Contents
What is bladder spasms
Bladder spasms also known as overactive bladder syndrome, is a symptom-based clinical diagnosis. It is characterized by a sudden urge to urinate, urinary frequency and nocturia (excessive urination at night time disrupting sleep), with or without urge urinary incontinence 1. The urge may be difficult to stop, and overactive bladder may lead to the involuntary loss of urine (urge incontinence) 2.
Bladder spasms can have a significant effect on quality of life, you may feel embarrassed, isolate yourself, or limit your work and social life. The good news is that a brief evaluation can determine whether there’s a specific cause for your overactive bladder symptoms.
Overactive bladder syndrome affects 12–17% of the population. Prevalence increases with age. The management of overactive bladder syndrome involves exclusion of underlying pathology. First line treatment includes lifestyle interventions, pelvic floor exercises, bladder training and antimuscarinic agents. Failure of conservative management necessitates second line therapies, which are more invasive and include botulinum toxin, neuromodulation or surgical interventions such as augmentation cystoplasty or urinary diversion.
Management of bladder spasms often begins with behavioral strategies, such as fluid schedules, timed voiding and bladder-holding techniques using your pelvic floor. If these initial efforts don’t help enough with your overactive bladder symptoms, medications are available.
Figure 1. Urinary bladder location
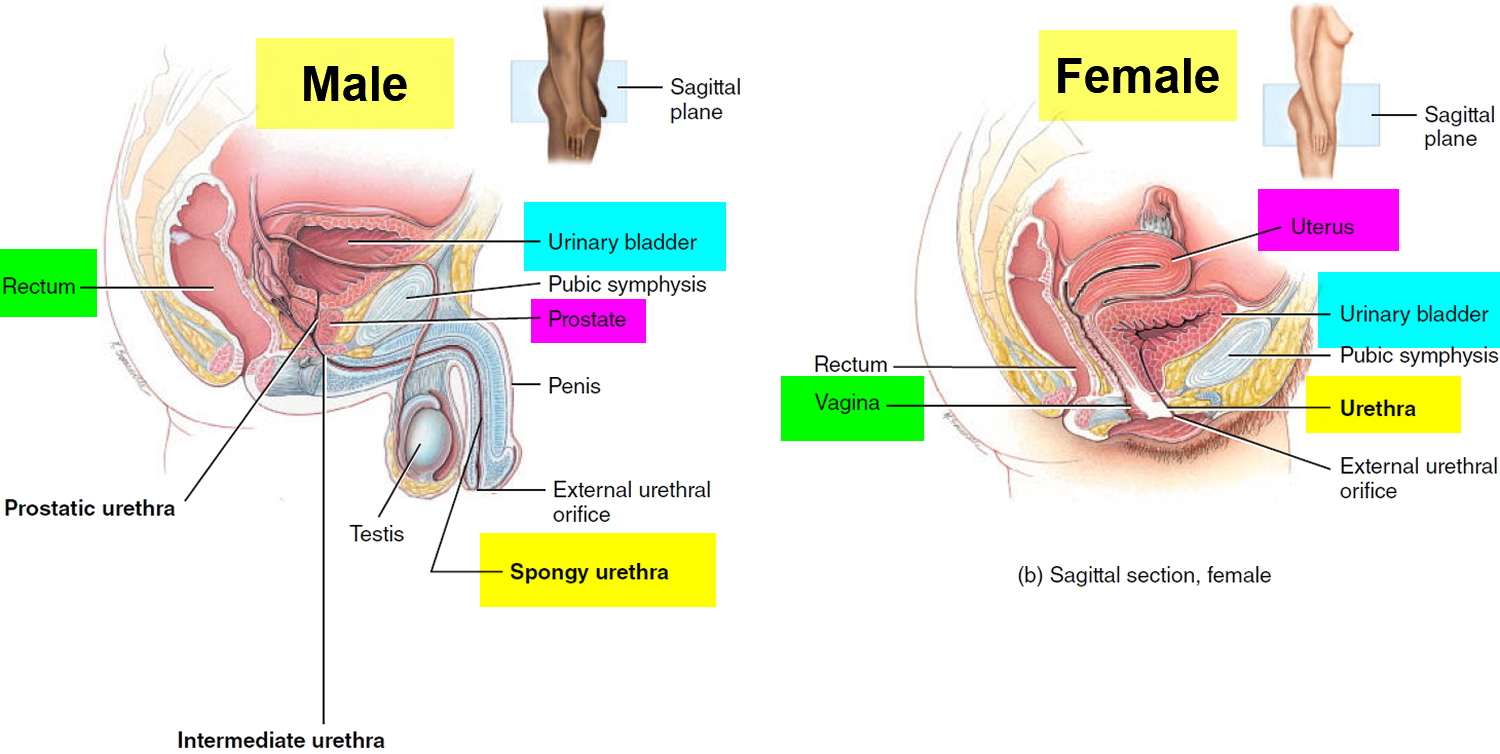
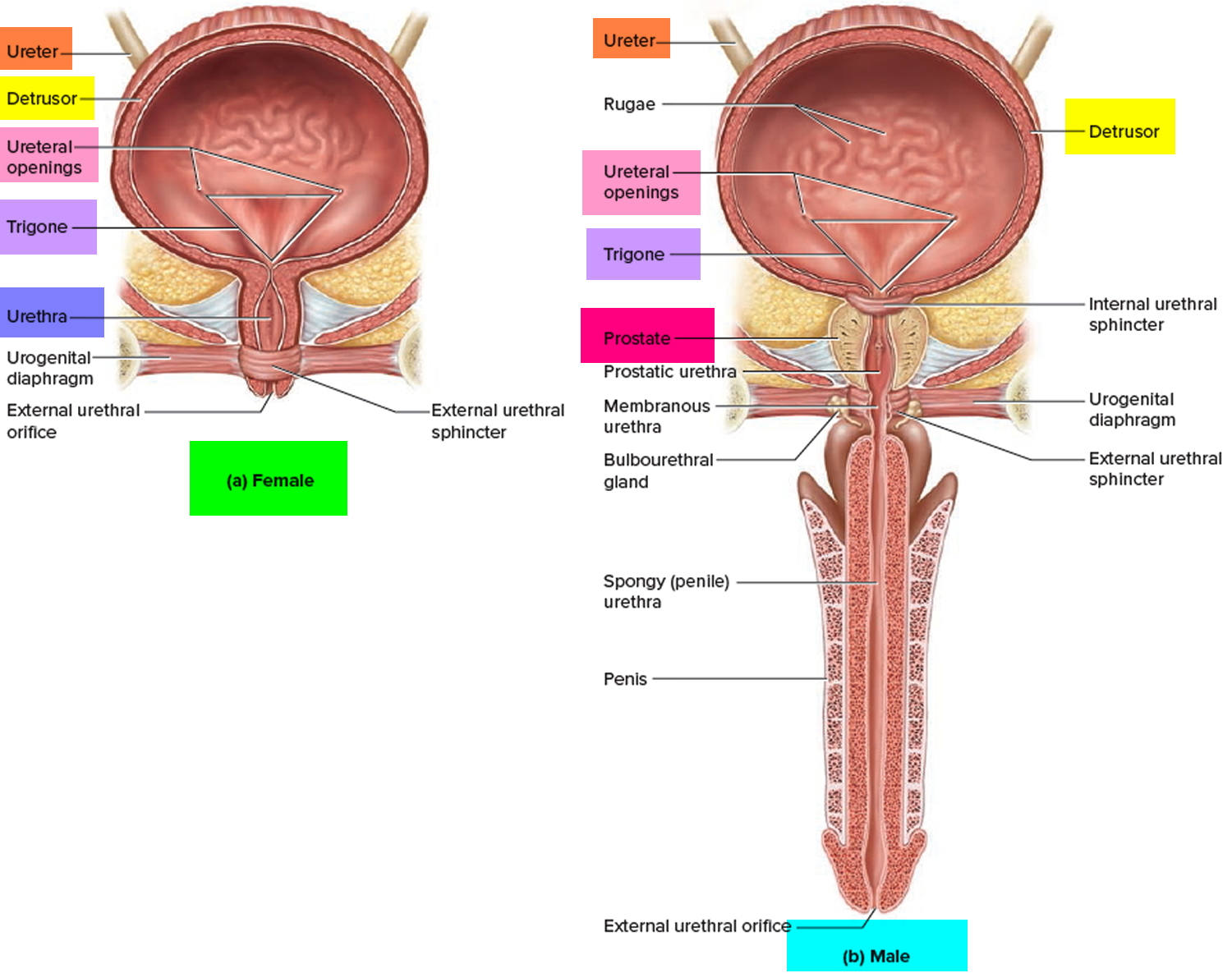
Figure 2. Urinary bladder anatomy
Symptoms of bladder spasms
With an overactive bladder, you may:
- Feel a sudden urge to urinate that’s difficult to control
- Experience urge incontinence — the involuntary loss of urine immediately following an urgent need to urinate
- Urinate frequently, usually eight or more times in 24 hours
- Awaken two or more times in the night to urinate (nocturia)
Although you may be able to get to the toilet in time when you sense an urge to urinate, unexpected frequent urination and nighttime urination can disrupt your life.
When to see a doctor
Although it’s not uncommon among older adults, bladder spasms isn’t a normal part of aging. If your symptoms distress you or disrupt your life, talk to your doctor. Treatments are available that might help you.
Discussing such a private matter with your doctor might not be easy, but it’s worthwhile to take that risk — especially if your symptoms disrupt your work schedule, social interactions and everyday activities.
