Contents
What is ALS disease
ALS disease is short for Amyotrophic Lateral Sclerosis, which is a progressive motor neuron that attacks nerve cells called neurons in your brain and spinal cord that are responsible for controlling voluntary muscle movement, such as those in our arms, legs, and face 1. ALS is also called Lou Gehrig’s disease. As these motor neurons degenerate or die, they stop sending signals to muscles. Unable to function, the muscles gradually weaken and waste away.
Normally, messages from motor neurons in the brain (called upper motor neurons) are transmitted to motor neurons in the spinal cord and to motor nuclei of brain (called lower motor neurons) and from the spinal cord and motor nuclei of brain to a particular muscle or muscles (See Nervous System below for better explanation).
In ALS, both the upper motor neurons and the lower motor neurons degenerate or die, and stop sending messages to the muscles. Unable to function, the muscles gradually weaken, start to twitch (called fasciculations), and waste away (atrophy). Eventually, the brain loses its ability to initiate and control voluntary movements.
Unfortunately, people with ALS usually have a shortened lifespan and may die within a few years of diagnosis. ALS is age related; most people find out they have it when they are between 55 and 75 years of age, and live from 2 to 5 years after symptoms develop. How long a person lives with ALS seems to be related to age; people who are younger when the illness starts live slightly longer. ALS affects people of all races and ethnicities, however ALS is most common in whites, males, and people over the age of 60. Over 17,000 people are estimated to be living with ALS in the United States 2. ALS most commonly strikes between the ages of 40 and 60, but younger and older people also can develop the disorder 3. Men are more likely than women to be affected.
At first only a single limb may be affected, such as some weakness in a hand or a leg, or a person may have problems speaking or swallowing. Other symptoms may include stiff muscles, cramps, or stumbling. It may become hard to turn a key, lift a coffee pot, or button a shirt.
Eventually, all muscles under voluntary control are affected, and people lose the ability to move different parts of their body.
When breathing-related muscles fail, ventilation support can help people breathe. Most people with ALS die from respiratory failure, usually within 3 to 5 years after symptoms first appeared. However, about 10% of people with ALS survive for 10 or more years 3.
In most ALS cases, the underlying causes are unknown and there is no cure for ALS. Currently, there is no cure for ALS and no effective treatment to halt, or reverse, the progression of the disease, but medicines can relieve symptoms and sometimes, prolong survival.
There is no definite method to prevent ALS.
In 2016 the Centers for Disease Control and Prevention estimated that between 14,000 – 15,000 Americans have ALS. ALS is a common neuromuscular disease worldwide. It affects people of all races and ethnic backgrounds.
There are several potential risk factors for ALS including:
- Age. Although the disease can strike at any age, symptoms most commonly develop between the ages of 55 and 75.
- Gender. Men are slightly more likely than women to develop ALS. However, as we age the difference between men and women disappears.
- Race and ethnicity. Most likely to develop the disease are Caucasians and non-Hispanics.
Some studies suggest that military veterans are about 1.5 to 2 times more likely to develop ALS. Although the reason for this is unclear, possible risk factors for veterans include exposure to lead, pesticides, and other environmental toxins. ALS is recognized as a service-connected disease by the U.S. Department of Veterans Affairs.
Multidisciplinary ALS clinics provide specialty care to people living with the disease. Attending multidisciplinary ALS clinics may improve the quality and length of life of people living with ALS. You can learn more about ALS providers here: https://wwwn.cdc.gov/ALS/ALSRegistryResources.aspx 4
ALS Resource Links
- ALS Association
- MDA ALS Division
- Northeast Amyotrophic Lateral Sclerosis Consortium (NEALS)
- Mayo Clinic ALS Information
- National Institutes of Health (NIH) ALS Clinical Trials
- National Library of Medicine ALS Information
- National Institutes of Health ALS Information
- Emory ALS Center
- ALS Therapy Development Institute
- Les Turner ALS Foundation
- ALS Biorepository Brain Bank
- CReATe
- CReATe
- ALS Family Charitable Foundation
ALS life expectancy
Most people with ALS die from respiratory failure, usually within 3 to 5 years from when the symptoms first appear. However, about 10 percent of people with ALS survive for 10 or more years 5.
