampling, taking blood samples from each adrenal vein to measure aldosterone and cortisol. This test will demonstrate which adrenal glands produces aldosterone in excess. When both adrenals are overactive, treatment includes medication and lifestyle changes. Your doctor may prescribe a special type of diuretic (“water pill”) that works to block the action of aldosterone in your body. You will also need to limit sodium (salt) in your diet.
Treatment for an adrenal gland tumor
An adrenal gland tumor may be treated with surgery or medications and lifestyle changes.
- Surgical removal of the gland. Surgical removal of the adrenal gland containing the tumor (adrenalectomy) is usually recommended because it may permanently resolve high blood pressure and potassium deficiency, and it can bring aldosterone levels back to normal. Blood pressure usually drops gradually after a unilateral adrenalectomy. Your doctor will follow you closely after surgery and progressively adjust or eliminate your high blood pressure medications. An adrenalectomy carries the usual risks of abdominal surgery, including bleeding and infection. However, adrenal hormone replacement is not necessary after a unilateral adrenalectomy because the other adrenal gland is able to produce adequate amounts of all the hormones on its own.
- Aldosterone-blocking drugs. If you’re unable to have surgery or prefer not to, primary aldosteronism caused by a benign tumor can also be treated with aldosterone-blocking drugs (mineralocorticoid receptor antagonists) and lifestyle changes. But high blood pressure and low potassium will return if you stop taking your medications.
Treatment for overactivity of both adrenal glands
When only one adrenal gland is overactive, medication and lifestyle modifications can effectively treat primary aldosteronism caused by overactivity of both adrenal glands (bilateral adrenal hyperplasia). However, doctors usually recommend surgery to remove the culprit adrenal gland. After surgery, you may still need to take medication. You should also follow a healthy lifestyle by:
Lifestyle changes
- Reducing sodium in your diet
- Losing weight, if needed
- Exercising regularly
- Limiting alcohol intake
- Stopping smoking
- Medications. Mineralocorticoid receptor antagonists block the action of aldosterone in your body. Your doctor may first prescribe spironolactone. This medication helps correct high blood pressure and low potassium, but it may cause problems. In addition to blocking aldosterone receptors, spironolactone blocks androgen and progesterone receptors and may inhibit the action of these hormones. Side effects can include male breast enlargement (gynecomastia), decreased sexual desire, impotence, menstrual irregularities and gastrointestinal distress. A newer, more expensive mineralocorticoid receptor antagonist called eplerenone acts just on aldosterone receptors, but eliminates the sex hormone side effects associated with spironolactone. Your doctor may recommend eplerenone if you have serious side effects with spironolactone. You may also need other medications for high blood pressure.
- High blood pressure medications are more effective when combined with a healthy diet and lifestyle. Work with your doctor to create a plan to reduce the sodium in your diet and maintain a healthy body weight. Getting regular exercise, limiting the amount of alcohol you drink and stopping smoking also may improve your response to medications.
Lifestyle and home remedies
A healthy lifestyle is essential for keeping blood pressure low and maintaining long-term heart health. Here are some healthy lifestyle suggestions:
- Follow a healthy diet. Limit the sodium in your diet by focusing on fresh foods and reduced-sodium products, avoiding condiments, and removing salt from recipes. (3p6) Diets that also emphasize a healthy variety of foods — including grains, fruits, vegetables and low-fat dairy products — can promote weight loss and help lower blood pressure. Try the Dietary Approaches to Stop Hypertension (DASH) diet — it has proven benefits for your heart.
- Achieve a healthy weight. If your body mass index (BMI) is 25 or more, losing as few as 10 pounds (4.5 kilograms) may reduce your blood pressure.
- Exercise. Regular aerobic exercise can help lower blood pressure. You don’t have to hit the gym — taking vigorous walks most days of the week can significantly improve your health. Try walking with a friend at lunch instead of dining out.
- Don’t smoke. Quitting smoking will improve your overall cardiovascular health. Nicotine in tobacco makes your heart work harder by constricting your blood vessels and increasing your heart rate and blood pressure. Talk to your doctor about medications that can help you stop smoking.
- Limit alcohol and caffeine. Both substances can raise your blood pressure, and alcohol can interfere with the effectiveness of some blood pressure medications. Ask your doctor whether moderate alcohol consumption is safe for you.
- Ashley B. Grossman, MD, FRCP. Hyperaldosteronism. Merck Manual. http://www.merckmanuals.com/home/hormonal-and-metabolic-disorders/adrenal-gland-disorders/hyperaldosteronism[↩]
- US Department of Health and Human Services. National Institutes of Health. About Adrenal Gland Disorders. https://www.nichd.nih.gov/health/topics/adrenalgland/conditioninfo/Pages/default.aspx[↩][↩]
- U.S. National Library of Medicine. Medline Plus. Adrenal glands. https://medlineplus.gov/ency/article/002219.htm[↩][↩]