Contents
What is conversion disorder
Conversion disorder is a mental condition in which a person has blindness, paralysis, or other nervous system (neurologic) symptoms that cannot be explained by medical evaluation, neurological or general medical condition 1. Conversion disorder is also called functional neurological symptom disorder or hysterical neurosis 2. Psychological factors, such as conflicts or stress, are judged to be associated with the deficits 3. The term conversion disorder was coined by Sigmund Freud, who hypothesized that the occurrence of certain symptoms not explained by organic diseases reflect unconscious conflict 3. The word conversion refers to the substitution of a somatic symptom for a repressed idea 4.
Common examples of conversion symptoms include blindness, paralysis, dystonia, psychogenic nonepileptic seizures, anesthesia, swallowing difficulties, motor tics, difficulty walking, hallucinations, anesthesia, and dementia 5. In patients with conversion disorder, these symptoms are not caused directly by a physiological effect; rather these symptoms are caused by a psychological conflict. Patients diagnosed with conversion disorder are not feigning the signs and symptoms. Despite the lack of a definitive organic diagnosis, the patient’s distress is very real and the physical symptoms the patient is experiencing cannot be controlled at will (i.e., the patient is not malingering an illness).
Patients who convert their emotional problems into physical symptoms spend nine times the cost for healthcare as people who do not, and 82 percent of adults with conversion disorder stop working because of their symptoms 6. The annual bill for conversion disorder in the United States is $20 billion, not counting absenteeism from work and disability payments 6. Despite its clinical importance, there has been only marginal progress in our understanding of conversion disorder relative to many other neurological and psychiatric disorders 7.
The reported incidence of conversion symptoms varies widely depending on the population studied. Studies have estimated that 20 to 25 percent of patients in a general hospital setting have individual symptoms of conversion, and five percent of patients in this setting meet the criteria for the full disorder 8. Medically unexplained neurological symptoms account for approximately 30 percent of referred neurology outpatients 9. In a study of 100 randomly selected patients from a psychiatry clinic, 24 were noted to have unexplained neurological symptoms 9.
