Contents
What is ameloblastoma
Ameloblastoma is a rare noncancerous (benign) locally aggressive but slow growing tumor of the jaw involving abnormal tissue growth. The word ameloblastoma comes from the English word “amel” which means enamel and the Greek word “blastos” which means germ 1. The resulting tumors or cysts are usually not malignant (benign) but the tissue growth may be aggressive in the involved area. On occasion, tissue near the jaws, such as around the sinuses and eye sockets, may become involved as well, giving rise to facial distortion.
Ameloblastoma begins in the cells that form the protective enamel lining on your teeth from the residual epithelium of the tooth germ, epithelium of odontogenic cysts stratified squamous epithelium and epithelium of the enamel organ 2. Ameloblastoma arises from the mandible in approximately 80% of cases, mostly in association with an unerupted tooth. In addition, ameloblastoma may arise from the tuberosity of maxillary sinus in approximately 20% of cases 3. In the United States, ameloblastoma accounts for 1% of all tumors/cysts of jaw, 1% of all head and neck neoplasms, and 10% of all tumors arising from mandible or maxilla 4. Ameloblastoma accounts for 9–11% of all odontogenic tumors with an incidence rate of 0.5 cases per-million 5. Ameloblastoma occurs in men more often than it occurs in women. Though it can be diagnosed at any age, ameloblastoma is most often diagnosed in adults in their 30s and 40s. Ameloblastoma can be very aggressive, growing into the jawbone and causing swelling and pain. Ameloblastoma rarely invades the orbit; if it does, it involves the orbit in the elderly with male predilection 6. Very rarely, ameloblastoma cells can spread to other areas of the body, such as the lymph nodes in the neck and the lungs. Malignancy is uncommon as are metastases, but when they occur, lungs are involved in over 80% of cases 7.
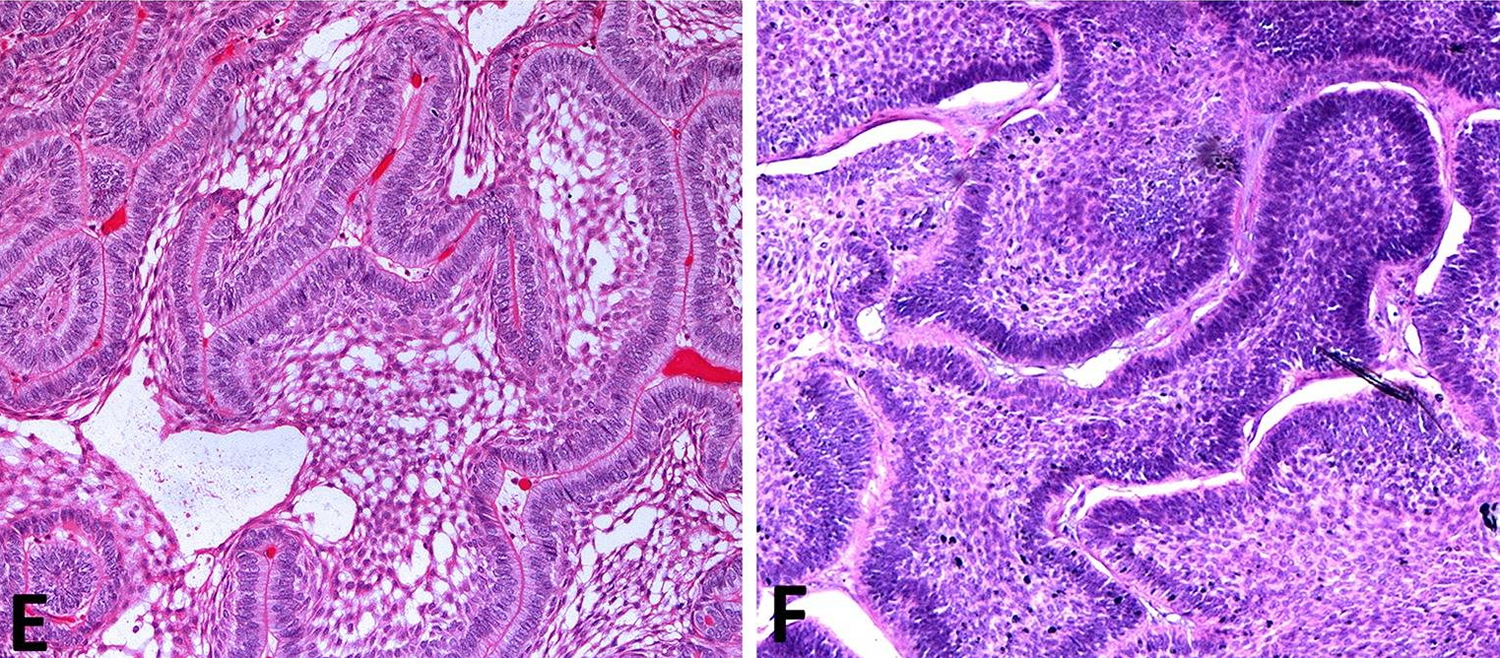
Several histologic types of ameloblastoma are described in the literature including plexiform, follicular, basal cell, granular cell, clear cell, and acanthomatous. The plexiform and follicular types are the most common patterns 5. The follicular ameloblastoma (Figure 4 E) is further subdivided into acanthomatous, granular, spindle cell, and basal cell types. Ameloblastomas are classified by the most predominant histologic pattern present 8. In the plexiform pattern (see Figure 2 A), the connective tissue is surrounded by epithelial components while in the follicular pattern, the epithelium is surrounded by the connective tissue 4. The basal cell-like pattern (Figure 4 F) is apparently benign and tends to grow in an island-like pattern. The basaloid appearing cells tend to stain basophilic deeply. The cells in the central portion may be polyhedral to spindle shaped; stellate reticulum-like areas are notably absent 9. It is reported that tumors with follicular and acanthomatous histology have the highest and lowest recurrence rates, respectively 10.
