Contents
What is aplastic anemia
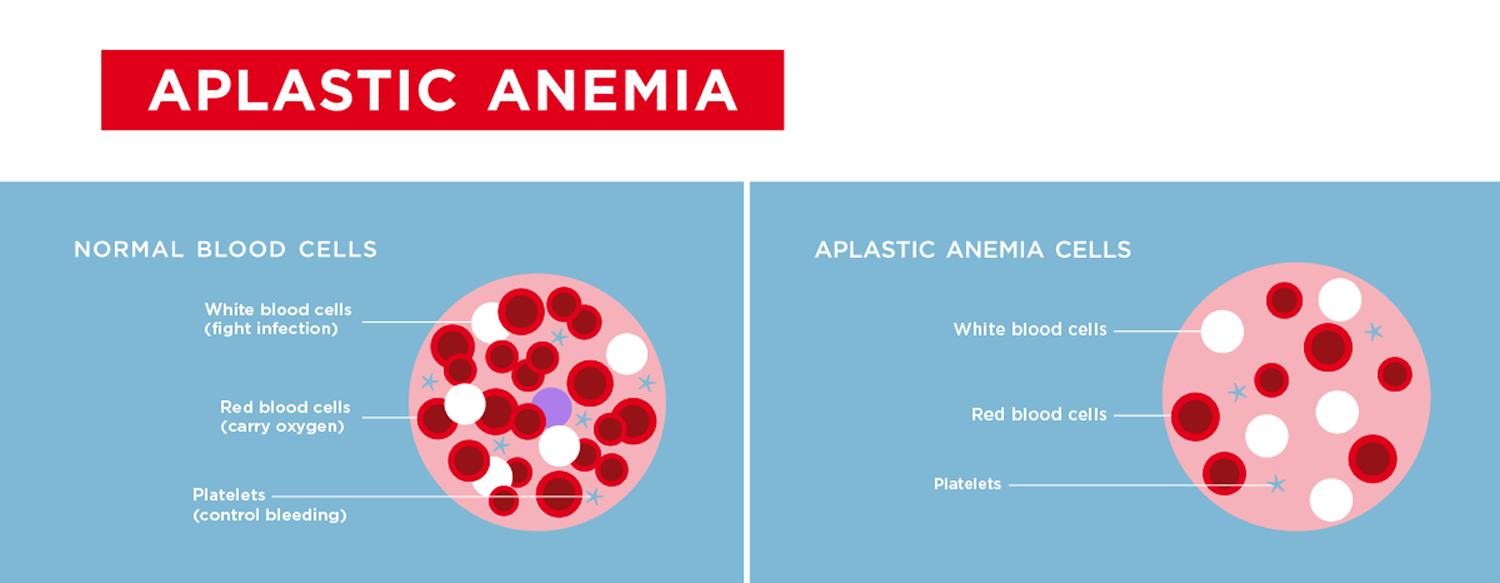
Aplastic anemia is a rare disease but serious blood disorder caused by a decrease in the number of all types of blood cells that bone marrow produces 1. Normally, the bone marrow produces a sufficient number of new red blood cells (RBCs), white blood cells (WBCs), and platelets for normal body function. Each type of cell enters the blood, circulates, and then dies within a certain time frame. For example, the normal lifespan of red blood cells (RBCs) is about 120 days. If the bone marrow is not able to produce enough blood cells to replace those that die, a number of symptoms, including those due to anemia, may result. This form of anemia can be severe or even fatal.
Red blood cells carry oxygen to all parts of your body. They also carry carbon dioxide (a waste product) to your lungs to be exhaled. White blood cells help your body fight infections. Platelets are blood cell fragments that stick together to seal small cuts or breaks on blood vessel walls and stop bleeding.
If your bone marrow can’t make enough new blood cells, many health problems can occur. These problems include irregular heartbeats called arrhythmias, an enlarged heart, heart failure, infections, and bleeding. Severe aplastic anemia can even cause death.
Aplastic anemia can develop at any age. Aplastic anemia may occur suddenly, or it can occur slowly and get worse over a long period of time.
Between 600 and 900 people are diagnosed with aplastic anemia each year in the U.S. It can strike people of any age, race or gender, but it’s more common among children, teenagers and older adults. It is also more likely to occur in people of Asian heritage.
There are different types of aplastic anemia, including Fanconi anemia. Causes include:
- Toxic substances, such as pesticides, arsenic, and benzene
- Radiation therapy and chemotherapy for cancer
- Certain medicines
- Infections such as hepatitis, Epstein-Barr virus, or HIV
- Autoimmune disorders
- Certain inherited conditions
- Pregnancy
In many people, the cause is unknown.
Symptoms of aplastic anemia can appear abruptly or can develop more slowly. Some general symptoms that are common to different types of anemia may appear first and are due to the decrease in number of red blood cells (RBCs).
Some additional signs and symptoms that occur with aplastic anemia include those due to decreased platelets:
- Prolonged bleeding
- Frequent nosebleeds and bleeding gums
- Easy bruising
- Pinpoint red spots on skin
- Blood in the stool
- Heavy menstrual bleeding
There may also be signs and symptoms due to a low white blood cell count:
- Increased frequency and severity of infections
- Fever
Your doctor will diagnose aplastic anemia based on your medical and family histories, a physical exam, and test results. Once your doctor knows the cause and severity of the condition, he or she can create a treatment plan for you. Treatments include blood transfusions, blood and marrow stem cell transplants, and medicines.
Confusion with myelodysplastic syndrome
Aplastic anemia can be mistaken for a condition called myelodysplastic syndrome. In myelodysplastic syndrome disorders, the bone marrow produces new blood cells, but they’re deformed and underdeveloped. Doctors consider myelodysplastic syndromes to be a slow growing form of blood and bone marrow cancer. The bone marrow in myelodysplastic syndrome is sometimes called hyperplastic — meaning that it’s packed with blood cells. But some people with myelodysplastic syndrome have empty marrow that’s difficult to distinguish from aplastic anemia.
Doctors must do a bone marrow biopsy to be certain of the diagnosis. Symptoms and the course of myelodysplastic syndrome vary for each patient depending on which blood cells are affected.
The exact number of people who have myelodysplastic syndrome is unknown, but about 10,300 new cases were reported in the U.S. in 2003. This number is the result of data collected by the Surveillance, Epidemiology, and End Results (SEER) Program of the Centers for Disease Control (CDC) and the National Cancer Institute (NCI). This program only started collecting data in 2001. The number of people may be higher than reported because some doctors are still don’t know that they need to report myelodysplastic syndrome cases to a national registry. Some doctors believe there are as many as 12,000 to 15,000 new myelodysplastic syndrome cases a year.