The nervous system
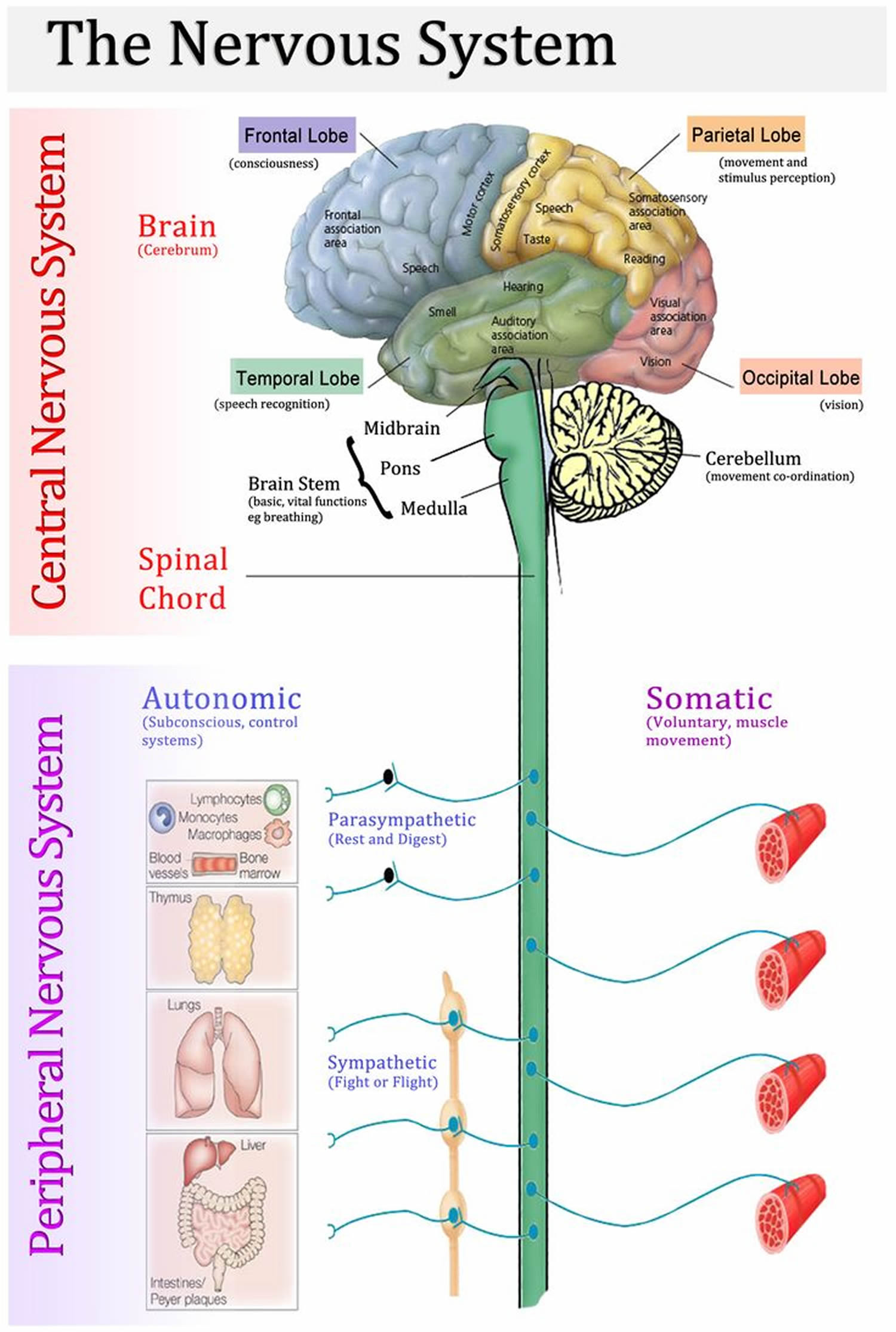
The nervous system has two major anatomical subdivisions:
- The central nervous system (CNS) consists of the brain and spinal cord, which are enclosed and protected by the cranium and vertebral column. The central nervous system is discussed further in the other posts: Human brain and Spinal cord.
- The peripheral nervous system (PNS) consists of all the rest; it is composed of nerves and ganglia. A nerve is a bundle of nerve fibers (axons) wrapped in fibrous connective tissue. Nerves emerge from the central nervous system (CNS) through foramina of the skull and vertebral column and carry signals to and from other organs of the body. A ganglion (plural, ganglia) is a knotlike swelling in a nerve where the cell bodies of peripheral neurons are concentrated.
Figure 1. Nervous system and its parts
Nervous system function
The communicative role of the nervous system is carried out by nerve cells, or neurons. These cells have three fundamental physiological properties that enable them to communicate with other cells:
- Excitability. All cells are excitable—that is, they respond to environmental changes (stimuli). Neurons exhibit this property to the highest degree.
- Conductivity. Neurons respond to stimuli by producing electrical signals that are quickly conducted to other cells at distant locations.
- Secretion. When the signal reaches the end of a nerve fiber, the neuron secretes a neurotransmitter that crosses the gap and stimulates the next cell.
