What is dry socket
Dry socket also called alveolar osteitis, is a painful complication of a tooth extraction and is more likely to occur following extraction of wisdom teeth in the lower jaw or mandibular molar teeth. It is normal to feel sore or uncomfortable after having a tooth extracted. However, a dry socket pain can be intense. Dry socket is associated with severe pain developing 2 to 3 days post-operatively. Dry socket pain can persist for up to 10 days after extraction and may include pain so severe that it is not relieved by even the strongest of analgesic medications 1. There may also be an unpleasant smell or taste from the empty tooth socket. If you look into the socket, you might be able to see exposed bone rather than a blood clot. If you have dry socket pain a few days after the extraction, you will need to return to your dentist or oral surgeon. They will talk to you and examine you. You may need an X-ray to rule out other conditions such as osteomyelitis (a bone infection).
Dry socket is a complication associated with 0.5% to 5% of routine extractions 2, and is reported to occur more often after the extraction of mandibular molars, especially impacted wisdom teeth (1% to 37.5%) 3.
Women appear to be at higher risk from dry socket compared to men. A number of explanations for this gender difference in prevalence have been suggested e.g. changes that occur in the blood clotting mechanism during the menstrual cycle and the use of oral contraceptives 4. The highest incidence of dry socket is reported in the fourth decade of life 5, but this figure may be artefactual in view of the increased likelihood of tooth loss in later life 6. There is some evidence that people who have experienced dry sockets previously may be at greater risk to experiencing dry socket compared to those who have never had a dry socket 7.
You’re more at risk of developing dry socket if:
- you don’t follow your dentist’s instructions after the extraction
- you smoke or use tobacco, which slows healing
- you’ve had the condition before
- you’re over 25 years old
- the extraction was complicated
- have poor oral health
- use birth control pills, which may interfere with healing
- do not take proper care of your mouth after having a tooth pulled
- have had dry socket in the past
- drink from a straw after the tooth is pulled
- rinse and spit a lot after the tooth is pulled
Dry socket is thought to be linked to the loss of some or all of the blood clot that forms at the bottom of a socket after a tooth is taken out, although other factors are probably also involved. Normally, a blood clot forms at the site of a tooth extraction. This blood clot serves as a protective layer over the underlying bone and nerve endings in the empty tooth socket. The clot also provides the foundation for the growth of new bone and for the development of soft tissue over the clot. Exposure of the underlying bone and nerves results in intense pain, not only in the socket but also along the nerves radiating to the side of your face. The socket becomes inflamed and may fill with food debris, adding to the pain. If you develop dry socket, the pain usually begins one to three days after your tooth is removed. People with dry socket can also experience bad breath (halitosis). The condition can result in more visits to the dentist or dental hospital and other inconveniences such as time lost from work.
The risk of developing dry socket depends on many factors, some of which are unknown. Your dentist or dental care professional should be able to advise you of your own risk status.
To prevent dry socket after a tooth extraction, follow your dentist’s instructions including how to clean your mouth.
If you do develop dry socket, your dentist or oral surgeon may:
- flush out any food particles stuck in the socket
- put a medicated dressing in the socket.
Your dentist may prescribe antibiotics or pain medication. They may ask you to rinse your mouth with a mouthwash or salt water at home. The condition should improve quickly after treatment.