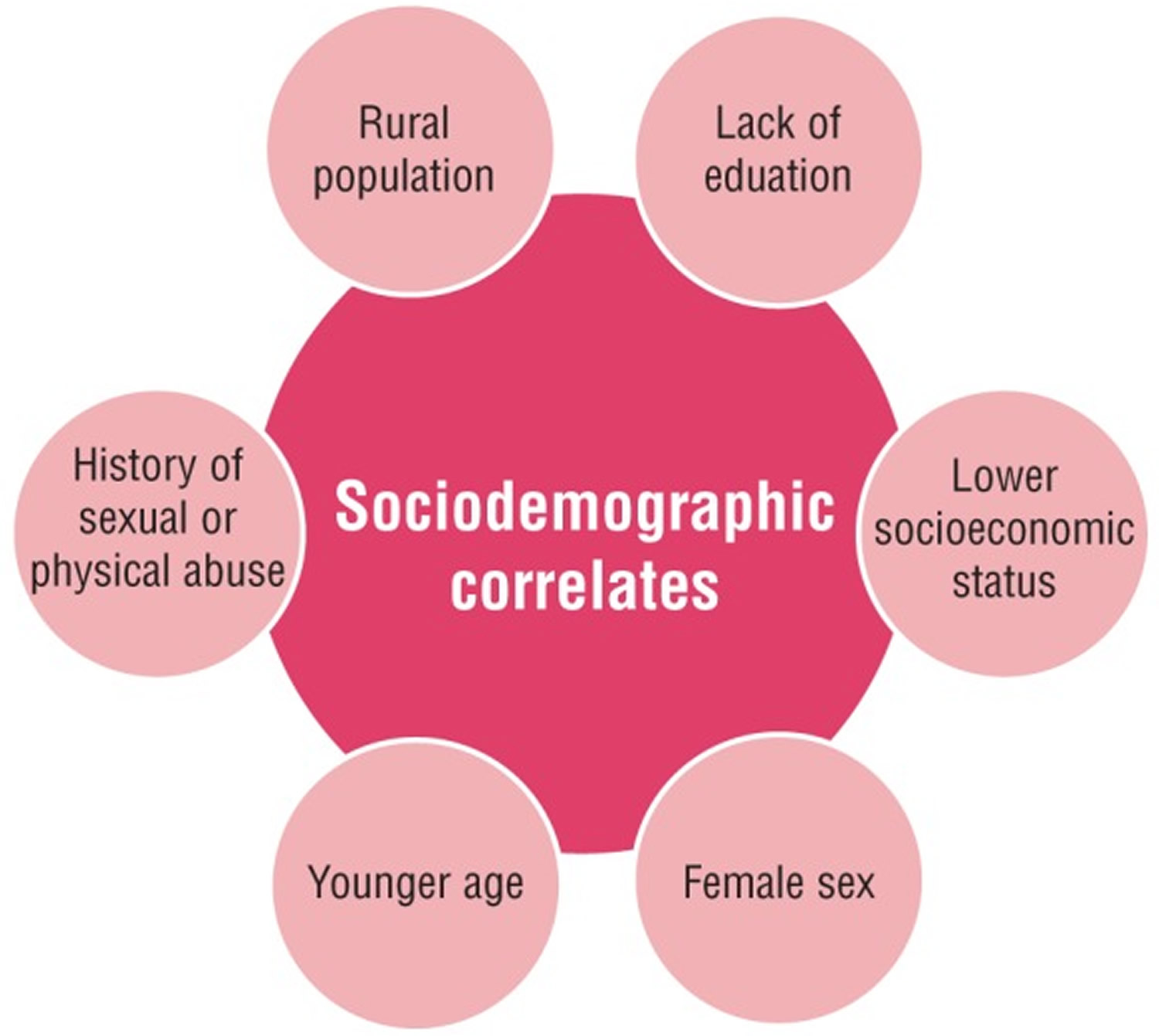
Among adults, women diagnosed with conversion disorder outnumber men by a 2:1 to 10:1 ratio; less educated people and those of lower socioeconomic status are more likely to develop conversion disorder; race by itself does not appear to be a factor 6. There is a major difference between the populations of developing/third world countries compared to developed countries; in developing countries, the prevalence of conversion disorder may run as high as 31 percent 6. Figure 1 illustrates the sociodemographic factors common in conversion disorder.
Figure 1. Sociodemographic factors of conversion disorder
[Source 10]Conversion disorder DSM 5
Conversion disorder diagnostic criteria (DSM-5) 2
- A. One or more symptoms of altered voluntary motor or sensory function.
- B. Clinical findings provide evidence of incompatibility between the symptom and recognized neurological or medical conditions.
- C. The symptom or deficit is not better explained by another medical or mental disorder.
- D. The symptom or deficit causes clinically significant distress or impairment in social, occupational or other important areas of functioning or warrants medical evaluation.
Symptom type:
- With weakness or paralysis
- With abnormal movement (e.g., tremor, dystonic movement, myoclonus, gait disorder)
- With swallowing symptoms
- With speech symptom (e.g., dysphonia, slurred speech)
- With attacks or seizures
- With anesthesia or sensory loss
- With special sensory symptom (e.g., visual , olfactory, or hearing disturbance)
- With mixed symptoms
Conversion disorder outlook (prognosis)
Symptoms usually last for days to weeks and may suddenly go away. Usually the symptom itself is not life threatening, but complications can be debilitating.
A good prognosis can be expected in patients where conversion disorder had a sudden onset, a short duration, an early identifiable stressor, no ongoing litigation, good premorbid functioning, and lack of comorbid psychiatric disorders 3.