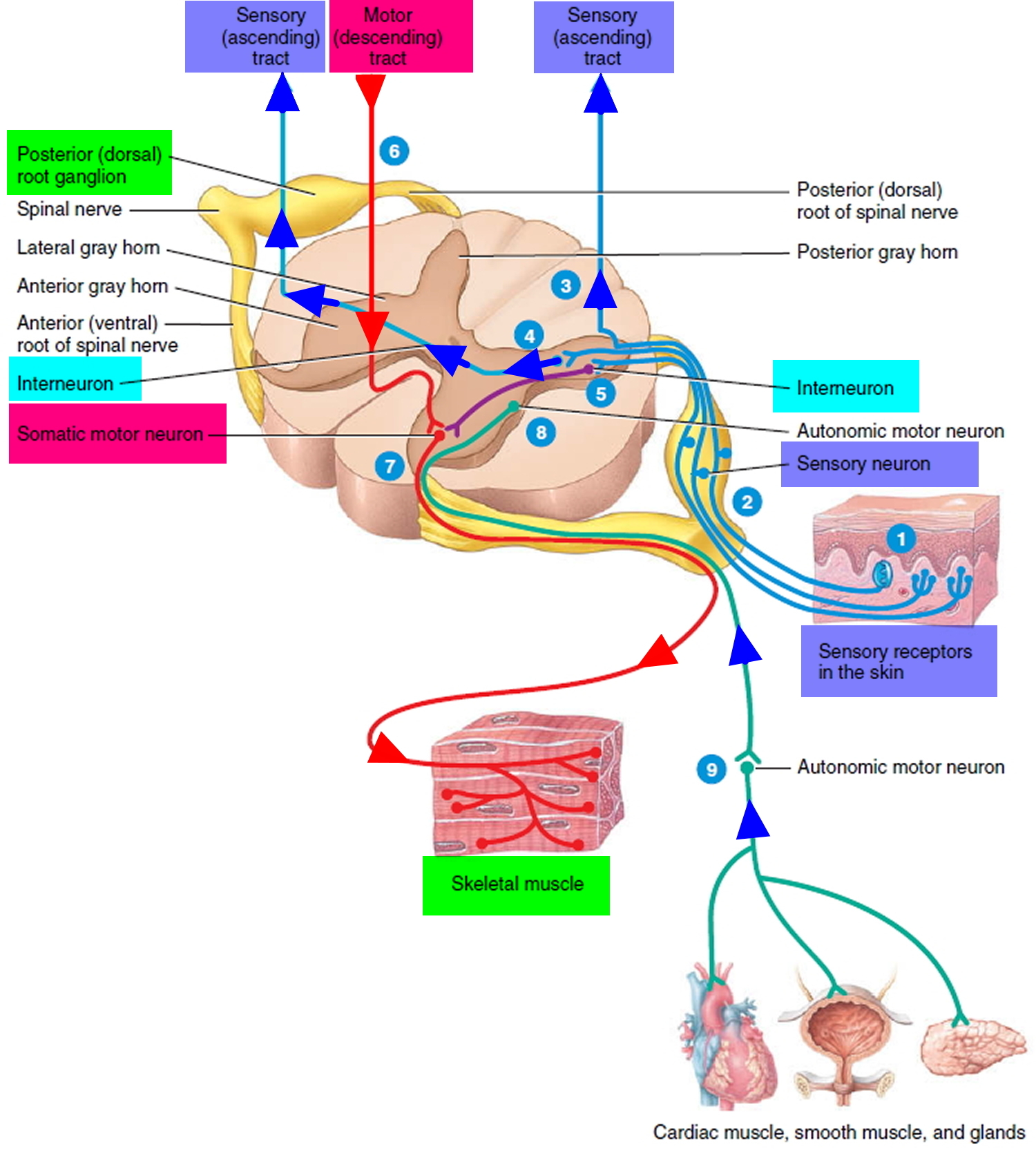
Functional Classes of Neurons
There are three general classes of neurons corresponding to the three major aspects of nervous system function listed above (e.g. excitability, conductivity and secretion):
- Sensory (afferent) neurons are specialized to detect stimuli such as light, heat, pressure, and chemicals, and transmit information about them to the central nervous system (CNS). Such neurons begin in almost every organ of the body and end in the central nervous system (CNS); the word afferent refers to signal conduction toward the central nervous system (CNS). Some receptors, such as those for pain and smell, are themselves neurons. In other cases, such as taste and hearing, the receptor is a separate cell that communicates directly with a sensory neuron.
- Interneurons lie entirely within the central nervous system (CNS). They receive signals from many other neurons and carry out the integrative function of the nervous system—that is, they process, store, and retrieve information and “make decisions” that determine how the body responds to stimuli. About 90% of our neurons are interneurons. The word interneuron refers to the fact that they lie between, and interconnect, the incoming sensory pathways and the outgoing motor pathways of the central nervous system (CNS).
- Motor (efferent) neurons send signals predominantly to muscle and gland cells, the effectors. They are called motor neurons because most of them lead to muscle cells, and efferent neurons to signify signal conduction away from the central nervous system (CNS).
