Contents
- What is cataract
- Types of cataracts
- What causes cataracts
- Cataract Prevention
- Cataract symptoms
- Cataract diagnosis
- Cataract treatment
- Congenital cataracts
What is cataract
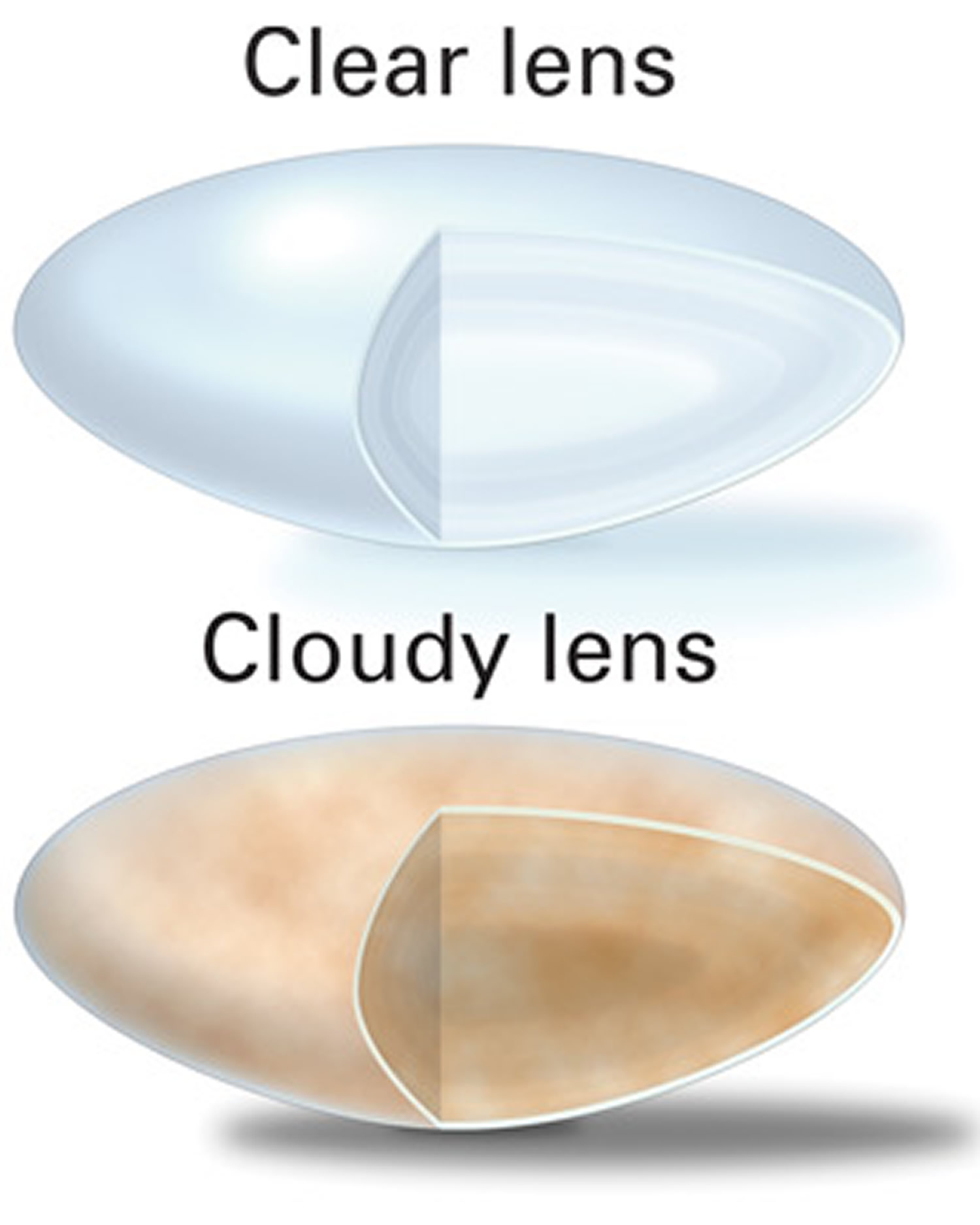
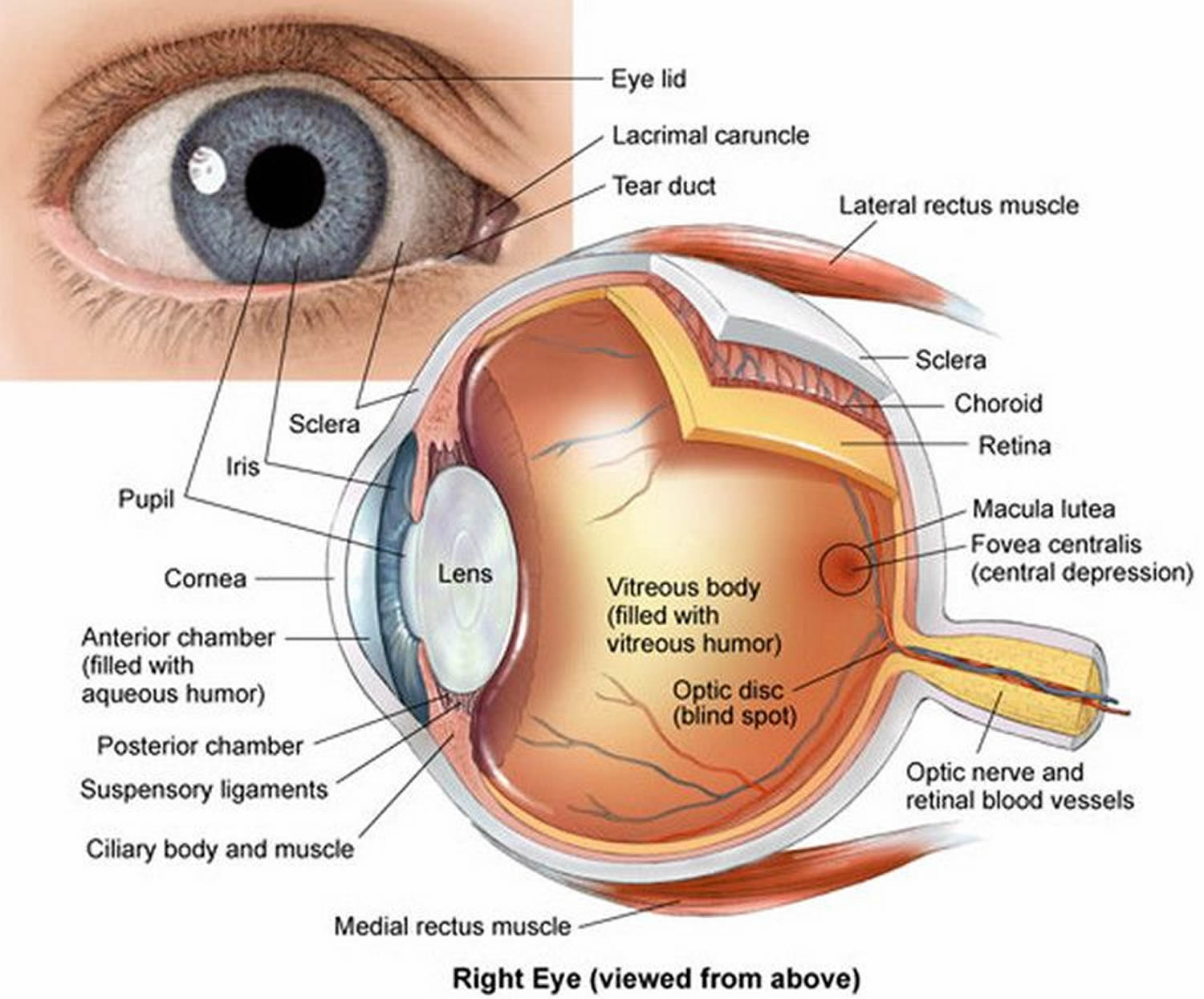
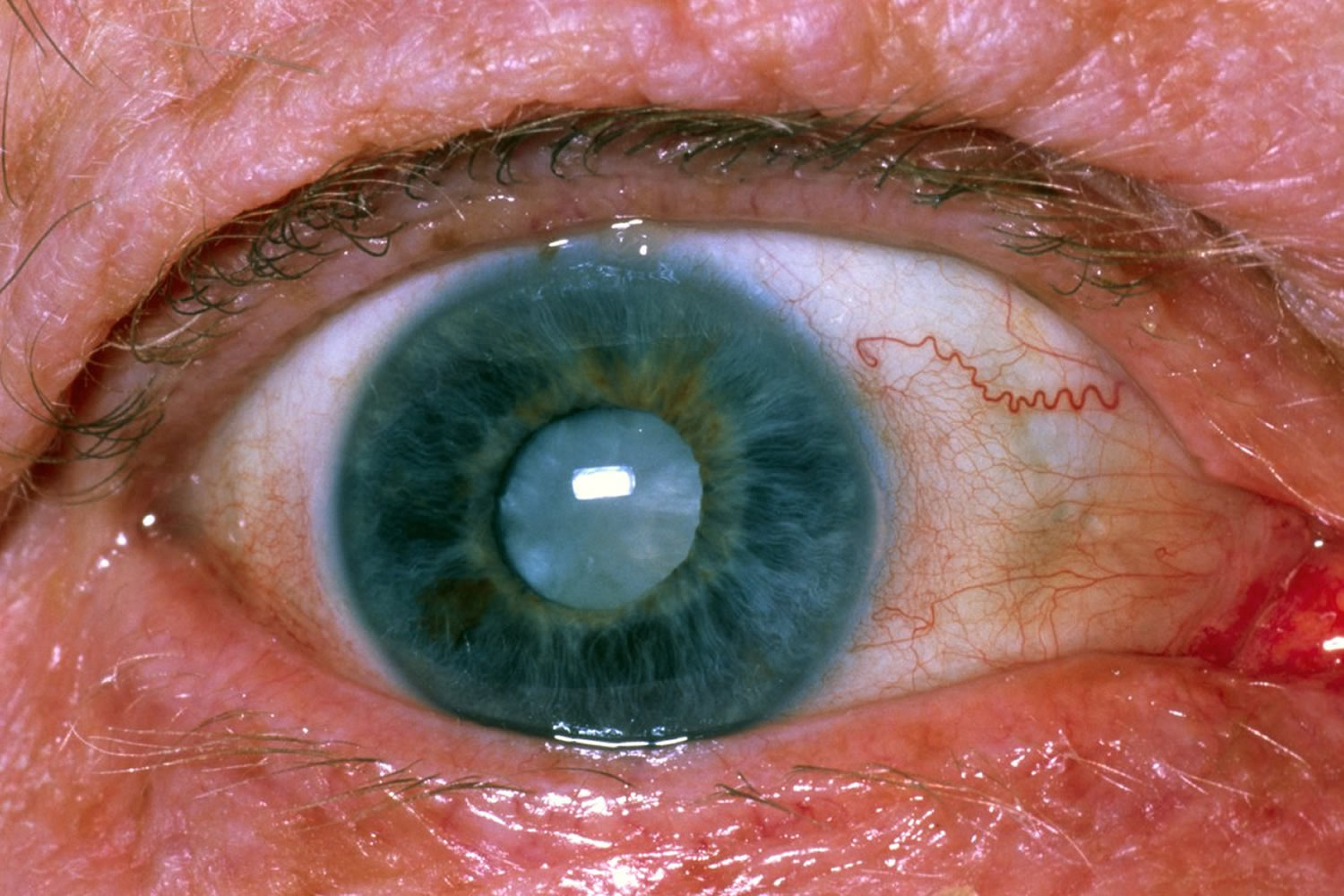
Cataracts are when the lens, a small transparent disc inside your eye, develops cloudy patches (see Figures 2 and 3). Inside your eyes, you have a natural lens. The lens bends (refracts) light rays that come into your eye to help you see. The lens should be clear, like the top lens in Figure 1 and 2.
Cataracts usually appear in both eyes. They may not necessarily develop at the same time or be the same in each eye.
When you’re young, your lenses are usually like clear glass, allowing you to see through them. As you get older, they start to become frosted, like bathroom glass, and begin to limit your vision.
If you have a cataract, your lens has become cloudy, like the bottom lens in the illustration. It is like looking through a foggy or dusty car windshield. Things look blurry, hazy or less colorful with a cataract. Over time these patches usually become bigger causing blurry, misty vision and eventually blindness.
