Contents
What is an aortic aneurysm
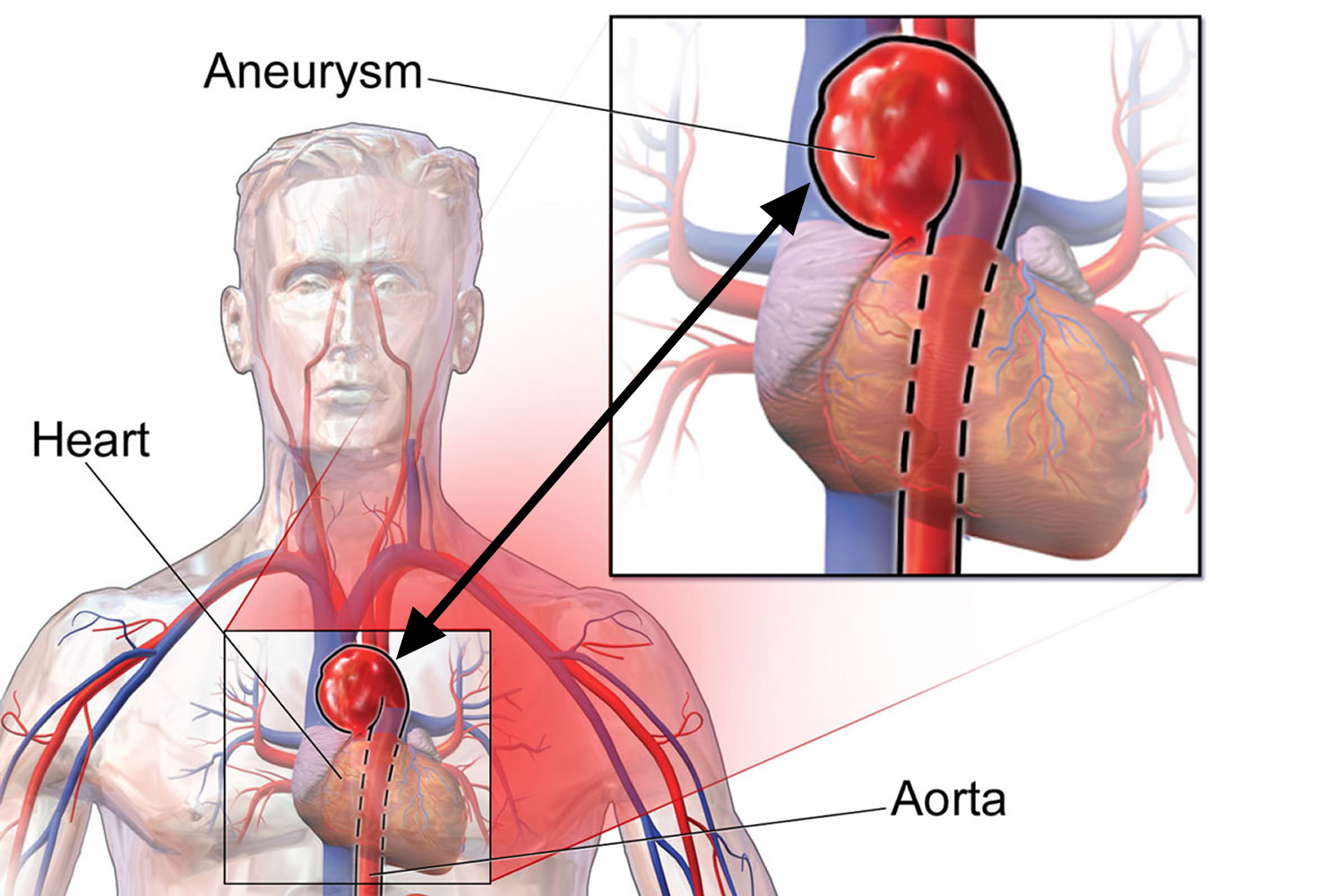
An aneurysm occurs when part of an artery wall weakens, allowing it to widen abnormally or balloon out 1. An aortic aneurysm is an abnormal bulge that occurs in the wall of the major blood vessel (aorta) that carries blood from your heart to your body. Aortic aneurysms can occur anywhere in your aorta and may be tube-shaped (fusiform) or round (saccular).
In older people, aneurysms are most likely to occur in areas where arteries branch (for example, where the abdominal aorta branches into the iliac arteries) or in areas of stress (for example, in the popliteal artery).
Arteries have thick walls to withstand normal blood pressure. However, certain medical problems, genetic conditions, and trauma can damage or injure artery walls. The force of blood pushing against the weakened or injured walls can cause an aneurysm. If an aneurysm grows large, it can burst and cause dangerous bleeding or even death 2. About 13,000 Americans die each year from aortic aneurysms. Most of the deaths result from rupture or dissection.
An aneurysm can grow large and rupture (burst) or dissect. A rupture causes dangerous bleeding inside the body. A dissection is a split in one or more layers of the artery wall. The split causes bleeding into and along the layers of the artery wall.
Both rupture and dissection often are fatal.
Having an aortic aneurysm increases your risk of developing an aortic dissection.
An aortic dissection occurs when a tear develops in the inner layer of the wall of the aorta. This causes one or more of the layers of the wall of the aorta to separate, which weakens the wall of the aorta. Having an aortic aneurysm also increases your risk that the aneurysm can burst (rupture).
The causes of aneurysms are sometimes unknown. Some may be congenital, meaning a person is born with them. An aneurysm may also occur as the result of aortic disease or an injury.
Aortic aneurysms include:
- Abdominal aortic aneurysm. An abdominal aortic aneurysm occurs along the part of the aorta that passes through the abdomen.
- Thoracic aortic aneurysm. A thoracic aortic aneurysm occurs along the part of the aorta that passes through the chest cavity.
In some cases, an individual may have an abdominal aortic aneurysm and a thoracic aortic aneurysm.
According to the Centers for Disease Control and Prevention 3 aortic aneurysms were the primary cause of 9,863 deaths in 2014 and a contributing cause in more than 17,215 deaths in the United States in 2009 4.
About two-thirds of people who have an aortic dissection are male 5.
Besides advanced age and genetics or family history, people who have the following conditions may be at higher risk for an aortic aneurysm or dissection:
- High blood pressure: the increased force of blood can weaken the artery walls
- Genetic conditions, such as Marfan’s Syndrome: that causes problems in the body’s ability to make healthy connective tissue
- High cholesterol or atherosclerosis: a build-up of plaque may cause increased inflammation in and around the aorta and other blood vessels
- Inflamed arteries: Trauma such as car accidents, certain diseases, and conditions like vasculitis can cause the body’s blood vessels to become inflamed
- Smoking: People with a history of smoking are 3 to 5 times more likely to develop an aortic aneurysm
The U.S. Preventive Services Task Force recommends that men aged 65–75 years who have ever smoked should get an ultrasound screening for abdominal aortic aneurysms, even if they have no symptoms.
Most aneurysms are found during tests done for other reasons. Some people are at high risk for aneurysms. It is important for them to get screening, because aneurysms can develop and become large before causing any symptoms.
- Screening is recommended for people between the ages of 65 and 75 if they have a family history, or if they are men who have smoked. Doctors use imaging tests to find aneurysms.
Early diagnosis and treatment can help prevent rupture and dissection. However, aneurysms can develop and become large before causing any symptoms. Often doctors can stop aneurysms from bursting if they find and treat them early. They use imaging tests to find aneurysms. Often aneurysms are found by chance during tests done for other reasons. Medicines and surgery are the two main treatments for aneurysms.
People living with aortic disease or other heart-related conditions can improve their odds for a longer, healthier life. It’s important to:
- Report any symptoms immediately.
- Get regular check-ups.
- Always take care of your overall heart health.
