Contents
What is arthritis
Arthritis literally means joint inflammation 1. Although joint inflammation is a symptom or sign rather than a specific diagnosis, the term arthritis is often used to refer to any disorder that affects the joints.
Joints are places where two bones meet, such as your elbow or knee.
There are different types of arthritis. In some diseases in which arthritis occurs, other organs, such as your eyes, heart, or skin, can also be affected.
Fortunately, current treatments allow most people with arthritis to lead active and productive lives.
Figure 1. Arthritis
 Types of arthritis
Types of arthritis
There are several types of arthritis. Common ones include:
- Ankylosing Spondylitis is arthritis that affects the spine. It often involves redness, heat, swelling, and pain in the spine or in the joint where the bottom of the spine joins the pelvic bone.
- Gout is caused by uric acid crystals that build up in the joints. It usually affects the big toe, but many other joints may be affected.
- Juvenile Arthritis is the term used to describe arthritis in children. Arthritis is caused by inflammation of the joints.
- Osteoarthritis usually comes with age and most often affects the fingers, knees, and hips. Sometimes osteoarthritis follows a joint injury. For example, you might have badly injured your knee when young and develop arthritis in your knee joint years later.
- Psoriatic Arthritis can occur in people who have psoriasis (scaly red and white skin patches). It affects the skin, joints, and areas where tissues attach to bone.
- Reactive Arthritis is pain or swelling in a joint that is caused by an infection in your body. You may also have red, swollen eyes and a swollen urinary tract. Reactive arthritis can cause inflammation of the joints, eyes and urethra (the tube that urine passes through). It develops shortly after an infection of the bowel, genital tract or, less frequently, after a throat infection.
- Rheumatoid arthritis happens when the body’s own defense system doesn’t work properly. It affects joints and bones (often of the hands and feet), and may also affect internal organs and systems. You may feel sick or tired, and you may have a fever.
- Enteropathic arthritis – a form of chronic, inflammatory arthritis associated with inflammatory bowel disease (IBD), the two best-known types being ulcerative colitis and Crohn’s disease. About one in five people with Crohn’s or ulcerative colitis will develop enteropathic arthritis. The most common areas affected by inflammation are the peripheral (limb) joints and the spine.
- Cervical spondylosis – also known as degenerative osteoarthritis, cervical spondylitis affects the joints and bones in the neck, which can lead to pain and stiffness.
- Secondary arthritis – a type of arthritis that can develop after a joint injury and sometimes occurs many years afterwards.
Arthritis is also seen with other conditions. These include:
- Systemic Lupus Erythematosus (Lupus). Lupus happens when the body’s defense system harms the joints, heart, skin, kidneys, and other organs.
- Infection (septic arthritis) that gets into a joint and destroys the cushion between the bones.
- Fibromyalgia – causes pain in the body’s muscles, ligaments and tendons.
- Polymyalgia rheumatica – a condition that almost always affects people over 50 years of age, where the immune system causes muscle pain and stiffness, usually across the shoulders and tops of the legs. It can also cause joint inflammation.
What is Ankylosing Spondylitis
Ankylosing spondylitis is a type of arthritis that affects the spine 2. Ankylosing spondylitis often involves redness, heat, swelling, and pain in the spine or in the joint where the bottom of the spine (sacrum) joins the pelvic bone (ilium).
In some people, ankylosing spondylitis can also affect the shoulders, ribs, hips, knees, and feet. It can also affect areas where the tendons and ligaments attach to the bones. Sometimes it can affect the eyes, bowel, and very rarely, the heart and lungs.
Many people with ankylosing spondylitis have mild back pain that comes and goes. Others have severe pain that doesn’t go away. Sometimes the spine becomes stiff. In the worst cases, the swelling can cause two or more bones of the spine to fuse. This may stiffen the rib cage, making it hard to take a deep breath.
Who gets ankylosing spondylitis ?
A combination of genes may make it more likely you will get ankylosing spondylitis. The environment also probably plays a role. Men are about twice more likely than women to get ankylosing spondylitis.
What causes ankylosing spondylitis ?
- The cause of ankylosing spondylitis is unknown. It’s likely that genes (passed from parents to children) and the environment both play a role. The main gene associated with the risk for AS is called HLA-B27. Having the gene doesn’t mean you will get ankylosing spondylitis. Fewer than 1 of 20 people with HLA-B27 gets ankylosing spondylitis. Scientists recently discovered two more genes (IL23R and ERAP1) that, along with HLA-B27, make it more likely you will get ankylosing spondylitis.
Diagnosis of ankylosing spondylitis
Your doctor will give you a physical exam and ask you about your medical history in order to diagnose you with ankylosing spondylitis. Bone/joint scans and lab tests may help confirm a diagnosis.
Medical history
Your doctor will probably ask you the following questions during a medical history:
- How long have you had pain?
- Where is the pain in your back or neck? Are other joints affected?
- Is back pain better with exercise and worse after inactivity, such as when you first get up in the morning?
- Do you have other problems, such as eye problems or fatigue?
- Does anyone in your family have back problems or arthritis?
- Have you recently suffered from a stomach upset or diarrhea?
- Do you have any skin rashes such as psoriasis?
Physical exam
During the physical exam, your doctor will look for symptoms of ankylosing spondylitis. These include pain in the spine, pelvis, joint between the pelvis and spine, heels, or chest. Your doctor may ask you to move and bend in different directions. This is to check the flexibility of your spine. You will also be asked to breathe deeply. This is to check for rib stiffness caused by continued swelling of the joints where the ribs attach to the spine.
Bone and joint scans
Your doctor may confirm you have ankylosing spondylitis by taking pictures of your spine and of the joint between your spine and pelvic bone. Pictures are taken using x-rays or magnetic resonance imaging (MRI), which uses magnets and radio waves (not radiation). However, you may have the disease for years before changes show on x-rays. MRI may allow for earlier diagnosis, because it can show damage to soft tissues and bone before it can be seen on an x-ray. Both tests may also be used to see if the disease worsens.
Lab tests
Your blood may be tested for the HLA-B27 gene, which is present in most people with ankylosing spondylitis. The test is less useful if you are African American or from some Mediterranean countries, since you are less likely to have the gene even if you do have ankylosing spondylitis. The gene is also found in many people who do not have ankylosing spondylitis, and will never get it. Still, having the gene is one more indicator you have ankylosing spondylitis, when you also have symptoms and x-ray evidence of the disease.
Treatment of ankylosing spondylitis
There is no cure for ankylosing spondylitis, but some treatments relieve symptoms may possibly prevent the disease from getting worse. In most cases, treatment involves a combination of medication, exercise, and self-help measures. In some cases, surgery may be used to repair some of the joint damage caused by the disease.
You should work with your doctor to find the safest and most effective medications for you, which will likely include one or more of the following:
Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs relieve pain and inflammation, and are commonly used to treat ankylosing spondylitis. Examples include aspirin, ibuprofen, and naproxen.
Some NSAIDs are available over the counter, but others are available only with a prescription.
NSAIDs can have side effects, and some people seem to respond better to one NSAID than another. You should see your doctor on a regular basis if you take NSAIDs over a long period of time.
Corticosteroids. These strong inflammation-fighting drugs are similar to the cortisone made by your body. If NSAIDs alone do not control your joint swelling, your doctor may inject corticosteroids directly into the affected joints to bring quick but temporary relief. Injections may be given to the hip joint, knee joint, or joint between the spine and pelvic bone. Injections are not given in the spine.
Disease-modifying antirheumatic drugs (DMARDs). These drugs work in different ways. The most common DMARDs for ankylosing spondylitis are sulfasalazine and methotrexate.
Biologic agents. These medications block proteins involved in your body’s inflammatory response. Several biologics are approved by the Food and Drug Administration (FDA) for treating ankylosing spondylitis. These drugs are either injected or given intravenously (IV) and are often effective for ankylosing spondylitis when other treatments are not.
Surgery. Total joint replacement may be an option if ankylosing spondylitis causes severe joint damage that makes it difficult to do your daily activities. Your surgeon will remove the damaged joint and replace it with a man-made one made of metals, plastics, and/or ceramic materials. The most commonly replaced joints are the knee and hip.
