Contents
- What is burning pain in stomach after eating ?
- What You Must Do If You Have Chest Pain ?
- Who is more likely to have gastroesophageal reflux disease (GERD) ?
- What causes heartburn and GERD ?
- What are the complications of GERD ?
- Ignoring persistent heartburn symptoms can lead to severe consequences
- What are symptoms of gastroesophageal reflux
- How do doctors diagnose gastroesophageal reflux ?
- Treatment for GER & GERD
- How do doctors treat gastroesophageal reflux disease (GERD) ?
What is burning pain in stomach after eating ?
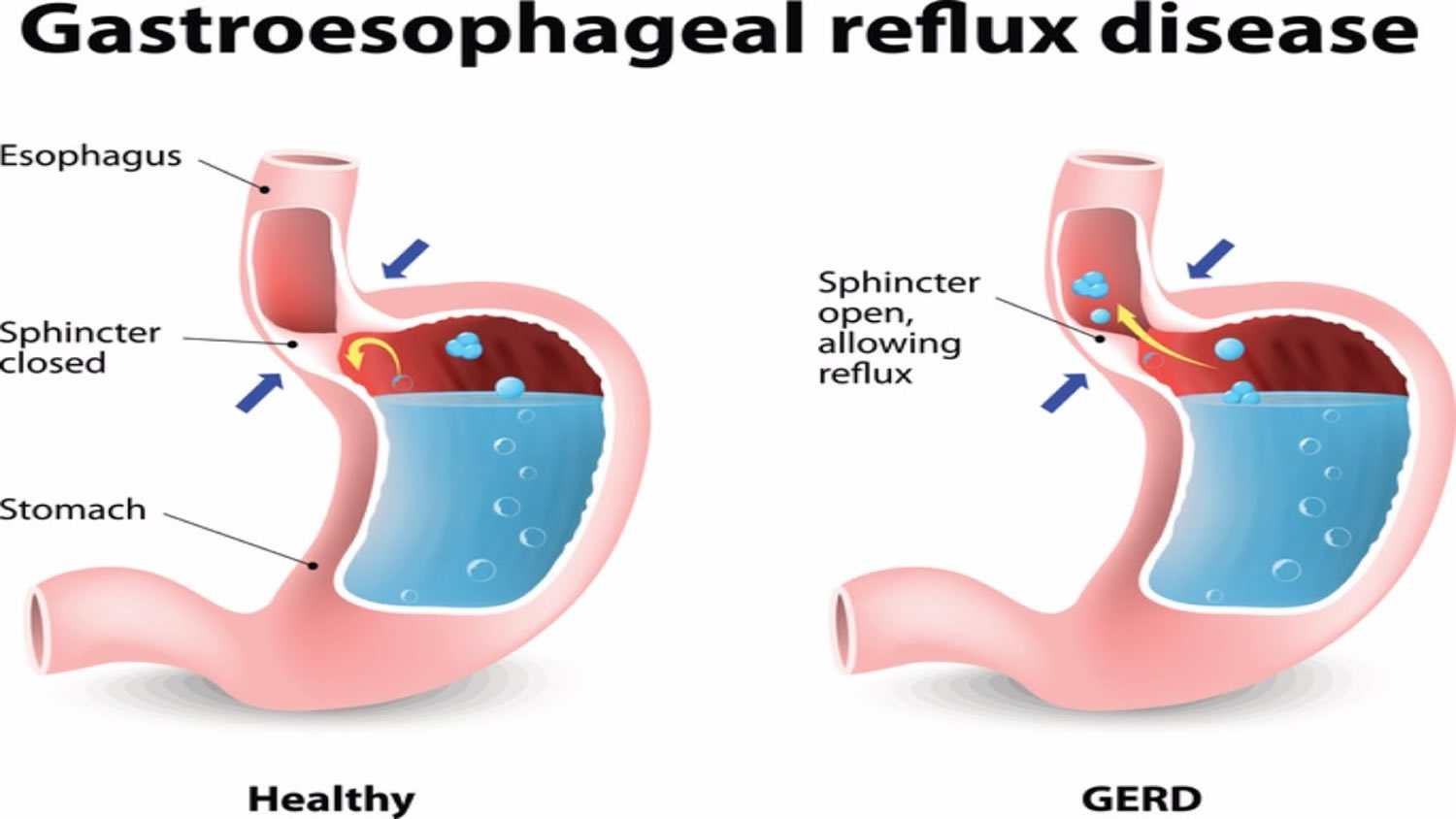
Your esophagus is the tube that carries food from your mouth to your stomach. Gastroesophageal reflux (GER) is a physical condition when a muscle (the lower esophageal sphincter or “LES”) at the end of your esophagus does not close properly, allowing the acid from the stomach to flow backward up into the esophagus and irritate it 1. Stomach acid that touches the lining of your esophagus can cause heartburn, also called acid indigestion 2. You may feel a burning in the chest or throat called heartburn. Sometimes, you can taste the bitter or sour taste of the stomach acid fluid in the back of the throat. Many describe heartburn as a feeling of burning discomfort, localized behind the breastbone, that moves up toward the neck and throat. The burning and pressure symptoms of heartburn can last for several hours and often worsen after eating food 3.