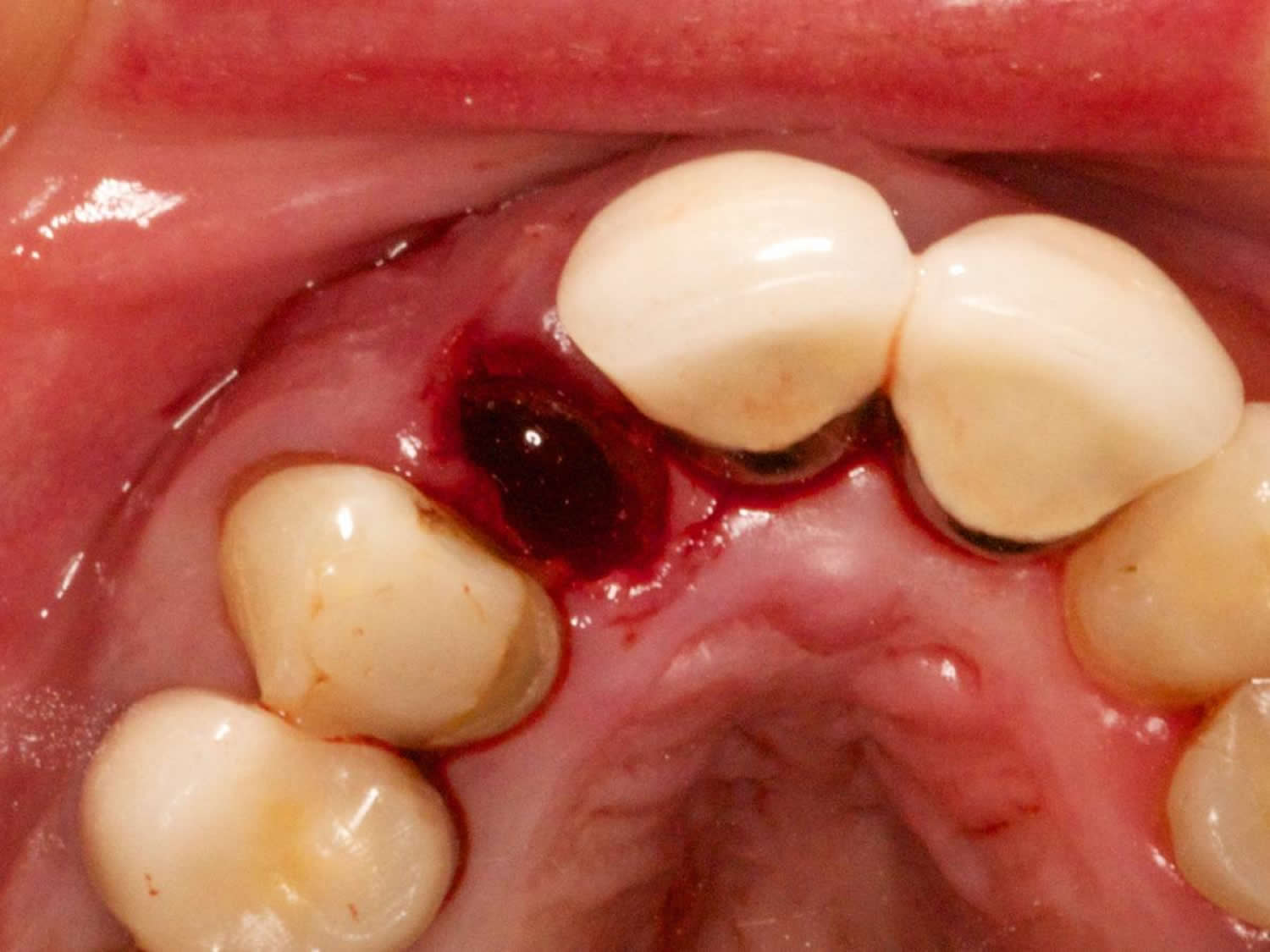
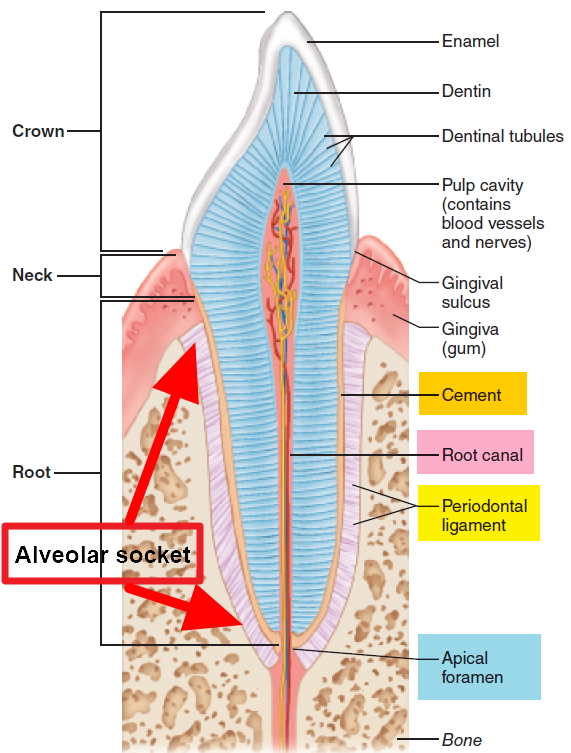
Figure 1. Tooth socket
What causes dry socket
When a tooth is pulled, a blood clot usually forms in the socket. The word ‘socket’ refers to the hole in the jaw bone where your tooth used to be. This blood clot protects the bone and nerve. But if the blood clot is dislodged or does not form well, the bone and nerve are left exposed. This causes the pain.
Dry socket occurs more often with wisdom teeth than with other teeth. You are also more likely than others to develop dry socket if you:
- smoke
- previously had dry socket
- had a difficult tooth extraction
- use oral contraceptives (birth control pills)
- don’t have good dental hygiene
- have had a tooth extracted from the lower jaw, especially a wisdom or molar tooth.
The cause of dry socket is not fully understood and a number of mechanisms and factors have been postulated that include: flap extent and design, bacterial contamination of the socket, surgical trauma, experience of the surgeon, perioperative patient stress factors and focal fibrinolytic activity 3. The focal fibrinolytic activity mechanisms were postulated to occur through plasminogen mediated fibrinolysis, non-plasminogen mediated fibrinolysis and leukocyte mediated fibrinolysis 1.
Several reviews have suggested a causal relationship between the complexity of the dental extraction and the occurrence of dry socket 8, 9. Smoking is considered to be another factor that may increase the risk of developing dry socket after tooth extraction 10. Additional risk factors include: infection around the tooth to be extracted, inadequate oral hygiene 11, and poor after care 9. There is very limited supportive evidence for some of the other reasons that may account for the loss of blood clot from a socket which include forceful spitting, sucking through a straw, coughing or sneezing 12. While bacterial breakdown and fibrinolysis is widely accepted as a major contributor to the loss of the blood clot, no studies have convincingly demonstrated an unequivocal bacterial cause for dry socket 13.
