Contents
What is Eisenmenger syndrome
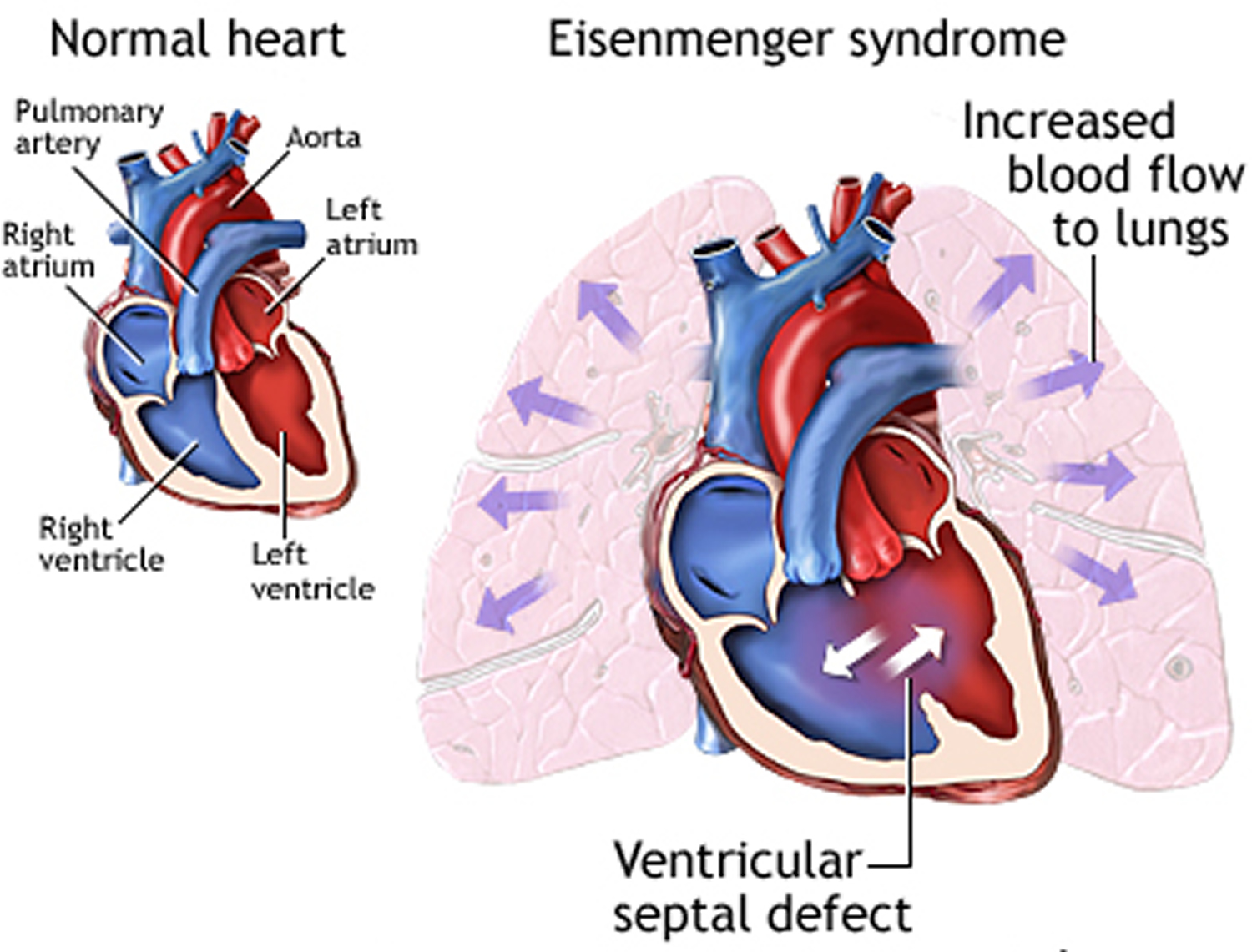
Eisenmenger syndrome is a rare progressive heart condition that develops in some individuals with structural malformations of the heart that are present from birth (congenital heart defects). A heart defect that causes a hole (shunt) to develop between two chambers of your heart is the most common cause of Eisenmenger syndrome. Children born with Eisenmenger syndrome are born with a hole between the two pumping chambers — the left and right ventricles — of the heart (ventricular septal defect). The hole allows blood that has already picked up oxygen from the lungs to flow back into the lungs, instead of going out to the rest of the body. Increased blood flow returns to your lungs instead of going to the rest of your body. The increased blood flow and high pressure damages the small blood vessels in the lungs. The blood vessels in your lung arteries become stiff and narrow, increasing the pressure in your lungs’ arteries. This permanently damages the blood vessels in your lungs.
