Contents
Lower back surgery
Back pain is very common and affects people of all ages, but back surgery often fails to relieve it. Back surgery can help relieve some causes of back pain, but it’s rarely necessary. Most back pain resolves on its own within three months. Most back problems typically respond to nonsurgical treatments — such as anti-inflammatory medications, heat and physical therapy. If you are experiencing back pain yourself, it is important not to restrict your movement too much. Even if your back is very painful, slow and gentle movements are better than lying still in bed. If you keep your back moving, it will become more supple and flexible. While it generally improves in a few days, or sometimes weeks, back pain can continue for a long period. Several things can cause it, including a sudden movement or fall, an injury, or a medical condition. The pain is usually related to the way the bones, discs, tendons, muscles and ligaments work together.
A very recent large prospective cohort study 1 showed that persistent pain after lumbar spine surgery is common, with 11% reporting no improvement and 28% little-to-moderate improvement at 2 years. Spinal fusion accounted for 38% of the sample. Further analysis showed greater preoperative pain, and revision surgery (having a second operation for the same problem – or to solve a complication of the previous operation) were associated with poorer outcomes, and this is not surprising 1. These findings have what surgeons call “face validity” – ie it seems to make sense even to which is as expected. Perhaps not as expected is the fact that there were poorer outcomes associated with patients who had a psychological diagnosis, or had a degenerative diagnosis. If a patient is depressed for example, the outcome of their back surgery is likely to be not as good. This is the same for patients who have degenerative spines as opposed to those who have had an injury to a single disc.
One of the interesting outcomes of this study 1 was that patients who were expecting a greater pain improvement preoperatively showed less improvement of pain. The message here is that patients need to be told what the realistic outcome is likely to be and not guaranteed a total fix.
For that reason, the medical profession as a whole is cautious about referring people with back pain for surgery unless there is a strong reason for believing that the back surgery is going to benefit. Not every spinal condition is suitable for surgery – this is sometimes why your surgeon may say “I’m sorry but I can’t help you”. This doesn’t mean “you are too far gone” or “I don’t believe you have pain” – it just means that surgery is either too tricky or too dangerous or known not to help your particular condition.
Almost everyone will experience low back pain at some point in their lives. This pain can vary from mild to severe. It can be short-lived or long-lasting.
Back problems are a common reason for pain among younger and middle-aged adults, but they can also start early in life – between the ages of 8 and 10.
Treatment for low back pain focuses on relieving your symptoms. In many cases, a combination of treatments will help you to return to all the activities you want to do. Treatment typically begins with reducing inflammation. Applying ice, taking an anti-inflammatory and allowing relative rest for three days will aid in the healing process. Then, you may begin incorporating a low intensity aerobic activity, like walking, based upon your physician’s recommendations.
Therapeutic exercise as directed by a physical therapist can help with pain reduction, improve movement patterns to reduce repetitive overload and work to prevent future injury. The physical therapist will develop an individualized program for you to perform independently at home to improve faulty movement patterns and improve your core stability.
Commitment to performing the prescribed exercise program will enhance your recovery. This process does not occur immediately; soft tissue changes can be slow and patience is important.
Your spine is a bony support for your trunk. The individual bones, vertebra, stack on top of each other creating the spinal column. The spinal cord is in the canal in the center of the vertebra for protection and is the central relay for nerve activity to and from the brain.
At each level of the spine, a nerve exits to provide stimulation to a group of muscles and sensation in a specific area of the skin. Surrounding the bony column are ligaments and muscles. Between the vertebra bodies are discs. The discs work together with the ligaments and muscles to allow for movement of the spine.
The discs between the vertebra contain 70-80% liquid material until about age 30. Around that age, the disc begins to dehydrate as a normal process of aging. This process can be accelerated when a tear occurs in the outer layer of the disc known as the annulus. If the tear results in a piece of the disc protruding beyond its usual confines between the vertebra, it is referred to as a herniated, slipped, ruptured or disc protrusion. When the tear or protrusion occurs, fluid leaks from the disc causing an inflammatory reaction that may be associated with pain. If the disc contacts a nerve, pain may travel along the distribution of that nerve causing pain and even weakness in the arm or leg.
Because the body constantly attempts to heal itself, many cells help to remove this disc material. Because the mechanism involves inflammation and the nervous system, spine pain can be intense. The spine will “exaggerate” what is happening to the brain. Your brain will interpret the signals as they come in as intense.
The good news is that most of the time, the area of injury heals itself in 6-8 weeks.