Figure 2. Functional classes of neurons
What causes ALS disease
No one knows what causes most cases of ALS, but ALS is inherited in 5 to 10 percent of cases, while the rest have no known cause.
Sporadic ALS
The majority of ALS cases (90 percent or more) are considered sporadic. This means the disease seems to occur at random with no clearly associated risk factors and no family history of the disease. Although family members of people with sporadic ALS are at an increased risk for the disease, the overall risk is very low and most will not develop ALS.
Familial (Genetic) ALS
About 5 to 10 percent of all ALS cases are familial, which means that an individual inherits the disease from his or her parents. The familial form of ALS usually only requires one parent to carry the gene responsible for the disease. Mutations in more than a dozen genes have been found to cause familial ALS. About 25 to 40 percent of all familial cases (and a small percentage of sporadic cases) are caused by a defect in a gene known as “chromosome 9 open reading frame 72,” or C9ORF72. Interestingly, the same mutation can be associated with atrophy of frontal-temporal lobes of the brain causing frontal-temporal lobe dementia. Some individuals carrying this mutation may show signs of both motor neuron and dementia symptoms (ALS-FTD). Another 12 to 20 percent of familial cases result from mutations in the gene that provides instructions for the production of the enzyme copper-zinc superoxide dismutase 1 (SOD1).
Most familial cases are inherited in an autosomal dominant manner. This means that only one altered (mutated) copy of the disease-causing gene in each cell is sufficient to cause the condition. In most of these cases, an affected individual has one parent with the condition. When an individual with an autosomal dominant form of ALS has children, each child has a 50% (1 in 2) risk to inherited the mutated copy of the gene and be affected.
Less frequently, ALS is inherited in an autosomal recessive manner. In autosomal recessive inheritance, both copies of the disease-causing gene (typically one copy inherited from each parent) must have a mutation for the individual to be affected. The parents of an individual with an autosomal recessive condition, who presumably each carry one mutated copy of the gene, are referred to as carriers. Carriers typically do not have any signs or symptoms of the condition. When two carriers for the same condition are having children, each child has a 25% (1 in 4) risk to have the condition, a 50% (1 in 2) risk to be a carrier like each parent, and a 25% risk to not have the condition and not be a carrier. Autosomal recessive forms of ALS may be mistaken for non-inherited (sporadic) forms due to having a negative family history of the condition.
In rare cases, ALS is inherited in an X-linked dominant manner. This occurs when the disease-causing gene is located on the X chromosome (a sex chromosome). Although females have 2 X chromosomes, having a mutation in one X chromosome is still sufficient to cause the condition. Males who have a mutation (and only one X chromosome) will have the condition. Usually, males with an X-linked dominant form of ALS experience more severe symptoms than females with the same form.
Some individuals who do inherit a mutation known to cause ALS never develop signs and symptoms of ALS, although the reason for this is unclear. This phenomenon is referred to as reduced penetrance 6.
Scientists have been studying many factors that could be linked with ALS such as heredity and environmental exposures. Other scientists have looked at diet or injury. Although no cause has been found for most cases of ALS, a number of inherited factors have been found to cause familial ALS. In the future, scientists may find that many factors together cause ALS.
Researchers are studying several possible causes of ALS, including:
- Gene mutation. Various genetic mutations can lead to inherited ALS, which causes nearly the same symptoms as the noninherited form.
- Chemical imbalance. People with ALS generally have higher than normal levels of glutamate, a chemical messenger in the brain, around the nerve cells in their spinal fluid. Too much glutamate is known to be toxic to some nerve cells.
- Disorganized immune response. Sometimes a person’s immune system begins attacking some of his or her body’s own normal cells, which may lead to the death of nerve cells.
- Protein mishandling. Mishandled proteins within the nerve cells may lead to a gradual accumulation of abnormal forms of these proteins in the cells, destroying the nerve cells.
Clinical genetic testing is currently available for several genes in which mutations are known to cause ALS. Genetic testing on a research basis is also available for select susceptibility genes associated with ALS 7.
You can find laboratories offering clinical and research genetic testing for ALS through the Genetic Testing Registry (GTR). The intended audience for the GTR is health care providers and researchers. Patients and consumers with specific questions about a genetic test should contact a health care provider or a genetics professional.
Risk factors for ALS
Established risk factors for ALS include:
- Heredity. Five to 10 percent of the people with ALS inherited it (familial ALS). In most people with familial ALS, their children have a 50-50 chance of developing the disease.
- Age. ALS risk increases with age, and is most common between the ages of 40 and 60.
- Sex. Before the age of 65, slightly more men than women develop ALS. This sex difference disappears after age 70.
- Genetics. Some studies examining the entire human genome (genomewide association studies) found many similarities in the genetic variations of people with familial ALS and some people with noninherited ALS. These genetic variations might make people more susceptible to ALS.