What causes bladder spasms
Normal bladder function
The urinary bladder is a hollow, collapsible muscular sac that stores and expels urine situated in the pelvic cavity posterior to the pubic symphysis. When slightly distended due to the accumulation of urine, the urinary bladder is spherical. When it is empty, it collapses. As urine volume increases, it becomes pear shaped and rises into the abdominal cavity.
Urinary bladder capacity averages 700–800 mL. It is smaller in females because the uterus occupies the space just superior to the urinary bladder.
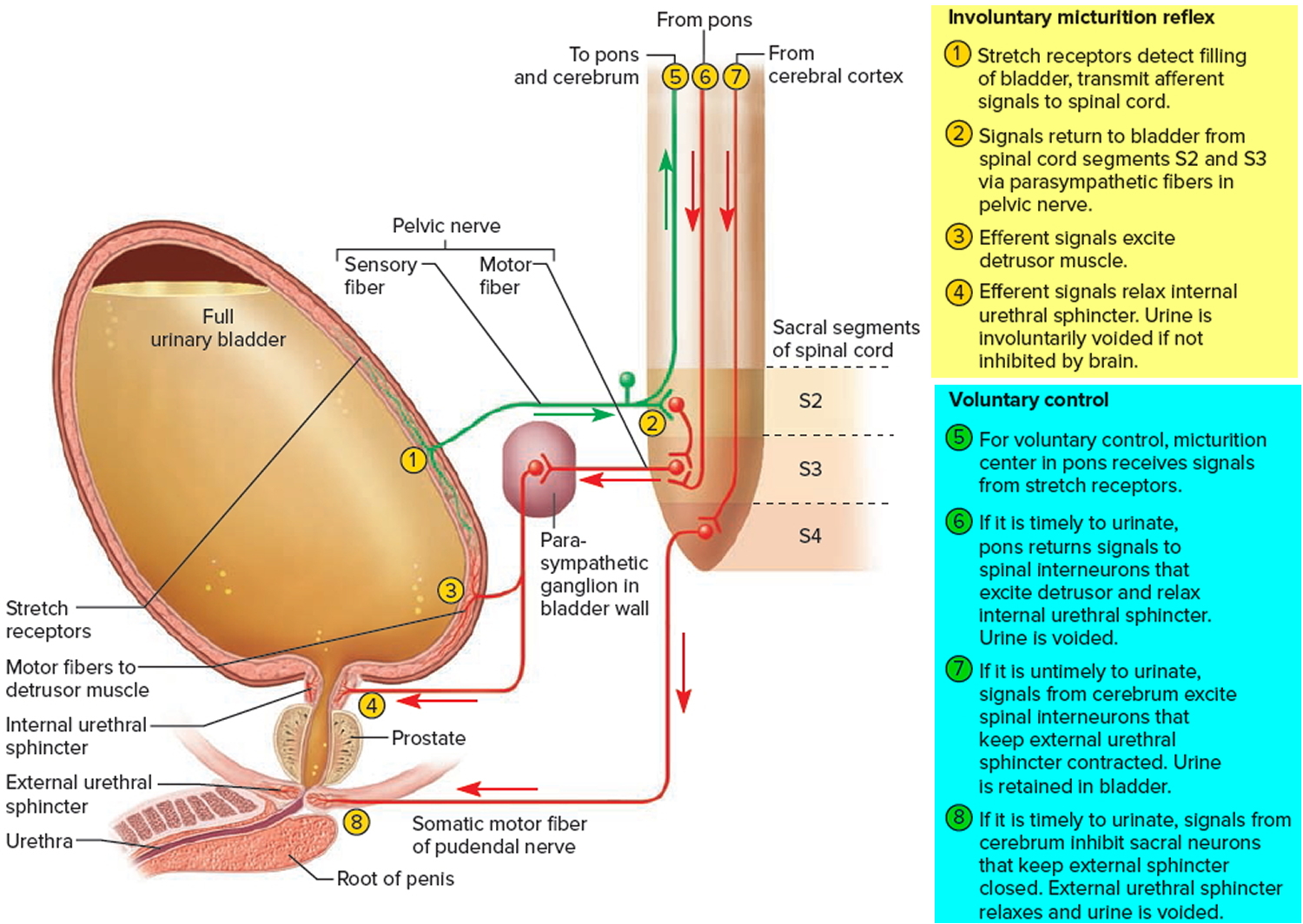
For the urinary system to do its job, muscles and nerves must work together to hold urine in the bladder and then release it at the right time. Nerves carry messages from the bladder to the brain to let it know when the bladder is full. They also carry messages from the brain to the bladder, telling muscles either to tighten or release. A nerve problem might affect your bladder control if the nerves that are supposed to carry messages between the brain and the bladder do not work properly.