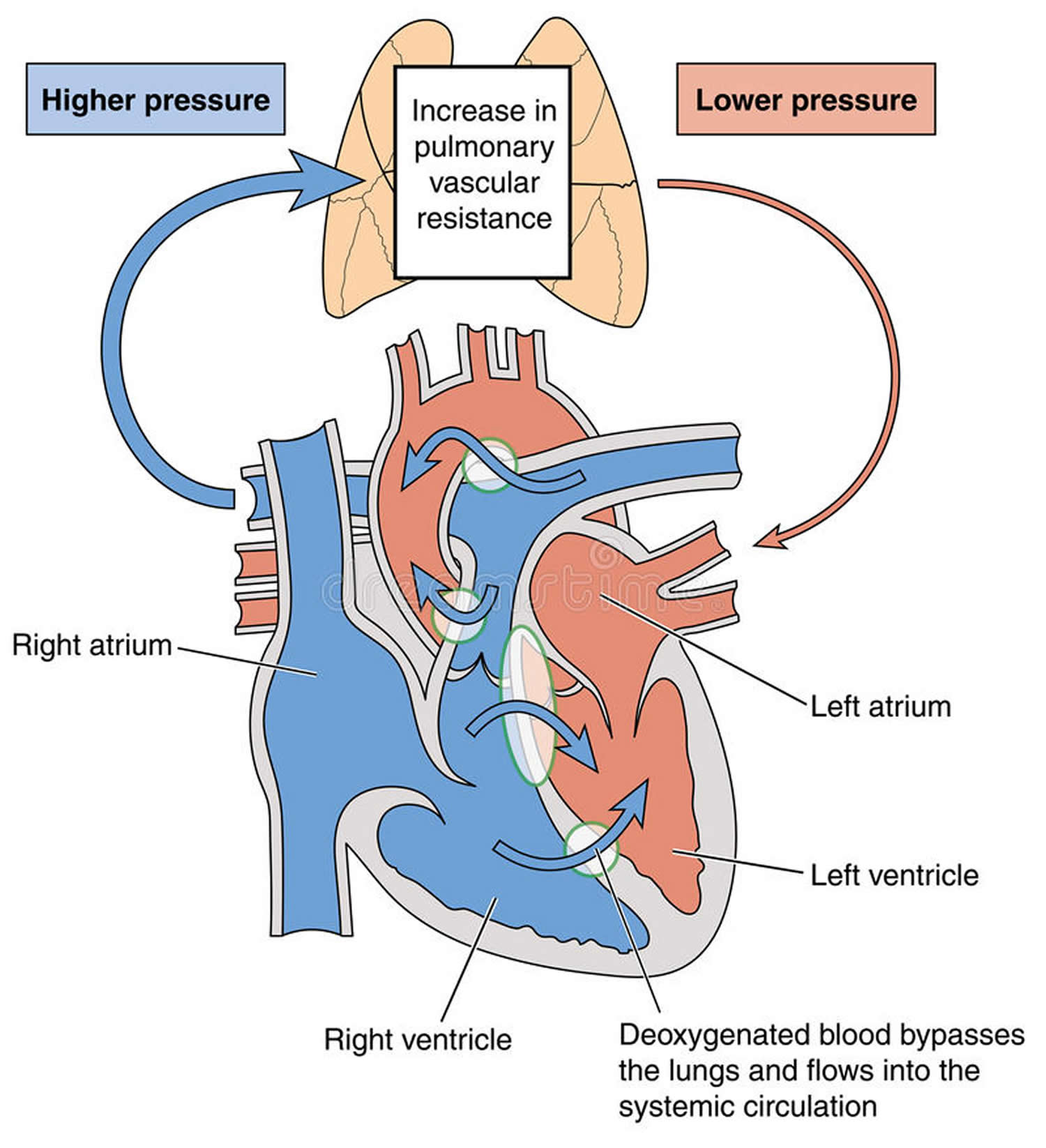
Eisenmenger syndrome is characterized by congenital heart defects with the combination of pulmonary hypertension (elevated pulmonary arterial pressure and pulmonary vascular resistance) and right-to-left shunting of the blood within the heart. Pulmonary hypertension is high blood pressure in the pulmonary arteries to your lungs. Pulmonary hypertension is a serious condition. If you have it, the blood vessels (pulmonary arteries) that carry blood from your heart to your lungs become hard and narrow. Your heart has to work harder to pump the blood through. Over time, your heart weakens and cannot do its job and you can develop heart failure.
The first clinical description of Eisenmenger syndrome originates from the Viennese physician Victor Eisenmenger in 1897 1, where he reported on a 32-year-old man with cyanosis and dyspnea since infancy. This patient had a reasonably active life until 3 years before his death, when dyspnea increased and right heart failure began. He succumbed suddenly after massive hemoptysis. Autopsy revealed a nonrestrictive membranous malalignment ventricular septal defect (VSD), marked right ventricular hypertrophy, an overriding aorta, and atheromatosis of the major pulmonary arteries 1.
Eisenmenger syndrome is a life-threatening condition requiring careful medical monitoring. Eisenmenger syndrome occurs when the increased pressure of the blood flow in the lung becomes so great that the direction of blood flow through the shunt reverses. Oxygen-poor (blue) blood from the right side of the heart flows into the left ventricle and is pumped to your body so you don’t receive enough oxygen to all your organs and tissues. Medications can improve symptoms and prognosis.
