Contents
- What is rectal bleeding or bleeding from rectum ?
- Causes of rectal bleeding
- Understanding Minor Rectal Bleeding
- What are hemorrhoids ?
- What are anal fissures ?
- What is rectal ulcer syndrome ?
- What is proctitis ?
- What are colon polyps ?
- What is colon cancer ?
- Symptoms of colon cancer
- Causes of colon cancer
- Risk factors for colon cancer
- Prevention of colon cancer
- Screening for colon cancer
- Diagnosing colon cancer
- Staging colon cancer
- Treatment for colon cancer
- Surgery for invasive colon cancer
- Surgery for advanced cancer
- Chemotherapy for colon cancer
- Radiation therapy for colon cancer
- Targeted drug therapy for colon cancer
- Supportive (palliative) care for colon cancer
What is rectal bleeding or bleeding from rectum ?
Rectal bleeding can refer to any blood that passes from your anus, although rectal bleeding is usually assumed to refer to bleeding from your lower colon or rectum 1. Your rectum makes up the last few inches of your large intestine.
Rectal bleeding may show up as blood in your stool, on the toilet paper or in the toilet bowl 1. Blood that results from rectal bleeding is usually bright red in color, but occasionally can be dark maroon.
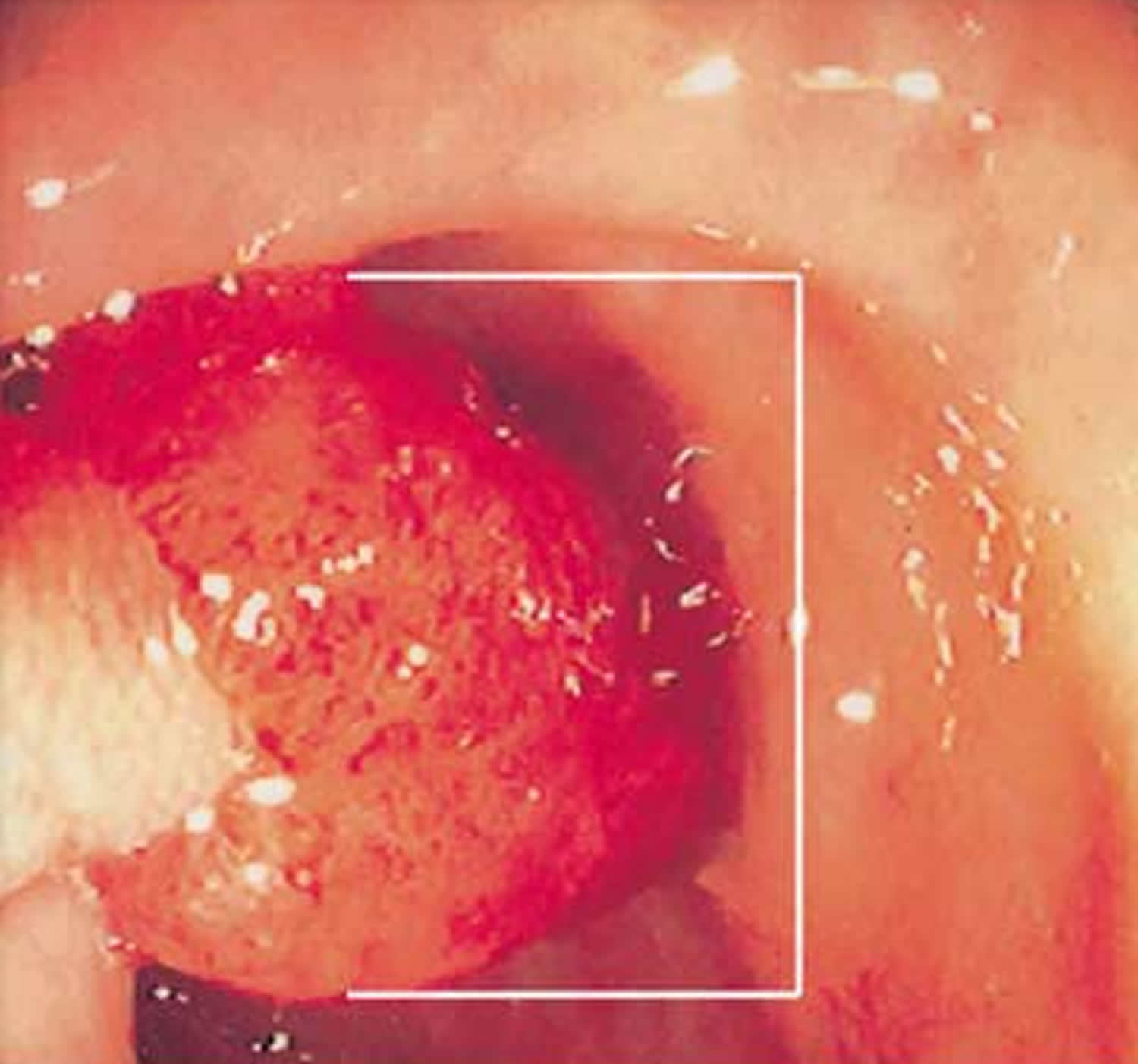
Figure 1. Rectum anatomy and Anus (anal canal)
Causes of rectal bleeding
Rectal bleeding may occur for many reasons. Common causes of rectal bleeding include 2:
- Anal fissure (tear in the skin of the anus)
- Chronic constipation
- Hard stools
- Hemorrhoids
Less common causes of rectal bleeding:
- Anal cancer
- Angiodysplasia (abnormalities in the blood vessels near the intestines)
- Colon cancer
- Colon polyps
- Crohn’s disease
- Diarrhea (causing anal irritation)
- Diverticulosis (a bulging pouch that forms on the wall of the intestine)
- Ischemic colitis (colon inflammation caused by reduced blood flow)
- Proctitis (inflammation of the rectum)
- Pseudomembranous colitis (colon inflammation caused by an infection)
- Radiation therapy
- Rectal cancer
- Solitary rectal ulcer syndrome (a sore on the wall of the rectum)
- Ulcerative colitis
Seek emergency help if you have significant rectal bleeding and any signs of shock:
- Rapid, shallow breathing
- Dizziness or lightheadedness after standing up
- Blurred vision
- Fainting
- Confusion
- Nausea
- Cold, clammy, pale skin
- Low urine output
Seek immediate medical attention:
Have someone drive you to an emergency room if rectal bleeding is:
- Continuous or heavy
- Accompanied by severe abdominal pain or cramping
Schedule a doctor’s visit
Make an appointment to see your doctor if you have rectal bleeding that lasts more than a day or two, or earlier if the bleeding worries you.
Generally, people younger than 40 who whose rectal bleeding is from an obvious cause, such as hemorrhoids, don’t need testing. However, many doctors recommend tests such as a colonoscopy for people older than 40 to rule out any possibility of also having cancer that’s contributing to the bleeding.
Understanding Minor Rectal Bleeding
Minor rectal bleeding refers to the passage of a few drops of bright red (fresh) blood from the rectum, which may appear on the stool, on the toilet paper or in the toilet bowl. This post addresses minor rectal bleeding that occurs from time to time. Continuous passage of significantly greater amounts of blood from the rectum or stools that appear black, tarry or maroon in color can be caused by other diseases that will not be discussed here. Call your doctor immediately if these more serious conditions occur. Because there are several possible causes for minor rectal bleeding, a complete evaluation and early diagnosis by your doctor is very important. Rectal bleeding, whether it is minor or not, can be a symptom of colon cancer, a type of cancer that can be cured if detected early.
Possible causes of minor rectal bleeding:
- Hemorrhoids
- Anal fissures
- Proctitis (inflammation of the rectum)
- Polyps
- Colon or anal cancer
- Rectal ulcers
What are hemorrhoids ?
Hemorrhoids (also called piles) are swollen blood vessels in the anus and rectum that become engorged from increased pressure, similar to what occurs in varicose veins in the legs 3. Hemorrhoids can either be internal (inside the anus) or external (under the skin around the anus).
Hemorrhoids are very common in both men and women and affect about 1 in 20 Americans 4. About half of adults older than age 50 have hemorrhoids 5.
The most common symptom of hemorrhoids inside the anus is bright red blood covering the stool, on toilet paper or in the toilet bowl 4. Symptoms usually go away within a few days 4.
- However, if you have rectal bleeding you should see a doctor. You need to make sure bleeding is not from a more serious condition such as colorectal or anal cancer.
