Contents
What is DVT
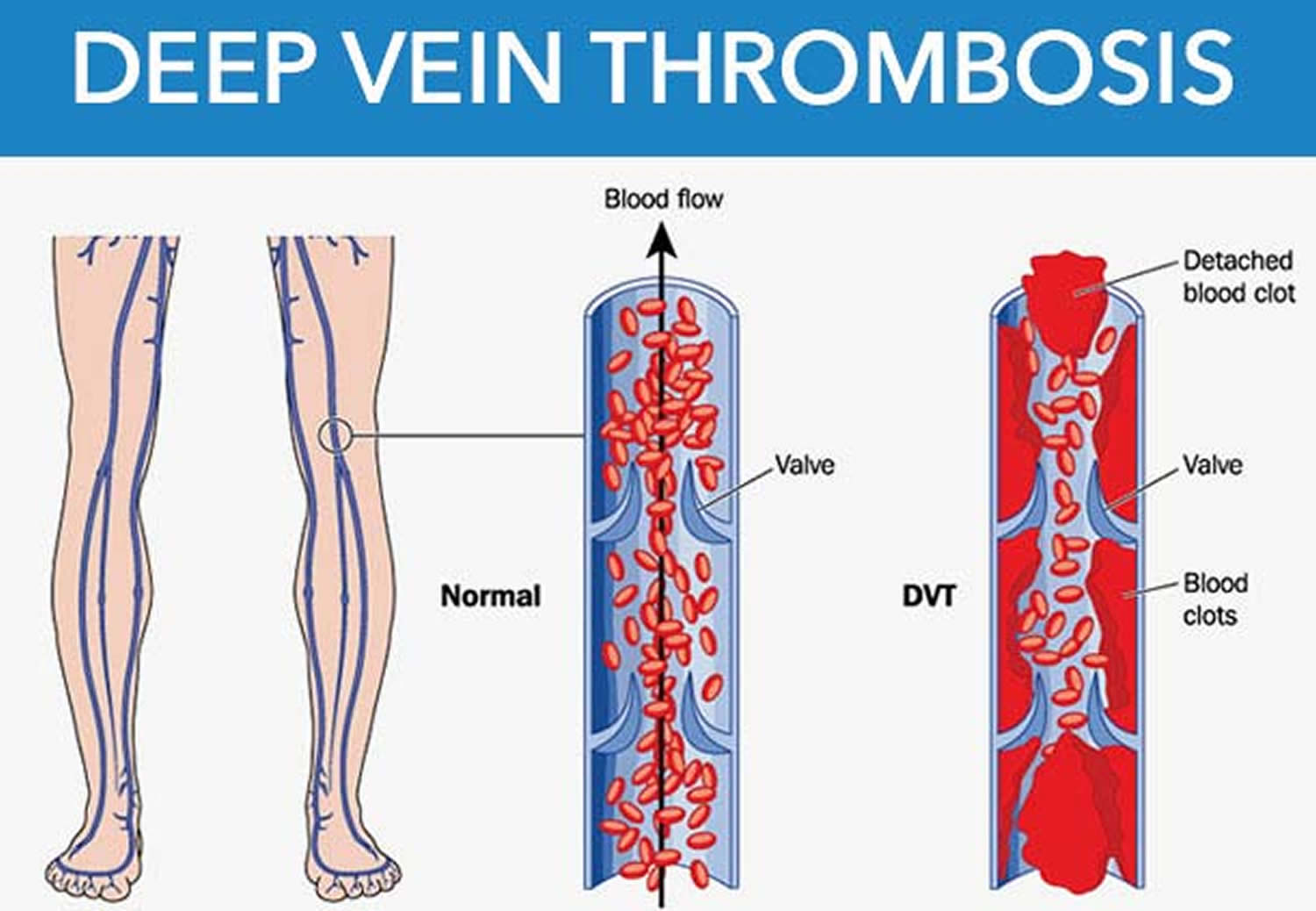
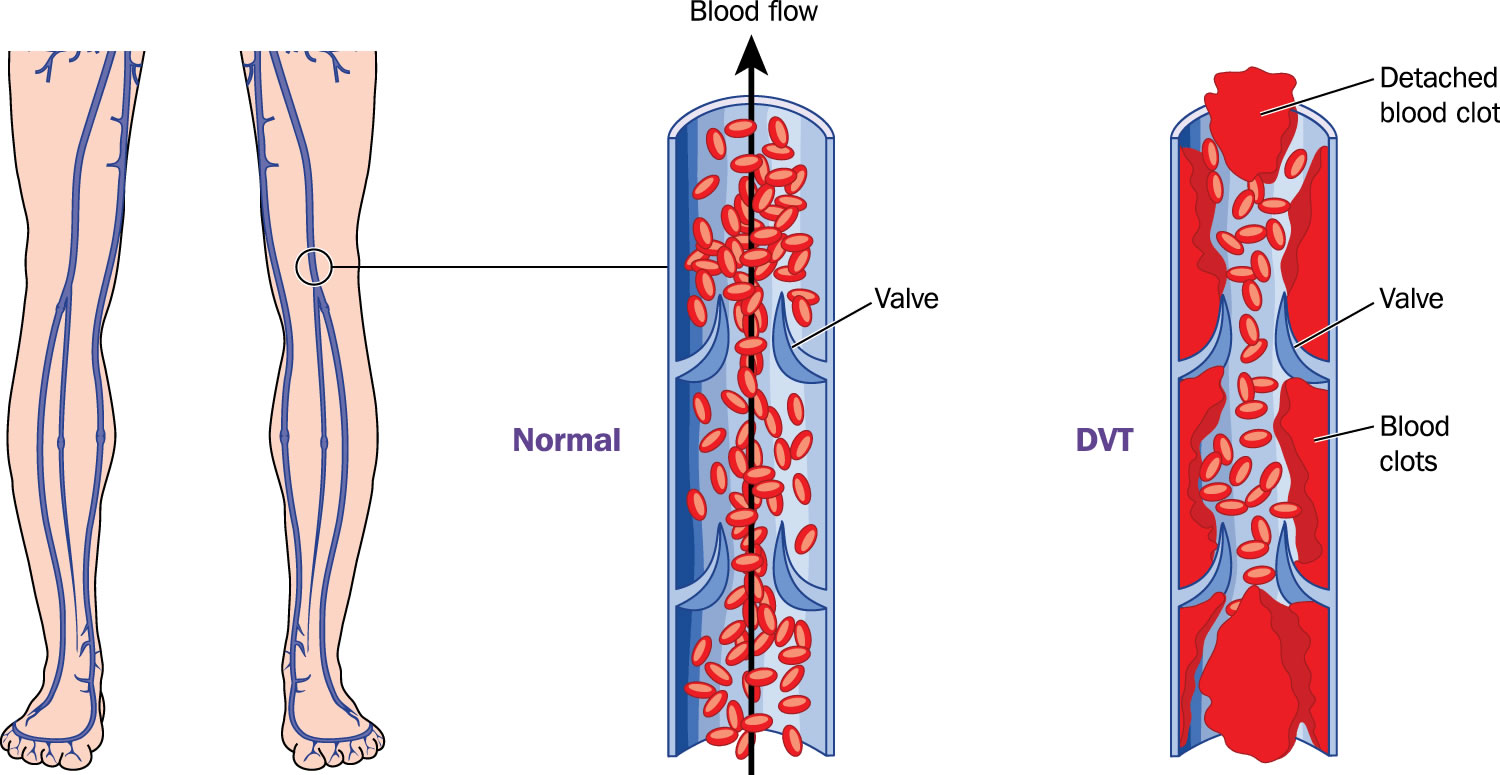
Deep vein thrombosis (DVT) is a blood clot that develops within a deep vein in the body. Most deep vein clots or DVTs occur in the lower leg, thigh or pelvis, but they can also occur in the arm. If the vein swells and cause pain and swelling in the leg, the condition is called thrombophlebitis. A deep vein thrombosis can break loose and cause a serious problem in the lung, called a pulmonary embolism. This is a serious condition that occurs when a piece of blood clot breaks off into the bloodstream and blocks one of the blood vessels in the lungs. Although rare, pulmonary embolism—can be fatal.
Even if a blood clot does not break free, it may cause permanent damage to the valves in the vein. This damage can lead to long-term problems in the leg such as pain, swelling, and leg sores.
- Blood clots that develop in a vein are also known as venous thrombosis.
- DVT usually occurs in a deep leg vein, a larger vein that runs through the muscles of the calf and the thigh.
- DVT and pulmonary embolism together are known as venous thromboembolism (VTE).
Sitting still for a long time can make you more likely to get a DVT. Some medicines and disorders that increase your risk for blood clots can also lead to DVTs.
How blood clots
Blood contains cells called platelets and proteins known as clotting factors. When a blood vessel is cut, the platelets and clotting factors form a solid clot that acts as a plug to stop the wound bleeding.