Risk factors for developing a dry socket
Factors that can increase your risk of developing dry socket include:
- Smoking and tobacco use. Chemicals in cigarettes or other forms of tobacco may prevent or slow healing and contaminate the wound site. The act of sucking on a cigarette may physically dislodge the blood clot prematurely.
- Oral contraceptives. High estrogen levels from oral contraceptives may disrupt normal healing processes and increase the risk of dry socket.
- Improper at-home care. Failure to follow home-care guidelines and poor oral hygiene may increase the risk of dry socket.
- Having dry socket in the past. If you’ve had dry socket in the past, you’re more likely to develop it after another extraction.
- Tooth or gum infection. Current or previous infections around the extracted tooth increase the risk of dry socket.
Dry socket complications
Painful, dry socket rarely results in infection or serious complications. However, potential complications may include delayed healing of or infection in the socket or progression to chronic bone infection (osteomyelitis).
How to prevent dry socket
In a well conducted systematic Cochrane review of dry socket prevention, there is some evidence that rinsing both before and after tooth extraction with chlorhexidine gluconate rinse (at 0.12% and 0.2% strength) or placing chlorhexidine gel (0.2%) in the sockets of extracted teeth, provides a benefit in preventing dry socket 14. However, there was insufficient evidence to conclude whether any treatments relieved established dry socket or not 14.
