Contents
What is bicornuate uterus
Bicornate uterus (also called heart-shaped uterus), is a congenital (present at birth) condition where the uterus has two cavities (spaces) instead of one large cavity 1. Most women with this condition don’t need surgery to repair it.
Bicornuate uterus has a prevalence of 0.4% in the general population 2. A 2011 review shows that bicornuate uteri are more prevalent and certainly not uncommon, in women with infertility (1.1%) 2. It is often asymptomatic before puberty and thereafter has a significant association with infertility and miscarriage 2.
A bicornuate uterus consists of two symmetric uterine horns unified by caudal fusion. Both endometrial cavities communicate with the vagina either through a single uterine cervix (unicollis, most frequent) or through two uterine cervices (bicollis, less frequent). The occurrence of cervical atresia with bicornuate uterus is rare 3. Patients may present with pelvic pain due to hematometra and retrograde menstruation from a non-communicating uterine horn 3. Treatment options are controversial and include hysterectomy or utero-vaginal canalization with the principal goal of relieving the symptoms and preserving fertility 4.
Figure 1. Bicornuate uterus
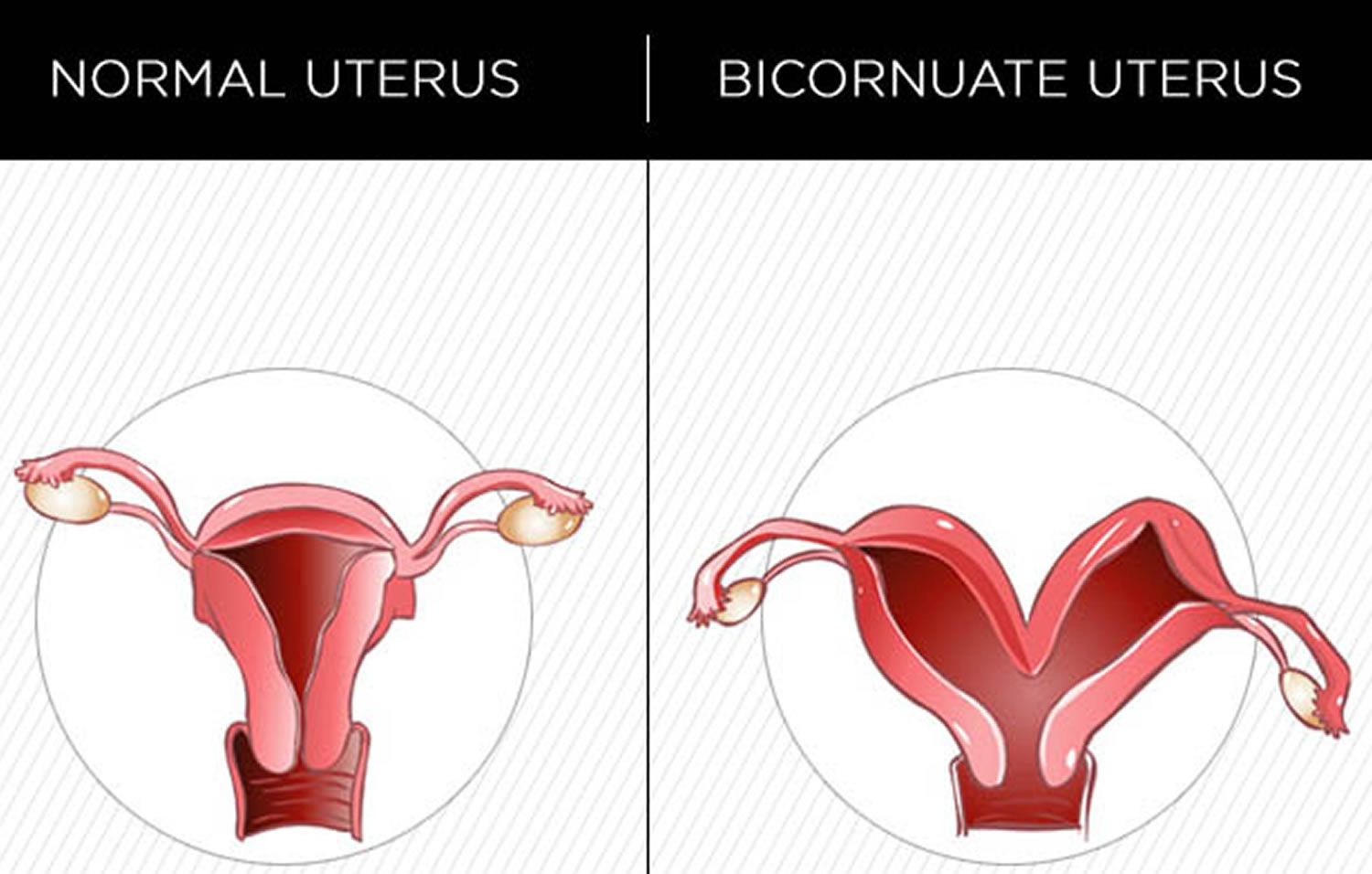
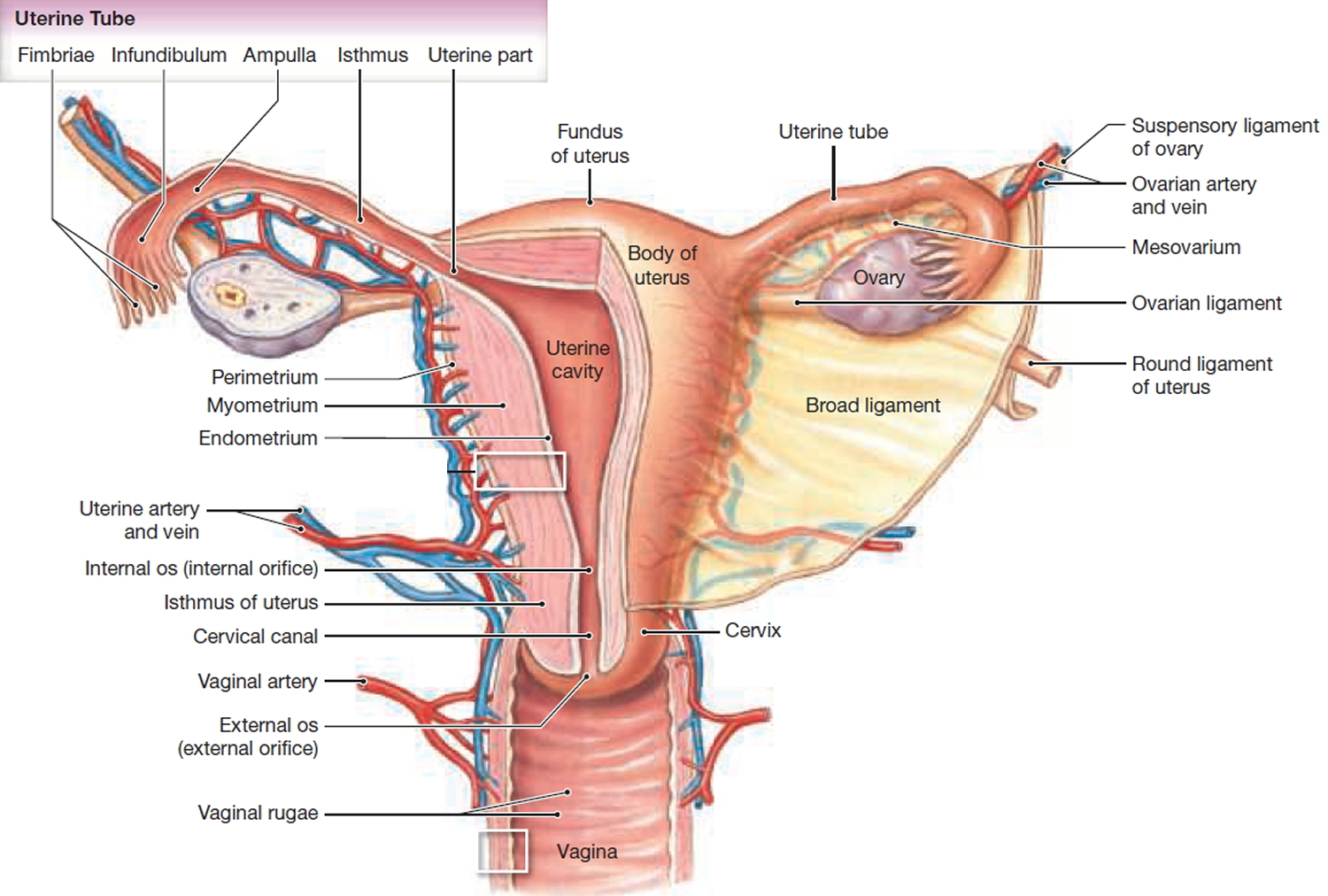