Figure 1. Herniated disc (the rubbery disks that lie between the vertebrae in your spine consist of a soft center (nucleus) surrounded by a tougher exterior (annulus). A herniated disk occurs when a portion of the nucleus pushes through a crack in the annulus. Symptoms may occur if the herniation compresses a nerve.)
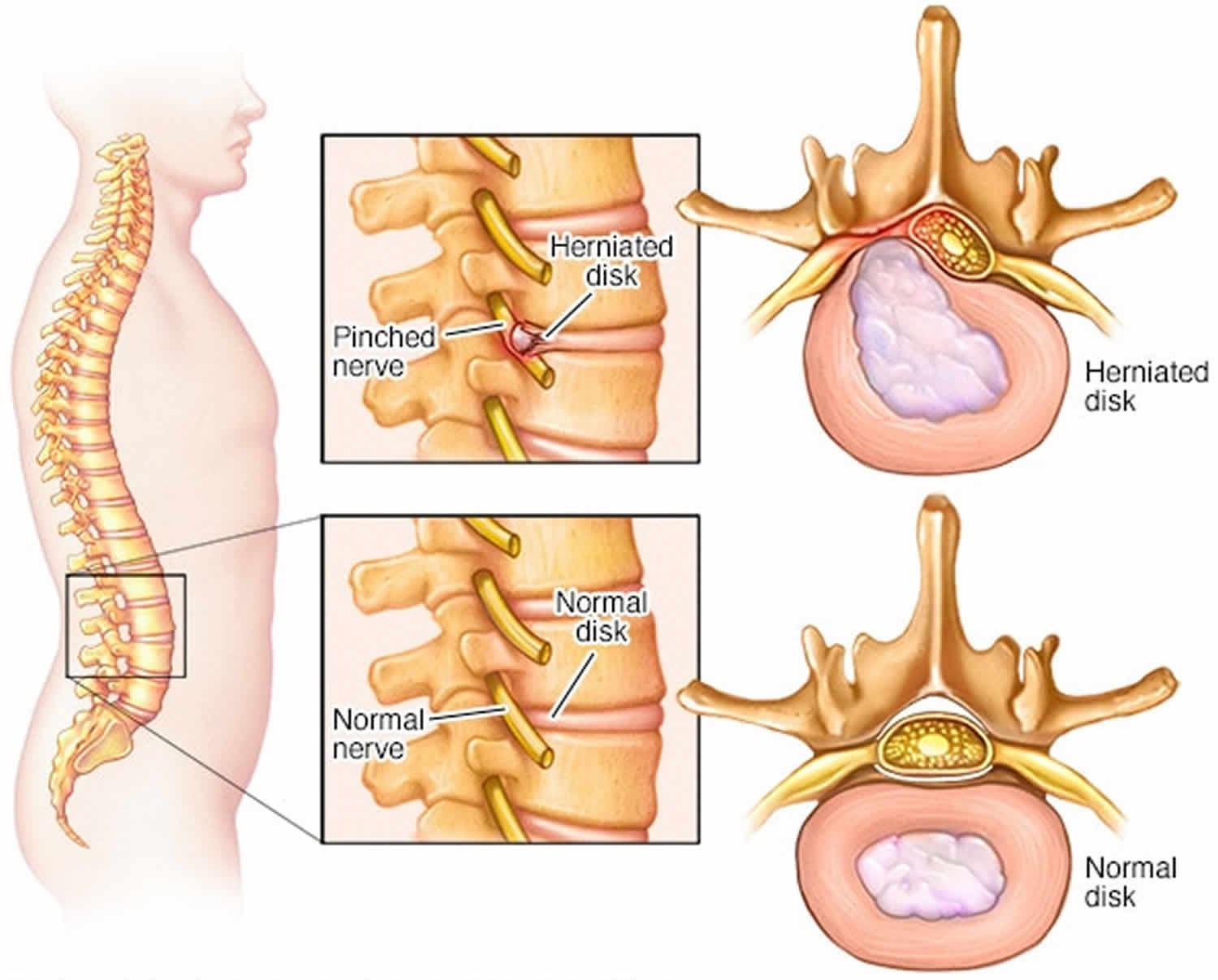
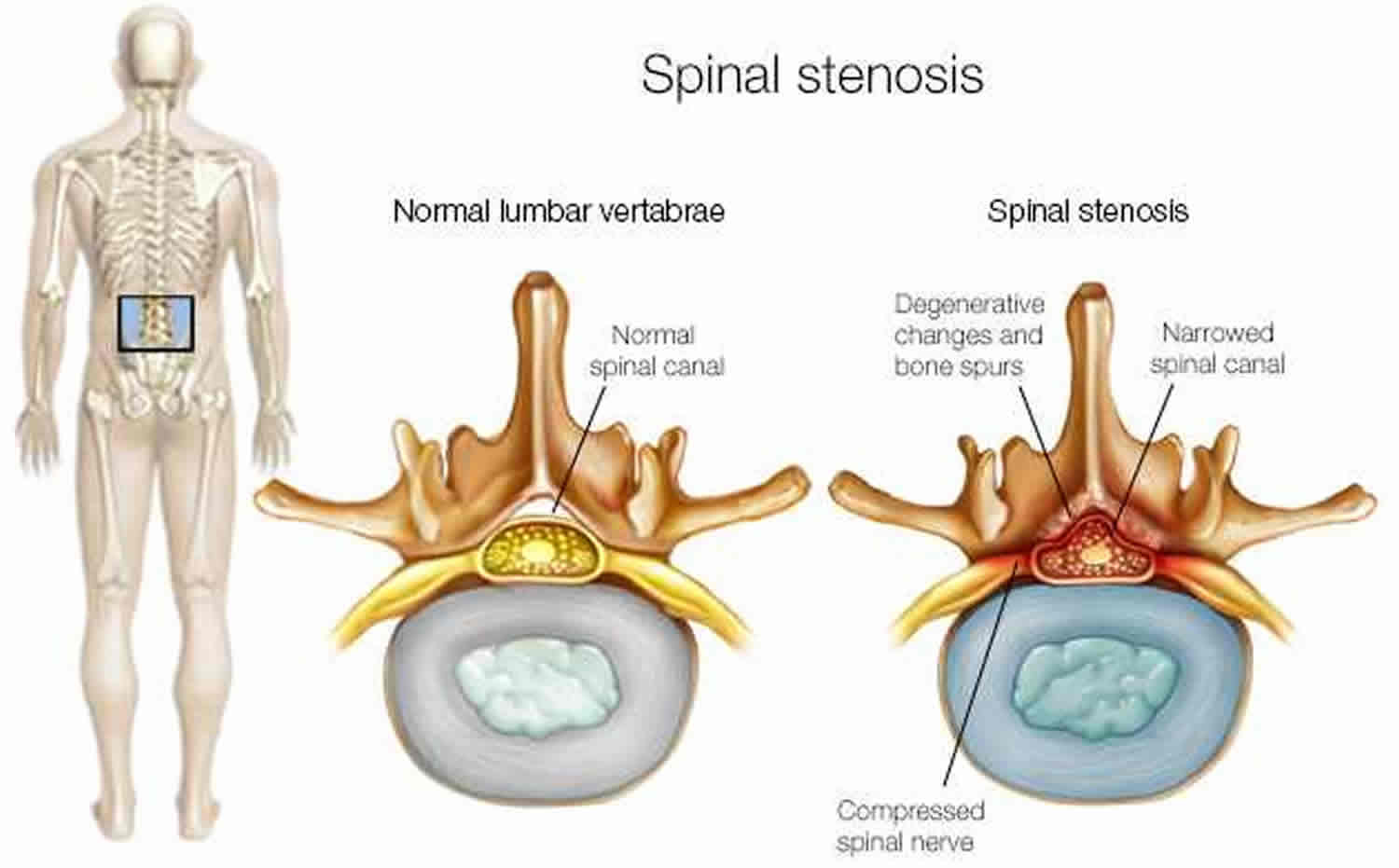
Figure 2. Spinal stenosis (spinal stenosis occurs when the space within the spinal canal or around the nerve roots becomes narrowed)
Do you need back surgery?
Back surgery might be an option if conservative treatments haven’t worked and your pain is persistent and disabling. Back surgery often more predictably relieves associated pain or numbness that goes down one or both arms or legs.
These symptoms often are caused by compressed nerves in your spine. Nerves may become compressed for a variety of reasons, including:
- Disk problems. Bulging or ruptured (herniated) disks — the rubbery cushions separating the bones of your spine — can sometimes press too tightly against a spinal nerve and affect its function.
- Overgrowth of bone. Osteoarthritis can result in bone spurs on your spine. This excess bone most commonly affects the hinge joints on the back part of the spinal column and can narrow the amount of space available for nerves to pass through openings in your spine.
It can be very difficult to pinpoint the exact cause of your back pain, even if your X-rays show that you have disk problems or bone spurs. X-rays taken for other reasons often reveal bulging or herniated disks that cause no symptoms and need no treatment.
However, if you and your orthopaedic surgeon have determined that your low back problem might be helped by surgery, there are several things you can do to help ensure that you are prepared for the procedure.
Low back surgery usually takes from 1 to 3 hours, depending upon the procedure.
When your back surgery is over, you will be moved to the recovery room, where you will be observed and monitored by a nurse until you awaken from the anesthesia. You will have an intravenous (IV) line inserted into a vein in your arm. You may also have a catheter inserted into your bladder to make urination easier.
When you are fully awake and alert, you will be taken to your hospital room.
For outpatient procedures, the nurses in the recovery room will make sure that you are able to walk, eat, and go to the bathroom before discharging you home. They will also go over any postoperative instructions with you and make sure that you understand the directions for your pain medications.
Preparing for back surgery
Preoperative Checkup
Depending on your age and general medical fitness, your surgeon may ask you to have a checkup by your family doctor and any other doctor that you see regularly, such as your cardiologist (heart doctor).
Smoking
If you smoke or use smokeless tobacco, you should quit several months before surgery. Nicotine users are at greater risk for serious complications after surgery, including wound infections and a delay in the bone healing needed for successful fusion surgeries. It is extremely important to inform your surgeon about your nicotine usage in advance of your procedure so that, together, you can determine a plan for you to quit.
Medications
Some medications can affect your surgery by causing bleeding or interfering with anesthesia. These medications include aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen. Certain over-the-counter dietary supplements and herbal remedies can also interfere with surgery. Your surgeon will tell you which supplements and medications you should stop taking in preparation for your procedure.
Donating Blood
It is not usually necessary to donate blood for low back surgery. However, there is always a chance that some blood loss will occur during the procedure. Your surgeon will talk with you about the advantages and disadvantages of donating your own blood versus using someone else’s blood. If you decide to donate your own blood, your surgeon may prescribe an iron supplement to help build up your blood before surgery.
Advance Planning
You will be able to walk after surgery, but you may need to arrange for someone to help you for a few days after your return home with activities like washing, dressing, cleaning, laundry, and shopping.
Even after minor spine surgery, your doctor may recommend that you do not drive for 2 weeks, or possibly even longer. For this reason, you will need to arrange in advance for transportation to and from your hospital appointments and other places that you need to go during this time. You should consult your doctor in advance if you have an extended car trip planned during your recovery. He or she may recommend that you postpone your trip until your recovery is complete.
Back surgery types
Different types of back surgery include:
- Diskectomy. This involves removal of the herniated portion of a disk to relieve irritation and inflammation of a nerve. Diskectomy typically involves full or partial removal of the back portion of a vertebra (lamina) to access the ruptured disk.
- Laminectomy. This procedure involves the removal of the bone overlying the spinal canal. It enlarges the spinal canal and is performed to relieve nerve pressure caused by spinal stenosis.
- Spinal Fusion. Spinal fusion permanently connects two or more bones in your spine. It can relieve pain by adding stability to a spinal fracture. It is occasionally used to eliminate painful motion between vertebrae that can result from a degenerated or injured disk.
- Artificial discs. Implanted artificial discs are a treatment alternative to spinal fusion for painful movement between two vertebrae due to a degenerated or injured disk. But these relatively new devices aren’t an option for most people.