There have been a number of theories as to the cause of dry socket and a range of preventative agents have been advocated according to the prevailing theory of causation at the time including: plaque control, antiseptic rinses, preoperative systemic antibiotics and direct placement of medicaments into the socket 3, 15, 16, 9. Several studies have reported that preoperative and postoperative antiseptic chlorhexidine rinses can be effective in reducing the incidence of dry socket 17. Other studies have reported on the use of intrasocket antibiotic medicaments 18, and intrasocket antifibrinolytic agents 19. Studies have also reported upon the use of flap design to minimize trauma and risk of dry socket 20. The prophylactic use of systemic antibiotics is not generally advocated and there is a consensus that these measures should be reserved for individual patients reporting a history of multiple incidents of dry socket or for the immunocompromised patient 21.
What you can do after surgery
You’ll receive instructions about what to expect during the healing process after a tooth extraction and how to care for the wound. Proper at-home care after a tooth extraction helps promote healing and prevent damage to the wound. These instructions will likely address the following issues, which can help prevent dry socket:
- Activity. After your surgery, plan to rest for the remainder of the day. Follow your dentist’s or oral surgeon’s recommendations about when to resume normal activities and how long to avoid rigorous exercise and sports that might result in dislodging the blood clot in the socket.
- Pain management. Put cold packs on the outside of your face on the first day after extraction and warm packs after that, to help decrease pain and swelling. Follow your dentist’s or oral surgeon’s instructions on applying cold or heat to your face. Take pain medications as prescribed.
- Beverages. Drink lots of water after the surgery. Avoid alcoholic, caffeinated, carbonated or hot beverages for as long as your dentist or oral surgeon recommends. Don’t drink with a straw for at least a week because the sucking action may dislodge the blood clot in the socket.