How quickly the cataract develops varies among individuals and may even be different between the two eyes. Most age-related cataracts progress gradually over a period of years.
Cataracts more common in older adults and can affect your ability to carry out daily activities such as driving.
Cataracts can also affect babies and young children.
- Cataracts are a very common reason people lose vision, but they can be treated. You and your ophthalmologist should discuss your cataract symptoms. Together you can decide whether you are ready for cataract surgery.
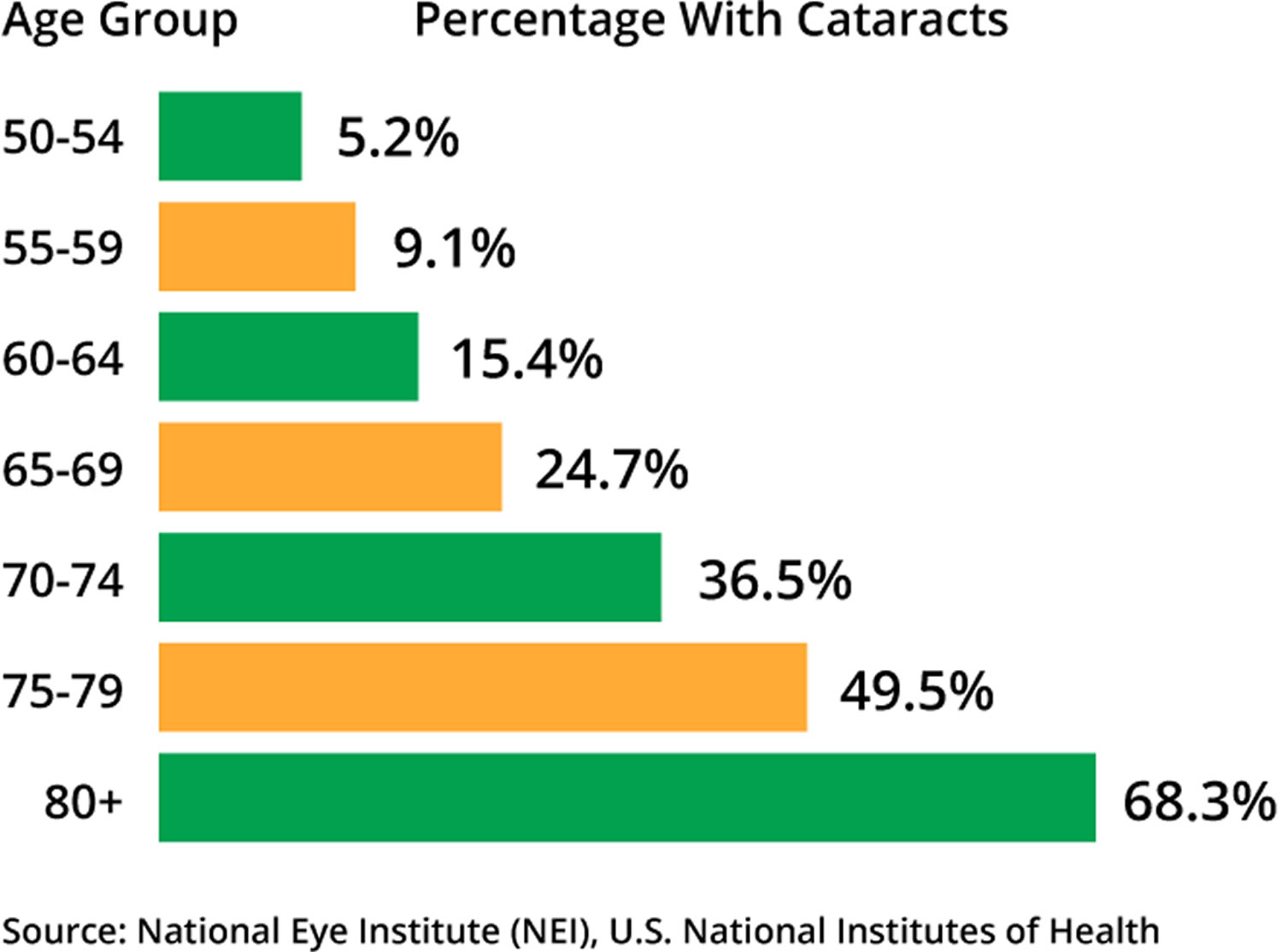
According to the National Eye Institute, 68.3 percent of Americans 80 and older had cataracts in 2010. And the prevalence of cataracts in the U.S. is expected to grow significantly in the years ahead, due in part to the aging of the population. In 2010, roughly 24.4 million Americans had cataracts, and that number is projected to grow to 50.2 million by the year 2050, according to the National Eye Institute.