Discharge of urine from the urinary bladder, called micturition, is also known as urination or voiding. Micturition occurs via a combination of involuntary and voluntary muscle contractions. When the volume of urine in the urinary bladder exceeds 200–400 mL, pressure within the bladder increases considerably, and stretch receptors in its wall transmit nerve impulses into the spinal cord. These impulses propagate to the micturition center in sacral spinal cord segments S2 and S3 and trigger a spinal reflex called the micturition reflex. In this reflex arc, parasympathetic impulses from the micturition center propagate to the urinary bladder wall and internal urethral sphincter.
The nerve impulses cause contraction of the detrusor muscle and relaxation of the internal urethral sphincter muscle. Simultaneously, the micturition center inhibits somatic motor neurons that innervate skeletal muscle in the external urethral sphincter. On contraction of the urinary bladder wall and relaxation of the sphincters, urination takes place. Urinary bladder filling causes a sensation of fullness that initiates a conscious desire to urinate before the micturition reflex actually occurs. Although emptying of the urinary bladder is a reflex, in early childhood we learn to initiate it and stop it voluntarily.
Human bladder contraction is mediated mainly through stimulation of muscarinic receptors in the detrusor muscle by acetylcholine 3. Antimuscarinic agents act during the filling/storage phase of the micturition cycle by inhibiting afferent (sensory) input from the bladder, and directly inhibiting smooth muscle contractility 4. They are competitive antagonists, so with massive release of acetylcholine during micturition the drug effect is decreased and the muscle can contract 5.
Through learned control of the external urethral sphincter muscle and certain muscles of the pelvic floor, the cerebral cortex can initiate micturition or delay its occurrence for a limited period.
Figure 3. Bladder control
Involuntary bladder contractions
Bladder spasms occurs because the muscles of the bladder start to contract involuntarily even when the volume of urine in your bladder is low. This involuntary contraction creates the urgent need to urinate.
Overactive bladder symptoms are usually associated with involuntary contractions of the detrusor (bladder) muscle, which can result in urge incontinence, depending on the response of the sphincter 6. The most common cause of overactive bladder symptoms is detrusor overactivity 3; 64% of all patients with overactive bladder symptoms have detrusor overactivity on cystometry, and 69% of men and 44% of women with urgency have detrusor overactivity 7. Detrusor overactivity is thought to result not only from efferent (motor) hyper function/dysfunction but also most likely by afferent (sensory) noise. Patients with overactive bladder symptoms seem to respond to antimuscarinic treatment irrespective of the presence of detrusor overactivity 8.
Several conditions may contribute to signs and symptoms of overactive bladder, including:
- Neurological disorders, such as stroke and multiple sclerosis
- Diabetes
- Medications that cause a rapid increase in urine production or require that you take them with lots of fluids
- Acute urinary tract infections that can cause symptoms similar to an overactive bladder
- Abnormalities in the bladder, such as tumors or bladder stones
- Factors that obstruct bladder outflow — enlarged prostate, constipation or previous operations to treat other forms of incontinence
- Excess consumption of caffeine or alcohol
- Declining cognitive function due to aging, which may make it more difficult for your bladder to understand the signals it receives from your brain
- Difficulty walking, which can lead to bladder urgency if you’re unable to get to the bathroom quickly
- Incomplete bladder emptying, which may lead to symptoms of overactive bladder, as you have little urine storage space left
The specific cause of an overactive bladder may be unknown.
Risk factors for bladder spasms
As you age, you’re at increased risk of developing overactive bladder. You’re also at higher risk of diseases and disorders, such as enlarged prostate and diabetes, which can contribute to other problems with bladder function.
Many people with cognitive decline — for instance, after a stroke or with Alzheimer’s disease — develop an overactive bladder. Incontinence that results from situations like this can be managed with fluid schedules, timed and prompted voiding, absorbent garments, and bowel programs.
Other risk factors include: vaginal birth delivery 9, with 40% of parous women experiencing urge urinary incontinence, older age, obesity and chronic constipation 10. Childhood urinary symptoms in women have been found to be independently associated with adult lower urinary tract symptoms, specifically urgency, frequency and nocturia 11.
Some people with an overactive bladder also have bowel control problems; tell your doctor if this is a problem for you.
Complications of bladder spasms
Any type of incontinence can affect your overall quality of life. If your overactive bladder symptoms cause a major disruption to your life, you might also have:
- Emotional distress or depression
- Anxiety
- Sleep disturbances and interrupted sleep cycles
- Issues with sexuality
Your doctor might recommend treatment of associated conditions, to see if effective treatment of an associated condition will help with your urinary symptoms.
Some women also may have a disorder called mixed incontinence, when both urge and stress incontinence occur. Stress incontinence is the loss of urine when you exert physical stress or pressure on your bladder, such as during activities that include running or jumping. Treatment of the stress incontinence is not likely to help the overactive bladder symptoms.
Older people may have a common combination of bladder storage problems and bladder-emptying issues. The bladder may cause a lot of urgency and even incontinence, but it doesn’t empty well. A specialist may be able to help you with this combination of bladder problems.