- Food. Eat only soft foods, such as yogurt or applesauce, for the first day. Be careful with hot and cold liquids or biting your cheek until the anesthesia wears off. Start eating semisoft foods when you can tolerate them. Avoid chewing on the surgery side of your mouth.
- Cleaning your mouth. After surgery, you may gently rinse your mouth and brush your teeth, but avoid the extraction site for the first 24 hours. After the first 24 hours, gently rinse your mouth with warm salt several times a day for a week after your surgery. Mix 1/2 teaspoon (2.5 milliliters) of table salt in 8 ounces (237 milliliters) of water. Follow the instructions of your dentist or oral surgeon.
- Tobacco use. If you smoke or use tobacco, don’t do so for at least 48 hours after surgery and as long as you can after that. Any use of tobacco products after oral surgery can delay healing and increase the risk of complications.
Dry socket signs and symptoms
If you have dry socket you may have:
- Severe pain within a few days (1 to 3 days) of the tooth extraction – the pain may extend to your ear, eye, temple or neck on the same side of your face as the extraction
- Bad breath or a foul odor coming from your mouth
- A slight fever
- Unpleasant taste in your mouth
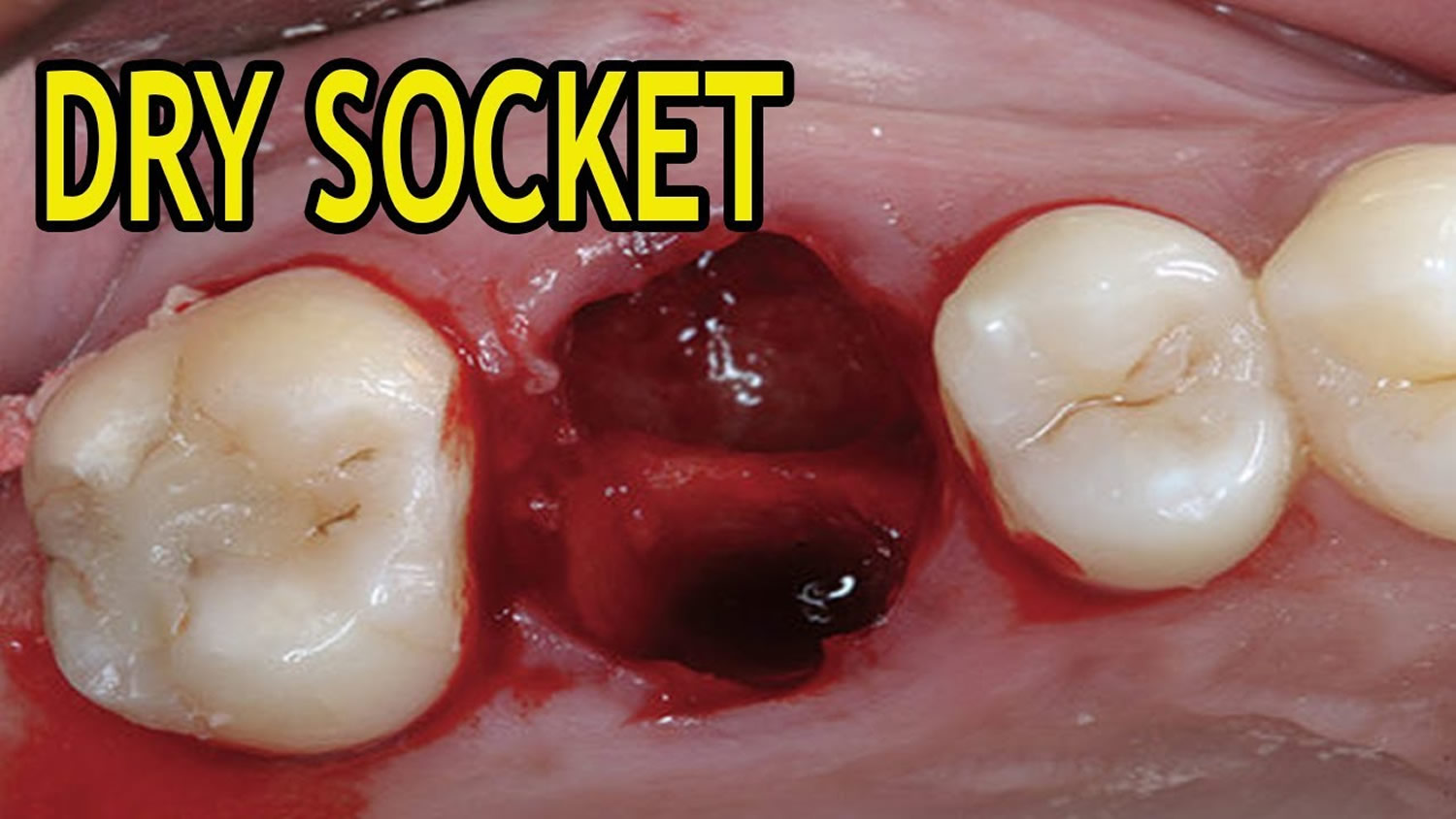
- Partial or total loss of the blood clot at the tooth extraction site, which you may notice as an empty-looking (dry) socket
- Visible bone in the socket
Dry socket was frequently conflated with an infected socket. A continuous throbbing pain that radiates to the ear, temple and neck is the most common symptom of dry socket 22. Classically, this starts 1 to 3 days post-extraction and may be accompanied by other signs and symptoms e.g. foul taste, bad breath, localized swelling and lymph-node involvement 8. The symptoms can persist for up to 10 days after extraction and may include pain so severe that it is not relieved by even the strongest of analgesic medications 1.
Dry socket diagnosis
Severe pain following a tooth extraction is often enough for your dentist or oral surgeon to suspect dry socket. He or she will also ask about any other symptoms and examine your mouth to see if you have a blood clot in your tooth socket and whether you have exposed bone.