In adults, a cataract needs to be removed only when vision loss interferes with your everyday activities, such as driving, reading, or watching TV. Sometimes a cataract should be removed even if it does not cause problems with your vision. For example, a cataract should be removed if it prevents examination or treatment of another eye problem, such as age-related macular degeneration (AMD) or diabetic retinopathy.
Talk with your eye care professional about cataract surgery and make sure it’s right for you. Most eye doctors suggest considering cataract surgery when your cataracts begin to affect your quality of life or interfere with your ability to perform normal daily activities, such as reading or driving at night.
It’s up to you and your doctor to decide when cataract surgery is right for you. For most people, there is no rush to remove cataracts because they usually don’t harm the eye. But cataracts can worsen faster in people with diabetes.
Delaying cataract eye surgery generally won’t affect how well your vision recovers if you later decide to have cataract surgery. Take time to consider the benefits and risks of cataract surgery with your doctor.
If you choose not to undergo cataract surgery now, your eye doctor may recommend periodic follow-up exams to see if your cataracts are progressing. How often you’ll see your eye doctor depends on your situation.
How a cataract forms
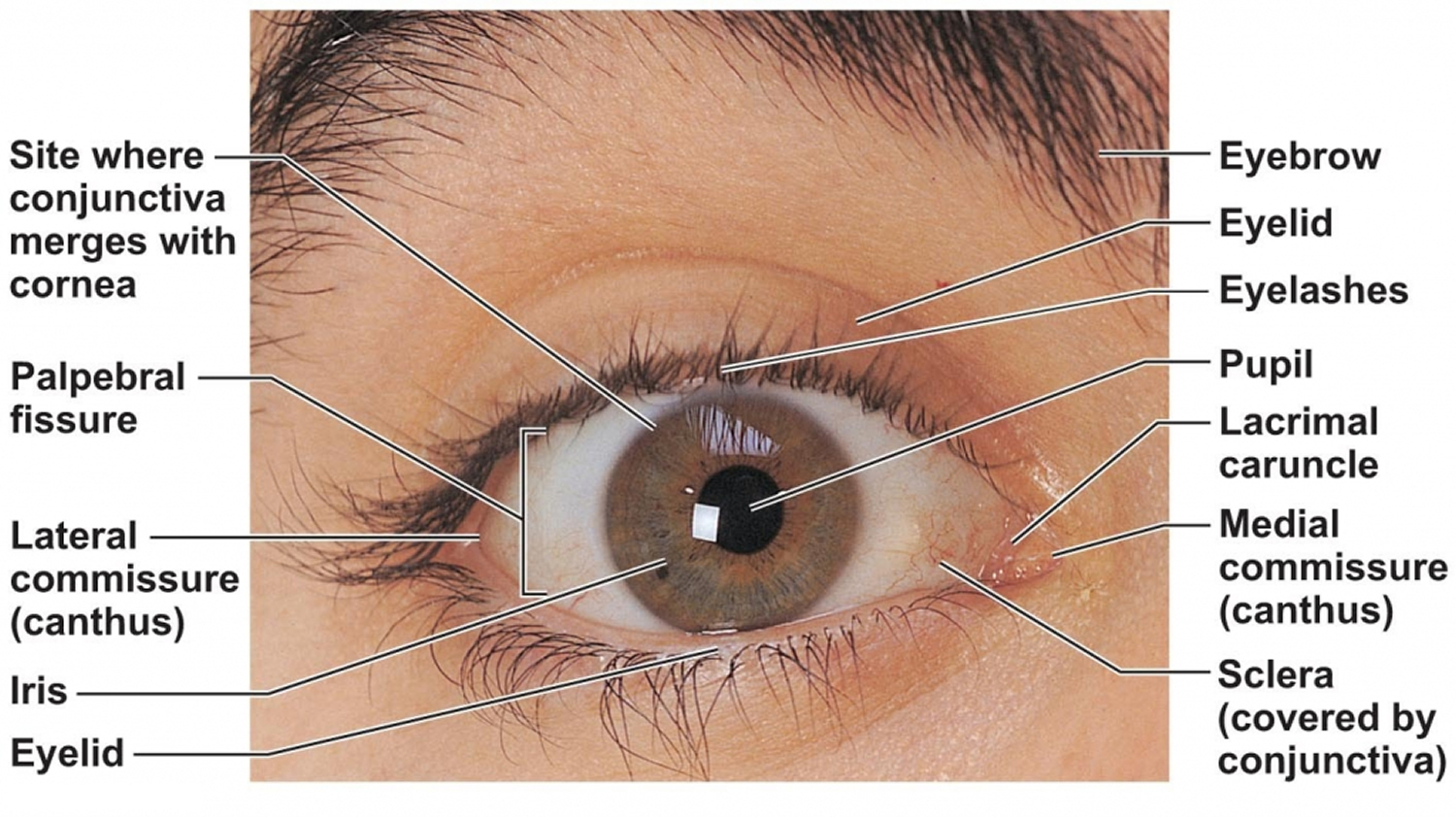
The lens, where cataracts form, is positioned behind the colored part of your eye (iris). The lens focuses light that passes into your eye, producing clear, sharp images on the retina — the light-sensitive membrane in the eye that functions like the film in a camera.
As you age, the lenses in your eyes become less flexible, less transparent and thicker. Age-related and other medical conditions cause tissues within the lens to break down and clump together, clouding small areas within the lens.
As the cataract continues to develop, the clouding becomes denser and involves a bigger part of the lens. A cataract scatters and blocks the light as it passes through the lens, preventing a sharply defined image from reaching your retina. As a result, your vision becomes blurred.
Cataracts generally develop in both eyes, but not evenly. The cataract in one eye may be more advanced than the other, causing a difference in vision between eyes.