Eisenmenger syndrome appears to affect males and females in relatively equal numbers. Experts indicate that the incidence of Eisenmenger syndrome has decreased due to prevention of prolonged pulmonary hypertension by early surgical correction of certain congenital defects (e.g., large ventricular septal defects). The prevalence of Eisenmenger syndrome is not known. According to historical data, approximately 8 percent of individuals with congenital heart disease and 11 percent of those with left-to-right shunts develop Eisenmenger syndrome 2.
Eisenmenger syndrome signs and symptoms include:
- Bluish or grayish skin color (cyanosis)
- Large, rounded fingernails or toenails (clubbing)
- Easily tiring and shortness of breath with activity
- Shortness of breath while at rest
- Chest pain or tightness
- Skipped or racing heartbeats (palpitations)
- Fainting (syncope)
- Coughing up blood (hemoptysis)
- Dizziness
- Numbness or tingling in the fingers or toes
- Headaches
- Abdominal swelling
Eisenmenger syndrome is a life-threatening condition. The clinical presentation of Eisenmenger syndrome includes central cyanosis, dyspnea (shortness of breath), fatigue, syncope (fainting), and right heart failure 3. The survival of patients with Eisenmenger syndrome is reduced in comparison to patients with simple congenital heart disease without Eisenmenger syndrome. The prognosis for people diagnosed with Eisenmenger syndrome depends on the type of congenital heart defect and other medical conditions. According to a large cohort of patients with adult congenital heart disease in the UK, the median life expectancy of patients with Eisenmenger syndrome is 42 years 4. What median survival means is that the chance of surviving beyond 42 years of age is 50 percent. There are people who are diagnosed with Eisenmenger syndrome who can survive as long as age 50 to 60 and sometimes longer. Hemoptysis is a frequent complication and a major cause of mortality in Eisenmenger syndrome 3. The management of hemoptysis (coughing up blood) is important for patients with Eisenmenger syndrome because the frequency increases with age, with almost all patients experiencing hemoptysis by their forties 5.
Eisenmenger syndrome in pregnancy
According to experts, due to the demands pregnancy puts on a mother’s heart and lungs, women who have Eisenmenger syndrome shouldn’t become pregnant. Pregnancy for a woman who has Eisenmenger syndrome poses a high risk of death for both the mother and baby.
Eisenmenger syndrome in adults
The natural historyof Eisenmenger syndrome is comprised of a long symptom-free time period. Patients have adjusted to a lower exercise capacity since childhood. Patients may even do well throughout adolescence and early adulthood. Many become symptomatic during their 30s and gradually develop complaints and complications, particularly cyanosis, exercise intolerance, dyspnea upon exertion, syncope, chest pain, stroke or brain abscesses, right sided congestive heart failure, hyperviscosity complications, pulmonary hemorrhage/ hemoptysis and endocarditis 6. Rhythm disturbances, particularly atrial fibrillation, corresponds to clinical deterioration and right heart failure. According to historical data, patients with Eisenmenger syndrome usually die between 30 and 35 years 7. However, survival to late adulthood has been reported.
Importantly, prognosis of patients with spontaneous Eisenmenger syndrome is by far better than the prognosis of patients with idiopathic forms of pulmonary arterial hypertension, although there are many similarities regarding the histological changes 8. The ventricular remodeling in patients with Eisenmenger syndrome differs from that in patients with idiopathic pulmonary hypertension 9. The better prognosis of Eisenmenger patients is believed to be to the fact that the subpulmonary ventricle has been exposed to high pressures and has been primed since birth; it is better adapted because of the long-standing volume and pressure overload. Furthermore, regression of the physiologic right ventricular hypertrophy does not occur and the right-to-left shunt serves as an excess flow valve.
The actuarial survival rate is 80% at 10 years, 77% at 15 years 42% at 25 years 10. Most Eisenmenger syndrome patients die from sudden cardiac death, congestive heart failure, hemoptysis, cerebral abscesses, thromboembolic events, from complications during pregnancy or due to noncardiac surgery 11.