People diagnosed with myelodysplastic syndrome are:
- More often men than women
- Most often age 60 or older; 72 is the average age of diagnosis
- Most often white (Caucasian)
Native Americans, African-Americans, Inuits, Asians, and Pacific Islanders are less likely to get myelodysplastic syndrome.
Blood Cell Formation
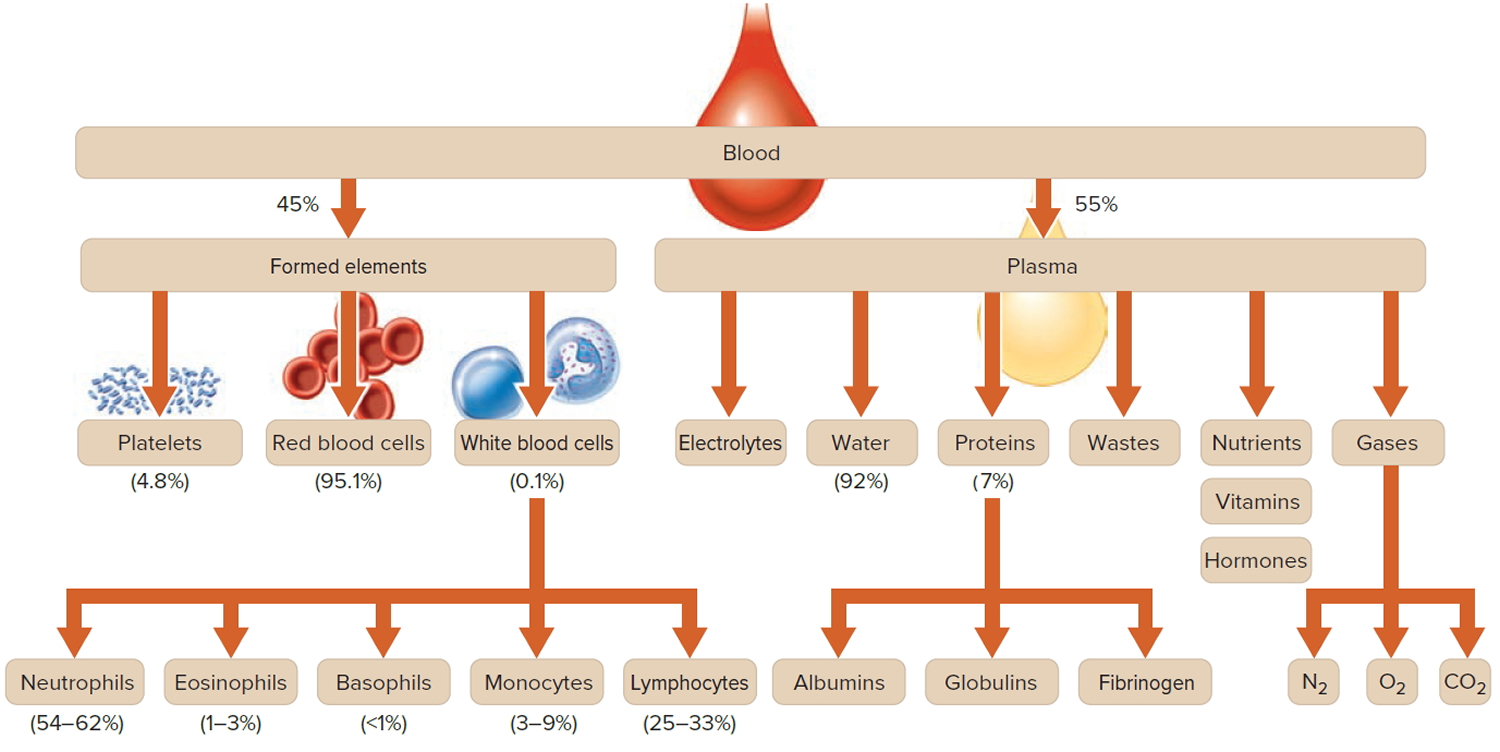
Blood is a complex mixture of formed elements in a liquid extracellular matrix, called blood plasma. Note that water and proteins account for 99% of the blood plasma.
Figure 1. Blood composition
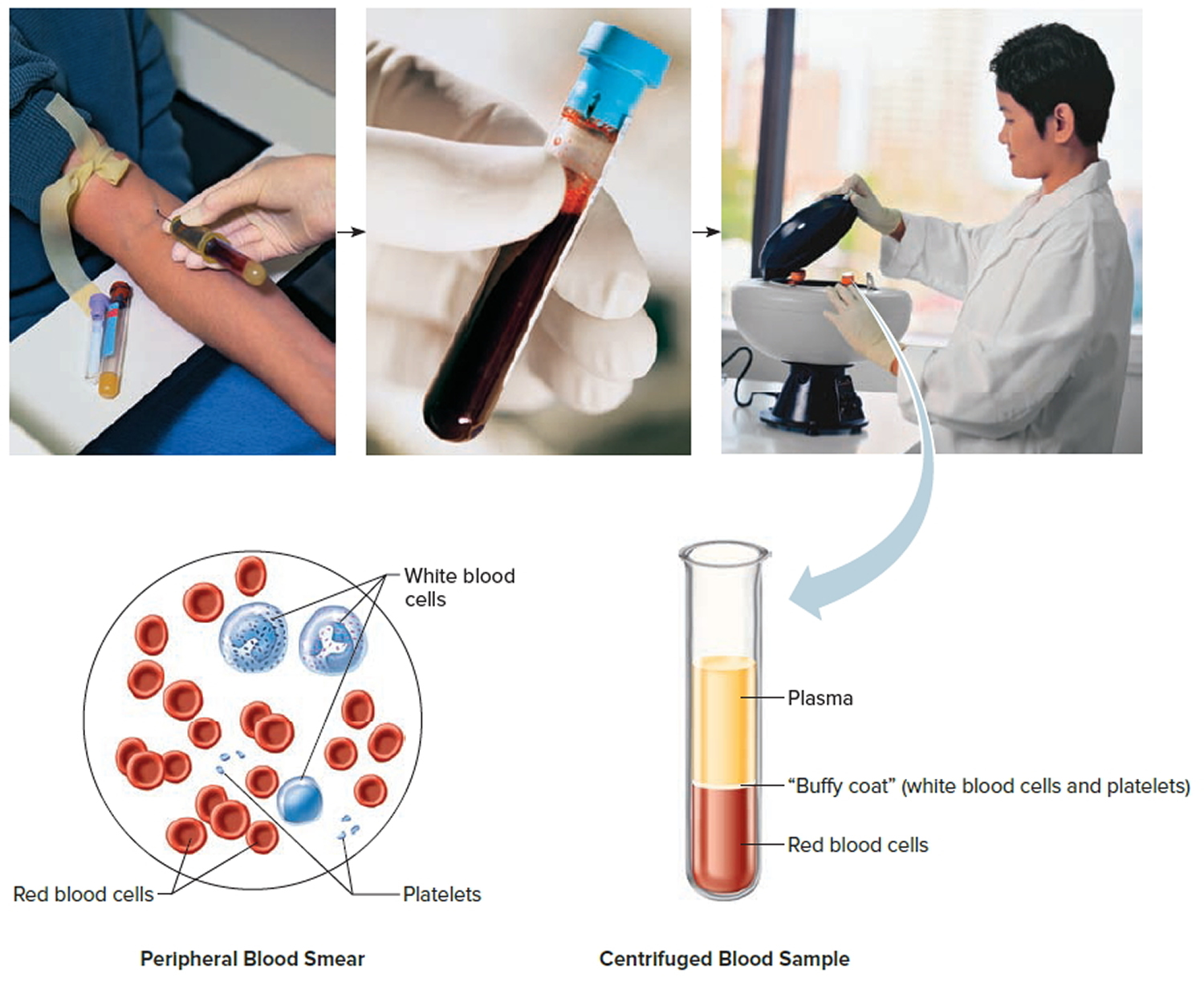
Note: Blood consists of a liquid portion called plasma and a solid portion (the formed elements) that includes red blood cells, white blood cells, and platelets. When blood components are separated by centrifugation, the white blood cells and platelets form a thin layer, called the “buffy coat,” between the plasma and the red blood cells, which accounts for about 1% of the total blood volume. Blood cells and platelets can be seen under a light microscope when a blood sample is smeared onto a glass slide.