Figure 2. Normal uterus
Bicornuate uterus causes
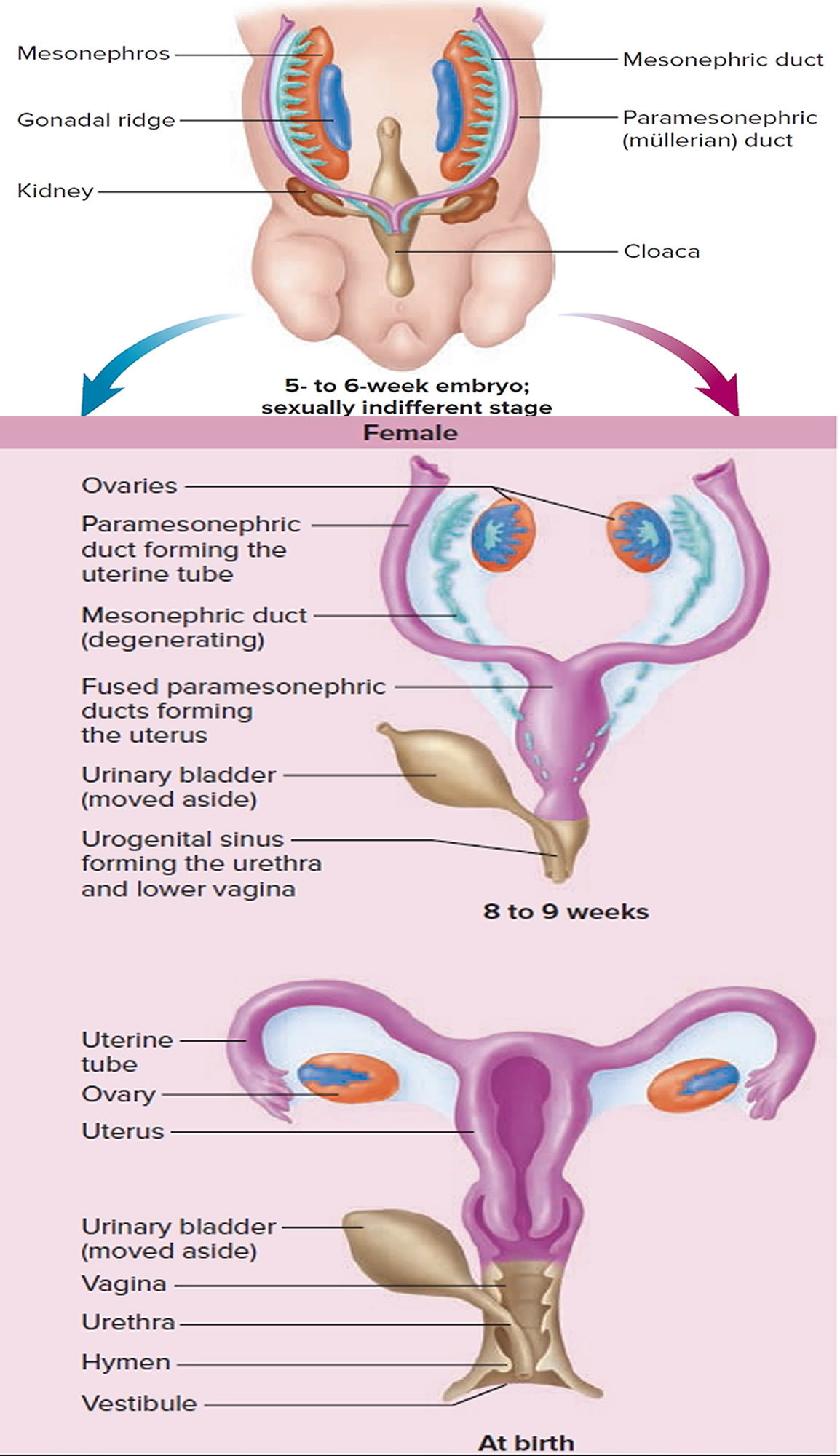
The uterus is formed during embryogenesis by the fusion of the two paramesonephric ducts, usually at about 10 weeks gestation (10 weeks of pregnancy) to form the uterus (see Figure 3. Uterus embyology). For some baby girls, the lack of fusion and incomplete fusion of the paramesonephric ducts lead to various types of malformations of the female genital tract 5. The most common mullerian anomalies include uterine septum, unicornuate uterus, bicornuate uterus and uterus didelphys (uterus malformation where the uterus is present as a paired organ) 6.