There is also surgery to straighten the spine, if it has fused into a curved-forward position. This is generally considered a high-risk procedure, and it is only done in very rare cases. A surgeon who is highly experience in the procedure will cut through the spine so that it can be placed into a straighter up/down position. Hardware may be needed to hold the spine in its new position while it heals.
Home Remedies for ankylosing spondylitis
- Exercise: Besides seeing your doctor regularly and following your treatment plan, staying active is probably the best thing you can do for ankylosing spondylitis. Regular exercise can help relieve pain, improve posture, and maintain flexibility. Before beginning an exercise program, speak with your doctor or physical therapist about designing a program that’s right for you. Some helpful exercises include:
- Strengthening exercises, performed with weights or done by tightening muscles without moving the joints, build the muscles around your painful joints to better support them. Exercises that don’t require joint movement can be done even when your joints are painful and inflamed.
- You should gently straighten and bend your joints as far as they will comfortably go. This will improve movement flexibility and reduce stiffness in the painful joint. If the spine is painful and/or inflamed, exercises to stretch and extend the back can be helpful in preventing long-term disability.
- You may find it helpful to exercise in water.
- Diet: A healthy diet is good for everyone, and it may be very helpful if you have ankylosing spondylitis. There is no specific diet for people with ankylosing spondylitis, but keeping a healthy weight is important. It reduces stress on painful joints. Omega-3 fatty acids, found in coldwater fish (such as tuna and salmon), flax seeds, and walnuts, might reduce disease activity. This is still being studied.
- Posture: Another important thing you can do for yourself is to practice good posture. A good test for posture is to check yourself in a mirror. First, stand with a full-length mirror to your side and, if possible, turn your head to look at your profile. Next, imagine you have dropped a weighted string from the top of your head to the soles of your feet. Where does the string fall? If your posture is good, it should pass through your earlobe, the front of your shoulder, the center of your hip, behind your kneecap, and in front of your anklebone. If you are not standing that way already, practice holding your body that way in front of a mirror until you know well how it feels. Practicing good posture can help you avoid some of the complications that can occur with ankylosing spondylitis.
Arthritis pilates workout
A pilates exercise is suitable for people with arthritis.
This 32-minute class takes you through a series of gentle exercises to get your joints moving safely. You will need a cushion or a pillow for this class.
Regular pilates practice can help improve posture, muscle tone, balance and joint mobility, as well as relieve stress and tension.
What is Gout
Gout is a kind of arthritis that causes attacks of pain and stiffness in your joints, especially your big toe. Gout is caused by crystals of a substance called uric acid building up in your joints 3. Many people get their first attack of gout in one of their big toes, but it can also affect other joints in your feet, arms, and legs. In addition to pain, your joint may feel swollen, red, warm, and stiff.
Gout attacks often start suddenly at night. Intense pain and swelling may be bad enough to wake you up. Gout attacks are often triggered by stressful events, alcohol, drugs, or another illness.
Usually, a gout attack will get better in three to 10 days, even without treatment. After that, you may not have another attack for months or even years. Over time, however, your attacks may last longer and happen more often.
It can also cause lumps under the skin and kidney stones.
For some people, gout progresses through several stages:
- Hyperuricemia, when you have elevated levels of uric acid in your blood, but no symptoms.
- Acute gout, when you have an attack of intense pain and swelling in your joints. Acute attacks often come on at night and can be triggered by stress, drugs, alcohol, or another illness. An acute attack usually clears up within three to 10 days, even without treatment.
- Interval or intercritical gout, which is the time between gout attacks when you don’t have any symptoms.
- Chronic tophaceous gout, a late stage of gout when the condition may have permanently damaged your joints and kidneys. With proper treatment, most people do not reach this stage.
Who gets Gout
Millions of people get gout. It is especially common in men between the ages of 40 and 50. Women rarely develop gout before menopause.
You are more likely to get it if you:
- Have a family history of gout.
- Have had an organ transplant.
- Are a man.
- Are an adult.
- Are overweight.
- Drink alcohol.
- Eat foods that are rich in purines, a substance that breaks down into uric acid.
- Are exposed to lead in your environment.
Some health problems can also increase your risk of getting gout, including:
- Renal insufficiency, a condition in which your kidneys don’t eliminate enough waste.
- High blood pressure.
- Hypothyroidism, a condition in which your thyroid gland is underactive.
- A condition that cause your cells to turnover rapidly, such as psoriasis, hemolytic anemia, or some cancers.
- Kelley-Seegmiller syndrome or Lesch-Nyhan syndrome, two rare conditions in which your body either doesn’t have the enzyme that regulates uric acid levels or doesn’t have enough of that enzyme.
Some medications can increase your risk of getting gout, including:
- Diuretics, which help your body eliminate excess fluid.
- Salicylate-containing drugs, such as aspirin.
- Niacin, a vitamin.
- Cyclosporine, a medication used to treat some autoimmune diseases and people who have had organ transplants.
- Levodopa, a medication prescribed to treat Parkinson’s disease.
What causes gout ?
Gout is caused when a substance in your body called uric acid forms crystals in your joints. This causes pain, swelling, and other symptoms.
Uric acid comes from purines, which are found in your body’s tissues and many foods. When purines break down, they become uric acid. Uric acid normally dissolves in your blood and passes out of your body in urine. When too much of it builds up in your blood, however, it can form the crystals in your joints that cause gout.
Things that can cause uric acid to build up in the blood include:
- Your body increasing the amount of uric acid it makes.
- Your kidneys not getting rid of enough uric acid.
- Eating too many foods high in purines, such as liver, dried beans and peas, and anchovies.
Symptoms of gout
Gout causes pain in your joints, often in the big toe. Many people get their first attack of gout in one of their big toes, but it can also affect other joints in your feet, arms, and legs. In addition to pain, your joint may feel swollen, red, warm, and stiff.
Gout attacks often start suddenly at night. Intense pain and swelling may be bad enough to wake you up. Gout attacks are often triggered by stressful events, alcohol, drugs, or another illness.
Usually, a gout attack will get better in three to 10 days, even without treatment. After that, you may not have another attack for months or even years. Over time, however, your attacks may last longer and happen more often.
Diagnosis of gout
Gout can be difficult to diagnose because its symptoms are similar to several different conditions. Your doctor may test your blood to see if you have high levels of uric acid. They may also draw a sample of fluid from one of your painful joints to look for crystals of uric acid.
How is gout treated ?
Proper treatment can reduce the pain from gout attacks, help prevent future attacks, and prevent damage to your joints.
Your doctor may recommend medications to treat your pain. These may include:
- Anti-inflammatory drugs (NSAIDs), which can reduce pain and swelling.
- Corticosteroids, such as prednisone, which are strong anti-inflammatory hormones.
- Colchicine, which works best when taken within the first 12 hours of a gout attack.
- Other medications to reduce symptoms or reduce the build-up of uric acid in your blood.
Your doctor may also recommend diet and lifestyle changes, such as losing weight, since being overweight puts you at a greater risk of gout attacks, and cutting back on alcohol and foods that are high in purines.
In addition to taking medications recommended by your doctor, you can make some changes to your diet to help you have fewer gout attacks. As always, talk with your doctor before making any changes to your diet or medications.
Your doctor may recommend that you lose weight, if you are overweight, or drink less alcohol. You can also avoid eating foods with lots of purines, since they can increase your uric acid levels. Foods that are high in purines include:
- Anchovies.
- Asparagus.
- Beef kidneys.
- Brains.
- Dried beans and peas.
- Game meats.
- Gravy.
- Herring.
- Liver.
- Mackerel.
- Mushrooms.
- Sardines.
- Scallops.
- Sweetbreads.
What is Juvenile Arthritis
Juvenile arthritis is a term that describes arthritis in children. There are more than 100 arthritic or rheumatic diseases that may affect the joints but can also cause pain, swelling, and stiffness in other supporting structures of the body such as muscles, tendons, ligaments, and bones. Some rheumatic diseases can also affect other parts of the body, including various internal organs.
In the Unites States, juvenile arthritis and other rheumatic conditions affect nearly 294,000 children age 0 to 17.