The process of blood cell formation, called hematopoiesis, begins in the yolk sac, which lies outside the human embryo. Later in the fetal development, red blood cells are manufactured (erythropoiesis) in the liver and spleen, and still later they form in bone marrow. After birth, these cells are produced in the red bone marrow.
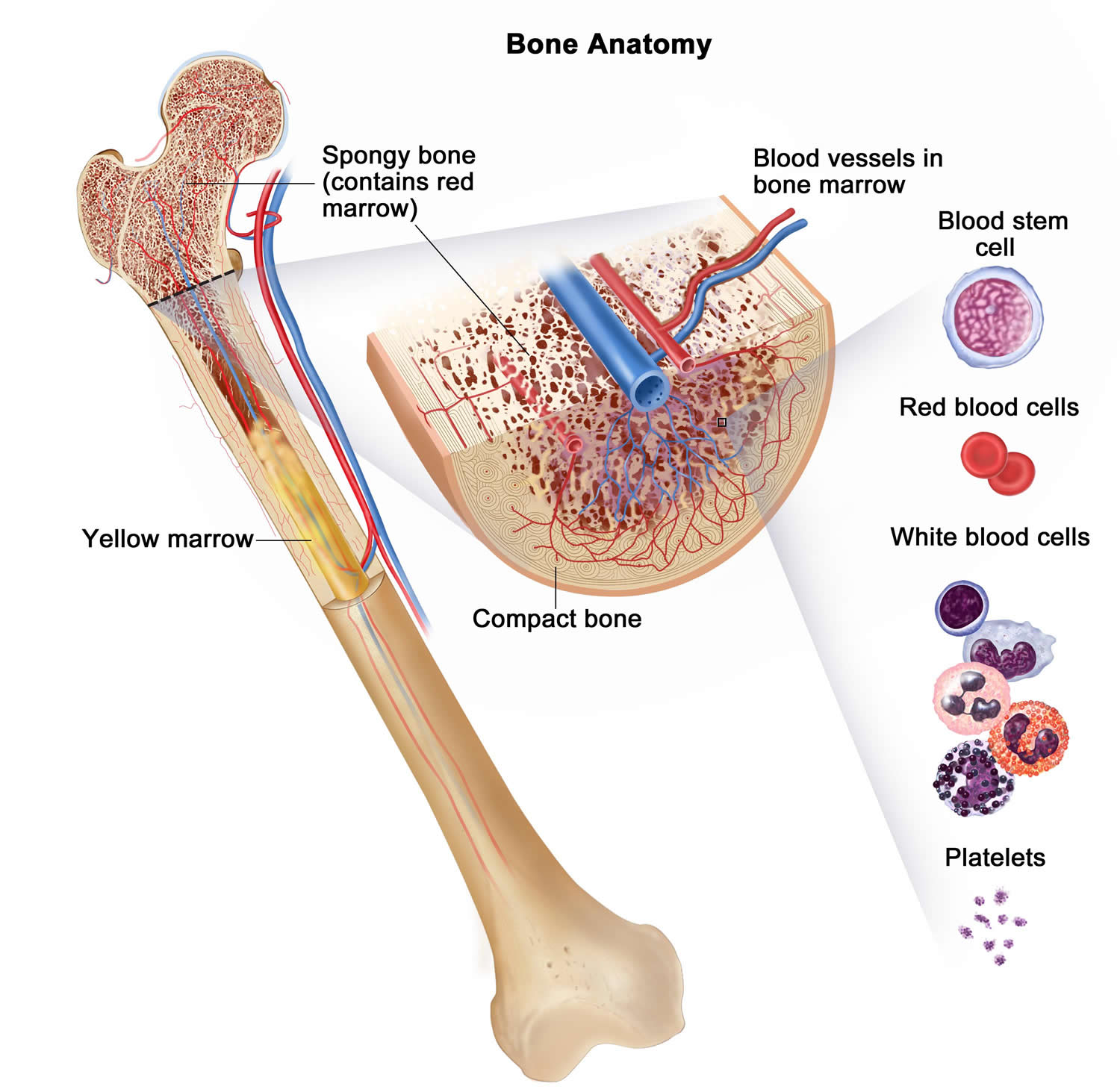
Bone marrow is a soft, netlike mass of connective tissue within the medullary cavities of long bones, in the irregular spaces of spongy bone, and in the larger central canals of compact bone tissue. It is of two kinds: red and yellow. Red bone marrow functions in the formation of red blood cells (erythrocytes), white blood cells (leukocytes), and blood platelets. The color comes from the oxygen-carrying pigment hemoglobin in the red blood cells.
