Contents
- What is aortic valve regurgitation
- Aortic valve regurgitation life expectancy
- Complications of aortic valve regurgitation
- Prevention of aortic valve regurgitation
- What are heart valves ?
- Causes of Aortic Valve Regurgitation
- Aortic valve regurgitation symptoms
- How is aortic valve regurgitation diagnosed?
- How is aortic valve regurgitation treated?
What is aortic valve regurgitation
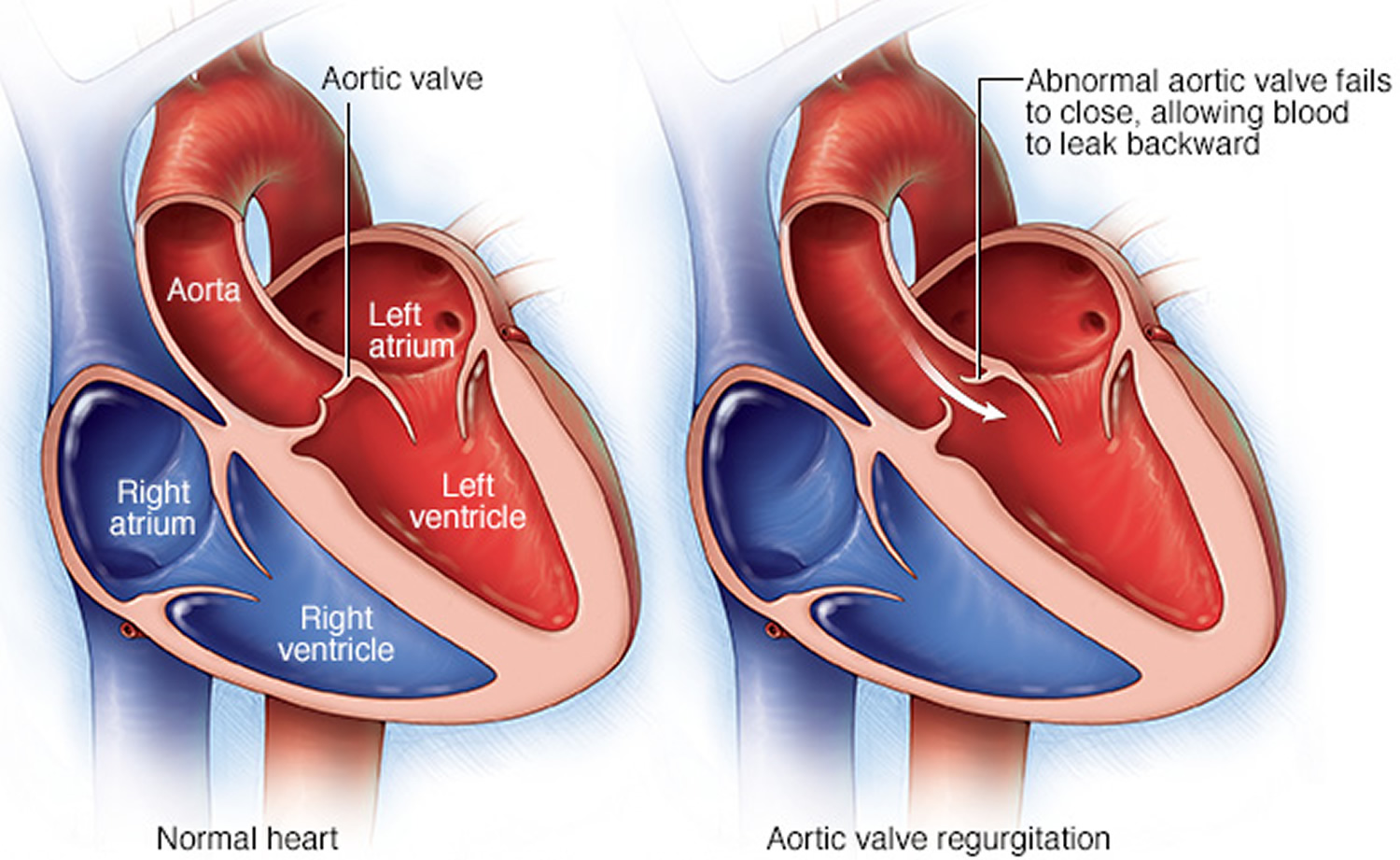
Aortic valve regurgitation is a condition that occurs when your heart’s aortic valve doesn’t close tightly. Aortic valve regurgitation allows some of the blood that was pumped out of your heart’s main pumping chamber (left ventricle) to leak back into it, because of an incompetent aortic valve which would normally stop this from happening.
The leakage may prevent your heart from efficiently pumping blood to the rest of your body. As a result, you may feel fatigued and short of breath.
The regurgitation of blood back into the left ventricle of the heart leads to dilatation of the ventricle. This reflects and attempt to maintain heart output by increasing the volume of blood being pumped out. This dilatation leads eventually leads to heart failure.
Left ventricular dilatation also decreases the amount of blood entering the heart causing angina and can also cause atrial fibrillation, infective endocarditis and mitral regurgitation. However, there are frequently no clinical symptoms until the onset of ventricular failure.
Aortic valve regurgitation can develop suddenly or over decades. Once aortic valve regurgitation becomes severe, surgery is often required to repair or replace the aortic valve.
Aortic valve regurgitation increases in incidence with increasing age and the vast majority of people over 80 years of age show evidence of regurgitation on testing with or without symptoms. Aortic valve regurgitation occurs more commonly in men, but the majority of patients with rheumatic aortic valve regurgitation are women.
Aortic valve regurgitation can have many causes, including diseases that affect connective tissue, which is the substance of the aortic valve and the ascending aorta. In most of these diseases, aortic valve regurgitation progresses gradually, allowing time for the left ventricle to accommodate the large diastolic volume by increasing its end-diastolic size and developing eccentric hypertrophy. A few diseases can cause sudden severe aortic valve regurgitation. In these diseases, the clinical picture of acute aortic valve regurgitation results from a sudden and marked increase in diastolic filling volume, with no chance for the left ventricle or the stiff pericardium to accommodate this increase.
Aortic valve regurgitation life expectancy
Compensation usually prevents the disease from becoming symptomatic for many years. As many as 85-95% of patients with mild-moderate regurgitation will live another 10 years. However after the onset of symptoms of heart failure, there is a fairly rapid deterioration within a couple of years.
Natural history of aortic valve regurgitation
The natural history of chronic aortic regurgitation is well recognized. The asymptomatic patient who has moderate to severe aortic regurgitation may not have symptoms for many years. In seven studies, 490 asymptomatic patients with moderate to severe aortic regurgitation were followed for a mean of 6.4 years 1, 2, 3, 4, 5, 6, 7. Based on these studies, the following can be concluded about asymptomatic chronic aortic regurgitation with normal left ventricular systolic function (i.e., an ejection fraction of 50 percent or greater) 8:
- The rate of progression to symptoms and/or left ventricular dysfunction is less than 6 percent per year.
- The rate of progression to asymptomatic left ventricular dysfunction is less than 3.5 percent per year.
- The rate of sudden death is less than 0.2 percent per year.
In patients with asymptomatic chronic aortic regurgitation and left ventricular dysfunction, the rate of progression to symptoms is higher than 25 percent per year. In symptomatic patients, the mortality rate is greater than 10 percent per year 8.
