Contents
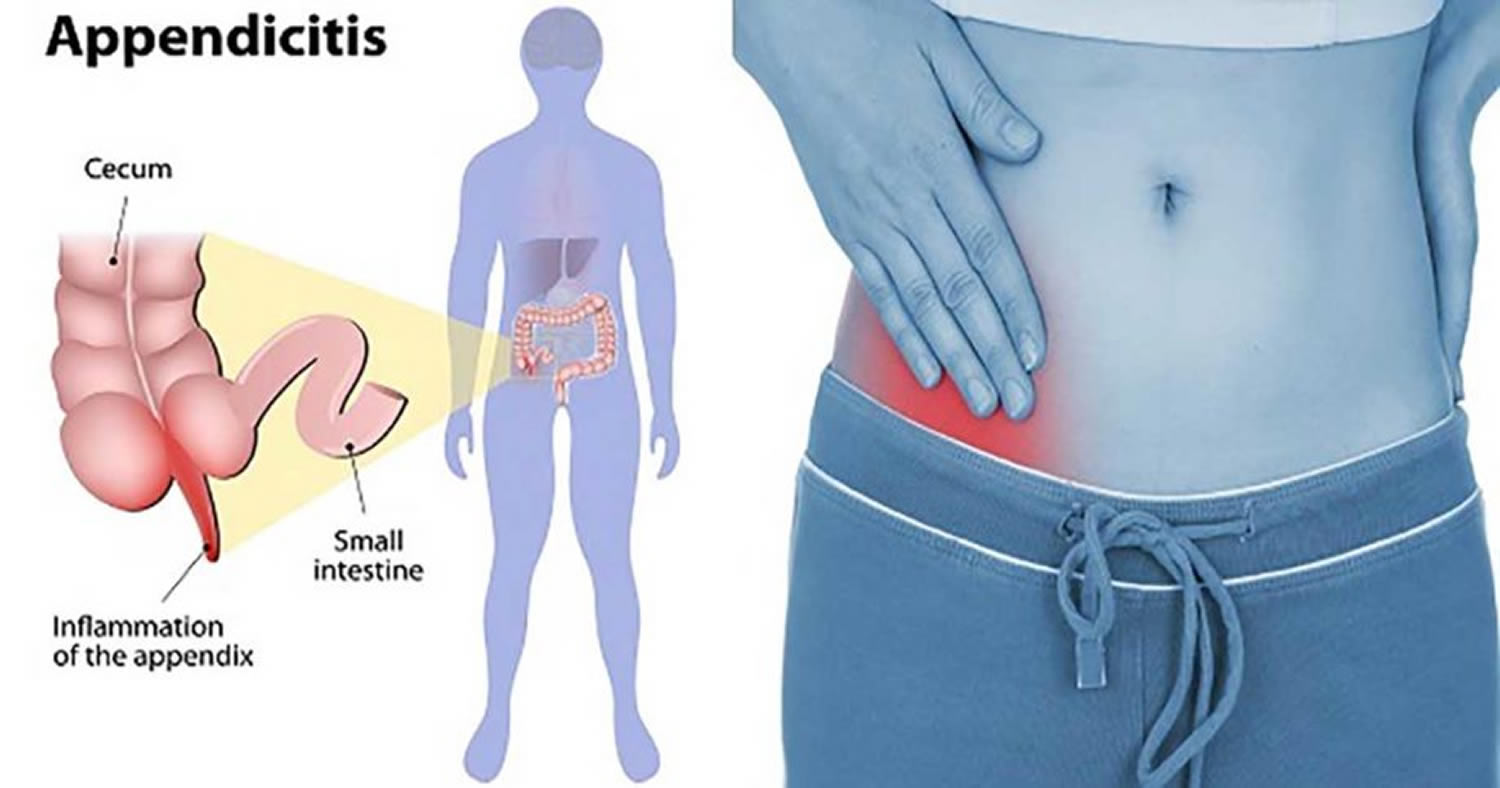
What is appendicitis ?
Appendicitis is inflammation of your appendix 1.
- Appendicitis is a medical emergency that requires immediate care. See a health care professional or go to the emergency room right away if you think you or a child has appendicitis. A doctor can help treat the appendicitis and reduce symptoms and the chance of complications.
In the United States, appendicitis is the most common cause of acute abdominal pain requiring surgery. Over 5% of the population develops appendicitis at some point 2. Appendicitis most commonly occurs in the teens and 20’s but may occur at any age.
What are the complications of appendicitis ?
If appendicitis is not treated, it may lead to complications. The complications of a ruptured appendix are:
- peritonitis, which can be a dangerous condition. Ruptured appendix may infect the double-layer peritoneal membrane that lines the abdominal cavity. The medical term for this is peritonitis. Peritonitis happens if your appendix bursts and infection spreads in your abdomen. If you have peritonitis, you may be very ill and have
- fever
- nausea
- severe tenderness in your abdomen
- vomiting
- an abscess of the appendix called an appendiceal abscess.