In an infant, red marrow occupies the cavities of most bones. As a person ages, yellow bone marrow, which stores fat, replaces much of the red marrow. Yellow marrow is not active in blood cell production. In an adult, red marrow is primarily found in the spongy bone of the skull, ribs, breastbone (sternum), collarbones (clavicles), backbones (vertebrae), and hip bones. If the supply of blood cells is deficient, some yellow marrow may become red marrow, which then reverts to yellow marrow when the deficiency is corrected.
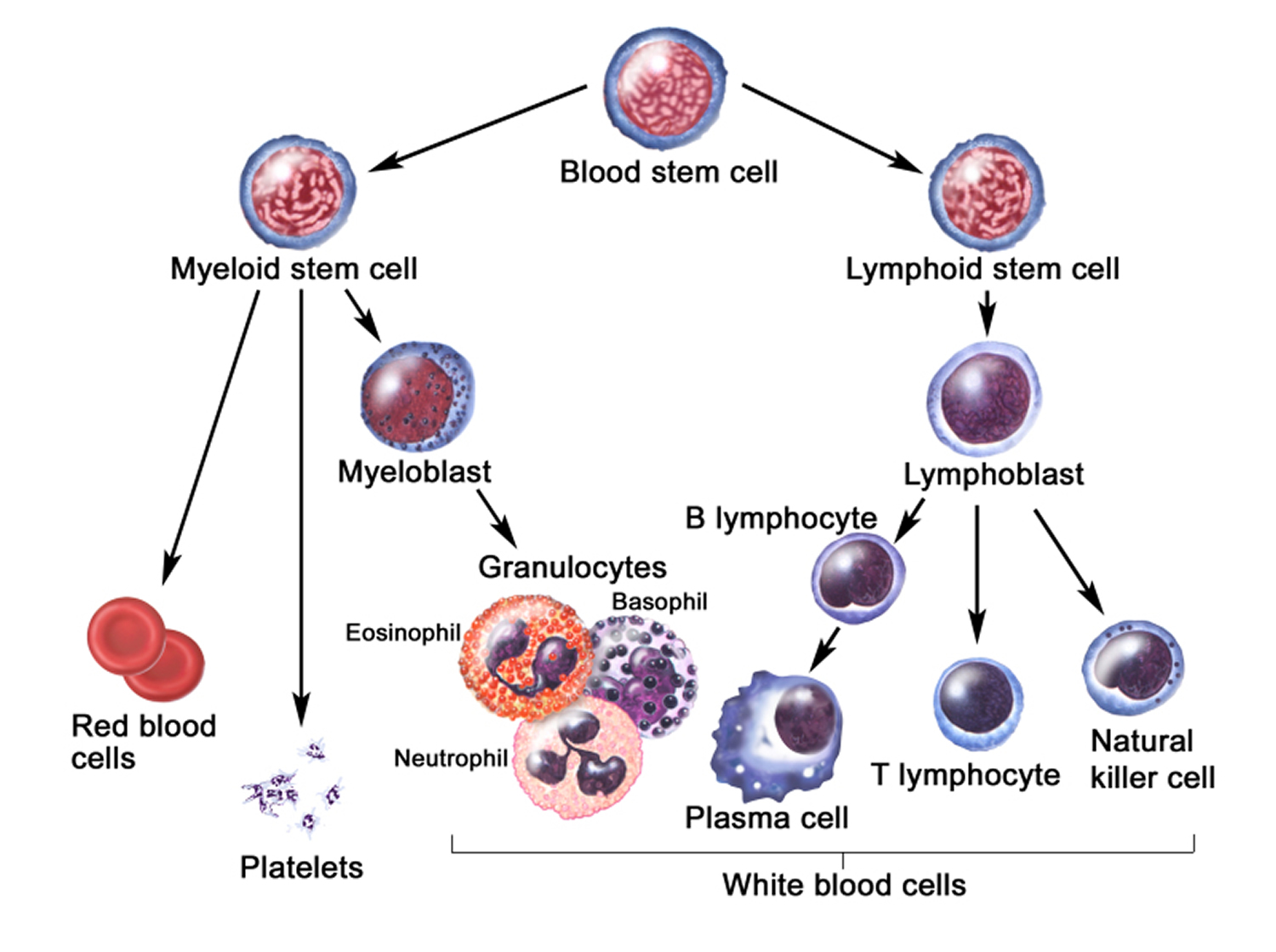
Figure 2 illustrates the stages in the formation of red blood cells from hematopoietic stem cells (blood-forming cells), which are also called hemocytoblasts.
Red blood cells have nuclei during their early stages of development but lose their nuclei as the cells mature. Losing the nuclei provides more space for hemoglobin. Because mature red blood cells do not have nuclei, they cannot divide. They use none of the oxygen they carry because they do not have mitochondria. Mature red blood cells produce ATP through glycolysis only.
The average life span of a red blood cell is 120 days. Many of these cells are removed from the circulation each day, and yet the number of cells in the circulating blood remains relatively stable. This observation suggests a homeostatic control of the rate of red blood cell production.
The hormone erythropoietin controls the rate of red blood cell formation through negative feedback. The kidneys, and to a lesser extent the liver, release erythropoietin in response to prolonged oxygen deficiency (Figure 5). At high altitudes, for example, where the amount of oxygen in the air is reduced, the blood oxygen level initially decreases. This drop in the blood oxygen level triggers the release of erythropoietin, which travels via the blood to the red bone marrow and stimulates red blood cell production.
After a few days of exposure to high altitudes, many newly formed red blood cells appear in the circulating blood. The increased rate of production continues until the number of erythrocytes in the circulation is sufficient to supply tissues with oxygen. When the availability of oxygen returns to normal, erythropoietin release decreases, and the rate of red blood cell production returns to normal as well. An excessive increase in red blood cells is called polycythemia. This condition increases blood viscosity, slowing blood flow and impairing circulation.
Figure 2. Bone marrow anatomy
Anatomy of the bone. The bone is made up of compact bone, spongy bone, and bone marrow. Compact bone makes up the outer layer of the bone. Spongy bone is found mostly at the ends of bones and contains red marrow. Bone marrow is found in the center of most bones and has many blood vessels. There are two types of bone marrow: red and yellow. Red marrow contains blood stem cells that can become red blood cells, white blood cells, or platelets. Yellow marrow is made mostly of fat.
Figure 3. Blood cell development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell
 Aplastic anemia prognosis and life expectancy
Aplastic anemia prognosis and life expectancy
Aplastic anemia is a rare but serious disorder. It can develop suddenly or slowly. The disorder tends to get worse over time, unless its cause is found and treated. Treatments for aplastic anemia include blood transfusions, blood and marrow stem cell transplants, and medicines.