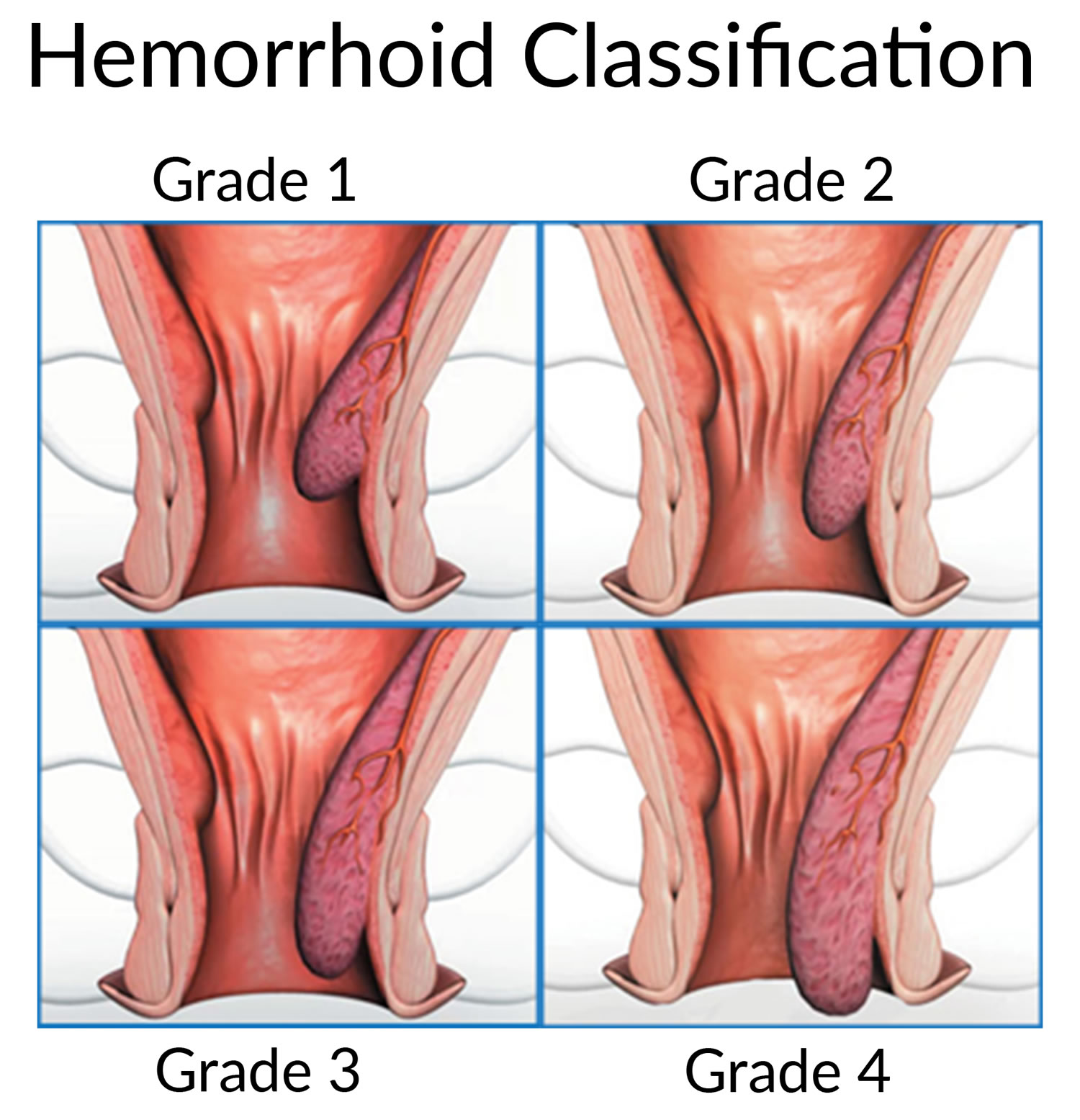
The two types of hemorrhoids are 6:
- External hemorrhoids, which form under the skin around the anus.
- Internal hemorrhoids, which form in the lining of the anus and lower rectum.
The exact cause of bleeding from hemorrhoids is not known, but it often seems to be related to constipation, diarrhea, sitting or standing for long periods, obesity heavy lifting and pregnancy.
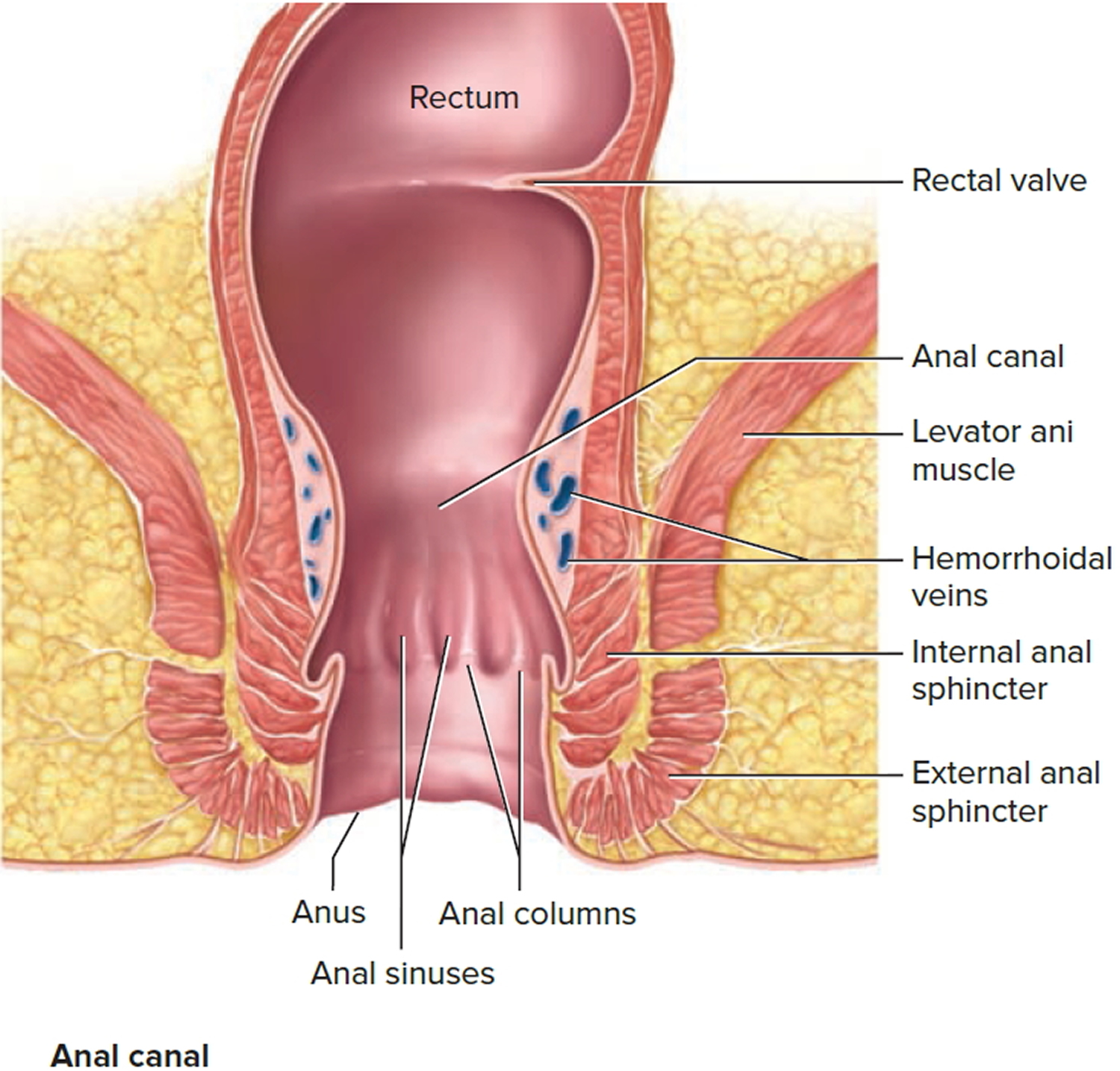
Figure 2. Hemorrhoids
You are more likely to get hemorrhoids if you:
- strain during bowel movements
- sit on the toilet for long periods of time
- have chronic constipation or diarrhea
- eat foods that are low in fiber
- are older than age 50
- are pregnant
- often lift heavy objects
Complications of hemorrhoids can include the following:
- blood clots in an external hemorrhoid
- skin tags—extra skin left behind when a blood clot in an external hemorrhoid dissolves
- infection of a sore on an external hemorrhoid
- strangulated hemorrhoid—when the muscles around your anus cut off the blood supply to an internal hemorrhoid that has fallen through your anal opening
- anemia
How are hemorrhoids treated ?