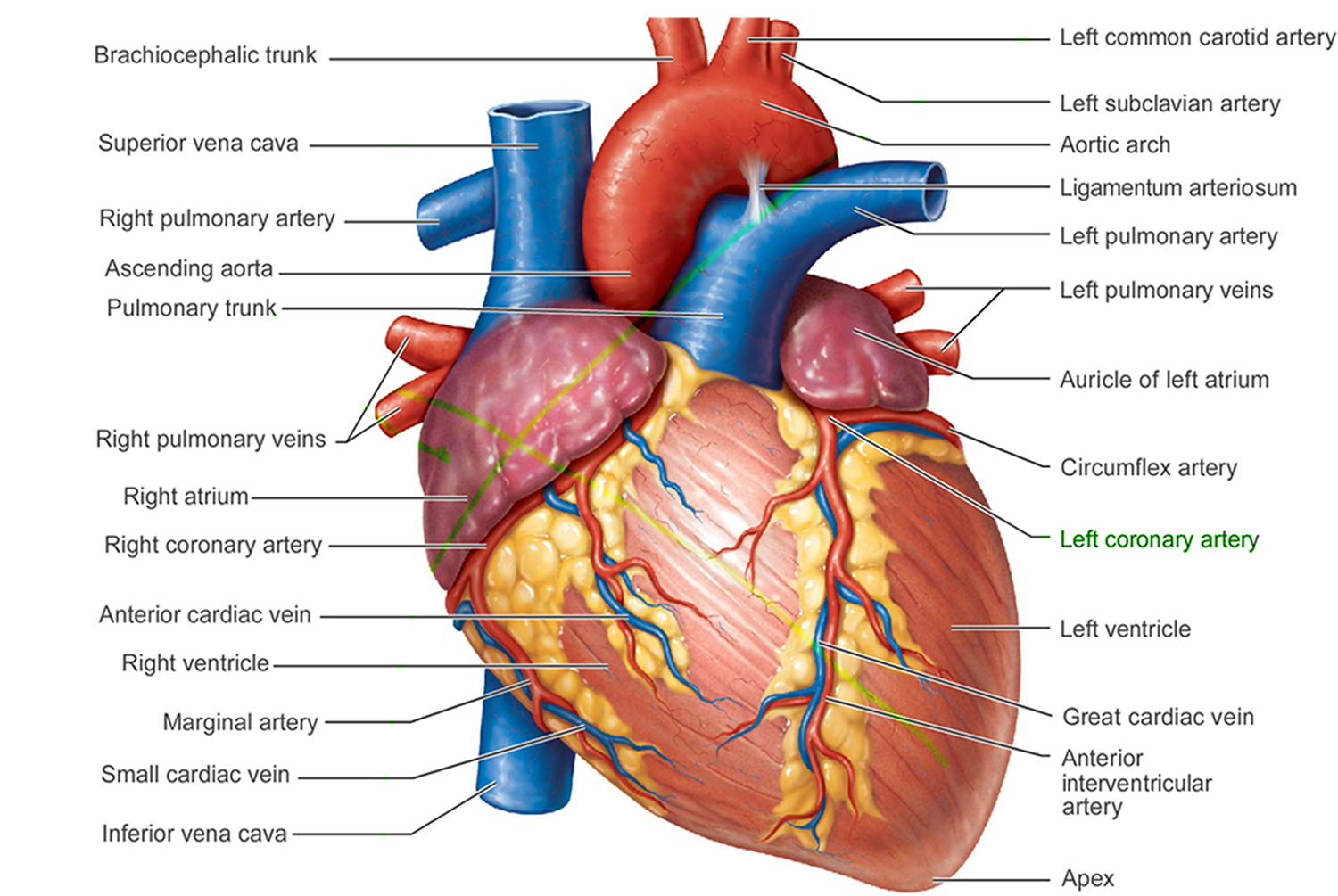
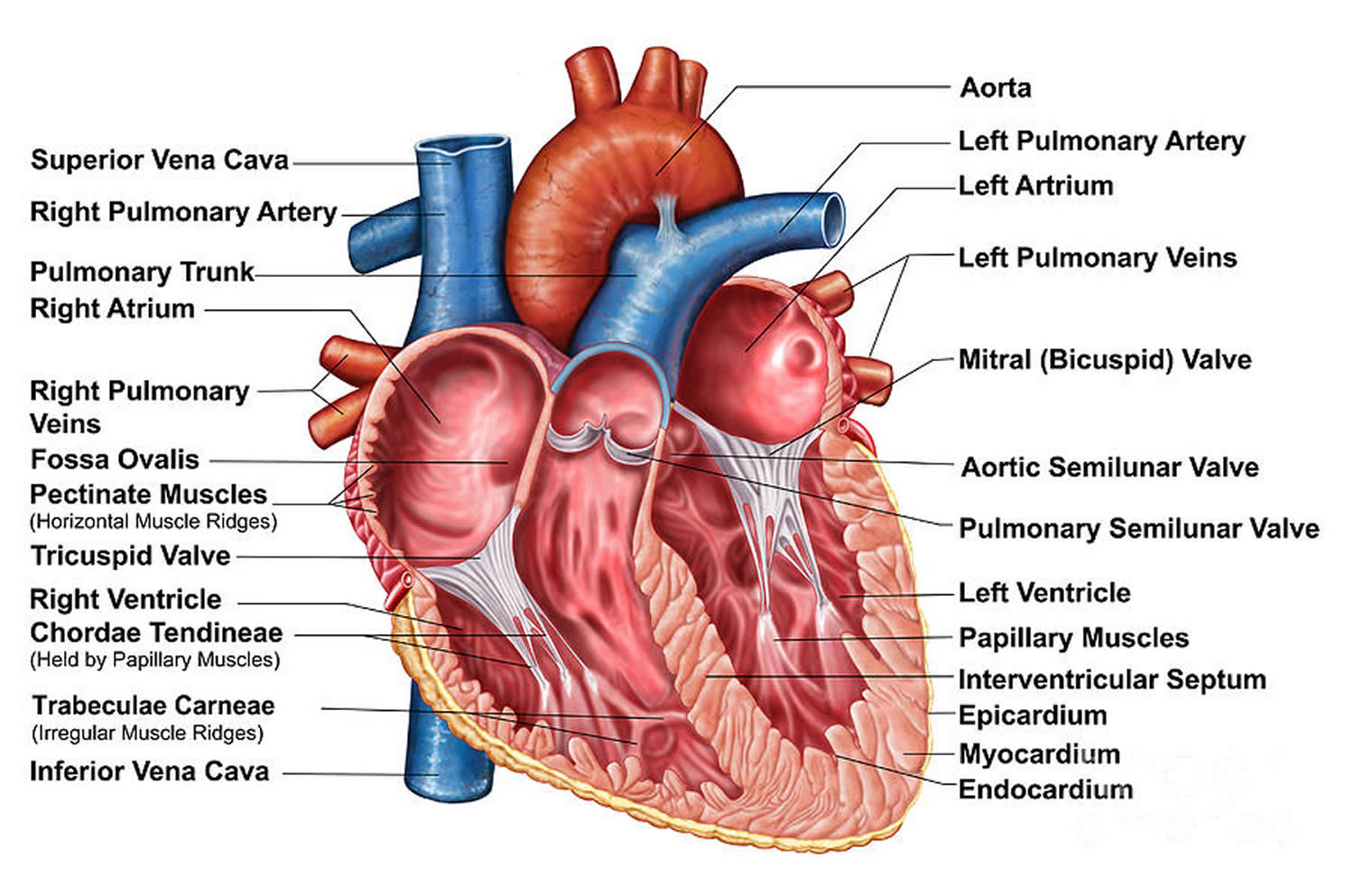
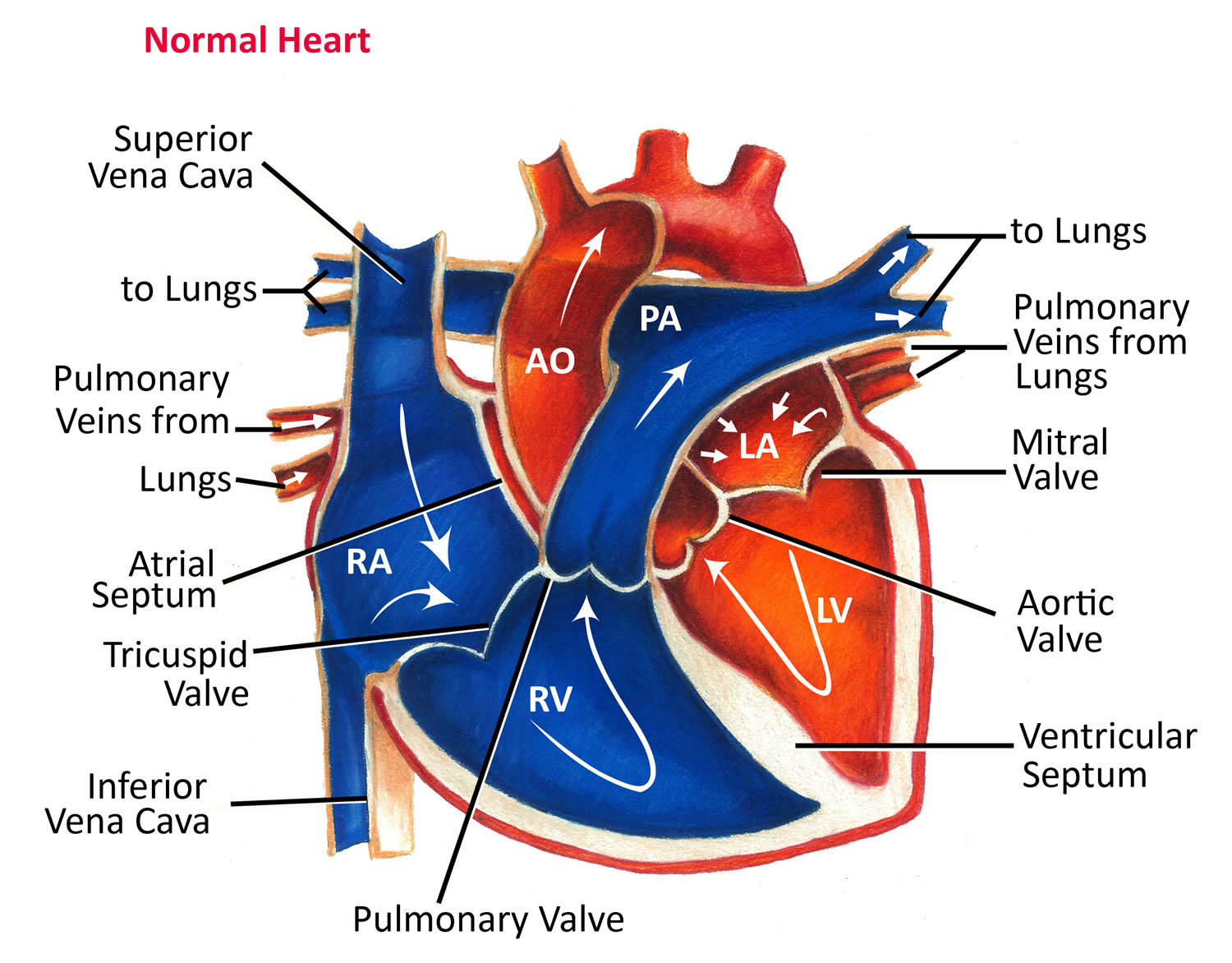
Human heart
The normal heart has four chambers. The two upper chambers, known as atria, are separated from each other by a fibrous partition known as the atrial septum. The two lower chambers are known as ventricles and are separated from each other by the ventricular septum. Valves connect the atria (left and right) to their respective ventricles. The valves allow for