Before you agree to back surgery, consider getting a second opinion from a qualified spine specialist. Spine surgeons may hold different opinions about when to operate, what type of surgery to perform and whether — for some spine conditions — surgery is warranted at all. Back and leg pain can be a complex issue that may require a team of health professionals to diagnose and treat.
Fortunately, very few people who experience low back or neck pain will require a surgery to obtain relief from their discomfort. But if conservative treatments haven’t resolved your pain within six months and your doctor has determined that your disk joint is the source of your chronic pain, you might be a candidate for disk replacement surgery.
Spinal fusion — the most common type of back surgery for painful joints — involves fusing two or more vertebrae together. Disk replacement surgery is a newer procedure that replaces the problem disk joint with an artificial one made of metal and plastic.
In general, it appears that spinal fusion and disk replacement procedures are equally effective. There are some special considerations and restrictions that you should review with your spine care provider before pursuing this treatment option. In some cases, intensive rehabilitation programs appear to work just as well as either type of surgery — at a lower cost and with fewer complications.
Diskectomy
Diskectomy (discectomy) is a surgical procedure to remove the damaged portion of a herniated disk (also called a slipped, ruptured or bulging disk or disk prolapse) in your spine. A herniated disk can irritate or compress nearby spinal nerves. Diskectomy is most effective for treating pain that radiates down your arms or legs.
Diskectomy procedure is less helpful for treating actual back pain or neck pain. Most people who have back pain or neck pain find relief with more-conservative treatments, such as physical therapy.
Your doctor may suggest diskectomy if conservative, nonsurgical treatments haven’t worked or if your symptoms worsen. There are several ways to perform a diskectomy. Many surgeons now prefer minimally invasive diskectomy, which uses small incisions and a tiny video camera for viewing the procedure.
Your doctor may recommend diskectomy if:
- You have trouble standing or walking because of nerve weakness
- Conservative treatment, such as physical therapy or steroid injections, fails to improve your symptoms after six to 12 weeks
- Pain radiating into your buttocks, legs, arms or chest becomes too much to manage
Diskectomy risks
Diskectomy is considered a safe procedure. But as with any surgery, diskectomy carries a risk of complications. Potential complications include:
- Bleeding
- Infection
- Leaking spinal fluid
- Injury to blood vessels or nerves in and around the spine
Diskectomy prep
You’ll likely need to avoid eating and drinking for a certain amount of time before surgery. If you take blood-thinning medications, you may need to adjust your dosing schedule before surgery. Your doctor will give you specific instructions.
During diskectomy surgery
Surgeons usually perform diskectomy using general anesthesia, so you’re unconscious during the procedure. Small amounts of spinal bone and ligament may be removed to gain access to the herniated disk.
Ideally, just the fragment of disk that is pinching the nerve is removed, relieving the pressure but leaving most of the disk intact.
If the entire disk must be taken out, your surgeon may need to fill the space with a piece of bone — taken from a deceased donor or from your own pelvis — or a synthetic bone substitute. The adjoining vertebrae are then fused together with metal hardware.
After diskectomy surgery
After surgery, you’re moved to a recovery room where the health care team watches for complications from the surgery and anesthesia. You may be healthy enough to go home the same day you have surgery, although a short hospital stay may be necessary — particularly if you have any serious pre-existing medical conditions.
Depending on the amount of lifting, walking and sitting your job involves, you may be able to return to work in two to six weeks. If you have a job that includes heavy lifting or operating heavy machinery, your doctor may advise you to wait six to eight weeks before returning to work.
Diskectomy results
Diskectomy reduces herniated disk symptoms in most people who have clear signs of nerve compression, such as radiating pain. However, diskectomy may not be a permanent cure, because it doesn’t do anything to reverse the process that allowed the disk to become herniated in the first place.
To avoid re-injuring your spine, your doctor may recommend weight loss, prescribe a low-impact exercise program, and ask that you limit some activities that involve extensive or repetitive bending, twisting or lifting.
Laminectomy
A lumbar laminectomy also known as decompression surgery, involves the removal of the back portion of a vertebra in your lower back to create more room within the spinal canal to relieve pressure on the spinal cord or nerves. Laminectomy is generally used only when more-conservative treatments — such as medication, physical therapy or injections — have failed to relieve symptoms. Laminectomy may also be recommended if symptoms are severe or worsening dramatically.
Figure 3. Lumbar laminectomy
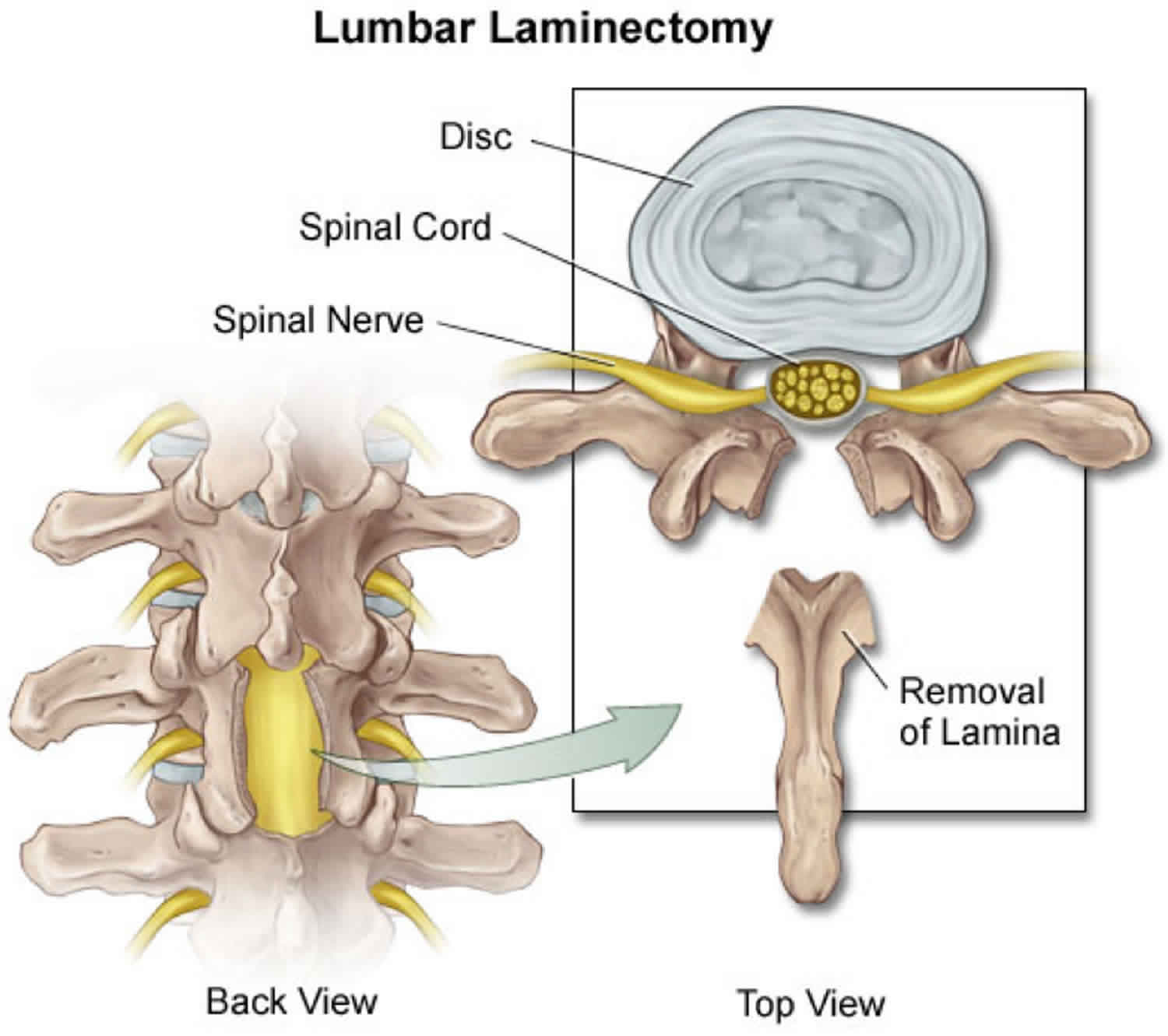
Why is laminectomy done?
Bony overgrowths within the spinal canal can narrow the space available for your spinal cord and nerves. This pressure can cause pain, weakness or numbness that can radiate down your arms or legs.
Because the laminectomy restores spinal canal space but does not cure you of arthritis, it more reliably relieves radiating symptoms from compressed nerves than it does back pain from spinal joints.