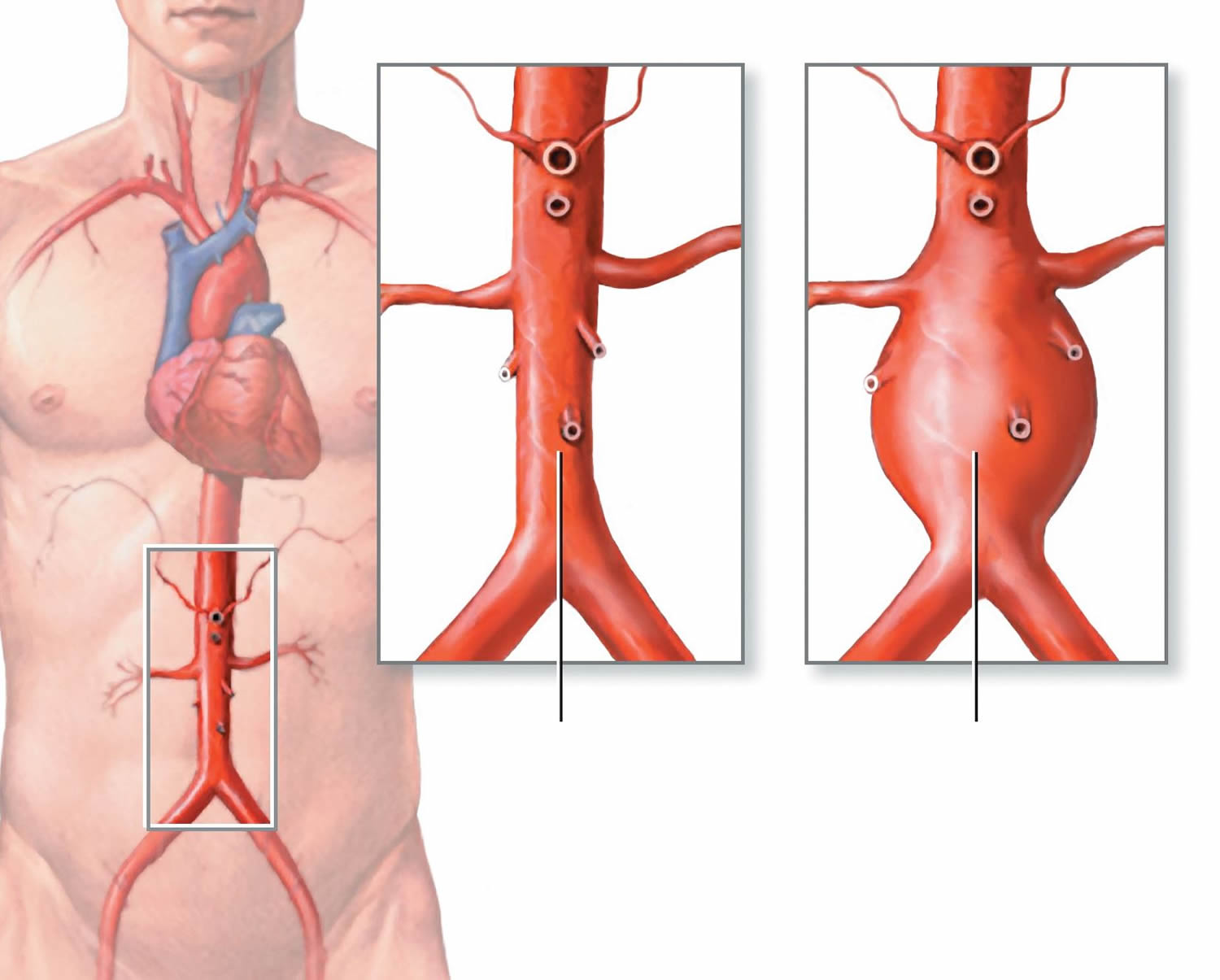
Figure 1. Aortic Aneurysm
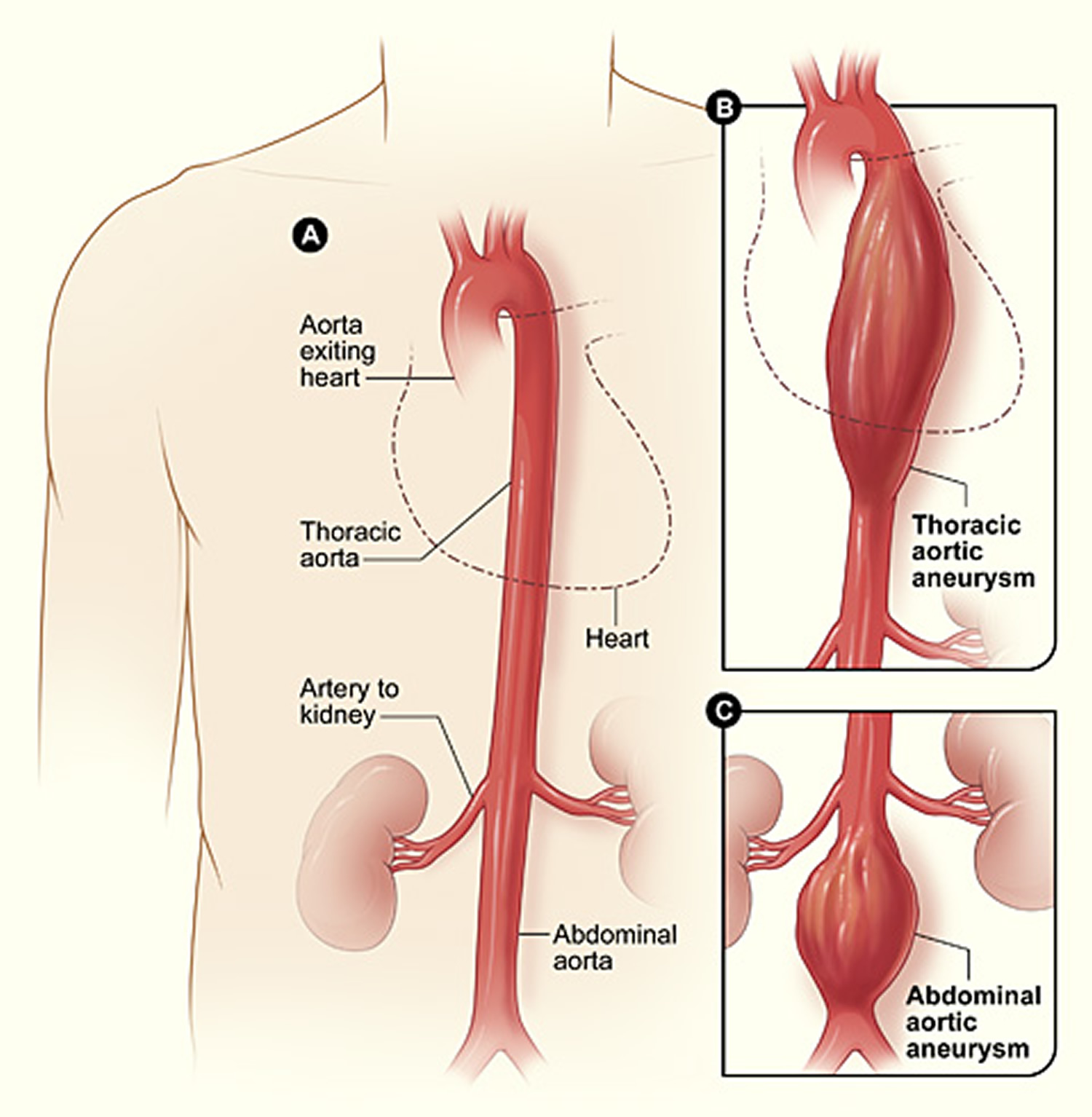 Note: (A) shows a normal aorta. Figure B shows a thoracic aortic aneurysm, which is located behind the heart. Figure C shows an abdominal aortic aneurysm, which is located below the arteries that supply blood to the kidneys.