Environmental factors may trigger ALS. Some that may affect ALS risk include:
- Smoking. Smoking is the only likely environmental risk factor for ALS. The risk seems to be greatest for women, particularly after menopause.
- Environmental toxin exposure. Some evidence suggests that exposure to lead or other substances in the workplace or at home may be linked to ALS. Much study has been done, but no single agent or chemical has been consistently associated with ALS.
- Military service. Recent studies indicate suggest that military veterans are about 1.5 to 2 times more likely to develop ALS. It’s unclear exactly what about military service may trigger the development of ALS. It may include exposure to certain metals or chemicals, traumatic injuries, viral infections, intense exertion, pesticides, and other environmental toxins. ALS is recognized as a service-connected disease by the U.S. Department of Veterans Affairs.
ALS disease early symptoms
Early symptoms of ALS usually include muscle weakness or stiffness. Gradually all muscles under voluntary control are affected, and individuals lose their strength and the ability to speak, eat, move, and even breathe.
For many individuals the first sign of ALS may appear in the hand or arm as they experience difficulty with simple tasks such as buttoning a shirt, writing, or turning a key in a lock. In other cases, symptoms initially affect one of the legs, and people experience awkwardness when walking or running or they notice that they are tripping or stumbling more often.
Early signs and symptoms of ALS include 8:
- Difficulty walking or doing your normal daily activities
- Tripping and falling
- Weakness affecting your leg, feet, ankles, neck or diaphragm
- Hand weakness or clumsiness
- Slurred speech and nasal speech
- Trouble swallowing and chewing
- Muscle cramps
- Muscle twitching (fasciculations) in your arms, shoulders and tongue
- Difficulty holding your head up or keeping good posture
- Tight and stiff muscles (spasticity)
ALS often starts in the hands, feet or limbs, and then spreads to other parts of your body. As the disease advances and nerve cells are destroyed, your muscles progressively weaken. This eventually affects chewing, swallowing, speaking and breathing.
Regardless of where the symptoms first appear, muscle weakness and atrophy spread to other parts of the body as the disease progresses. Individuals may develop problems with moving, swallowing (dysphagia), speaking or forming words (dysarthria), and breathing (dyspnea).
Although the sequence of emerging symptoms and the rate of disease progression vary from person to person, eventually individuals will not be able to stand or walk, get in or out of bed on their own, or use their hands and arms.
ALS doesn’t usually affect your bowel or bladder control, your senses or your thinking ability. It’s possible to remain actively involved with your family and friends.
Individuals with ALS usually have difficulty swallowing and chewing food, which makes it hard to eat normally and increases the risk of choking. They also burn calories at a faster rate than most people without ALS. Due to these factors, people with ALS tend to lose weight rapidly and can become malnourished.
Because people with ALS usually retain their ability to perform higher mental processes such as reasoning, remembering, understanding, and problem solving, they are aware of their progressive loss of function and may become anxious and depressed.
A small percentage of individuals may experience problems with language or decision-making, and there is growing evidence that some may even develop a form of dementia over time.
Individuals with ALS will have difficulty breathing as the muscles of the respiratory system weaken. They eventually lose the ability to breathe on their own and must depend on a ventilator. Affected individuals also face an increased risk of pneumonia during later stages of the disease. Besides muscle cramps that may cause discomfort, some individuals with ALS may develop painful neuropathy (nerve disease or damage).
Complications of ALS
As the disease progresses, people with ALS experience complications, which may include:
Breathing problems
Over time, ALS paralyzes the muscles you use to breathe. You may need a device to help you breathe at night, similar to what someone with sleep apnea might wear. For example, you may be given continuous positive airway pressure (CPAP) or bi-level positive airway pressure (BiPAP) to assist with your breathing at night.
Some people with advanced ALS choose to have a tracheostomy — a surgically created hole at the front of the neck leading to the windpipe (trachea) — for full-time use of a respirator that inflates and deflates their lungs.
The most common cause of death for people with ALS is respiratory failure. On average, death occurs within three to five years after symptoms begin.
Speaking problems
Most people with ALS will develop trouble speaking over time. This usually starts as occasional, mild slurring of words, but progresses to become more severe. Speech eventually becomes more difficult for others to understand, and people with ALS often rely on other communication technologies to communicate.
Eating problems
People with ALS can develop malnutrition and dehydration from damage to the muscles that control swallowing. They are also at higher risk of getting food, liquids or saliva into the lungs, which can cause pneumonia. A feeding tube can reduce these risks and ensure proper hydration and nutrition.
Dementia
Some people with ALS experience problems with memory and making decisions, and some are eventually diagnosed with a form of dementia called frontotemporal dementia.