Medical treatment of hemorrhoids includes treatment of any underlying constipation, taking warm baths and applying an over-the-counter cream or suppository that may contain hydrocortisone. If medical treatment fails there are a number of ways to reduce the size or eliminate internal hemorrhoids. Each method varies in its success rate, risks and recovery time. Your doctor will discuss these options with you. Rubber band ligation is the most common outpatient procedure for hemorrhoids in the United States. It involves placing rubber bands around the base of an internal hemorrhoid to cut off its blood supply. This causes the hemorrhoid to shrink, and in a few days both the hemorrhoid and the rubber band fall off during a bowel movement. Possible complications include pain, bleeding and infection. After band ligation, your doctor may prescribe medications, including pain medication and stool softeners, before sending you home. Contact your doctor immediately if you notice severe pain, fever or significant rectal bleeding. Laser or infrared coagulation and sclerotherapy (injection of medicine directly into the hemorrhoids) are also officebased treatment procedures, although they are less common. Surgery to remove hemorrhoids may be required in severe cases or if symptoms persist despite rubber band ligation, coagulation or sclerotherapy.
What are anal fissures ?
Tears that occur in the lining of the anus are called anal fissures 3. This condition is most commonly caused by constipation and passing hard stools, although it may also result from diarrhea or inflammation in the anus. In addition to causing bleeding from the rectum, anal fissures may also cause a lot of pain during and immediately after bowel movements. Most fissures are treated successfully with simple remedies such as fiber supplements, stool softeners (if constipation is the cause) and warm baths. Your doctor may also prescribe a cream to soothe the inflamed area. Other options for fissures that do not heal with medication include treatment to relax the muscles around the anus (sphincters) or surgery.
Symptoms of anal fissures
Signs and symptoms of an anal fissure include 7:
- Pain, sometimes severe, during bowel movements
- Pain after bowel movements that can last up to several hours
- Bright red blood on the stool or toilet paper after a bowel movement
- Itching or irritation around the anus
- A visible crack in the skin around the anus
- A small lump or skin tag on the skin near the anal fissure
When to see a doctor
- See your doctor if you have pain during bowel movements or notice blood on stools or toilet paper after a bowel movement.
Causes of anal fissures
Common causes of anal fissure include 7:
- Passing large or hard stools
- Constipation and straining during bowel movements
- Chronic diarrhea
- Inflammation of the anorectal area, caused by Crohn’s disease or another inflammatory bowel disease
- Childbirth
Less common causes of anal fissures include:
- Anal cancer
- HIV
- Tuberculosis
- Syphilis
- Herpes
Risk factors for anal fissure
Factors that may increase your risk of developing an anal fissure include:
- Infancy. Many infants experience an anal fissure during their first year of life; experts aren’t sure why.
- Aging. Older adults may develop an anal fissure partly due to slowed circulation, resulting in decreased blood flow to the rectal area.
- Constipation. Straining during bowel movements and passing hard stools increase the risk of tearing.
- Childbirth. Anal fissures are more common in women after they give birth.
- Crohn’s disease. This inflammatory bowel disease causes chronic inflammation of the intestinal tract, which may make the lining of the anal canal more vulnerable to tearing.
- Anal intercourse.
Complications of anal fissures
Complications of anal fissure can include:
- Failure to heal. An anal fissure that fails to heal within six weeks is considered chronic and may need further treatment.
- Recurrence. Once you’ve experienced an anal fissure, you are prone to having another one.
- A tear that extends to surrounding muscles. An anal fissure may extend into the ring of muscle that holds your anus closed (internal anal sphincter), making it more difficult for your anal fissure to heal. An unhealed fissure can trigger a cycle of discomfort that may require medications or surgery to reduce the pain and to repair or remove the fissure.
Prevention of anal fissure
You may be able to prevent an anal fissure by taking measures to prevent constipation. Eat high-fiber foods, drink fluids and exercise regularly to keep from having to strain during bowel movements.
Diagnosis of anal fissure
If possible, your doctor will perform a digital rectal exam, which involves inserting a gloved finger into your anal canal, or use a short, lighted tube (anoscope) to inspect your anal canal. However, if this is too painful for you, your doctor may be able to diagnose an anal fissure only by observation.
An acute anal fissure looks like a fresh tear, somewhat like a paper cut. A chronic anal fissure likely has the tear, as well as two separate lumps or tags of skin, one internal (sentinel pile) and one external (hypertrophied papilla).
The fissure’s location offers clues about its cause. A fissure that occurs on the side of the anal opening, rather than the back or front, is more likely to be a sign of another disorder, such as Crohn’s disease. Your doctor may recommend further testing if he or she thinks you have an underlying condition:
- Flexible sigmoidoscopy. Your doctor will insert a thin, flexible tube with a tiny video into the bottom portion of your colon. This test may be done if you’re younger than 50 and have no risk factors for intestinal diseases or colon cancer.
- Colonoscopy. Your doctor will insert a flexible tube into your rectum to inspect the entire colon. This test may be done if you are older than age 50 or you have risk factors for colon cancer, signs of other conditions, or other symptoms such as abdominal pain or diarrhea.
Treatment of anal fissure
Anal fissures often heal within a few weeks if you take steps to keep your stool soft, such as increasing your intake of fiber and fluids. Soaking in warm water for 10 to 20 minutes several times a day, especially after bowel movements, can help relax the sphincter and promote healing.
If your symptoms persist, you’ll likely need further treatment.
Nonsurgical treatments
Your doctor may recommend:
- Externally applied nitroglycerin (Rectiv), to help increase blood flow to the fissure and promote healing and to help relax the anal sphincter. Nitroglycerin is generally considered the medical treatment of choice when other conservative measures fail. Side effects may include headache, which can be severe.
- Topical anesthetic creams such as lidocaine hydrochloride (Xylocaine) may be helpful for pain relief.
- Botulinum toxin type A (Botox) injection, to paralyze the anal sphincter muscle and relax spasms.
- Blood pressure medications, such as oral nifedipine (Procardia) or diltiazem (Cardizem) can help relax the anal sphincter. These medications may be taken by mouth or applied externally and may be used when nitroglycerin is not effective or causes significant side effects.
Surgery
If you have a chronic anal fissure that is resistant to other treatments, or if your symptoms are severe, your doctor may recommend surgery. Doctors usually perform a procedure called lateral internal sphincterotomy (LIS), which involves cutting a small portion of the anal sphincter muscle to reduce spasm and pain, and promote healing. Studies have found that for chronic fissure, surgery is much more effective than any medical treatment. However, surgery has a small risk of causing incontinence.
Home remedies for anal fissure
Take steps to avoid constipation, such as drinking plenty of water, adding fiber to your diet and exercising regularly. Also, avoid straining during bowel movements. The extra pressure may lengthen the fissure or create a new one.
Several lifestyle changes may help relieve discomfort and promote healing of an anal fissure, as well as prevent recurrences:
- Add fiber to your diet. Eating about 25 to 30 grams of fiber a day can help keep stools soft and improve fissure healing. Fiber-rich foods include fruits, vegetables, nuts and whole grains. You also can take a fiber supplement. Adding fiber may cause gas and bloating, so increase your intake gradually.
- Drink adequate fluids. Fluids help prevent constipation.
- Exercise regularly. Engage in 30 minutes or more of moderate physical activity, such as walking, most days of the week. Exercise promotes regular bowel movements and increases blood flow to all parts of your body, which may promote healing of an anal fissure.
- Avoid straining during bowel movements. Straining creates pressure, which can open a healing tear or cause a new tear.
If your infant has an anal fissure, be sure to change diapers frequently, wash the area gently and discuss the problem with your child’s doctor.
What is rectal ulcer syndrome ?
Solitary rectal ulcer syndrome is a condition that occurs when one or more open sores (ulcers) develop in the rectum 8.
Solitary rectal ulcer syndrome is a rare and poorly understood disorder that often occurs in people with chronic constipation 8. Solitary rectal ulcer syndrome can cause rectal bleeding and straining during bowel movements. Despite its name, sometimes more than one rectal ulcer occurs in solitary rectal ulcer syndrome 8.
Treatments for solitary rectal ulcer syndrome range from changing your diet along with fluid intake to surgery.
Symptoms of solitary rectal ulcer syndrome
Signs and symptoms of solitary rectal ulcer syndrome include:
- Constipation
- Rectal bleeding
- Straining during bowel movements
- Pain or a feeling of fullness in your pelvis
- A feeling of incomplete passing of stool
- Passing mucus from your rectum
- Fecal incontinence
- Rectal pain
However, some people with solitary rectal ulcer syndrome may experience no symptoms.
When to see a doctor
Make an appointment with your doctor if you notice any signs or symptoms that worry you.
Other diseases and conditions may cause signs and symptoms similar to those of solitary rectal ulcer syndrome. At your appointment, your doctor may recommend tests and procedures to rule out other causes of your signs and symptoms.
Causes of solitary rectal ulcer syndrome
It’s not always clear what causes solitary rectal ulcer syndrome. Doctors believe stress or injury to the rectum may cause rectal ulcers to form.