Your doctor may recommend laminectomy if:
- Conservative treatment, such as medication or physical therapy, fails to improve your symptoms
- You have muscle weakness or numbness that makes standing or walking difficult
- You experience loss of bowel or bladder control
In some situations, laminectomy may be necessary as part of surgery to treat a herniated spinal disk. Your surgeon may need to remove part of the lamina to gain access to the damaged disk.
Laminectomy risks
Laminectomy is generally a safe procedure. But as with any surgery, complications may occur. Potential complications include:
- Bleeding
- Infection
- Blood clots
- Nerve injury
- Spinal fluid leak
Laminectomy preparation
You’ll need to avoid eating and drinking for a certain amount of time before surgery. Your doctor can give you specific instructions about the types of medications you should and shouldn’t take before your surgery.
During laminectomy surgery
Surgeons usually perform laminectomy using general anesthesia, so you’re unconscious during the procedure.
The surgical team monitors your heart rate, blood pressure and blood oxygen levels throughout the procedure. After you’re unconscious and can’t feel any pain:
- The surgeon makes an incision in your back over the affected vertebrae and moves the muscles away from your spine as needed. Small instruments are used to remove the appropriate lamina. The size of the incision may vary depending on your condition and body size. Minimally invasive surgeries typically use smaller incisions than those used for open procedures.
- If laminectomy is being performed as part of surgical treatment for a herniated disk, the surgeon also removes the herniated portion of the disk and any pieces that have broken loose (diskectomy).
- If one of your vertebrae has slipped over another or if you have curvature of the spine, spinal fusion may be necessary to stabilize your spine. During spinal fusion, the surgeon permanently connects two or more of your vertebrae together using bone grafts and, if necessary, metal rods and screws.
- Depending on your condition and individual needs, the surgeon may use a smaller (minimally invasive) incision and a special surgical microscope to perform the operation.
After laminectomy surgery
After surgery, you’re moved to a recovery room where the health care team watches for complications from the surgery and anesthesia. You may also be asked to move your arms and legs. Your doctor may prescribe medication to relieve pain at the incision site.
You might go home the same day as the surgery, although some people may need a short hospital stay. Your doctor may recommend physical therapy after a laminectomy to improve your strength and flexibility.
Depending on the amount of lifting, walking and sitting your job involves, you may be able to return to work within a few weeks. If you also have spinal fusion, your recovery time will be longer.
Laminectomy results
Most people report measurable improvement in their symptoms after laminectomy, particularly a decrease in pain that radiates down the leg or arm. But this benefit may lessen over time if you have a particularly aggressive form of arthritis. Laminectomy is less likely to improve pain in the back itself.
Spinal fusion
Spinal fusion is a surgical technique in which one or more of the vertebrae of the spine are united together (“fused”) so that motion no longer occurs between them. Spinal fusion involves techniques designed to mimic the normal healing process of broken bones. During spinal fusion, your surgeon places bone or a bonelike material within the space between two spinal vertebrae. Metal plates, screws and rods may be used to hold the vertebrae together, so they can heal into one solid unit. The body heals the grafts over several months – similar to healing a fracture – which joins, or “welds,” the vertebrae together.
Spinal fusion surgery can take 3 to 4 hours.
When is spinal fusion recommended?
Spinal fusion permanently connects two or more vertebrae in your spine to improve stability, correct a deformity or reduce pain.
There are many potential reasons for a surgeon to consider fusing the vertebrae. These include: treatment of a fractured (broken) vertebra; correction of deformity (spinal curves or slippages); elimination of pain from painful motion; treatment of instability; and treatment of some cervical disc herniations.
One of the less controversial reasons to do spinal fusion is a vertebral fracture. Although not all spinal fractures need surgery, some fractures – particularly those associated with spinal cord or nerve injury – generally require fusion as part of the surgical treatment.
Sometimes a hairline fracture allows one vertebra to slip forward on another. This condition is called spondylolisthesis and can be treated by fusion surgery.
Another condition that is treated by fusion surgery is actual or potential instability. Instability refers to abnormal or excessive motion between two or more vertebrae. It is commonly believed that instability can either be a source of back or neck pain or cause potential irritation or damage to adjacent nerves. Although there is some disagreement on the precise definition of instability, many surgeons agree that definite instability of one or more segments of the spine is an indication for fusion.
Spinal fusion is sometimes considered in the treatment of a painful spinal condition without clear instability. A major obstacle to the successful treatment of spine pain by fusion is the difficulty in accurately identifying the source of a patient’s pain. The theory is that pain can originate from painful spinal motion and fusing the vertebrae together to eliminate the motion will get rid of the pain. Unfortunately, current techniques to precisely identify which of the many structures in the spine could be the source of a patient’s back or neck pain are not perfect. Because it can be so hard to locate the source of pain, treatment of back or neck pain alone by spinal fusion is somewhat controversial. Fusion under these conditions is usually viewed as a last resort and should be considered only after other conservative (nonsurgical) measures have failed.
Your doctor may recommend spinal fusion to treat:
- Deformities of the spine. Spinal fusion can help correct spinal deformities, such as a sideways curvature of the spine (scoliosis).
- Spinal weakness or instability. Your spine may become unstable if there’s abnormal or excessive motion between two vertebrae. This is a common side effect of severe arthritis in the spine. Spinal fusion can be used to restore spinal stability in such cases.
- Herniated disk. Spinal fusion may be used to stabilize the spine after removal of a damaged (herniated) disk.
Spinal fusion risks
Spinal fusion is generally a safe procedure. But as with any surgery, spinal fusion carries the potential risk of complications.
Potential complications include:
- Infection
- Poor wound healing
- Bleeding
- Blood clots
- Injury to blood vessels or nerves in and around the spine
- Pain at the site from which the bone graft is taken
Spinal fusion preparation
Before surgery, you will undergo imaging studies of your spine. Your surgeon uses these images to plan and guide surgery. Mayo Clinic surgeons work with radiologists to create detailed, high-resolution images and precise 3D models. Mayo Clinic also uses an advanced robotic surgery system that offers enhanced preoperative planning and verification during surgery.
Preparation before surgery may involve trimming hair over the surgical site and cleaning the area with a special soap or antiseptic. Additionally, the surgical team may order monitoring of any unhealthy bacteria in your nose by taking a swab sample. Tell your doctor about any medications you are taking. You may be asked to stop taking some medications before the surgery.
During spinal fusion surgery
Surgeons perform spinal fusion while you’re under general anesthesia so you’re unconscious during the procedure. Surgeons have developed a variety of techniques for performing spinal fusion surgery. The technique your surgeon uses depends on the location of the vertebrae to be fused, the reason for the spinal fusion, and in some instances, your general health and body shape.
Generally, the spinal fusion procedure involves the following:
- Incision. To gain access to the vertebrae being fused, the surgeon makes an incision in one of three locations: in your neck or back directly over your spine, on either side of your spine, or in your abdomen or throat so that your surgeon can access the spine from the front.
- Bone graft preparation. The bone grafts that actually fuse two vertebrae together may come from a bone bank or from your own body, usually from your pelvis. If your own bone is used, the surgeon makes an incision above your pelvic bone, removes a small portion of it and then closes the incision.
- Fusion. To fuse the vertebrae together permanently, the surgeon places the bone graft material between the vertebrae. Metal plates, screws or rods may be used to help hold the vertebrae together while the bone graft heals.
In selected cases, some surgeons use a synthetic substance instead of bone grafts. These synthetic substances help promote bone growth and speed the fusion of the vertebrae.
After spinal fusion surgery
A hospital stay of two to three days is usually required following spinal fusion. Depending on the location and extent of your surgery, you may experience some pain and discomfort but the pain can usually be controlled well with medications.
After you go home, contact your doctor if you exhibit signs of infection, such as:
- Redness, tenderness or swelling
- Wound drainage
- Shaking chills
- Fever higher than 100.4 °F (38 °C)
It my take several months for the affected bones in your spine to heal and fuse together. Your doctor may recommend that you wear a brace for a time to keep your spine aligned correctly. Physical therapy can teach you how to move, sit, stand and walk in a manner that keeps your spine properly aligned.
Spinal fusion results
Spinal fusion is typically an effective treatment for fractures, deformities or instability in the spine. But study results are more mixed when the cause of the back or neck pain is unclear. In many cases, spinal fusion is no more effective than nonsurgical treatments for nonspecific back pain.