Conversion disorder causes
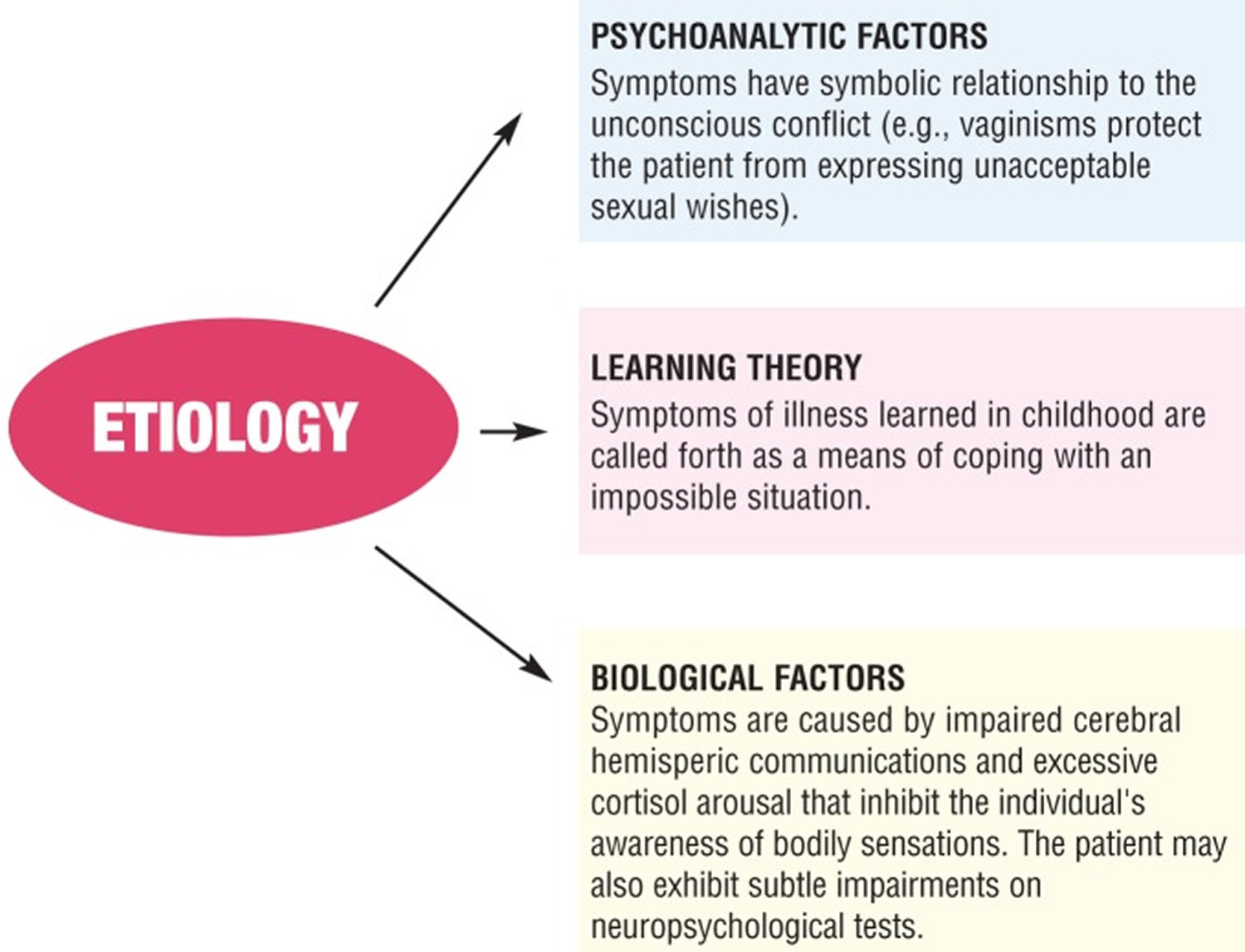
Conversion disorder symptoms may occur because of a psychological conflict or recent stressors and its symptoms manifest as a result of unconscious conflict between a forbidden wish of the patient and his or her conscience. The conversion symptoms symbolically represent a partial wish fulfillment without the individual’s full awareness of the unacceptable desire (e.g., vaginismus with sexual desire, syncope with arousal, paralysis with anger) 3. Conversion disorder has been attributed to both nonbiological and biological factors (Figure 1) 11.