Examples of situations that could injure the rectum include:
- Constipation or impacted stool
- Straining during bowel movements
- Rectal prolapse, which occurs when the rectum protrudes from the anus
- Uncoordinated tightening of the pelvic floor muscles that slows blood flow to the rectum
- Attempts to manually remove impacted stool
- Intussusception, which occurs when part of the intestine slides inside another part
Diagnosis of solitary rectal ulcer syndrome
Tests and procedures used to diagnose solitary rectal ulcers include:
- Sigmoidoscopy. During this test, your doctor inserts a flexible tube equipped with a lens into your rectum to examine your rectum and part of your colon. If a lesion is found, your doctor may take a tissue sample (biopsy) for laboratory testing.
- Ultrasound. This imaging technique uses sound waves to create pictures. Your doctor may recommend an ultrasound to help differentiate solitary rectal ulcer syndrome from other conditions.
- Imaging studies. Your doctor may recommend an imaging procedure, such as defecation proctography. This test allows the doctor to look at your rectum.
During this procedure, your doctor inserts a soft paste made of barium into your rectum. You then pass the barium paste as you would stool. The barium shows up on X-rays and may reveal a prolapse or problems with muscle function and muscle coordination.
Specialized centers may offer magnetic resonance defecography. This test is done on a magnetic resonance imaging (MRI) machine and provides a 3-dimensional image of the rectum.
Treatment for solitary rectal ulcer syndrome
Treatment for solitary rectal ulcer syndrome depends on the severity of your condition. People with mild signs and symptoms may find relief through lifestyle changes, while people with more-severe signs and symptoms may require treatment.
Lifestyle changes. Dietary changes, including increasing fiber in your diet
Behavior therapy to stop straining during bowel movements
Some people strain during bowel movements out of habit. Behavior therapy can help you learn to relax your pelvic muscles during bowel movements.
In one technique called biofeedback, a specialist teaches you to control certain involuntary body responses, such as tightening of your anus or pelvic floor muscles during defecation. Biofeedback may make you more aware of your straining and help you to control it.
Medications
Certain treatments such as topical steroids, sulfasalazine enemas and botulinum toxin (Botox) may help ease your rectal ulcer symptoms. However, these treatments don’t work for everyone, and some are still considered experimental.
Surgery
Surgical procedures used to treat solitary rectal ulcer syndrome include:
- Rectal prolapse surgery. If you have a rectal prolapse that’s causing symptoms, your doctor may recommend a rectopexy procedure. Rectopexy secures the rectum in its anatomically correct position.
- Surgery to remove the rectum. An operation to remove the rectum may be an option for people with severe signs and symptoms who haven’t been helped by other treatments. The surgeon may connect the colon to an opening in the abdomen for waste to leave the body (colostomy). If you have a colostomy, a pouch or bag is then attached to your abdomen to collect waste.
Home remedies for solitary rectal ulcer syndrome
You can make changes to your daily life that may help relieve your symptoms, including:
- Increase the amount of fiber in your diet. Fiber adds bulk to your stool. The bulk helps push the contents of your intestines along so that they can be eliminated when you have a bowel movement. Try to eat at least 20 to 35 grams of fiber each day. Nutrition labels on food packaging list the amount of fiber in a serving.
The best sources of fiber are fruits, vegetables and whole grains. Eat fruits and vegetables with the skin on, and choose whole fruits and vegetables over juices. Look for breads and cereals that list whole wheat, oats or bran as the first ingredients.
- Try bulk laxatives and stool softeners. Bulk laxatives, such as Metamucil and FiberCon, absorb fluid in the intestines and make stools bulkier, which helps trigger the bowel to contract and push stool out. However, they should be taken with water, or they can cause obstruction. Stool softeners help mix fluid into stools, making them easier to pass.
- Drink water throughout the day. Drinking enough water and other fluids helps to keep your bowel movements soft and easy to pass. For variety, you may want to add lemon juice to water for flavor. Or try other noncarbonated and caffeine-free beverages. Prune juice can be helpful because it has a natural laxative effect.
What is proctitis ?
Proctitis refers to inflammation of the lining of the rectum 9. It may cause the sensation that you didn’t completely empty your bowels after a bowel movement, and may give you the frequent urge to have a bowel movement. Other symptoms include passing mucus through the rectum, rectal bleeding and pain in the area of the anus and rectum. Treatment for proctitis depends on the cause. Your doctor will discuss the appropriate course of action with you.
It can be caused by previous radiation therapy for various cancers, medications, infections or a limited form of inflammatory bowel disease (IBD) 3.
Proctitis signs and symptoms
Proctitis signs and symptoms may include:
- A frequent or continuous feeling that you need to have a bowel movement
- Rectal bleeding
- The passing of mucus through your rectum
- Rectal pain
- Pain on the left side of your abdomen
- A feeling of fullness in your rectum
- Diarrhea
- Pain with bowel movements
When to see a doctor
Make an appointment with your doctor if you have any signs or symptoms of proctitis.
Causes of proctitis
Several diseases and conditions can cause the lining of the rectum to become inflamed (proctitis). They include:
- Inflammatory bowel disease. About 30 percent of people with inflammatory bowel disease (Crohn’s disease or ulcerative colitis) have inflammation of the rectum.
- Infections. Sexually transmitted infections, spread particularly by people who engage in anal intercourse, can result in proctitis. Sexually transmitted infections that can cause proctitis include gonorrhea, genital herpes and chlamydia. Infectious proctitis is also associated with HIV. Infections associated with foodborne illness, such as salmonella, shigella and campylobacter infections, also can cause proctitis.
- Radiation therapy for cancer. Radiation therapy directed at your rectum or nearby areas, such as the prostate, can cause inflammation of the lining of your rectum. Radiation proctitis can begin during radiation treatment and last for a few months after treatment. Or it can occur years after treatment.
- Antibiotics. Sometimes antibiotics used to treat an infection can kill helpful bacteria in the bowels, allowing the harmful Clostridium difficile bacteria to grow in the rectum.
- Diversion proctitis. Proctitis can occur in people following some types of colon surgery in which the passage of stool is diverted from the rectum.
- Food protein-induced proctitis. This can occur in infants who drink either cow’s milk- or soy-based formula, and in those who are breastfed by mothers who eat dairy products.
- Eosinophilic proctitis. A form of proctitis caused by accumulation of a kind of white blood cell (eosinophil) in the lining of the rectum that affects only children younger than 2.
Prevention of proctitis
To reduce your risk of proctitis, take steps to protect yourself from sexually transmitted infections (STIs). The surest way to prevent an sexually transmitted infection is to abstain from sex, especially anal sex. If you choose to have sex, reduce your risk of an sexually transmitted infection by:
- Limiting your number of sex partners
- Using a latex condom during each sexual contact
- Not having sex with anyone who has any unusual sores or discharge in the genital area
If you’re diagnosed with a sexually transmitted infection, stop having sex until after you’ve completed treatment. That way you can avoid passing the infection to your partner. Ask your doctor when it’s safe to have sex again.
Risk factors for proctitis
Risk factors for proctitis include:
- Unsafe sex. Practices that increase your risk of a sexually transmitted infection (STI) can increase your risk of proctitis. Your risk of contracting an STI increases if you have multiple sex partners, don’t use condoms and have sex with a partner who has an STI.
- Inflammatory bowel diseases. Having an inflammatory bowel disease (ulcerative colitis or Crohn’s disease) increases your risk of proctitis.
- Radiation therapy for cancer. Radiation therapy directed at or near your rectum (such as for rectal, ovarian or prostate cancer) increases your risk of proctitis.
Complications of proctitis
Proctitis that isn’t treated or that doesn’t respond to treatment may lead to complications, including:
- Anemia. Chronic bleeding from your rectum can cause anemia. With anemia, you don’t have enough red blood cells to carry adequate oxygen to your tissues. Anemia causes you to feel tired, and you may also experience dizziness, shortness of breath, headache, pale skin and irritability.
- Ulcers. Chronic inflammation in the rectum can lead to open sores (ulcers) on the inside lining of the rectum.
- Fistulas. Sometimes ulcers extend completely through the intestinal wall, creating a fistula, an abnormal connection that can occur between different parts of your intestine, between your intestine and skin, or between your intestine and other organs, such as the bladder and vagina.
How is proctitis diagnosed ?
Tests and procedures used to diagnose proctitis include:
- Blood tests. These can detect blood loss or infections.
- Stool test. You may be asked to collect a stool sample for testing. A stool test may help determine if your proctitis is caused by a bacterial infection.
- Scope exam of the final portion of your colon. During a flexible sigmoidoscopy, your doctor uses a slender, flexible, lighted tube to examine the sigmoid, the last part of your colon — including the rectum. During the procedure, your doctor can also take small samples of tissue (biopsy) for laboratory analysis.
- Scope exam of your entire colon. A colonoscopy allows your doctor to view your entire colon using a thin, flexible, lighted tube with an attached camera. Your doctor can also take a biopsy during this test.
- Testing for sexually transmitted infections. This involves obtaining a sample of discharge from your rectum or from the tube that drains urine from your bladder (urethra).