Doctors also refer to gastroesophageal reflux (GER) as 2:
- acid indigestion
- acid reflux
- acid regurgitation
- heartburn
- reflux
Gastroesophageal reflux (GER) that occurs more than twice a week for a few weeks could be gastroesophageal reflux disease (GERD) 2. Gastroesophageal reflux disease (GERD) can lead to more serious health problems over time. If you think you have GERD, you should see your doctor.
All of us may have occasional heartburn. However, frequent heartburn (two or more times a week), food sticking, blood or weight loss may be associated with a more severe problem known as gastroesophageal reflux disease or GERD 3. If you have these symptoms more than twice a week, you may have gastroesophageal reflux disease (GERD) 3.
- You can also have gastroesophageal reflux disease (GERD) without having heartburn. Your symptoms could include a dry cough, asthma symptoms, or trouble swallowing 1.
More than 60 million persons in the United States report symptoms of gastroesophageal reflux disease (GERD) at least weekly and and some studies have suggested that more than 15 million Americans experience heartburn symptoms each day 3. Your typical full-time family physician can expect to diagnose and treat 40 to 60 patients with this condition each month 4.
- Heartburn is a common, but not trivial condition.
In fact, if left untreated, longstanding, severe and chronic heartburn has been linked with esophageal cancer 3. Don’t ignore frequent heartburn — instead consult with your physician regarding an endoscopy and treatment to achieve early symptom resolution.
Anyone, including infants and children, can have GERD. If not treated, it can lead to more serious health problems. In some cases, you might need medicines or surgery. However, many people can improve their symptoms by:
- Avoiding alcohol and spicy, fatty or acidic foods that trigger heartburn
- Eating smaller meals
- Not eating close to bedtime
- Losing weight if needed
- Wearing loose-fitting clothes.
What You Must Do If You Have Chest Pain ?
Because the pain is similar to heart pain or heart attack, patients and physicians frequently attribute this pain to the heart. In fact, many patients present to emergency rooms concerned about a heart attack and commonly undergo cardiac studies. After these cardiac tests fail to show evidence of heart disease, the patients receive the diagnosis of non-cardiac chest pain, leading the physician to examine other causes for this chest pain.
- Many people aren’t sure what’s wrong when they are having symptoms of a heart attack.
Heart attack treatment works best when it’s given right after symptoms occur.
- Don’t Wait–Get Help Quickly
- Quick Action Can Save Your Life !
- If you think you or someone else is having a heart attack, even if you’re not sure, don’t feel embarrassed to call your local emergency number right away !
- Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. Take a nitroglycerin pill if your doctor has prescribed this type of treatment.
Symptoms of a heart attack
- Remember acting fast at the first sign of heart attack symptoms can save your life and limit damage to your heart 5. Treatment works best when it’s given right after symptoms occur.
- Not all heart attacks begin with the sudden, crushing chest pain that often is shown on TV or in the movies. In one study, for example, one-third of the patients who had heart attacks had no chest pain 6. These patients were more likely to be older, female, or diabetic.