Figure 2. Factors that can contribute to or cause conversion disorder
Symptoms usually begin suddenly after a stressful experience. People are at risk of conversion disorder if they also have:
- A medical illness
- A dissociative disorder (escape from reality that is not on purpose)
- A personality disorder (inability to manage feelings and behaviors that are expected in certain social situations)
People who have conversion disorder are not making up their symptoms (malingering). Some health care providers falsely believe that this disorder is not a real condition and may tell people that the problem is all in their head. But this condition is real. It causes distress and cannot be turned on and off at will.
The physical symptoms are thought to be an attempt to resolve the conflict the person feels inside. For example, a woman who believes it is not acceptable to have violent feelings may suddenly feel numbness in her arms after becoming so angry that she wanted to hit someone. Instead of allowing herself to have violent thoughts about hitting someone, she experiences the physical symptom of numbness in her arms.
Neural correlates of conversion disorder
The growing trend to measure structural and functional changes in the brain through imaging has contributed significantly to improving understanding of the neural mechanisms of many psychiatric conditions, including conversion disorder 12. Functional imaging findings suggest the involvement of prefrontal cortex as a candidate region in conversion disorder 13.
Marshall et al 14 performed positron emission tomography (PET) on a woman with chronic left-sided paralysis (without sensory loss) in whom no organic lesion could be found. Regional cerebral blood flow was measured when she tried to move either her paralyzed leg or her other leg. The attempt to move the paralyzed leg failed to activate the right primary cortex. Instead there was activation of the right orbitofrontal and right anterior cingulate gyrus. The authors hypothesized that inhibitory pathways involving the orbitofrontal cortex and anterior cingulate may “disconnect” the premotor areas from the primary motor cortex, preventing the patient’s conscious intention from being translated into action. The authors suggested that the activation seen when this patient was preparing to move her affected limb provides evidence against feigning. The case report also suggests that inhibition of willed movement may play an important role in people with functional paralysis 14.
Vuilleumier et al 13 proposed another hypothesis in which it is argued that patients who exhibit symptoms of conversion disorder have a deficit in volition that involves the left dorsolateral prefrontal cortex and striatothalamocortical circuits. This explanation implicates different structures and functions in seeking to explain the cause(s) of conversion disorder. It is possible, given the complexity of brain structure and function, that conversation disorder is associated with deficits in both planning and execution (premotor stage).
Conversion disorder symptoms
Conversion symptoms typically begin with some stressor, trauma, or psychological distress that manifests itself as a physical deficit. There is no underlying physical cause for the symptom(s), and the affected individual cannot control the symptom(s). Symptoms may vary in severity and may come and go or be persistently present.
Symptoms of a conversion disorder include the loss of one or more bodily functions, such as:
- Blindness
- Inability to speak
- Numbness
- Paralysis
Common signs of conversion disorder include:
- A debilitating symptom that begins suddenly
- History of a psychological problem that gets better after the symptom appears
- Lack of concern that usually occurs with a severe symptom
Conversion disorder diagnosis
The diagnosis of conversion disorder continues to be a clinical challenge. A thorough psychiatric history and examination is necessary to explicate the onset of symptoms, the presence of stressors, and the presence of comorbid conditions. According to a study, 47.7 percent of the subjects with conversion disorder experienced some type of dissociative disorder 15. The diagnosis of conversion disorder should be made after establishing positive clinical findings that are incompatible with organic disease or are inconsistent across different parts of the examination19 and after ruling out any medical conditions the symptoms are mimicing 16.
Differential diagnoses of conversion disorder: organic diseases
- Myasthenia gravis (muscle weakness disorder)
- Multiple sclerosis (blindness resulting from optic neuritis)
- Periodic paralysis (muscle weakness)
- Polymyositis (muscle weakness)
- Stroke
- Lupus
- Spinal cord injury.