What causes appendicitis
Appendicitis can have more than one cause, and in many cases the cause is not clear. Possible causes include:
- Blockage of the opening inside the appendix
- Enlarged tissue in the wall of your appendix, caused by infection in the gastrointestinal (GI) tract or elsewhere in your body
- Inflammatory bowel disease
- Stool, parasites, or growths that can clog your appendiceal lumen
- Trauma to your abdomen
Appendicitis is thought to result from obstruction of the appendix lumen, typically by lymphoid (lymphocytes) hyperplasia, but occasionally by a fecalith, foreign body, or even worms. The obstruction leads to distention, bacterial overgrowth, ischemia, and inflammation. If untreated, necrosis, gangrene, and perforation occur. If the perforation is contained by the omentum, an appendiceal abscess results.
Symptoms and signs of appendicitis
The most common symptom of appendicitis is pain in your abdomen.
If you have appendicitis, you’ll most often have pain in your abdomen that 3:
- begins near your belly button and then moves lower and to your right
- gets worse in a matter of hours
- gets worse when you move around, take deep breaths, cough, or sneeze
- is severe and often described as different from any pain you’ve felt before
- occurs suddenly and may even wake you up if you’re sleeping
- occurs before other symptoms
Other symptoms of appendicitis may include 3:
- loss of appetite
- nausea
- vomiting
- constipation or diarrhea
- an inability to pass gas
- a low-grade fever
- swelling in your abdomen
- the feeling that having a bowel movement will relieve discomfort
Symptoms can be different for each person and can seem like the following conditions that also cause pain in the abdomen:
- abdominal adhesions
- constipation
- inflammatory bowel disease, which includes Crohn’s disease and ulcerative colitis, long-lasting disorders that cause irritation and ulcers in the GI tract
- intestinal obstruction
- pelvic inflammatory disease
The following are signs that you have appendicitis:
- Rovsing’s sign: If palpation of the left lower quadrant of a person’s abdomen increases the pain felt in the right lower quadrant, the patient is said to have a positive Rovsing’s sign and may have appendicitis.
- Psoas sign: It is elicited by performing the psoas test by passively extending the thigh of a patient lying on his side with knees extended, or asking the patient to flex his thigh at the hip. If abdominal pain results, it is a “positive psoas sign”.
- Obturator sign: the obturator test, is carried out on each leg in succession. The patient lies on her/his back with the hip and knee both flexed at ninety degrees. The examiner holds the patient’s ankle with one hand and knee with the other hand. The examiner internally rotates the hip by moving the patient’s ankle away from the patient’s body while allowing the knee to move only inward. This is flexion and internal rotation of the hip. This causes pain and is evidence in support of an inflamed appendix.
- Guarding: Is the tensing of the abdominal wall muscles to guard inflamed organs within the abdomen from the pain of pressure upon them. The tensing is detected when the abdominal wall is pressed.
- Rebound tenderness (Blumberg’s sign): Is a clinical sign that is elicited during physical examination of a patient’s abdomen by a doctor. It refers to pain upon removal of pressure rather than application of pressure to the abdomen. It is indicative of peritonitis.
Diagnosis of Appendicitis
Most often, health care professionals suspect the diagnosis of appendicitis based on your symptoms, your medical history, and a physical exam. A doctor can confirm the diagnosis with an ultrasound, x-ray, or MRI exam.
Medical history
A health care professional will ask specific questions about your symptoms and health history to help rule out other health problems. The health care professional will want to know:
- when your abdominal pain began
- the exact location and severity of your pain
- when your other symptoms appeared
- your other medical conditions, previous illnesses, and surgical procedures
- whether you use medicines, alcohol, or illegal drugs
Physical exam
Health care professionals need specific details about the pain in your abdomen to diagnose appendicitis correctly. A health care professional will assess your pain by touching or applying pressure to specific areas of your abdomen.
The following responses to touch or pressure may indicate that you have appendicitis:
- Rovsing’s sign: If palpation of the left lower quadrant of a person’s abdomen increases the pain felt in the right lower quadrant, the patient is said to have a positive Rovsing’s sign and may have appendicitis.
- Psoas sign: It is elicited by performing the psoas test by passively extending the thigh of a patient lying on his side with knees extended, or asking the patient to flex his thigh at the hip. If abdominal pain results, it is a “positive psoas sign”.
- Obturator sign: the obturator test, is carried out on each leg in succession. The patient lies on her/his back with the hip and knee both flexed at ninety degrees. The examiner holds the patient’s ankle with one hand and knee with the other hand. The examiner internally rotates the hip by moving the patient’s ankle away from the patient’s body while allowing the knee to move only inward. This is flexion and internal rotation of the hip. This causes pain and is evidence in support of an inflamed appendix.