If the cause of your proctitis is likely to be an sexually transmitted infection, your doctor may insert a narrow swab into the end of your urethra or anus to obtain the sample, which is then tested for the presence of bacteria or other infectious organisms. The results can be used to select the most effective treatment.
Treatment for proctitis
Treatment for proctitis depends on the underlying cause of the inflammation.
Treatment for proctitis caused by an infection
Your doctor may recommend medications to treat your infection. Options may include:
- Antibiotics. For proctitis caused by bacterial infections, your doctor may recommend an antibiotic, such as doxycycline (Periostat, Vibramycin).
- Antivirals. For proctitis caused by viral infections, such as the sexually transmitted virus herpes, your doctor may prescribe an antiviral medication, such as acyclovir (Sitavig, Zovirax, others).
Treatment for proctitis caused by radiation therapy
Mild cases of radiation proctitis may not require treatment. In other cases, radiation proctitis can cause severe pain and bleeding that requires treatment. Your doctor may recommend treatments such as:
- Medications. Medications are given in pill, suppository or enema form. They include sucralfate (Carafate), mesalamine (Asacol, Canasa, others) and sulfasalazine (Azulfidine), and metronidazole (Flagyl). These medications can help control inflammation and reduce bleeding.
- Stool softeners and dilation. These can help open up obstructions in the bowel.
- Treatment to destroy damaged tissue. These techniques improve proctitis symptoms by destroying abnormal tissue (ablation) that is bleeding. Ablation procedures used to treat proctitis include argon plasma coagulation (APC), electrocoagulation and other therapies.
Proctitis caused by inflammatory bowel disease
Treatment of proctitis related to Crohn’s disease or ulcerative colitis is aimed at reducing the inflammation in your rectum. Treatment may include:
- Medications to control rectal inflammation. Your doctor may prescribe anti-inflammatory medications, either by mouth or as a suppository or enema — such as mesalamine (Asacol, Canasa, others) — or corticosteroids — such as prednisone (Rayos) or budesonide (Entocort EC, Uceris). Inflammation in people with Crohn’s disease often requires treatment with a medication that suppresses the immune system, such as azathioprine (Azasan, Imuran) or infliximab (Remicade).
- Surgery. If drug therapy doesn’t relieve your signs and symptoms, your doctor may recommend surgery to remove a damaged portion of your digestive tract.
Home remedies for proctitis
For temporary relief of mild pain and inflammation, try the following self-care measures:
- Ask your doctor before using over-the-counter (OTC) diarrhea medicines. Don’t take OTC anti-diarrhea drugs, such as loperamide (Imodium A-D), without your doctor’s OK.
- Avoid food just before bedtime. Eating just before going to bed may stimulate your digestive system and cause you to have bowel movements and discomfort at night.
- Take over-the-counter pain relievers. Acetaminophen (Tylenol, others) may be helpful, but ask your doctor before taking aspirin or ibuprofen (Advil, Motrin IB, others), as in some cases these may make your proctitis worse.
- Use a sitz bath with warm water. A sitz bath is a warm water bath used for healing or cleansing purposes 10. You sit in the bath. The water covers only your hips and buttocks. The water may contain medicine.Sitz baths are often used to relieve pain, itching, or muscle spasms. The baths are often recommended to relieve pain and speed healing after hemorrhoid surgery or an episiotomy (surgical cut to widen the vagina opening during childbirth). You can get one at a medical supply store or some pharmacies. This may provide some comfort if you experience anal inflammation.
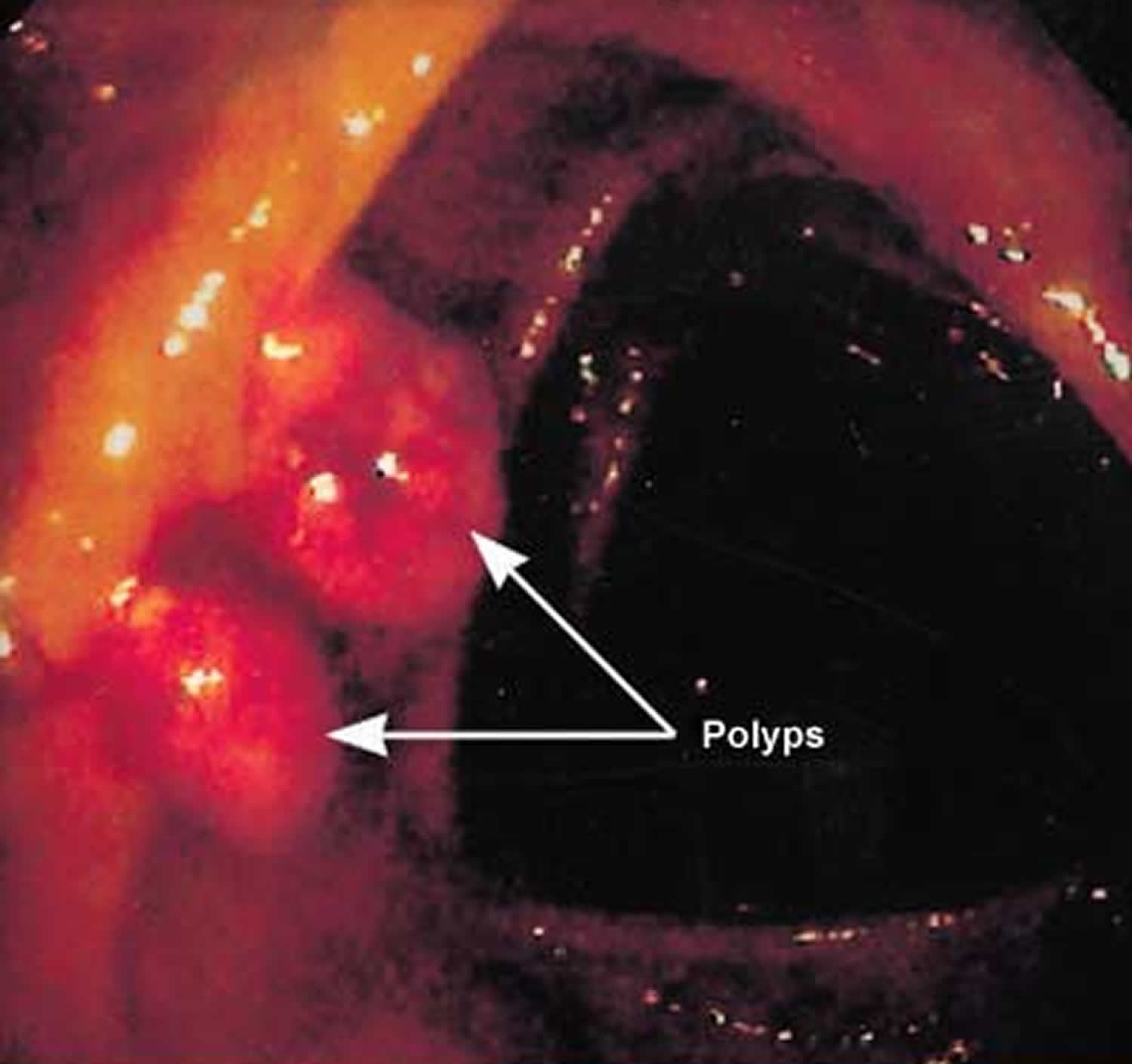
What are colon polyps ?
Polyps are benign growths (a small clump of cells) within the lining of the large bowel. Most colon polyps are harmless and do not cause symptoms, however, some polyps located in the lower colon and rectum may cause minor bleeding. It is important to remove these polyps because some of them may later turn into colon cancer if left alone, which is often fatal when found in its later stages 11.
There are two main categories of polyps, non-neoplastic and neoplastic:
- Non-neoplastic polyps include hyperplastic polyps, inflammatory polyps and hamartomatous polyps. These types of polyps typically do not become cancerous.
- Neoplastic polyps include adenomas and serrated types. In general, the larger a polyp, the greater the risk of cancer, especially with neoplastic polyps.
Anyone can develop colon polyps. You’re at higher risk if you’re 50 or older, are overweight or a smoker, or have a personal or family history of colon polyps or colon cancer 11.
Colon polyps often don’t cause symptoms. It’s important to have regular screening tests, such as a colonoscopy, because colon polyps found in the early stages can usually be removed safely and completely. The best prevention for colon cancer is regular screening for polyps 11.
You should be screened regularly for polyps if 11:
- You’re age 50 or older.
- You have risk factors, such as a family history of colon cancer. Some high-risk individuals should begin regular screening much earlier than age 50.
Figure 3. Colon polyps
Symptoms of colon polyps
Colon polyps often cause no symptoms. You might not know you have a polyp until your doctor finds it during an examination of your bowel.
But some people with colon polyps experience:
- Rectal bleeding. This can be a sign of colon polyps or cancer or other conditions, such as hemorrhoids or minor tears in your anus.