Figure 3. Step-wise guide for diagnosing conversion disorder
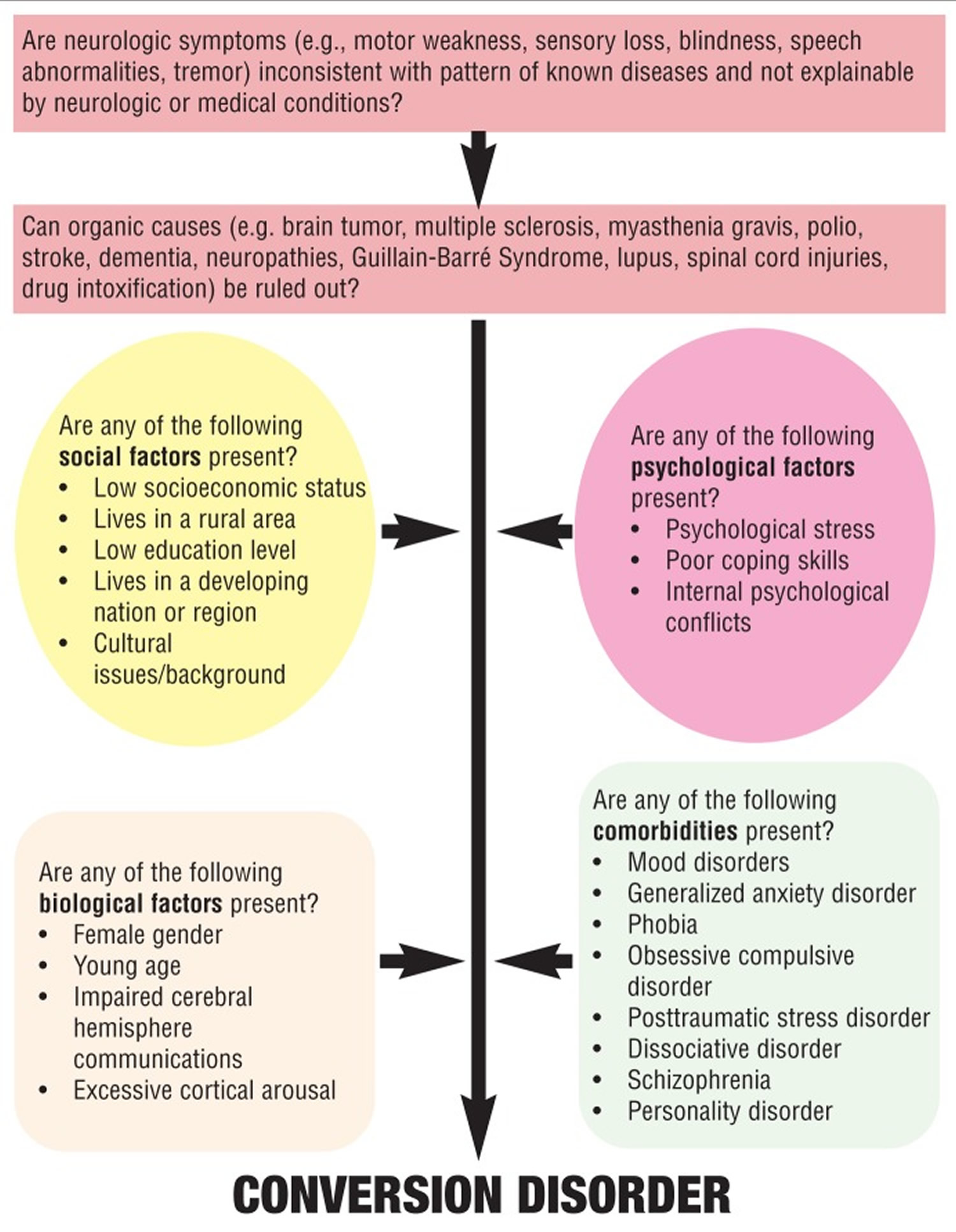 [Source 10]
[Source 10]
Patients with conversion disorder may present with blindness, deafness, pseudo seizures, dystonia, paralysis, syncope, or other neurological symptoms. The presenting symptoms depend on the cultural milieu, the patient’s degree of medical knowledge (i.e., individuals with a high degree of medical knowledge tend to have more subtle symptoms and deficits that may closely simulate neurological or other general medical conditions, whereas those with less medical knowledge may have more implausible symptoms), and the underlying psychiatric issue(s) 17. Table 1 lists the differentiating features of conversion disorder symptoms from those of organic disease. The following paragraphs review several examples of psychiatric disorders that should be ruled out before a diagnosis of conversion disorder is made.