Normally, blood clotting occurs when a blood vessel is damaged and bleeds. If the blood clots when a vessel isn’t damaged, a clot can form within a vein or artery (thrombosis) and restrict the blood flow.
Figure 1. Deep vein thrombosis (DVT)
Common DVT symptoms are:
- Warmth and tenderness over the vein
- Pain or swelling in the part of the body affected
- Skin redness
In many cases, DVT occurs without noticeable symptoms and is very difficult to detect. For this reason, doctors focus on preventing the development of DVT using different types of therapies, depending upon a patient’s needs. Your doctor will take steps to prevent DVT if you have a major fracture or are having lower extremity surgery—including total hip or total knee replacement.
It is important to know about DVT because it can happen to anybody and can cause serious illness, disability, and in some cases, death. The good news is that DVT is preventable and treatable if discovered early.
Treatment includes medicines to ease pain and inflammation, break up clots and keep new clots from forming. Keeping the affected area raised and applying moist heat can also help. If you are taking a long car or plane trip, take a break, walk or stretch your legs and drink plenty of liquids.
Other Names for DVT:
- Blood clot in the leg.
- Thrombophlebitis.
- Venous thrombosis.
- Venous thromboembolism (VTE). This term is used for both deep vein thrombosis and pulmonary embolism.
What causes DVT?