Figure 1. Esophagus
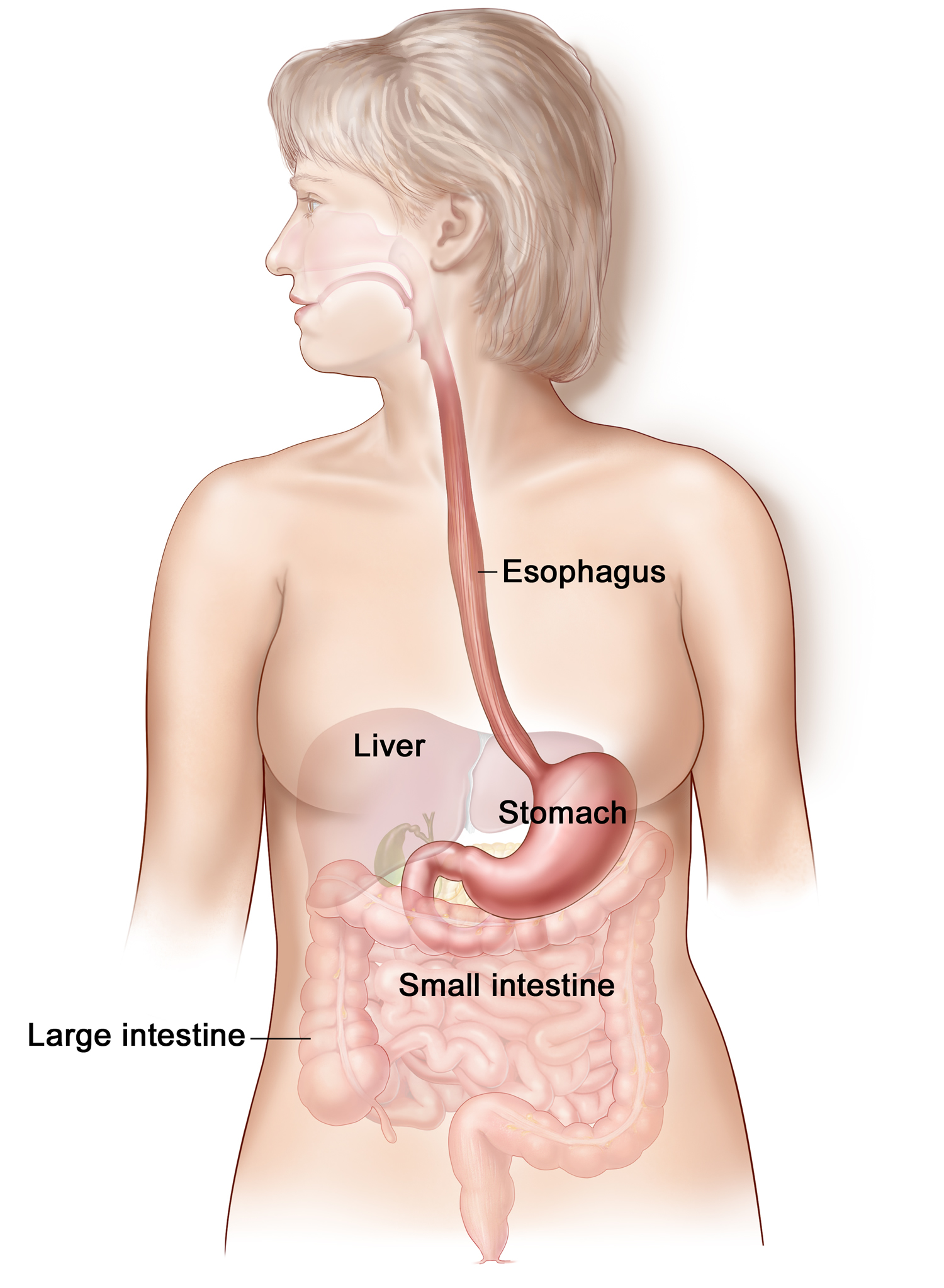
Figure 2. Gastroesophageal reflux disease (GERD)
Who is more likely to have gastroesophageal reflux disease (GERD) ?
Anyone can develop gastroesophageal reflux disease (GERD), some for unknown reasons. You are more likely to have GERD if you are:
- overweight or obese
- a pregnant woman
- taking certain medicines
- a smoker or regularly exposed to secondhand smoke
What causes heartburn and GERD ?
To understand gastroesophageal reflux disease or GERD, it is first necessary to understand what causes heartburn. Most people will experience heartburn if the lining of the esophagus comes in contact with too much stomach juice for too long a period of time. This stomach juice consists of acid, digestive enzymes, and other injurious materials. The prolonged contact of acidic stomach juice with the esophageal lining injures the esophagus and produces a burning discomfort. Normally, a muscular valve at the lower end of the esophagus called the lower esophageal sphincter or “LES” — keeps the acid in the stomach and out of the esophagus. In gastroesophageal reflux disease or GERD, the lower esophageal sphincter relaxes too frequently, which allows stomach acid to reflux, or flow backward into the esophagus.
The lower esophageal sphincter becomes weak or relaxes due to certain things, such as:
- increased pressure on your abdomen from being overweight, obese, or pregnant
- smoking, or inhaling secondhand smoke
- certain medicines, including:
+ those that doctors use to treat asthma —a long-lasting disease in your lungs that makes you extra sensitive to things that you’re allergic to
+ calcium channel blockers—medicines that treat high blood pressure
+ antihistamines—medicines that treat allergy symptoms
+ painkillers
+ sedatives—medicines that help put you to sleep
+ antidepressants —medicines that treat depression
- A hiatal hernia can also cause GERD. Hiatal hernia is a condition in which the opening in your diaphragm lets the upper part of the stomach move up into your chest, which lowers the pressure in the esophageal sphincter.
You should see a doctor if you have persistent gastroesophageal reflux symptoms that do not get better with over-the-counter medications or change in your diet.
See a doctor right away if you:
- vomit large amounts
- have regular projectile, or forceful, vomiting
- vomit fluid that is
+ green or yellow
+ looks like coffee grounds
+ contains blood - have problems breathing after vomiting
- have pain in the mouth or throat when you eat
- have problems swallowing or painful swallowing
What are the complications of GERD ?