- Children can develop almost all types of arthritis that affect adults, but the most common type that affects children is juvenile idiopathic arthritis.
Juvenile idiopathic arthritis is an umbrella term, or classification system, for all of the more specific types of chronic, or long-lasting, arthritis in children. These conditions used to fall under the term, juvenile rheumatoid arthritis, which is no longer used.
Types of Juvenile idiopathic arthritis
There are seven separate subtypes of juvenile idiopathic arthritis, each with distinct symptoms. However, with every subtype, a child will have arthritis symptoms of joint pain, swelling, tenderness, warmth, or stiffness that last for more than 6 continuous weeks.
The subtypes are:
- Systemic juvenile idiopathic arthritis (formerly known as systemic juvenile rheumatoid arthritis). Systemic means the arthritis can affect the whole body, rather than just a specific organ or joint. A child has arthritis with, or that was preceded by, a fever that has lasted for at least 2 weeks. The fever has come and gone, but spiked, or hit its highest temperature, for at least 3 days. The fever occurs with at least one or more of the following:
- Generalized enlargement of the lymph nodes.
- Enlargement of the liver or spleen.
- Inflammation of the lining of the heart (pericarditis) or the lungs (pleuritis).
- The characteristic rheumatoid rash, which is flat, pale, pink, and generally not itchy. The individual spots of the rash are usually the size of a quarter or smaller. They are present for a few minutes to a few hours, and then disappear without any changes in the skin. The rash may move from one part of the body to another.
- Oligoarticular juvenile idiopathic arthritis (formerly known as pauciarticular juvenile rheumatoid arthritis). A child has arthritis affecting one to four joints during the first 6 months of disease. Two subcategories of this type are:
- Persistent oligoarthritis, which means the child never has more than four joints involved throughout the disease course.
- Extended oligoarthritis, which means that more than four joints are involved after the first 6 months of the disease.
- Polyarticular juvenile idiopathic arthritis – rheumatoid factor negative (formerly known as polyarticular juvenile rheumatoid arthritis – rheumatoid factor negative). A child has arthritis in five or more joints during the first 6 months of disease, and all tests for rheumatoid factor (proteins produced by the immune system that can attack healthy tissue, which are commonly found in rheumatoid arthritis and juvenile arthritis) are negative.
- Polyarticular juvenile idiopathic arthritis – rheumatoid factor positive (formerly known as polyarticular rheumatoid arthritis – rheumatoid factor positive). A child has arthritis in five or more joints during the first six months of the disease. Also, at least two tests for rheumatoid factor, at least three months apart, are positive.
- Psoriatic juvenile idiopathic arthritis. A child has both arthritis and psoriasis (a skin disease), or has arthritis and at least two of the following:
- Inflammation and swelling of an entire finger or toe (this is called dactylitis)
- Nail pitting or splitting
- A first-degree relative with psoriasis.
- Enthesitis-related juvenile idiopathic arthritis. The enthesis is the point at which a ligament, tendon, or joint capsule attaches to the bone. If this point becomes inflamed, it can be tender, swollen, and painful with use. The most common locations are around the knee and at the Achilles tendon on the back of the ankle. A child is diagnosed with this condition if he or she has both arthritis and inflammation of an enthesitis site, or has either arthritis or enthesitis with at least two of the following:
- Inflammation of the sacroiliac joints (at the bottom of the back) or pain and stiffness in the lumbosacral area (in the lower back).
- A positive blood test for the human leukocyte antigen (HLA) B27 gene.
- Onset of arthritis in males after age six years.
- A first-degree relative diagnosed with ankylosing spondylitis, enthesitis-related arthritis, or inflammation of the sacroiliac joint in association with inflammatory bowel disease or acute inflammation of the eye.
- Undifferentiated arthritis. A child is said to have this condition if the signs and symptoms of the arthritis do not fulfill the criteria for one of the other six categories or if they fulfill the criteria for more than one category.
Symptoms of Juvenile arthritis
The most common symptom of all types of juvenile arthritis is persistent joint swelling, pain, and stiffness that is typically worse in the morning or after a nap. The pain may limit movement of the affected joint, although many children, especially younger ones, will not complain of pain.
One of the earliest signs of juvenile arthritis may be limping in the morning because of an affected knee.
Besides joint symptoms, children with systemic juvenile arthritis may have:
- A high fever that may appear and disappear very quickly.
- A skin rash that may appear and disappear very quickly.
- Swollen lymph nodes located in the neck and other parts of the body.
- Inflammation of internal organs, including the heart (fewer than half of the cases) and the lungs (very rarely).
What causes juvenile arthritis
Most forms of juvenile arthritis are autoimmune disorders in which the body’s immune system – which normally helps to fight off bacteria or viruses – mistakenly attacks some of its own healthy cells and tissues. The result is inflammation, marked by redness, heat, pain, and swelling. Inflammation can cause joint damage.
Doctors do not know why the immune system attacks healthy tissues in children who develop juvenile arthritis. Scientists suspect that it is a two-step process. First, something in a child’s genetic makeup gives him or her a tendency to develop juvenile arthritis; then an environmental factor, such as a virus, triggers the development of the disease.
Not all cases of juvenile arthritis are autoimmune, however. Recent research has shown that some people, such as many with systemic arthritis, have what is called an autoinflammatory condition. Although the two terms sound similar, the disease processes behind autoimmune and autoinflammatory disorders are different.
- Autoimmune Disorders
When the immune system is working properly, foreign invaders such as bacteria and viruses provoke the body to produce proteins called antibodies. Antibodies attach to these invaders so the immune system can recognize and destroy them. In an autoimmune reaction, the antibodies attach to the body’s own healthy tissues by mistake, signaling the body to attack them. Because they target the self, these proteins are called autoantibodies.
- Autoinflammatory Disorders
Like autoimmune disorders, autoinflammatory conditions also cause inflammation. And like autoimmune disorders, they also involve an overactive immune system. However, autoinflammation is not caused by autoantibodies. Instead, autoinflammation involves a more primitive part of the immune system that, in healthy people, causes white blood cells to destroy harmful substances. When this system goes awry, it causes inflammation for unknown reasons. Besides inflammation, autoinflammatory diseases often cause fever and rashes.
Treatment of juvenile arthritis
The main goals of treatment are to:
- Preserve a high level of physical and social functioning.
- Maintain a good quality of life.
To achieve these goals, doctors recommend treatments that:
- Reduce swelling.
- Maintain full movement in the affected joints.
- Relieve pain.
- Prevent, identify, and treat complications.
Most children with juvenile arthritis need a combination of medication and other treatments to reach these goals.
- Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs). Aspirin, ibuprofen, naproxen, and naproxen sodium are examples of NSAIDs. They are often the first type of medication doctors prescribe for juvenile arthritis. All NSAIDs work similarly by blocking substances called prostaglandins that add to inflammation and pain. However, each NSAID is a different chemical, and each has a slightly different effect on the body. For unknown reasons, some children seem to respond better to one NSAID than another. NSAIDs should only be used at the lowest dose possible for the shortest time needed.
You can buy some NSAIDs over the counter, while several others, including a subclass called COX-2 inhibitors, need a prescription.
All NSAIDs can have significant side effects, so consult your child’s doctor before giving any of them. Your child’s doctor should monitor your child if he or she takes NSAIDs regularly to control juvenile arthritis.
Side effects of NSAIDs include stomach problems; skin rashes; high blood pressure; fluid retention; and liver, kidney, and heart problems. The longer a person uses NSAIDs, the more likely he or she is to have side effects, ranging from mild to serious. Many other medicines cannot be taken when a person is taking NSAIDs because NSAIDs alter the way the body uses or eliminates these other medicines.
Disease-modifying antirheumatic drugs (DMARDs). If NSAIDs do not relieve symptoms of your child’s juvenile arthritis, the doctor may prescribe this type of medication. DMARDs slow the progression of juvenile arthritis, but because they may take weeks or months to relieve symptoms, they often are taken with an NSAID. Although there are many different types of DMARDs, many doctors prescribe one called methotrexate.