- Change in stool color. Blood can show up as red streaks in your stool or make stool appear black. A change in color may also be caused by foods, medications and supplements.
- Change in bowel habits. Constipation or diarrhea that lasts longer than a week may indicate the presence of a large colon polyp. But a number of other conditions can also cause changes in bowel habits.
- Pain. A large colon polyp can partially obstruct your bowel, leading to crampy abdominal pain.
- Iron deficiency anemia. Bleeding from polyps can occur slowly over time, without visible blood in your stool. Chronic bleeding robs your body of the iron needed to produce the substance that allows red blood cells to carry oxygen to your body (hemoglobin). The result is iron deficiency anemia, which can make you feel tired and short of breath.
When to see a doctor
See your doctor if you experience:
- Abdominal pain
- Blood in your stool
- A change in your bowel habits that lasts longer than a week.
Causes of colon polyps
Healthy cells grow and divide in an orderly way. Mutations in certain genes can cause cells to continue dividing even when new cells aren’t needed. In the colon and rectum, this unregulated growth can cause polyps to form. Polyps can develop anywhere in your large intestine.
There are two main categories of polyps, non-neoplastic and neoplastic.
Non-neoplastic polyps include hyperplastic polyps, inflammatory polyps and hamartomatous polyps. Non-neoplastic polyps typically do not become cancerous.
Inflammatory polyps may be seen with ulcerative colitis or Crohn’s disease of the colon. Although the polyps themselves are not a significant threat, having ulcerative colitis or Crohn’s disease of the colon increases your overall risk of colon cancer.
Neoplastic polyps include adenomas and serrated types. Most colon polyps are adenomas. Serrated polyps may become cancerous, depending on their size and location in the colon. In general, the larger a polyp, the greater the risk of cancer, especially with neoplastic polyps.
Risk factors for colon polyps
Factors that may contribute to the formation of colon polyps or cancer include:
- Age. Most people with colon polyps are 50 or older.
- Inflammatory intestinal conditions, such as ulcerative colitis and Crohn’s disease.
- Family history. You’re more likely to develop colon polyps or cancer if you have a parent, sibling or child with them. If many family members have them, your risk is even greater. In some people, this connection isn’t hereditary.
- Tobacco and alcohol use.
- Obesity and lack of exercise.
- Race. African-Americans are at higher risk of developing colon cancer.
- Type 2 diabetes that isn’t well-controlled.
Hereditary polyp disorders
Rarely, people inherit genetic mutations that cause colon polyps to form. If you have one of these genetic mutations, you are at much higher risk of developing colorectal cancer. Screening and early detection can help prevent the development or spread of these cancers.
Hereditary disorders that cause colon polyps include:
- Lynch syndrome, also called hereditary nonpolyposis colorectal cancer. People with Lynch syndrome tend to develop relatively few colon polyps, but those polyps can quickly become malignant. Lynch syndrome is the most common form of inherited colon cancer and is also associated with tumors in the breast, stomach, small intestine, urinary tract and ovaries.
- Familial adenomatous polyposis (FAP), a rare disorder that causes hundreds or even thousands of polyps to develop in the lining of your colon beginning during your teenage years. If the polyps aren’t treated, your risk of developing colon cancer is nearly 100 percent, usually before age 40. Genetic testing can help determine your risk of familial adenomatous polyposis.
- Gardner’s syndrome, a variant of familial adenomatous polyposis that causes polyps to develop throughout your colon and small intestine. You may also develop noncancerous tumors in other parts of your body, including your skin, bones and abdomen.
- MYH-associated polyposis (MAP), a condition similar to familial adenomatous polyposis that is caused by mutations in the MYH gene. People with MAP often develop multiple adenomatous polyps and colon cancer at a young age. Genetic testing can help determine your risk of MAP.
- Peutz-Jeghers syndrome, a condition that usually begins with freckles developing all over the body, including the lips, gums and feet. Then noncancerous polyps develop throughout the intestines. These polyps may become malignant, so people with this condition have an increased risk of colon cancer.
- Serrated polyposis syndrome, a condition that leads to multiple serrated adenomatous polyps in the upper part of the colon. These polyps may become malignant.
Complications of colon polyps
Some colon polyps may become cancerous. The earlier polyps are removed, the less likely it is that they will become malignant.
Prevention of colon polyps
You can greatly reduce your risk of colon polyps and colorectal cancer by having regular screenings. Certain lifestyle changes also can help:
- Adopt healthy habits. Include plenty of fruits, vegetables and whole grains in your diet and reduce your fat intake. Limit alcohol consumption and quit tobacco. Stay physically active and maintain a healthy body weight.
- Talk to your doctor about calcium and vitamin D. Studies have shown that increasing your consumption of calcium may help prevent recurrence of colon adenomas. But it isn’t clear whether calcium has any protective benefits against colon cancer. Other studies have shown that vitamin D may have a protective effect against colorectal cancer.
- Consider your options if you’re at high risk. If you have a family history of colon polyps, consider having genetic counseling. If you’ve been diagnosed with a hereditary disorder that causes colon polyps, you’ll need regular colonoscopies starting in young adulthood.
Diagnosis of colon polyps
Screening tests play a key role in detecting polyps before they become cancerous. These tests can also help find colorectal cancer in its early stages, when you have a good chance of recovery.
Screening methods include:
- Colonoscopy, the most sensitive test for colorectal polyps and cancer. If polyps are found, your doctor may remove them immediately or take tissue samples (biopsies) for analysis.
- Virtual colonoscopy (CT colonography), a minimally invasive test that uses a CT scan to view your colon. Virtual colonoscopy requires the same bowel preparation as a colonoscopy. If a polyp is found, you’ll need a colonoscopy to have it removed.
- Flexible sigmoidoscopy, in which a slender, lighted tube is inserted in your rectum to examine it and the last third of your colon (sigmoid) and rectum. If a polyp is found, you’ll need a colonoscopy to have it removed.
- Stool-based tests. This type of test works by checking for the presence of blood in the stool or assessing your stool DNA. If your stool test is positive you will need a colonoscopy.
Treatment of colon polyps
Your doctor is likely to remove all polyps discovered during a bowel examination. The options for removal include:
- Removal with forceps or a wire loop (polypectomy). If a polyp is larger than 0.4 inches (about 1 centimeter), a liquid may be injected under it to lift and isolate the polyp from surrounding tissue so that it can be removed.
- Minimally invasive surgery. Polyps that are too large or that can’t be removed safely during screening are usually removed laparoscopically, which is performed by inserting an instrument called a laparoscope into the bowel.
- Colon and rectum removal. If you have a rare inherited syndrome, such as familial adenomatous polyposis (FAP), you may need surgery to remove your colon and rectum (total proctocolectomy).
Some types of colon polyp are far likelier to become malignant than are others. But a doctor who specializes in analyzing tissue samples (pathologist) usually must examine polyp tissue under a microscope to determine whether it’s potentially cancerous.
Follow-up care for colon polyps
If you have had an adenomatous polyp or a serrated polyp, you are at increased risk of colon cancer. The level of risk depends on the size, number and characteristics of the adenomatous polyps that were removed.
You’ll need follow-up screenings for polyps. Your doctor is likely to recommend a colonoscopy:
- In five to 10 years if you had only one or two small adenomas
- In three years if you had more than two adenomas, adenomas measuring 0.4 inches (about 1 centimeter) or larger, or certain adenomas
- Within three years if you had more than 10 adenomas
- Within six months if you had a very large adenoma or an adenoma that had to be removed in pieces
It’s important to fully prepare your colon before a colonoscopy. If stool remains in the colon and obstructs your doctor’s view of the colon wall, you will likely need a follow-up colonoscopy sooner than the guidelines specify.
What is colon cancer ?
Colon cancer is cancer of the large intestine (colon), the lower part of your digestive system 12. Rectal cancer is cancer of the last several inches of the colon. Together, they’re often referred to as colorectal cancers.
Most cases of colon cancer begin as small, noncancerous (benign) clumps of cells called adenomatous polyps. Over time some of these polyps become colon cancers.
Polyps may be small and produce few, if any, symptoms. For this reason, doctors recommend regular screening tests to help prevent colon cancer by identifying and removing polyps before they become colon cancer.
Symptoms of colon cancer
Signs and symptoms of colon cancer include:
- A change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool, that lasts longer than four weeks
- Rectal bleeding or blood in your stool
- Persistent abdominal discomfort, such as cramps, gas or pain
- A feeling that your bowel doesn’t empty completely
- Weakness or fatigue
- Unexplained weight loss
Many people with colon cancer experience no symptoms in the early stages of the disease. When symptoms appear, they’ll likely vary, depending on the cancer’s size and location in your large intestine.
When to see a doctor
If you notice any symptoms of colon cancer, such as blood in your stool or a persistent change in bowel habits, make an appointment with your doctor.