Without treatment, GERD can sometimes cause serious complications over time, such as:
Esophagitis
Esophagitis is inflammation in the esophagus. Adults who have chronic esophagitis over many years are more likely to develop precancerous changes in the esophagus.
Esophageal stricture
This results from chronic acid injury and scarring of the lower esophagus. Patients complain of food sticking in the lower esophagus or problems with swallowing. Heartburn symptoms may actually lessen as the esophageal opening narrows down preventing acid reflux. Stretching of the esophagus and proton pump inhibitor medication are needed to control and prevent peptic strictures.
Respiratory problems
With GERD you might breathe stomach acid into your lungs. The stomach acid can then irritate your throat and lungs, causing respiratory problems, such as:
- Asthma —a long-lasting disease in your lungs that makes you extra sensitive to things that you’re allergic to
- Chest congestion, or extra fluid in your lungs
- A dry, long-lasting cough or a sore throat
- Hoarseness—the partial loss of your voice
- Laryngitis—the swelling of your voice box that can lead to a short-term loss of your voice
- Pneumonia—an infection in one or both of your lungs—that keeps coming back
- Wheezing—a high-pitched whistling sound when you breathe.
Barrett’s esophagus
GERD can sometimes cause Barrett’s esophagus. Here the lining of the esophagus changes to resemble the intestine. People with Barrett’s esophagus have approximately a 30-fold increased risk of developing esophageal cancer 3. Barrett’s esophagus can be found in 5 to 15% of patients who have endoscopy for symptoms of GERD and tends to be seen at the higher end of this range in patients with long duration of symptoms, who are over the age of 50, male, and Caucasian 7.
If you have GERD, speak to your doctor about how to prevent or treat long-term problems.
Esophageal Cancer
Recent scientific reports have confirmed that if GERD is left untreated for many years, it could lead to this most serious complication — Barrett’s esophagus and esophageal cancer. Frequent heartburn symptoms with a duration of several years cannot simply be dismissed — there can be severe consequences of delaying diagnosis and treatment. This increased risk of chronic, longstanding GERD sufferers to develop cancer demonstrates the true severity of heartburn. In patients with chronic heartburn, an endoscopy will often be recommended to visually monitor the condition of the lining of the esophagus and identify or confirm the absence of any suspicious or pre-malignant lesions, such as Barrett’s esophagus. So, do not ignore your heartburn. If you are having heartburn two or more times a week, it is time to see your physician and in all likelihood a gastrointestinal specialist. In most cases an endoscopy should be performed to evaluate the severity of GERD and identify the possible presence of the pre-malignant condition — Barrett’s esophagus. The preventative strategy is to treat GERD. If it goes untreated and cancer does develop, the survival rate for esophageal cancer, at this time, is dismal.
GERD can masquerade as other diseases
Increasingly, doctors are becoming aware that the irritation and damage to the esophagus from continual presence of acid can prompt an entire array of symptoms other than simple heartburn. Experts recognize that often the role of acid reflux has been overlooked as a potential factor in the diagnosis and treatment of patients with chronic cough, hoarseness and asthma-like symptoms. In some instances, patients have never reported heartburn, and in others the potential causal link between reflux and the onset of these so-called “extra-esophageal manifestations” has not been fully recognized. Physicians are increasingly becoming aware that it is good clinical practice to evaluate the possible presence of reflux in patients with chronic cough and asthma-like symptoms, as well as the importance that acid suppression and treating underlying reflux can have in potentially improving the symptoms in these patients.
- Chest Pain: Patients with GERD may have chest pain similar to angina or heart pain. Usually, they also have other symptoms like heartburn and acid regurgitation. If your doctor says your chest pain is not coming from the heart, don’t forget the esophagus. On the other hand, if you have chest pain, you should not assume it is your esophagus until you have been evaluated for a potential heart cause by your physician.
- Asthma: Acid reflux may aggravate asthma. Recent studies suggest that the majority of asthmatics have acid reflux. Clues that GERD may be worsening your asthma include: 1) asthma that appears for the first time during adulthood; 2) asthma that gets worse after meals, lying down or exercise; and 3) asthma that is mainly at night. Treatment of acid reflux may cure asthma in some patients and decrease the need for asthmatic medications in others.
- Ear, Nose and Throat Problems: Acid reflux may be a cause of chronic cough, sore throat, laryngitis with hoarseness, frequent throat clearing, or growths on the vocal cords. If these problems do not get better with standard treatments, think about GERD.
Ignoring persistent heartburn symptoms can lead to severe consequences
Study links duration of heartburn to severity of esophageal disease
Esophageal disease may be perceived in many forms, with heartburn being the most common. The severity of heartburn is measured by how long a given episode lasts, how often symptoms occur, and/or their intensity. Since the esophageal lining is sensitive to stomach contents, persistent and prolonged exposure to these contents may cause changes such as inflammation, ulcers, bleeding and scarring with obstruction. A pre-cancerous condition called Barrett’s esophagus may also occur. Barrett’s esophagus causes severe damage to the lining of the esophagus when the body attempts to protect the esophagus from acid by replacing its normal lining with cells that are similar to the intestinal lining.