Prevention of bladder spasms
These healthy lifestyle choices may reduce your risk of overactive bladder:
- Maintain a healthy weight.
- Get regular, daily physical activity and exercise.
- Limit consumption of caffeine and alcohol.
- Quit smoking.
- Manage chronic conditions, such as diabetes, that might contribute to overactive bladder symptoms.
- Learn where your pelvic floor muscles are and then strengthen them by doing Kegel exercises — tighten (contract) muscles, hold the contraction for two seconds and relax muscles for three seconds. Work up to holding the contraction for five seconds and then 10 seconds at a time. Do three sets of 10 repetitions each day.
Diagnosis of overactive bladder syndrome
If you have an abnormal urge to urinate, your doctor will check to make sure that you don’t have an infection or blood in your urine. Your doctor may also want to make sure that you’re emptying your bladder completely when you urinate.
Your doctor will look for clues that might also indicate contributing factors. The work-up will likely include a:
- Medical history
- Physical exam, focusing on your abdomen and genitals
- Urine sample to test for infection, traces of blood or other abnormalities
- Focused neurological exam that may identify sensory problems or abnormal reflexes
Special tests
Your doctor may order a simple urodynamic test to assess the function of your bladder and its ability to empty steadily and completely. These tests usually require a referral to a specialist, and may not be necessary to make a diagnosis or begin treatment. Tests include:
- Measuring urine left in the bladder. This test is important if your bladder doesn’t empty completely when you urinate or experience urinary incontinence. Remaining urine (postvoid residual urine) may cause symptoms identical to an overactive bladder. To measure residual urine after you have voided, your doctor may request an ultrasound scan of your bladder or pass a thin tube (catheter) through the urethra and into your bladder to drain and measure the remaining urine.
- Measuring urine flow rate. To measure the volume and speed of your voiding, you may be asked to urinate into a uroflowmeter. This device translates the data into a graph of changes in your flow rate.
- Testing bladder pressures. Cystometry measures pressure in your bladder and in the surrounding region during bladder filling. During this test, your doctor uses a thin tube (catheter) to fill your bladder slowly with warm water. Another catheter with a pressure-measuring sensor is placed in your rectum or, if you’re a woman, in your vagina.This procedure can identify whether you have involuntary muscle contractions or a stiff bladder that’s not able to store urine under low pressure.
Your doctor will review the results of any tests with you and suggest a treatment strategy.
Treatment of overactive bladder syndrome
A combination of treatment strategies may be the best approach to relieve overactive bladder symptoms.
Behavioral interventions
Behavioral interventions are the first choice in helping manage an overactive bladder. They’re often effective, and they carry no side effects.
Behavioral treatments have been shown to be effective in older adults, reducing leakage by 50–80% 12. Behavioral training requires a highly motivated patient, and 20–30% will become dry. As behavioral treatments work gradually at first and rely on patient self management.
Behavioral interventions may include:
Pelvic floor muscle exercises
Kegel exercises strengthen your pelvic floor muscles and urinary sphincter. These strengthened muscles can help you stop the bladder’s involuntary contractions.
Your doctor or a physical therapist can help you learn how to do Kegel exercises correctly. It may take as long as six to eight weeks before you notice a difference in your symptoms.
What are Kegel exercises ?
To do Kegel exercises, you just squeeze your pelvic floor muscles. The part of your body including your hip bones is the pelvic area. At the bottom of the pelvis, several layers of muscle stretch between your legs. The muscles attach to the front, back, and sides of the pelvic bone.
Kegel exercises are designed to make your pelvic floor muscles stronger. These are the muscles that hold up your bladder and help keep it from leaking.
Building up your pelvic muscles with Kegel exercises can help with your bladder control.
How do you exercise your pelvic muscles ?
Find the right muscles. Try one of the following ways to find the right muscles to squeeze.
- Imagine that you are trying to stop passing gas. Squeeze the muscles you would use. If you sense a “pulling” feeling, you are squeezing the right muscles for pelvic exercises.
- Imagine that you are sitting on a marble and want to pick up the marble with your vagina. Imagine “sucking” the marble into your vagina.
- If you still are not sure you are tightening the right muscles: Lie down and put your finger inside your vagina. Squeeze as if you were trying to stop urine from coming out. If you feel tightness on your finger, you are squeezing the right pelvic muscles.
Once you know what the movement feels like, do Kegel exercises three times a day:
- Make sure your bladder is empty, then sit or lie down.
- Tighten the pelvic floor muscles. Hold tight and count to 6 to 8.
- Relax the muscles and count to 10.
- Repeat 10 times, three times a day (morning, afternoon, and night).
At first, find a quiet spot to practice—your bathroom or bedroom—so you can concentrate. Lie on the floor. Pull in the pelvic muscles and hold for a count of 6 to 8. Then relax for a count of 10. Work up to 10 to 15 repeats each time you exercise.