- Guarding: Is the tensing of the abdominal wall muscles to guard inflamed organs within the abdomen from the pain of pressure upon them. The tensing is detected when the abdominal wall is pressed.
- Rebound tenderness (Blumberg’s sign): Is a clinical sign that is elicited during physical examination of a patient’s abdomen by a doctor. It refers to pain upon removal of pressure rather than application of pressure to the abdomen. It is indicative of peritonitis.
- Digital rectal exam
- Pelvic exam
Lab tests
Doctors use lab tests to help confirm the diagnosis of appendicitis or find other causes of abdominal pain.
Blood tests. A health care professional draws your blood for a blood test at a doctor’s office or a commercial facility. The health care professional sends the blood sample to a lab for testing. Blood tests can show a high white blood cell count, a sign of infection. Blood tests also may show dehydration or fluid and electrolyte imbalances.
Urinalysis. Urinalysis is testing of a urine sample. You will provide a urine sample in a special container in a doctor’s office, a commercial facility, or a hospital. Health care professionals can test the urine in the same location or send it to a lab for testing. Doctors use urinalysis to rule out a urinary tract infection or a kidney stone.
Pregnancy test. For women, health care professionals also may order blood or urine samples to check for pregnancy.
Imaging tests
Doctors use imaging tests to confirm the diagnosis of appendicitis or find other causes of pain in the abdomen.
Abdominal ultrasound. In an ultrasound, a health care professional uses a device, called a transducer, to bounce safe, painless sound waves off of your organs to create an image of their structure. He or she can move the transducer to different angles to examine different organs.
In an abdominal ultrasound, a health care professional applies a gel to your abdomen and moves a hand-held transducer over your skin. A health care professional performs this procedure in a doctor’s office, an outpatient center, or a hospital, and you don’t need anesthesia.
A radiologist reviews the images, which can show signs of:
- a blockage in your appendiceal lumen
- a burst appendix
- inflammation
- other sources of abdominal pain
Health care professionals use an ultrasound as the first imaging test for possible appendicitis in infants, children, young adults, and pregnant women.
Magnetic resonance imaging (MRI). MRI machines use radio waves and magnets to produce detailed pictures of your body’s internal organs and soft tissues without using x-rays.
A health care professional performs the procedure in an outpatient center or a hospital. A radiologist reviews the images. Patients don’t need anesthesia, although a health care professional may give light sedation, taken by mouth, to children and people with a fear of small spaces. A health care professional may inject a special dye, called contrast medium, into your body.
In most cases, you’ll lie on a table that slides into a tunnel-shaped device. The tunnel may be open ended or closed at one end.
An MRI can show signs of:
- a blockage in your appendiceal lumen
- a burst appendix
- inflammation
- other sources of abdominal pain
When diagnosing appendicitis and other sources of abdominal pain, doctors can use an MRI as a safe, reliable alternative to a computerized tomography (CT) scan 4.
CT scan. CT scans use x-rays and computer technology to create images.
A health care professional may give you a solution to drink and an injection of contrast medium. You’ll lie on a table that slides into a tunnel-shaped device that takes the x-rays. X-ray technicians perform CT scans in an outpatient center or a hospital. Radiologists review the images.
Patients don’t need anesthesia, although health care professionals may give children a sedative to help them fall asleep for the test.
A CT scan of the abdomen can show signs of inflammation, such as:
- an enlarged or a burst appendix
- an appendiceal abscess
- a blockage in your appendiceal lumen
Women of childbearing age should have a pregnancy test before having a CT scan. The radiation from CT scans can be harmful to a developing fetus.
Appendicitis treatment
Doctors typically treat appendicitis with surgery to remove the appendix. Surgeons perform the surgery in a hospital with general anesthesia. Your doctor will recommend surgery if you have continuous abdominal pain and fever, or signs of a burst appendix and infection. Prompt surgery decreases the chance that your appendix will burst.
Health care professionals call the surgery to remove the appendix an appendectomy. A surgeon performs the surgery using one of the following methods:
- Laparoscopic surgery. During laparoscopic surgery, surgeons use several smaller incisions and special surgical tools that they feed through the incisions to remove your appendix. Laparoscopic surgery leads to fewer complications, such as hospital-related infections, and has a shorter recovery time.
- Laparotomy. Surgeons use laparotomy to remove the appendix through a single incision in the lower right area of your abdomen.
After surgery, most patients completely recover from appendicitis and don’t need to make changes to their diet, exercise, or lifestyle. Surgeons recommend that you limit physical activity for the first 10 to 14 days after a laparotomy and for the first 3 to 5 days after laparoscopic surgery.