ALS disease diagnosis
Amyotrophic lateral sclerosis (ALS) is difficult to diagnose early because it may mimic several other neurological diseases.
No one test can provide a definitive diagnosis of ALS. ALS is primarily diagnosed based on detailed history of the symptoms and signs observed by a physician during physical examination along with a series of tests to rule out other mimicking diseases. However, the presence of upper and lower motor neuron symptoms strongly suggests the presence of the disease.
Physicians will review an individual’s full medical history and conduct a neurologic examination at regular intervals to assess whether symptoms such as muscle weakness, atrophy of muscles, and spasticity are getting progressively worse.
ALS symptoms in the early stages of the disease can be similar to those of a wide variety of other, more treatable diseases or disorders. Appropriate tests can exclude the possibility of other conditions.
Tests to rule out other conditions may include:
- Electromyogram (EMG). During an EMG, your doctor inserts a needle electrode through your skin into various muscles. The test evaluates the electrical activity of your muscles when they contract and when they’re at rest. Abnormalities in muscles seen in an electromyogram can help doctors diagnose ALS, or determine if you have a different muscle or nerve condition that may be causing your symptoms. It can also help guide your exercise therapy.
- Nerve conduction study. This study measures your nerves’ ability to send impulses to muscles in different areas of your body. This test can determine if you have nerve damage or certain muscle diseases.
- Magnetic resonance imaging (MRI). Using radio waves and a powerful magnetic field, an MRI produces detailed images of your brain and spinal cord. An MRI can spot spinal cord tumors, herniated disks in your neck or other conditions that may be causing your symptoms.
- Blood and urine tests. Analyzing samples of your blood and urine in the laboratory may help your doctor eliminate other possible causes of your signs and symptoms.
- Spinal tap (lumbar puncture). Sometimes a specialist may remove a sample of your spinal fluid for analysis. A specialist inserts a small needle between two vertebrae in your lower back and removes a small amount of cerebrospinal fluid for testing in the laboratory.
- Muscle biopsy. If your doctor believes you may have a muscle disease rather than ALS, you may undergo a muscle biopsy. While you’re under local anesthesia, a small portion of your muscle is removed and sent to a lab for analysis.
Treatment for ALS
No cure has yet been found for ALS. Treatments can’t reverse the damage of amyotrophic lateral sclerosis, but they can slow the progression of symptoms, prevent complications and make you more comfortable and independent.
You may need an integrated team of doctors trained in many areas and other health care professionals to provide your care. This may prolong your survival and improve your quality of life.
Your team will help you select the right treatments for you. You always have the right to choose or refuse any of the treatments suggested.
Medications for ALS
Two medications are currently approved by the Food and Drug Administration for the treatment of ALS.
- Riluzole (Rilutek) — This drug appears to slow the disease’s progression in some people, perhaps by reducing levels of a chemical messenger in the brain (glutamate) that’s often present in higher levels in people with ALS. Clinical trials in people with ALS showed that riluzole prolongs survival by a few months, particularly in the bulbar form of the disease, but does not reverse the damage already done to motor neurons. Edaravone has been shown to slow the decline in clinical assessment of daily functioning in persons with ALS. Riluzole is taken as a pill and may cause side effects such as dizziness, gastrointestinal conditions and liver function changes.
- Edaravone (Radicava) — The FDA approved edaravone in 2017 based on six-month clinical trial that showed it reduced the decline in daily functioning associated with ALS. The drug is given via intravenous infusion (typically 10-14 days in a row, once a month), and side effects may include bruising, gait disturbance, hives, swelling and shortness of breath.Edaravone contains sodium bisulfite, which may cause serious allergic reactions in people with sulfite sensitivity.
Your doctor may also prescribe medications to provide relief from other symptoms, including:
- Muscle cramps and spasms
- Spasticity
- Constipation
- Fatigue
- Excessive salivation
- Excessive phlegm
- Pain
- Depression
- Sleep problems
- Uncontrolled outbursts of laughing or crying
Therapies for ALS
- Breathing care. As the muscles responsible for breathing start to weaken, people may experience shortness of breath during physical activity and difficulty breathing at night or when lying down. Doctors may test an individual’s breathing to determine when to recommend a treatment called noninvasive ventilation (NIV). Noninvasive ventilation (NIV) refers to breathing support that is usually delivered through a mask over the nose and/or mouth. Initially, NIV may only be necessary at night. When muscles are no longer able to maintain normal oxygen and carbon dioxide levels, NIV may be used full-time. NIV improves the quality of life and prolongs survival for many people with ALS.Because the muscles that control breathing become weak, individuals with ALS may also have trouble generating a strong cough. There are several techniques to help people increase forceful coughing, including mechanical cough assist devices and breath stacking. In breath stacking, a person takes a series of small breaths without exhaling until the lungs are full, briefly holds the breath, and then expels the air with a cough.