Researchers have learned that methotrexate is safe and effective for some children with juvenile arthritis whose symptoms are not relieved by other medications. Because children only need small doses of methotrexate for relief of arthritis symptoms, potentially dangerous side effects rarely occur. The most serious complication can be liver damage, which a doctor can help prevent with regular blood tests and check-ups. Careful monitoring for side effects is important for people taking methotrexate. When side effects are noticed early, the doctor can reduce the dose and eliminate the side effects.
Corticosteroids. If your child has very severe juvenile arthritis, stronger medicines may be needed to stop serious symptoms, such as inflammation of the sac around the heart (pericarditis). Corticosteroids, such as prednisone, may be added to the treatment plan to control severe symptoms. This medication can be given by IV (intravenous), mouth, or injection directly into a joint. Corticosteroids are powerful anti-inflammatory medicines. Corticosteroids can interfere with your child’s normal growth and can cause other side effects, such as a round face, weakened bones, and an increased chance of having infections. Once the medication controls severe symptoms, the doctor will reduce the dose gradually and, in time, stop it completely. It can be dangerous to stop taking corticosteroids suddenly. Carefully follow the doctor’s instructions about how to take or reduce the dose. For inflammation in one or just a few joints, injecting a corticosteroid compound into the affected joint or joints can often bring quick relief without the systemic side effects of oral or IV medication.
Biologic agents. If your child has received little relief from other medications, he or she may be given one of a newer class of medications called biologic response modifiers, or biologic agents. These are based on compounds made by living cells. Tumor necrosis factor (TNF) inhibitors are biologic agents that work by blocking the actions of TNF, a naturally occurring protein in the body that helps cause inflammation. Other biologic agents block other inflammatory proteins, such as interleukin-1 or immune cells called T cells. Different biologics tend to work better for the different subtypes of the disease.
All medicines can have side effects. Some medicines and side effects are mentioned in this publication. Some side effects may be more severe than others. You should review the package insert that comes with your medicine and ask your child’s health care provider or pharmacist if you have any questions about the possible side effects.
- Other Treatments
Physical therapy. A regular, general exercise program is an important part of a child’s treatment plan. Exercise can help to maintain muscle tone and preserve and recover the range of motion of the joints. A physiatrist (rehabilitation specialist) or a physical therapist can design an appropriate exercise program for your child. The specialist also may recommend using splints and other devices to help maintain normal bone and joint growth.
Complementary and alternative therapies. Many adults seek alternative ways of treating arthritis, such as special diets, supplements, acupuncture, massage, or even magnetic jewelry or mattress pads. Research shows that increasing numbers of children are using alternative and complementary therapies as well.
Although there is little research to support many alternative treatments, some people seem to benefit from them. If your child’s doctor feels the approach has value and is not harmful, you can incorporate it into the treatment plan. However, do not neglect regular health care or treatment of serious symptoms.
What is Osteoarthritis
Osteoarthritis is the most common type of arthritis and is seen especially among older people. It is sometimes called degenerative joint disease.
Osteoarthritis initially affects the smooth cartilage lining of the joint. This makes movement more difficult than usual, leading to pain and stiffness.
Once the cartilage lining starts to roughen and thin out, the tendons and ligaments have to work harder. This can cause swelling and the formation of bony spurs, called osteophytes.
Severe loss of cartilage can lead to bone rubbing on bone, altering the shape of the joint and forcing the bones out of their normal position.
The most commonly affected joints are those in the:
- hands
- spine
- knees
- hips
People with osteoarthritis usually have joint pain and stiffness. The most commonly affected joints are in the hands (ends of the fingers and thumbs), neck, lower back, knees, and hips. Unlike some other forms of arthritis, osteoarthritis does not affect the skin, lungs, eyes, or blood vessels. It can also occur in only one joint or can affect a joint on one side of the body much more severely.
Osteoarthritis affects each person differently. For some people, osteoarthritis is relatively mild and interferes little with day-to-day life. For others, it causes significant pain and disability. Joint damage usually develops gradually over years, although it could worsen quickly in some people.
What happens in osteoarthritis ?
Osteoarthritis damages cartilage, the tissue that covers the ends where two bones meet to form a joint. This allows the bones to rub together, causing pain, swelling, and loss of joint motion. Over time, the joint may lose its normal shape. Also, small bone growths, called osteophytes or bone spurs, may grow on the edges of the joint. Bits of bone or cartilage can also break off and float inside the joint space. This causes more pain and damage.
Who gets osteoarthritis ?
Osteoarthritis becomes more common with age. However, younger people can also develop it, usually as the result of a joint injury, an abnormal joint structure, or a genetic defect in joint cartilage.
Before age 45, more men than women have osteoarthritis. After age 45, it is more common in women. It is also more likely to occur in people who are overweight and in those with jobs that stress particular joints.
What causes Osteoarthritis ?
Osteoarthritis usually happens gradually over time. Some things that might make it more likely include:
- Being overweight.
- Getting older.
- Joint injury.
- Joints that are not properly formed.
- A genetic defect in joint cartilage.
What are the symptoms of osteoarthritis ?
Early in the disease, your joints may ache after physical work or exercise. Later on, joint pain may become more persistent. You may also experience joint stiffness, especially when you first wake up in the morning or have been in one position for a long time.
Joints often affected by osteoarthritis include:
- Hands: If your mother or grandmother has or had osteoarthritis in their hands, you’re at an increased risk of having it too. Women are more likely than men to have osteoarthritis in the hands. For most women, it develops after menopause.
- Knees: Stiffness, swelling, and pain in the knees can make it hard to walk, climb, and get in and out of chairs and bathtubs. Osteoarthritis in the knees can lead to disability.
- Hips: You might feel pain and stiffness in the hip joint or in the groin, inner thigh, buttocks, or even knees. Moving and bending may be limited, making daily activities such as dressing and putting on shoes a challenge.
- Spine: You may feel stiffness and pain in the neck or lower back. In some cases, arthritis-related changes in the spine can cause pressure on the nerves where they exit the spinal column, resulting in weakness, tingling, or numbness of the arms and legs. In severe cases, this can even affect bladder and bowel function.
How is Osteoarthritis treated ?
Treatment for osteoarthritis can include medications or surgery to reduce pain and improve functioning.
Medications commonly used in treating osteoarthritis include:
- Over-the-counter pain relievers such as acetaminophen.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to treat pain and inflammation. Ibuprofen and naproxen sodium, are available over the counter, whereas other NSAIDS are available by prescription only.
- Creams, rubs or sprays that are applied to the skin over sore joints to relieve pain.
- Prescription opioid pain relievers are sometimes prescribed when over-the-counter medications don’t work or a person may not be able to take NSAIDs.
- Corticosteroids are strong inflammation-fighting drugs that can be injected into the joint to temporarily relive pain. This type of treatment is usually not recommended for more than two to four treatments per year. These types of drugs are not typically given by mouth to treat osteoarthritis, unless treating inflammatory flares.
- Hyaluronic acid substitutes (viscosupplements) are injected into the knee to replace a normal component of the joint involved in lubrication and nutrition.
Surgery may be a factor after considering a variety of factors, including your age, occupation, level of disability, pain intensity, and the degree to which arthritis interferes with your lifestyle. Surgeries can include one or more of the following:
- Arthroscopic debridement: Removal of loose pieces of bone and cartilage from the joint.
- Osteotomy: Repositioning of bones.
- Joint resurfacing: Smoothing out bones.
- Prostheses are artificial joints that replace affected joints. The artificial joints can be made from metals, high-density plastic, or ceramic material. Artificial joints can last 10 to 15 years or longer. In some cases, your surgeon may replace only the damaged part of the knee joint, leaving undamaged parts of the joint in place.
Transcutaneous electrical nerve stimulation (TENS) directs mild electric pulses to nerve endings that lie beneath the skin in the painful area. It seems to work by blocking pain messages to the brain and by changing pain perception.
Alternative therapies for osteoarthritis can include:
- Massage can increase blood flow and bring warmth to a stressed area. However, arthritis-stressed joints are sensitive, so the therapist must be familiar with the problems of the disease.
- Acupuncture uses thin needles to relieve pain and restore health. Scientists think the needles stimulate the release of natural, pain-relieving chemicals produced by the nervous system.