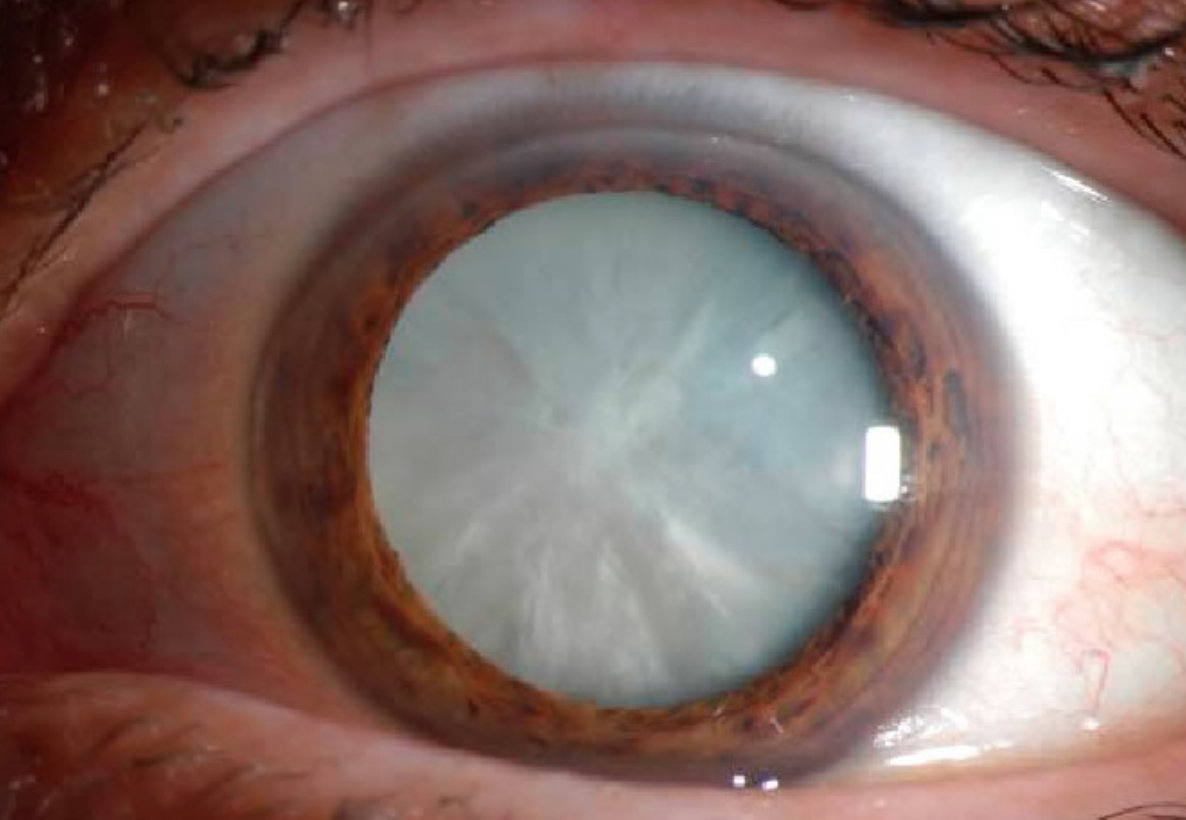
Figure 2. Structure of the human eye
Figure 3. Eye cataract
Types of cataracts
Cataract types include:
- Cataracts affecting the center of the lens (nuclear cataracts). A nuclear cataract may at first cause more nearsightedness or even a temporary improvement in your reading vision. But with time, the lens gradually turns more densely yellow and further clouds your vision.
As the cataract slowly progresses, the lens may even turn brown. Advanced yellowing or browning of the lens can lead to difficulty distinguishing between shades of color.
- Cataracts that affect the edges of the lens (cortical cataracts). A cortical cataract begins as whitish, wedge-shaped opacities or streaks on the outer edge of the lens cortex. As it slowly progresses, the streaks extend to the center and interfere with light passing through the center of the lens.
- Cataracts that affect the back of the lens (posterior subcapsular cataracts). A posterior subcapsular cataract starts as a small, opaque area that usually forms near the back of the lens, right in the path of light. A posterior subcapsular cataract often interferes with your reading vision, reduces your vision in bright light, and causes glare or halos around lights at night. These types of cataracts tend to progress faster than other types do.
- Cataracts you’re born with (congenital cataracts). Some people are born with cataracts or develop them during childhood. These cataracts may be genetic, or associated with an intrauterine infection or trauma. These cataracts also may be due to certain conditions, such as myotonic dystrophy, galactosemia, neurofibromatosis type 2 or rubella. Congenital cataracts don’t always affect vision, but if they do they’re usually removed soon after detection.
There are other types of cataract:
- Secondary cataract. Cataracts can form after surgery for other eye problems, such as glaucoma. Cataracts also can develop in people who have other health problems, such as diabetes. Cataracts are sometimes linked to steroid use.
- Traumatic cataract. Cataracts can develop after an eye injury, sometimes years later.
- Congenital cataract. Some babies are born with cataracts or develop them in childhood, often in both eyes. These cataracts may be so small that they do not affect vision. If they do, the lenses may need to be removed.
- Radiation cataract. Cataracts can develop after exposure to some types of radiation.
What causes cataracts
Though there are other risk factors for cataracts, aging is the most common cause. This is due to normal eye changes that happen after around age 40. That is when normal proteins in the lens start to break down. This is what causes the lens to get cloudy. People over age 60 usually start to have some clouding of their lenses. However, vision problems may not happen until years later.
Most age-related cataracts develop gradually. Other cataracts can develop more quickly, such as those in younger people or those in people with diabetes. Doctors cannot predict how quickly a person’s cataract will develop.
Some inherited genetic disorders that cause other health problems can increase your risk of cataracts. Cataracts can also be caused by other eye conditions, past eye surgery or medical conditions such as diabetes. Long-term use of steroid medications, too, can cause cataracts to develop.
Cataract Risk Factors
Besides aging, other cataract risk factors include:
- having parents, brothers, sisters, or other family members who have cataracts
- having certain medical problems, such as diabetes
- having had an eye injury, eye surgery, or radiation treatments on your upper body
- having spent a lot of time in the sun, especially without sunglasses that protect your eyes from damaging ultraviolet (UV) rays
- smoking
- obesity
- high blood pressure
- previous eye injury or inflammation
- previous eye surgery
- prolonged use of corticosteroid medications
- drinking excessive amounts of alcohol
If you have any of these risk factors for cataract, you should schedule an appointment with your ophthalmologist.
Cataract Prevention
Protecting your eyes from sunlight is the best way to do this. Wear sunglasses that screen out the sun’s ultraviolet (UV) light rays. You may also wear regular eyeglasses that have a clear, anti-UV coating. Ultraviolet light from the sun may contribute to the development of cataracts. Wear sunglasses that block ultraviolet B (UVB) rays when you’re outdoors.Talk with your eye doctor to learn more.
No studies have proved how to prevent cataracts or slow the progression of cataracts. But doctors think several strategies may be helpful, including:
- Have regular eye examinations. Eye examinations can help detect cataracts and other eye problems at their earliest stages. Ask your doctor how often you should have an eye examination.
- Quit smoking. Ask your doctor for suggestions about how to stop smoking. Medications, counseling and other strategies are available to help you.
- Manage other health problems. Follow your treatment plan if you have diabetes or other medical conditions that can increase your risk of cataracts.
- Choose a healthy diet that includes plenty of fruits and vegetables. Adding a variety of colorful fruits and vegetables to your diet ensures that you’re getting many vitamins and nutrients. Fruits and vegetables have many antioxidants, which help maintain the health of your eyes. Studies haven’t proved that antioxidants in pill form can prevent cataracts. But, a large population study recently showed that a healthy diet rich in vitamins and minerals was associated with a reduced risk of developing cataracts. Fruits and vegetables have many proven health benefits and are a safe way to increase the amount of minerals and vitamins in your diet.
- Reduce alcohol use. Excessive alcohol use can increase the risk of cataracts.
Cataract symptoms
Most age-related cataracts develop gradually. As a result, you may not notice signs or changes in your vision right away when cataracts first develop.
At first, the cloudiness in your vision caused by a cataract may affect only a small part of the eye’s lens and you may be unaware of any vision loss. As the cataract grows larger, it clouds more of your lens and distorts the light passing through the lens. This may lead to more noticeable symptoms.