Research was conducted to determine whether the duration of heartburn symptoms increases the risk of having esophageal complications. The study found that inflammation in the esophagus not only increased with the duration of reflux symptoms, but that Barrett’s esophagus likewise was more frequently diagnosed in these patients. Those patients with reflux symptoms and a history of inflammation in the past were more likely to have Barrett’s esophagus than those without a history of esophageal inflammation.
Study links chronic heartburn to esophageal cancer
Over the past 20 years, the incidence of esophageal cancer, a highly fatal form of cancer, has rapidly increased in the United States. A recent research study has linked chronic, longstanding, untreated heartburn with an increased risk of developing esophageal cancer. As reported by Lagergren et al. in the study that was published in the New England Journal of Medicine, patients who experienced chronic, unresolved heartburn markedly increase the risk of esophageal cancer, a rare but often deadly malignancy. According to the study, the incidence of adenocarcinoma of the esophagus was nearly eight times more likely among frequent heartburn sufferers (two times a week or more) compared to individuals without symptoms, while among patients with longstanding, severe and unresolved heartburn (e.g. frequent symptoms 20 years duration), the risk of developing esophageal cancer was 43.5 times as great as for those without chronic heartburn.
Persistent symptoms of heartburn and reflux should not be ignored. By seeing your doctor early, the physical cause of GERD can be treated and more serious problems avoided.
What are symptoms of gastroesophageal reflux
If you have gastroesophageal reflux (GER), you may taste food or stomach acid in the back of your mouth.
The most common symptom of gastroesophageal reflux disease (GERD) is regular heartburn, a painful, burning feeling in the middle of your chest, behind your breastbone, and in the middle of your abdomen. Not all adults with GERD have heartburn.
Other common GERD symptoms include 8:
- bad breath
- nausea
- pain in your chest or the upper part of your abdomen
- problems swallowing or painful swallowing
- respiratory problems
- vomiting
- the wearing away of your teeth
Some symptoms of GERD come from its complications, including those that affect your lungs.
How do doctors diagnose gastroesophageal reflux ?
In most cases, your doctor diagnoses gastroesophageal reflux (GER) by reviewing your symptoms and medical history. If your symptoms don’t improve with lifestyle changes and medications, you may need testing.
How do doctors diagnose gastroesophageal reflux disease (GERD) ?
If your gastroesophageal reflux symptoms don’t improve, if they come back frequently, or if you have trouble swallowing, your doctor may recommend testing you for gastroesophageal reflux disease (GERD).
Your doctor may refer you to a gastroenterologist to diagnose and treat GERD.
What tests do doctors use to diagnose gastroesophageal reflux disease (GERD) ?
Several tests can help a doctor diagnose GERD. Your doctor may order more than one test to make a diagnosis.
Upper gastrointestinal (GI) endoscopy and biopsy
In an upper GI endoscopy, a gastroenterologist, surgeon, or other trained health care professional uses an endoscope to see inside your upper GI tract. This procedure takes place at a hospital or an outpatient center.
An intravenous (IV) needle will be placed in your arm to provide a sedative. Sedatives help you stay relaxed and comfortable during the procedure. In some cases, the procedure can be performed without sedation. You will be given a liquid anesthetic to gargle or spray anesthetic on the back of your throat. The doctor carefully feeds the endoscope down your esophagus and into your stomach and duodenum. A small camera mounted on the endoscope sends a video image to a monitor, allowing close examination of the lining of your upper GI tract. The endoscope pumps air into your stomach and duodenum, making them easier to see.
The doctor may perform a biopsy with the endoscope by taking a small piece of tissue from the lining of your esophagus. You won’t feel the biopsy. A pathologist examines the tissue in a lab.
In most cases, the procedure only diagnoses GERD if you have moderate to severe symptoms.
Upper GI series
An upper GI series looks at the shape of your upper GI tract.
An x-ray technician performs this procedure at a hospital or an outpatient center. A radiologist reads and reports on the x-ray images. You don’t need anesthesia. A health care professional will tell you how to prepare for the procedure, including when to stop eating and drinking.
During the procedure, you will stand or sit in front of an x-ray machine and drink barium to coat the inner lining of your upper GI tract. The x-ray technician takes several x-rays as the barium moves through your GI tract. The upper GI series can’t show GERD in your esophagus; rather, the barium shows up on the x-ray and can find problems related to GERD, such as:
- hiatal hernias
- esophageal strictures
- ulcers
You may have bloating and nausea for a short time after the procedure. For several days afterward, you may have white or light-colored stools from the barium. A health care professional will give you instructions about eating, drinking, and taking your medicines after the procedure.