Note: (A) shows a normal aorta. Figure B shows a thoracic aortic aneurysm, which is located behind the heart. Figure C shows an abdominal aortic aneurysm, which is located below the arteries that supply blood to the kidneys.The Aorta
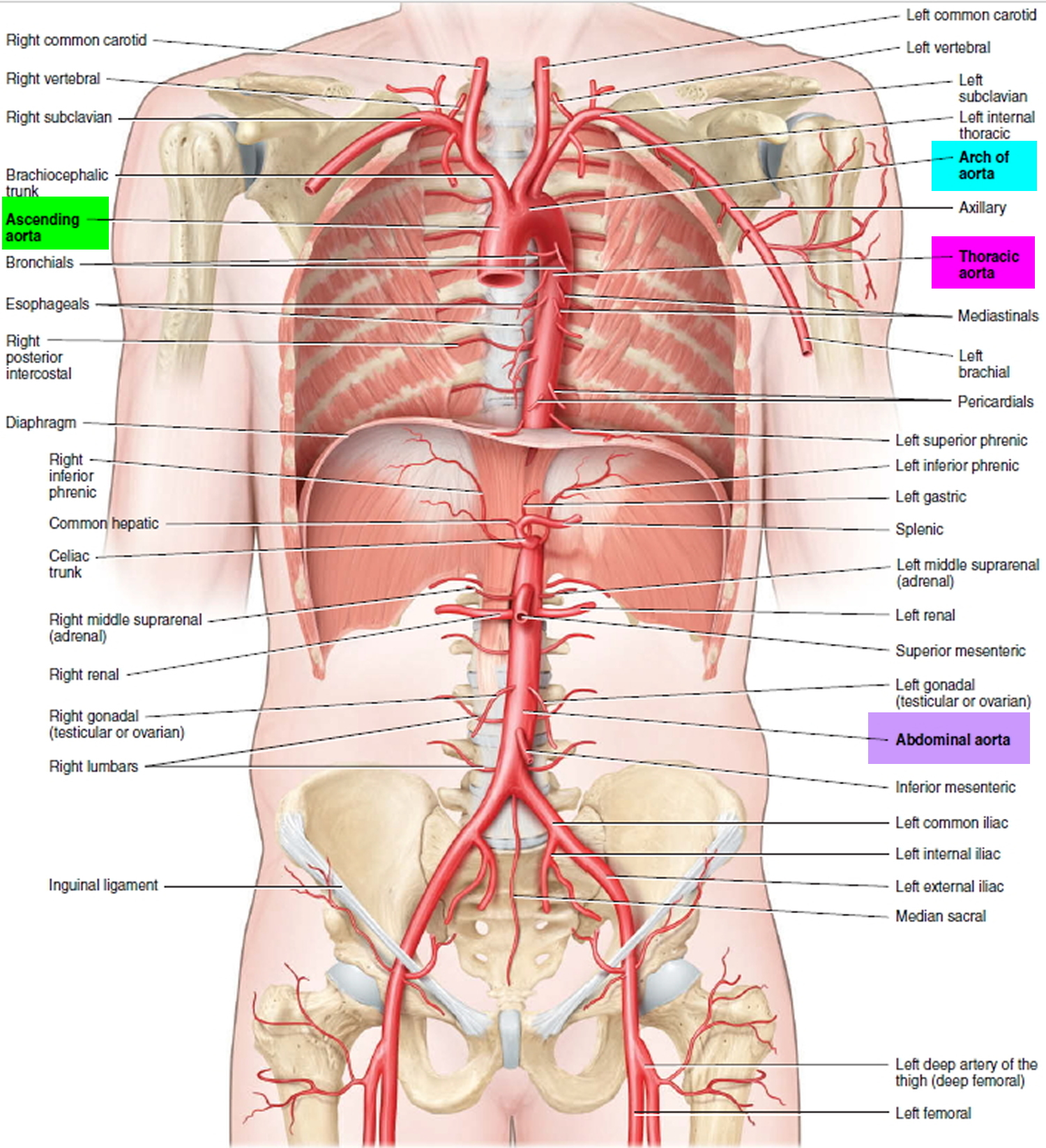
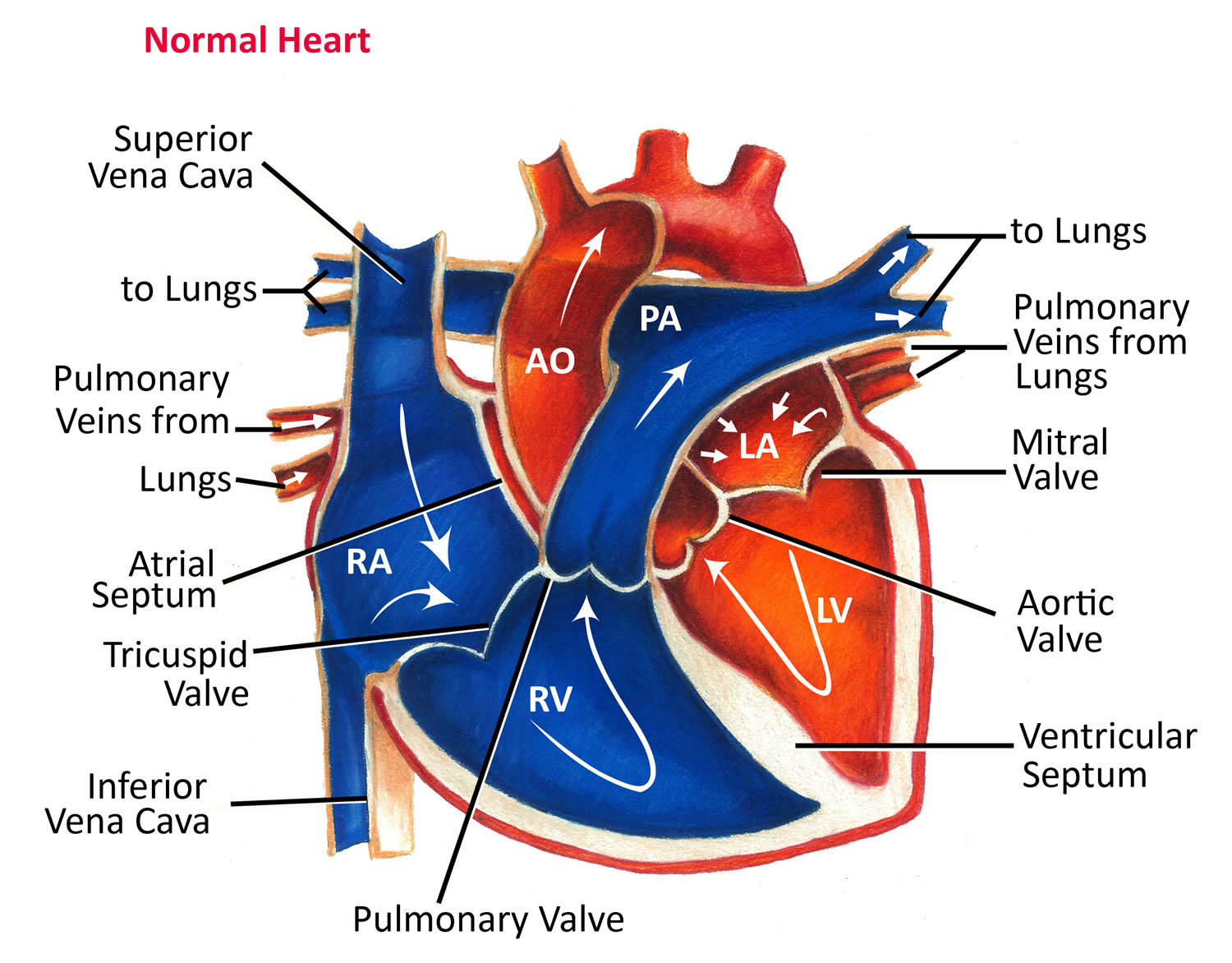
The aorta is the largest artery of the body, with a diameter of 2–3 cm (about 1 inch). Its four principal divisions are (see Figure 1):
- Ascending aorta,
- Arch of the aorta,
- Thoracic aorta,
- Abdominal aorta.