Although there is only a small chance of sudden death or left ventricular dysfunction in patients with asymptomatic chronic aortic regurgitation, these adverse events are possible. Therefore, it is important for asymptomatic patients to get regular check up with their cardiologists to detect for the progression of aortic valve regurgitation and identify severity and development of symptoms. In addition, periodic quantitative evaluation of left ventricular function is necessary in patients with moderate to severe aortic regurgitation. When the history of exercise tolerance or symptoms is equivocal, exercise stress testing can be helpful.
Preoperative Risk Assessment
Many investigators have studied factors that predict survival and recovery of left ventricular function after aortic valve replacement. In several studies 9, 10, the development of New York Heart Association 11 class III and IV symptoms, especially with an ejection fraction of less than 50 percent, was most predictive of increased mortality and decreased left ventricular myocardial function after aortic valve replacement. The duration of symptoms can also be important: the longer the patient has symptoms and the longer left ventricular dysfunction has been present before surgery, the worse the outcome 9, 12.
New York Heart Association Functional Classification
- Class I: No symptoms or minimal symptoms with ordinary physical activity
- Class II: Symptoms with ordinary activity; slight limitation of activity
- Class III: Symptoms with less than ordinary activity; marked limitation of activity
- Class IV: Symptoms with any physical activity, or even at rest
Complications of aortic valve regurgitation
Aortic valve regurgitation can cause complications, including:
- Heart failure
- Infections that affect the heart, such as endocarditis
- Heart rhythm abnormalities
- Death
Prevention of aortic valve regurgitation
For any heart condition, see your doctor regularly so he or she can monitor you and possibly catch aortic valve regurgitation or other heart condition before it develops or in the early stages, when it’s more easily treatable. If you have been diagnosed with a leaking aortic valve (aortic valve regurgitation) or a tight aortic valve (aortic valve stenosis), you’ll probably require regular echocardiograms to be sure the aortic valve regurgitation doesn’t become severe.
Also, be aware of conditions that contribute to developing aortic valve regurgitation, including:
- Rheumatic fever. If you have a severe sore throat, see a doctor. Untreated strep throat can lead to rheumatic fever. Fortunately, strep throat is easily treated with antibiotics.
- High blood pressure. Check your blood pressure regularly. Make sure it’s well-controlled to prevent aortic regurgitation.
What are heart valves ?
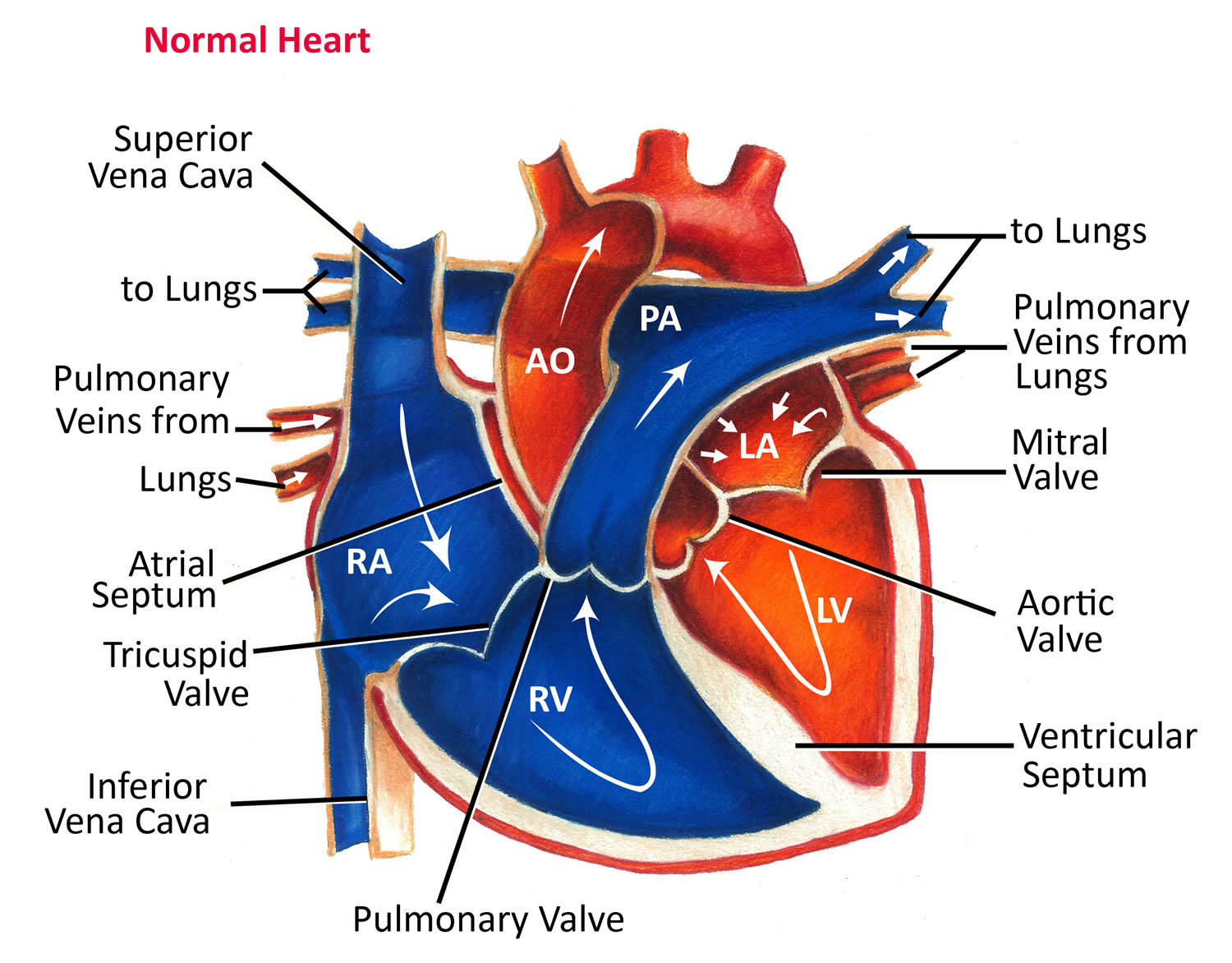
Your heart is a strong muscle about the size of the palm of your hand. Your body depends on the heart’s pumping action to deliver oxygen- and nutrient-rich blood to the body’s cells. When the cells are nourished properly, the body can function normally. Just like an engine makes a car go, the heart keeps your body running. The heart has two pumps separated by an inner wall called the septum. The right side of the heart pumps blood to the lungs to pick up oxygen. The left side of the heart receives the oxygen-rich blood from the lungs and pumps it to the body.
The heart has four chambers 13, two on the right and two on the left:
- Two upper chambers are called atrium (two is called an atria). The atria collect blood as it flows into the heart.
- Two lower chambers are called ventricles. The ventricles pump blood out of the heart to the lungs or other parts of the body.