It can be difficult to be certain about what exactly is causing your back pain, even if a herniated disk or bone spurs show up on your X-rays. Many people have X-ray evidence of back issues that have never caused them any pain. So your pain might not be associated with whatever problem has been revealed on your imaging scans.
Even when spinal fusion provides symptom relief, it does not prevent you from developing more back pain in the future. Most of the degenerative conditions in the spine are caused by arthritis, and surgery will not cure your body of that disease.
Immobilizing a section of your spine places additional stress and strain on the areas around the fused portion. This may increase the rate at which those areas of your spine degenerate — so you may need additional spinal surgery in the future.
Artificial Disc Replacement
An artificial disc also called a disc replacement, disc prosthesis or spine arthroplasty device, is a device that is implanted into the spine to imitate the functions of a normal disc (carry load and allow motion).
There are many artificial disc designs classified into two general types: total disc replacement and disc nucleus replacement. As the names imply, with a total disc replacement, all or most of the disc tissue is removed and a replacement device is implanted into the space between the vertebra. With a disc nucleus replacement, only the center of the disc (the nucleus) is removed and replaced with an implant. The outer part of the disc (the annulus) is not removed.
Most often, artificial disc replacement surgery is done for only one disk, but at times, two levels next to each other may be replaced.
The artificial disc replacement surgery is done under general anesthesia. You will be asleep and not feel any pain.
Artificial discs are usually made of metal or plastic-like (biopolymer) materials, or a combination of the two. These materials have been used in the body for many years. Total disc replacements have been used in Europe since the late 1980s. The most commonly used total disc replacement designs have two plates. One attaches to the vertebrae above the disc being replaced and the other to the vertebrae below. Some devices have a soft, compressible plastic-like piece between these plates. The devices allow motion by smooth, usually curved, surfaces sliding across each other.
Most nucleus replacement devices are made of plastic-like (biopolymer) materials. One such material is called hydrogel. This material expands as it absorbs water. The device is placed into the nuclear cavity of the disc and hydrates to expand and fill the cavity. The device is compressible and by this means, allows motion, much like a normal disc nucleus. Another design consists of a piece of a plastic-like material that coils around to fill the nuclear cavity. No nuclear replacement devices are available for use in the United States at this time, even as a part of an FDA-approved study.
There are also disc replacements designed for use in the cervical spine (the neck). These devices have only been used a relatively short time, and several are currently undergoing evaluation in FDA-approved trials in the United States.
Who needs an artificial disc replacement?
The indications for disc replacement may vary for each type of implant. Some general indications are pain arising from the disc that has not been adequately reduced with non-operative care such as medication, injections, chiropractic care and/or physical therapy. Typically, you will have had an MRI that shows disc degeneration. Often discography is performed to verify which disc(s), if any, is related to your pain. Discography is a procedure in which dye is injected into the disc and X-rays and a CT scan are taken. The surgeon will correlate the results of these tests with findings from your history and physical examination to help determine the source of your pain.
There are several conditions that may prevent you from receiving a disc replacement. These include spondylolisthesis (the slipping of one vertebral body across a lower one), osteoporosis, vertebral body fracture, allergy to the materials in the device, spinal tumor, spinal infection, morbid obesity, significant changes of the facet joints (joints in the back portion of the spine), pregnancy, chronic steroid use or autoimmune problems. Also, total disc replacements are designed to be implanted from an anterior approach (through the abdomen). You may be excluded from receiving and artificial disc if you previously had abdominal surgery or if the condition of the blood vessels in front of your spine increases the risk of significant injury during this type of spinal surgery.
Back pain is sometimes produced by an injured or degenerated disc. To treat this condition, alternatives to disc replacement include fusion, nonoperative care or no treatment. Typically, surgery is not considered for disc-related pain unless the pain has been severe for a prolonged period (typically over six months) and the patient has gone through nonoperative treatments (such as active physical therapy, medication, injections, activity modification and/or spinal manipulation).
Traditionally, the operative treatment for disc pain has been spinal fusion. This is a surgical procedure in which disc tissue is removed and bone is placed between the vertebral bodies. The goal of this surgery is to fuse the vertebra around the disc that is causing pain. It is thought that by removing disc tissue and eliminating movement, the pain will be significantly reduced.
A normal healthy spine allows motion at each of the discs throughout the spine. Ideally, your surgeon would like to restore your spine to this normal state. Currently the treatment for many painful spinal conditions is fusion, which eliminates motion of the painful spinal segment. Artificial discs are designed to allow motion after surgery that is as normal as possible.
With fusion there also is a possibility that the fusion of one part of the spine forces the discs and vertebra above and/or below to carry more load and motion. This may result in more wear and tear than normal. The artificial disc may significantly reduce this risk.
Another potential advantage of disc replacement is a more rapid return to activities than occurs after fusion surgery. Fusion patients have limited activities during the time required for the bone graft to grow into a solid mass. Because one of the goals of artificial discs is motion, patients are encouraged to return to motion early, although at a gradual progression. Although artificial discs offer several advantages over fusion, this is a relatively new technology with no long-term randomized, controlled clinical study results. Fusion has a long-standing record of success in permanently correcting problems in the fused motion segment. Discuss both options thoroughly with your health care provider before deciding which procedure is best for you.
The type of artificial disc to use, if any, depends on the cause of your back and/or leg pain, the severity of the problem and the training of your surgeon. A nucleus replacement may be an option for patients with early stage symptomatic disc degeneration where the annulus is in good condition. These devices also may be implanted after a discectomy involving the removal of a large amount of disc tissue. In discs with more severe degeneration, a total disc replacement may be indicated.
Artificial disc replacement risks
As with any surgery, there are risks associated with disc replacement. The complications when using artificial discs are similar to those associated with anterior spinal fusion. Possible complications include but are not limited to: infection, injury to blood vessels, nerve injury, dislodgement or breakage of the device, wear of the device materials, continued or increasing pain, development of new pain, sexual dysfunction, injury to urologic structures and death. Discuss these risks with your surgeon before deciding to have an artificial disc implanted.
Risks of anesthesia and surgery in general are:
- Allergic reaction to medicines
- Breathing problems
- Bleeding, blood clots, and infection
Risks for total artificial disc replacement are:
- Increase in back pain
- Difficulty with movement
- Injury to the gut
- Blood clots in legs
- Abnormal bone formation in the muscles and tendons surrounding the spinal cord
- Sexual dysfunction (more common in men)
- Damage to the ureter and bladder
- Infection at the surgical site
- Breakage of the artificial disk
- Artificial disk may move out of place
- Loosening of the implant
- Paralysis
Artificial disc replacement preparation
Your doctor will order an imaging test such as an MRI, CT scan, or x-ray to check if you need surgery.
Your doctor will want to know if you:
- Are pregnant
- Are taking any medicines, supplements, or herbs
- Are diabetic, hypertensive, or have any other medical condition
- Are a smoker
Tell your health care doctor what medicines you are taking. This includes medicines, supplements, or herbs you bought without a prescription.
During the days before the surgery:
- Prepare your home for when you leave the hospital.
- If you are a smoker, you need to stop. People who have total disc replacement and continue to smoke may not heal as well. Ask your doctor for help quitting.
- One week before surgery, your doctor may ask you to stop taking medicines that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn).
- If you have diabetes, heart disease, or other medical problems, your surgeon will ask you to see your regular doctor.
- Talk with your doctor if you have been drinking a lot of alcohol.
- Ask your doctor which medicines you should still take on the day of the surgery.
- Let your doctor know right away if you get a cold, flu, fever, herpes breakout, or other illnesses you may have.
- You may want to visit a physical therapist to learn exercises to do before surgery.
On the day of the surgery:
- Follow instructions on not drinking or eating anything before the procedure. This may be 6 to 12 hours before surgery.
- Take the medicines your doctor told you to take with a small sip of water.
- Your doctor will tell you when to arrive at the hospital. Be sure to arrive on time.
Artificial disc replacement surgery
During artificial disc replacement surgery:
- You will lie on your back on the operating table.
- Your arms are padded at the elbow area and folded in front of your chest.
- Your surgeon makes a horizontal incision (cut) on your abdomen. Doing the operation through the abdomen allows the surgeon to access the spine without disturbing the spinal nerves.
- The gut organs and blood vessels are moved to the side to get access to the backbone.