In a literature review 11, the most common pattern of orbital ameloblastoma was follicular (48.1%), followed by plexiform (37%), basal cell-like (7.4%), and mixed ( 7.4%). In males, the most common tumor pattern was plexiform (50%), followed by follicular (35%), mixed (10%), and basal cell-like (5%). In females, the most prevalent type was follicular (6/7; 85.7%) followed by basal cell-like (14.3%). Plexiform pattern was not reported in female cases 11.
The causative mutation leading to ameloblastoma is the activation of FGFR2, BRAF, and RAS that can lead to the dysregulation of the MAPK signaling as a pivotal step in the pathogenesis of the tumor 12. It seems that different mutations are involved in maxillary and mandibular ameloblastoma, and this may partially explain the higher aggressive behavior of the maxillary type. McClary et al. 5 in their review, proposed that specifically smoothened (SMO) and RAS were the most prevalent mutated genes in maxillary ameloblastoma, while, BRAF was the most one in the mandibular counterpart.
Four distinct growth variants of ameloblastoma are recognized in the current 2005 WHO classification for head and neck tumors 13:
- Peripheral, in which tumor is extraosseous and shows continuity with the oral mucosal stratified squamous epithelium,
- Unicystic, in which a single cystic intraosseous growth pattern is observed grossly and radiographically,
- Solid/multicystic, in which invasive tumor permeates bone marrow spaces and may show multicystic foci, and
- Desmoplastic, an infiltrative intraosseous tumor dominated by the stromal component, radiographically reminiscent of a fibro-osseous lesion 14.
The intraosseous ameloblastomas are collectively termed “central ameloblastomas” 14. Approximately 80 % of central ameloblastomas arise in the mandible, but involvement of the maxilla is rare 15. Various histologic patterns are recognized in unicystic, solid/multicystic, and peripheral growth variants of ameloblastoma.