You may need to have X-rays taken of your mouth and teeth to rule out other conditions, such as a bone infection (osteomyelitis) or small fragments of root or bone remaining in the wound after surgery.
Dry socket treatment
Treatment of dry socket focuses on reducing symptoms, particularly pain. Dry socket treatment may include:
- Flushing out the socket. Flushing out the socket can remove any food particles or other debris that may contribute to pain or possible infection.
- Medicated dressings. Your dentist or oral surgeon may pack the socket with medicated gel or paste and medicated dressings. These can provide relatively fast pain relief. The severity of your pain and other symptoms will determine whether you need dressing changes and how often or if you need other treatment.
- Pain medication. Ask which pain medication is best for your situation. You’ll likely need a prescription pain medication.
- Self-care. Once the dressing is removed, you may need to flush the socket at home to promote healing and eliminate debris. Typically you’ll receive instructions and a plastic syringe with a curved tip to squirt water, salt water or a prescription rinse into the socket. You’ll likely need to continue the rinse until the socket no longer collects any debris.
- Your dentist may also decide to:
- Start you on antibiotics
- Have you rinse with salt water or special mouthwash
- Give you a prescription for pain medicine or irrigation solution
Once treatment is started, you may soon begin to feel some pain relief. Pain and other symptoms should continue to improve and will likely be gone within a few days. However, keep scheduled appointments with your dentist or oral surgeon for dressing changes and other care.
Home remedies for dry socket
You can help promote healing and reduce symptoms during treatment of dry socket by following your dentist’s or oral surgeon’s instructions for self-care. You’ll likely be told to:
- Take pain medications as prescribed
- Avoid smoking or using tobacco products
- Drink plenty of clear liquids to remain hydrated and to prevent nausea that may be associated with some pain medications
- Rinse your mouth gently with warm salt water several times a day
- Brush your teeth gently around the dry socket area
- Use caution with eating or drinking, avoid carbonated beverages, and avoid smoking or using a straw to prevent dislodging the dressing
- Vezeau PJ. Dental extraction wound management: medicating postextraction sockets. Journal of Oral and Maxillofacial Surgery 2000;58(5):531-7. https://www.ncbi.nlm.nih.gov/pubmed/10800909[↩][↩][↩]
- Vezeau PJ. Dental extraction wound management: medicating postextraction sockets. Journal of Oral and Maxillofacial Surgery 2000;58(5):531-7. https://www.ncbi.nlm.nih.gov/pubmed/10800909 [↩]
- Caso A, Hung LK, Beirne OR. Prevention of alveolar osteitis with chlorhexidine: a meta-analytic review. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2005;99(2):155-9. https://www.ncbi.nlm.nih.gov/pubmed/15660084[↩][↩][↩]
- Garcia AG, Grana PM, Sampedro FG, Diago MP, Rey JM. Does oral contraceptive use affect the incidence of complications after extraction of a mandibular third molar?. British Dental Journal 2003;194(8):453-5. https://www.ncbi.nlm.nih.gov/pubmed/12778101[↩]
- Rood JP, Danford M. Metronidazole in the treatment of dry socket. International Journal of Oral Surgery 1981;10(5):345-7. https://www.ncbi.nlm.nih.gov/pubmed/6807922[↩]
- Butler DP, Sweet JB. Effect of lavage on the incidence of localized osteitis in mandibular third molar extraction sites. Oral Surgery, Oral Medicine, and Oral Pathology 1977;44(1):14-20. https://www.ncbi.nlm.nih.gov/pubmed/267872[↩]