Esophageal pH and impedance monitoring
The most accurate procedure to detect acid reflux is esophageal pH and impedance monitoring. Esophageal pH and impedance monitoring measures the amount of acid in your esophagus while you do normal things, such as eating and sleeping.
A gastroenterologist performs this procedure at a hospital or an outpatient center as a part of an upper GI endoscopy. Most often, you can stay awake during the procedure.
A gastroenterologist will pass a thin tube through your nose or mouth into your stomach. The gastroenterologist will then pull the tube back into your esophagus and tape it to your cheek. The end of the tube in your esophagus measures when and how much acid comes up your esophagus. The other end of the tube attaches to a monitor outside your body that records the measurements.
You will wear a monitor for the next 24 hours. You will return to the hospital or outpatient center to have the tube removed.
This procedure is most useful to your doctor if you keep a diary of when, what, and how much food you eat and your GERD symptoms are after you eat. The gastroenterologist can see how your symptoms, certain foods, and certain times of day relate to one another. The procedure can also help show whether acid reflux triggers any respiratory symptoms.
Bravo wireless esophageal pH monitoring
Bravo wireless esophageal pH monitoring also measures and records the pH in your esophagus to determine if you have GERD. A doctor temporarily attaches a small capsule to the wall of your esophagus during an upper endoscopy. The capsule measures pH levels in the esophagus and transmits information to a receiver. The receiver is about the size of a pager, which you wear on your belt or waistband.
You will follow your usual daily routine during monitoring, which usually lasts 48 hours. The receiver has several buttons on it that you will press to record symptoms of GERD such as heartburn. The nurse will tell you what symptoms to record. You will be asked to maintain a diary to record certain events such as when you start and stop eating and drinking, when you lie down, and when you get back up.
To prepare for the test talk to your doctor about medicines you are taking. He or she will tell you whether you can eat or drink before the procedure. After about seven to ten days the capsule will fall off the esophageal lining and pass through your digestive tract.
Esophageal manometry
Esophageal manometry measures muscle contractions in your esophagus. A gastroenterologist may order this procedure if you’re thinking about anti-reflux surgery.
The gastroenterologist can perform this procedure during an office visit. A health care professional will spray a liquid anesthetic on the back of your throat or ask you to gargle a liquid anesthetic.
The gastroenterologist passes a soft, thin tube through your nose and into your stomach. You swallow as the gastroenterologist pulls the tube slowly back into your esophagus. A computer measures and records the pressure of muscle contractions in different parts of your esophagus.
The procedure can show if your symptoms are due to a weak sphincter muscle. A doctor can also use the procedure to diagnose other esophagus problems that might have symptoms similar to heartburn. A health care professional will give you instructions about eating, drinking, and taking your medicines after the procedure.
Treatment for GER & GERD
Gastroesophageal reflux disease (GERD) is a problem that is symptomatic by day but in which much damage is done by night.
Treatment should be designed to:
- Eliminate symptoms;
- Heal esophagitis; and
- Prevent the relapse of esophagitis or development of complications in patients with esophagitis.
All treatments are based on attempts to a) decrease the amount of acid that refluxes from the stomach back into the esophagus, or b) make the refluxed material less irritating to the lining of the esophagus.
In many patients, GERD is a chronic, relapsing disease. Long-term maintenance is the key to therapy; therefore, continuous long-term therapy, possibly life-long therapy, to control symptoms and prevent complications is appropriate. Maintenance therapy will vary in individuals ranging from mere lifestyle modifications to prescription medication as treatment.
You may be able to control gastroesophageal reflux (GER) and gastroesophageal reflux disease (GERD) by:
- not eating or drinking items that may cause GER, such as greasy or spicy foods and alcoholic drinks
- not overeating
- not eating 2 to 3 hours before bedtime 9, 10
- losing weight if you’re overweight or obese 11, 12, 13
- quitting smoking and avoiding secondhand smoke 14, 15, 16
- cessation of chocolate, caffeine, peppermint, citrus, carbonated beverages, tomatoes and tomato products
- taking over-the-counter medicines, such as Maalox , or Rolaids
- head of bed elevation 17, 18, 19
How do doctors treat gastroesophageal reflux disease (GERD) ?
Depending on the severity of your symptoms, your doctor may recommend lifestyle changes, medicines, surgery, or a combination.
Lifestyle changes
Making lifestyle changes can reduce your GER and GERD symptoms. You should:
- lose weight, if needed.
- wear loose-fitting clothing around your abdomen. Tight clothing can squeeze your stomach area and push acid up into your esophagus.
- stay upright for 3 hours after meals. Avoid reclining and slouching when sitting.
- sleep on a slight angle. Raise the head of your bed 6 to 10 inches by safely putting blocks under the bedposts. Just using extra pillows will not help.