Anyone can develop DVT, but it becomes more common over the age of 40. As well as age, there are also a number of other risk factors that can affect blood flow in the deep veins and increase the risk for developing blood clots. These include:
- Deep vein thrombosis (DVT) sometimes occurs for no apparent reason.
- Older age. Being older than 60 is a risk factor for DVT, although DVT can occur at any age.
- Personal or family history of DVT or pulmonary embolism
- Injury to a deep vein from surgery, a broken bone, or other trauma.
- Slow blood flow in a deep vein due to lack of movement. This may occur after surgery, if you’re ill and in bed for a long time, or if you’re traveling for a long time.
- A central venous catheter. This is a tube placed in a vein to allow easy access to the bloodstream for medical treatment.
- Having certain types of malignant cancers
- Recent or ongoing treatment for cancer.
- Having a vein disease, such as varicose veins
- Blood flow is sluggish or slow. Lack of motion can cause sluggish or slow blood flow. This may occur after surgery, if you’re ill and in bed for a long time, or if you’re traveling for a long time.
- Smoking
- Using combined contraceptive pill and hormone replacement therapy (HRT) both contain the female hormone estrogen, which causes the blood to clot more easily. If you’re taking either of these, your risk of developing DVT is slightly increased.
- Pregnancy and the first 6 weeks after giving birth.
- Being overweight or obese
- Inheriting a blood-clotting disorder. Your blood is thicker or more likely to clot than normal. Some inherited conditions (such as factor V Leiden) increase the risk of blood clotting.
- A vein’s inner lining is damaged. Injuries caused by physical, chemical, or biological factors can damage the veins. Such factors include surgery, serious injuries, inflammation, and immune responses.
Your risk for DVT increases if you have more than one of the risk factors listed above.
A broken hip or leg, or having major surgery on your hip, knee or lower leg can affect normal blood flow and clotting. In these orthopaedic situations, three primary factors contribute to the formation of blood clots in veins: slow blood flow, hypercoagulation, and damage to the veins.
Blood thickens, or coagulates, around matter that does not belong in the veins. During surgery, matter such as tissue debris, collagen, or fat may be released into the blood system and can cause the blood to coagulate. In addition, during total hip replacement, reaming and preparing the bone to receive the prosthesis may cause the body to release chemical substances called antigens into the blood system. These antigens can also stimulate clot formation.
- Surgery and some medical treatments can increase your risk of getting DVT. It’s estimated that around 25,000 people who are admitted to hospital die from preventable blood clots each year.
Inactivity
The walls of the veins are smooth. This helps blood flow freely and mix with naturally occurring agents (anticoagulants) in the blood that keep the blood cells from clotting. Blood that does not flow freely and does not mix with anticoagulants may be more likely to lead to blood clots. This is why it is important to watch for signs of DVT in people who are on bed rest, immobilized in a splint or cast, or not able to move for long periods of time.
When you’re inactive your blood tends to collect in the lower parts of your body, often in your lower legs. This is usually nothing to worry about because when you start to move, your blood flow increases and moves evenly around your body.
However, if you’re unable to move for a long period of time – such as after an operation, because of an illness or injury, or during a long journey – your blood flow can slow down considerably. A slow blood flow increases the chances of a blood clot forming.
In hospital
If you have to go into hospital for an operation or procedure, your risk of getting a blood clot increases. This is because DVT is more likely to occur when you’re unwell or inactive, or less active than usual.
As a patient, your risk of developing DVT depends on the type of treatment you’re having. You may be at increased risk of DVT if any of the following apply:
- you’re having an operation that takes longer than 90 minutes, or 60 minutes if the operation is on your leg, hip or abdomen
- you’re having an operation for an inflammatory or abdominal condition, such as appendicitis
- you’re confined to a bed, unable to walk, or spending a large part of the day in a bed or chair for at least three days
You may also be at increased risk of DVT if you’re much less active than usual because of an operation or serious injury and have other DVT risk factors, such as a family history of the condition.
When you’re admitted to hospital you’ll be assessed for your risk of developing a blood clot and, if necessary, given preventative treatment.
Damage to the Vein Walls
If the wall of a blood vessel is damaged, it may become narrowed or blocked, which can cause a blood clot to form.
Blood vessels can be damaged by injuries such as broken bones or severe muscle damage. Sometimes, blood vessel damage that occurs during surgery can cause a blood clot, particularly in operations on the lower half of your body.
During surgery, the doctor must move, or retract, soft tissues such as ligaments, muscles, and tendons to reach the area being operated on. In some cases, this can release naturally occurring substances that promote blood clotting.
Conditions such as vasculitis (inflammation of the blood vessels), varicose veins and some forms of medication, such as chemotherapy, can also damage blood vessels.
Medical and genetic conditions
Your risk of getting DVT is increased if you have a condition that causes your blood to clot more easily than normal. These conditions include:
- cancer – cancer treatments such as chemotherapy and radiotherapy can increase this risk further
- heart disease and lung disease
- infectious conditions, such as hepatitis
- inflammatory conditions, such as rheumatoid arthritis
- thrombophilia – a genetic condition where your blood has an increased tendency to clot
- antiphospholipid syndrome – an immune system disorder that causes an increased risk of blood clots.