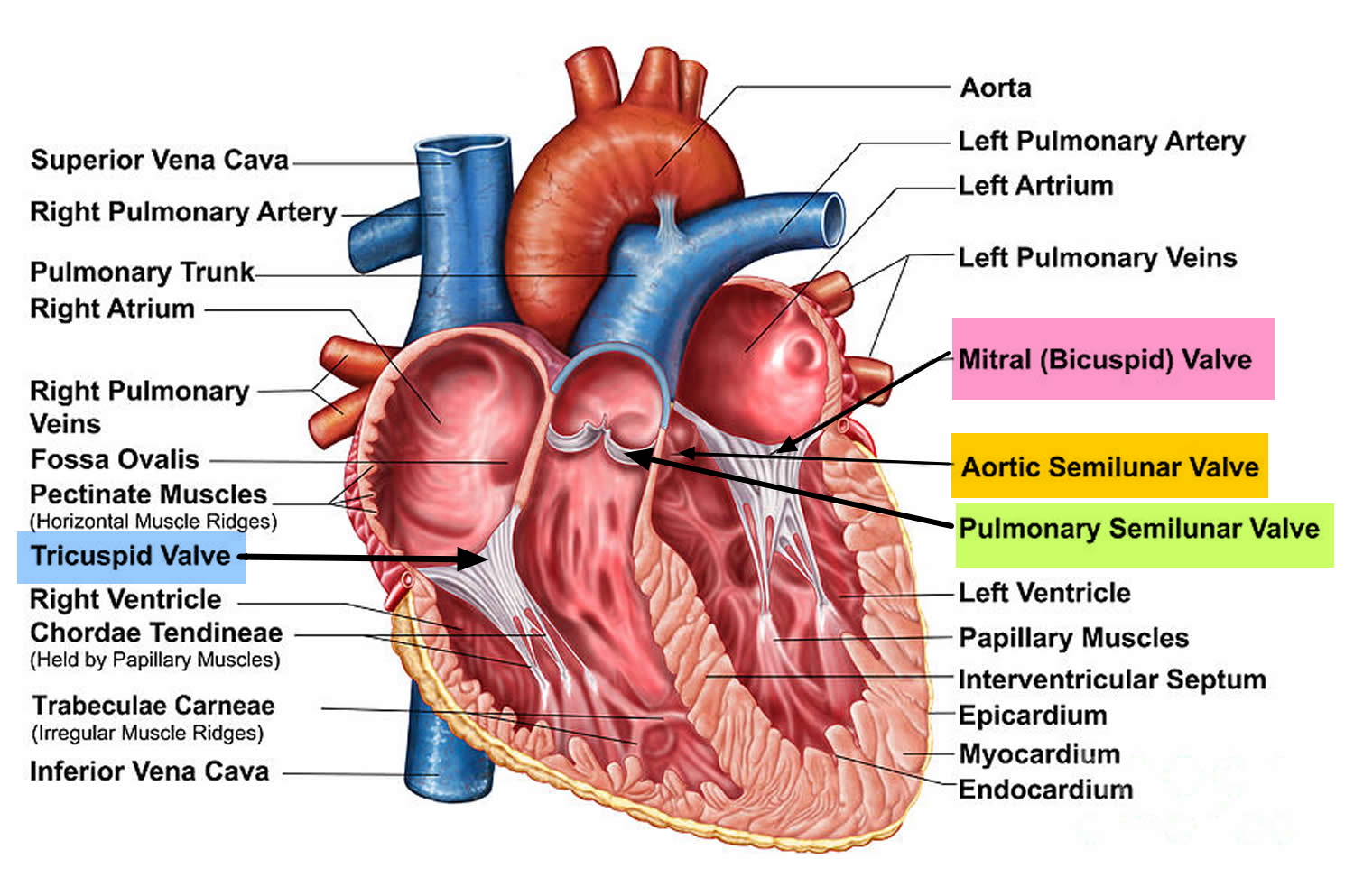
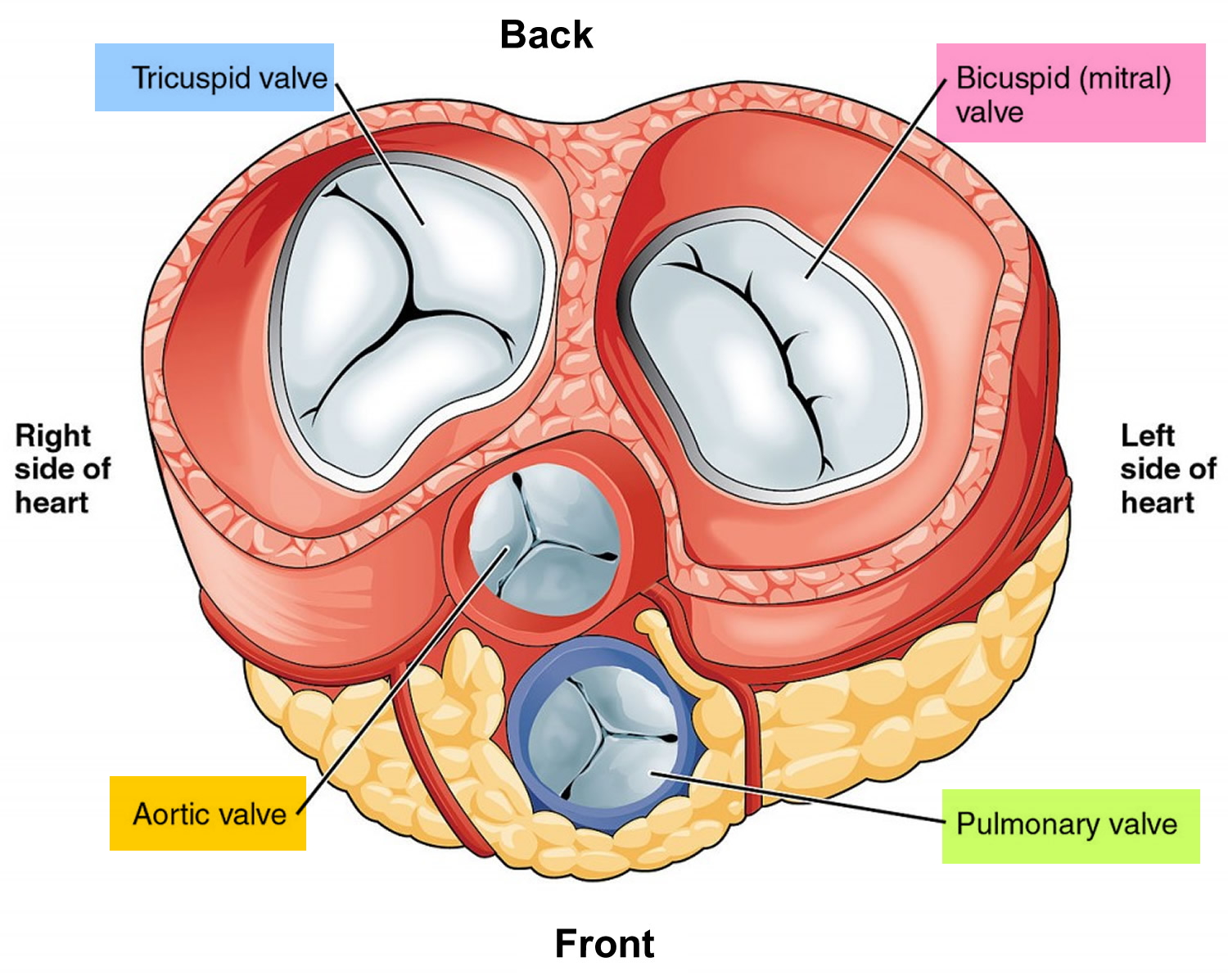
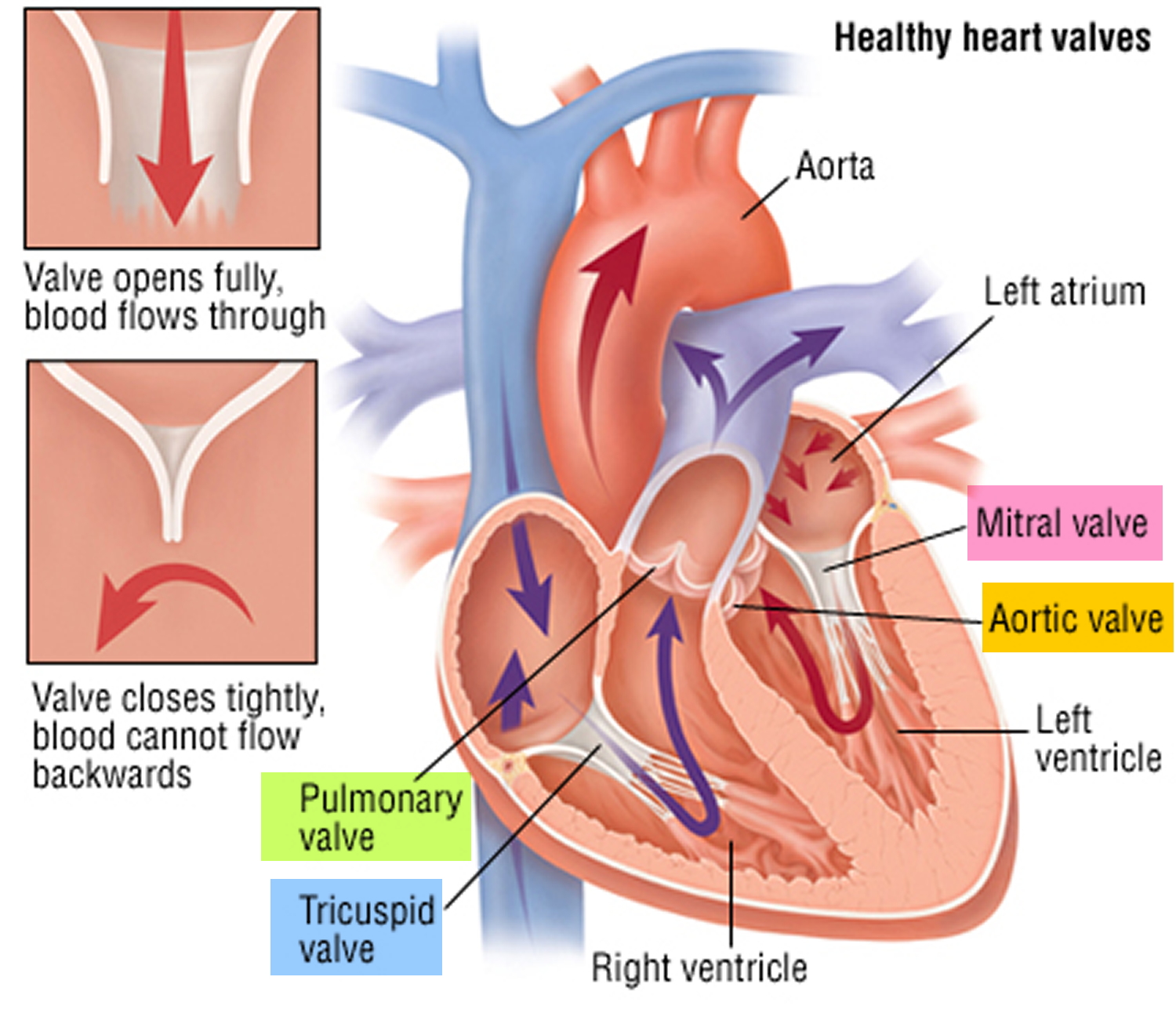
The heart also has four valves that open and close to let blood flow from the atria to the ventricles and from the ventricles into the two large arteries connected to the heart in only one direction when the heart contracts (beats). The four heart valves are:
- Tricuspid valve, located between the right atrium and right ventricle
- Pulmonary or pulmonic valve, between the right ventricle and the pulmonary artery. This artery carries blood from the heart to the lungs.
- Mitral valve, between the left atrium and left ventricle
- Aortic valve, between the left ventricle and the aorta. This aorta carries blood from the heart to the rest of the body.
Each valve has a set of flaps (also called leaflets or cusps). The mitral valve has two flaps; the others have three. Valves are like doors that open and close. They open to allow blood to flow through to the next chamber or to one of the arteries. Then they shut to keep blood from flowing backward. Blood flow occurs only when there’s a difference in pressure across the valves, which causes them to open. Under normal conditions, the valves permit blood to flow in only one direction.
The heart four chambers and four valves and is connected to various blood vessels. Veins are blood vessels that carry blood from the body to the heart. Arteries are blood vessels that carry blood away from the heart to the body.
The heart pumps blood to the lungs and to all the body’s tissues by a sequence of highly organized contractions of the four chambers. For the heart to function properly, the four chambers must beat in an organized way.
When the heart’s valves open and close, they make a “lub-DUB” sound that a doctor can hear using a stethoscope 14.
- The first sound—the “lub”—is made by the mitral and tricuspid valves closing at the beginning of systole. Systole is when the ventricles contract, or squeeze, and pump blood out of the heart.
- The second sound—the “DUB”—is made by the aortic and pulmonary valves closing at the beginning of diastole. Diastole is when the ventricles relax and fill with blood pumped into them by the atria.