In the bicornuate uterus, the lower uterus and cervix are completely fused, resulting in 2 separate but communicating endometrial cavities, a single-chamber cervix and vagina. A muscular intrauterine septum is also present, and this defect corresponds externally to an indentation or groove at the fundus. Subclassification into complete or partial categories depends on septum length. Complete uterine septa that extend either to the internal or external os are known as bicornuate unicollis uterus and bicornuate bicollis uterus.
Figure 3. Uterus embryology
Bicornuate uterus symptoms
Bicornuate uterus does not reduce fertility 7, but may present with menstrual abnormalities or miscarriages or may be asymptomatic only to be discovered during pregnancy or at the time of abortion or during evaluation for infertility 8. This may be during management for miscarriages, caesarean delivery, or hysteroscopy or following hysterosalpingography for fertility workup 9.
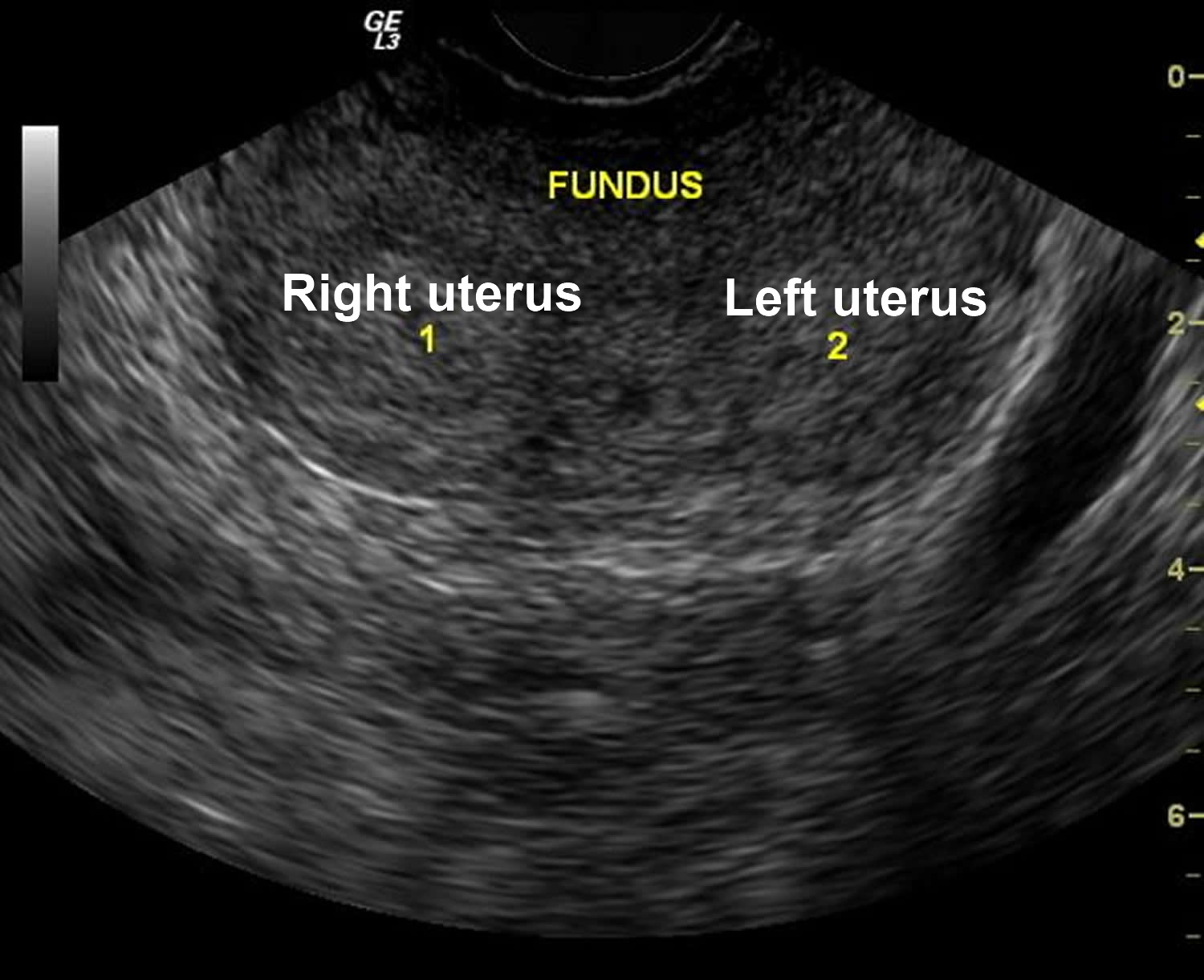
Women with uterine anomalies may go through their reproductive functions undetected but when uterine anomaly is associated with reproductive failure such as recurrent miscarriages, recurrent preterm deliveries or infertility, the relevant investigations often reveal the anomalies. Sonography is useful in diagnosing uterine anomalies in experienced hands as the investigation is operator-dependent. Pregnancy with associated uterine anomaly should be managed conservatively with extra care. High index of suspicion is required in order to diagnose this uncommon anomaly.
Bicornuate uterus can be diagnosis by method of ultrasonography, MRI, hysterosalpingogram (is an X-ray test where the radiographic contrast (dye) is injected into the uterine cavity through the vagina and cervix), hysteroscopy and laparoscopy.
Figure 4. Bicornuate uterus ultrasound
Bicornuate uterus and pregnancy
Most women with uterine anomalies are asymptomatic and can carry a pregnancy to term and delivery without complications 10. A woman with a bicornuate uterus has a 62.5% chance of having a live birth 11, 12. In a case report, a woman had had five consecutive uncomplicated live births, that is 82.3% of all her pregnancies and a miscarriage in the index pregnancy 10. This has shown that pregnancy outcome may be good in women with bicornuate uteri.