Pregnancy
During pregnancy, blood clots more easily. It’s the body’s way of preventing too much blood being lost during childbirth.
Venous thromboembolism (VTE) – DVT and pulmonary embolism – affects about one in 100,000 women of childbearing age.
DVTs are also rare in pregnancy, although pregnant women are up to 10 times more likely to develop thrombosis than non-pregnant women of the same age. A clot can form at any stage of pregnancy and up to six weeks after the birth.
Having thrombophilia (a condition where the blood has an increased tendency to clot), or having a parent, or brother or sister, who’s had a thrombosis, increase your risk of developing a DVT during pregnancy.
Other risk factors during pregnancy include:
- having had thrombosis (a clot) before
- being over 35 years old
- being obese (with a BMI of 30 or more)
- having thrombophilia – a condition that makes clots more likely
- expecting two or more babies
- having recently had a caesarean section
- not moving (being immobile) for long periods of time, including long-distance travel of more than four hours, or after an operation
- smoking (find out how to quit smoking)
- having severe varicose veins – if they are painful or above the knee with redness or swelling
- dehydration
- having a parent, brother or sister who has had a thrombosis
- having fertility treatment
Low molecular weight heparin (LMWH) is usually used to treat pregnant women with DVT. LMWH is an anticoagulant, which means it prevents the blood clot getting bigger. It’s given by injection and doesn’t affect your developing baby.
Contraceptive pill and HRT
The combined contraceptive pill and hormone replacement therapy (HRT) both contain the female hormone oestrogen. Oestrogen causes the blood to clot a bit more easily than normal, so your risk of getting DVT is slightly increased. There’s no increased risk from the progestogen-only contraceptive pill.
Other causes
Your risk of getting DVT is also increased if you or a close relative have previously had DVT and:
- you’re overweight or obese
you smoke - you’re dehydrated
- you’re over 60 – particularly if you have a condition that restricts your mobility.
Complications of DVT
The two main complications of deep vein thrombosis (DVT) are pulmonary embolism and post-thrombotic syndrome.
Pulmonary embolism
A pulmonary embolism is the most serious complication of DVT. It happens when a piece of blood clot (DVT) breaks off and travels through your bloodstream to your lungs, where it blocks one of the blood vessels. In severe cases this can be fatal.
If the clot is small, it might not cause any symptoms. If it’s medium-sized, it can cause chest pain and breathing difficulties. A large clot can cause the lungs to collapse, resulting in heart failure, which can be fatal.
About one in 10 people with an untreated DVT develops a severe pulmonary embolism.
Post-thrombotic syndrome
If you’ve had a DVT, you may develop long-term symptoms in your calf known as post-thrombotic syndrome. This affects around 20-40% of people with a history of DVT.
If you have DVT, the blood clot in the vein of your calf can divert the flow of blood to other veins, causing an increase in pressure. This can affect the tissues of your calf and lead to symptoms, including:
- calf pain
- swelling
- a rash
- ulcers on the calf (in severe cases)
When a DVT develops in your thigh vein, there’s an increased risk of post-thrombotic syndrome occurring. It’s also more likely to occur if you’re overweight or if you’ve had more than one DVT in the same leg.
DVT prophylaxis
You can take steps to prevent deep vein thrombosis (DVT) and pulmonary embolism (PE). If you’re at risk for these conditions:
- See your doctor for regular checkups.
- Take all medicines as your doctor prescribes.
- Get out of bed and move around as soon as possible after surgery or illness (as your doctor recommends). Moving around lowers your chance of developing a blood clot.
- Exercise your lower leg muscles during long trips. This helps prevent blood clots from forming.
If you’ve had DVT or PE before, you can help prevent future blood clots. Follow the steps above and:
- Take all medicines that your doctor prescribes to prevent or treat blood clots
- Follow up with your doctor for tests and treatment
- Use compression stockings as your doctor directs to prevent leg swelling
If you’re admitted to hospital or planning to go into hospital for surgery, your risk of developing a blood clot while you’re there will be assessed.
Surgery and some medical treatments can increase your risk of developing DVT.
Contact your doctor at once if you have any signs or symptoms of DVT or PE.
Before going into hospital
If you’re going into hospital to have an operation, and you’re taking the combined contraceptive pill or hormone replacement therapy (HRT), you’ll be advised to temporarily stop taking your medication four weeks before your operation.
Similarly, if you’re taking medication to prevent blood clots, such as aspirin, you may be advised to stop taking it one week before your operation.
There’s less risk of getting DVT when having a local anaesthetic compared with a general anaesthetic. Your doctor will discuss whether it’s possible for you to have a local anaesthetic.
While you’re in hospital
There are a number of things your healthcare team can do to help reduce your risk of getting DVT while you’re in hospital.
For example, they’ll make sure you have enough to drink so you don’t become dehydrated, and they’ll also encourage you to move around as soon as you’re able to.