With prompt and proper care, many people who have aplastic anemia can be successfully treated. Blood and marrow stem cell transplants may offer a cure for some people who have aplastic anemia.
Prognosis guidelines based on current data 2
Aplastic Anemia
With standard treatments, about 7 out of 10 aplastic anemia patients get better. Standard treatments include immunosuppressive therapy with antithymocyte globulin (ATG) with cyclosporine, or a bone marrow transplant. The chance for recovery depends on many factors, including how severe your case is and how you respond to treatment.
Myelodysplastic syndrome
There are many different subtypes of myelodysplastic syndromes, which are identified by testing the blood and bone marrow. Your myelodysplastic syndrome subtype is a key factor in a doctor’ decision about your treatment and your prognosis (an educated guess about the likely course of your disease and how long you might live).
To figure out a prognosis for a given patient, doctors also use a prognostic scoring system. The most common one used today is the International Prognostic Scoring System (IPSS). This system looks at three things:
- Number of low blood counts you have
- Percentage of young white blood cells (blasts) in bone marrow cells
- Number of cytogenetic changes (abnormal gene changes) in bone marrow cells
This prognostic scoring system tells your doctor how severe your disease is and how likely it is that your myelodysplastic syndrome might become acute myeloid leukemia (AML). It also gives your doctor a general idea about how long you might live.
With current treatments, patients with lower-risk types of some myelodysplastic syndrome can live for 5 years or even longer. Patients with higher-risk myelodysplastic syndrome that becomes acute myeloid leukemia (AML) are likely to have a shorter life span. About 30 out of 100 myelodysplastic syndrome patients will develop acute myeloid leukemia (AML).
Paroxysmal nocturnal hemoglobinuria
Many people with paroxysmal nocturnal hemoglobinuria live for decades. People with paroxysmal nocturnal hemoglobinuria who develop blood clots in key parts of the body or develop MDS (myelodysplastic syndromes) or AML (acute myeloid leukemia) may have a shorter life span.
New treatments becoming available for paroxysmal nocturnal hemoglobinuria are helping people with paroxysmal nocturnal hemoglobinuria to live longer. Older research you may have come across state that paroxysmal nocturnal hemoglobinuria patients live an average of 15 to 20 years after diagnosis. More recent research shows how that lifespan has climbed over the past 20 years. It’s possible that paroxysmal nocturnal hemoglobinuria patients – who rarely develop myelodysplastic syndrome or acute myeloid leukemia (AML) – will soon have a lifespan that is normal compared with people their own age.
Aplastic anemia causes
Causes of aplastic anemia usually have to do with damage to the stem cells in the bone marrow that are responsible for blood cell production. When stem cells are damaged, they don’t grow into healthy blood cells.
The cause of the damage can be acquired or inherited. “Acquired” means you aren’t born with the condition, but you develop it. “Inherited” means your parents passed the gene for the condition on to you.
Acquired aplastic anemia is more common, and sometimes it’s only temporary. Inherited aplastic anemia is rare.
In many people who have aplastic anemia, the cause is unknown. Some research suggests that stem cell damage may occur because the body’s immune system attacks its own cells by mistake.
Some factors that may be involved with bone marrow damage and that can lead to aplastic anemia include:
- Exposure to toxic substances like arsenic, benzene (found in gasoline), or pesticides. Exposure to toxic chemicals, such as some used in pesticides and insecticides, may cause aplastic anemia. Exposure to benzene — an ingredient in gasoline — also has been linked to aplastic anemia. This type of anemia may get better on its own if you avoid repeated exposure to the chemicals that caused your initial illness.
- Cancer therapy (radiation or chemotherapy). While these cancer-fighting therapies kill cancer cells, they can also damage healthy cells, including stem cells in bone marrow. Aplastic anemia can be a temporary side effect of these treatments.
- Autoimmune disorders such as lupus or rheumatoid arthritis. An autoimmune disorder, in which your immune system begins attacking healthy cells, may involve stem cells in your bone marrow.
- Use of certain drugs. Some medications, such as those used to treat rheumatoid arthritis and some antibiotics, can cause aplastic anemia.
- Viral infections such as hepatitis, HIV, EBV (Epstein-Barr virus), or CMV (cytomegalovirus). Viral infections that affect bone marrow may play a role in the development of aplastic anemia in some people. Viruses that have been linked to the development of aplastic anemia include hepatitis, Epstein-Barr, cytomegalovirus, parvovirus B19 and HIV.
- Medicines such as chloramphenicol (an antibiotic rarely used in the U.S.).
- Pregnancy. Aplastic anemia that occurs in pregnancy may be related to an autoimmune problem — your immune system may attack your bone marrow during pregnancy.
- Unknown factors. In many cases, doctors aren’t able to identify the cause of aplastic anemia. This is called idiopathic aplastic anemia.
Rarely, aplastic anemia is due to an inherited (genetic) disorder such as Fanconi anemia. For more on this rare blood condition, see the Fanconi Anemia. Other genetic disorders leading to aplastic anemia include Shwachman-Diamond syndrome and dyskeratosis congenita.
Acquired Causes
Many diseases, conditions, and factors can cause aplastic anemia, including:
- Toxins, such as pesticides, arsenic, and benzene.
- Radiation and chemotherapy (treatments for cancer).
- Medicines, such as chloramphenicol (an antibiotic rarely used in the United States).
- Infectious diseases, such as hepatitis, Epstein-Barr virus (EBV), cytomegalovirus (CMV), parvovirus B19, and HIV.
- Autoimmune disorders, such as lupus and rheumatoid arthritis.
- Pregnancy. Aplastic anemia that occurs during pregnancy often goes away after delivery.
Sometimes, cancer from another part of the body can spread to the bone and cause aplastic anemia.
Inherited Causes
Certain inherited conditions can damage the stem cells and lead to aplastic anemia. Examples include Fanconi anemia, Shwachman-Diamond syndrome, dyskeratosis congenita, and Diamond-Blackfan anemia.
Risk Factors for aplastic anemia
Aplastic anemia is a rare but serious blood disorder. People of all ages can develop aplastic anemia. However, it’s most common in adolescents, young adults, and the elderly. Men and women are equally likely to have it.
The disorder is two to three times more common in Asian countries.
Your risk of aplastic anemia is higher if you:
- Have been exposed to toxins
- Have taken certain medicines or had radiation or chemotherapy (treatments for cancer)
- Have certain infectious diseases, autoimmune disorders, or inherited conditions.