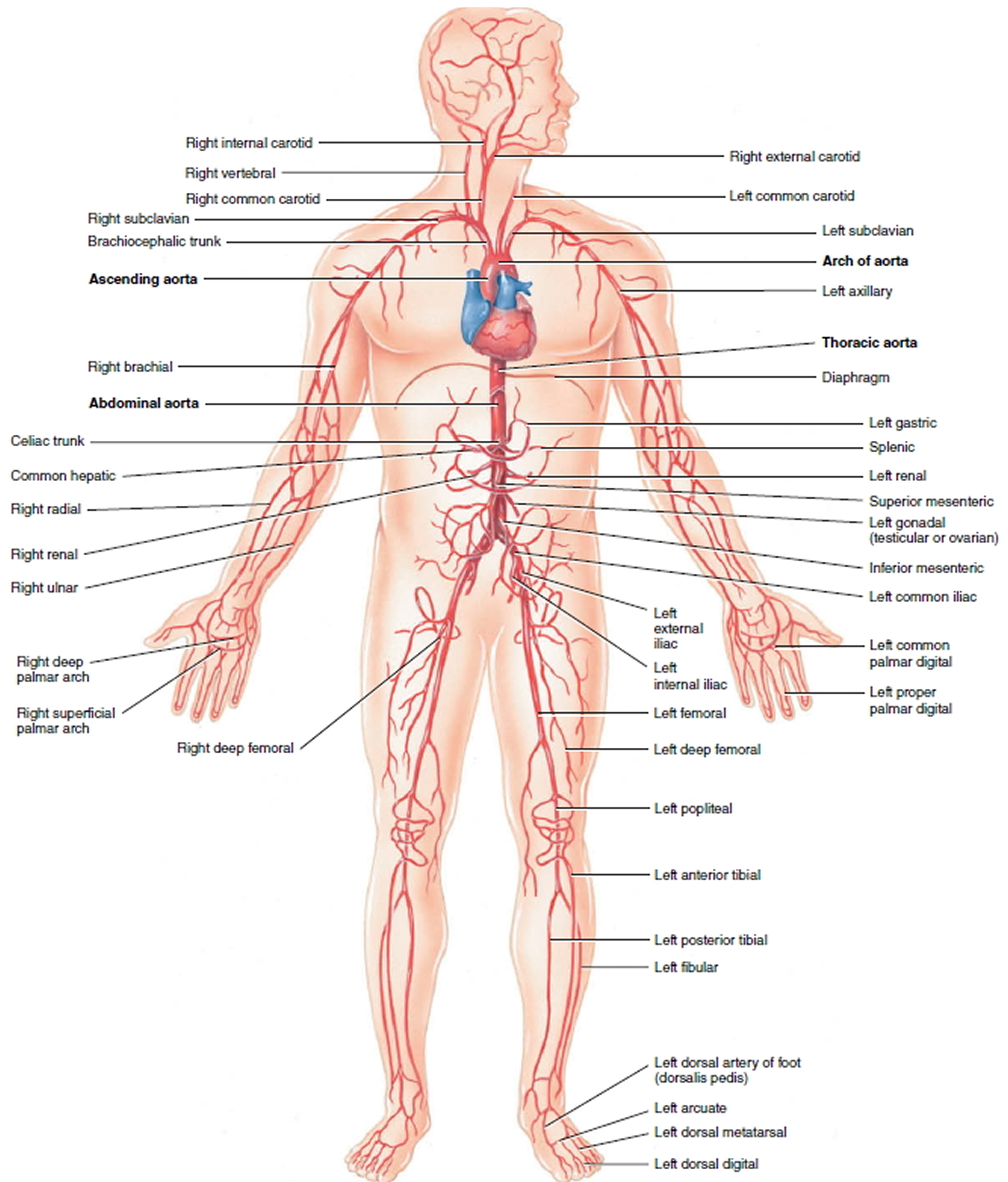
The portion of the aorta that emerges from the left ventricle posterior to the pulmonary trunk is the ascending aorta (see Figures 1 and 2). The beginning of the aorta contains the aortic valve (see Figure 3). The ascending aorta gives off two coronary arteries that supply the myocardium of the heart. Then the ascending aorta arches to the left, forming the arch of the aorta, which descends and ends at the level of the intervertebral disc between the fourth and fifth thoracic vertebrae. As the aorta continues to descend, it lies close to the vertebral bodies and is called the thoracic aorta. When the thoracic aorta reaches the bottom
of the thorax it passes through the aortic hiatus of the diaphragm to become the abdominal aorta. The abdominal aorta descends to the level of the fourth lumbar vertebra where it divides into two common iliac arteries, which carry blood to the pelvis and lower limbs. Each division of the aorta gives off arteries that branch into distributing arteries that lead to various organs. Within the organs, the arteries divide into arterioles and then into capillaries that service the systemic tissues (all tissues except the alveoli of the lungs).
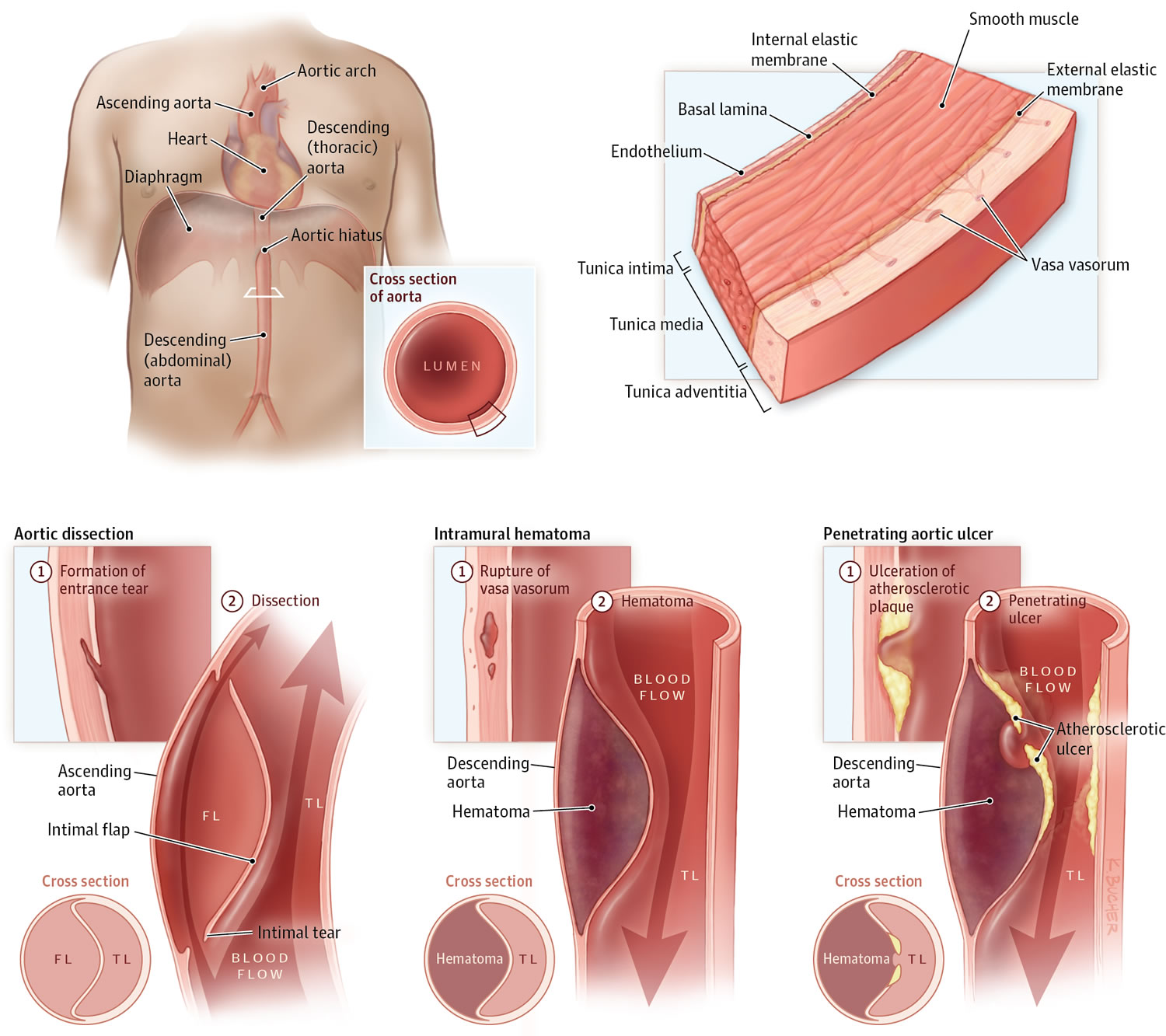
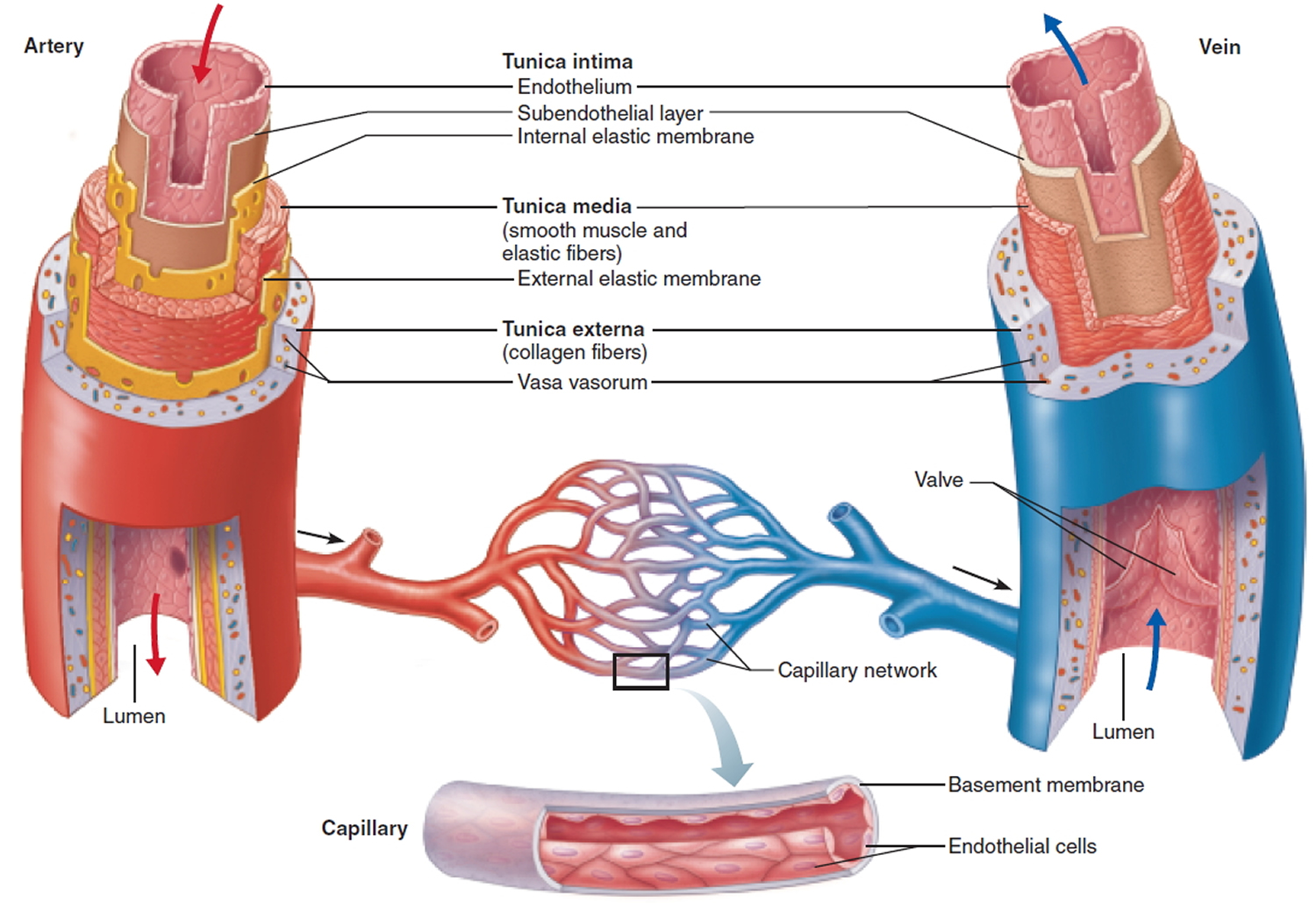
The aorta has three layers (see Figure 4):
- The inner layer (or intima)
- The middle layer (or media)
- The outer layer (or adventitia)
The aorta is composed of the intima, media, and adventitia. The intima, the innermost layer, is thin, delicate, lined by endothelium, and easily traumatized.