Figure 1. The anatomy of the heart valves
Figure 2. Top view of the 4 heart valves
Figure 3. Normal heart blood flow
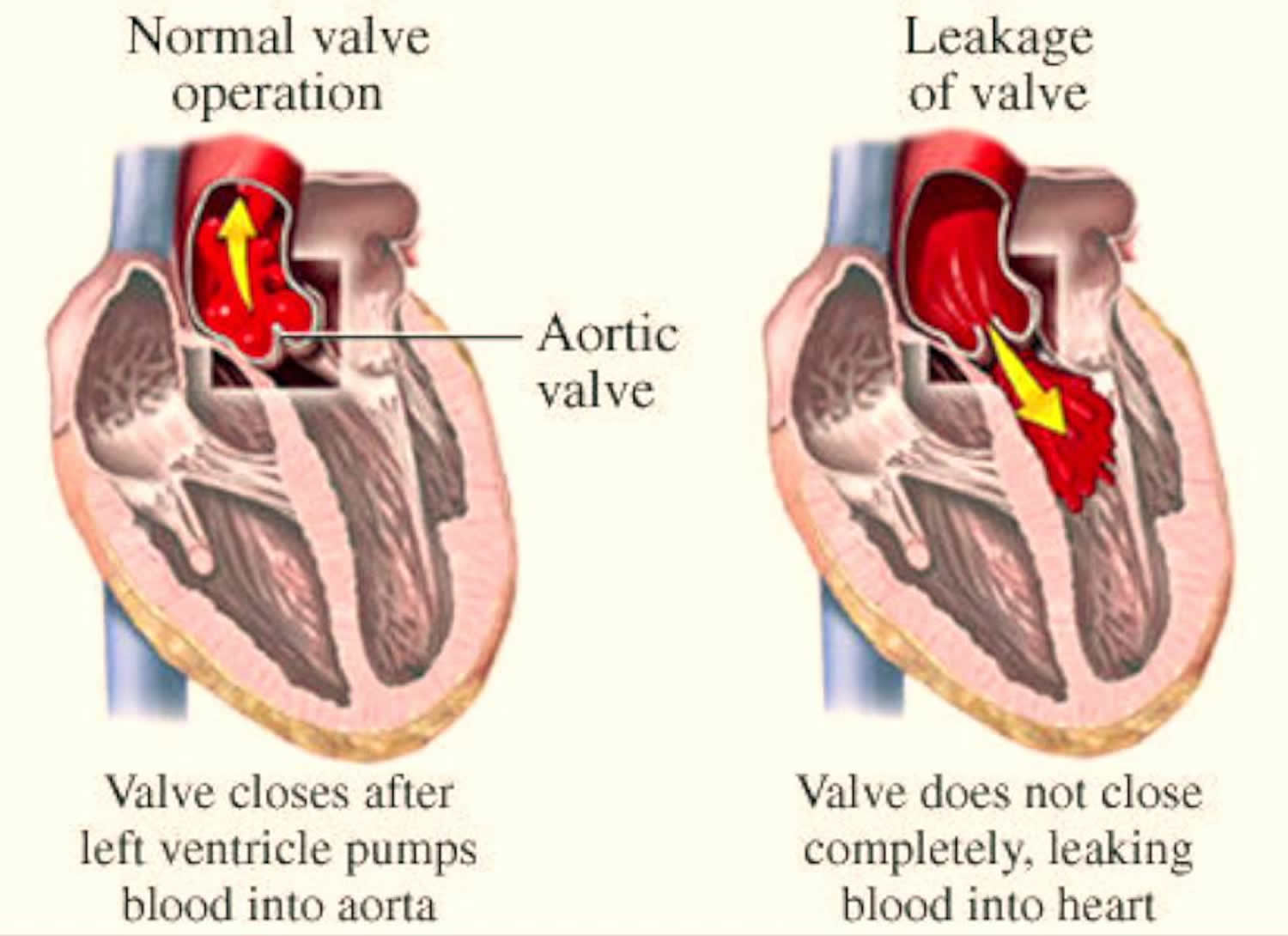
Figure 4. Heart valves function
Figure 5. Aortic valve regurgitation
Note: In aortic valve regurgitation, the aortic valve doesn’t close properly, causing blood to leak backward from the aorta into the left ventricle.
Causes of Aortic Valve Regurgitation
Any condition that damages a valve can cause regurgitation.
Causes of aortic valve regurgitation include:
- Congenital heart valve disease (e.g., bicuspid aortic valve, prolapsed aortic cusp with supracristal ventricular septal defect). You may have been born with an aortic valve that has only two cusps (bicuspid valve) or fused cusps rather than the normal three separate cusps. In some cases a valve may only have one cusp (unicuspid) or four cusps (quadricuspid), but this is less common. These congenital heart defects put you at risk of developing aortic valve regurgitation at some time in your life. If you have a parent or sibling with a bicuspid valve, it increases the risk that you may have a bicuspid valve, but it can also occur if you don’t have a family history of a bicuspid aortic valve.
- Age-related changes to the heart. Calcium deposits can build up on the aortic valve over time, causing the aortic valve’s cusps to stiffen. This can cause the aortic valve to become narrow, and it may also not close properly.
- Endocarditis. The aortic valve may be damaged by endocarditis — an infection inside your heart that involves heart valves.
- Rheumatic fever. Rheumatic heart disease — a complication of strep throat and once a common childhood illness in the United States — can damage the aortic valve. Rheumatic fever is still prevalent in developing countries but rare in the United States. Some older adults in the United States were exposed to rheumatic fever as children, although they may not have developed rheumatic heart disease.
- Connective tissue disease (e.g., Marfan syndrome, Turner’s syndrome, pseudoxanthoma elasticum, ankylosing spondylitis, Ehlers-Danlos syndrome, polymyalgia rheumatica)
- Collagen vascular diseases. Some autoimmune conditions, such as systemic lupus erythematosus, also can lead to aortic valve regurgitation.
- Ascending aortic aneurysm
- Aortitis (e.g., syphilis, Takayasu’s arteritis, granulomatous aortitis)
- Myxomatous aortic valve*
- Calcific changes in aortic valve (together with aortic stenosis)
- Anorectic drugs
- Infective endocarditis*
- Aortic dissection*
- Trauma*. Damage to the aorta near the site of the aortic valve, such as damage from injury to your chest or from a tear in the aorta, also can cause backward flow of blood through the valve.
*— Associated with clinically acute aortic regurgitation.
Risk Factors for aortic valve regurgitation
The major predisposing factors are:
- Rheumatic heart disease, syphilis;
- Damage to the cusps of the valve secondary to infective endocarditis;
- Any primary cause of aortic stenosis (progressive narrowing of the aortic valve) can lead to aortic valve regurgitation when the valve cusps become fixed and can not close adequately any longer.
- Older age
- Certain heart conditions present at birth (congenital heart disease)
- History of infections that can affect the heart
- Other heart valve conditions, such as aortic valve stenosis
- High blood pressure
Rarer associations include:
- Ankylosing spondilitis;
- Aortic cusp fenestration;
- Marfan’s syndrome;
- Systemic lupus erythematosis; and
- Aortitis.
Aortic valve regurgitation symptoms
Most often, aortic valve regurgitation develops gradually, and your heart compensates for the problem. You may have no signs or symptoms for years, and you may even be unaware that you have the condition.
However, as aortic valve regurgitation worsens, signs and symptoms may include:
- Fatigue and weakness, especially when you increase your activity level
- Shortness of breath with exercise or when you lie down
- Swollen ankles and feet
- Chest pain (angina), discomfort or tightness, often increasing during exercise
- Lightheadedness or fainting
- Irregular pulse (arrhythmia)
- Heart murmur
- Sensations of a rapid, fluttering heartbeat (palpitations).
How is aortic valve regurgitation diagnosed?
The diagnosis of aortic valve regurgitation is made with the stethoscope and is based on the finding of a “decrescendo” blowing diastolic murmur, which is best heard along the left sternal border.
The presence and severity of aortic regurgitation can usually be determined based on the physical examination alone. However, Doppler echocardiography should be performed to confirm the presence of the regurgitation, quantify its severity and look for other cardiac problems (e.g., valvular vegetations, ventricular septal defect or aortic root aneurysm) that may be important in guiding therapy.
Your doctor may order several tests to diagnose your condition, and determine the cause and severity of your condition.
Tests may include:
- Electrocardiogram (ECG): In this test, wires (electrodes) attached to pads on your skin measure the electrical activity of your heart. An ECG can detect enlarged chambers of your heart, heart disease and abnormal heart rhythms. May detect ventricular ischemia. Also associated myocardial infarction and atrial fibrillation.
- Chest x-ray: This enables your doctor to determine whether your heart is enlarged — a possible indicator of aortic valve regurgitation — or whether you have an enlarged aorta. It can also help doctors determine the condition of your lungs. Chest x-ray may show calcification of the aortic valve. In late disease, pulmonary edema may be seen.