In a 2011 systematic review 7 between different types of congenital uterine anomaly and various reproductive outcomes. Unification defects, such as the bicornuate, unicornuate and didelphic uterus, do not appear to reduce fertility but are associated with aberrant outcomes throughout the course of pregnancy 7. The exact effects are, however, dependent on the type of anomaly. Women with bicornuate and unicornuate uteri have an increased risk of miscarriage, preterm birth and fetal malpresentation while women with uterus didelphys seem to have only a modestly increased risk of preterm labor 7. These findings are consistent with those of previous studies 13, 14, 15, 16.
A retrospective review of reproductive performance in patients with untreated uterine anomalies has suggested that these women experience high rates of miscarriage and preterm delivery and a term delivery rate of about 50% 17. It has also been shown that in general, complications such as preterm delivery and first trimester miscarriages are higher in women with abnormal uteri 18. Women with bicornuate uteri have a 62.5% chance of having a live birth and 25% risk of preterm birth and spontaneous abortion 18. It may rarely be misdiagnosed for ectopic pregnancy as the pregnant horn may sonographically resemble an ectopic with the attendant nonpregnant uterus.
Can congenital uterine conditions cause problems during pregnancy ?
Yes. Some may not cause any problems at all. But some may increase your chances of having these complications:
- Premature birth. This is birth that happens too early, before 37 weeks of pregnancy.
- Birth defects (called deformation birth defects) that may be caused by restricting (limiting) growth of parts of a baby in the womb causing those parts to be deformed. Birth defects are health conditions that are present at birth. Birth defects change the shape or function of one or more parts of the body. They can cause problems in overall health, how the body develops, or in how the body works.
- Slow growth in your baby
- Breech position or other problems with the baby’s position in the womb. Breech position is when your baby’s bottom or feet are facing down right before birth. The best position for birth is when your baby is head-down.
- Needing to have a cesarean birth (also called c-section). This is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus.