The media is responsible for imparting strength to the aorta and consists of laminated but intertwining sheets of elastic tissue. The arrangement of these sheets in a spiral provides the aorta with its maximum allowable tensile strength. The aortic media contains very little smooth muscle and collagen between the elastic layers and thus has increased distensibility, elasticity, and tensile strength. This contrasts with peripheral arteries, which, in comparison, have more smooth muscle and collagen between the elastic layers.
The outermost layer of the aorta is adventitia. This largely consists of collagen. The vasa vasorum, which supplies blood to the outer half of the aortic wall, lies within the adventitia. The nervi vascularis, bundles of nerve fibers found in the aortic adventitia, are involved in the production of pain, which occurs with acute stretching of the aortic wall from a dissection 6. The aorta does not have a serosal layer.
When a problem occurs with the aorta, the heart and the entire body’s blood supply can be jeopardized.
Figure 1. Aorta and its principal branches
Figure 2. Aorta and its principal branches
Figure 3. Normal heart blood flow
Figure 4. Layers of blood vessels
 Dissecting aortic aneurysm
Dissecting aortic aneurysm
When the inner lining of the aorta separates (tears) from the middle layer of the aorta, blood can push between these layers, separating (dissecting) the middle layer of the wall from the still intact outer layer. As a result, a new, false channel forms in the wall of the aorta. Virtually everyone who has an aortic dissection experiences pain—typically sudden, excruciating pain, often described as tearing or ripping. As the dissection advances further along the aorta, it can close off the points at which one or more arteries branch off from the aorta, blocking blood flow. The consequences vary depending on which arteries are blocked.
- Most aortic dissections occur because high blood pressure causes the artery’s wall to deteriorate.
- People have sudden, excruciating pain, most commonly across the chest but also in the back between the shoulder blades.
- Doctors usually do x-rays or computed tomography to confirm the diagnosis.
- People usually take drugs to decrease blood pressure, and doctors do surgery to repair the tear or place stent grafts to cover the tear.
Aortic dissections are 3 times more common among men and are more common among blacks (specifically African-Americans) and less common among Asians. About three fourths of aortic dissections occur in people aged 40 to 70.
Figure 5. Aortic dissection
The most common cause of aortic dissection is:
- Deterioration of the artery’s wall because of longstanding high blood pressure
More than two thirds of people who have an aortic dissection have high blood pressure.
Less common causes of aortic dissection include:
- Hereditary connective tissue disorders, especially Marfan syndrome and Ehlers-Danlos syndrome
- Birth defects of the heart and blood vessels, such as coarctation (narrowing) of the aorta, patent ductus arteriosus (a connection between the aorta and the pulmonary artery), and defects of the aortic valve
- Arteriosclerosis
- Injury such as a car crash or fall causing a strong blow to the chest
Rarely, a dissection occurs accidentally when doctors are inserting a catheter into an artery (for example, during aortography or angiography) or doing surgery on the heart or blood vessels.
Dissecting aortic aneurysm prognosis
Without treatment, about 80% of people who have an aortic dissection die within the first 2 weeks. With treatment, about 70% who have dissection of the first part of the aorta and about 90% of those who have dissection of the aorta farther from the heart survive to leave the hospital. About 60% of people who survive the first 2 weeks are still alive 5 years after treatment, and 40% live at least 10 years. Of people who die after the first 2 weeks, about one third die of complications of the dissection, and the other two thirds die of other disorders.
Dissecting aortic aneurysm complications
Complications include:
- Stroke (if the cerebral arteries, which supply the brain, are blocked),
- Heart attack (if the coronary arteries, which supply the heart muscle, are blocked),
- Kidney failure (if the renal arteries, which supply the kidneys, are blocked)
- Nerve and/or spinal cord damage that causes tingling or an inability to move a limb (if the spinal arteries are blocked).
Blood may leak from the dissection and accumulate in the chest. Blood leaking from a dissection near the heart may enter the pericardial space (between the two layers of membranes that surround the heart), preventing the heart from filling properly and causing cardiac tamponade—a life-threatening disorder.
A dissection that involves the first few inches of the aorta (ascending aorta) closest to the heart may affect the attachments of the aortic valve, the heart valve that keeps blood from flowing back into the heart. If the aortic valve attachments are weakened, the valve can leak, causing heart failure.
Dissecting aortic aneurysm symptoms
Virtually everyone who has an aortic dissection experiences pain—typically sudden, excruciating pain, often described as tearing or ripping. Some people may faint as a result of the pain. Most commonly, the pain is felt across the chest but is often also felt in the back between the shoulder blades. The pain frequently travels along the path of the dissection as it advances along the aorta. Thus, people may have abdominal pain or lower back pain if the mesenteric arteries, which supply the intestines, are blocked.
As the aortic dissection lengthens along the aorta, it can close off the points at which one or more arteries branch off from the aorta, blocking blood flow. The consequences vary depending on which arteries are blocked.
In most cases, the symptoms begin suddenly, and include severe chest pain. The pain may feel like a heart attack.
- Pain can be described as sharp, stabbing, tearing, or ripping.
- It is felt below the chest bone, and then moves under the shoulder blades or to the back.
- Pain can move to the shoulder, neck, arm, jaw, abdomen, or hips.
- The pain changes position, often moving to the arms and legs as the aortic dissection gets worse.
Symptoms are caused by a decrease of blood flowing to the rest of the body, and can include:
- Anxiety and a feeling of doom
- Fainting or dizziness
- Heavy sweating (clammy skin)
- Nausea and vomiting
- Pale skin (pallor)
- Rapid, weak pulse
- Shortness of breath and trouble breathing when lying flat (orthopnea)
Other symptoms may include:
- Pain in the abdomen
- Stroke symptoms
- Swallowing difficulties from pressure on the esophagus
Dissecting aortic aneurysm diagnosis
- Imaging tests such as CT scan, MRI, or ultrasonography
The distinctive symptoms of an aortic dissection usually make the diagnosis obvious to doctors, although the disorder causes a variety of symptoms that sometimes resemble those of other disorders. In about two thirds of people with aortic dissection, pulses in the arms and legs are diminished or absent. Depending on the location of the dissection along the aorta, there may be a difference in blood pressure between the right and left arm. A dissection that is moving backward toward the heart may cause a murmur that can be heard through a stethoscope.