The benign histology and indolent behavior of ameloblastoma have led to a traditionally conservative surgical approach. However, while histologically benign, ameloblastoma, particularly the solid/multicystic variant, is characterized by locally aggressive spread with up to 90 % recurrence rate following conservative excision 8. Prolonged tumor duration and multiple recurrences have been associated with metastases of the histologically benign-appearing ameloblastoma, so called “metastasizing ameloblastoma” 16. Additionally, long-standing and recurrent ameloblastoma has been shown to occasionally transform into an aggressive ameloblastic carcinoma 17.
Recent data from several centers suggests that the initial surgical management approach and histologic growth pattern are the most important prognostic determinants in ameloblastoma 17, 18. Radical surgery can achieve recurrence rates as low as 0–4.5 % and wider resection may be required for ameloblastomas with more aggressive histologic patterns, such as follicular, granular cell, and acanthomatous variants 18. Despite these findings, the debate on an ideal management that would achieve cure without unnecessary compromise of cosmesis and function, is ongoing. The continued controversy stems in part from the outcome data generated by the small retrospective case series without sufficient patient follow-up 19.
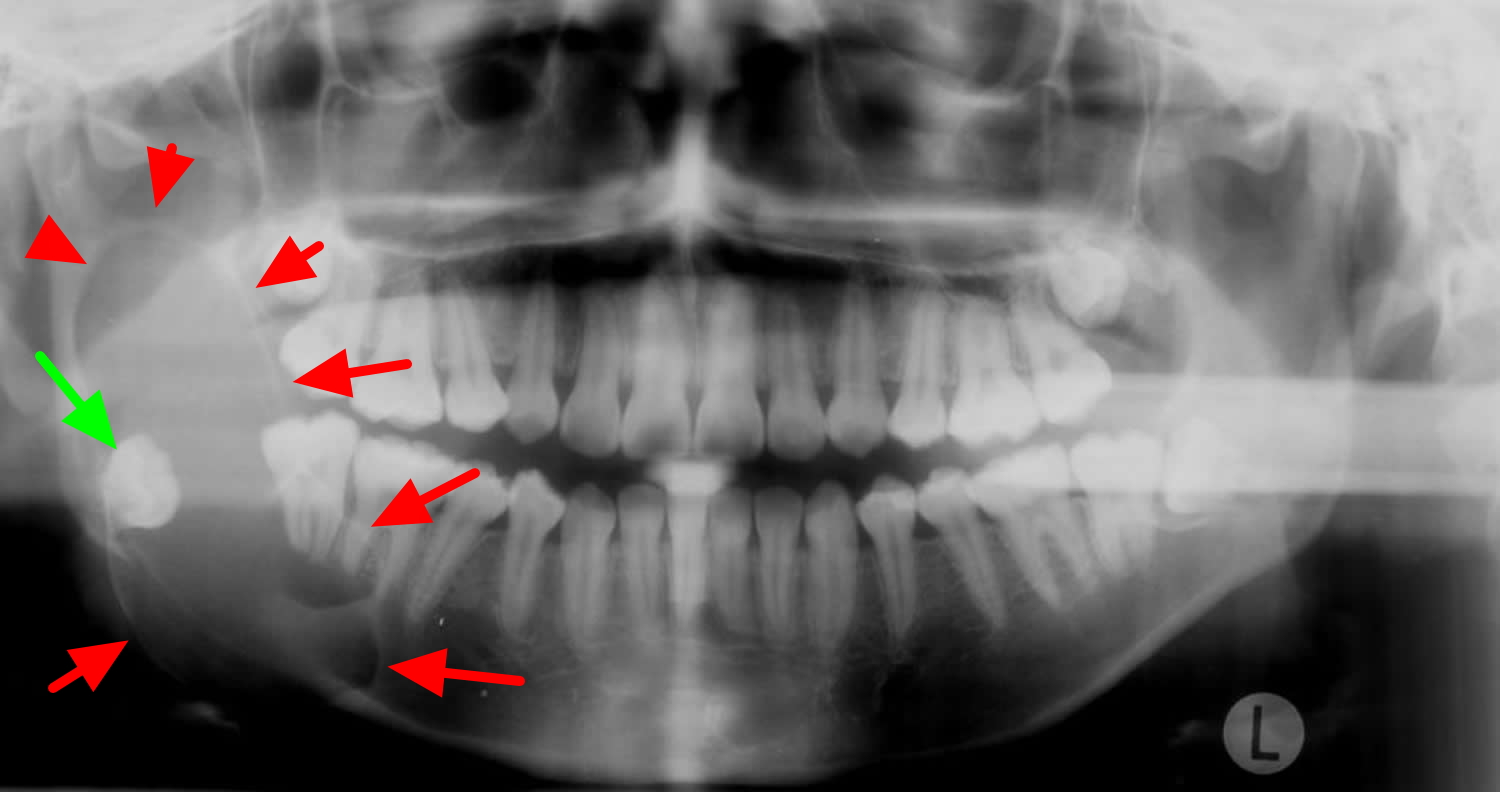
Figure 1. Ameloblastoma histology
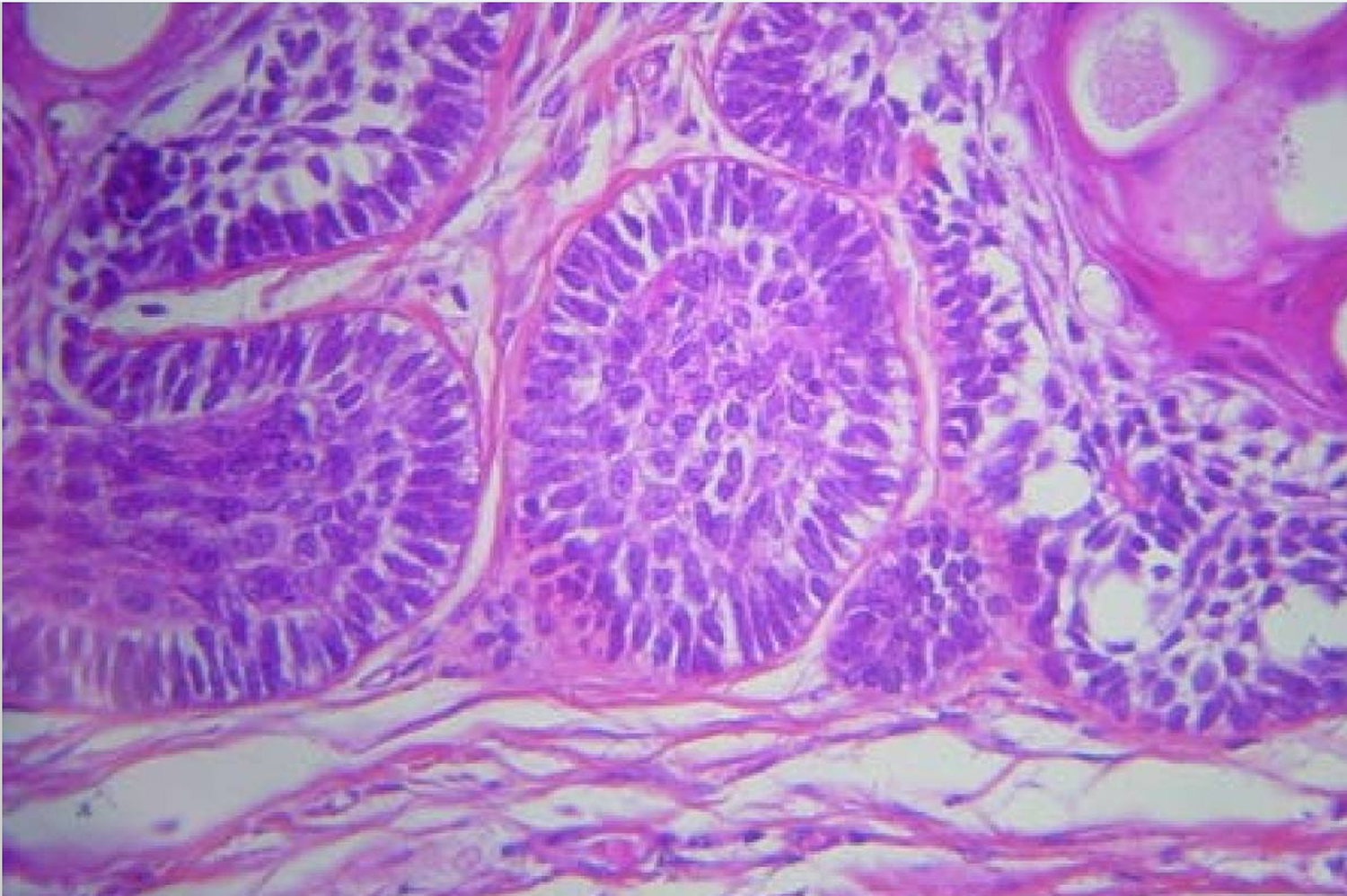
[Source 20]Figure 2. Ameloblastoma histology – Histologic patterns in solid/multicystic ameloblastoma. A) Plexiform ameloblastoma demonstrates interweaving fascicles of neoplastic cells with hyperchromatic columnar nuclei, polarized away from the basement membrane (“reversed polarity”, “piano-key” arrangement). B) Islands of granular ameloblastoma demonstrate central stellate reticulum-like cells with abundant eosinophilic granular cytoplasm.