- Your surgeon removes the damaged portion of the disk and puts the new artificial disk in its place.
- All the organs are put back into place.
- The incision is closed with stitches.
The surgery takes about 2 hours to complete.
After artificial disc replacement surgery
You will stay in the hospital 2 to 3 days after surgery. Your doctor will encourage you to stand and start walking as soon as the anesthesia wears off. You may have to wear a corset brace for support and faster healing. In the beginning, you’ll be given clear liquids. You’ll later progress to a liquid and semi-solid diet.
Your doctor will ask you not to:
- Do any activity that stretches your spine too much
- Take part in activities that involve jarring, bending, and twisting such as driving and lifting heavy objects for at least 3 months after surgery
Follow instructions on how to take care of your back at home.
You can likely return to normal activities 3 months after the surgery.
Artificial disc replacement surgery results
The risk of complications are low after lumbar disk replacement. The surgery usually improves movement of the backbone better than other (spine surgeries). It is a safe procedure and pain relief occurs soon after surgery. The risk of spinal muscle (paravertebral muscle) injury is less than with other types of spine surgeries.
Back surgery for herniated disc
A spinal disc is a little like a jelly donut, with a softer center encased within a tougher exterior. A herniated disc refers to a problem with one of the rubbery cushions (disks) between the individual bones (vertebrae) that stack up to make your spine. Sometimes called a “slipped disc” or a “ruptured disc”, although the whole disc does not rupture or slip. Only the small area of the crack is affected. A herniated disk occurs when some of the softer “jelly” pushes out through a tear in the outer layer of cartilage, allowing some of the softer inner cartilage to protrude out of the disc.
A bulging disk, on the other hand, doesn’t always affect the entire perimeter of a disc, but at least a quarter if not half of the disc’s circumference is usually affected. Only the outer layer of tough cartilage is involved.
Compared with a bulging disk, a herniated disk is more likely to cause pain because it generally protrudes farther and is more likely to irritate nerve roots. The irritation can be from compression of the nerve or, much more commonly, the herniation causes a painful inflammation of the nerve root.
A herniated disc can irritate nearby nerves and result in pain, numbness or weakness in an arm or leg. On the other hand, many people experience no symptoms from a herniated disk. Many people have MRI evidence of herniated disks and have no back pain at all. Most people who have a herniated disk don’t need surgery to correct the problem.
There are a few different operations that alter the shape of the intervertebral disc (‘discectomy’ or diskectomy) or replace it altogether.
These are generally only recommend for those with slipped discs in the lower back (lumbar spine) that have occurred recently or suddenly and have not improved with non-surgical forms of treatment, like physiotherapy.
Alternatively, disc operations may be performed semi-urgently if your doctor is concerned about your symptoms becoming worse or causing significant disability.
Diskectomy (discectomy) involves accessing the spine then removing sections of the disc that are pressing on nerves.
Disc operations can be very successful at relieving the symptoms of disc herniation, including pain and ‘nerve symptoms’ like tingling and weakness in the legs. However, disc operations should not be used to treat general back pain.
Spinal stenosis surgery
Surgery may be considered if other treatments haven’t helped or if you’re disabled by your symptoms. The goals of surgery include relieving the pressure on your spinal cord or nerve roots by creating more space within the spinal canal. Surgery to decompress the area of stenosis is the most definitive way to try to resolve symptoms of spinal stenosis.
Research shows that spine surgeries result in fewer complications when done by highly experienced surgeons. Don’t hesitate to ask about your surgeon’s experience with spinal stenosis surgery. If you have any doubts, get a second opinion.
Examples of surgical procedures to treat spinal stenosis include:
In most cases, these space-creating operations help reduce spinal stenosis symptoms. But some people’s symptoms stay the same or get worse after surgery. Other surgical risks include infection, a tear in the membrane that covers the spinal cord, a blood clot in a leg vein and neurological deterioration.
Laminectomy
Laminectomy procedure removes the back part (lamina) of the affected vertebra. A laminectomy is sometimes called decompression surgery because it eases the pressure on the nerves by creating more space around them.
In some cases, that vertebra may need to be linked to adjoining vertebrae with metal hardware and a bone graft (spinal fusion) to maintain the spine’s strength.
Laminotomy
Laminotomy procedure removes only a portion of the lamina, typically carving a hole just big enough to relieve the pressure in a particular spot.
Laminoplasty
Laminoplasty procedure is performed only on the vertebrae in the neck (cervical spine). It opens up the space within the spinal canal by creating a hinge on the lamina. Metal hardware bridges the gap in the opened section of the spine.
Minimally invasive surgery
Minimally invasive surgery removes bone or lamina in a way that reduces the damage to nearby healthy tissue. This results in less need to do fusions.
While fusions are a useful way to stabilize the spine and reduce pain, by avoiding them you can reduce potential risks, such as post-surgical pain and inflammation and disease in nearby sections of the spine. In addition to reducing the need for spinal fusion, a minimally invasive approach to surgery has been shown to result in a shorter recovery time.
Back surgery complications
The incidence of complications after low back surgery is low. Risks for any type of surgery include bleeding, infection, and reaction to anesthesia. Complications that are specific to spine surgery include:
- Difficulty with urination (retention)
- Difficulty with intestinal function
- Heart attack
- Stroke
- Blood clots
- Recurrent disk herniation
- Problems related to rods or screws
- Nerve damage resulting in pain, numbness, and/or weakness
- Spinal headache
Warning Signs
Your doctor will talk with you about how to recognize the warning signs of a blood clot or infection. These complications are most likely to occur during the first few weeks after surgery.
Blood Clots
Warning signs of a blood clot include:
- Swelling in the calf, ankle or foot
- Tenderness or redness, which may extend above or below the knee
- Pain in the calf
Occasionally, a blood clot will travel through the bloodstream and may settle in the lungs. If this happens, you may experience sudden chest pain and shortness of breath or coughing. If you experience any of these symptoms, notify your doctor immediately. If you cannot reach your doctor, call 911 or have someone drive you to the hospital emergency room.
Infection
Infection following spine surgery occurs rarely. Warning signs of an infection include:
- Redness, tenderness, and swelling around the edges of the wound
- Drainage from the wound
- Pain or tenderness
- Shaking chills
- Elevated temperature, usually above 100°F if taken with an oral thermometer
If any of these symptoms occur, you should contact your doctor immediately or go to the nearest emergency room.
Failed back surgery syndrome
Failed back surgery syndrome is characterized by chronic pain that persists following spine surgery 2.
The International Association for the Study of Pain 3 defines failed back surgery syndrome as:
“Lumbar spinal pain of unknown origin either persisting despite surgical intervention or appearing after surgical intervention for spinal pain originally in the same topographical location.”
Failed back surgery syndrome is a term that defines an unsatisfactory result of a patient who suffered from spinal surgery regardless of the type and intervention area 4. Failed back surgery syndrome is associated with chronic pain in the lumbosacral area with or without radiation to the leg 5 and have had one or more surgical interventions that have failed to treat the pain 6. This can give rise to persistent pain and disability which often impose serious emotional and financial burden on the patient 7. This study 4 demonstrated that pain intensity, pain catastrophizing, and depression were significantly associated with clinical insomnia in failed back surgery syndrome patients.
A recent systematic literature review of discectomies for lumbar disc herniation in patients under the age of 70 years demonstrated a range of recurrent back or leg pain in 5%–36% of patients after 2 years 8. Another prospective study by Skolasky et al. 9 involving 260 patients who underwent a surgical laminectomy with or without fusion for lumbar spinal stenosis secondary to degenerative changes demonstrated that 29.2% of patients had either no change or increased pain after 12 months. Improved outcomes associated with failed back surgery syndrome will rely more on comprehensive knowledge of the physician in order to effectively prevent, diagnose, and treat failed back surgery syndrome.
Management of failed back surgery syndrome
The approach toward failed back surgery syndrome involves conservative management that first followed minimally invasive procedures, including injections, and finally surgical options as a last line therapy. In general, revision surgeries are not associated with improved pain scores and have a higher rate of comorbidities including increased bleeding, infections, acute respiratory distress syndrome, and longer hospital stays and even have higher mortality rates than the primary surgeries 10. Careful consideration of the type of therapy most appropriate for the treatment of failed back surgery syndrome is dependent on the etiology of the pain, likelihood that the intervention will succeed and the associated risks with the procedure. These risks include a return of symptoms and even an exacerbation of pain. All of these factors should be discussed with the patient and a consensus between the patient and physician should be made after careful consideration of the risks and benefits.