Cataract symptom progression
Here are some vision changes you may notice if you have a cataract:
- Clouded, blurred or dim vision
- Seeing double (when you see two images instead of one)
- Being extra sensitive to light
- Having trouble seeing well at night, or needing more light when you read
- Seeing bright colors as faded or yellow instead
- Increasing difficulty with vision at night
- Sensitivity to light and glare
- Need for brighter light for reading and other activities
- Seeing “halos” around lights
- Frequent changes in eyeglass or contact lens prescription
- Fading or yellowing of colors
- Double vision in a single eye
Cataract diagnosis
Your ophthalmologist will examine and test your eyes to make a cataract diagnosis. This comprehensive eye exam will include dilation. This means eye drops will widen your pupils.
Refraction and Visual acuity test
A visual acuity test uses an eye chart to measure how well you can read a series of letters. Your eyes are tested one at a time, while the other eye is covered. Using a chart or a viewing device with progressively smaller letters, your eye doctor determines if you have 20/20 vision or if your vision shows signs of impairment.
Slit-lamp exam
A slit lamp allows your eye doctor to see the structures at the front of your eye under magnification. The microscope is called a slit lamp because it uses an intense line of light, a slit, to illuminate your cornea, iris, lens, and the space between your iris and cornea. The slit allows your doctor to view these structures in small sections, which makes it easier to detect any tiny abnormalities. Your ophthalmologist will examine your cornea, iris, lens and the other areas at the front of the eye. The special slit-lamp microscope makes it easier to spot abnormalities.
Retinal exam
To prepare for a retinal exam, your eye doctor puts drops in your eyes to open your pupils wide (dilate). When your eye is dilated, the pupils are wide open so the doctor can more clearly see the back of the eye. Using the slit lamp, an ophthalmoscope or both, the doctor looks for signs of cataract. Your ophthalmologist will also look for glaucoma, and examine the retina and optic nerve.
Once I have a cataract diagnosis, what should I do?
- Have an eye exam every year if you’re older than 65, or every two years if younger.
- Protect your eyes from UV light by wearing sunglasses that block at least 99 percent UV and a hat.
- If you smoke, quit. Smoking is a key risk factor for cataracts.
- Use brighter lights for reading and other activities. A magnifying glass may be useful, too.
- Limit driving at night once night vision, halos or glare become problems.
- Take care of any other health problems, especially diabetes.
- Get the right eyeglasses or contact lenses to correct your vision.
- When it becomes difficult to complete your regular activities, consider cataract surgery.
- Make an informed decision about cataract surgery. Have a discussion with your ophthalmologist about:
- the surgery,
- preparation for and recovery after surgery,
- benefits and possible complications of cataract surgery,
- cataract surgery costs,
- other questions you have.
Cataract treatment
If your cataract symptoms are not bothering you very much, you don’t have to remove a cataract. You might just need a new eyeglass prescription to help you see better. You should consider surgery when cataracts keep you from doing things you want or need to do.
When your prescription glasses can’t clear your vision, the only effective treatment for cataracts is surgery.
- Do NOT use eye drops or other treatments that claim to dissolve or remove cataracts. There is no proven way to dissolve cataracts with eye drops. The only way to remove a cataract is with surgery. Your ophthalmologist will recommend removing a cataract when it keeps you from doing things you want or need to do 1.
When to consider cataract surgery
Talk with your eye doctor about whether surgery is right for you. Most eye doctors suggest considering cataract surgery when your cataracts begin to affect your quality of life or interfere with your ability to perform normal daily activities, such as reading or driving at night.
It’s up to you and your doctor to decide when cataract surgery is right for you. For most people, there is no rush to remove cataracts because they usually don’t harm the eye. But cataracts can worsen faster in people with diabetes.
Delaying the procedure generally won’t affect how well your vision recovers if you later decide to have cataract surgery. Take time to consider the benefits and risks of cataract surgery with your doctor.
If you choose not to undergo cataract surgery now, your eye doctor may recommend periodic follow-up exams to see if your cataracts are progressing. How often you’ll see your eye doctor depends on your situation.
What happens during cataract surgery
During cataract surgery, your eye surgeon will remove your eye’s cloudy natural lens. Then he or she will replace it with a clear artificial lens. This new lens is called an intraocular lens (IOL), is positioned in the same place as your natural lens. It remains a permanent part of your eye. When you decide to have cataract surgery, your doctor will talk with you about IOLs and how they work.
An intraocular lens (IOL) is a tiny, artificial lens for the eye. It replaces the eye’s natural lens that is removed during cataract surgery.
Intraocular lenses (IOLs) come in different focusing powers, just like prescription eyeglasses or contact lenses. Your ophthalmologist will measure the length of your eye and the curve of your cornea. These measurements are used to set your IOLs focusing power.
What are IOLs made of?
Most intraocular lenses (IOLs) are made of silicone or acrylic. They are also coated with a special material to help protect your eyes from the sun’s harmful ultraviolet (UV) rays.
Monofocal IOLs
The most common type of lens used with cataract surgery is called a monofocal IOL. It has one focusing distance. It is set to focus for up close, medium range or distance vision. Most people have them set for clear distance vision. Then they wear eyeglasses for reading or close work.
Multifocal IOLs
Some IOLs have different focusing powers within the same lens. These are called multifocal and accommodative lenses. These IOLs reduce your dependence on glasses by giving you clear vision for more than one set distance.
These IOLs provide both distance and near focus at the same time. The lens has different zones set at different powers. It is designed so that your brain learns to select the right focus automatically.
Accommodative IOLs
These lens move or change shape inside your eye, allowing focusing at different distances.
Toric IOLs
For people with astigmatism, there is an IOL called a toric lens. Astigmatism is a refractive error caused by an uneven curve in your cornea or lens. The toric lens is designed to correct that refractive error.
As you plan for your cataract surgery, talk to your ophthalmologist about your vision needs and expectations. He or she will explain IOL options for you in more detail.
However, for some people, other eye problems prohibit the use of an artificial lens. In these situations, once the cataract is removed, vision may be corrected with eyeglasses or contact lenses.
Cataract surgery is generally done on an outpatient basis, which means you won’t need to stay in a hospital after the surgery. During cataract surgery, your eye doctor uses local anesthetic to numb the area around your eye, but you usually stay awake during the procedure.
If you need cataract surgery in both eyes, your doctor will schedule surgery to remove the cataract in the second eye after you’ve healed from the first surgery.
What to expect with cataract surgery
Before surgery:
Your ophthalmologist will measure your eye to set the proper focusing power for your intraocular lens (IOL). Also, you will be asked about any medicines you take. You might be asked not to take some of these medicines before surgery.
You may be prescribed eyedrop medicines to start before surgery. These medicines help prevent infection and reduce swelling during and after surgery.
The day of surgery:
Your ophthalmologist may ask you not to eat any solid food at least 6 hours before your surgery.
Cataract removal surgery may be done in an outpatient surgery center or in a hospital. Here is what will happen:
- Your eye will be numbed with eye drops or with an injection around the eye. You may also be given a medicine to help you relax.
- You will be awake during surgery. You may see light and movement during the procedure, but you will not see what the doctor is doing to your eye.
- Your surgeon will enter into the eye through tiny incisions (cuts, created by laser or a blade) near the edge of your cornea (the clear covering on the front of your eye). The surgeon uses these incisions to reach the lens in your eye. Using very small instruments, he or she will break up the lens with the cataract and remove it. Then your new lens is inserted into place.
- Usually your surgeon will not need to stitch the incisions closed. These “self sealing” incisions eventually will close by themselves over time. A shield will be placed over your eye to protect it while you heal from surgery.
- You will rest in a recovery area for about 15–30 minutes. Then you will be ready to go home.
Cataract surgery complications
Cataract surgery is generally safe, but it carries a risk of infection and bleeding. Cataract surgery increases the risk of retinal detachment.
Like any surgery, cataract surgery carries risks of problems or complications. Here are some of those risks:
- Eye infection.
- Bleeding in the eye.
- Ongoing swelling of the front of the eye or inside of the eye.