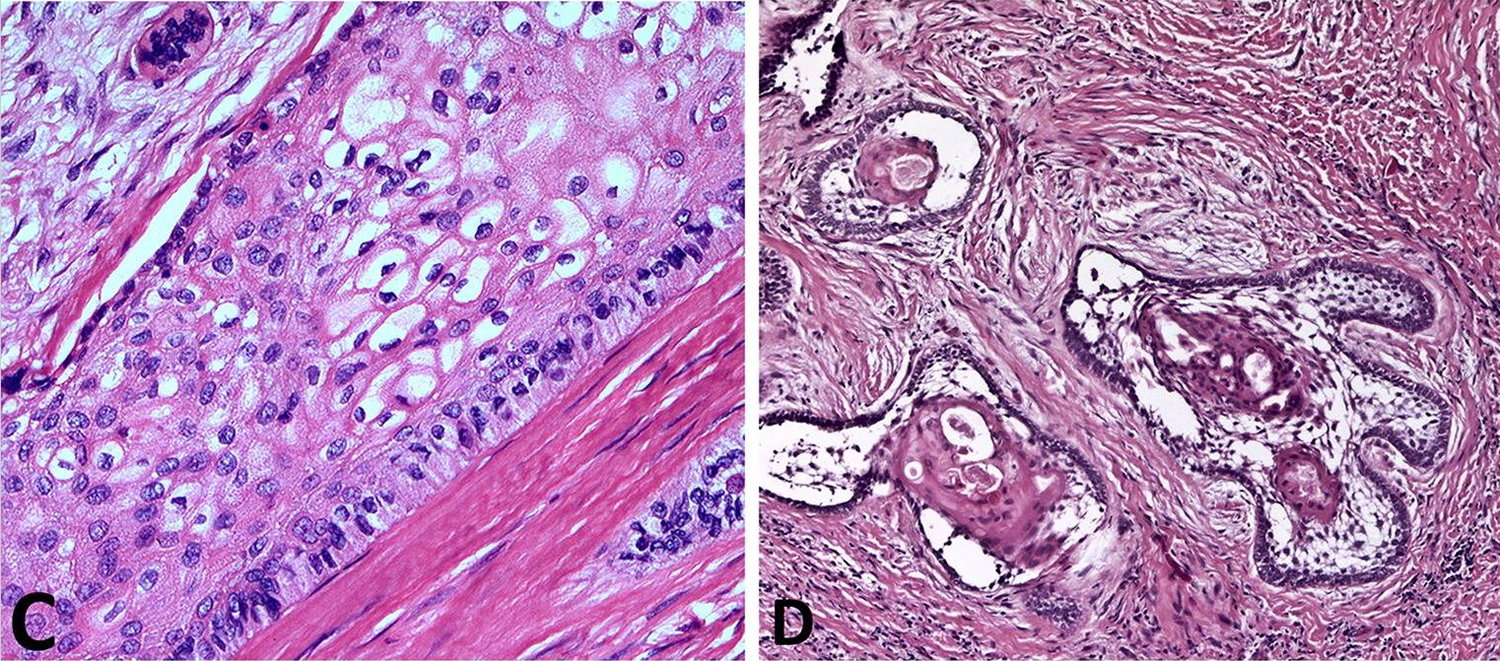
Figure 3. Ameloblastoma histology – Histologic patterns in solid/multicystic ameloblastoma. C) Acanthomatous ameloblastoma shows squamous-type differentiation of the central stellate reticulum-like cells, while maintaining the reverse polarization of the nuclei in columnar cells lining the nests. D) Desmoplastic ameloblastoma shows islands of odontogenic epithelium in abundant desmoplastic stroma.
Figure 4. Ameloblastoma histology – Histologic patterns in solid/multicystic ameloblastoma. E) Follicular ameloblastoma islands demonstrate peripheral columnar cells exhibiting reversal of polarity and central stellate-reticulum like cells with cystic degeneration. F) Basal cell type ameloblastoma islands contain basaloid cells with scant cytoplasm and peripheral palisading, reminiscent of basal cell carcinoma.
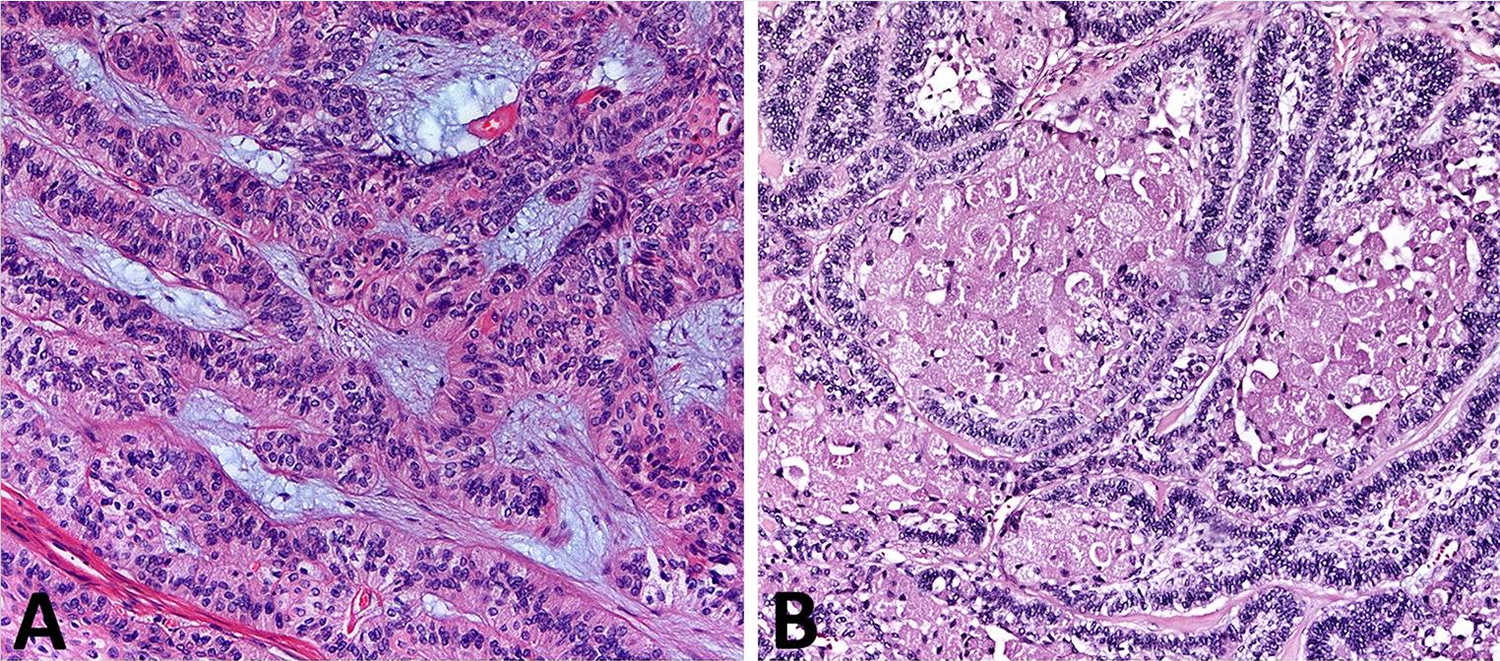
Figure 5. Ameloblastoma on OPG (orthopantomography) – there is a large lucent lesion expanding the right ramus of the mandible (red arrows). It is associated with the crown of the unerrupted right mandibular 3rd molar (green arrow) and has features most in keeping with an ameloblastoma
Figure 6. Ameloblastoma CT scan
Acanthomatous ameloblastoma
Acanthomatous ameloblastoma type of ameloblastoma is one of the rarest types. Acanthomatous ameloblastoma is usually seen in older aged human population and most commonly reported in canine region of dogs in literature 21. Acanthomatous ameloblastoma is a benign tumor, but is locally aggressive and frequently invades the alveolar bone or recurs after marginal surgical excision. It is classified as an ameloblastoma; however controversies exist as to whether this tumor should be classified as a basal cell carcinoma, epulis or an odontal origin tumor 22.
Patients may complain or present with the history of a slow growing mass, malocclusion, loose teeth or more rarely paresthesia and pain, however many lesions are detected incidentally on radiographic studies in asymptomatic patients. The lesions usually progress slowly but if left untreated can resorb the cortical plate and extend into adjacent tissue7. In our case the patient only reported regarding slowly progressive swelling and difficulty in mastication.
The treatment of choice is complete surgical resection. If possible, conservative surgery can be used if an assured complete removal can be performed 23. In addition to low sensitivity of this neoplasm, the intraosseous location of the ameloblastoma prevents the use of radiotherapy as an effective therapeutic option because radiation induces the potential development of secondary tumors. Therefore, in all types of ameloblastomas, a thorough long term clinical and radiographic follow up is always recommended 24.
Ameloblastoma prognosis