Aplastic anemia signs and symptoms
Lower than normal numbers of red blood cells, white blood cells, and platelets cause most of the signs and symptoms of aplastic anemia.
Aplastic anemia symptoms may include:
- Fatigue
- Shortness of breath with exertion
- Rapid or irregular heart rate
- Pale skin
- Frequent or prolonged infections
- Unexplained or easy bruising
- Nosebleeds and bleeding gums
- Prolonged bleeding from cuts
- Skin rash
- Dizziness
- Headache
Aplastic anemia can progress slowly over weeks or months, or it may come on suddenly. The illness may be brief, or it may become chronic. Aplastic anemia can be very severe and even fatal.
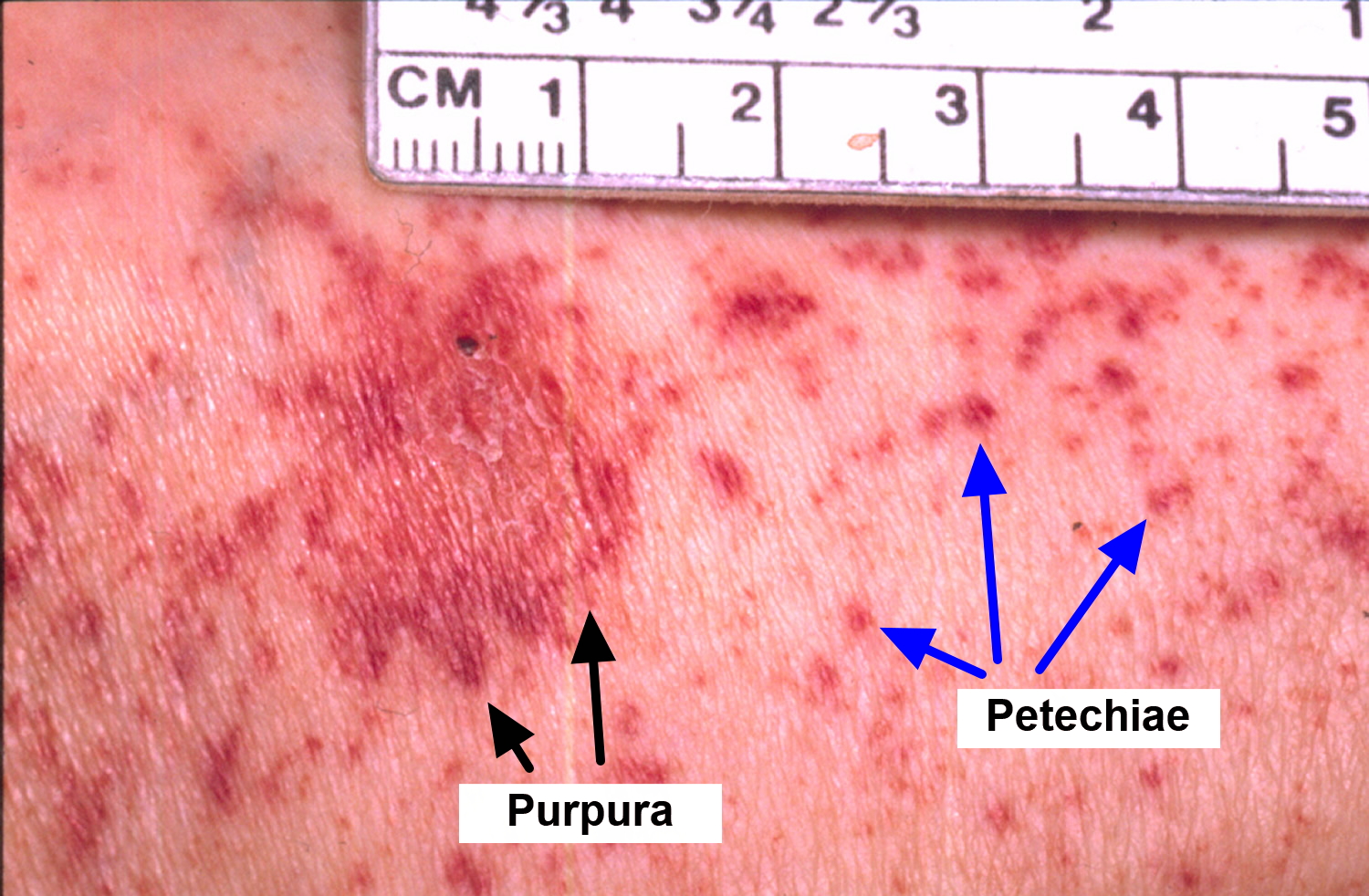
Figure 4. Aplastic anemia rash
Signs and Symptoms of Low Blood Cell Counts
Red Blood Cells
The most common symptom of a low red blood cell count is fatigue (tiredness). A lack of hemoglobin in the blood causes fatigue. Hemoglobin is an iron-rich protein in red blood cells. It helps carry oxygen to the body.
A low red blood cell count also can cause shortness of breath; dizziness, especially when standing up; headaches; coldness in your hands or feet; pale skin; and chest pain.
If you don’t have enough hemoglobin-carrying red blood cells, your heart has to work harder to move the reduced amount of oxygen in your blood. This can lead to arrhythmias (irregular heartbeats), a heart murmur, an enlarged heart, or even heart failure.
White Blood Cells
White blood cells help fight infections. Signs and symptoms of a low white blood cell count include fevers, frequent infections that can be severe, and flu-like illnesses that linger.
Platelets
Platelets stick together to seal small cuts or breaks on blood vessel walls and stop bleeding. People who have low platelet counts tend to bruise and bleed easily, and the bleeding may be hard to stop.
Common types of bleeding associated with a low platelet count include nosebleeds, bleeding gums, pinpoint red spots on the skin, and blood in the stool. Women also may have heavy menstrual bleeding.
Other Signs and Symptoms
Aplastic anemia can cause signs and symptoms that aren’t directly related to low blood cell counts. Examples include nausea (feeling sick to your stomach) and skin rashes.
Paroxysmal Nocturnal Hemoglobinuria
Some people who have aplastic anemia have a condition called paroxysmal nocturnal hemoglobinuria. This is very rare blood disease that causes red blood cells to break apart. Most people who have paroxysmal nocturnal hemoglobinuria don’t have any signs or symptoms.