Table 1. Differentiating features of conversion disorder symptoms
| SYMPTOM | DISTINGUISHING FEATURES AND PRESENTATION |
|---|---|
| Blindness | In conversion disorder, the patient, though complaining of recent onset of blindness, neither sustains injury while maneuvering around the office nor displays any expected bruises or scrapes. The pupillary reflex is present, thus demonstrating the intactness of the optic nerve, chiasm, tract, lateral geniculate body, and mesencephalon. |
| Deafness | In conversion deafness, the blink reflex to a loud and unexpected sound is present, thus demonstrating the intactness of the brain stem. |
| Psychogenic nonepileptic seizures | Patients with psychogenic nonepileptic seizures generally lack response to treatment with antiepileptic drugs or have a paradoxical increase in seizures with antiepileptic drug treatment. The negative history of injury or loss of control of bladder or bowel during the seizure episode is also significant. |
| Tremor | When weights are added to the affected limb, patients with functional tremor tend to have greater tremor amplitude, whereas in those with organic tremor, the tremor amplitude tends to diminish. |
| Dystonia | Useful distinguishing features include an inverted foot or “clenched fist,” adult onset, a fixed posture that is apparently present during sleep, and the presence of severe pain. |
| Paralysis | In conversion paralysis, the patient loses the use of half of his or her body or of a single limb, but the paralysis does not follow anatomical patterns and is often inconsistent upon repeat examination. |
| Syncope | The conversion patient may report feeling faint or fainting, but no autonomic changes are identified, such as pallor, and there is no associated injury. In addition, the fainting spells have a “swooning” character to them, heightening the drama of these events. |
| Aphonia | Conversion aphonia may be suspected when the patient is asked to cough, for example, during auscultation of the lungs. In contrast with other aphonias, the cough is normally full and loud. |
| Anesthesia | Conversion anesthesia may occur anywhere, but it is most common on the extremities. One may see a typical “glove and stocking” distribution; however, unlike the “glove and stocking” distribution that may occur in a polyneuropathy, the areas of conversion anesthesia have a very precise and sharp boundary, often located at a joint. |
| Paraplegia | In conversion paraplegia, one finds normal, rather than increased, deep tendon reflexes, and the Babinski sign is absent. In doubtful cases, the issue may be resolved by demonstrating normal motor evoked potentials. |
Hypochondriasis. Hypochondriasis is the excessive preoccupancy or worry about having one (or more) serious physical illnesses. This debilitating condition is the result of an inaccurate perception of the condition of body or mind despite the absence of an actual medical condition (e.g., “I know I’ve got cancer; they just haven’t done the right test yet”) 18.
Factitious disorder. Factitious disorder is a condition in which a person acts as if he or she has a physical or mental illness when he or she is not really sick. Factitious disorder by proxy is when a person acts as if a person in his or her care has an illness when the person does not. Factitious disorder is considered a mental illness because it is associated with severe emotional difficulties. People with factitious disorder deliberately create or exaggerate symptoms of an illness in several ways. They may lie about or fake symptoms, hurt themselves to bring on symptoms, or alter tests (such as contaminating a urine sample) to make it look like they or the person in their care is sick. Those with factitious disorder have an inner need to be seen as ill or injured without the need to achieve personal or financial gain 10.
Somatisation. Somatisation is a condition in which a person experiences physical symptoms that are inconsistent with or cannot be fully explained by any underlying general medical or neurological condition. Preoccupation with these symptoms leads to excessive distress in the patient 19.