Generally, prognosis of maxillary ameloblastoma is worse than the mandibular type due to its more recurrence rate, invasion to vital structures, and more advanced stages at the time of diagnosis due to lack of pain or other harbinger symptoms 25. Orbital ameloblastoma has an additional tendency to be transformed into the carcinomatous variant. Hence, the prognosis of orbital ameloblastomas in line with tumors involving skull base seems to be the worst 26.
Ameloblastoma is, in essence, a lifelong disease. Although most tumors recur within 5 years of original diagnosis, late recurrences are not uncommon, and were seen in 23 % of the patients in the current study. While neglected and recurrent ameloblastoma can cause significant morbidity, mortality is extremely rare and is seen typically in a setting of maxillary ameloblastoma extending into the cranium 17. The rare metastasizing ameloblastoma and ameloblastic carcinoma, each described in up to 2 % of patients with ameloblastoma, can also infrequently lead to mortality 17.
In a review, survival among all cases was 13.47 ± 12.81 years and among different patterns of tumor varied. Among the cases with more than five years of survival (five cases died before 5 years), survival was 16.4 ± 15.1 years in follicular and 18.1 ± 9.9 years in plexiform types, respectively 11.
Maxillary ameloblastoma is a locally aggressive neoplasm so that physicians must be alert to the biologic behavior of this tumor to detect any invasion to critical structures such as orbit and cranium. Meticulous patient follow-up with regular clinical examinations and diagnostic work-up (especially MRI) for timely detection of any invasion or recurrence of this tumor.
Orbital ameloblastoma causes significant morbidity and mortality. In extensive and longstanding tumors, a multidisciplinary approach is required that may span several specialties i.e. neurosurgery, head and neck surgery/otolaryngology, maxillofacial surgery, ophthalmology, and radiotherapy. This joint effort may take several years to handle the condition to the extent that a recurrence may be detected as late as three decades since the initial diagnosis.
Ameloblastoma signs and symptoms
Ameloblastomas typically occur as hard, painless lesions near the angle of the mandible in the region of the 3rd molar tooth (48 and 38) although they can occur anywhere along the alveolus of the mandible (80%) and maxilla (20%). When the maxilla is involved, the tumor is located in the premolar region and can extend up into the maxillary sinus.
Although benign, it is a locally aggressive neoplasm with a high rate of recurrence. Approximately 20% of cases are associated with dentigerous cysts and unerupted teeth.
Ameloblastomas do not usually become malignant. There is evidence that tissue is more likely to become malignant if the condition reoccurs after surgery.