What if the surgeon finds a normal appendix ?
In some cases, a surgeon finds a normal appendix during surgery. In this case, many surgeons will remove it to eliminate the future possibility of appendicitis. Sometimes surgeons find a different problem, which they may correct during surgery.
Can doctors treat appendicitis without surgery ?
Some cases of mild appendicitis may be cured with antibiotics alone. All patients suspected of having appendicitis are treated with antibiotics before surgery, and some patients may improve completely before surgery is performed.
How do doctors treat complications of a burst appendix ?
Treating the complications of a burst appendix will depend on the type of complication. In most cases of peritonitis, a surgeon will remove your appendix immediately with surgery. The surgeon will use laparotomy to clean the inside of your abdomen to prevent infection and then remove your appendix. Without prompt treatment, peritonitis can cause death.
A surgeon may drain the pus from an appendiceal abscess during surgery or, more commonly, before surgery. To drain an abscess, the surgeon places a tube in the abscess through the abdominal wall. You leave the drainage tube in place for about 2 weeks while you take antibiotics to treat infection. When the infection and inflammation are under control, about 6 to 8 weeks later, surgeons operate to remove what remains of the burst appendix.
Prognosis of appendicitis
Without surgery or antibiotics (e.g, in a remote location or historically), the mortality rate for appendicitis is > 50% 2.
With early surgery, the mortality rate is < 1%, and convalescence is normally rapid and complete 2. With complications (rupture and development of an abscess or peritonitis) and/or advanced age, the prognosis is worse: Repeat operations and a long convalescence may follow 2.
Appendicitis in kids
Early adolescence is prime time for appendicitis, a potentially serious inflammation of the appendix.
In adolescents, appendicitis begins as a vague stomachache near the navel 5. Then patients feel it in the lower part of the right side of the abdomen. The appendicitis pain is often described as a peculiar combination of pressure and fullness.
Symptoms that Suggest Appendicitis may Include 5:
- Persistent abdominal pain that migrates from the midsection to the right lower abdomen. “Pain is unlike any other kind of pain”
- Nausea and vomiting
- Constipation
- Gas pain
- Diarrhea
- Low fever, beginning after other symptoms
- Tenderness in the right lower abdomen
- Abdominal swelling
- Elevated white blood cell count
- Appetite loss
If You Think You Have Appendicitis
- Get help from your doctor right away if you suspect that you have appendicitis, because this is a surgical emergency. Quick treatment of appendicitis can help prevent complications and get you back on your feet.
How Appendicitis Is Diagnosed in Kids
Physical examination and thorough medical history, plus one or more of the following procedures:
- White blood cell count
- Urinalysis, to rule out a urinary-tract infection
- Ultrasound
- Lower GI series (barium enema)
- CT scan
- Exploratory laparoscopic surgery
How Appendicitis Is Treated in Kids
Surgery: Appendicitis can be difficult to diagnose definitely. Therefore, your physician may not schedule the appendectomy until the symptoms have progressed somewhat. Conventional “open” surgery usually requires a two day hospital stay, barring complications, and leaves youngsters with a small scar, but completely cured.
Prevention for Appendicitis
Youngsters should be encouraged to follow these basic guidelines for a healthy digestive tract:
- Eat at regular hours.
- Drink lots of water (at least eight cups of water or other liquid every day).
- Keep physically active.
- Chew food slowly and thoroughly before swallowing.
- Use aspirin and nonsteroidal anti-inflammatory medications sparingly; these drugs can irritate the fragile gastrointestinal lining.
- Don’t smoke; cigarettes, too, contribute to ulcers.
- Listen to your body! Don’t suppress the urge to move your bowels.
- Try not to strain during bowel movements.
- And most important, even with a busy schedule regular meals should be taken daily. Attempts should be made to have at least some of these meals sitting around a table preferably allowing time to talk, chew and digest. This will not only help your teens’ gut, but help the whole family stay connected.
- Appendicitis. The National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/appendicitis[↩]
- Appendicitis. Merck Manual. http://www.merckmanuals.com/professional/gastrointestinal-disorders/acute-abdomen-and-surgical-gastroenterology/appendicitis[↩][↩][↩][↩]
- What are the symptoms of appendicitis ? The National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/appendicitis[↩][↩]
- Heverhagen J, Pfestroff K, Heverhagen A, Klose K, Kessler K, Sitter H. Diagnostic accuracy of magnetic resonance imaging: a prospective evaluation of patients with suspected appendicitis (diamond). Journal of Magnetic Resonance Imaging. 2012;35:617–623.[↩]
- Appendicitis in Teens. American Academy of Pediatrics. https://www.healthychildren.org/English/health-issues/conditions/abdominal/Pages/Appendicitis-in-Teens.aspx[↩][↩]