What is Psoriatic Arthritis
Psoriatic arthritis is a form of arthritis (joint inflammation) that can occur in people who have psoriasis (scaly red and white skin patches) 4.
What happens in psoriatic arthritis ?
Psoriatic arthritis affects the joints, and areas where muscles and ligaments attach to bone. Typically, skin disease precedes the arthritis, sometimes by several years. In some cases, arthritis occurs first.
The joints most commonly affected are:
- The outermost joints of the fingers or toes.
- Wrists.
- Knees.
- Ankles.
- Lower back.
Who gets psoriatic arthritis
Anyone can be affected by psoriatic arthritis, but certain risk factors are associated with a greater risk for the disease:
- Race: Psoriatic arthritis is more common in Caucasians than African Americans or Asian Americans.
- Age: The disease typically begins between the ages of 30 and 50, but can begin in childhood.
What causes psoriatic arthritis
No one knows what causes psoriatic arthritis. People with the condition often have a family member with psoriasis or arthritis, suggesting that genetics are involved. In people with the disease gene, an infection may activate the immune system to trigger the development of psoriatic arthritis. This indicates that environment is also involved.
Symptoms of psoriatic arthritis
Symptoms of psoriatic arthritis include:
- Joint pain and swelling that may come and go and may be accompanied by redness and warmth.
- Tenderness where muscles or ligaments attach to the bones, particularly the heel and bottom of the foot.
- Inflammation of the spinal column, called spondylitis, which can cause pain and stiffness in the neck and lower back.
- Morning stiffness.
- Reduced range of motion of the joints.
- Painful, sausage-like swelling of the fingers and/or toes.
- Thickness and reddening of the skin with flaky, silver white patches called scales.
- Pitting of the nails or separation from the nail bed.
- Tiredness.
- Pink eye, inflammation, or infection of the membrane lining the eyelid and part of the eyeball.
Treatment for psoriatic arthritis
Treatment for psoriatic arthritis depends on its severity. Milder forms of the disease may be treated by:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to treat pain and inflammation. Ibuprofen and naproxen sodium, are available over the counter, whereas other NSAIDS are available by prescription only.
- Corticosteroids, strong inflammation-fighting drugs, may be injected directly into the affected joint(s).
Forms of the disease that are persistent or affect multiple joints may be treated by:
- Disease-modifying anti-rheumatic drugs (DMARDs) that slow or stop the immune system from attacking the joints and causing damage.
- Anti-tumor necrosis factor (TNF) agents.
What is Reactive Arthritis
Reactive arthritis is a type of spondyloarthritis, a group of disorders that can cause inflammation throughout the body (especially in the knees, feet, toes, hips and ankles). Reactive arthritis is associated with inflammation of the joints, eyes, and urinary tract and its associated genital structures. These symptoms may occur alone, together, or not at all. Any of these symptoms may be so mild that you may not notice them.
Reactive arthritis usually develops after you’ve had an infection, particularly a sexually transmitted infection or food poisoning.
The symptoms of reactive arthritis usually last several months, it clears up within a few months and causes no long-term problems. The symptoms can return or develop into a long-term disease in a small percentage of people.
Men and women of any age can get it, but it’s more common in men, and people aged between 20 and 40.
Reactive arthritis is not contagious; that is, a person with the disorder cannot pass the arthritis on to someone else. However, the bacteria that can trigger reactive arthritis can be passed from person to person.
Most people with reactive arthritis recover fully from the initial flare of symptoms. They may have mild arthritis symptoms that last up to a year, although symptoms don’t usually interfere with daily activities. Some people will have long-term, mild arthritis. A few patients will have long-term, severe arthritis that is difficult to control with treatment and may cause joint damage.
Some patients will re-develop symptoms, such as back pain and arthritis, after the initial flare has disappeared. These relapses may be caused by reinfection.
What happens in reactive arthritis ?
In many patients, reactive arthritis is triggered by an infection in the bladder, urethra, or vagina that is often transmitted through sexual contact (sexually transmitted infection). Another form of reactive arthritis is caused by an intestinal infection from eating food or handling substances that are contaminated with bacteria.
Who gets Reactive arthritis
Men are nine times more likely than women to develop reactive arthritis caused by sexually acquired infections. However, women and men are equally likely to develop reactive arthritis as a result of food-borne infections. Women with reactive arthritis often have milder symptoms than men.
What are the symptoms of reactive arthritis ?
Symptoms of reactive arthritis may be so mild that you do not notice them. They can come and go over a period of weeks or months. In a few people, symptoms can turn into a long-term disease.
Symptoms of reactive arthritis can include:
- Joint swelling and pain.
- Inflammation of the urinary and genital tract – causing pain when peeing, or discharge from the penis or vagina
- Redness and swelling of the eyes – causing eye pain, sticky discharge, conjunctivitis and, rarely, inflammation of the eye (iritis)
- Mouth sores and skin rashes.
See an eye specialist or go to emergency room as soon as possible if one of your eyes becomes very painful and the vision becomes misty. This could be a symptom of iritis – and the sooner you get treatment, the more successful it is likely to be.
Most people will not get all the above symptoms. They can come on suddenly but usually start to develop a few days after you get an infection somewhere else in your body.
What causes reactive arthritis
In many patients, reactive arthritis is triggered by a bacterial infection in the bladder, urethra, or vagina that is often transmitted through sexual contact. Another form of reactive arthritis is caused by an intestinal infection from eating food or handling substances that are contaminated with bacteria. Reactive arthritis typically begins within two to four weeks after infection.
Doctors do not know exactly why some people exposed to these bacteria develop reactive arthritis and others do not. One gene, human leukocyte antigen (HLA) B27, increases a person’s chance of developing reactive arthritis. However, inheriting the HLA B27 gene does not necessarily mean you will get reactive arthritis.
A person with the disorder cannot pass the arthritis on to someone else. However, the bacteria that can trigger reactive arthritis can be passed from person to person.
Diagnosis for reactive arthritis
Although there is no single test for reactive arthritis, your doctor may do the following to diagnosis you with the condition:
- Medical history to learn about your symptoms and any previous medical problems or infections.
- Blood tests to:
- Detect the genetic factor HLA B27. A positive result does not always mean that you the disorder.
- Confirm inflammation somewhere in the body.
- Rule out other conditions.
- Take samples from the throat, urethra, cervix, urine, stool, or joints to test for bacteria.
- X-rays to help diagnose reactive arthritis and to rule out other causes of arthritis.
Treatment for reactive arthritis
Although there is no cure for reactive arthritis, certain medications can relieve symptoms of the disorder:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to treat pain and inflammation. Ibuprofen and naproxen sodium are available over the counter, whereas other NSAIDS are available by prescription only.
- Corticosteroids, strong inflammation-fighting drugs, may be applied directly on skin ulcers, or injected into a joint to temporarily relieve pain. Because they are potent drugs, your doctor will seek the lowest dose required to achieve the desired benefit.
- Antibiotics eliminate the bacterial infection that triggered reactive arthritis.
- Immunosuppressive medicines or biologics to stop the immune system from attacking the tissues.
What is Rheumatoid Arthritis
Rheumatoid arthritis, is an inflammatory disease that causes pain, swelling, stiffness, and loss of function in the joints. It occurs when the immune system, which normally helps protect the body from infection and disease, attacks the membrane lining the joints.
Rheumatoid arthritis is different from other kinds of arthritis in several ways. For example:
- Rheumatoid arthritis generally occurs in a symmetrical pattern, meaning that if one knee or hand is involved, the other one also is.
- Rheumatoid arthritis often affects the wrist joints and the finger joints closest to the hand.
- Rheumatoid arthritis can also affect other parts of the body besides the joints, such as the heart, lungs, blood, nerves, eyes, and skin.
- People with rheumatoid arthritis may have fatigue, occasional fevers, and a loss of appetite.
Fortunately, current treatments allow most people with the disease to lead active and productive lives. In recent years, research has led to a new understanding of rheumatoid arthritis, which may result in even better ways to treat the disease.