- Swelling of the retina (the nerve layer at the back of your eye).
- Detached retina (when the retina lifts up from the back of the eye).
- Damage to other parts of your eye.
- Pain that does not get better with over-the-counter medicine.
- Vision loss.
- The intraocular lens (IOL) implant may become dislocated, moving out of position.
Your ophthalmologist will talk with you about the risks and benefits of cataract surgery.
Cataract surgery recovery time
- After the procedure, you’ll have some discomfort for a few days.
- Healing generally occurs within eight weeks.
Days or weeks after surgery:
- You will have to use eye drops after surgery. Be sure to follow your doctor’s directions for using these drops.
- Avoid getting soap or water directly in the eye.
- Do not rub or press on your eye. Your ophthalmologist may ask you to wear eyeglasses or a shield to protect your eye.
- You will need to wear a protective eye shield when you sleep.
- Your ophthalmologist will talk with you about how active you can be soon after surgery. He or she will tell you when you can safely exercise, drive or do other activities again.
Posterior capsular opacification
Your vision could become cloudy or blurry weeks, months or years after cataract surgery. This is not unusual. Your doctor might call this a “posterior capsular opacification (PCO).” It’s also called “secondary cataract” or “scar tissue.” It’s not like a scar you get on your skin. But because it happens after the eye has healed from cataract surgery, some people think of it as a scar. It happens when a membrane called the posterior capsule becomes cloudy. It might help to think of the posterior capsule as a transparent pocket. It holds your intraocular lens (IOL) in place. It also once held your eye’s natural lens (what became the cataract) in place. If you notice cloudy vision again, you might need to have a laser procedure. The laser creates an opening in the cloudy capsule and is called a posterior capsulotomy (or a YAG laser capsulotomy). This procedure helps restore clear vision.
Cataract surgery cost
Cataract surgery costs are generally covered by Medicare if you are Medicare eligible. Private insurance usually covers cataract surgery as well.
Medicare will cover your costs if your vision tests at a certain level of acuity or clarity. Private insurance plans may have similar vision requirements. If your surgery is covered you may still have some costs. Special types of IOLs will cost more. Choosing to have cataract surgery before your vision has deteriorated enough will cost more.
In certain cases, it might be possible to get coverage before you meet the age or vision requirements. Talk with your ophthalmologist if you are considering having early cataract surgery.
What do you do if you don’t have Medicare or private insurance coverage? You may still be able to reduce and manage the cost of cataract surgery. Ask about payment plans through your doctor’s office. See if your employer offers flexible spending accounts that can help. Your ophthalmologist can help you learn more about costs of cataract surgery. Discuss your options for affording the procedure.
Cataract Surgery vs. Laser-Assisted Cataract Surgery
Are you planning to have cataract surgery? If so, you may be offered a choice of two surgical options: traditional cataract surgery or laser-assisted cataract surgery.
Traditional cataract surgery is one of the most common surgeries in the world. It is recognized as being safe and effective. Laser cataract surgery, which is not covered by most insurance plans, costs more than traditional cataract surgery and may provide some advantages in terms of precision and consistency—in the proper situation. So how do you decide which type of cataract surgery to have?
Here are some things you should understand about both kinds of cataract surgery. Talk with your ophthalmologist (and get another ophthalmologist’s opinion as well, if you prefer) to determine the best type of surgery for you.
Traditional cataract surgery
With traditional cataract surgery, called phacoemulsification, the eye surgeon creates a small incision in the side of the cornea by hand with a scalpel blade. An instrument is inserted through this incision into the area behind the pupil where the eye’s lens sits in a capsule or bag. The surgeon uses the microsurgical instrument to create a circular opening in the lens capsule. Then a special pen-shaped probe is inserted through that opening to apply sound waves (ultrasound) to break up the cloudy center of the lens. Then the broken-up pieces of lens are suctioned out of the eye. An artificial intraocular lens (IOL) is implanted to replace the cloudy natural lens. The side walls of the corneal incision will be filled with a special liquid and self-seal after surgery, so most commonly stitches are not needed.
Laser-assisted cataract surgery
With laser-assisted cataract surgery, a camera/ultrasound imaging device is placed over your eye to map its surface and gather information about the lens. The device sends detailed information to a computer that programs the laser for the exact location, size and depth of the incisions. The surgeon uses the laser to make the corneal incision and the opening in the lens capsule. Energy from the laser may also be used to soften the cataract. Then the ultrasound probe used in traditional cataract surgery is used to break the lens into pieces and suction them out of the eye. The IOL is implanted. As with traditional cataract surgery, the corneal incision usually does not require stitches.
Who can be offered laser-assisted cataract surgery?
Under today’s Medicare guidelines, only certain patients may be offered laser-assisted cataract surgery.
Specifically, your ophthalmologist can offer it if you have astigmatism diagnosed during your cataract consultation and would like to have that refractive error corrected during cataract surgery. In this situation, the laser is used to create specific incisions in the cornea to reshape it, treating the astigmatism.
You may also be offered laser cataract surgery if you choose to have a premium lens implanted, such as an astigmatism-correcting toric IOL or a multifocal IOL. Ophthalmologists who use laser cataract removal technology explain that it allows them to see and map the lens capsule better and place the opening in the capsule more precisely, allowing for better centering of the IOL.
Can you choose to have laser-assisted cataract surgery if you don’t have either of the conditions above?
Current Medicare guidelines say that a surgeon may not offer and charge for the laser-assisted cataract surgery unless one of the two conditions above is met.
Which type of cataract surgery has a shorter recovery time?
The recovery period for both laser-assisted cataract surgery and traditional cataract surgery is the same. Some people can see clearly almost immediately, while others may find their vision clears within about a week or two. Remember that it takes about 3 months to fully recover from cataract surgery.
What benefits does laser cataract surgery offer that traditional cataract surgery does not?
Using a laser to do cataract surgery allows the surgeon to make very precise incisions in less time. It can improve accuracy and consistency in the surgical steps. And in some cases, laser-assisted cataract surgery can provide a higher degree of correction for a refractive error, such as astigmatism, than traditional cataract surgery.
However, it is important to be aware that studies have not shown that laser-assisted cataract surgery results in fewer complications or better visual outcomes than traditional cataract surgery. With any type of cataract surgery, your outcome depends in large part on the skill and experience of your eye surgeon.
What do you want from cataract surgery?
For some people, simply replacing a cloudy lens with a clear implant and wearing glasses for some activities is perfect. For others, achieving the best possible vision without glasses after cataract surgery is the goal. Your vision needs and expectations can help you and your ophthalmologist decide the best surgical option for you.
Lifestyle and home remedies
To deal with symptoms of cataracts until you decide to have surgery, try to:
- Make sure your eyeglasses or contact lenses are the most accurate prescription possible
- Use a magnifying glass to read if you need additional help reading
- Improve the lighting in your home with more or brighter lamps
- When you go outside during the day, wear sunglasses or a broad-brimmed hat to reduce glare
- Limit your night driving
Self-care measures may help for a while, but as the cataract progresses, your vision may deteriorate further. When vision loss starts to interfere with your everyday activities, consider cataract surgery.
Congenital cataracts
Many people think cataracts only happen to older people, but children can get cataracts too. Both pediatric cataracts and cataracts from aging are a clouding in the lens of the eye that can cause blurry vision or blindness.
- Pediatric cataracts that affect vision that aren’t quickly treated can sometimes cause irreversible damage to eyesight, including a permanently lazy eye and even blindness in severe cases.
In adults, cataracts occur after the eyes and vision are developed and stable. Most adults can have good vision again after the cataracts are removed. Because children’s eyes are still developing until they’re 8 or 10 years old, untreated cataracts can have serious long-term effects on their vision. But early detection and prompt treatment can prevent permanent vision loss in children with cataracts.
Types of Pediatric Cataracts
- Pediatric cataracts can be congenital (present at birth) or acquired (develop after birth).