Chest x-rays are the first step in detecting aortic dissection. X-rays show a widened aorta in 90% of people with symptoms. However, this finding may be due to other disorders. Computed tomography (CT) done after injecting a contrast agent (dye) can quickly and reliably detect aortic dissection and thus is useful in an emergency. Standard or transesophageal echocardiography or magnetic resonance angiography can also reliably detect aortic dissections, even very small ones.
Dissecting aortic aneurysm treatment
Surgery or sometimes an endovascular stent graft
People with an aortic dissection are admitted to an intensive care unit, where their vital signs (pulse, blood pressure, and rate of breathing) are closely monitored. Death can occur a few hours after an aortic dissection begins. Therefore, as soon as possible, drugs are given intravenously to reduce the heart rate and blood pressure to the lowest level that can maintain a sufficient blood supply to the brain, heart, and kidneys. The lower heart rate and blood pressure help limit the spread of the dissection. Soon after drug therapy begins, doctors must decide whether to recommend surgery or to continue drug therapy without surgery.
Doctors almost always recommend surgery for dissections that involve the first few inches of the aorta (ascending aorta) closest to the heart, unless complications of the dissection make the risk of surgery too high. During surgery, surgeons remove the largest possible area of dissected aorta, close the channel that was torn between the middle and outer layers of the aorta’s wall, and rebuild the aorta with a synthetic graft. If the aortic valve is leaking, surgeons repair or replace it. Removal and repair of a dissected aorta usually takes 3 to 6 hours, and the hospital stay is usually 7 to 10 days.
For dissections in the aorta farther from the heart (descending aorta), doctors usually continue drug therapy without surgery or consider placement of an endovascular stent-graft, To do an endovascular stent-graft, doctors thread a long, thin wire through the large artery in the groin (femoral artery) and up to the dissecting area. Then they slide the stent-graft, which is a hollow tube like a collapsible straw, over the wire and inside the damaged area of the aorta. Then the stent-graft is opened, forming a stable channel for blood flow . This procedure takes 2 to 4 hours, and the hospital stay is usually 1 to 3 days. Stent-grafts, which are less invasive than open surgery, have improved the survival rate and lowered the risk of complications for people with dissections of the descending aorta.
Surgery or a stent-graft repair is always necessary if the dissection causes the artery to leak blood, blocks the blood supply to the legs or to vital organs in the abdomen, causes symptoms, is enlarging, or occurs in a person with Marfan syndrome.
All people who have an aortic dissection, including those treated surgically, have to take drug therapy to keep their blood pressure down, usually for the rest of their lives. Such therapy helps reduce stress on the aorta. Drug therapy to lower blood pressure usually consists of a beta-blocker or calcium channel blocker plus another antihypertensive drug such as an angiotensin-converting enzyme (ACE) inhibitor. Cholesterol-lowering drugs and diet modification are used if the person has atherosclerosis.
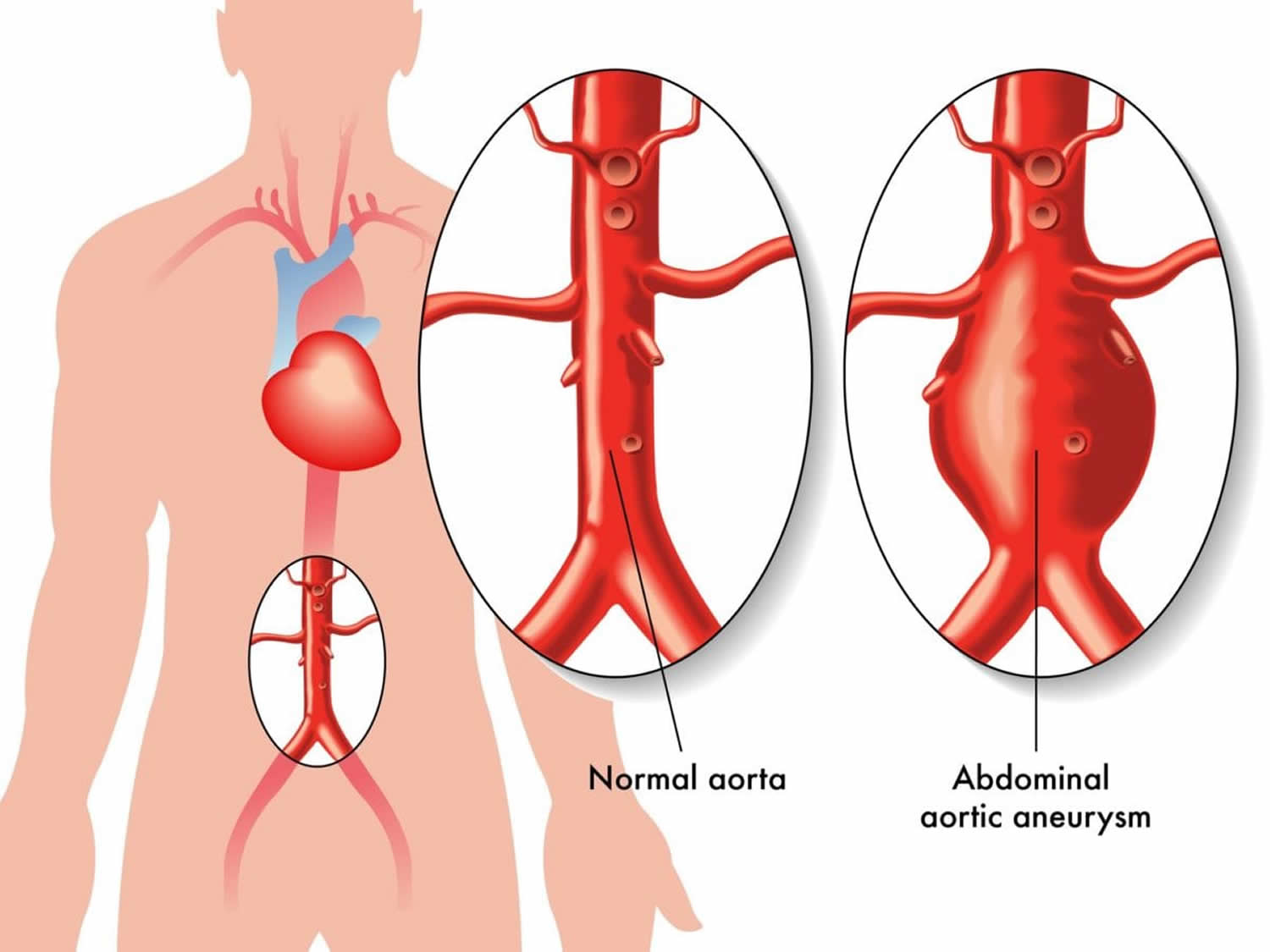
Doctors watch closely for complications that can occur in people who have had an aortic dissection. The most important are another dissection, development of aneurysms in the weakened aorta, and increasing leakage backward through the aortic valve. Any of these complications may require surgical repair.
Types of Aortic Aneurysms
The two types of aortic aneurysm are abdominal aortic aneurysm and thoracic aortic aneurysm. Some people have both types.
Abdominal Aortic Aneurysms
An aneurysm that occurs in the abdominal portion of the aorta is called an abdominal aortic aneurysm (AAA). Most aortic aneurysms are abdominal aortic aneurysms. Abdominal aortic aneurysms may occur at any age, but are most common in men between 50 and 80 years of age. Many people with an abdominal aortic aneurysm have no symptoms, but some people have a pulsing sensation in the abdomen and/or pain in the back 7. If the aneurysm ruptures, it may cause deep, severe pain; nausea; vomiting; fast heart rate; clammy skin; and/or shock 8. About 20% of abdominal aortic aneurysms eventually rupture and are often fatal 7. The condition has multiple genetic and environmental risk factors, and may sometimes occur as part of an inherited syndrome. When more than one family member is affected, it may be considered “familial abdominal aortic aneurysm” 9. Treatment depends on the size of the aneurysm and may include blood pressure medications, or surgery to repair the aneurysm 7.
Abdominal aortic aneurysms are found more often now than in the past because of computed tomography scans, or CT scans, done for other medical problems.
Small abdominal aortic aneurysms rarely rupture. However, abdominal aortic aneurysms can grow very large without causing symptoms. Routine checkups and treatment for an abdominal aortic aneurysm can help prevent growth and rupture.
Abdominal aortic aneurysm outlook (prognosis)
The outcome is often good if you have surgery to repair the aneurysm before it ruptures.