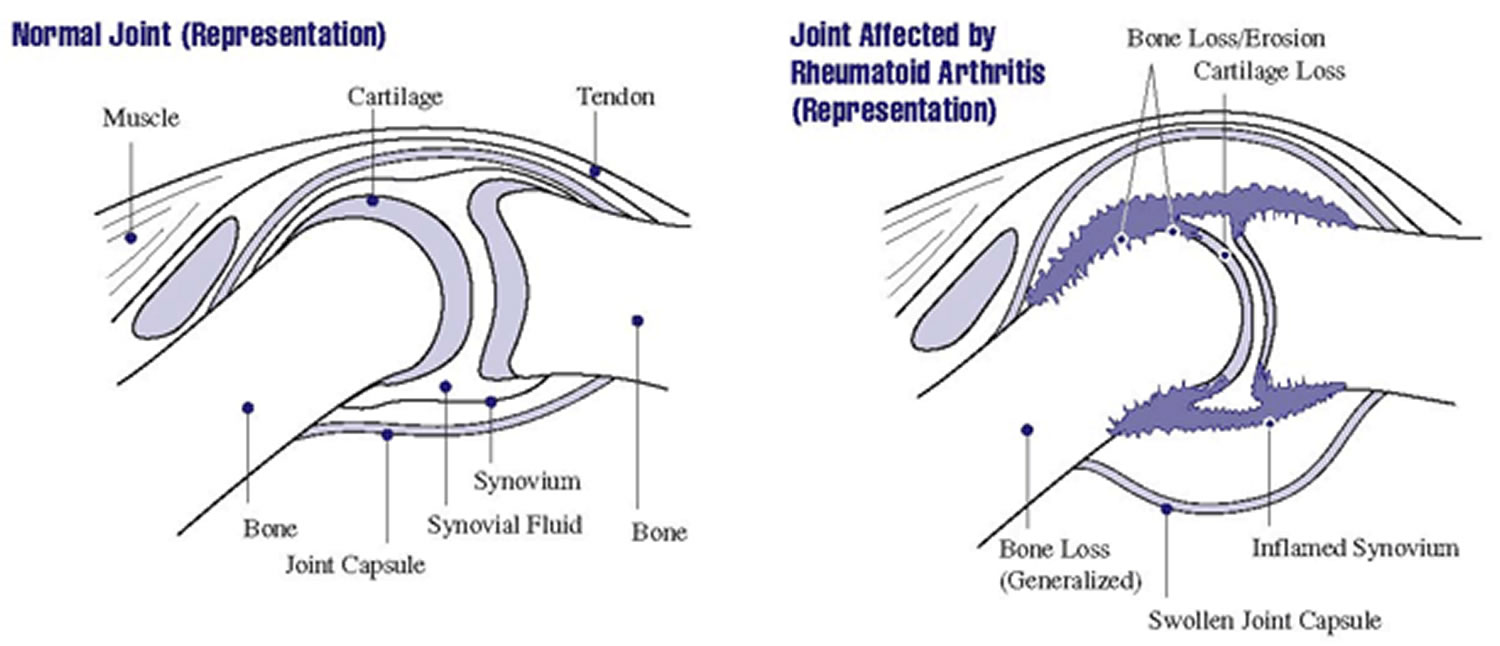
What happens in rheumatoid arthritis ?
Rheumatoid arthritis is an autoimmune disease (auto means self). The immune system attacks joint tissues for unknown reasons. Rheumatoid arthritis occurs when:
- White blood cells in the immune system travel to tissue that surrounds the joint, called synovium, and cause inflammation.
- The normally thin synovium becomes thick, making the joint swollen, red, painful, and sometimes warm to the touch.
- As rheumatoid arthritis progresses, the inflamed synovium invades and destroys the cartilage and bone within the joint.
- The surrounding muscles, ligaments, and tendons that support and stabilize the joint become weak and don’t work normally. This may cause the bone and cartilage to break down. This leads to pain and joint damage.
- People with rheumatoid arthritis can also develop problems with other tissues and organs in their body.
Researchers now believe that rheumatoid arthritis begins to damage the bones within the joint during the first year or two that a person has the disease. This is one reason why early diagnosis and treatment are so important.
Who gets Rheumatoid arthritis
About 1.5 million people, or about 0.6 percent of the U.S. adult population, have rheumatoid arthritis. Rheumatoid arthritis is more common among certain groups:
- Age: The disease often begins in middle age and is more common in older adults, between 40 and 50 years old. However, older teenagers and young adults may also get the disease. Children and younger teenagers may be diagnosed with juvenile idiopathic arthritis, a condition related to rheumatoid arthritis.
- Sex: Like some other forms of arthritis, rheumatoid arthritis is more common among women than men. About two to three times as many women as men have the disease.
- Race/Ethnicity: Rheumatoid arthritis occurs in all races and ethnic groups.
What are the symptoms of rheumatoid arthritis ?
Symptoms of rheumatoid arthritis, which can range from mild to severe, include:
- Tender, warm, swollen joints.
- Swollen joints on both sides of the body, such as in both your right and left wrist.
- Swollen joints often in the wrist and finger joints closest to the hand.
- Swollen joints sometimes in other joints, including the neck, shoulders, elbows, hips, knees, ankles, and feet.
- Feeling tired and having low energy.
- Fevers.
- Pain and stiffness lasting for more than 30 minutes in the morning or after a long rest.
- Symptoms that last for many years.
What causes rheumatoid arthritis
Scientists still do not know exactly what causes the immune system to turn against the body’s own tissues in rheumatoid arthritis. Research over the last few years has begun to piece together the factors involved. These include:
Genetic (inherited) factors: Scientists have discovered that certain genes known to play a role in the immune system are associated with rheumatoid arthritis. However, some people who have these particular genes never develop the disease. This suggests that genes are not the only factor in the development of rheumatoid arthritis. What is clear, however, is that more than one gene is involved in determining whether a person develops rheumatoid arthritis and how severe the disease will become.
Environmental factors: Many scientists think that something must occur to trigger the disease process in people whose genetic makeup puts them at risk for rheumatoid arthritis. Many factors have been suggested, but a specific one has not been confirmed.
Other factors: Some scientists also think that hormonal factors, such as shortages or changes in certain sex hormones, may play a role when genetic and environmental factors also are involved. Scientists believe this because:
- Women are more likely to develop rheumatoid arthritis than men.
- The disease may improve during pregnancy and flare after pregnancy.
- Breastfeeding may worsen the disease.
We do not know all the answers, but we do know that rheumatoid arthritis develops from an interaction of many factors. Researchers are trying to understand these factors and how they work together.
Diagnosis of Rheumatoid arthritis
Rheumatoid arthritis can be difficult to diagnose in its early stages for several reasons:
- There is no single test for the disease.
- Symptoms differ from person to person and can be more severe in some people than in others.
- Symptoms can be similar to those of other types of arthritis and joint conditions, and it may take some time for other conditions to be ruled out.
- The disease develops over time, and only a few symptoms may be present in the early stages.
As a result, doctors use a variety of the following tools to diagnose the disease and to rule out other conditions.
Medical History
The doctor will begin by asking you to describe your symptoms, when and how they started, and how they have changed over time. The doctor will also ask about any other medical problems you and close family members have and about any medications you’re taking. Answers to these questions can help the doctor make a diagnosis and understand the impact the disease has on your life.
Physical Examination
The doctor will:
- Check your reflexes and general health, including muscle strength.
- Examine bothersome joints and watch how you walk, bend, and carry out activities of daily living.
- Look at your skin for a rash.
- Listen to your chest for signs of inflammation in the lungs.
Laboratory Tests
A number of lab tests may be useful in confirming a diagnosis of rheumatoid arthritis. Some of the common tests include:
- Rheumatoid factor (RF): This blood test checks for RF, an antibody most people with rheumatoid arthritis eventually have in their blood. (An antibody is a special protein made by the immune system that normally helps fight invaders in the body.) Not all people with rheumatoid arthritis test positive for RF, and some people test positive for RF but never develop the disease. RF also can be positive in some other diseases. However, a positive RF in a person who has symptoms consistent with rheumatoid arthritis can be useful in confirming a diagnosis. Also, high levels of RF are associated with more severe rheumatoid arthritis.