Paroxysmal Nocturnal Hemoglobinuria occurs because of a genetic change to some of your blood-forming stem cells. These defective stem cells become paroxysmal nocturnal hemoglobinuria blood cells that are missing an important coating (protein) that protects them from your immune system. If you have paroxysmal nocturnal hemoglobinuria, there will be times when your immune system destroys many red blood cells very quickly, causing low red blood cell counts, as well as blood clots, muscle spasms and dark urine. This destruction of blood cells is called hemolysis.
Paroxysmal Nocturnal Hemoglobinuria can strike people of any age, race or gender. Only about 500 people are diagnosed with paroxysmal nocturnal hemoglobinuria in the U.S. each year. Paroxysmal Nocturnal Hemoglobinuria tends to be more common in adults in their thirties and early forties.
If paroxysmal nocturnal hemoglobinuria symptoms do occur, they may include:
- Shortness of breath
- Swelling or pain in the abdomen or swelling in the legs caused by blood clots
- Blood in the urine
- Headaches
- Jaundice (a yellowish color of the skin or whites of the eyes)
In people who have aplastic anemia and paroxysmal nocturnal hemoglobinuria, either condition can develop first.
Aplastic anemia diagnosis
Your doctor will diagnose aplastic anemia based on your medical and family histories, a physical exam, and test results.
A physical examination or complete medical history may reveal possible causes for aplastic anemia, such as exposure to toxins or certain drugs (e.g., chloramphenicol) or prior treatment for cancer. Some cases of aplastic anemia are temporary while others have lasting damage to the bone marrow.
Once your doctor knows the cause and severity of the condition, he or she can create a treatment plan for you.
Medical and Family Histories
Your doctor may ask questions about your medical history, such as whether:
- You’ve had anemia or a condition that can cause anemia
- You have shortness of breath, dizziness, headaches, or other signs and symptoms of anemia
- You’ve been exposed to certain toxins or medicines
- You’ve had radiation or chemotherapy (treatments for cancer)
- You’ve had infections or signs of infections, such as fever
- You bruise or bleed easily
Your doctor also may ask whether any of your family members have had anemia or other blood disorders.
Physical Exam
Your doctor will do a physical exam to check for signs of aplastic anemia. He or she will try to find out how severe the disorder is and what’s causing it.
The exam may include checking for pale or yellowish skin and signs of bleeding or infection. Your doctor may listen to your heart and lungs for abnormal heartbeats and breathing sounds. He or she also may feel your abdomen to check the size of your liver and feel your legs for swelling.
Laboratory Tests
The initial test for anemia, the complete blood count (CBC), may reveal many abnormal results.
- Hemoglobin and/or hematocrit may be low.
- Red blood cell (RBC) and white blood cell (WBC) counts are low.
- Platelet count is low.
- Red blood cell indices are usually normal.
- The differential white blood count shows a decrease in most types of cells but not lymphocytes.
Some additional tests that may be performed to help determine the type and cause of anemia include:
- Reticulocyte count—result is low
- Erythropoietin—usually increased in aplastic anemia
- Bone marrow aspiration or biopsy will show a decrease in the number of all types of cells.
- Tests for infections such as hepatitis, HIV, EBV, CMV help to determine the cause.
- Tests for arsenic (a heavy metal) and other toxins
- Iron tests or tests for vitamin B12 may be done to rule out other causes.
- ANA—to determine if the cause is autoimmune disease
Complete Blood Count
Often, the first test used to diagnose aplastic anemia is a complete blood count (CBC). The CBC measures many parts of your blood.
This test checks your hemoglobin and hematocrit levels. Hemoglobin is an iron-rich protein in red blood cells. It carries oxygen to the body. Hematocrit is a measure of how much space red blood cells take up in your blood. A low level of hemoglobin or hematocrit is a sign of anemia.
The normal range of these levels varies in certain racial and ethnic populations. Your doctor can explain your test results to you.
The CBC also checks the number of red blood cells, white blood cells, and platelets in your blood. Abnormal results may be a sign of aplastic anemia, an infection, or another condition.
Finally, the CBC looks at mean corpuscular volume (MCV). MCV is a measure of the average size of your red blood cells. The results may be a clue as to the cause of your anemia.
Reticulocyte Count
A reticulocyte count measures the number of young red blood cells in your blood. The test shows whether your bone marrow is making red blood cells at the correct rate. People who have aplastic anemia have low reticulocyte levels.
Bone Marrow Tests
Bone marrow tests show whether your bone marrow is healthy and making enough blood cells. The two bone marrow tests are aspiration (as-pi-RA-shun) and biopsy.
Bone marrow aspiration may be done to find out if and why your bone marrow isn’t making enough blood cells. For this test, your doctor removes a small amount of bone marrow fluid through a needle. The sample is looked at under a microscope to check for faulty cells.
A bone marrow biopsy may be done at the same time as an aspiration or afterward. For this test, your doctor removes a small amount of bone marrow tissue through a needle.
The tissue is checked for the number and types of cells in the bone marrow. In aplastic anemia, the bone marrow has a lower than normal number of all three types of blood cells.
Other Tests
Other conditions can cause symptoms similar to those of aplastic anemia. Thus, other tests may be needed to rule out those conditions. These tests may include:
- X ray, computed tomography (CT) scan, or an ultrasound imaging test. These tests can show enlarged lymph nodes in your abdomen. Enlarged lymph nodes may be a sign of blood cancer. Doctors also may use these tests to look at the kidneys and the bones in the arms and hands, which are sometimes abnormal in young people who have Fanconi anemia. This type of anemia can lead to aplastic anemia.
- Chest x ray. This test creates pictures of the structures inside your chest, such as your heart, lungs, and blood vessels. A chest x ray may be used to rule out infections.
- Liver tests and viral studies. These tests are used to check for liver diseases and viruses.
- Tests that check vitamin B12 and folate levels in the blood. These tests can help rule out anemia caused by vitamin deficiency.
Your doctor also may recommend blood tests for paroxysmal nocturnal hemoglobinuria and to check your immune system for proteins called antibodies. Antibodies in the immune system that attack your bone marrow cells may cause aplastic anemia.
Aplastic anemia treatment
The treatment of aplastic anemia depends on the cause. Reducing or eliminating exposure to certain toxins or drugs may help resolve the condition.
Treatments for aplastic anemia include blood transfusions, blood and marrow stem cell transplants, and medicines. These treatments can prevent or limit complications, relieve symptoms, and improve quality of life.
- Medications may be given to stimulate bone marrow production, to treat infections, or to suppress the immune system in cases of autoimmune disorders.
- Blood transfusions and a bone marrow transplant may be needed in severe cases.
Blood and marrow stem cell transplants may cure the disorder in some people who are eligible for a transplant. Removing a known cause of aplastic anemia, such as exposure to a toxin, also may cure the condition.