blood to be pumped through the chambers. Blood travels from the right ventricle through the pulmonary artery to the lungs where it receives oxygen. The blood returns to the heart through pulmonary veins and enters the left ventricle. The left ventricle sends the now oxygen-filled blood into the main artery of the body (aorta). The aorta sends the blood throughout the body.
Figure 1. The anatomy of the heart
Figure 2. The anatomy of the heart chambers
Figure 3. Normal heart blood flow
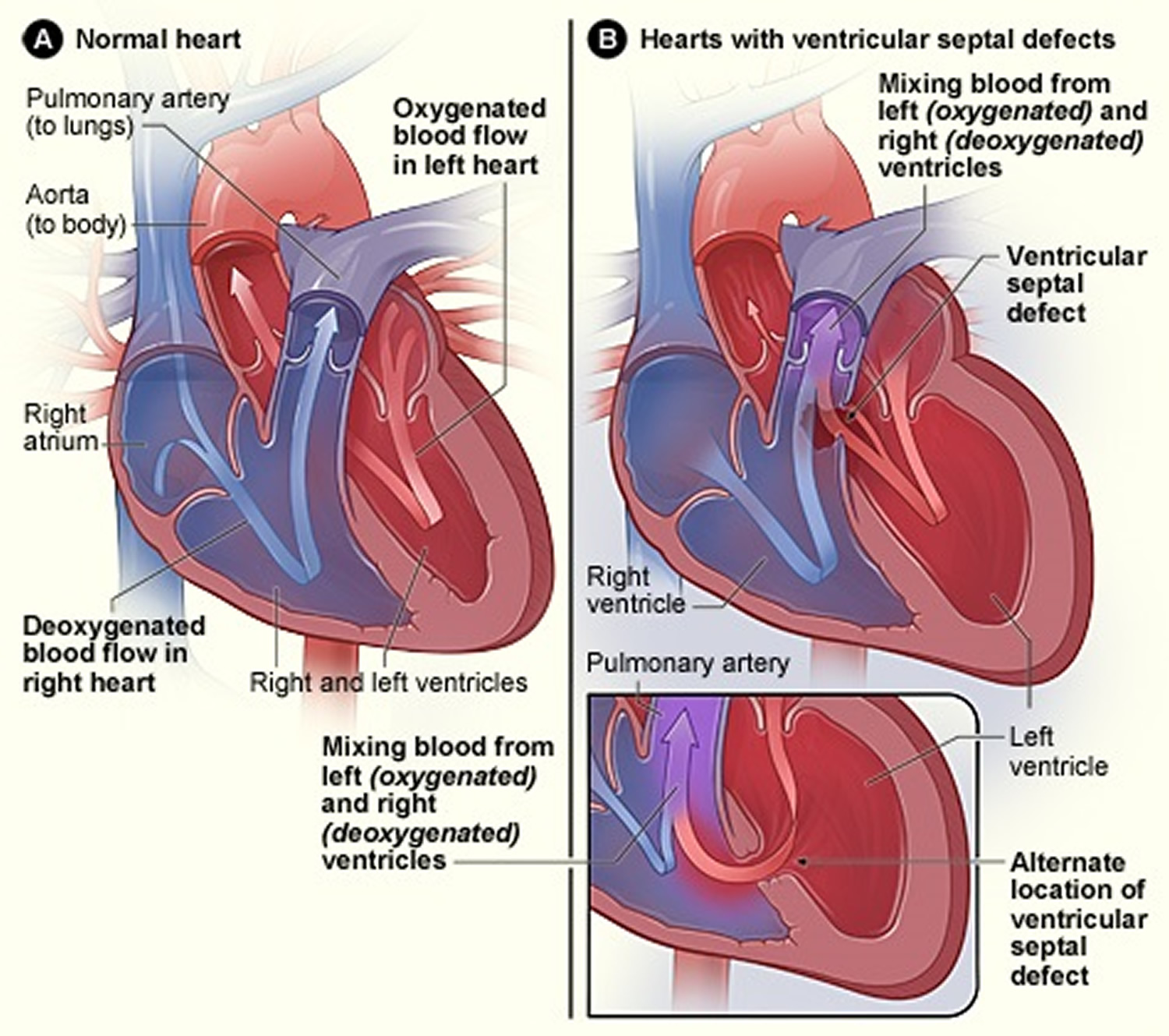
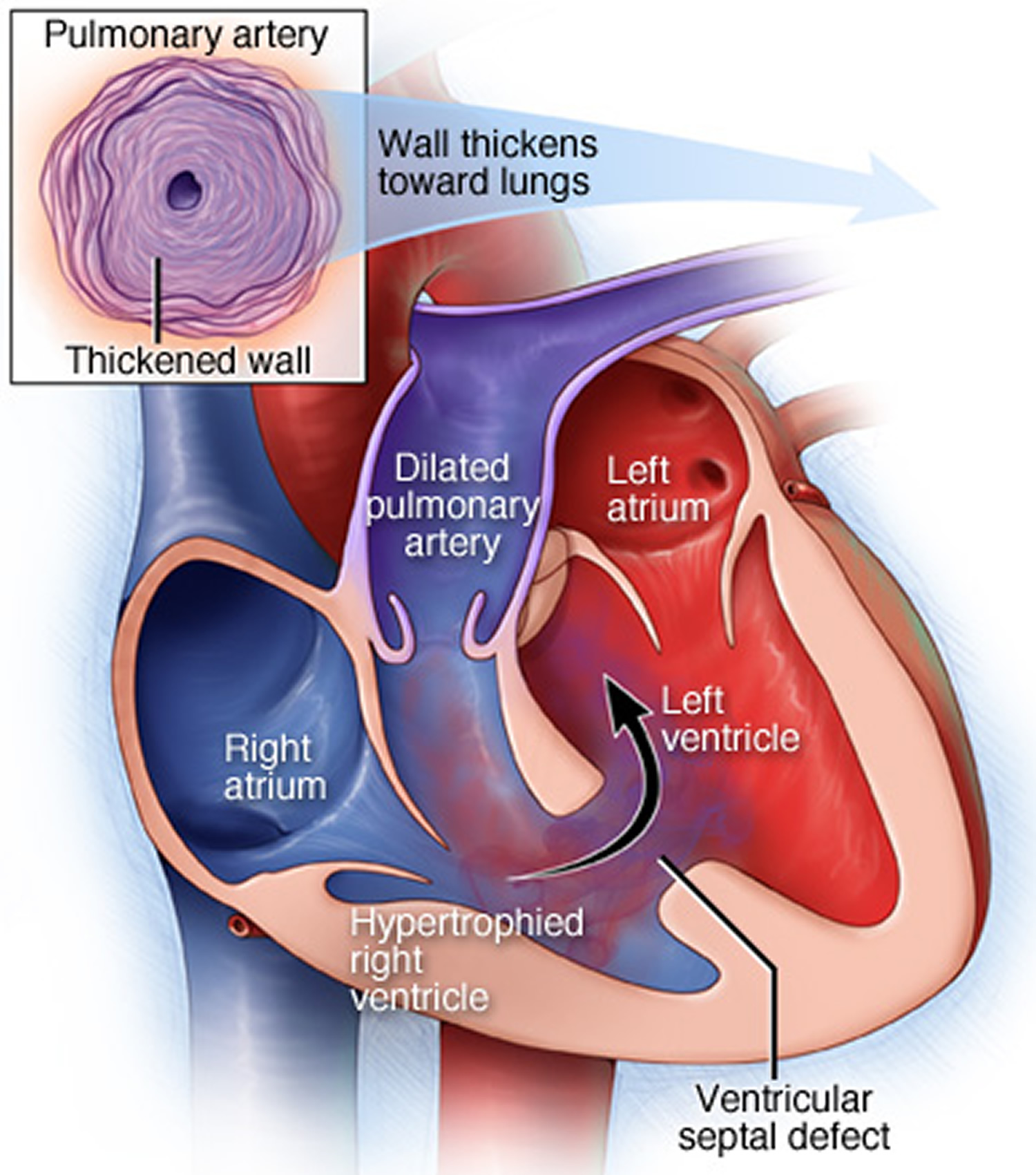
The most common congenital heart defect associated with Eisenmenger syndrome is a ventricular septal defect (VSD) or a “hole in the heart” between the two lower chambers of the heart (left ventricle and right ventricle. This defect allows blood to flow from the left ventricle into the right ventricle (left-to-right shunt). The shunt causes increased blood flow into the lungs eventually resulting in pulmonary hypertension, which causes progressive damage to the small blood vessels in lungs (pulmonary vascular disease). As the damage continues, pulmonary hypertension increases and the small blood vessels become thickened or blocked hampering the flow of blood. Ultimately, blood flow is reversed back through the shunt so that blood flows from the right ventricle into the left ventricle (right-to-left shunt) bypassing the lungs completely. A variety of symptoms including life-threatening complications may occur.