- When an abdominal aortic aneurysm begins to tear or ruptures, it is a medical emergency.
- Only about 1 in 5 people survive a ruptured abdominal aneurysm.
Figure 6. Abdominal aortic aneurysm
Causes of abdominal aortic aneurysms
The exact cause of an aneurysm is unknown. It occurs due to weakness in the wall of the artery. Factors that can increase your risk of having this problem include:
- Smoking
- High blood pressure
- Male gender
- Genetic factors
An abdominal aortic aneurysm is most often seen in males over age 60 who have one or more risk factors. The larger the aneurysm, the more likely it is to break open or tear. This can be life threatening.
Abdominal aortic aneurysm prevention
To reduce the risk of aneurysms:
- Eat a heart-healthy diet, exercise, stop smoking (if you smoke), and reduce stress.
- If you have high blood pressure or diabetes, take your medicines as your provider has told you.
People over age 65 who have ever smoked should have a screening ultrasound done once.
Abdominal aortic aneurysm symptoms
Aneurysms can develop slowly over many years, often with no symptoms. Symptoms may come on quickly if the aneurysm expands rapidly, tears open or leaks blood within the wall of the vessel (aortic dissection).
Symptoms of rupture include:
- Pain in the abdomen or back. The pain may be severe, sudden, persistent, or constant. It may spread to the groin, buttocks, or legs.
- Passing out.
- Clammy skin.
- Dizziness.
- Nausea and vomiting.
- Rapid heart rate.
- Shock.
Abdominal aortic aneurysm diagnosis
Your health care provider will examine your abdomen and feel the pulses in your legs. The provider may find:
- A lump (mass) in the abdomen
- Pulsating sensation in the abdomen
- Stiff or rigid abdomen
Your provider may find this problem by doing the following tests:
- Ultrasound of the abdomen when the abdominal aneurysm is first suspected
- CT scan of the abdomen to confirm the size of the aneurysm
- CTA (computed tomographic angiogram) to help with surgical planning
Any one of these tests may be done when you are having symptoms.
You may have an abdominal aortic aneurysm that is not causing any symptoms.
Your provider may order an ultrasound of the abdomen to screen for an aneurysm.
- Most men between the ages of 65 to 75, who have smoked during their life should have this test one time.
- Some men between the ages of 65 to 75, who have never smoked during their life may need this test one time.
Abdominal aortic aneurysm treatment
If you have bleeding inside your body from an aortic aneurysm, you will need surgery right away.
If the aneurysm is small and there are no symptoms:
- Surgery is rarely done.
- You and your provider must decide if the risk of having surgery is smaller than the risk of bleeding if you do not have surgery.
- Your provider may want to check the size of the aneurysm with ultrasound tests every 6 months.
Most of the time, surgery is done if the aneurysm is bigger than 2 inches (5 centimeters) across or growing quickly. The goal is to do surgery before complications develop.
There are two types of surgery:
- Open repair: A large cut is made in your abdomen. The abnormal vessel is replaced with a graft made of man-made material.
- Endovascular stent grafting: This procedure can be done without making a large cut in your abdomen, so you may recover more quickly. This may be a safer approach if you have certain other medical problems or are an older adult. Endovascular repair can sometimes be done for a leaking or bleeding aneurysm.
Thoracic Aortic Aneurysms
An aneurysm that occurs in the chest portion of the aorta (above the diaphragm, a muscle that helps you breathe) is called a thoracic aortic aneurysm.
Thoracic aortic aneurysms don’t always cause symptoms, even when they’re large. Only half of all people who have thoracic aortic aneurysms notice any symptoms. Thoracic aortic aneurysms are found more often now than in the past because of chest CT scans done for other medical problems.
With a common type of thoracic aortic aneurysm, the walls of the aorta weaken and a section close to the heart enlarges. As a result, the valve between the heart and the aorta can’t close properly. This allows blood to leak back into the heart.
A less common type of thoracic aortic aneurysm can develop in the upper back, away from the heart. A thoracic aortic aneurysm in this location may result from an injury to the chest, such as from a car crash.
Figure 7. Thoracic aortic aneurysm
Thoracic aortic aneurysm outlook (prognosis)
The long-term outlook for patients with thoracic aortic aneurysm depends on other medical problems, such as heart disease, high blood pressure, and diabetes, which may have caused or contributed to the condition.
Thoracic aortic aneurysm complications
Serious complications after aortic surgery can include:
- Bleeding
- Graft infection
- Heart attack
- Irregular heartbeat
- Kidney damage
- Paralysis
- Stroke
- Death soon after the operation occurs in 5 – 10% of patients.
- Complications after aneurysm stenting include damage to the blood vessels supplying the leg, which may require another operation.
Causes of thoracic aortic aneurysms
The most common cause of a thoracic aortic aneurysm is hardening of the arteries (atherosclerosis). This condition is more common in people with high cholesterol, long-term high blood pressure, or who smoke.
Other risk factors for a thoracic aneurysm include:
- Changes caused by age
- Connective tissue disorders such as Marfan syndrome
- Inflammation of the aorta
- Injury from falls or motor vehicle accidents
- Syphilis.
Thoracic aortic aneurysm prevention
To prevent atherosclerosis:
- Control your blood pressure and blood lipid levels.
- Do not smoke.
- Eat a healthy diet.
- Exercise regularly.
Thoracic aortic aneurysm symptoms
Aneurysms develop slowly over many years. Most patients have no symptoms until the aneurysm begins to leak or expand. The aneurysm may be found only when imaging tests are done for other reasons.
When they do occur, symptoms result from the pressure of the enlarging thoracic aorta against nearby organs, nerves, or muscles and thus depend on where the aneurysm develops.
Typical symptoms are pain (usually high in the back), coughing, and wheezing. Rarely, a person coughs up blood because of pressure on or erosion of the windpipe (trachea) or nearby airways. Swallowing may be difficult if an aneurysm puts pressure on the esophagus, which carries food to the stomach. Hoarseness may result from pressure on the nerve to the voice box (larynx).
Symptoms often begin suddenly when:
- The aneurysm grows quickly
- The aneurysm tears open (called a rupture)
- Blood leaks along the wall of the aorta (aortic dissection)
When a thoracic aortic aneurysm ruptures, excruciating pain usually begins high in the back. It may radiate down the back and into the abdomen as the rupture progresses. The pain may also be felt in the chest and arms, as it is during a heart attack. A person can quickly go into shock and die because of internal bleeding.
If the aneurysm presses on nearby structures, the following symptoms may occur:
- Hoarseness
- Swallowing problems
- High-pitched breathing (stridor)
- Swelling in the neck
A group of symptoms called Horner syndrome may result from pressure on certain nerves in the chest. Symptoms include a constricted pupil, drooping eyelid, and lack of sweating on one side of the face. Abnormal pulsations felt in the chest may indicate a thoracic aortic aneurysm. A windpipe that is farther to the side than usual may be seen on chest x-rays.
Other symptoms may include:
- Chest or upper back pain
- Clammy skin
- Nausea and vomiting
- Rapid heart rate
- Sense of impending doom
Thoracic aortic aneurysm diagnosis
The physical examination is often normal unless a rupture or leak has occurred.
Most thoracic aortic aneurysms are detected by tests performed for other reasons, usually a chest x-ray, echocardiogram, or a chest CT scan or MRI. A chest CT scan shows the size of the aorta and the exact location of the aneurysm.
An aortogram (a special set of x-ray images made when dye is injected into the aorta) can identify the aneurysm and any branches of the aorta that may be involved.
Thoracic aortic aneurysm treatment
There is a risk that the thoracic aortic aneurysm may open up (rupture) if you do not have surgery to repair it.
People are given regular CT scans every 6 to 12 months so doctors can monitor the aneurysm and determine whether it is expanding.
Patients are given a beta-blocker, calcium channel blocker, or another antihypertensive drug to reduce the rate at which the aneurysms grows and to reduce the risk that it might rupture. For people who smoke, quitting is very important.
It is much better to treat a thoracic aortic aneurysm before it ruptures, so once it becomes 2½ inches (5.5 to 6.0 centimeters) wide or larger, doctors will recommend repair. In people who have Marfan syndrome, a rupture is more likely, so doctors may recommend surgical repair even for smaller aneurysms.
The choice of aneurysm repair technique depends on many factors, including the person’s age and general health and the anatomy of their aorta and aneurysm. In general, stent-grafts are the first choice now for thoracic aortic aneurysms because they are much less invasive, avoiding an open chest incision that is more painful and that requires longer recovery. Open surgery is less commonly done and generally only necessary when a stent-graft does not fit the shape of the aorta.