Who Needs Treatment
People who have mild or moderate aplastic anemia may not need treatment as long as the condition doesn’t get worse. People who have severe aplastic anemia need medical treatment right away to prevent complications.
People who have very severe aplastic anemia need emergency medical care in a hospital. Very severe aplastic anemia can be fatal if it’s not treated right away.
Blood Transfusions
Blood transfusions can help keep blood cell counts at acceptable levels. A blood transfusion is a common procedure in which blood is given to you through an intravenous (IV) line in one of your blood vessels.
Transfusions require careful matching of donated blood with the recipient’s blood.
Blood transfusions help relieve the symptoms of aplastic anemia, but they’re not a permanent treatment.
Blood and Marrow Stem Cell Transplants
A blood and marrow stem cell transplant replaces damaged stem cells with healthy ones from another person (a donor).
During the transplant, which is like a blood transfusion, you get donated stem cells through a tube placed in a vein in your chest. Once the stem cells are in your body, they travel to your bone marrow and begin making new blood cells.
Blood and marrow stem cell transplants may cure aplastic anemia in people who can have this type of treatment. The transplant works best in children and young adults with severe aplastic anemia who are in good health and who have matched donors.
Older people may be less able to handle the treatments needed to prepare the body for the transplant. They’re also more likely to have complications after the transplant.
If you have aplastic anemia, talk with your doctor about whether a blood and marrow stem cell transplant is an option for you.
Medicines
If you have aplastic anemia, your doctor may prescribe medicines to:
- Stimulate your bone marrow
- Suppress your immune system
- Prevent and treat infections
Medicines To Stimulate Bone Marrow
Man-made versions of substances that occur naturally in the body can stimulate the bone marrow to make more blood cells. Examples of these types of medicines include erythropoietin such as epoetin alfa (Epogen, Procrit) and colony-stimulating factors, such as sargramostim (Leukine), filgrastim (Neupogen) and pegfilgrastim (Neulasta) — may help stimulate the bone marrow to produce new blood cells. Growth factors are often used in combination with immune-suppressing drugs..
These medicines have some risks. You and your doctor will work together to decide whether the benefits of these medicines outweigh the risks. If this treatment works well, it can help you avoid the need for blood transfusions.
Medicines To Suppress the Immune System (Immunosuppressants)
Research suggests that aplastic anemia may sometimes occur because the body’s immune system attacks its own cells by mistake. For this reason, your doctor may prescribe medicines to suppress your immune system.
These medicines allow your bone marrow to start making blood cells again. They also may help you avoid the need for blood transfusions.
Medicines that suppress the immune system don’t cure aplastic anemia. However, they can relieve its symptoms and reduce complications. These medicines often are used for people who can’t have blood and marrow stem cell transplants or who are waiting for transplants.
Three medicines—often given together—can suppress the body’s immune system. They are antithymocyte globulin (ATG), cyclosporine, and methylprednisolone.
It may take a few months to notice the effects of these medicines. Most often, as blood cell counts rise, symptoms lessen. Blood cell counts in people who respond well to these medicines usually don’t reach normal levels. However, the blood cell counts often are high enough to allow people to do their normal activities.
People who have aplastic anemia may need long-term treatment with these medicines.
Medicines that suppress the immune system can have side effects. They also may increase the risk of developing leukemia or myelodysplasia. Leukemia is a cancer of the blood cells. Myelodysplasia is a condition in which the bone marrow makes too many faulty blood cells.
Medicines To Prevent and Treat Infections
If you have aplastic anemia, you might be at risk for infections due to low white blood cell counts. Your doctor may prescribe antibiotic and antiviral medicines to prevent and treat infections.
Lifestyle and home remedies
If you have aplastic anemia, take care of yourself by:
- Resting when you need to. Anemia can cause fatigue and shortness of breath with even mild exertion. Take a break and rest when you need to.
- Avoiding contact sports. Because of the risk of bleeding associated with a low platelet count, avoid activities that may result in a cut or fall.
- Protecting yourself from germs. You can reduce your risk of infections with frequent hand-washing and by avoiding sick people. If you develop a fever or other indicators of an infection, see your doctor for treatment.
Coping and support
Tips to help you and your family better cope with your illness include:
- Research your disease. The more you know, the better prepared you’ll be to make treatment decisions.
- Ask questions. Be sure to ask your doctor about anything related to your disease or treatment that you don’t understand. It may help you to record or write down what your doctor tells you.
- Be vocal. Don’t be afraid to express any concerns you have to your doctor or any other health care professional treating you.
- Seek support. Ask family and friends for emotional support. Ask them to consider becoming blood donors or bone marrow donors. Consider joining an aplastic anemia support group. It may be helpful to talk to others coping with the disease. Ask your doctor if he or she knows of any local support groups, or contact the Aplastic Anemia & MDS International Foundation 3. It offers a peer support network and can be reached at http://www.aamds.org/.
- Take care of yourself. Proper nutrition and sleep are important to optimize blood production.
Living with Aplastic Anemia
With prompt and proper care, most people who have aplastic anemia can be successfully treated, and some may be cured.
Most people who have the disorder are able to go back to their normal routines after treatment. However, it may take some time to get good results from treatment. You may need repeated treatments, or you may need to try several treatments to find one that works.
It’s important to get ongoing medical care to make sure the disorder doesn’t worsen and to check for possible complications.
Ongoing Care
Treatment for aplastic anemia may cause side effects or complications. Talk with your doctor about how to cope with these issues.
People who have aplastic anemia may be at higher risk for infections due to low white blood cell counts. Ask your doctor about ways to lower your risk of infection. For example, you may want to:
- Stay away from people who are sick and avoid large crowds of people.
- Avoid certain foods that can expose you to bacteria, such as uncooked foods.
- Wash your hands often.
- Brush and floss your teeth and get regular dental care to reduce the risk of infections in your mouth and throat.
- Get a yearly flu shot and pneumonia vaccine. Ask your doctor whether these shots will benefit you.
Know the signs of infection, such as fever. Call your doctor right away if you think you have an infection.
Physical Activity
Talk with your doctor about what types and amounts of physical activity are safe for you. You may want to avoid activities that cause chest pain or shortness of breath. You also may want to stay away from activities that could result in injuries and bleeding, such as contact sports.
Support Groups
You or your family members may find it helpful to know about resources that can give you emotional support and information about aplastic anemia.
Your doctor or hospital social worker may have information about counseling and support services. They also may be able to refer you to support groups that offer help with financial planning, because treatment for aplastic anemia can be costly.