- They can occur in one eye (unilateral) or both eyes (bi-lateral).
- Bi-lateral cataracts can be asymmetric (one cataract is more severe than the other).
- Cataracts may appear in different parts of the lens and range in size from tiny dots to dense clouds.
Causes of Pediatric Cataracts
There are a number of reasons why a child may be born with cataracts or develop them while they’re still young. However, in many cases it isn’t possible to determine the exact cause.
Possible causes of pediatric cataracts include:
- a genetic fault inherited from the child’s parents that caused the lens to develop abnormally
- certain genetic conditions, including Down’s syndrome
- certain infections picked up by the mother during pregnancy, including rubella and chickenpox
- an injury to the eye after birth
Genes and genetic conditions
Cataracts present from birth (congenital cataracts) are sometimes caused by a faulty gene being passed to a child from their parents. This fault means that the lens doesn’t develop properly.
It’s estimated that there’s a family history of congenital cataracts in around one in every five cases of the condition, and recent research suggests genetic causes are responsible for the majority of bilateral congenital cataracts in the US.
Cataracts can also be associated with conditions caused by chromosome abnormalities, such as Down’s syndrome. Chromosomes are the parts of the body’s cells that carry the genes.
Infections during pregnancy
Congenital cataracts can also be caused by infections caught by the mother during pregnancy. The main infections linked to an increased risk of congenital cataracts include:
- rubella (German measles) – a viral infection that can cause a red-pink spotty skin rash
- toxoplasmosis – a parasitic infection caught by consuming food, water or soil contaminated with infected cat’s faeces
- cytomegalovirus (CMV) – a common virus that can cause flu-like symptoms
- chickenpox – a mild but highly infectious condition caused by the varicella-zoster virus
- herpes simplex virus – a virus that often causes cold sores
Causes of acquired cataracts
Cataracts that develop in children after they’re born are known as acquired, infantile or juvenile cataracts.
Causes of this type of cataracts can include:
- galactosaemia – where the sugar galactose (which mainly comes from lactose, the sugar in milk) can’t be broken down by the body
- diabetes – a lifelong condition that causes a person’s blood sugar level to become too high
- eye trauma – as a result of an injury to the eye or eye surgery
- toxocariasis – a rare parasitic infection that can sometimes infect the eyes, spread from animals to humans via their infected faeces
However, most of these problems are either rare or don’t usually cause cataracts to develop in children.
Symptoms of cataracts in children
In children, cataracts can affect one or both eyes. Symptoms of childhood cataracts can vary depending on how cloudy the lens is, where the cloudiness is in the lens, and whether one or both eyes are affected.
Cloudy patches in the lens can sometimes get bigger and more can develop, resulting in the child’s vision becoming increasingly affected.
As well as poor vision, cataracts can also cause “wobbling eyes” and a squint (where the eyes point in different directions).
When your child is very young, it can be difficult to spot signs of cataracts. However, your baby’s eyes will be routinely examined within 72 hours of birth and again when they’re six to eight weeks old. Sometimes, cataracts can develop in children after these screening tests.
Sometimes, cataracts can develop in children after these screening tests.
Signs that your child may have developed cataracts can include:
- poor vision – you may notice your child has difficulty recognizing and following objects or people with their eyes
- rapid uncontrolled eye movements or “wobbling” eyes – known as nystagmus
- the eyes pointing in different directions – known as a squint
- a white or grey pupil – this can also be a sign of other serious conditions, such as retinoblastoma, and should be checked by a doctor immediately
Your child may also find it difficult to see clearly in bright light or if there’s any glare.
- It’s particularly important to spot cataracts in children quickly because early treatment can reduce the risk of long-term vision problems. Therefore, you should visit your doctor or tell your health visitor if you have any concerns about your child’s eyesight.
Early Detection and Swift Treatment
It’s important childhood cataracts are diagnosed as early as possible because early treatment can significantly reduce the risk of long-term vision problems.
- An eye’s lens must be clear to focus the images it sees onto the retina, which then transmits the images to the brain. A cataract can prevent light from reaching the retina or cause light rays to scatter as they pass through the cloudiness. This distorts the retinal image.
- For children, whose eyes and brain are still learning to see, distortion can lead to lazy eye (amblyopia). Without proper treatment, pediatric cataracts can cause abnormal connections between the brain and the eye. Once made, these connections are irreversible.
- Most pediatric cataracts are detected when the child is examined at birth, before they even leave the hospital. Many more are detected by pediatricians at well-baby exams and some are noticed by parents. They are often noticed as a missing or irregular red reflex test on pediatric screening exams.
- Acquired cataracts are most often diagnosed at vision screenings by the pediatrician or after an eye injury.
Newborn screening
All parents are offered a physical examination for their baby within 72 hours of birth and again when their baby is six to eight weeks old.
Childhood cataracts are among the conditions screened for during the newborn physical examination.
Your baby’s eyes are checked by looking at their general appearance and how they move. If your baby’s eye looks cloudy, it could be a sign they have cataracts.
An important part of the check is looking for the “red reflex” using a bright light. The red reflex is a reflection from the back of the eye that’s similar to the red eye effect sometimes seen in flash photography. If no red reflex, or a weak one, is seen, it may mean there’s cloudiness in the lens.
Vision tests for older babies and children
Although cataracts can be present from birth (congenital), they sometimes don’t develop until a child is older. Visit your GP or tell your health visitor if you have any concerns about your child’s eyesight at any stage.
You should also make sure your child has routine eye tests to check for any problems with their vision. All children under the age of 16 are entitled to free sight tests, which they should have about every two years.
When will my child’s eyes be checked?
Your child’s eyes may be checked:
- within 72 hours of birth – this is known as the newborn physical examination and it can be used to check for obvious physical problems
- between six and eight weeks old – this is a follow-up physical examination to check for any obvious problems that weren’t detected soon after birth
- at around one year old or between two and two-and-a-half years old – you may be asked whether you have any concerns about your child’s eyesight as part of a review of your child’s health and development; eye tests can be arranged, if necessary
- at around four or five years old – some children will have an eye test when they start school, although this varies, depending on where you live
It’s also recommended that children have regular eye tests at least once every two years. These tests can be done at a high street opticians and are free for all children under 16 years old (and those under 19 years old in full-time education).
Speak to your doctor or health visitor if you have any concerns about your child’s vision at any stage.
What eye tests may be carried out?
A number of tests may be carried out to check for vision or eye problems in babies and children. Some of these are described below.
The red reflex test
The red reflex test is usually carried out alongside a general examination of your baby’s eyes, as part of newborn checks. It involves using an instrument called an ophthalmoscope, which magnifies the eyes and produces a light that allows the eyes to be examined clearly.
When light is shone into your baby’s eyes, a red reflection should be seen as it’s reflected back. If a white reflection is seen, it could be a sign of an eye problem.
The pupil reflex test
The pupil reflex test involves shining a light into each of your baby’s eyes to check how their pupils (black dots at the centre of the eyes) react to light.
Your baby’s pupils should automatically shrink in response to the light. If they don’t, it could be a sign of a problem with their eyes.
Attention to visual objects
This is a simple test to check whether a newborn baby pays attention to visual objects. A midwife or doctor will try to catch your baby’s attention with an interesting object. They then move it to see if the child’s eyes follow.
These sorts of tests can also be used to check the eyesight of older babies and young children who are not yet able to speak. If your child can speak, but is not yet able to recognise letters, pictures may be used instead of objects.
Snellen and LogMAR charts
When your child can recognise or match letters, their vision is tested using charts that have rows of letters and numbers of decreasing sizes. Your child will be asked to read out or match the letters they can see from a specific distance. These charts are called Snellen or LogMAR charts.
For younger children, a similar test using pictures or symbols may be carried out instead.