Do your pelvic exercises at least three times a day. Every day, use three positions: lying down, sitting, and standing. You can exercise while lying on the floor, sitting at a desk, or standing in the kitchen. Using all three positions makes the muscles strongest.
Breathe deeply, and relax your body when you are doing these exercises. Make sure you are not tightening your stomach, thigh, buttock, or chest muscles.
After 4 to 6 weeks, you should feel better and have fewer symptoms. Keep doing the exercises, but do not increase how many you do. Overdoing it can lead to straining when you urinate or move your bowels.
Some notes of caution:
- Once you learn how to do them, do not practice Kegel exercises at the same time you are urinating more than twice a month. Doing the exercises while you are urinating can weaken your pelvic floor muscles over time.
- In women, doing Kegel exercises incorrectly or with too much force may cause vaginal muscles to tighten too much. This can cause pain during sexual intercourse.
- Incontinence will return if you stop doing these exercises. Once you start doing them, you may need to do them for the rest of your life.
It may take several months for your incontinence to lessen once you start doing these exercises.
Let your doctor, nurse, or therapist help you. Many people have trouble finding the right muscles. Your doctor, nurse, or therapist can check to make sure you are doing the exercises correctly. You can also exercise by using special weights or biofeedback. Ask your health care team about these exercise aids.
Don’t squeeze other muscles at the same time. Be careful not to tighten your stomach, legs, or other muscles. Squeezing the wrong muscles can put more pressure on your bladder control muscles. Just squeeze the pelvic muscle. Don’t hold your breath.
Be patient. Don’t give up. It’s just 5 minutes, three times a day. You may not feel your bladder control improve until after 3 to 6 weeks. Still, most women do notice an improvement after a few weeks.
Method
Pelvic floor muscle training with or without biofeedback. Mastering a voluntary contraction of the pelvic floor muscles will help to increase pressure within the urethra, inhibit detrusor contractions and control leakage of urine. Coaching and verbal feedback during vaginal examination can be as effective as biofeedback and electrical stimulation
- An initial approach is by verbal explanation of the technique reinforced with written materials
- An effective verbal explanation of proper contraction of the pelvic floor muscles is to tell the patient to tighten up the muscles that they use to hold in flatus.
- These muscles can also be identified during a pelvic or digital rectal examination
- An effective exercise prescription for older adults is to contract and relax their pelvic floor muscles for 2 seconds with 15 repetitions, three times per day. Patients should gradually increase the duration of squeeze/relaxations by about 1 second per week, until they achieve 10 second contractions and relaxations. At this point they can begin a maintenance prescription of 10 second contractions and relaxations with 10 repetitions once a day
- Freeze and squeeze:
- when a sense of urgency occurs, instead of rushing to the bathroom, stay still and repeatedly tighten the pelvic floor muscles without relaxing them until the urgency is gone. Walk to the bathroom at a normal pace
- Repeat as needed.
+ A maintenance program is essential to maintain strength and effectiveness
+ At least 3 months of supervised pelvic floor muscle training is required to see benefits
+ Continence management is often best guided by a continence trained professional (eg. nurse or physiotherapist).
Bladder training
| Goal To modify bladder function, reduce voiding frequency, increase bladder capacity and eliminate detrusor overactivity by using scheduled voiding rather than voiding in response to urgency |
Method
|
| A minimum of 6 weeks training is required to see benefits |
Altering fluid intake – decreasing to reduce incontinence and frequency, increasing to improve urine concentration
Smoking cessation
Dietary modification to eliminate possible bladder irritants (eg. reducing caffeine, alcohol and carbonated beverages). Caffeine is a mild diuretic and bladder irritant, and reducing intake can reduce both urge and stress incontinence
Regulating bowel function to avoid constipation and straining during bowel movements
Healthy weight. If you’re overweight, losing weight may ease symptoms central obesity places pressure on the bladder and may worsen urge incontinence 12. Weight loss may help if you also have stress urinary incontinence.
Scheduled toilet trips. Setting a schedule for toileting — for example, every two to four hours — gets you on track to urinate at the same times every day rather than waiting until you feel the urge to urinate.
Intermittent catheterization. Using a catheter periodically to empty your bladder completely helps your bladder do what it can’t do by itself. Ask your doctor if this approach is right for you.
Absorbent pads. Wearing absorbent pads or undergarments can protect your clothing and help you avoid embarrassing incidents, which means that you won’t have to limit your activities. Absorbent garments come in a variety of sizes and absorbency levels.
Bladder training. Bladder training involves training yourself to delay voiding when you feel an urge to urinate. You begin with small delays, such as 30 minutes, and gradually work your way up to urinating every three to four hours. Bladder training is possible only if you’re able to tighten (contract) your pelvic floor muscles successfully.