Malingering. Malingering is not a mental disorder; however, psychiatrists and neurologists will likely encounter an individual malingering a psychiatric or neurological illness at some point in their careers. Malingering is defined as intentionally feigning the symptoms of a physical, psychiatric, or neurological disorder in order to achieve personal or financial gain. The individual is fully aware that he or she is feigning the symptoms and has clear knowledge of why he or she is doing it (e.g., for financial gain, recognition, or revenge) 20.
Conversion disorder treatment
Once conversion disorder is confirmed, the key to successful treatment is the establishment of a strong therapeutic alliance with the patient and the incorporation of a goal-oriented treatment program. Many patients who experience conversion disorder are unable to understand the inner conflict, which is perhaps occurring on an unconscious level. Confronting patients about the “psychological nature” of their symptoms can and usually does make the symptoms worse. However, patients can only achieve resolution of the conflict and the physical symptoms once they are able to recognize the connection.
Effective presentation of the diagnosis
Because patients with conversion disorder may be less open to psychological explanations than patients with defined neurological illness, the groundwork for a discussion of psychological and stress-related factors must be approached carefully.
- Do not inform the patient of the diagnosis on the first encounter.
- Reassure the patient that the symptoms are very real despite the lack of a definitive organic disease.
- Avoid giving the patient the impression that you feel there is nothing wrong with him or her.
- Provide socially acceptable examples of diseases that often are deemed stress-related (e.g., pepticular disease, hypertension).
- Provide common examples of producing symptoms (e.g., queasy stomach when talking in front of an audience, heart racing with asking someone for a date).
- Provide examples of how the subconscious influences behavior (e.g., nail biting, pacing, foot tapping)
- Emphasize that the symptoms are potentially reversible (unlike many neurological diseases). Patients can be told that although their bodies are not functioning properly, improvement is possible because there is no structural damage.
- Explain that understanding and accepting the diagnosis often leads to improvement because it allows proper engagement with rehabilitation rather than being stuck wondering or worrying about what is wrong.
Talk therapy and stress management training may help reduce symptoms.
The affected body part or physical function may need physical or occupational therapy until the symptoms go away. For example, a paralyzed arm must be exercised to keep the muscles strong.
Psychotherapy. The cornerstone of treatment for conversion disorder is psychotherapy aimed at elucidating the emotional bases of symptoms 21. Psychotherapy can include individual or group therapy, behavioral therapy, hypnosis, biofeedback, and relaxation training. Cognitive behavioral therapy (CBT) has shown the highest efficacy in treatment of pseudoseizures 22. Behavioral interventions should focus on improving self-esteem, increasing the capacity to express emotions, and improving the ability to communicate comfortably with others 22.
Physical therapy. Research has shown that physical therapy can be an effective method of treatment 23. Physiotherapy treatment is essential in the management of people with conversion disorder to allow them to overcome their physical symptoms and prevent secondary complications, such as muscle weakness and stiffness, that may occur as a result of inactivity 23. Progressive exercises that start as simple tasks and move to more challenging ones has shown to be effective in those with neurological disorders as well as conversion disorder. The physical therapist seeks to build the patient’s motor skills by gradually providing less verbal and tactile cueing or other assistance while the patient performs certain tasks 23.
Medication. Conversion disorder can also be improved through the use of medications to treat underlying psychiatric issues, such as depression and anxiety. Medications may include antidepressants, anxiolytics, or others depending on the psychiatric co-morbidity 21. Regular follow-up appointments with a neurologist and/or psychiatrist should be provided to the patient to limit emergency room visits and unnecessary diagnostic or invasive tests 21.