- Reekie D, Downes P, Devlin CV, Nixon GM, Devlin H. The prevention of ‘dry socket’ with topical metronidazole in general dental practice. British Dental Journal 2006;200(4):210-3. https://www.ncbi.nlm.nih.gov/pubmed/16501533[↩]
- Blum IR. Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. International Journal of Oral and Maxillofacial Surgery 2002;31(3):309-17. https://www.ncbi.nlm.nih.gov/pubmed/12190139[↩][↩]
- Noroozi AR, Philbert RF. Modern concepts in understanding and management of the “dry socket” syndrome: comprehensive review of the literature. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2009;107(1):30-5. https://www.ncbi.nlm.nih.gov/pubmed/18755610[↩][↩][↩]
- Sweet JB, Butler DP. Predisposing and operative factors: effect on the incidence of localized osteitis in mandibular third-molar surgery. Oral Surgery, Oral Medicine, and Oral Pathology 1978;46(2):206-15. https://www.ncbi.nlm.nih.gov/pubmed/280828[↩]
- Tjernberg A. Influence of oral hygiene measures on the development of alveolitis sicca dolorosa after surgical removal of mandibular third molars. International Journal of Oral Surgery 1979;8(6):430-4. https://www.ncbi.nlm.nih.gov/pubmed/120340[↩]
- Bloomer CR. Straws do not cause dry sockets when third molars are extracted. Texas Dental Journal 2012;129(1):25-32. https://www.ncbi.nlm.nih.gov/pubmed/22432232[↩]
- Alexander RE. Dental extraction wound management: a case against medicating postextraction. Journal of Oral and Maxillofacial Surgery 2000;58(5):538-51. https://www.ncbi.nlm.nih.gov/pubmed/10800910[↩]
- Daly B, Sharif MO, Newton T, Jones K, Worthington HV. Local interventions for the management of alveolar osteitis (dry socket). Cochrane Database of Systematic Reviews 2012, Issue 12. Art. No.: CD006968. DOI: 10.1002/14651858.CD006968.pub2. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006968.pub2/full[↩][↩]
- Hedstrom L, Sjogren P. Effect estimates and methodological quality of randomised controlled trials about prevention of alveolar osteitis following tooth extraction: a systematic review. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2007;103(1):8-15. https://www.ncbi.nlm.nih.gov/pubmed/17178488[↩]
- Kolokythas A, Olech E, Miloro M. Alveolar osteitis: a comprehensive review of concepts and controversies. International Journal of Dentistry 2010;2010:249073. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2905714/[↩]
- Berwick JE, Lessin ME. Effects of a chlorhexidine gluconate oral rinse on the incidence of alveolar osteitis in mandibular third molar surgery. Journal of Oral and Maxillofacial Surgery 1990;48(5):444-8. https://www.ncbi.nlm.nih.gov/pubmed/2329393[↩]
- van Eeden SP, Butow K. Post-operative sequelae of lower third molar removal: a literature review and pilot study on the effect of Covomycin D. SADJ Journal of the South African Dental Association 2006;61(4):154-9. https://www.ncbi.nlm.nih.gov/pubmed/16808181[↩]
- Gersel-Pedersen N. Tranexamic acid in alveolar sockets in the prevention of alveolitis sicca dolorosa. International Journal of Oral Surgery 1979;8(6):421-9. https://www.ncbi.nlm.nih.gov/pubmed/120339[↩]
- Bello SA, Olaitan AA, Ladeinde AL. A randomized comparison of the effect of partial and total wound closure techniques on postoperative morbidity after mandibular third molar surgery. Journal of Oral and Maxillofacial Surgery 2011;69(6):e24-30. https://www.ncbi.nlm.nih.gov/pubmed/21497001[↩]
- Epstein JB, Chong S, Le ND. A survey of antibiotic use in dentistry. Journal of the American Dental Association 2000;131(11):1600-9. https://www.ncbi.nlm.nih.gov/pubmed/11103580[↩]
- Swanson AE. A double-blind study on the effectiveness of tetracycline in reducing the incidence of fibrinolytic alveolitis. Journal of Oral and Maxillofacial Surgery 1989;47(2):165-7. https://www.ncbi.nlm.nih.gov/pubmed/2913252[↩]