- Miscarriage.
Figure 5. Bicornuate uterus and pregnancy
- Uterine conditions. March of Dimes Foundation. https://www.marchofdimes.org/complications/uterine-conditions.aspx[↩]
- The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. Hum Reprod Update. 2011 Nov-Dec; 17(6):761-71. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3191936/[↩][↩][↩]
- Massive Hematometra due to Congenital Cervicovaginal Agenesis in an Adolescent Girl Treated by Hysterectomy: A Case Report. Gasim T, Al Jama FE. Case Rep Obstet Gynecol. 2013; 2013():640214. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3600265/[↩][↩]
- Xie Z, Zhang X, Liu J, et al. Clinical characteristics of congenital cervical atresia based on anatomy and ultrasound: a retrospective study of 32 cases. European Journal of Medical Research. 2014;19(1):10. doi:10.1186/2047-783X-19-10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3996070/[↩]
- Reproductive outcomes in women with uterine anomalies. Lin PC. J Womens Health (Larchmt). 2004 Jan-Feb; 13(1):33-9. https://www.ncbi.nlm.nih.gov/pubmed/15006276/[↩]
- Nwosu B, Ogboaja JO, Obi-Nwosu A. Spontaneous rupture of the gravid horn of bicornuate uterus at term. Nig Med J. 2010;5(4):184–185.[↩]
- Chan, Y. Y., Jayaprakasan, K., Tan, A., Thornton, J. G., Coomarasamy, A. and Raine-Fenning, N. J. (2011), Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet Gynecol, 38: 371–382. doi:10.1002/uog.10056[↩][↩][↩][↩]
- Uterus didelphys: a report of 26 cases. Heinonen PK. Eur J Obstet Gynecol Reprod Biol. 1984 Jul; 17(5):345-50. https://www.ncbi.nlm.nih.gov/pubmed/6479426/[↩]
- Congenital Müllerian anomalies: diagnostic accuracy of three-dimensional ultrasound. Raga F, Bonilla-Musoles F, Blanes J, Osborne NG. Fertil Steril. 1996 Mar; 65(3):523-8. https://www.ncbi.nlm.nih.gov/pubmed/8774280/[↩]
- Aliyu L, Abdullahi M. BICORNUATE UTERUS MIMICKING ECTOPIC PREGNANCY – A case report . Journal of the West African College of Surgeons. 2012;2(1):84-90. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4170284/[↩][↩]
- Solimi B, Pallab Kumar M. win pregnancy in a woman with uterus didelphys. Online Journal of Health & Allied Sciences, 2010;9(4):162–4.[↩]
- Braun P, Grau FV, Pons RM, Enquix DP. Is HSG able to diagnose all uterine malformations correctly? A retrospective study. Eur J Radiol. 2005;;53:274–279. https://www.ncbi.nlm.nih.gov/pubmed/15664292[↩]
- Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update 2001; 7: 161–174. https://www.ncbi.nlm.nih.gov/pubmed/11284660[↩]
- Heinonen PK, Saarikoski S, Pystynen P. Reproductive performance of women with uterine anomalies. An evaluation of 182 cases. Acta Obstet Gynecol Scand 1982; 61: 157–162. https://www.ncbi.nlm.nih.gov/pubmed/7113692[↩]
- Reichman D, Laufer MR, Robinson BK. Pregnancy outcomes in unicornuate uteri: a review. Fertil Steril 2009; 91: 1886–1894. https://www.ncbi.nlm.nih.gov/pubmed/18439594[↩]
- Lin PC. Reproductive outcomes in women with uterine anomalies. J Womens Health (Larchmt). 2004; 13: 33–39. https://www.ncbi.nlm.nih.gov/pubmed/15006276[↩]
- Reproductive impact of congenital Müllerian anomalies. Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simón C, Pellicer A. Hum Reprod. 1997 Oct; 12(10):2277-81. https://www.ncbi.nlm.nih.gov/pubmed/9402295/[↩]
- Is hysterosalpingography able to diagnose all uterine malformations correctly? A retrospective study. Braun P, Grau FV, Pons RM, Enguix DP. Eur J Radiol. 2005 Feb; 53(2):274-9. https://www.ncbi.nlm.nih.gov/pubmed/15664292/[↩][↩]