- quit smoking and avoid secondhand smoke.
Raise the Head of the Bed. The simplest method is to use a 4″ x 4″ piece of wood to which two jar caps have been nailed an appropriate distance apart to receive the legs or casters at the upper end of the bed. Failure to use the jar caps inevitably results in the patient being jolted from sleep as the upper end of the bed rolls off the 4″ x 4″.
Alternatively, one may use an under-mattress foam wedge to elevate the head about 6-10 inches. Pillows are not an effective alternative for elevating the head in preventing reflux.
Over-the-counter and prescription medicines
You can buy many GERD medicines without a prescription. However, if you have symptoms that will not go away, you should see your doctor.
All GERD medicines work in different ways. You may need a combination of GERD medicines to control your symptoms.
Antacids. Doctors often first recommend antacids to relieve heartburn and other mild GER and GERD symptoms. Antacids include over-the-counter medicines such as:
- Maalox
- Mylanta
- Riopan
- Rolaids
Antacids can have side effects, including diarrhea and constipation.
H2 blockers. H2 blockers decrease acid production. They provide short-term or on-demand relief for many people with GER and GERD symptoms. They can also help heal the esophagus, although not as well as other medicines. You can buy H2 blockers over-the-counter or your doctor can prescribe one. Types of H2 blockers include:
- cimetidine (Tagamet HB)
- famotidine (Pepcid AC)
- nizatidine (Axid AR)
- ranitidine (Zantac 75)
If you get heartburn after eating, your doctor may recommend that you take an antacid and an H2 blocker. The antacid neutralizes stomach acid, and the H2 blocker stops your stomach from creating acid. By the time the antacid stops working, the H2 blocker has stopped the acid.
Proton pump inhibitors (PPIs). PPIs lower the amount of acid your stomach makes. PPIs are better at treating GERD symptoms than H2 blockers.2 They can heal the esophageal lining in most people with GERD. Doctors often prescribe PPIs for long-term GERD treatment.
However, studies show that people who take PPIs for a long time or in high doses are more likely to have hip, wrist, and spinal fractures. You need to take these medicines on an empty stomach so that your stomach acid can make them work.
Several types of PPIs are available by a doctor’s prescription, including:
- esomeprazole (Nexium)
- lansoprazole (Prevacid)
- omeprazole (Prilosec, Zegerid)
- pantoprazole (Protonix)
- rabeprazole (AcipHex)
Talk with your doctor about taking lower-strength omeprazole or lansoprazole, sold over the counter.
Prokinetics. Prokinetics help your stomach empty faster. Prescription prokinetics include
- bethanechol (Urecholine)
- metoclopramide (Reglan)
Both of these medicines have side effects, including:
- nausea
- diarrhea
- fatigue, or feeling tired
- depression
- anxiety
- delayed or abnormal physical movement.
Prokinetics can cause problems if you mix them with other medicines, so tell your doctor about all the medicines you’re taking.
Antibiotics. Antibiotics, including erythromycin , can help your stomach empty faster. Erythromycin has fewer side effects than prokinetics; however, it can cause diarrhea.
When symptoms of heartburn are not controlled with modifications in lifestyle, and over-the-counter medicines are needed two or more times a week, or symptoms remain unresolved on the medication you are taking, you should see your doctor. You may have GERD.
- When GERD is not treated, serious complications can occur, such as severe chest pain that can mimic a heart attack, esophageal stricture (a narrowing or obstruction of the esophagus), bleeding, or a pre-malignant change in the lining of the esophagus called Barrett’s esophagus. A 1999 study reported in the New England Journal of Medicine showed that patients with chronic, untreated heartburn of many years duration were at substantially greater risk of developing esophageal cancer, which is one of the fastest growing, and among the more lethal forms of cancer in this country.
Symptoms suggesting that serious damage may have already occurred include:
- Dysphagia: difficulty swallowing or a feeling that food is trapped behind the breast bone.
- Bleeding: vomiting blood, or having tarry, black bowel movements.
- Choking: sensation of acid refluxed into the windpipe causing shortness of breath, coughing, or hoarseness of the voice.
- Weight Loss
Surgery
Your doctor may recommend surgery if your GERD symptoms don’t improve with lifestyle changes or medicines. You’re more likely to develop complications from surgery than from medicines.
Fundoplication is the most common surgery for GERD. In most cases, it leads to long-term reflux control.
A surgeon performs fundoplication using a laparoscope, a thin tube with a tiny video camera. During the operation, a surgeon sews the top of your stomach around your esophagus to add pressure to the lower end of your esophagus and reduce reflux. The surgeon performs the operation at a hospital. You receive general anesthesia and can leave the hospital in 1 to 3 days. Most people return to their usual daily activities in 2 to 3 weeks.