- Doppler echocardiography would show a regurgitant aortic jet in a small percentage of the general population. The leak is so small in volume that a murmur is not heard. It is presumed that this degree of aortic regurgitation is normal and does not represent disease. If no murmur or peripheral signs of aortic regurgitation are present, a diagnosis of aortic regurgitation should not be made, and no follow-up echocardiography is needed. If the aortic regurgitation is mild, the murmur may be quite high-pitched and may fade out during diastole. If the aortic regurgitation is moderate to severe and chronic, the murmur, although still blowing, is of lower frequency and louder, and usually lasts throughout diastole. Because of the large left ventricular stroke volume, a systolic ejection murmur may also be heard. This murmur can be loud and long enough to sound like aortic stenosis. When both diastolic and systolic murmurs are heard, the decision as to which lesion (aortic stenosis or regurgitation) is significant is based on the presence of peripheral signs. If the patient has peripheral signs of aortic regurgitation, no matter how loud the systolic murmur or how soft the diastolic murmur, significant aortic regurgitation should be presumed.
- Exercise tests or stress tests. Exercise tests help doctors see whether you have signs and symptoms of aortic valve disease during physical activity, and these tests can help determine the severity of your condition. If you are unable to exercise, medications that have similar effects as exercise on your heart may be used.
- Cardiac MRI. Using a magnetic field and radio waves, this test produces detailed pictures of your heart, including the aorta and aortic valve. This test may be used to determine the severity of your condition.
- Cardiac catheterization. This test isn’t often used to diagnose aortic valve regurgitation, but it may be used if other tests aren’t able to diagnose the condition or determine its severity. Doctors may also conduct cardiac catheterization prior to valve replacement surgery to see if there are obstructions in the coronary arteries, so they can be fixed at the time of the valve surgery.In cardiac catheterization, a doctor threads a thin tube (catheter) through a blood vessel in your arm or groin to an artery in your heart and injects dye through the catheter to make the artery visible on an X-ray. This provides your doctor with a detailed picture of your heart arteries and how your heart functions. It can also measure the pressure inside the heart chambers.
How is aortic valve regurgitation treated?
Treatment of aortic valve regurgitation depends on the severity of your condition, whether you’re experiencing signs and symptoms, and if your condition is getting worse.
Treatment also include treating the underlying causes- such as syphilis and infective endocarditis. Antibiotic prophylaxis against development of infective endocarditis should also be used.
If your symptoms are mild or you aren’t experiencing symptoms, your doctor may monitor your condition with regular follow-up appointments. Your doctor may recommend that you make healthy lifestyle changes and take medications to treat symptoms or reduce the risk of complications.
You may eventually need surgery to repair or replace the diseased aortic valve. In some cases, your doctor may recommend surgery even if you aren’t experiencing symptoms. If you’re having another heart surgery, doctors may perform aortic valve surgery at the same time. In some cases, you may need a section of the aorta (aortic root) repaired or replaced at the same time as aortic valve surgery if the aorta is enlarged.
If you have aortic valve regurgitation, consider being evaluated and treated at a medical center with a multidisciplinary team of cardiologists and other doctors and medical staff trained and experienced in evaluating and treating heart valve disease. This team can work closely with you to determine the most appropriate treatment for your condition.
In chronic aortic valve regurgitation, valvular surgery is needed when the regurgitant volume becomes moderate to severe. However, certain causes may dictate surgery even if the degree of regurgitation is mild. For instance, the patient with aortic regurgitation resulting from dissection of the ascending aorta requires immediate surgery to repair the dissection. The patient with a prosthetic aortic valve who presents with infective endocarditis and an extensive annular abscess should undergo surgery before massive dehiscence occurs. Finally, the patient with a large ascending aortic aneurysm and minimal aortic regurgitation must have surgery because of the aneurysm.
Surgery to repair or replace an aortic valve is usually performed through a cut (incision) in the chest. In some cases, doctors may perform minimally invasive heart surgery, which involves the use of smaller incisions than those used in open-heart surgery.
Medical Management of the Patient with Chronic Aortic Regurgitation
- Follow the patient with a careful history for exercise capacity and symptoms, and perform physical examinations at regular intervals.
- If the patient has physical signs of moderate to severe aortic regurgitation, perform Doppler echocardiography.
- If the patient has moderate to severe aortic regurgitation and echocardiographic evidence of increased size of the left ventricle, start vasodilator therapy using nifedipine (Procardia), an angiotensin-converting enzyme inhibitor or hydralazine (Apresoline).
- If the patient’s exercise capacity cannot be evaluated accurately based on the history, perform exercise stress (treadmill) testing.
- If the patient develops symptoms of decreasing exercise tolerance, angina, syncope or heart failure, repeat Doppler echocardiography and consider aortic valve replacement.
- If the patient remains asymptomatic with physical signs of moderate to severe aortic regurgitation, consider yearly Doppler echocardiography to follow the left ventricular end-diastolic and end-systolic size and the ejection fraction.
- If the patient is asymptomatic and has a progressive decline in left ventricular end-diastolic and end-systolic size and a fall in the ejection fraction, consider aortic valve replacement.
Aortic valve regurgitation surgery
Surgical replacement of the valve should be undertaken but timing of the operation is important. Because a significantly enlarged heart will not recover completely, the operation should take place before the development of severe disease. Any heart failure should be treated with drug regimes.
The goal of heart valve surgery is to cure the problem or lengthen life by restoring the function of your heart valves, whether they are diseased or damaged.
Repair or Replace?
When possible, it’s generally best to repair a valve and preserve a person’s own tissue in the heart. However, when the tissue is too damaged, a replacement valve may be used from another human heart, an animal or a manufactured mechanical valve.
Aortic valve repair
To repair an aortic valve, surgeons may conduct several different types of repair, including separating valve flaps (cusps) that have fused, reshaping or removing excess valve tissue so that the cusps can close tightly, or patching holes in a valve.
Doctors may use a catheter procedure to insert a plug or device to repair a leaking replacement aortic valve.
Balloon Valvuloplasty – Repair Procedure
For many, valve tightness can be relieved during a procedure called balloon valvuloplasty. It is done as part of a cardiac catheterization, which is less invasive than general surgery or open heart surgery.
In a balloon valvuloplasty, a small catheter holding an expandable balloon is threaded into the heart and placed into the tightened valve. Next, the balloon is expanded to stretch open the valve and separate the leaflets.
In some cases the valve cannot be successfully treated by balloon valvuloplasty, and a different surgical treatment is needed to open the valve and allow better blood flow.
Treatment results can vary depending on the experience and training of your medical care team; hospitals can become very proficient at managing care around certain conditions, too. When a valve problem is complex, it is very important to choose an experienced team to do the repair.
Aortic valve replacement
Aortic valve replacement is often needed to treat aortic valve regurgitation. In aortic valve replacement, your surgeon removes the damaged valve and replaces it with a mechanical valve or a valve made from cow, pig or human heart tissue (biological tissue valve). Another type of biological tissue valve replacement that uses your own pulmonary valve is sometimes possible.
Biological tissue valves degenerate over time and may eventually need to be replaced. People with mechanical valves will need to take blood-thinning medications for life to prevent blood clots. Your doctor will discuss with you the benefits and risks of each type of valve and discuss which valve may be appropriate for you.
Doctors may also conduct a catheter procedure to insert a replacement valve into a failing biological tissue valve that is no longer working properly. Other procedures using catheters to repair or replace aortic valves to treat aortic valve regurgitation continue to be researched.