Depending on your risk factors and individual circumstances, a number of different medications can be used to help prevent DVT. For example:
- anticoagulant medicines – such as dabigatran etexilate or fondaparinux sodium, which are often used to help prevent blood clots after certain types of surgery, including orthopaedic surgery
- low molecular weight heparin (LMWH) – often used in many cases to help prevent blood clots, including during and shortly after pregnancy
- unfractionated heparin (UFH) – often used in people with severe kidney impairment or established kidney failure
Compression stockings or compression devices are also commonly used to help keep the blood in your legs circulating.
Compression stockings are worn around your feet, lower legs and thighs, and fit tightly to encourage your blood to flow more quickly around your body.
Compression devices are inflatable and work in the same way as compression stockings, inflating at regular intervals to squeeze your legs and encourage blood flow.
Your healthcare team will usually advise you to walk regularly after you’ve been prescribed compression stockings. Keeping mobile can help prevent the symptoms of DVT returning and may help prevent or improve complications of DVT, such as post-thrombotic syndrome.
When you leave hospital
You may need to continue to take anticoagulant medicine and wear compression stockings when you leave hospital.
Before you leave, your healthcare team should advise you about how to use your treatment, how long to continue using it for, and who to contact if you experience any problems.
Lifestyle changes
You can reduce your risk of getting DVT by making changes to your lifestyle, such as:
- quit smoking
- eating a healthy, balanced diet
- getting regular exercise
- maintaining a healthy weight or losing weight if you’re obese
Travel Tips
The risk of developing DVT while traveling is low. The risk increases if the travel time is longer than 4 hours or you have other DVT risk factors.
During long trips, it may help to:
- Walk up and down the aisles of the bus, train, or airplane. If traveling by car, stop about every hour and walk around.
- Move your legs and flex and stretch your feet to improve blood flow in your calves.
- Wear loose and comfortable clothing.
- Drink plenty of fluids and avoid alcohol. Avoid drinking excessive amounts of alcohol because it can cause dehydration.
- Avoid taking sleeping pills because they can cause immobility
- Perform simple leg exercises, such as regularly flexing your ankles
- Take occasional short walks when possible – for example, during refuelling stopovers
- Wear elastic compression stockings
If you have risk factors for DVT, your doctor may advise you to wear compression stockings while traveling. Or, he or she may suggest that you take a blood-thinning medicine before traveling.
Wearing compression stockings during flights of four hours or more can significantly reduce your risk of DVT, as well as leg swelling (edema).
The below-knee stockings apply gentle pressure to the ankle to help blood flow. They come in a variety of sizes and there are also different levels of compression. Class 1 stockings (exerting a pressure of 14-17 mmHg at the ankle) are generally sufficient.
It’s vital that compression stockings are measured and worn correctly. Ill-fitting stockings could further increase the risk of DVT.
Flight socks are available from pharmacies, airports and many retail outlets. Take advice on size and proper fitting from a pharmacist or another health professional.
DVT signs and symptoms
The signs and symptoms of deep vein thrombosis (DVT) might be related to DVT itself or pulmonary embolism (PE). See your doctor right away if you have signs or symptoms of either condition. Both DVT and PE can cause serious, possibly life-threatening problems if not treated.
Deep Vein Thrombosis
Only about half of the people who have DVT have signs and symptoms. These signs and symptoms occur in the leg affected by the deep vein clot. They include:
- Swelling of the leg or along a vein in the leg
- Pain, swelling and tenderness in one of your legs (usually your calf)
- Pain or tenderness in the leg, which you may feel only when standing or walking
- Heavy ache in the affected area
- Increased warmth in the area of the leg that’s swollen or painful
- Red or discolored skin on the leg, particularly at the back of your leg below the knee
DVT usually (although not always) affects one leg. The pain may be worse when you bend your foot upward towards your knee.
Pulmonary Embolism
If left untreated, about 1 in 10 people with a DVT will develop a pulmonary embolism. A pulmonary embolism is a very serious condition that can cause death.
Some people aren’t aware of a deep vein clot until they have signs and symptoms of PE. Signs and symptoms of pulmonary embolism include:
- Unexplained shortness of breath – which may come on gradually or suddenly
- Pain with deep breathing
- Coughing up blood
- Sudden collapse
Rapid breathing and a fast heart rate also may be signs of PE.
Both DVT and pulmonary embolism require urgent investigation and treatment.
Seek immediate medical attention if you have pain, swelling and tenderness in your leg, and you develop breathlessness and chest pain.
DVT diagnosis
See your doctor as soon as possible if you think you may have DVT – for example, if you have pain, swelling and a heavy ache in your leg.
Your doctor will diagnose deep vein thrombosis (DVT) based on your medical history, a physical exam, and test results. He or she will identify your risk factors and rule out other causes of your symptoms.
For some people, DVT might not be diagnosed until after they receive emergency treatment for pulmonary embolism (PE).
Medical History
To learn about your medical history, your doctor may ask about:
- Your overall health
- Any prescription medicines you’re taking
- Any recent surgeries or injuries you’ve had
- Whether you’ve been treated for cancer
Physical Exam
Your doctor will check your legs for signs of DVT, such as swelling or redness. He or she also will check your blood pressure and your heart and lungs.
Diagnostic Tests
Your doctor may recommend tests to find out whether you have DVT.