An endovascular stent-graft is a hollow tube composed of fabric supported by a metal mesh that can be placed inside the aorta at the site of the aneurysm. To do an endovascular stent-graft, doctors thread a long, thin wire through the large artery in the groin (femoral artery) and up to the dissecting area, Then they slide the stent-graft over the wire and advance it to the site of the aneurysm within the aorta. Then they open the stent-graft inside the damaged part of the aorta to form a stable channel for blood flow. The stent is left in place permanently. This procedure takes 2 to 4 hours, and the hospital stay is usually 1 to 3 days. By contrast, after open surgery, the hospital stay is usually 5 to 8 days.
The risk of death is less than 4% during stent graft repair of thoracic aortic aneurysms but is about 30 to 50% during a stent graft repair or surgery for a ruptured thoracic aneurysm. Untreated ruptured thoracic aortic aneurysms are always fatal.
The treatment depends on the location of the aneurysm. The aorta is made of three parts:
- The first part moves upward towards the head. It is called the ascending aorta.
- The middle part is curved. It is called the aortic arch.
- The last part moves downward, toward the feet. It is called the descending aorta.
For patients with aneurysms of the ascending aorta or aortic arch:
- Surgery to replace the aorta is recommended if an aneurysm is larger than 5 – 6 centimeters.
- A cut is made in the middle of the chest bone.
- The aorta is replaced with a plastic or fabric graft.
- This is major surgery that requires a heart-lung machine.
For patients with aneurysms of the descending thoracic aorta:
- Majory surgery is done to replace the aorta with a fabric graft if the aneurysm is larger than 6 centimeters.
- This surgery is done through a cut on the left side of the chest, which may reach to the abdomen.
- Endovascular stenting is a less invasive option. A stent is a tiny metal or plastic tube that is used to hold an artery open. Stents can be placed into the body without cutting the chest. Not all patients with descending thoracic aneurysms are candidates for stenting, however.
Aortic aneurysm causes
The exact cause of an aneurysm is unknown. It occurs due to weakness in the wall of the artery.
The most common cause of aortic aneurysms is:
- Atherosclerosis, which weakens the wall of the aorta
Less common causes include:
- Injuries to the aorta, most often due to a motor vehicle crash
- Inflammatory diseases of the aorta (aortitis)
- Hereditary connective tissue disorders, such as Marfan syndrome
- Some infectious diseases, such as syphilis
Factors that can increase your risk of having this problem include:
- Smoking
- High blood pressure
- Male gender
- Genetic factors
In people with Marfan syndrome, an aneurysm is most likely to develop in the first part of the aorta, where it emerges from the heart (the ascending aorta). In older people, almost all aneurysms are associated with atherosclerosis. High blood pressure, which is common among older people, and cigarette smoking increase the risk of an aneurysm.
A blood clot (thrombus) often develops in the aneurysm because blood flow inside the aneurysm is sluggish. The clot may extend along the entire wall of the aneurysm. A blood clot may break loose (becoming an embolus), travel through the bloodstream, and block arteries. Aneurysms in the popliteal arteries are more likely to produce emboli than aneurysms in other arteries. Occasionally, calcium is gradually deposited in the wall of an aneurysm, making it easier to see on x-rays.
Aortic aneurysm symptoms
Some of the symptoms, such as chest pain and jaw pain, are generally associated with a heart attack, but the sudden stabbing, radiating pain, fainting, difficulty breathing, and sometimes even sudden weakness on one side are also symptoms of an aortic event. Because the aorta travels from above the heart to below the navel, severe pain may occur at any place along this major vessel. Additional accompanying symptoms of a rupture may include clammy skin, nausea and vomiting, or even shock.
Aneurysms and dissections of the aorta are life-threatening conditions and should be treated as a medical emergency.
Aortic aneurysm surgery
Different surgery treat the different kinds of aneurysms. Surgery to treat aortic aneurysms, those that occur in the body’s main artery, depends on the size and location of the aneurysm and your overall health. Aortic aneurysms in the upper chest (the ascending aorta) are usually operated on right away. Aneurysms in the lower chest and the area below your stomach (the descending thoracic and abdominal parts of the aorta) may not be as life threatening. Aneurysms in these locations are watched for varying periods, depending on their size. If they become about 5 centimeters (almost 2 inches) in diameter, continue to grow, or begin to cause symptoms, you may need surgery to repair the artery before the aneurysm bursts.
Aortic aneurysm repair
Surgery involves replacing the weakened section of the vessel with an artificial tube, called a graft. This means that surgeons will have to open either the stomach area (for abdominal aneurysms) or the chest (for thoracic aneurysms).
The cardiovascular surgeon leads the surgical team, which includes other assisting surgeons, an anesthesiologist, and surgical nurses. When the operation begins, the surgeon will make a cut (called an incision) either in the abdomen or the chest. The incision depends on where the aneurysm is located.
Surgeons will then place clamps on the artery above and below the aneurysm to stop blood flow to that part of the aorta. Your heart and brain still get blood because other vessels take over.
The bulging section of the aorta is cut out (excised). The surgeon will then replace the missing piece with a fabric tube called a graft. The clamps are then removed slowly to allow blood to flow through the vessel again.
Sometimes surgeons do not cut out the bulging section of the aorta. In these cases, the operation is the same except that surgeons place the fabric graft inside the vessel, like a lining, to decrease the pressure on the wall of the artery. This procedure is called endoaneurysmorrhaphy.
If the aneurysm is located in the ascending aorta just above the heart, the heart-lung machine will be used.
The surgery takes about 2 to 4 hours.
Recovery time
You can expect to stay in the hospital for 5 to 7 days, including at least 1 to 2 days in the Intensive Care Unit (ICU).
You will be given medicines called diuretics, which help to control any fluid buildup after surgery. You may also need to take aspirin for the first 6 weeks after surgery to stop any blood clots from forming.
Life after aneurysm surgery
After aneurysm surgery, your doctor will recommend that you join a cardiac rehabilitation program. These programs help you make lifestyle changes such as modifying your diet, exercising to get your strength back, quitting smoking, maintaining a healthy weight, and learning to deal with stress.
If you have an office job, you can go back to work in about 4 weeks. If you have a more physically demanding job, you may have to wait 6 to 8 weeks, or more.
Non-surgical repair of abdominal aortic aneurysms
This technique is useful for patients who cannot have surgery because their overall health would make it too dangerous.
The procedure uses a catheter to insert a device called a stent graft. The stent graft is placed within the artery at the site of the aneurysm. The stent graft acts as a barrier between the blood and the diseased wall of the artery. The blood flows through the stent graft, decreasing the pressure on the wall of the weakened artery. This decrease in pressure can prevent the aneurysm from growing or bursting.
Benefits of the procedure include no general anesthesia (you are awake for the procedure), a shorter hospital stay (about 24 hours), a faster recovery, and no large scars. Time and experience will prove whether this procedure will eliminate the long-term risk of an aneurysm’s bursting.
- Aneurysms. Medline Plus. https://medlineplus.gov/aneurysms.html[↩]
- Aneurysm. National Heart, Lung and Blood Institute. https://www.nhlbi.nih.gov/health/health-topics/topics/arm/[↩]
- Aortic Aneurysm Fact Sheet. https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_aortic_aneurysm.htm[↩]
- Centers for Disease Control and Prevention. Underlying Cause of Death 1999-2013 on CDC WONDER Online Database, released 2015. Data are from the Multiple Cause of Death Files, 1999-2013, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. https://wonder.cdc.gov/ucd-icd10.html[↩]
- Ramanath VS, Oh JK, Sundt TM, Eagle KA. Acute aortic syndromes and thoracic aortic aneurysm. Mayo Clin Proc. 2009;84(5):465–81.[↩]
- Spiegel EA, Wassreman S. Experimentalstudien uber die Entsehungdes Aortenschmerzes und seine Leitung zum zentralnervensystem. Ztschr F. d. ges. Exper Med. 1926. 52:180-196.[↩]
- John W. Hallett. Abdominal Aortic Aneurysms. Merck Manuals. http://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/aneurysms-and-aortic-dissection/introduction-to-aortic-aneurysms-and-aortic-dissection?qt=abdominal%20aortic%20aneurysm[↩][↩][↩]
- Weinrauch LA. Abdominal aortic aneurysm. MedlinePlus. https://medlineplus.gov/ency/article/000162.htm[↩]
- Ada Hamosh. AORTIC ANEURYSM, FAMILIAL ABDOMINAL, 1; AAA1. OMIM. http://omim.org/entry/100070[↩]