Ameloblastoma diagnosis
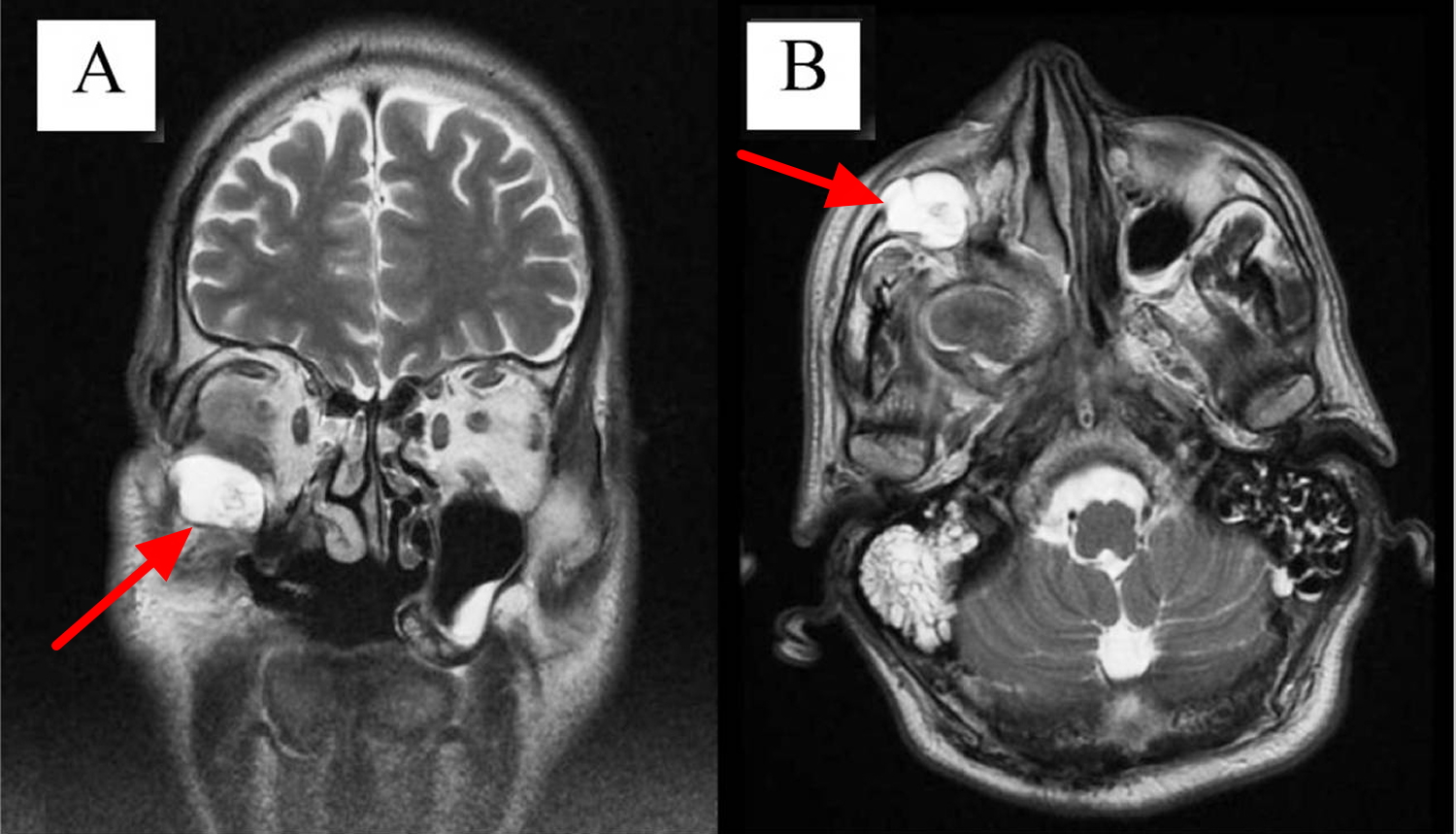
Ameloblastoma can show up either in a regular x-ray or in an MRI imaging study. Radiographic studies play a cardinal role in pre-operative and post-operative management of patients with ameloblastoma. Dental X-rays (orthopantomography) typically demonstrate a lytic lesion with scalloped margins or a “soap bubble” appearance, which can be associated with resorption of tooth roots and impacted teeth 8. Orthopantomography can help detect asymptomatic ameloblastomas. CT has emerged as the most useful diagnostic imaging modality, demonstrating expansile, lytic, unilocular or multilocular cystic lesions with or without soft tissue extension. In addition to CT, MRI has been recommended in evaluation of patients with maxillary ameloblastoma, because of its potential to more precisely evaluate the soft tissue extent of the lesion 8.
Ameloblastoma radiology
Ameloblastomas originated within bone are mostly diagnosed incidentally in pan-tomography imaging or plain films. The routine radiographic picture is the ‘soap bubble’ appearance 27. Plain X-ray imaging has limited sensitivity and specificity to evaluate tumor invasion. CT can be useful in detecting bone extensions, and MRI provides better resolution in detecting soft tissue extensions and tumor margins, particularly in maxillary ameloblastoma 28. Particularly, in diagnosing the desmoplastic type, the MRI plays a pivotal role due to poor defined soft tissue extensions in addition to the similarity to fibro-osseous lesions 29.
Figure 7. Ameloblastoma MRI T2 (A: Coronal view showing a round enhanced mass in the inferior orbit. B: Axial view.)
Ameloblastoma treatment
In treating ameloblastoma, the mainstay is radical surgery including en-bloc resection 5. Concerning the management of mandibular ameloblastoma, some authors maintain that partial resection or curettage is enough while many recommend radical excision. This inconsistency comes from easier follow-up and lower invasion risk of mandibular type to vital structures 5.
Radiotherapy when employed as the first line treatment has a recurrence rate as high as 70% 10. Even more, there is a study in which all the patients were reported to experience recurrence following the sole radiation therapy 30. Hence, radiotherapy alone is not wise in the management of ameloblastoma. However, radiotherapy has been shown to be effective in decreasing the tumor size and pain palliation. Therefore, radiotherapy can still be placed in the therapeutic arsenal for cases with recurrence, unresectable tumors, and patients who are unable to undergo surgery for any reason 5.