- Anti-CCP antibodies: This blood test detects antibodies to cyclic citrullinated peptide (anti-CCP). This test is positive in most people with rheumatoid arthritis and can even be positive years before rheumatoid arthritis symptoms develop. When used with the RF, this test’s results are very useful in confirming a rheumatoid arthritis diagnosis.
- Others: Other common blood tests include:
- White blood cell count.
- Blood test for anemia, which is common in rheumatoid arthritis.
- Erythrocyte sedimentation rate (often called the sed rate), which measures inflammation in the body.
- C-reactive protein, another common test for inflammation that is useful both in making a diagnosis and monitoring disease activity and response to anti-inflammatory therapy.
Imaging Tests
Doctors use x-rays to see the degree of joint damage. They are not useful in the early stages of rheumatoid arthritis before damage is evident. Doctors may use them to rule out other causes of joint pain. X-rays may also be used later to monitor the progression of the disease. Magnetic resonance imaging (MRI) and ultrasound may be useful in identifying the early stages of rheumatoid arthritis and can help determine the severity of the disease.
Treatment for rheumatoid arthritis
Doctors use a variety of approaches to treat rheumatoid arthritis. They may be used in combination and at different times during the course of the disease. Your doctor will choose treatments based on your situation.
No matter which treatment is chosen, the goals are the same:
- Relieve pain.
- Reduce inflammation.
- Slow down or stop joint damage.
- Improve well-being and ability to function.
To treat rheumatoid arthritis, doctors may suggest:
- Medications.
- Surgery.
- Routine monitoring and ongoing care.
- Complementary therapies.
Medications
Most people who have rheumatoid arthritis take medications. Studies show that early treatment with powerful drugs and drug combinations instead of one medication alone may be more effective in reducing or preventing joint damage than beginning with aspirin or other pain relievers. If you have persistent rheumatoid arthritis symptoms, see a doctor familiar with the disease and its treatment to reduce the risk of damage.
Many of the drugs used to treat rheumatoid arthritis reduce the inflammation that can cause pain and joint damage. However, inflammation is also one way the body fights infection and disease. But the level of risk is hard to judge because infections and cancer can occur in people with rheumatoid arthritis who are not on treatment. It is important to talk with your doctor about these risks.
Pain Relief and Anti-Inflammatory Drugs
Your doctor may prescribe some medications (analgesics) that only help with pain relief. Others, such as corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), can reduce inflammation.
Disease-Modifying Anti-Rheumatic Drugs (DMARDS)
DMARDs may to slow the course of the disease. Common DMARDs your doctor may prescribe include:
- Hydroxychloroquine.
- Leflunomide.
- Methotrexate.
- Sulfasalazine.
Other DMARDs, called biologic response modifiers, may be used if your disease is more severe. These are genetically engineered medications that help reduce inflammation and damage to the joints by interrupting the inflammatory process. Currently, several biologic response modifiers are approved for rheumatoid arthritis, including:
- Abatacept.
- Adalimumab.
- Anakinra.
- Certolizumab.
- Etanercept.
- Golimumab.
- Infliximab.
- Rituximab.
- Tocilizumab.
Another DMARD, tofacitinib, is from a new class of drugs called jak kinase (JAK) inhibitors. It fights inflammation from inside the cell.
Surgery
The primary purpose of surgery is to reduce pain, improve the affected joint’s function, and improve your ability to perform daily activities.
Surgery is not for everyone. Talk with your doctor and together decide what is the right choice for you. Discuss:
- Your overall health.
- The condition of the joint or tendon that will be operated on.
- The reason for, and the risks and benefits of the surgery.
Routine Monitoring and Ongoing Care
Regular medical care is important to monitor the course of the disease, determine the effectiveness and any negative effects of medications, and change therapies as needed.
Monitoring typically includes regular visits to the doctor. It also may include blood, urine, and other lab tests and x-rays.
Good communication between you and your doctor is necessary for effective treatment. Talking to the doctor regularly can help ensure that you receive:
- Necessary exercise and pain management programs.
- Necessary and appropriate medications.
- Information about surgical options if necessary.
Another factor to discuss with your doctor is the risk of osteoporosis, which is a condition in which bones become weakened and fragile. Having rheumatoid arthritis increases your risk of developing osteoporosis, particularly if you take corticosteroids. You may want to discuss with your doctor the potential benefits of calcium and vitamin D supplements or other osteoporosis treatments.
Complementary Therapies
Special diets, vitamins, and other complementary therapies are sometimes suggested to treat rheumatoid arthritis.
Research shows that some of these approaches, such as taking fish oil supplements, may help reduce inflammation. However, few, if any controlled scientific studies have been conducted on complementary approaches, and some studies have found no definite benefit to these therapies.
As with any therapy, you should discuss the benefits and risks with your doctor before beginning any complementary or new type of therapy. However, it is important not to neglect regular health care.
What is Systemic Lupus Erythematosus (Lupus)
Systemic lupus erythematosus (lupus) is a disease that can damage many parts of the body, such as the joints, skin, kidneys, heart, lungs, blood vessels, and brain. You can’t catch lupus from another person.
If you have lupus you will have periods of illness (flares) and periods of wellness (remission).
What happens in lupus ?
Lupus occurs when the immune system, which normally helps protect the body from infection and disease, attacks different parts of the body.
Who gets systemic lupus erythematosus (lupus) ?
We know that many more women than men have systemic lupus erythematosus (lupus). Lupus is more common in African American women than in Caucasian women and is also more common in women of Hispanic, Asian, and Native American descent. African American and Hispanic women are also more likely to have active disease and serious organ system involvement. In addition, lupus can run in families, but the risk that a child or a brother or sister of a patient will also have lupus is still quite low.
Although systemic lupus erythematosus (lupus) usually first affects people between the ages of 15 and 45 years, it can occur in childhood or later in life as well.
What causes systemic lupus erythematosus (lupus)
No one completely understands what causes systemic lupus erythematosus (lupus). Studies suggest that a number of different genes may determine your risk for developing the disease.
Some environmental factors also appear to play a role in lupus. In particular, scientists are studying the effects of sunlight, stress, hormones, cigarette smoke, certain drugs, and viruses.
Symptoms of systemic lupus erythematosus (lupus)
Each person with systemic lupus erythematosus (lupus) has slightly different symptoms that can range from mild to severe. You may have symptoms in only one or in many parts of your body. Symptoms may also come and go over time.
Some of the most common symptoms of lupus include:
- Painful or swollen joints (arthritis).
- Unexplained fever.
- Extreme fatigue.
- Red rashes, most often on the face.
- Chest pain upon deep breathing.
- Hair loss.
- Sensitivity to the sun.
- Mouth sores.
- Pale or purple fingers and toes from cold and stress.
- Swollen glands.
- Swelling in the legs or around the eyes.
Other symptoms could include:
- Anemia (a decrease in red blood cells).
- Kidney inflammation, which typically requires drug treatment to prevent permanent damage.
- Headaches, dizziness, depression, confusion, or seizures if the disease affects the central nervous system.
- Inflammation of the blood vessels.
- Decreased number of white blood cells or platelets.
- Increased risk of blood clots.
- Inflammation of the heart or the lining that surrounds it.
- Heart valve damage.
Diagnosis of systemic lupus erythematosus (lupus)
Diagnosing systemic lupus erythematosus (lupus) can be difficult and may take months or even years. Although there is no single test for lupus, your doctor may do the following to diagnosis you with the condition:
- Ask you about your medical history.
- Give you a physical exam.
- Take samples of blood, skin, kidney, or urine for laboratory tests. The most useful tests look for certain antibodies in the blood.
Treatment for systemic lupus erythematosus (lupus)
Treatments for systemic lupus erythematosus (lupus) have improved dramatically in recent decades, giving doctors more choices in how to manage the disease. Because some treatments may cause harmful side effects, you should immediately report any new symptoms to your doctor. You should also talk to your doctor before stopping or changing treatments.
Treatments for lupus include:
- Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to treat joint or chest pain or fever. Ibuprofen and naproxen sodium are available over the counter, whereas other NSAIDS are available by prescription only.