Talk to your doctor about when you should begin screening for colon cancer. Guidelines generally recommend that colon cancer screenings begin at age 50. Your doctor may recommend more frequent or earlier screening if you have other risk factors, such as a family history of the disease.
Causes of colon cancer
In most cases, it’s not clear what causes colon cancer. Doctors know that colon cancer occurs when healthy cells in the colon develop errors in their DNA.
Healthy cells grow and divide in an orderly way to keep your body functioning normally. But when a cell’s DNA is damaged and becomes cancerous, cells continue to divide — even when new cells aren’t needed. As the cells accumulate, they form a tumor.
With time, the cancer cells can grow to invade and destroy normal tissue nearby. And cancerous cells can travel to other parts of the body.
Inherited gene mutations that increase the risk of colon cancer
Inherited gene mutations that increase the risk of colon cancer can be passed through families, but these inherited genes are linked to only a small percentage of colon cancers. Inherited gene mutations don’t make cancer inevitable, but they can increase an individual’s risk of cancer significantly.
The most common forms of inherited colon cancer syndromes are:
- Hereditary nonpolyposis colorectal cancer (HNPCC). HNPCC, also called Lynch syndrome, increases the risk of colon cancer and other cancers. People with HNPCC tend to develop colon cancer before age 50.
- Familial adenomatous polyposis (FAP). FAP is a rare disorder that causes you to develop thousands of polyps in the lining of your colon and rectum. People with untreated FAP have a greatly increased risk of developing colon cancer before age 40.
FAP, HNPCC and other, rarer inherited colon cancer syndromes can be detected through genetic testing. If you’re concerned about your family’s history of colon cancer, talk to your doctor about whether your family history suggests you have a risk of these conditions.
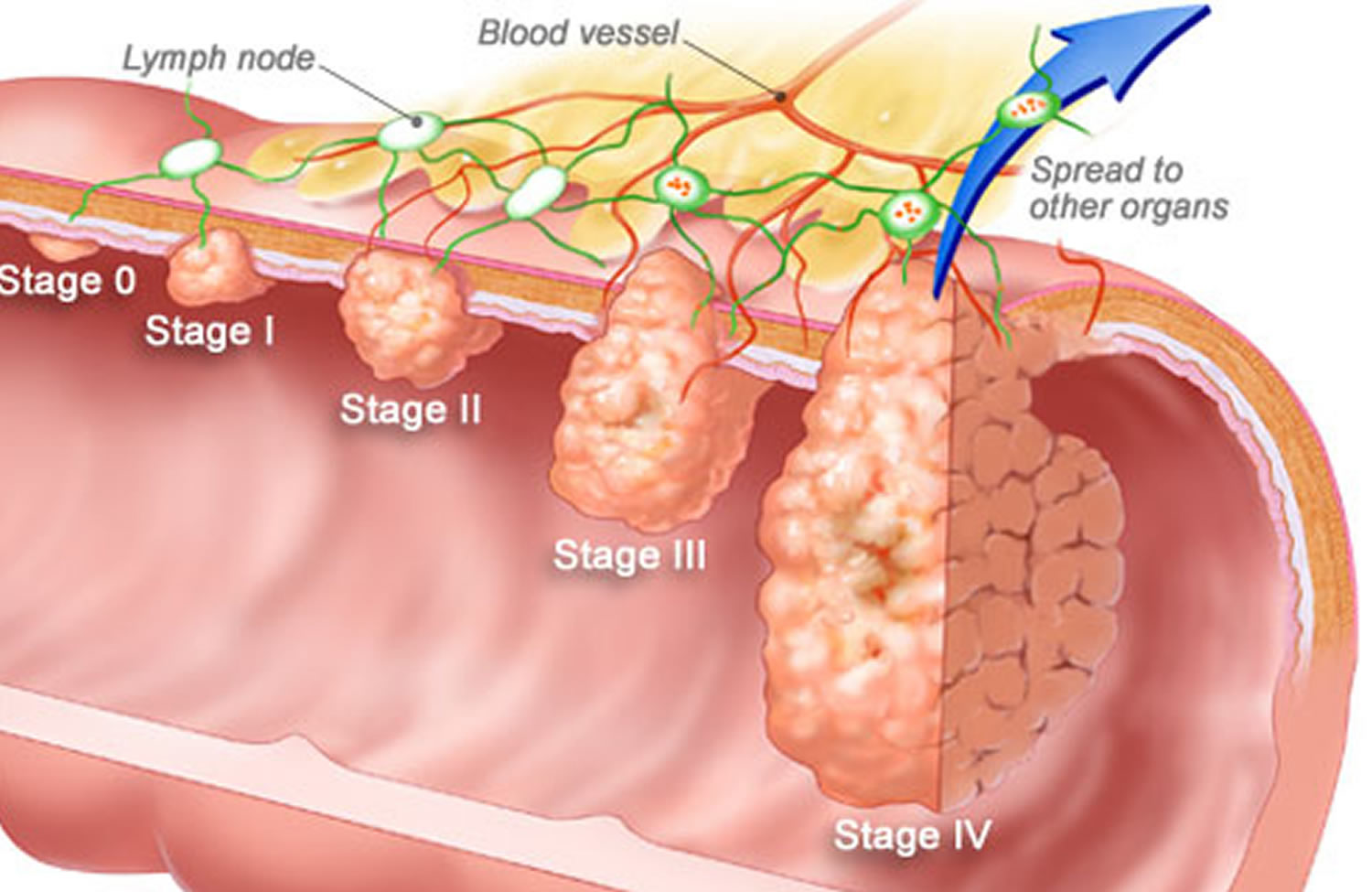
Figure 4. Colon cancer
Association between diet and increased colon cancer risk
Studies of large groups of people have shown an association between a typical Western diet and an increased risk of colon cancer. A typical Western diet is high in fat and low in fiber.
When people move from areas where the typical diet is low in fat and high in fiber to areas where the typical Western diet is most common, the risk of colon cancer in these people increases significantly. It’s not clear why this occurs, but researchers are studying whether a high-fat, low-fiber diet affects the microbes that live in the colon or causes underlying inflammation that may contribute to cancer risk. This is an area of active investigation and research is ongoing.
Risk factors for colon cancer
Factors that may increase your risk of colon cancer include:
- Older age. The great majority of people diagnosed with colon cancer are older than 50. Colon cancer can occur in younger people, but it occurs much less frequently.
- African-American race. African-Americans have a greater risk of colon cancer than do people of other races.
- A personal history of colorectal cancer or polyps. If you’ve already had colon cancer or adenomatous polyps, you have a greater risk of colon cancer in the future.
- Inflammatory intestinal conditions. Chronic inflammatory diseases of the colon, such as ulcerative colitis and Crohn’s disease, can increase your risk of colon cancer.
- Inherited syndromes that increase colon cancer risk. Genetic syndromes passed through generations of your family can increase your risk of colon cancer. These syndromes include familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer, which is also known as Lynch syndrome.
- Family history of colon cancer. You’re more likely to develop colon cancer if you have a parent, sibling or child with the disease. If more than one family member has colon cancer or rectal cancer, your risk is even greater.
- Low-fiber, high-fat diet. Colon cancer and rectal cancer may be associated with a diet low in fiber and high in fat and calories. Research in this area has had mixed results. Some studies have found an increased risk of colon cancer in people who eat diets high in red meat and processed meat.
- A sedentary lifestyle. If you’re inactive, you’re more likely to develop colon cancer. Getting regular physical activity may reduce your risk of colon cancer.
- Diabetes. People with diabetes and insulin resistance may have an increased risk of colon cancer.
- Obesity. People who are obese have an increased risk of colon cancer and an increased risk of dying of colon cancer when compared with people considered normal weight.
- Smoking. People who smoke may have an increased risk of colon cancer.
- Alcohol. Heavy use of alcohol may increase your risk of colon cancer.
- Radiation therapy for cancer. Radiation therapy directed at the abdomen to treat previous cancers may increase the risk of colon cancer.
Prevention of colon cancer
Get screened for colon cancer
People with an average risk of colon cancer can consider screening beginning at age 50. But people with an increased risk, such as those with a family history of colon cancer, should consider screening sooner.
Several screening options exist — each with its own benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you.
Make lifestyle changes to reduce your risk for colon cancer
You can take steps to reduce your risk of colon cancer by making changes in your everyday life. Take steps to:
- Eat a variety of fruits, vegetables and whole grains. Fruits, vegetables and whole grains contain vitamins, minerals, fiber and antioxidants, which may play a role in cancer prevention. Choose a variety of fruits and vegetables so that you get an array of vitamins and nutrients.
- Drink alcohol in moderation, if at all. If you choose to drink alcohol, limit the amount of alcohol you drink to no more than one drink a day for women and two for men.
- Stop smoking. Talk to your doctor about ways to quit that may work for you.