The role of chemotherapy in the management of ameloblastoma is an issue of debate. Some authors suggest that ameloblastoma may be sensitive to platinum-based agents. Some 31, 32, 33 report promising results by this modality for advanced cases while others5, 12, 23 maintain that this method is not effective in reducing tumor size or even palliation. In the literature, there are sparse instances of molecular-targeted therapy that should be further examined in future studies. Kaye et al. 34 reported a patient with multiple recurrent ameloblastoma in the mandible and metastatic ameloblastoma in the lung who harbored a BRAF V600E mutation. The patient was treated with a combination of dabrafenib (BRAF inhibitor) and trametinib (MEK inhibitor) and achieved a dramatic response after 8 weeks of therapy. Additionally, in another study, reducing the tumor size using vismodegib (SMO inhibitor) was reported 35.
Ameloblastoma surgery
In the maxillary type, morphology, histopathology, and extension of the tumor are crucial in decision-making. The recommended safe margin for unicystic ameloblastoma, multicystic ameloblastoma, and ameloblastic carcinoma is proposed to be 1–1.5, 1.5–2, and 2–3 cm, respectively 36.
Regarding the management of maxillary ameloblastoma involving the orbit, the following strategies can be used alone or in combination with each other 37:
- (i) In tumors not involving orbital fat/soft tissue, a complete resection of the mass may suffice.
- (ii) For cases with orbital floor involvement, total maxillectomy is reasonable.
- (iii) In cases with orbital soft tissue involvement, orbital exenteration is inevitable.
- (iv) Skull base invasion, if occurred, necessitates resection of anterior skull base.
Recurrence after partial resection of the maxillary ameloblastoma results in a tumor with more aggressive behavior with higher mortality rates (33–60%) 38. To reduce the recurrence rate, it is wise to perform the MRI and CT for more investigation of tumor extension, preoperatively 5.
- Brazis PW, Miller NR, Lee AG, Holliday MJ. Neuro-ophthalmologic aspects of ameloblastoma. Skull Base Surg. 1995;5(4):233–244. doi: 10.1055/s-2008-1058921. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1656531/pdf/skullbasesurg00026-0046.pdf[↩]
- Masthan K.M., Anitha N., Krupaa J., Manikkam S. Ameloblastoma. J Pharm Bioallied Sci. 2015;7(Suppl 1):S167–S170. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4439660/[↩]
- Gold L. Biologic behavior of ameloblastoma. Oral Maxillofac Surg Clin North Am. 1991;3(1):21–27.[↩]
- Morgan P.R. Odontogenic tumors: a review. Periodontol 2000. 2011;57(1):160–176. https://www.ncbi.nlm.nih.gov/pubmed/21781186[↩][↩]
- McClary A.C., West R.B., McClary A.C. Ameloblastoma: a clinical review and trends in management. Eur Arch Oto-Rhino-Laryngol. 2016;273(7):1649–1661. https://www.ncbi.nlm.nih.gov/pubmed/25926124[↩][↩][↩][↩][↩][↩][↩]
- Chowdhury M.O.R., Islam S., Chowdhury W., Haque M. Extensive ameloblastoma of the mandible. TAJ J Teach Assoc. 2002;15(2):93–95.[↩]
- Pulmonary metastasis of ameloblastoma: case report and review of the literature. Henderson JM, Sonnet JR, Schlesinger C, Ord RA. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999 Aug; 88(2):170-6. https://www.ncbi.nlm.nih.gov/pubmed/10468461/[↩]
- McClary AC, West RB, McClary AC, Pollack JR, Fischbein NJ, Holsinger CF, Sunwoo J, Colevas AD, Sirjani D. Ameloblastoma: a clinical review and trends in management. Eur Arch Otorhinolaryngol. 2015 https://www.ncbi.nlm.nih.gov/pubmed/25926124[↩][↩][↩][↩]
- Kessler H.P. Intraosseous ameloblastoma. Oral Maxillofac Surg Clin North Am. 2004;16(3):309–322. https://www.ncbi.nlm.nih.gov/pubmed/18088733[↩]
- Reichart P.A., Philipsen H.P., Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31b(2):86–99. https://www.ncbi.nlm.nih.gov/pubmed/7633291[↩][↩]
- Abtahi M-A, Zandi A, Razmjoo H, et al. Orbital invasion of ameloblastoma: A systematic review apropos of a rare entity. Journal of Current Ophthalmology. 2018;30(1):23-34. doi:10.1016/j.joco.2017.09.001. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5859465/[↩][↩][↩]
- Brown N.A., Betz B.L. Ameloblastoma: a review of recent molecular pathogenetic discoveries. Biomarkers Cancer. 2015;7(Suppl 2):19–24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4597444/[↩]
- Milman T, Ying G-S, Pan W, LiVolsi V. Ameloblastoma: 25 Year Experience at a Single Institution. Head and Neck Pathology. 2016;10(4):513-520. doi:10.1007/s12105-016-0734-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5082058/[↩]
- Barnes L, Eveson JW, Reichart P, Sidransky D. World Health Organization classification of tumors. Pathology and genetics of head and neck tumours. Lyon: IARC Press; 2005.[↩][↩]
- Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer Part B Oral Oncol. 1995;31B:86–99. doi: 10.1016/0964-1955(94)00037-5. https://www.ncbi.nlm.nih.gov/pubmed/7633291[↩]