Endoscopic techniques, such as endoscopic sewing and radiofrequency, help control GERD in a small number of people. Endoscopic sewing uses small stitches to tighten your sphincter muscle. Radiofrequency creates heat lesions, or sores, that help tighten your sphincter muscle. A surgeon performs both operations using an endoscope at a hospital or an outpatient center, and you receive general anesthesia.
The results for endoscopic techniques may not be as good as those for fundoplication. Doctors don’t use endoscopic techniques often.
Table 1. Effectiveness of Therapies for GERD
| Class of Drugs | How It Works | Eliminate Symptoms | Heal Esophagitis | Manage or Prevent Complications | Maintain Remission |
| Antacids | neutralize acid | +1 | 0 | 0 | 0 |
| H2 Blockers Over-the-counter | mildly suppress acid | +1 | 0 | 0 | 0 |
| Promotility | increase LES pressure; move acid from esophagus and stomach | +2 | +1 | 0 | +1 |
| H2 Blockers Prescription | moderately suppress acid | +2 | +2 | +1 | +1 |
| H2 Blockers + Promotility | moderately suppress acid; move acid from esophagus to stomach | +3 | +3 | +1 | +1 |
| High Dose H2 Blockers | moderately suppress acid | +3 | +3 | +2 | +2 |
| Proton Pump Inhibitors | markedly suppress acid | +4 | +4 | +3 | +4 |
| Surgery | improve barrier between stomach and esophagus to prevent acid reflux | +4 | +4 | +3 | +4 |
- GERD. Medline Plus. https://medlineplus.gov/gerd.html[↩][↩]
- Definition & Facts for GER & GERD. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults/definition-facts[↩][↩][↩]
- Acid Reflux. American College of Gastroenterology. http://patients.gi.org/topics/acid-reflux/[↩][↩][↩][↩][↩][↩]
- El-Serag HB, et al. Gastroesophageal reflux among different racial groups in the United States. Gastroenterology. 2004;126(7):1692–1699.[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Heart Attack. https://www.nhlbi.nih.gov/health/health-topics/topics/heartattack[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. What Are the Symptoms of a Heart Attack ? https://www.nhlbi.nih.gov/health/health-topics/topics/heartattack/signs[↩]
- Westhoff B, Brotze S, Weston A et al. The frequency of Barrett’s esophagus in high-risk patients with chronic GERD. Gastrointest Endosc 2005;61:226–231.[↩]
- Symptoms & Causes of GER & GERD. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults/symptoms-causes[↩]
- Duroux P, Bauerfeind P, Emde C et al. Early dinner reduces nocturnal gastric acidity. Gut 1989;30:1063–1067.[↩]
- Orr WC, Harnish MJ. Sleep-related gastro-oesophageal reflux: provocation with a late evening meal and treatment with acid suppression. Aliment Pharmacol Ther 1998;12:1033–1038.[↩]
- Jacobson BC, Somers SC, Fuchs CS et al. Body-mass index and symptoms of gastroesophageal reflux in women. N Engl J Med 2006;354:2340–2348.[↩]
- Fraser-Moodie CA, Norton B, Gornall C et al. Weight loss has an independent beneficial effect on symptoms of gastro-oesophageal reflux in patients who are overweight. Scand J Gastroenterol 1999;34:337–340.[↩]
- Mathus-Vliegen LM, Tytgat GN. Twenty-four-hour pH measurements in morbid obesity: effects of massive overweight, weight loss and gastric distension. Eur J Gastroenterol Hepatol 1996;8:635–640.[↩]
- Schindlbeck NE, Heinrich C, Dendorfer A et al. Influence of smoking and esophageal intubation on esophageal pH-metry. Gastroenterology 1987;92:1994–1997.[↩]
- Waring JP, Eastwood TF, Austin JM et al. The immediate effects of cessation of cigarette smoking on gastroesophageal reflux. Am J Gastroenterol 1989;84:1076–1078.[↩]
- Kadakia SC, Kikendall JW, Maydonovitch C et al. Effect of cigarette smoking on gastroesophageal reflux measured by 24-h ambulatory esophageal pH monitoring. Am J Gastroenterol 1995;90:1785–1790.[↩]
- Stanciu C, Bennett JR. Effects of posture on gastro-oesophageal reflux. Digestion 1977;15:104–109.[↩]
- Hamilton JW, Boisen RJ, Yamamoto DT et al. Sleeping on a wedge diminishes exposure of the esophagus to refluxed acid. Dig Dis Sci 1988;33:518–522.[↩]
- Pollmann H, Zillessen E, Pohl J et al. Effect of elevated head position in bed in therapy of gastroesophageal reflux. Z Gastroenterol 1996;34(Suppl 2): 93–99.[↩]
- Acid Reflux.American College of Gastroenterology. http://patients.gi.org/topics/acid-reflux/[↩]