As the disease progresses and muscles weaken further, individuals may consider forms of mechanical ventilation (respirators) in which a machine inflates and deflates the lungs. Doctors may place a breathing tube through the mouth or may surgically create a hole at the front of the neck and insert a tube leading to the windpipe (tracheostomy). The tube is connected to a respirator.
Individuals with ALS and their families often consider several factors when deciding whether and when to use ventilation support. These devices differ in their effect on a person’s quality of life and in cost. Although ventilation support can ease problems with breathing and prolong survival, it does not affect the progression of ALS. People may choose to be fully informed about these considerations and the long-term effects of life without movement before they make decisions about ventilation support.
- Physical therapy. A physical therapist can address pain, walking, mobility, bracing and equipment needs that help you stay independent. Gentle, low-impact aerobic exercise such as walking, swimming, and stationary bicycling can strengthen unaffected muscles, improve cardiovascular health, and help people fight fatigue and depression. Range of motion and stretching exercises can help prevent painful spasticity and shortening (contracture) of muscles. Physical therapists can recommend exercises that provide these benefits without overworking muscles. Occupational therapists can suggest devices such as ramps, braces, walkers, and wheelchairs that help individuals conserve energy and remain mobile. A physical therapist can also help you adjust to a brace, walker or wheelchair and may suggest devices such as ramps that make it easier for you to get around. Regular exercise can also help improve your sense of well-being. Appropriate stretching can help prevent pain and help your muscles function at their best.
- Occupational therapy. An occupational therapist can help you find ways to remain independent despite hand and arm weakness. Adaptive equipment can help you perform daily activities such as dressing, grooming, eating and bathing. An occupational therapist can also help you modify your home to allow accessibility if you have trouble walking safely. Occupational therapists also have a good understanding of how assistive technology and computers can be used, even if your hands are weak.
- Speech therapy. Because ALS affects the muscles you use to speak, communication is an issue in advanced ALS. A speech therapist can teach you adaptive techniques to make your speech more clearly understood. Speech therapists can also help you explore other methods of communication, such as an alphabet board or simple pen and paper. Ask your therapist about the possibility of borrowing or renting devices such as tablet computers with text-to-speech applications or computer-based equipment with synthesized speech that use eye-tracking technology and can help people develop ways for responding to yes-or-no questions with their eyes or by other nonverbal means. Some people with ALS may choose to use voice banking while they are still able to speak as a process of storing their own voice for future use in computer-based speech synthesizers. These methods and devices help people communicate when they can no longer speak or produce vocal sounds.
- Nutritional support. Your team will work with you and your family members to ensure you’re eating foods that are easier to swallow and meet your nutritional needs. Nutritional support is an important part of the care of people with ALS. It has been shown that individuals with ALS will get weaker if they lose weight. Nutritionists can teach individuals and caregivers how to plan and prepare small meals throughout the day that provide enough calories, fiber, and fluid and how to avoid foods that are difficult to swallow. People may begin using suction devices to remove excess fluids or saliva and prevent choking. When individuals can no longer get enough nourishment from eating, doctors may advise inserting a feeding tube into the stomach. The use of a feeding tube also reduces the risk of choking and pneumonia that can result from inhaling liquids into the lungs.
- Psychological and social support. Your team may include a social worker to help with financial issues, insurance, and getting equipment and paying for devices you may need. Psychologists, social workers and others may provide emotional support for you and your family.
Potential future treatments
Clinical studies on promising medications and treatments are occurring in ALS all the time.
Whether you are eligible for a clinical study depends on many factors related to your ALS and also whether there are ongoing studies enrolling patients. While many of these studies are promising, they are still only studies, and it isn’t yet clear if these treatments will help people with ALS. Talk to your doctor about what might be available for you.
Cellular defects
Scientists are seeking to understand the mechanisms that selectively trigger motor neurons to degenerate in ALS, and to find effective approaches to halt the processes leading to cell death. Using both animal models and cell culture systems, scientists are trying to determine how and why ALS-causing gene mutations lead to the destruction of neurons. These animal models include fruit flies, zebrafish, and rodents.
Initially, genetically modified animal models focused on mutations in the SOD1 gene but more recently, models have been developed for defects in the C9ORF72, TARDP, FUS, PFN1, TUBA4A, and UBQLN2 genes. Research in these models suggests that, depending on the gene mutation, motor neuron death is caused by a variety of cellular defects, including in the processing of RNA molecules and recycling of proteins, and structural impairments of motor neurons. Increasing evidence also suggests that various types of glial support cells and inflammation cells of the nervous system may play an important role in the disease.
Stem Cells
In addition to animal models, scientists are also using innovative stem cells models to study ALS. Scientists have developed ways to take skin or blood cells from individuals with ALS and turn them into stem cells, which are capable of becoming any cell type in the body, including motor neurons and other cell types that may be involved in the disease. NINDS is supporting research on the development of stem cell lines for a number of neurodegenerative diseases, including ALS.