Range of movement tests
To test the range of movement of each eye, a child’s attention will be drawn to an interesting object, which is then moved to eight different positions: up, down, left, right, and halfway between each of these points. This tests how well the eye muscles work.
Refraction test
A refraction test is carried out by an ophthalmologist or an eye specialist and is used to determine if your child needs glasses and what prescription they need.
Before the test, your child may be given special eye drops that widen their pupils, so the back of their eyes can be examined more clearly. Your child will be asked to look at a light, or read letters on a chart if they’re old enough, while different lenses are placed in front of their eyes.
Color vision deficiency test
Color vision deficiency tests, also known as color blindness tests, are usually carried out in older children if a problem is suspected.
One of the tests used to check for color blindness is the Ishihara test. This involves looking at images that are made up of dots in two different colors. If a child’s color vision is normal, they’ll be able to recognize a letter or number within the image.
A child who can’t tell the difference between two colors won’t be able to see the number or letter, which means they may have a color vision problem.
Treatment Takes a Long-Term Strategy
Whether or not your child needs cataract surgery will largely depend on whether their vision is affected – depending on the type and severity.
If cataracts aren’t causing any problems, immediate treatment may not be necessary. Instead, your child may only need regular check-ups to monitor their vision. But the vast majority of children need surgery to remove the cataracts. Unlike adults with full-sized eyes, children require specialized surgical instrumentation and techniques. When performed by an experienced surgeon, cataract removal is generally safe. The most common risks include glaucoma, retinal detachment, infection and the need for more surgeries.
For most children, surgery is just the first step to rehabilitate the eyes. Ongoing treatment must repair eye-brain connections. This involves teaching the eyes how to focus properly.
After surgery, children often need some combination of contact lenses, intraocular lenses implanted in the eye or glasses. If amblyopia has developed, the child may need patching. This treatment involves covering the stronger eye to stimulate vision in the weaker eye.
Children who receive timely treatment and follow-up have a good prognosis. Successful outcomes may require years of individualized visual rehabilitation.
However, as childhood cataracts are rare, it’s difficult to predict how much a child’s vision will be improved by treatment. Many children are likely to have reduced vision in the affected eye (or eyes) even with treatment, although most will be able to go to mainstream schools and go on to live full lives.
Cataract surgery
Cataract surgery for babies and children will take place in hospital under general anesthetic, which means your child will be unconscious during the operation.
The operation, which usually takes between one and two hours, will be carried out by an ophthalmologist (a doctor specializing in the treatment of eye conditions).
If the cataracts are present from birth, the operation will be carried out as soon as possible, usually one to two months after your baby is born.
Before the operation, the ophthalmologist will apply drops to the eye to dilate (widen) the pupil. A very small cut is made in the surface (cornea) at the front of the eye, and the cloudy lens is removed.
In some cases, a clear plastic lens called an intraocular lens (IOL) or intraocular implant will be inserted during the operation to replace the lens that’s removed. This is because the eye can’t focus without a lens.
However, it’s more common in babies and young children for external contact lenses or glasses (if both eyes are affected) to be used to compensate for the removal of the lens. These will be fitted a week or two after the operation.
Most ophthalmologists recommend using contact lenses or glasses in children under 12 months old at the time of surgery. This is because there’s a higher risk of complications and further surgery being needed in babies who have an IOL inserted.
When the operation is complete, the incision in your child’s eye will usually be closed with stitches that gradually dissolve.
After the operation
After the operation, a pad or transparent shield will be placed over your child’s eye to protect it. Most children will need to stay in hospital overnight so their recovery can be monitored.
If your child has cataracts in both eyes (bilateral cataracts), the ophthalmologist will usually operate on each eye separately to reduce the risk of complications affecting both eyes. You and your child will be able to go home between operations. The second operation will usually take place within a week of the first.
You’ll be given eye drops to give to your child at home. These help reduce inflammation (swelling and redness) in the eye. You’ll need to put them into your child’s eye every two to four hours – you’ll be shown how to do this before you leave hospital.
Complications of Cataract surgery
Cataract surgery is usually very successful, but some children may experience complications and need further treatment.
Even if a child’s cataracts are successfully removed during surgery, their vision may still be affected by other eye conditions.
For example, lazy eye can occur if there’s weaker vision in one eye. The brain ignores the visual signals coming from the weaker eye, which leads to the vision in the affected eye not developing properly.
Lazy eye will need further treatment, usually wearing a patch over the stronger eye, although it may not always be possible to fully correct the problem.
Cloudy vision
If your child has an artificial lens fitted during cataract surgery, the main risk is a condition called posterior capsule opacification (PCO). This is where part of the lens capsule (the “pocket” that the lens sits inside) thickens and causes cloudy vision. This isn’t the cataract returning, but is caused by cells growing over the artificial lens.
Posterior capsule opacification is common after cataract surgery where an artificial lens is implanted, and it usually develops within four to 12 months of having the operation.
If your child develops posterior capsule opacification, they may need another operation to correct it. Laser eye surgery, where energy beams cut through part of the eye, may be used. During the procedure, the cloudy part of the lens capsule will be removed, with enough left to continue holding the artificial lens in place.
The procedure should only take around 15 minutes, and vision should be improved immediately or within a few days. As no surgical incisions or stitches are necessary, your child can usually return to their normal activities straight away.
Other complications
Other complications that can occur after an operation to remove childhood cataracts include:
- glaucoma – where vision is affected by increased pressure inside the eye; without successful treatment, glaucoma can cause irreversible damage to key structures in the eye and blindness; glaucoma is a lifelong risk for children who have cataract surgery, so these children will need their eye pressure measured at least once a year by an optician for the rest of their lives
- squint – where the eyes look in different directions
- abnormalities affecting the pupil, such as it becoming a more oval shape – this is common and doesn’t usually affect vision
- retinal detachment – where vision is affected by the retina (the layer of light-sensitive cells that line the back of the eye) becoming separated from the inner wall of the eye
- cystoid macular oedema – where fluid builds up between layers of the retina, sometimes affecting vision
- infection – such as endophthalmitis (a rare bacterial infection)
In many cases, medication or further surgery will be required to treat these problems if they develop.
If your child has any signs of pain, bleeding, or a lot of stickiness or redness in or around their eye after surgery, you should immediately contact the hospital where the operation was carried out.
Further treatment
Most children will need to wear glasses or contact lenses after having cataract surgery. This is because the vision in the treated eye or eyes will be blurred, as they’re no longer able to focus properly on their own. Replacing the focusing power of the cataract lens is as important as the surgery to remove it.
Glasses or contact lenses will also usually be needed if an artificial lens has been fitted, to allow your child to focus on closer objects. This is because artificial lenses can usually only focus on distant objects.
The glasses or contact lenses will often be fitted a few weeks after the operation, usually by an eye specialist called an optometrist. They’ll advise you about how often contact lenses should be replaced (usually every day) and teach you how to do this.
Your child will continue to have regular check-ups after surgery so that their vision can be monitored. As your child’s vision develops with age, the strength of their contact lenses or glasses can be adjusted.
Wearing a patch
For almost all cases of unilateral cataract (where one eye is affected), and if a child with bilateral cataracts has weaker vision in one eye, the optometrist may recommend they wear a temporary patch over their stronger eye. This is known as occlusion therapy.
Occlusion therapy aims to improve vision in the weaker eye by forcing the brain to recognise the visual signals from that eye that it may have been ignoring previously. Without treatment, most children with unilateral cataract won’t be able to develop good vision in their operated eye.
Orthoptists are hospital based specialists who are often described as “physiotherapists for the eye”. They assess visual function. Your orthoptist will tell you when your child should wear the patch and how long they may need it for.
This will depend on the type of cataract your child had, and how weak their vision is. Wearing a patch can be an unpleasant experience for your child, and they’ll need lots of encouragement to keep it on.
- Cataract Diagnosis and Treatment. https://www.aao.org/eye-health/diseases/cataracts-treatment[↩]