Medications
Medications that relax the bladder can be helpful for relieving symptoms of overactive bladder and reducing episodes of urge incontinence. These drugs include:
- Tolterodine (Detrol, Detrol LA)
- Oxybutynin (Ditropan XL)
- Oxybutynin as a skin patch (Oxytrol)
- Oxybutynin gel (Gelnique, Gelnique 3%)
- Trospium (Sanctura)
- Solifenacin (Vesicare)
- Darifenacin (Enablex)
- Mirabegron (Myrbetriq)
- Fesoterodine (Toviaz)
Common side effects of most of these drugs include dry eyes and dry mouth, but drinking water to quench thirst can aggravate symptoms of overactive bladder. Constipation — another potential side effect — can aggravate your bladder symptoms. Extended-release forms of these medications, including the skin patch or gel, may cause fewer side effects.
Side Effects in the elderly
Cognitive dysfunction including memory loss and attention deficits are particular side effects in the elderly 13.
Antimuscarinic medications differ in their propensity to cause central nervous system adverse events due to differences in lipophilicity and crossing of the blood-brain barrier. Oxybutinin may be the most likely to cross the blood-brain barrier 8.
The use of anticholinergics should be carefully weighed against the potential cognitive risks in the older adult population 4, as long term exposure to anticholinergics may be associated with increased Alzheimer type pathology 14.
The newer antimuscarinics for bladder spasms – darifenacin, solifenacin and tolterodine – have a significantly reduced impact on cognitition compared with traditional agents. Similarly, oxybutinin transdermal gel does not seem to adversely affect cognition 15. Despite this, their use in the elderly may still contribute to cognitive impairment and appropriate monitoring is recommended.
Prescribing in the elderly
Oxybutinin can be started at 2.5 mg twice per day. The morning dose can be increased or a lunchtime dose added depending on severity and timing of symptoms. The maximum dose is 5 mg three times per day 16. High doses are often not well tolerated due to dry mouth, gritty eyes, exacerbation of gastrointestinal reflux and constipation.
Nonantimuscarinic medications
Duloxetine (a serotonin noradrenaline reuptake inhibitor) can be effective in both stress and mixed stress and urge incontinence 17. In clinical practice, most women discontinue duloxetine within 4 weeks due to adverse effects (Table 1).
Failure of conservative and medical treatments warrants urology referral for further investigation with urodynamics, and more invasive therapies may be considered.
Your doctor may recommend that you suck on a piece of sugar-free candy or chew sugar-free gum to relieve dry mouth, and use eyedrops to keep your eyes moist. Over-the-counter preparations, such as Biotene products, can be helpful for long-term dry mouth. To avoid constipation, your doctor might recommend a fiber-rich diet or use of stool softeners.
Table 1. Medications proven to be effective for overactive bladder syndrome
| Drug | Adverse effects | Notes |
|---|---|---|
| Oxybutynin CR 5–15 mg/day |
| Dose response observed Take 1 hour before food |
| Oxybutynin transdermal 3.9 mg twice weekly |
| Transdermal delivery reduces the typical anticholinergic side effects of dry mouth and constipation |
| Tolterodine 2 mg twice per day |
| Dose dependent effect with immediate release Safe in men with bladder outlet obstruction Expensive, not subsidised on the PBS3,2 |
| Solifenacin 5–10 mg/day |
| Steady state at 10 days due to long half-life |
| Darifenacin 7.5–15 mg/day |
| Steady state 4–5 hours Dose response Safety, efficacy and tolerability maintained with long term use Not subsidised on the PBS |
| Vaginal oestrogen (topical) 0.5 g cream nightly for 2 weeks then twice per week |
| For postmenopausal women with vaginal atrophy Contraindications: past history of breast cancer |
| Duloxetine 40 mg twice per day increasing to 60 mg twice per day after 4 weeks (for stress urinary incontinence) |
| Efficacy for stress and mixed stress and urge incontinence Can be used if anticholinergics are contraindicated for overactive bladder syndrome33 TGA indicated and PBS subsidised in Australia for major depressive disorder |
Bladder injections (Second line therapy)
OnabotulinumtoxinA, also called Botox, is a protein from the bacteria that cause botulism illness. The technique is to place multiple injections under cystoscopic guidance directly into the detrusor. Used in small doses directly injected into bladder tissues, prevents acetylcholine release at the neuromuscular junction, resulting in temporary chemo-denervation and muscle relaxation (protein partially paralyzes muscles) for up to 6 months 18.
Complete continence can be achieved in 40–80% of patients and bladder capacity improved by 56% for up to 6 months 19. Maximal benefit is between 2 and 6 weeks, maintained over 6 months. The injections can be repeated 20.
About half of people had side effects from these injections, including 9 percent who had urinary retention. So, if you’re considering Botox treatments, you should be willing and able to catheterize yourself if urinary retention occurs.
Nerve stimulation (Third line therapy)
Regulating the nerve impulses to your bladder can improve overactive bladder symptoms.