Familial versus sporadic ALS
Overall, the work in familial ALS is already leading to a greater understanding of the more common sporadic form of the disease. Because familial ALS and sporadic ALS show many of the same signs and symptoms, some researchers believe that some familial ALS genes may also be involved in sporadic ALS.
Clinical research studies are looking into how ALS symptoms change over time in people with C9ORF72 mutations. Other research studies are working to identify additional genes that may cause or put a person at risk for either familial or sporadic ALS.
Additionally, researchers are looking at the potential role of epigenetics in the development of ALS. Epigenetic changes can switch genes on and off, and thus can profoundly affect the human condition in both health and disease. These changes can occur in response to multiple factors, including external or environmental conditions and events. Although this research is still at a very exploratory stage, scientists hope that understanding epigenetics can offer new information about how ALS develops.
Biomarkers
Biomarkers are biological measures that help to identify the presence or rate of progression of a disease or the effectiveness of a therapeutic intervention. Since ALS is difficult to diagnose, biomarkers could potentially help clinicians diagnose ALS earlier and faster.
Additionally, biomarkers are needed to help predict and accurately measure disease progression and enhance clinical studies aimed at developing more effective treatments. Biomarkers can be molecules derived from a bodily fluid (such as those in the blood and cerebrospinal fluid), an image of the brain or spinal cord, or a measure of the ability of a nerve or muscle to process electrical signals.
New treatment options
Potential therapies for ALS are being investigated in a range of disease models. This work involves tests of drug-like compounds, gene therapy approaches, antibodies, and cell-based therapies. Scientists are currently investigating whether lowering levels of the SOD1 enzyme in the brain and spinal cord of individuals with SOD1 gene mutations would slow the rate of disease progression. Other scientists are studying the use of glial-restricted progenitor cells (which have the ability to develop into other support cells) to slow disease progression and improve respiratory function. Additionally, a number of exploratory treatments are being tested in people with ALS. Investigators are optimistic that these and other basic, translational, and clinical research studies will eventually lead to new and more effective treatments for ALS.
Coping and support for ALS
Learning you have ALS can be devastating. The following tips may help you and your family cope:
- Take time to grieve. The news that you have a fatal condition that will reduce your mobility and independence can be difficult. You and your family will likely experience a period of mourning and grief after diagnosis.
- Be hopeful. Your team will help you focus on your ability and healthy living. Some people with amyotrophic lateral sclerosis live much longer than the three to five years usually associated with this condition. Some live 10 years or more. Maintaining an optimistic outlook can help improve quality of life for people with ALS.
- Think beyond the physical changes. Many people with amyotrophic lateral sclerosis lead rich, rewarding lives despite physical limitations. Try to think of ALS as only one part of your life, not your entire identity.
- Join a support group. You may find comfort in a support group with others who have ALS. Your family members and friends helping with your care also may benefit from a support group of other ALS caregivers. Find support groups in your area by talking to your doctor or by contacting the ALS Association.
- Make decisions now about your future medical care. Planning for the future allows you to be in control of decisions about your life and your care.With the help of your doctor, hospice nurse or social worker, you can decide whether you want certain life-extending procedures.You can also decide where you want to spend your final days. You may consider hospice care options. Planning for the future can help you and your loved ones put to rest some common anxieties.
- Amyotrophic Lateral Sclerosis (ALS) Fact Sheet. National Institute of Neurological Disorder and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Amyotrophic-Lateral-Sclerosis-ALS-Fact-Sheet[↩]
- Amyotrophic Lateral Sclerosis (ALS). Centers for Disease Control and Prevention. https://www.cdc.gov/dotw/als/index.html[↩]
- All About ALS. National Institutes of Health. https://newsinhealth.nih.gov/2015/08/all-about-als[↩][↩]
- National Amyotrophic Lateral Sclerosis (ALS) Registry. Agency for Toxic Substances and Disease Registry. https://wwwn.cdc.gov/ALS/ALSRegistryResources.aspx[↩]
- Amyotrophic Lateral Sclerosis (ALS) Fact Sheet. National Institute of Neurological Disorders. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Amyotrophic-Lateral-Sclerosis-ALS-Fact-Sheet[↩]
- Amyotrophic lateral sclerosis. Genetics Home Reference. https://ghr.nlm.nih.gov/condition/amyotrophic-lateral-sclerosis[↩]
- Kinsley L, Siddique T. Amyotrophic Lateral Sclerosis Overview. GeneReviews. https://www.ncbi.nlm.nih.gov/books/NBK1450/[↩]
- Amyotrophic lateral sclerosis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/amyotrophic-lateral-sclerosis/symptoms-causes/syc-20354022[↩]