Common Tests
The most common test for diagnosing deep vein blood clots is ultrasound. This test uses sound waves to create pictures of blood flowing through the arteries and veins in the affected leg.
Your doctor also may recommend a D-dimer test or venography.
D-dimer test
It can be difficult to diagnose DVT from symptoms alone, so your GP may advise that you have a specialised blood test called a D-dimer test.
A D-dimer test measures a substance in the blood that’s released when a blood clot dissolves. If the test shows high levels of the substance, you may have a deep vein blood clot. If your test results are normal and you have few risk factors, DVT isn’t likely.
However, the D-dimer test isn’t always reliable because blood clot fragments can increase after an operation, injury or during pregnancy. Additional tests, such as an ultrasound scan, will need to be carried out to confirm DVT.
Ultrasound scan
An ultrasound scan can be used to detect clots in your veins. A special type of ultrasound called a Doppler ultrasound can also be used to find out how fast the blood is flowing through a blood vessel. This helps doctors identify when blood flow is slowed or blocked, which could be caused by a blood clot.
Your doctor may suggest venography if an ultrasound doesn’t provide a clear diagnosis.
Venogram
A venogram may be used if the results of a D-dimer test and ultrasound scan can’t confirm a diagnosis of DVT.
For venography, a liquid called a contrast dye is injected into a vein in your foot. The dye travels up the leg and can be detected by X-ray image, which will highlight a gap in the blood vessel where a clot is stopping the flow of blood. The x ray will also show whether blood flow is slow in the vein, which may suggest a blood clot.
Other Tests
Other tests used to diagnose DVT include magnetic resonance imaging (MRI) and computed tomography or CT, scanning. These tests create pictures of your organs and tissues.
You may need blood tests to check whether you have an inherited blood clotting disorder that can cause DVT. This may be the case if you have repeated blood clots that are not related to another cause. Blood clots in an unusual location (such as the liver, kidney, or brain) also may suggest an inherited clotting disorder.
If your doctor thinks that you have PE, he or she may recommend more tests, such as a lung ventilation perfusion scan (VQ scan). A lung VQ scan shows how well oxygen and blood are flowing to all areas of the lungs.
DVT treatment
Doctors treat deep vein thrombosis (DVT) with medicines and other devices and therapies. The main goals of treating DVT are to:
- Stop the blood clot from getting bigger
- Prevent the blood clot from breaking off and moving to your lungs
- Reduce your chance of having another blood clot
Treatment for DVT usually involves taking anticoagulant medicines, which reduce the blood’s ability to clot and stop existing clots getting bigger.
Heparin and warfarin are two types of anticoagulant often used to treat DVT. Heparin is usually prescribed first because it works immediately to prevent further clotting. After initial treatment, you may also need to take warfarin to prevent another blood clot forming.
A number of anticoagulants, known as directly acting oral anticoagulants (DOACs), may also be used to treat conditions such as DVT. These medications include rivaroxaban and apixaban, and they’ve been shown to be as effective as heparin and warfarin with less serious side effects.
Anticoagulation
Anticoagulant medicines prevent blood clots getting bigger. They can also help stop part of the blood clot breaking off and becoming lodged in another part of your bloodstream (an embolism).
Although they’re often referred to as “blood-thinning” medicines, anticoagulants don’t actually thin the blood. They alter proteins within it, which prevents clots forming so easily.
Heparin and warfarin are two types of anticoagulants that are used to treat DVT. Heparin is usually prescribed first because it works immediately to prevent further clotting. After this initial treatment, you may also need to take warfarin to prevent another blood clot forming.
- The most common side effect of blood thinners is bleeding. Bleeding can happen if the medicine thins your blood too much. This side effect can be life threatening.
Sometimes the bleeding is internal (inside your body). People treated with blood thinners usually have regular blood tests to measure their blood’s ability to clot. These tests are called PT and PTT tests.
These tests also help your doctor make sure you’re taking the right amount of medicine. See your doctor right away if you have easy bruising or bleeding. These may be signs that your medicines have thinned your blood too much.
Heparin
Heparin is available in two different forms:
- standard (unfractioned) heparin
- low molecular weight heparin (LMWH)
Standard (unfractioned) heparin can be given as:
- an intravenous injection – an injection straight into one of your veins
- an intravenous infusion – where a continuous drip of heparin (via a pump) is fed through a narrow tube into a vein in your arm (this must be done in hospital)
- a subcutaneous injection – an injection under your skin
Low molecular weight heparin (LMWH) is usually given as a subcutaneous injection.
The dose of standard (unfractionated) heparin to treat a blood clot varies significantly from person to person, so the dosage must be carefully monitored and adjusted if necessary. You may need to stay in hospital for 5 to 10 days and have frequent blood tests to ensure you receive the right dose.
Low molecular weight heparin (LMWH) works differently from standard heparin. It contains small molecules, which means its effects are more reliable and you won’t have to stay in hospital and be monitored.
Both standard heparin and low molecular weight heparin (LMWH) can cause side effects, including:
- a skin rash and other allergic reactions
- bleeding
- weakening of the bones if taken for a long time (although rare with LMWH)
In rare cases, heparin can also cause an extreme reaction that makes existing blood clots worse and causes new clots to develop. This reaction, and weakening of your bones, is less likely to occur when taking low molecular weight heparin (LMWH).