- Antimalarials prevent and treat malaria, but doctors have found that they also are useful for treating fatigue, joint pain, skin rashes, and inflammation of the lungs caused by lupus. These drugs may also prevent flares from recurring.
- Corticosteroids, strong inflammation-fighting drugs, may be taken by mouth, in creams applied to the skin, by injection, or by intravenous (IV) infusion (dripping the drug into the vein through a small tube). Because they are potent drugs, your doctor will seek the lowest dose required to achieve the desired benefit.
- Immunosuppressives restrain an overactive immune system and may be prescribed if your kidneys or central nervous systems are affected by lupus. These drugs may be given by mouth or by IV infusion. The risk for side effects increases with the length of treatment.
- B-lymphocyte stimulator (BlyS)-specific inhibitors reduce the number of abnormal B cells thought to be a problem in lupus.
- Alternative and complementary therapies may improve symptoms, although research has not shown whether they help treat the disease. Examples include:
- Special diets.
- Nutritional supplements.
- Fish oils.
- Ointments and creams.
- Chiropractic treatment.
- Homeopathy.
In many cases you may need to take medications to treat problems related to lupus, such as high cholesterol, high blood pressure, or infection.
What is Septic arthritis (infectious arthritis)
Septic arthritis (also called infectious arthritis) is painful infection of a joint due to a bacterial, viral or fungal infection 5. The Septic arthritis infection can come from germs that travel through your bloodstream from another part of your body. Septic arthritis can also occur when a penetrating injury delivers germs directly into the joint.
The most common route of entry into the joint is hematogenous (bloodstream) spread during bacteremia (presence of bacteria in the blood) 6. Pathogens may also enter through direct inoculation (e.g., arthrocentesis, arthroscopy, trauma) or contiguous spread from local infections (e.g., osteomyelitis, septic bursitis, abscess) 7. Once in the joint, microorganisms are deposited in the synovial membrane, causing an acute inflammatory response 8. Inflammatory mediators and pressure from large effusions lead to the destruction of joint cartilage and bone loss 9.
Infants and older adults are most likely to develop septic arthritis. Knees are most commonly affected, but septic arthritis also can affect hips, shoulders and other joints. The infection can quickly and severely damage the cartilage and bone within the joint, so prompt treatment is crucial.
Septic arthritis causes
Septic arthritis develops when bacteria or other tiny disease-causing organisms (virus & fungi) spread through the blood to a joint. Septic arthritis can develop when an infection, such as a skin infection or urinary tract infection, spreads through your bloodstream to a joint. Less commonly, a puncture wound, drug injection, or surgery in or near a joint can give the microorganisms entry into the joint space. Joints that are commonly affected are the knee and hip.
The lining of your joints (synovium) has little ability to protect itself from infection. Your body’s reaction to the infection — including inflammation that can increase pressure and reduce blood flow within the joint — contributes to the damage.
Clinical presentations can be broadly grouped into three categories: nongonococcal, gonococcal, and other (e.g., Lyme disease, mycobacterial, fungal).
- Most cases of acute septic arthritis are caused by staphylococcus (40 percent) or streptococcus bacteria (28 percent) 10.
- Bacterial infection with Staphylococcus aureus (staph) is the most common cause. Staph commonly lives on even healthy skin.
Septic arthritis can also be due to the bacteria that cause gonorrhea [a common sexually transmitted infection 11], which is caused by the bacteria Neisseria gonorrhoeae. Gonococcal arthritis is a complication of gonorrhea. Gonococcal arthritis affects women more often than men. It is most common among sexually active teen girls. Any type of sex can spread gonorrhea. You can get it through contact with the mouth, vagina, penis, or anus. Gonorrhea is the second most commonly reported communicable disease. Approximately 330,000 cases occur in the US each year.
Septic arthritis symptoms
Symptoms usually come on quickly. Septic arthritis typically causes extreme joint pain and difficulty using the affected joint (usually in just one joint), which gets worse with movement. The joint could be swollen, red and warm, and you might have a fever.
Symptoms in newborns or infants:
- Crying when infected joint is moved (for example, during diaper changes)
- Fever
- Not able to move the limb with the infected joint (pseudoparalysis)
- Fussiness
Symptoms in children and adults:
- Not able to move the limb with the infected joint (pseudoparalysis)
- Severe joint pain
- Joint swelling
- Joint redness
- Fever
Chills may occur, but are uncommon.
Diagnosis of septic arthritis
The health care provider will examine the joint and ask about the symptoms.
The following tests typically help diagnose septic arthritis:
- Joint fluid analysis. Infections can alter the color, consistency, volume and makeup of the fluid within your joints. A sample of this fluid can be withdrawn from your affected joint with a needle. Laboratory tests can determine what organism is causing your infection, so your doctor will know which medications to prescribe.
- Blood tests. These can determine if there are signs of infection in your blood. A sample of your blood is removed from a vein with a needle.
- Imaging tests. X-rays and other imaging tests of the affected joint can assess damage to the joint.
There are no data on imaging studies that are pathognomonic for acute septic arthritis. Plain films establish a baseline and may detect fractures, chondrocalcinosis, or inflammatory arthritis. Ultrasonography is more sensitive for detecting effusions, particularly in difficult-to-examine joints, such as the hip 12. Magnetic resonance imaging findings that suggest an acute intraarticular infection include the combination of bone erosions with marrow edema 13. Imaging may allow guided arthrocentesis, particularly in difficult-to-examine joints (e.g., hip, sacroiliac, costochondral).
Septic arthritis treatment
Antibiotics are used to treat the infection.
Removing the infected joint fluid is crucial. Drainage methods include:
- Needle. In some cases, your doctor can withdraw the infected fluid with a needle inserted into the joint space.
- Scope procedure. In arthroscopy, a flexible tube with a video camera at its tip is placed in your joint through a small incision. Suction and drainage tubes are then inserted through small incisions around your joint.
- Open surgery. Some joints, such as the hip, are more difficult to drain with a needle or arthroscopy, so an open surgical procedure might be necessary.
Resting, raising the joint above heart level, and using cool compresses may help relieve pain. After the joint starts to heal, exercising it can help speed recovery.
Antibiotics
To select the most effective medication, your doctor must identify the microbe causing your infection. Antibiotics are usually given through a vein in your arm at first. Later, you may be able to switch to oral antibiotics.
Typically, treatment lasts from two to six weeks. Antibiotics carry a risk of side effects, including nausea, vomiting and diarrhea. Allergic reactions also can occur. Ask your doctor about what side effects to expect from your medication.
- Arthritis. https://www.niams.nih.gov/health-topics/arthritis[↩]
- Ankylosing spondylitis. https://www.niams.nih.gov/health-topics/ankylosing-spondylitis[↩]
- Gout. https://www.niams.nih.gov/health-topics/gout/advanced[↩]
- Psoriatic arthritis. https://www.niams.nih.gov/health-topics/psoriatic-arthritis/advanced[↩]
- Septic arthritis. https://medlineplus.gov/ency/article/000430.htm[↩]
- Margaretten ME, Kohlwes J, Moore D, Bent S. Does this adult patient have septic arthritis? JAMA. 2007;297(13):1478–1488.[↩]
- Ross JJ, Saltzman CL, Carling P, Shapiro DS. Pneumococcal septic arthritis: review of 190 cases. Clin Infect Dis. 2003;36(3):319–327.[↩]
- Goldenberg DL. Septic arthritis. Lancet. 1998;351(9097):197–202.[↩]
- Smith JW, Piercy EA. Infectious arthritis. Clin Infect Dis. 1995;20(2):225–230.[↩]
- Ryan MJ, Kavanagh R, Wall PG, Hazleman BL. Bacterial joint infections in England and Wales: analysis of bacterial isolates over a four year period. Br J Rheumatol. 1997;36(3):370–373.[↩]
- Gonorrhea. https://medlineplus.gov/ency/article/007267.htm[↩]
- Zieger MM, Dörr U, Schulz RD. Ultrasonography of hip joint effusions. Skeletal Radiol. 1987;16(8):607–611.[↩]
- Graif M, Schweitzer ME, Deely D, Matteucci T. The septic versus non-septic inflamed joint: MRI characteristics. Skeletal Radiol. 1999;28(11):616–620.[↩]