Surgical options for aortic valve replacement include:
- Mechanical valve — a long-lasting valve made of durable materials
- Tissue valve (which may include human or animal donor tissue)
- Ross Procedure — “Borrowing” your healthy valve and moving it into the position of the damaged valve aortic valve
- TAVI/TAVR procedure — Transcatheter aortic valve replacement
- Newer surgery options
The procedure chosen will depend on the valve that needs replacement, the severity of symptoms and the risk of surgery. Some procedures may require long-term medication to guard against blood clots.
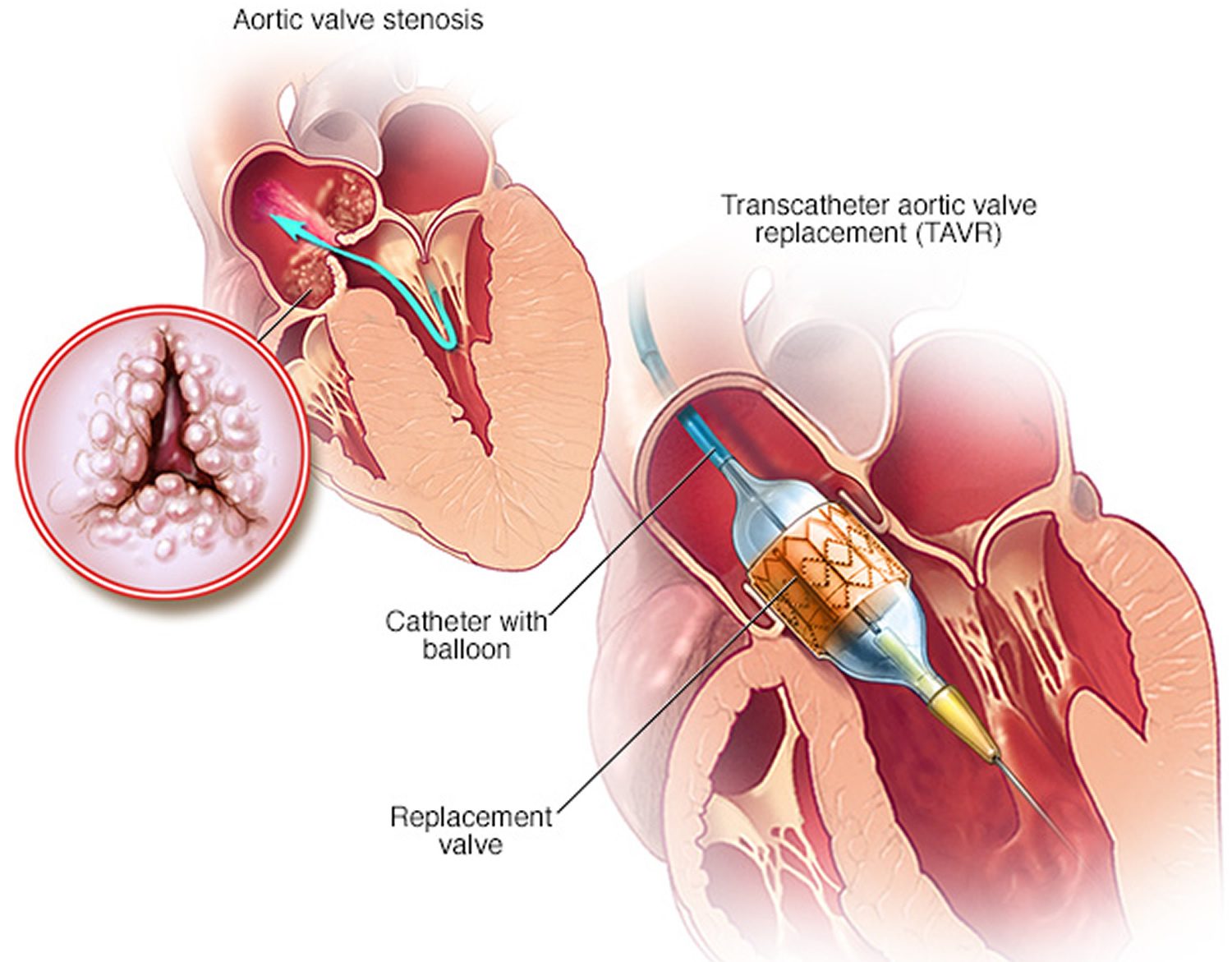
What is a TAVR?
This minimally invasive surgical procedure repairs the valve without removing the old, damaged valve. Instead, it wedges a replacement valve into the aortic valve’s place. The surgery may be called a transcatheter aortic valve replacement (TAVR) or transcatheter aortic valve implantation (TAVI).
Somewhat similar to a stent placed in an artery, the transcatheter aortic valve replacement (TAVR) approach delivers a fully collapsible replacement valve to the valve site through a catheter.
Once the new valve is expanded, it pushes the old valve leaflets out of the way and the tissue in the replacement valve takes over the job of regulating blood flow.
Figure 6. Transcatheter aortic valve replacement (TAVR)
How is TAVR or TAVI different from the standard valve replacement?
This procedure is fairly new and is FDA approved for people with symptomatic aortic stenosis who are considered an intermediate or high risk patient for standard valve replacement surgery. The differences in the two procedures are significant.
What is involved in a TAVR procedure?
Usually valve replacement requires an open heart procedure with a “sternotomy.”, in which the chest is surgically separated (open) for the procedure. The transcatheter aortic valve replacement (TAVR) or transcatheter aortic valve implantation (TAVI) procedures can be done through very small openings that leave all the chest bones in place.
A TAVR procedure is not without risks, but it provides beneficial treatment options to people who may not have been candidates for them a few years ago while also providing the added bonus of a faster recovery in most cases. A patient’s experience with a TAVR procedure may be comparable to a balloon treatment or even an angiogram in terms of down time and recovery, and will likely require a shorter hospital stay (average 3-5 days).
The TAVR procedure is performed using one of two different approaches, allowing the cardiologist or surgeon to choose which one provides the best and safest way to access the valve:
- Entering through the femoral artery (large artery in the groin), called the transfemoral approach, which does not require a surgical incision in the chest
or - Using a minimally invasive surgical approach with a small incision in the chest and entering through a large artery in the chest or through the tip of the left ventricle (the apex), which is known as the transapical approach.
Who is a good candidate for this type of valve surgery?
At this time the procedure is reserved for those people for whom an open heart procedure poses intermediate risk. For that reason, most people who have this procedure are in their 70s or 80 and often have other medical conditions that make them a better candidate for this type of surgery.
TAVR can be an effective option to improve quality of life in patients who otherwise have limited choices for repair of their aortic valve.
Aortic valve regurgitation exercise
Physical exercise has many benefits and should be a regular part of almost anyone’s life. That includes most people with congenital heart disease. Research on patients with congenital heart disease, even complex disease, has shown that routine moderate exercise is safe and can be beneficial. That’s why we recommend that almost all patients do some form of regular physical activity.
- There are a few exceptions, so it’s good to talk to your physician about your specific situation 15.