In most cases, you’ll be given low molecular weight heparin (LMWH) because it’s easier to use and causes fewer side effects.
Warfarin
Warfarin is taken as a tablet. (Coumadin® is a common brand name for warfarin.) Your doctor may treat you with both heparin and warfarin at the same time. Heparin acts quickly. Warfarin takes 2 to 3 days before it starts to work. Once the warfarin starts to work, the heparin is stopped. You may need to take it after initial treatment with heparin to prevent further blood clots occurring. Your doctor may recommend that you take warfarin for three to six months. In some cases, it may need to be taken for longer, even for life.
As with standard heparin, the effects of warfarin vary from person to person. You’ll need to be closely monitored by having frequent blood tests to ensure you’re taking the right dosage.
When you first start taking warfarin, you may need to have two to three blood tests a week until your regular dose is decided. After this, you should only need to have a blood test every four weeks at an anticoagulant outpatient clinic.
Warfarin can be affected by your diet, any other medicines you’re taking and by how well your liver is working.
If you’re taking warfarin you should:
- keep your diet consistent
- limit the amount of alcohol you drink (no more than 14 units of alcohol a week)
- take your dose of warfarin at the same time every day
- not start to take any other medicine without checking with your GP, pharmacist or anticoagulant specialist
- not take herbal medicines
Warfarin isn’t recommended for pregnant women who are given heparin injections for the full length of treatment. Pregnant women usually are treated with just heparin.
Treatment for DVT using blood thinners usually lasts for 6 months. The following situations may change the length of treatment:
- If your blood clot occurred after a short-term risk (for example, surgery), your treatment time may be shorter.
- If you’ve had blood clots before, your treatment time may be longer.
- If you have certain other illnesses, such as cancer, you may need to take blood thinners for as long as you have the illness.
Rivaroxaban
Rivaroxaban (Xarelto) is a medication recommended by the National Institute for Health and Care Excellence 1 as a possible treatment for adults with DVT or to help prevent recurrent DVT and pulmonary embolism.
Rivaroxaban is indicated for the ‘treatment of deep vein thrombosis (DVT), and prevention of recurrent DVT and pulmonary embolism (PE) following an acute DVT in adults’. For the initial treatment of acute deep vein thrombosis, the recommended dosage of rivaroxaban is 15 mg twice daily for the first 21 days followed by 20 mg once daily for continued treatment and prevention of recurrence.
Rivaroxaban comes in tablet form. It’s a type of anticoagulant known as a directly acting oral anticoagulant (DOAC). It prevents blood clots forming by inhibiting a substance called factor Xa and restricting the formation of thrombin (an enzyme that helps blood clot).
Treatment usually lasts three months and involves taking rivaroxaban twice a day for the first 21 days and then once a day until the end of the course.
The duration of treatment recommended in the summary of product characteristics depends on bleeding risk and other clinical criteria: short-term treatment (3 months) is recommended for those with transient risk factors such as recent surgery and trauma, and longer treatment for permanent risk factors or idiopathic (unprovoked) deep vein thrombosis. The summary of product characteristics further states that experience with rivaroxaban in this indication for more than 12 months is limited. A reduced dosage of 15 mg twice daily for 21 days followed by 15 mg once daily should be used in people with moderate (creatinine clearance 30–49 ml/min) or severe (creatinine clearance 15–29 ml/min) renal impairment. For full details of side effects and contraindications, see the summary of product characteristics 2.
Apixaban
National Institute for Health and Care Excellence 3 also recommends apixaban (Eliquis) as a possible method of treatment and prevention for DVT and pulmonary embolism.
Like rivaroxaban, apixaban is a directly acting oral anticoagulant that’s taken orally as a tablet, and prevents blood clots forming by hindering factor Xa and restricting the formation of thrombin.
Treatment usually lasts at least three months and involves taking apixaban twice a day.
To treat deep vein thrombosis (DVT) or pulmonary embolism (PE), 10 mg apixaban should be taken twice a day for the first 7 days, followed by 5 mg twice a day for at least 3 months. For the prevention of recurrent disease, people who have completed 6 months of treatment for DVT or PE should take 2.5 mg twice a day. The summary of product characteristics states that apixaban should be used with caution in people with severe renal impairment.
The most frequent adverse reactions to apixaban are bleeding, bruising, nausea and anaemia. For full details of adverse reactions and contraindications, see the summary of product characteristics 2.
Inferior vena cava filters
If you can’t take blood thinners or they’re not working well, your doctor may recommend a vena cava filter.
Inferior vena cava (IVC) filters are sometimes used as an alternative to anticoagulant medicines. This is usually because anticoagulant treatment needs to be stopped, isn’t suitable or isn’t working.
Inferior vena cava (IVC) filters are small mesh devices that can be placed inside a large vein called the inferior vena cava. The filter catches large fragments of a blood clot and stop it traveling to the heart and lungs, which prevents pulmonary embolism. However, the filter doesn’t stop new blood clots from forming.