- Luo DY, Feng CJ, Guo JB. Pulmonary metastases from an ameloblastoma: case report and review of the literature. J Craniomaxillofac Surg. 2012;40:e470–e474. doi: 10.1016/j.jcms.2012.03.006. https://www.ncbi.nlm.nih.gov/pubmed/22507293[↩]
- Zwahlen RA, Grätz KW. Maxillary ameloblastomas: a review of the literature and of a 15-year database. J Craniomaxillofac Surg. 2002;30:273–279. doi: 10.1016/S1010-5182(02)90317-3. https://www.ncbi.nlm.nih.gov/pubmed/12377199[↩][↩][↩][↩]
- Sham E, Leong J, Maher R, Schenberg M, Leung M, Mansour AK. Mandibular ameloblastoma: clinical experience and literature review. ANZ J Surg. 2009;79:739–744. doi: 10.1111/j.1445-2197.2009.05061.x. https://www.ncbi.nlm.nih.gov/pubmed/19878171[↩][↩]
- de Almeida R AC, Andrade ES, Barbalho JC, Vajgel A, Vasconcelos BC. Recurrence rate following treatment for primary multicystic ameloblastoma: systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2016;45:359–367. doi: 10.1016/j.ijom.2015.12.016. https://www.ncbi.nlm.nih.gov/pubmed/26792147[↩]
- Amzerin M, Fadoukhair Z, Belbaraka R, et al. Metastatic ameloblastoma responding to combination chemotherapy: case report and review of the literature. Journal of Medical Case Reports. 2011;5:491. doi:10.1186/1752-1947-5-491. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3198715/[↩]
- Ugrappa S, Jain A, Fuloria NK, Fuloria S. Acanthomatous Ameloblastoma in Anterior Mandibular Region of a Young Patient: A Rare Case Report. Annals of African Medicine. 2017;16(2):85-89. doi:10.4103/aam.aam_51_16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5452712/[↩]
- Acanthomatous ameloblastoma in dogs treated with intralesional bleomycin. Kelly JM, Belding BA, Schaefer AK. Vet Comp Oncol. 2010 Jun; 8(2):81-6. https://www.ncbi.nlm.nih.gov/pubmed/20579320/[↩]
- Schafer DR, Thompson LDR, Smith BC, Wenig BM. Primary ameloblastoma of the sinonasal tract. Cancer. 1998;82(4):667–674. https://www.ncbi.nlm.nih.gov/pubmed/9477098[↩]
- LR Olieira, BH Matos, PR Dominguete, VA Zorgetto, AR Silva. Ameloblastoma: Report of two cases and a brief literature review. Int.J. Odontostomat. 2011;5(3):293–299.[↩]
- Reija M.G., Izquierdo M., Rueda J.B., Cantera M.G., Hernández A.V. Ameloblastomas maxillaries: a propósito de dos casos clínicos. Acta otorrinolaringol Espanola. 2001;52(3):261–265. http://www.elsevier.es/es-revista-acta-otorrinolaringologica-espanola-102-linkresolver-ameloblastomas-maxilares-a-proposito-dos-S0001651901782064[↩]
- Oliveira L.R., Matos F., Dominguete R., Zorgetto A., Ribeiro A. Ameloblastoma: report of two cases and a brief literature review. Int J Odontostomat. 2011;5(3):293–299.[↩]
- Underhill T., Katz J., Pope T., Jr., Dunlap C. Radiologic findings of diseases involving the maxilla and mandible. AJR Am J Roentgenol. 1992;159(2):345–350. https://www.ajronline.org/doi/pdf/10.2214/ajr.159.2.1632353[↩]
- Becelli R., Carboni A., Cerulli G., Perugini M., Iannetti G. Mandibular ameloblastoma: analysis of surgical treatment carried out in 60 patients between 1977 and 1998. J Craniofacial Surg. 2002;13(3):395–400 https://www.ncbi.nlm.nih.gov/pubmed/12040207[↩]
- Cohen M.A., Hertzanu Y., Mendelsohn D.B. Computed tomography in the diagnosis and treatment of mandibular ameloblastoma: report of cases. J Oral Maxillofac Surg. 1985;43(10):796–800. https://www.ncbi.nlm.nih.gov/pubmed/3862780[↩]
- Sehdev M., Huvos A., Strong E., Gerold F., Willis G. Ameloblastoma of maxilla and mandible. Cancer. 1974;33(2):324–333. https://www.ncbi.nlm.nih.gov/pubmed/4812754[↩]
- [↩]
- Amzerin M., Fadoukhair Z., Belbaraka R. Metastatic ameloblastoma responding to combination chemotherapy: case report and review of the literature. J Med Case Rep. 2011;5:491. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3198715/[↩]
- Ciment L.M., Ciment A.J. Malignant ameloblastoma metastatic to the lungs 29 years after primary resection: a case report. CHEST J. 2002;121(4):1359–1361. https://www.ncbi.nlm.nih.gov/pubmed/11948077[↩]
- Kaye F.J., Ivey A.M., Drane W.E., Mendenhall W.M., Allan R.W. Clinical and radiographic response with combined BRAF-targeted therapy in stage 4 ameloblastoma. J Natl Cancer Inst. 2015;107(1):378. https://www.ncbi.nlm.nih.gov/pubmed/25475564[↩]
- Ally M.S., Tang J.Y., Joseph T. The use of vismodegib to shrink keratocystic odontogenic tumors in patients with basal cell nevus syndrome. JAMA Dermatol. 2014;150(5):542–545. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4024084/[↩]
- Becelli R., Carboni A., Cerulli G., Perugini M., Iannetti G. Mandibular ameloblastoma: analysis of surgical treatment carried out in 60 patients between 1977 and 1998. J Craniofacial Surg. 2002;13(3):395–400. https://www.ncbi.nlm.nih.gov/pubmed/12040207[↩]
- Jackson I., Callan P., Forté R.A. An anatomical classification of maxillary ameloblastoma as an aid to surgical treatment. J Cranio-Maxillofac Surg. 1996;24(4):230–236. https://www.ncbi.nlm.nih.gov/pubmed/8880449[↩]
- Zwahlen R.A., Gratz K.W. Maxillary ameloblastomas: a review of the literature and of a 15-year database. J Cranio-Maxillo-Facial Surg. 2002;30(5):273–279. https://www.ncbi.nlm.nih.gov/pubmed/12377199[↩]