- Ballmaier M, Schmidt R. Conversion disorder revisited. https://www.functionalneurology.com/materiale_cic/99_XX_3/892_conversion/index.html[↩]
- American Psychiatric Association. Conversion disorder (functional neurological symptom disorder). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Arlington, VA: American Psychiatric Publishing. 2013;318-321.[↩][↩]
- Blitzstein S. Recognizing and conversion disorder. Virtual Mentor. 2008;10(3):158–160. https://www.ncbi.nlm.nih.gov/pubmed/23206882[↩][↩][↩][↩]
- Freud S. Freud S, Strachey J, Freud A. London: Hogarth Press and the Institute of Psycho-Analysis; 1962. The neuro-psychoses of defense; Institute of Psychoanalysis (eds). The Standard Edition of the Complete Psychological Works of Sigmund Freud; pp. 45–61.[↩]
- Marshall S, Bienenfeld D. Conversion disorder. Medscape. Drugs and diseases. https://emedicine.medscape.com/article/287464-overview[↩]
- Encyclopedia of mental disorders. Conversion disorder. http://www.minddisorders.com/Br-Del/Conversion-disorder.html[↩][↩][↩][↩]
- Nicholson T, Stone J, Kanaan R. Conversion disorder: a problematic diagnosis. J Neurol Neurosurg Psychiatry. 2011;82(11):1267–1273. http://jnnp.bmj.com/content/82/11/1267.long[↩]
- Feinstein A. Conversion disorder: advances in our understanding. CMAJ. 2011;183(8):915–920. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3091899/[↩]
- Carson A, Best S, Postma K, et al. The outcome of neurology outpatients with medically unexplained symptoms: a prospective cohort study. J Neural Neurosurg Psychiatry. 2003;74(7):897–900. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1738573/[↩][↩]
- Ali S, Jabeen S, Pate RJ, et al. Conversion Disorder— Mind versus Body: A Review. Innovations in Clinical Neuroscience. 2015;12(5-6):27-33. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4479361/[↩][↩][↩][↩][↩]
- Sadock BJ, Kaplan VA. Kaplan and Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 10th Edition. Philadelphia: Lippincott Williams & Wilkins; 2007.[↩]
- Scott R, Anson J. Neural correlates of motor conversion disorder. Motor Control. 2009;13:161–184. https://www.ncbi.nlm.nih.gov/pubmed/19454778[↩]
- Vuilleumier P, Chicherio C, Assal F, et al. Functional neuroanatomical correlates of hysterical sensorimotor loss. Brain. 2001;124(Pt 6):1077–1090. https://www.ncbi.nlm.nih.gov/pubmed/11353724[↩][↩]
- Marshall J, Halligan P, Fink G, et al. The functional anatomy of hysterical paralysis. Cognition. 1997;64(1):B1–B8. https://www.ncbi.nlm.nih.gov/pubmed/9342933[↩][↩]
- Sar V, Akyüz G, Kundakçi T, et al. Childhood trauma, dissociation, and psychiatric comorbidity in patients with conversion disorder. Am J Psychiatry. 2004;161(12):2271–2276. https://ajp.psychiatryonline.org/doi/full/10.1176/ajp.161.12.2271[↩]
- Conversion disorder. https://www.mayoclinic.org/diseases-conditions/conversion-disorder/symptoms-causes/syc-20355197[↩]
- Marshall S, Bienenfeld D. Conversion disorder. Medscape. Drugs and diseases. http://emedicine.medscape.com/article/287464-overview[↩]
- Avia M, Ruiz M. Recommendations for the treatment of hypochondriac patients. J Contemp Psychother. 2005;35(3):301–313.[↩]
- Spratt E, Pataki C. Somatoform disorders. Medscape. Drugs and diseases. http://emedicine.medscape.com/article/918628-overview[↩]
- Owens C, Dein S. Conversion disorder: the modern hysteria. Adv Psychiatr Treat. 2006;12(2):152–157.[↩]
- Stonnington C, Barry J, Fisher R. Conversion disorder. Am J Psychiatry. 2006;163:1510–1517. https://ajp.psychiatryonline.org/doi/full/10.1176/ajp.2006.163.9.1510[↩][↩][↩]
- Ali S, Jabeen S, Arain A, et al. How to use your clinical judgment to screen for and diagnose psychogenic nonepileptic seizures without video electroencephalogram. Innov Clin Neurosci. 2011;8(1):36–42. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3036551/[↩][↩]
- Kaur J, Garnawat D, Ghimiray D, et al. Conversion disorder and physical therapy. Delhi Psychiatry J. 2012;15(2):394–397.[↩][↩][↩]