Inferior vena cava (IVC) filters can be placed in the vein permanently, or newer types of filters can be placed temporarily and removed after the risk of a blood clot has decreased.
The procedure to insert an IVC filter is carried out using a local anaesthetic (where you’re awake but the area is numb). A small cut is made in the skin and a catheter (a thin, flexible tube) is inserted into a vein in the neck or groin area. The catheter is guided using an ultrasound scan. The IVC filter is then inserted through the catheter and into the vein.
Thrombolytics
In some cases, your doctor may recommend using thrombolytics. These clot-dissolving medications are injected via a catheter directly into the blood clot and are used only when there is an extremely high risk for pulmonary embolism.
Compression stockings
If you have had DVT, you should NOT be offered special stockings, called compression stockings, to stop you getting it again or to stop you from getting post-thrombotic syndrome. This is because it isn’t clear if stockings help prevent these conditions.
Your healthcare team may still offer you stockings to treat your DVT or post-thrombotic syndrome symptoms, if they think it will help.
Graduated compression stockings can reduce leg swelling caused by a blood clot. These stockings are worn on the legs from the arch of the foot to just above or below the knee.
Compression stockings are tight at the ankle and become looser as they go up the leg. This creates gentle pressure up the leg. The pressure keeps blood from pooling and clotting.
There are three types of compression stockings.
- One type is support pantyhose, which offer the least amount of pressure.
- The second type is over-the-counter compression hose. These stockings give a little more pressure than support pantyhose. Over-the-counter compression hose are sold in medical supply stores and pharmacies.
- Prescription-strength compression hose offer the greatest amount of pressure. They also are sold in medical supply stores and pharmacies. However, a specially trained person needs to fit you for these stockings.
Talk with your doctor about how long you should wear compression stockings.
Pneumatic compression device
Your doctor may recommend that you use an external pneumatic compression device after surgery. This device, which is worn like a boot, applies pulsing pressures to the calf. This pressure is similar to that which you experience while you are walking. Compression devices not only improve venous blood flow but also stimulate the body’s own ability to prevent blood clots.
Exercise
Your healthcare team will usually advise you to walk regularly. This can help prevent symptoms of DVT returning and may help to improve or prevent complications of DVT, such as post-thrombotic syndrome.
Raising your leg
You might be advised to raise your leg whenever you’re resting. This helps to relieve the pressure in the veins of the calf and stops blood and fluid pooling in the calf itself.
When raising your leg, make sure your foot is higher than your hip. This will help the returning blood flow from your calf. Putting a cushion underneath your leg while you’re lying down should help raise your leg above the level of your hip.
You can also slightly raise the end of your bed to ensure that your foot and calf are slightly higher than your hip.
Living With Deep Vein Thrombosis
If you’ve had a deep vein blood clot, you’re at greater risk for another one. During treatment and after:
- Take steps to prevent deep vein thrombosis (DVT). (For more information, go to “How Can Deep Vein Thrombosis Be Prevented?”)
- Check your legs for signs of DVT. These include swollen areas, pain or tenderness, increased warmth in swollen or painful areas, or red or discolored skin on the legs.
- Contact your doctor right away if you have signs or symptoms of DVT.
Ongoing Health Care Needs
DVT often is treated with blood-thinning medicines. These medicines can thin your blood too much and cause bleeding (sometimes inside the body). This side effect can be life threatening.
Bleeding can occur in the digestive system or the brain. Signs and symptoms of bleeding in the digestive system include:
- Bright red vomit or vomit that looks like coffee grounds
- Bright red blood in your stools or black, tarry stools
- Pain in your abdomen
Signs and symptoms of bleeding in the brain include:
- Severe pain in your head
- Sudden changes in your vision
- Sudden loss of movement in your arms or legs
- Memory loss or confusion
If you have any of these signs or symptoms, seek medical care right away. If you have a lot of bleeding after a fall or injury, call your local emergency number. This could be a sign that your DVT medicines have thinned your blood too much.
You might want to wear a medical ID bracelet or necklace that states you’re at risk of bleeding. If you’re injured, the ID will alert medical personnel of your condition.
Talk with your doctor before taking any medicines other than your DVT medicines. This includes over-the-counter medicines. Aspirin, for example, also can thin your blood. Taking two medicines that thin your blood may raise your risk of bleeding.
Ask your doctor about how your diet affects these medicines. Foods that contain vitamin K can change how warfarin (a blood-thinning medicine) works. Vitamin K is found in green, leafy vegetables and some oils, like canola and soybean oils. Your doctor can help you plan a balanced and healthy diet.
Discuss with your doctor whether drinking alcohol will interfere with your medicines. Your doctor can tell you what amount of alcohol is safe for you.
- Rivaroxaban for the treatment of deep vein thrombosis and prevention of recurrent deep vein thrombosis and pulmonary embolism. https://www.nice.org.uk/guidance/ta261/chapter/1-Guidance[↩]
- https://www.nice.org.uk/guidance/ta341/chapter/3-The-companys-submission[↩][↩]
- Apixaban for the treatment and secondary prevention of deep vein thrombosis and/or pulmonary embolism. https://www.nice.org.uk/guidance/ta341/chapter/2-The-technology[↩]