Conservative management
Physical therapy and medication management are the cornerstone of first-line management of failed back surgery syndrome. Physical therapy can help the patient optimize gait and posture and can improve muscle strength and physical function 11. Other conservative measures that may help postoperative back pain involve psychotherapy measures including stress reduction and cognitive behavioral therapy 12. Finally, noninvasive procedures including acupuncture and scrambler therapy can be used to minimize the pain associated with failed back surgery syndrome 13. These conservative measures should be done in conjunction with medication management to optimize pain relief.
Pharmacological management
Oral pharmacological treatment of failed back surgery syndrome is multimodal and increasingly controversial. Treatments include antiepileptics, Non-steroidal anti-inflammatory drugs, oral steroids, antidepressants, and opioids. Antiepileptics such as Gabapentin and Pregabalin can be used to treat neuropathic pain with failed back surgery syndrome and may play a role in preventing pain after surgery 14. Chronic opioid use is associated with a multitude of side effects including immunosuppression, androgen deficiency, constipation, and depression. Chronic opioid therapy for noncancer pain is associated with an increased morbidity and mortality and does not reliably improve long-term pain and function scores. As a result, there has been an increasing push by the government and medical community to minimize or even completely avoid the use of opioids for long-term pain 15.
Interventional pain procedures
Epidural injections
Epidural steroid injections are the most commonly performed procedure in pain clinics around the world 16. These can be administered primarily by three approaches: transforaminal, interlaminar, or caudally, and are indicated for symptoms of radiculopathy. Radicular symptoms in the failed back patient may be due to a multitude of reasons including herniated disc, postoperative adhesions, a thickened ligamentum flavum, spondylolisthesis with or without an associated pars defect, osteophyte formation from facet arthropathy or other degenerative changes that may lead to central or transforaminal stenosis. Epidural steroid injection can be a useful tool for both treating the symptoms of radicular back pain after surgery and preventing or delaying the need for surgery. A recent meta-analysis suggests that between one-third and one-half of patients considering surgery for spinal pain can avoid it in the short term with epidural steroid injection, although the evidence for this is stronger in patients who have not had prior surgery 17. In a separate retrospective study involving 69 patients with persistent radicular pain after back surgery, 26.8% of patients had at least 50% pain relief after transforaminal epidural steroid injection. This number increased to 43% in patients with recurrent disc herniation.
Optimization of analgesia with epidural steroid injections in patients with failed back surgery syndrome can be achieved when performed in conjunction with pharmacologic agents aimed at treating neuropathic pain. Zencirci et al. 18 demonstrated that adding Gabapentin to epidural steroid injection in patients with failed back surgery syndrome from at least two prior surgeries for lumbar disc herniation had significantly lower pain levels at 1 and 3 months compared with those who received epidural steroid injection while taking naproxen sodium, tizanidine, and vitamin B and C complex 18. This study underlies the importance of a multimodal approach to treating failed back surgery syndrome.
Adhesiolysis
Postoperative scar formation is a natural part of tissue healing after any surgery. Naturally, spine surgery will result in the formation of fibrotic adhesions within the epidural space. These adhesions may cause back and leg pain by compressing nerve roots, decreasing range of motion in the back and inducing pain with movement. Adhesions may contribute to or cause 20%–36% of failed back surgery syndrome cases and may act to compromise the efficacy of epidural steroid injection by creating septations within the epidural space that prevent steroid from acting on its intended target 19. Adhesions can theoretically be lysed, thereby improving baseline pain scores and drug delivery of the epidural steroid injection. Lysis of adhesions typically occurs by delivering hyaluronidase with hypertonic saline into the epidural space. The use of hyaluronidase with steroid may be more effective and have longer duration of effect than either one alone 20. Lysis of adhesion can also be done by means of epiduroscopy, which may allow the physician to directly visualize the adhesions in the epidural space. In a systematic review performed by Helm et al 21, seven randomized control trials and three observational studies of 45 studies that met criteria demonstrated that Level I or strong evidence that percutaneous lysis of adhesions is efficacious in the treatment of chronic back and extremity pain, with weaker Level II or III evidence for epiduroscopy based on one randomized controlled trial and three observational studies.
Radiofrequency ablation
Radiofrequency ablation of nerves are often used to provide sustained relief that a diagnostic block or therapeutic injection cannot provide. Successfully targeting the intended nerve is achieved, maximizing the size of the lesion. This can be done by performing multiple radiofrequency ablation in different locations, increasing the temperature and time of the ablation, using bipolar radiofrequency or cooled radiofrequency 22. Medial branch block or facet blocks are used as a diagnostic tool for facet-mediated pain. After a positive response, an radiofrequency ablation of the corresponding medial branches is expected to provide pain relief for 6–12 months up to 2 years 23. Sacroiliac joint injections can be used for both diagnostic and therapeutic purposes with the addition of steroid often being used to prolong the analgesic effect. Patients who get effective but short-term relief from sacroiliac joint injections are optimal candidates for radiofrequency ablation of the S1–S3 lateral branches and L5 dorsal ramus innervating the sacroiliac joint 24.
Neuromodulation
Spinal cord stimulation is a treatment modality that has shown tremendous potential in the management of failed back surgery syndrome. The advent of spinal cord stimulation came just 2 years after Melzak and Wall’s 1965 groundbreaking paper on Gate Theory with Shealy and Mortimer’s case study on the complete elimination of pain in a 70-year-old male with metastatic bronchogenic carcinoma by means of electrical stimulation of the dorsal columns 25. Today, the technology of spinal cord stimulation is more refined, and the proposed mechanism of how spinal cord stimulation works is believed to be more complex than just gate theory mechanics. It has been proposed that spinal cord stimulation-induced analgesia occurs not only by its effects on the spinal cord but supraspinal components of the central nervous system as well as by inducing descending inhibitory pathways and inhibiting pain facilitation 26.
The utility of spinal cord stimulation for pain associated with failed back surgery syndrome has been well-studied. The Prospective Randomized Controlled Multicenter Trial of the Effectiveness of Spinal Cord Stimulation demonstrated improved outcomes with spinal cord stimulation compared with conventional medical medicine alone in the treatment of neuropathic pain from failed back surgery syndrome. Metric measures included pain scores, quality of life, functional capacity, and patient satisfaction 27. More recently in the PRECISE Study, Zucco et al. 28 performed an observational, multicenter, longitudinal ambispective study on 80 patients with failed back surgery syndrome with predominant leg pain refractory to conventional medical medicine and followed them for up to 24 months after spinal cord stimulation. Although total societal costs increased after spinal cord stimulation placement, the authors concluded that spinal cord stimulation implantation would be cost-effective in 80%–85% when adjusting for quality-adjusted life years. This study underscores the continued costs of untreated failed back surgery syndrome on society as a whole, including loss of productivity, costs associated with disability, emergency room visits, imaging costs, and costs of medications and hospitalizations 28. Future studies include the Prospective, randomized study of multicolumn implantable lead stimulation for predominant low back pain (PROMISE) Study, which is a multicenter, prospective, randomized trial comparing spinal cord stimulation + conventional medical medicine with conventional medical medicine alone in patients with failed back surgery syndrome and predominantly lower back pain. The study aims to compare the outcomes such as pain scores, functional disability, return to work, and functional utilization between the two groups. Recruitment will end in 2016 29. Improved outcomes with failed back surgery syndrome will be expected with improving neuromodulation activities including “Burst” technology, higher frequency stimulation including 10 kHz, dorsal root ganglion stimulation, and peripheral nerve field stimulation.
Considerations for surgical revision
As mentioned earlier, surgical revision for failed back surgery syndrome is associated with a high morbidity with corresponding low rates of success. Arts et al 30 demonstrated only a 35% success rate 15 months after an instrumented fusion for the treatment of failed back surgery syndrome. These poor results demonstrate that the surgical option for the treatment of failed back surgery syndrome should be limited to last line therapy. With that being said, there are times when reoperation is mandated, such as loss of bowel or bladder function, motor weakness, and progressive neurological impairments from spinal cord injury, with relative indications being severe incapacitating radiculopathy, pseudoarthrosis, instability, and surgical hardware malfunction 31.
Lower back surgery recovery time
After your discharge from the hospital, you will need to carefully follow your doctor’s instructions to ensure a successful recovery.