- Exercise most days of the week. Try to get at least 30 minutes of exercise on most days. If you’ve been inactive, start slowly and build up gradually to 30 minutes. Also, talk to your doctor before starting any exercise program.
- Maintain a healthy weight. If you are at a healthy weight, work to maintain your weight by combining a healthy diet with daily exercise. If you need to lose weight, ask your doctor about healthy ways to achieve your goal. Aim to lose weight slowly by increasing the amount of exercise you get and reducing the number of calories you eat.
Colon cancer prevention for people with a high risk
Some medications have been found to reduce the risk of precancerous polyps or colon cancer. However, not enough evidence exists to recommend these medications to people who have an average risk of colon cancer. These options are generally reserved for people with a high risk of colon cancer.
For instance, some evidence links a reduced risk of polyps and colon cancer to regular use of aspirin. But it’s not clear what dose and what length of time would be needed to reduce the risk of colon cancer. Taking aspirin daily has some risks, including gastrointestinal bleeding and ulcers, so doctors typically don’t recommend this as a prevention strategy unless you have an increased risk of colon cancer.
Screening for colon cancer
Doctors recommend certain screening tests for healthy people with no signs or symptoms in order to look for early signs of colon cancer. Finding colon cancer at its earliest stage provides the greatest chance for a cure. Screening has been shown to reduce your risk of dying of colon cancer.
People with an average risk of colon cancer can consider screening beginning at age 50. But people with an increased risk, such as those with a family history of colon cancer, should consider screening sooner. African-Americans and American Indians may consider beginning colon cancer screening at age 45.
Several screening options exist — each with its own benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you.
Diagnosing colon cancer
If your signs and symptoms indicate that you could have colon cancer, your doctor may recommend one or more tests and procedures, including:
- Using a scope to examine the inside of your colon. Colonoscopy uses a long, flexible and slender tube attached to a video camera and monitor to view your entire colon and rectum. If any suspicious areas are found, your doctor can pass surgical tools through the tube to take tissue samples (biopsies) for analysis.
- Blood tests. No blood test can tell you if you have colon cancer. But your doctor may test your blood for clues about your overall health, such as kidney and liver function tests.
Your doctor may also test your blood for a chemical sometimes produced by colon cancers (carcinoembryonic antigen or CEA). Tracked over time, the level of CEA in your blood may help your doctor understand your prognosis and whether your cancer is responding to treatment.
Staging colon cancer
Once you’ve been diagnosed with colon cancer, your doctor will order tests to determine the extent (stage) of your cancer. Staging helps determine what treatments are most appropriate for you.
Staging tests may include imaging procedures such as abdominal and chest CT scans. In many cases, the stage of your cancer may not be determined until after colon cancer surgery.
The stages of colon cancer are:
- Stage I. Your cancer has grown through the superficial lining (mucosa) of the colon or rectum but hasn’t spread beyond the colon wall or rectum.
- Stage II. Your cancer has grown into or through the wall of the colon or rectum but hasn’t spread to nearby lymph nodes.
- Stage III. Your cancer has invaded nearby lymph nodes but isn’t affecting other parts of your body yet.
- Stage IV. Your cancer has spread to distant sites, such as other organs — for instance, to your liver or lung.
Treatment for colon cancer
The type of treatment your doctor recommends will depend largely on the stage of your cancer. The three primary treatment options are surgery, chemotherapy and radiation.
Surgery for early-stage colon cancer
If your colon cancer is very small, your doctor may recommend a minimally invasive approach to surgery, such as:
- Removing polyps during colonoscopy. If your cancer is small, localized in a polyp and in a very early stage, your doctor may be able to remove it completely during a colonoscopy.
- Endoscopic mucosal resection. Removing larger polyps may require also taking a small amount of the lining of the colon in a procedure called endoscopic mucosal resection.
- Minimally invasive surgery. Polyps that can’t be removed during colonoscopy may be removed using laparoscopic surgery. In this procedure, your surgeon performs the operation through several small incisions in your abdominal wall, inserting instruments with attached cameras that display your colon on a video monitor. The surgeon may also take samples from lymph nodes in the area where the cancer is located.
Surgery for invasive colon cancer
If your colon cancer has grown into or through your colon, your surgeon may recommend:
Partial colectomy. During this procedure, the surgeon removes the part of your colon that contains the cancer, along with a margin of normal tissue on either side of the cancer. Your surgeon is often able to reconnect the healthy portions of your colon or rectum.
Surgery to create a way for waste to leave your body. When it’s not possible to reconnect the healthy portions of your colon or rectum, you may need to have a permanent or temporary colostomy. This involves creating an opening in the wall of your abdomen from a portion of the remaining bowel for the elimination of body waste into a special bag.
Sometimes the colostomy is only temporary, allowing your colon or rectum time to heal after surgery. In some cases, however, the colostomy may be permanent.
Lymph node removal. Nearby lymph nodes are usually also removed during colon cancer surgery and tested for cancer.
Surgery for advanced cancer
If your cancer is very advanced or your overall health very poor, your surgeon may recommend an operation to relieve a blockage of your colon or other conditions in order to improve your symptoms. This surgery isn’t done to cure cancer, but instead to relieve signs and symptoms, such as bleeding and pain.
In specific cases where the cancer has spread only to the liver and if your overall health is otherwise good, your doctor may recommend surgery to remove the cancerous lesion from your liver. Chemotherapy may be used before or after this type of surgery. This treatment may improve your prognosis.
Chemotherapy for colon cancer
Chemotherapy uses drugs to destroy cancer cells. Chemotherapy for colon cancer is usually given after surgery if the cancer has spread to the lymph nodes. In this way, chemotherapy may help reduce the risk of cancer recurrence. Chemotherapy may be used before surgery to shrink the cancer before an operation.
Chemotherapy can also be given to relieve symptoms of colon cancer that has spread to other areas of the body.
In people with rectal cancer, chemotherapy is typically used along with radiation therapy. This combination is often used before and after surgery.
Radiation therapy for colon cancer
Radiation therapy uses powerful energy sources, such as X-rays, to kill cancer cells that might remain after surgery, to shrink large tumors before an operation so that they can be removed more easily, or to relieve symptoms of colon cancer and rectal cancer.
Radiation therapy is rarely used in early-stage colon cancer, but is a routine part of treating rectal cancer, especially if the cancer has penetrated through the wall of the rectum or traveled to nearby lymph nodes. Radiation therapy, usually combined with chemotherapy, may be used before surgery in order to make the operation easier and to reduce the chance that an ostomy will be necessary. It can also be used after surgery to reduce the risk that the cancer may recur in the area of the rectum where it began.
Targeted drug therapy for colon cancer
Drugs that target specific defects that allow cancer cells to grow are available to people with advanced colon cancer, including:
- Bevacizumab (Avastin)
- Cetuximab (Erbitux)
- Panitumumab (Vectibix)
- Ramucirumab (Cyramza)
- Regorafenib (Stivarga)
- Ziv-aflibercept (Zaltrap)
Targeted drugs can be given along with chemotherapy or alone. Targeted drugs are typically reserved for people with advanced colon cancer.
Some people are helped by targeted drugs, while others are not. Researchers are working to determine who is most likely to benefit from targeted drugs. Until then, doctors carefully weigh the limited benefit of targeted drugs against the risk of side effects and the expensive cost when deciding whether to use these treatments.
Supportive (palliative) care for colon cancer
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
- Rectal bleeding. Mayo Clinic. http://www.mayoclinic.org/symptoms/rectal-bleeding/basics/definition/sym-20050740[↩][↩]
- Rectal bleeding causes. Mayo Clinic. http://www.mayoclinic.org/symptoms/rectal-bleeding/basics/causes/sym-20050740[↩]
- Understanding Minor Rectal Bleeding. American Society for Gastrointestinal Endoscopy. https://www.asge.org/home/for-patients/patient-information/understanding-minor-rectal-bleeding[↩][↩][↩]
- Hemorrhoids. Medline Plus. https://medlineplus.gov/hemorrhoids.html[↩][↩][↩]
- Fox A, Tietze PH, Ramakrishnan K. Anorectal conditions: hemorrhoids. FP Essentials. 2014;419:11–19.[↩]
- Definition & Facts of Hemorrhoids. The National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/definition-facts[↩]
- Anal fissure. Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/anal-fissure/symptoms-causes/syc-20351424[↩][↩]
- Solitary rectal ulcer syndrome. Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/rectal-ulcer/basics/definition/con-20027352[↩][↩][↩]
- Proctitis. Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/proctitis/basics/definition/con-20027855[↩]
- Huyck A, Broderick K. Hydrotherapy. In: Pizzorno JE, Murray MT, eds. Textbook of Natural Medicine. 4th ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2013:chap 40.[↩]
- Colon polyps. Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/colon-polyps/symptoms-causes/syc-20352875[↩][↩][↩][↩]
- Colon cancer. Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/colon-cancer/symptoms-causes/syc-20353669[↩]