One procedure uses a thin wire placed close to the sacral nerves — which carry signals to your bladder — where they pass near your tailbone.
This surgical procedure is often done with a trial of a temporary wire or as an advanced procedure in which the permanent electrode is implanted and a longer trial is performed prior to a surgical placement of the battery-powered pulse generator. Your doctor then uses a device connected to the wire to deliver electrical impulses to your bladder, similar to what a pacemaker does for the heart.
If this successfully reduces your symptoms, the wire is eventually connected to a small battery device that’s placed under your skin.
Surgery
Surgery to treat overactive bladder is reserved for people with severe symptoms who don’t respond to other treatments. The goal is to improve the bladder’s ability to store urine and reduce pressure in the bladder. However, these procedures won’t help relieve bladder pain. Interventions include:
- Surgery to increase bladder capacity. This procedure uses pieces of your bowel to replace a portion of your bladder. This surgery is used only in cases of severe urge incontinence that doesn’t respond to any other, more-conservative treatment measures. If you have this surgery, you may need to use a catheter intermittently for the rest of your life to empty your bladder.
- Bladder removal. This procedure is used as a last resort and involves removing the bladder and surgically constructing a replacement bladder (neobladder) or an opening in the body (stoma) to attach a bag on the skin to collect urine.
- Overactive bladder syndrome. Royal Australian College of General Practitioners. https://www.racgp.org.au/afp/2012/november/overactive-bladder-syndrome/[↩]
- Overactive bladder. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/overactive-bladder/symptoms-causes/syc-20355715[↩]
- Ballert K, Biggs G, Nitti V. Antimuscarinic agents. AUA update series 2008;27:137–47.[↩][↩]
- Saks EK, Arya LA. Pharmacologic management of urinary incontinence, voiding dysfunction, and overactive bladder. Obstet Gynecol Clin North Am 2009;36:493–507.[↩][↩]
- Andersson K-E. Antimuscarinics for treatment of overactive bladder. Lancet Neurol 2004;3:46–53.[↩]
- Chapple C, Gormley EA. Developments in pharmacological therapy for the overactive bladder. BJU Int 2006;98(1 Suppl):78–87.[↩]
- Abrams P, Andersson KE. Muscarinic receptor antagonists for overactive bladder. BJU Int 2007;100:987–1006.[↩]
- Chapple CR, Khullar V, Gabriel Z, Muston D, Bitoun CE, Weinstein D. The effects of antimuscarinic treatments in overactive bladder: an update of a systematic review and meta-analysis. Eur Urol 2008;54:543–62.[↩][↩]
- Lukacz ES, Lawrence JM, Contreras R, Nager CW, Luber KM. Parity, mode of delivery, and pelvic floor disorders. Obstet Gynaecol 2006;107:1253–60.[↩]
- Gamble TL, Du H, Sand PK, Botros SM, Rurak M, Goldberg RP. Urge incontinence: estimating environmental and obstetric risk factors using an identical twin study. Int Urogynecol J 2010;21:939–46.[↩]
- Fitzgerald MP, Thom DH, Wassel-Fyr C, et al. Childhood urinary symptoms predict adult overactive bladder symptoms. J Urol 2006;175:989–93.[↩]
- Markland AD, Vaughan CP, Johnson TM 2nd, Burgio KL, Goode PS. Incontinence. Med Clin North Am 2011;95:539–54.[↩][↩]
- Botlero R, Davis SR, Urquhart DM, Bell RJ. Incidence and resolution rates of different types of urinary incontinence in women: findings from a cohort study. J Urol 2011;185:1331–7.[↩]
- Boustani MA, Campbell NL, Munger S, Maidment I, Fox GC. Impact of anticholinergics on the ageing brain: a review and practical application. Aging Health 2008;4:311–20.[↩]
- Wagg A. Treating overactive bladder in the elderly. Can Urol Assoc J 2011;5(5 Suppl 2):S149–51.[↩]
- Kuteesa W, Moore K. Anticholinergic drugs for overactive bladder. Australian Prescriber 2006;29:22–4.[↩]
- Cartwright R, Srikrishna S, Cardozo L. New pharmacological interventions for overactive bladder. Expert Rev Obstet Gynaecol 2008;3:129–36.[↩]
- Anger JT, Weinberg A, Suttorp MJ, Litwin MS, Shekelle PG. Outcomes of intravesical botulinum toxin for idiopathic overactive bladder symptoms: a systematic review of the literature. J Urol 2010;183:2258–64.[↩]
- Smith C, Chancellor M. Botulinum toxin: clinical uses in urology. AUA update series 2008;27(15).[↩]
- Karsenty G, Denys P, Amarenco G, et al. Botulinum toxin A (Botox) intradetrusor injections in adults with neurogenic detrusor overactivity/neurogenic overactive bladder: a systematic literature review. Eur Urol 2008;53:275–87.[↩]