You should arrange for transportation home after surgery. Once home, you may do as much for yourself as you can, as long as you maintain a balanced position of your spine. You can sit, stand, and go up and down stairs; however, you should avoid prolonged sitting or standing to allow your spine to heal from surgery. Do not hesitate to ask for help from family members or friends if it is needed. If necessary, the hospital can help you make arrangements in advance for a home health aide.
Wound Care
If your wound was closed with stitches (sutures) or staples, they will be removed approximately 2 weeks after surgery. If your wound was closed with absorbable sutures, they do not have to be removed. If you have wound drainage after you are home, cover the wound with a bandage and call your surgeon.
Diet
Some loss of appetite is common after surgery. During your recovery, it is important to eat well-balanced meals and drink plenty of fluids. Your doctor may recommend an iron supplement or vitamins before and after your surgery. It is not advisable to go on a weight loss diet right after surgery. The lack of essential nutrition may delay wound or bone healing. Instead, you should focus on eating nutritious foods and getting adequate quantities of protein and fiber. Ask your doctor if you have questions about your postoperative diet.
Activity
Many people experience a loss of energy after major surgery, but this improves over time. It is very important that you do not stay in bed for prolonged periods of time right after surgery. You should get up every hour or so and take at least a few steps. This will help with your rehabilitation and decrease the chance of blood clots. Your doctor may prescribe an exercise program designed to gradually increase your strength and stamina.
Initially, your doctor will recommend that you participate in light activity like walking. Later, you will be encouraged to swim or use an exercise bike or treadmill to improve your general physical condition.
Back surgery recovery
After you have recovered from your surgery, you may continue to have some achy pain in your low back that may be persistent. You can reduce this pain by staying in good physical condition. Once you recover, if you are overweight, you should enroll in a program to help you lose weight and keep it off.
Your doctor will evaluate you after your surgery to make sure that your recovery is progressing as expected.
- Mancuso CA, Reid MC, Duculan R, Girardi FP. Improvement in Pain After Lumbar Spine Surgery: The Role of Preoperative Expectations of Pain Relief. Clin J Pain. 2017;33(2):93-98. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5040610/[↩][↩][↩]
- Walker BF. Failed back surgery syndrome. COMSIG Rev. 1992;1(1):3-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2050006/pdf/cr011-003b.pdf[↩]
- Harvey AM. Classification of chronic pain – descriptions of chronic pain syndromes and definitions of pain terms. Clin J Pain. 1995;11(2):163[↩]
- Yun SY, Kim DH, Do HY, Kim SH. Clinical insomnia and associated factors in failed back surgery syndrome: a retrospective cross-sectional study. Int J Med Sci. 2017;14(6):536-542. Published 2017 Apr 9. doi:10.7150/ijms.18926 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5479122/[↩][↩]
- Bordoni B, Marelli F. Failed back surgery syndrome: review and new hypotheses. J Pain Res. 2016;9:17–22[↩]
- Baber Z, Erdek MA. Failed back surgery syndrome: current perspectives. J Pain Res. 2016;9:979-987. Published 2016 Nov 7. doi:10.2147/JPR.S92776 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5106227/[↩]
- Onesti ST. Failed back syndrome. Neurologist. 2004;10:259–64.[↩]
- Parker SL, Mendenhall SK, Godil SS, Sivasubramanian P, Cahill K, Ziewacz J, McGirt MJ. Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res. 2015;473(6):1988–1999.[↩]
- Skolasky RL, Wegener ST, Maggard AM, Riely LH., 3rd The impact of reduction of pain after lumbar spine surgery: the relationship between changes in pain and physical function and disability. Spine. 2014;39(17):1426–1432[↩]
- Diebo BG, Passias PG, Marascalchi BJ, Jalai CM, Worley NJ, Errico TJ, Lafage V. Primary versus revision surgery in the setting of adult spinal deformity: a nationwide study on 10,912 patients. Spine. 2015;40(21):1674–1680[↩]
- Delitto A, Piva SR, Moore CG, et al. Surgery versus nonsurgical treatment of lumbar spinal stenosis: a randomized trial. Ann Intern Med. 2015;162(7):465–473.[↩]
- Cramer H, Haller H, Lauche R, Dobos G. Mindfulness-based stress reduction for low back pain. a systematic review. BMC Complement Altern Med. 2012;12(1):162.[↩]
- Cho Y-H, Kim CK, Heo KH, et al. Acupuncture for acute postoperative pain after back surgery: a systematic review and meta-analysis of randomized controlled trials. Pain Pract. 2015;15(3):279–291.[↩]
- Canos A, Cort L, Fernández Y, Rovira V, Pallarés J, Barberá M, Morales-Suárez-Varela M. Preventive analgesia with pregabalin in neuropathic pain from “failed back surgery syndrome”: assessment of sleep quality and disability. Pain Med. 2015 Sep 23; Epub[↩]
- Katz JA, Swerdloff MA, Brass SD, Argoff CE, Markman J, Backonja M, Katz N. Opioids for chronic noncancer pain: a position paper of the American Academy of Neurology. Neurology. 2015;84(14):1503–1505[↩]
- Manchikanti L. The growth of interventional pain management in the new millennium: a critical analysis of utilization in the Medicare population. Pain Physician. 2004;7(4):465–482[↩]
- Bicket MC, Horowitz JM, Benzon HT, Cohen SP. Epidural injections in prevention of surgery for spinal pain: systematic review and meta-analysis of randomized controlled trials. Spine J. 2015;15(2):348–362[↩]
- Zencirci B. Analgesic efficacy of oral gabapentin added to standard epidural corticosteroids in patients with failed back surgery. Clin Pharmacol. 2010;2:207–211[↩][↩]
- Rahimzadeh P, Sharma V, Imani F, Faiz HR, Ghodraty MR, Nikzad-Jamnani AR, Nader ND. Adjuvant hyaluronidase to epidural steroid improves the quality of analgesia in failed back surgery syndrome: a prospective randomized clinical trial. Pain Physician. 2014;17(1):E75–E82[↩]
- Kim SB, Lee KW, Lee JH, Kim MA, An BW. The effect of hyaluronidase in interlaminar lumbar epidural injection for failed back surgery syndrome. Ann Rehabil Med. 2012;36(4):466–473.[↩]
- Helm Ii S, Racz GB, Gerdesmeyer L, et al. Percutaneous and endoscopic adhesiolysis in managing low back and lower extremity pain: a systematic review and meta-analysis. Pain Physician. 2016;19(2):E245–E281[↩]
- Costandi S, Garcia-Jacques M, Dews T, et al. Optimal temperature for radiofrequency ablation of lumbar medial branches for treatment of facet – mediated back pain. Pain Pract. 2015 Sep 15; Epub.[↩]
- McCormick ZL, Marshall B, Walker J, McCarthy R, Walega DR. Long-Term Function, Pain and Medication Use Outcomes of Radiofrequency Ablation for Lumbar Facet Syndrome. Int J Anesth Anesth. 2015;2(2) pii:028.[↩]
- Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Rev Neurother. 2013;13(1):99–116.[↩]
- Melzack R, Wall PD. Pain mechanisms: a new theory. Survey Anesth. 1967;11(2):89–90[↩]
- Guan Y. Spinal cord stimulation: neurophysiological and neurochemical mechanisms of action. Curr Pain Headache Rep. 2012;16(3):217–225[↩]
- Kumar K, Taylor RS, Jacques L, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007;132(1):179–188[↩]
- Zucco F, Ciampichini R, Lavano A, et al. Cost-effectiveness and cost-utility analysis of spinal cord stimulation in patients with failed back surgery syndrome: results from the PRECISE study. Neuromodulation. 2015;18(4):266–276.[↩][↩]
- Rigoard P, Desai MJ, North RB, et al. Spinal cord stimulation for predominant low back pain in failed back surgery syndrome: study protocol for an international multicenter randomized controlled trial (PROMISE study) Trials. 2013;14(1):376 [↩]
- Arts MP, Kols NI, Onderwater SM, Peul WC. Clinical outcome of instrumented fusion for the treatment of failed back surgery syndrome: a case series of 100 patients. Acta Neurochir. 2012;154(7):1213–1217[↩]
- Hussain A, Erdek M. Interventional pain management for failed back surgery syndrome. Pain Practice. 2014;14(1):64–78[↩]