Most physicians will advise caution to a patient with an enlarged aorta, which is the major artery in the body. An enlarged aorta can occur in people with Marfan syndrome, Turner syndrome, coarctation of the aorta, or a bicuspid aortic valve. There is no proven link between exercise and harmful outcome from an enlarged aorta, but many physicians feel that such patients shouldn’t engage in strenuous exercise, particularly activity that involves straining or grunting like heavy weight lifting.
- It’s likely that for most patients, the benefits of exercise outweigh the perceived risks. Low-intensity activity is still preferred. If you have any questions about the appropriateness of exercise for you, talk to your doctor.
If you’ve been inactive for a long time and want to start a regular exercise routine, it’s often wise to talk with your doctor about how to get started safely. Your doctor may recommend an exercise test which can provide you with guidelines for exercise.
What types and how much?
The best and safest types of exercise are “aerobic” activities. These increase the heart rate and make you breath heavily. Examples include brisk walking, swimming, biking, jogging, rowing, cross-country skiing, hiking or stair climbing. Team or court sports such as basketball, soccer, football, tennis, squash and volleyball are also aerobic activities.
A good rule of thumb is to increase your activity so you breathe hard and fast but can still carry on a conversation with someone. If you can speak in full sentences but still feel your heart pounding, you’re likely benefiting from a safe level of activity.
Often patients are trained to check their heart rate during or immediately after activity. Their target heart rate is 70-80 percent of their predicted maximal heart rate (defined as 220 minus age).
It’s best to avoid activities that cause grunting or straining (medically referred to as a “valsalva maneuver”). This happens when a person bears down against a closed throat to increase the strength of arm or abdominal muscles. There’s often a tendency to do this when lifting heavy weights, doing sit-ups, push-ups or chin-ups, etc., but it may be harmful. Straining causes a sudden rise in blood pressure, which adds strain on the heart; it increases the pressure in the lungs, which can affect blood flow from the body into the lungs; and it often means there’s more force on the chest wall, and many congenital heart patients have surgical scars in the chest that can be damaged, particularly in the first year after surgery.
- Intensely physical sports such as football, boxing or hockey may increase the chance for injury and unnecessary strain on the cardiovascular system.
Any amount of activity is better than none, and the more physically active a person is, the greater the anticipated cardiovascular benefit. Guidelines for the general population suggest at least 30 minutes of dedicated aerobic activity a day for five or more days a week. This is a good target for congenital heart patients too. If it seems like too much, start with a more modest goal and build from there.
Lifestyle and home remedies
You’ll have regular follow-up appointments with your doctor to monitor your condition.
While lifestyle changes can’t prevent or treat your condition, your doctor might suggest that you incorporate several heart-healthy lifestyle changes into your life. These may include:
- Eating a heart-healthy diet. Eat a variety of fruits and vegetables, low-fat or fat-free dairy products, poultry, fish, and whole grains. Avoid saturated and trans fat, and excess salt and sugar.
- Maintaining a healthy weight. Aim to keep a healthy weight. If you’re overweight or obese, your doctor may recommend that you lose weight.
- Getting regular physical activity. Aim to include about 30 minutes of physical activity, such as brisk walks, into your daily fitness routine. Ask your doctor for guidance before starting to exercise, especially if you’re considering competitive sports.
- Managing stress. Find ways to help manage your stress, such as through relaxation activities, meditation, physical activity, and spending time with family and friends.
- Avoiding tobacco. If you smoke, quit. Ask your doctor about resources to help you quit smoking. Joining a support group may be helpful.
- Controlling high blood pressure. If you’re taking blood pressure medication, ensure you take it as your doctor has prescribed.
For women with aortic valve regurgitation, it’s important to talk with your doctor before you become pregnant. Your doctor can discuss with you which medications you can safely take, and whether you may need a procedure to treat your valve condition prior to pregnancy.
You’ll likely require close monitoring by your doctor during pregnancy. Doctors may recommend that women with severe valve conditions avoid pregnancy to avoid the risk of complications.
- Bonow RO, Lakatos E, Maron BJ, Epstein SE. Serial long-term assessment of the natural history of asymptomatic patients with chronic aortic regurgitation and normal left ventricular systolic function. Circulation. 1991;84:1625–35.[↩]
- Scognamiglio R, Fasoli G, Dalla Volta S. Progression of myocardial dysfunction in asymptomatic patients with severe aortic insufficiency. Clin Cardiol. 1986;9:151–6.[↩]
- Siemienczuk D, Greenberg B, Morris C, Massie B, Wilson RA, Topic N, et al. Chronic aortic insufficiency: factors associated with progression to aortic valve replacement. Ann Intern Med. 1989;110:587–92.[↩]
- Tornos MP, Olona M, Permanyer-Miralda G, Herrejon MP, Cam-precios M, Evangelista A, et al. Clinical outcome of severe asymptomatic chronic aortic regurgitation: a long-term prospective follow-up study. Am Heart J. 1995;130:333–9.[↩]
- Ishii K, Hirota Y, Suwa M, Kita Y, Onaka H, Kawamura K. Natural history and left ventricular response in chronic aortic regurgitation. Am J Cardiol. 1996;78:357–61.[↩]
- Scognamiglio R, Rahimtoola SH, Fasoli G, Nistri S, Dalla Volta S. Nifedipine in asymptomatic patients with severe aortic regurgitation and normal left ventricular function. N Engl J Med. 1994;331:689–94.[↩]
- Borer JS, Hochreiter C, Herrold EM, Supino P, Aschermann M, Wencker D, et al. Prediction of indications for valve replacement among asymptomatic or minimally symptomatic patients with chronic aortic regurgitation and normal left ventricular performance. Circulation. 1998;97:525–34.[↩]
- Bonow RO, Carabello B, de Leon AC Jr, Edmunds LH Jr, Fedderly BJ, Freed MD, et al. Guidelines for the management of patients with valvular heart disease: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients with Valvular Heart Disease). Circulation. 1998;88:1949–84.[↩][↩]
- Michel PL, Iung B, Abou Jaoude S, Cormier B, Porte JM, Vahanian A, et al. The effect of left ventricular systolic function on long term survival in mitral and aortic regurgitation. J Heart Valve Dis. 1995;4(suppl 2):S160–8.[↩][↩]
- Klodas E, Enriquez-Sarano M, Tajik AJ, Mullany CJ, Bailey KR, Seward JB. Optimizing timing of surgical correction in patients with severe aortic regurgitation: role of symptoms. J Am Coll Cardiol. 1997;30:746–52.[↩]
- Criteria Committee of the New York Heart Association. Diseases of the heart and blood vessels, nomenclature and criteria for diagnosis. 6th ed. Boston: Little, Brown, 1964.[↩]
- Bonow RO, Dodd JT, Maron BJ, O’Gara PT, White GG, McIntosh CL, et al. Long-term serial changes in left ventricular function and reversal of ventricular dilatation after valve replacement for chronic aortic regurgitation. Circulation. 1988;78(5 pt 1):1108–20.[↩]
- American Heart Association. About Arrhythmia. http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/About-Arrhythmia_UCM_002010_Article.jsp[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Congenital Heart Defects (CHDs). https://www.cdc.gov/ncbddd/heartdefects/index.html[↩]
- Congenital Heart Defects and Physical Activity. http://www.heart.org/HEARTORG/Conditions/CongenitalHeartDefects/CareTreatmentforCongenitalHeartDefects/Congenital-Heart-Defects-and-Physical-Activity_UCM_307738_Article.jsp[↩]