Figure 4. Heart with a Ventricular Septal Defect
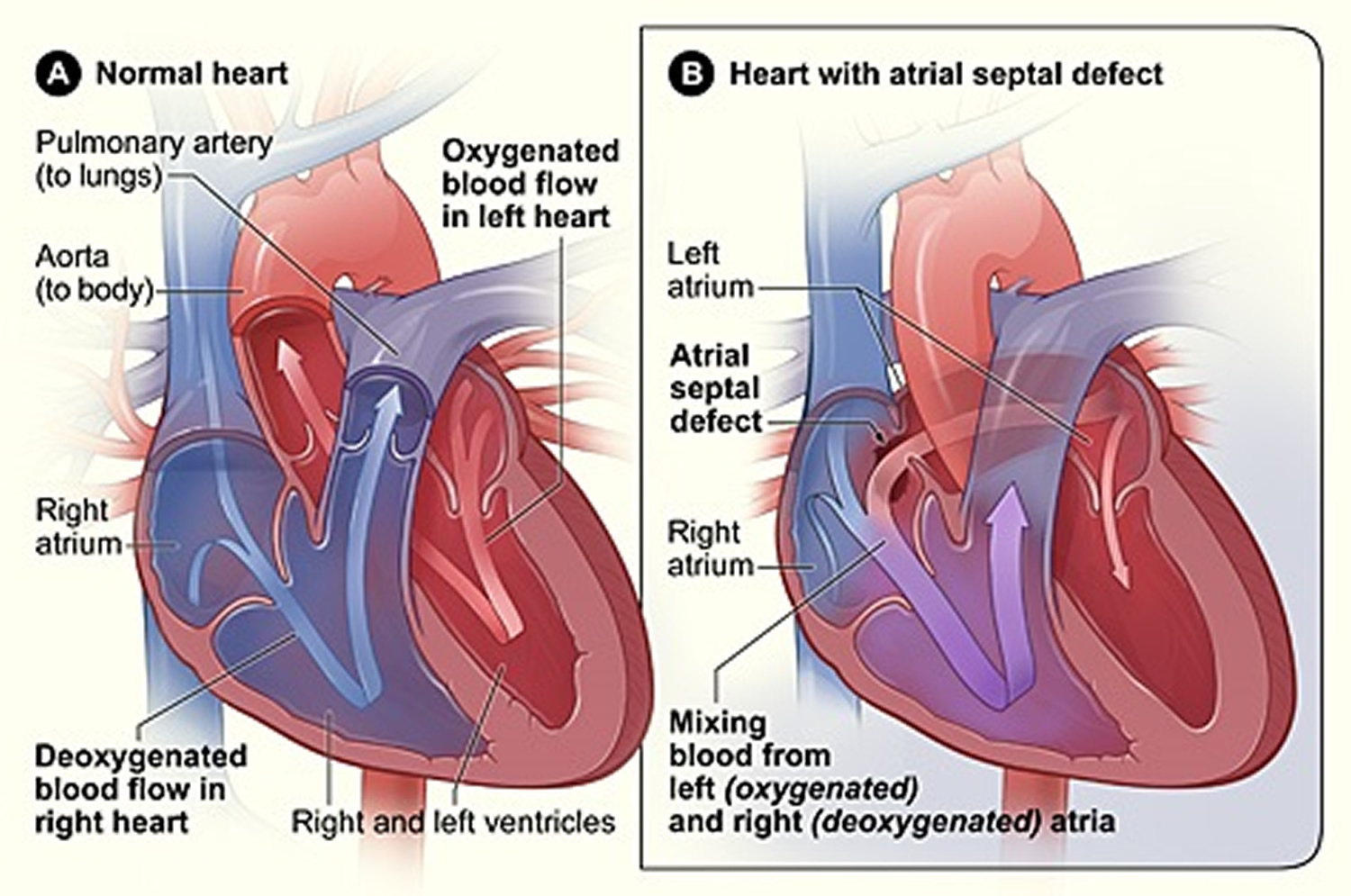
Figure 5. Heart With an Atrial Septal Defect
Figure 6. Heart defect in Eisenmenger syndrome
Figure 7. Eisenmenger syndrome
Eisenmenger syndrome complications
Without proper treatment and monitoring, you can develop complications of Eisenmenger syndrome, including:
- Low oxygen levels in your blood (cyanosis). The reversed blood flow through your heart lowers the amount of oxygen your body’s tissues and organs receive. This causes you to have a lower tolerance for physical activity and your skin to have a bluish or a grayish color. Cyanosis will worsen over time.
- High red blood cell count (erythrocytosis). Because you aren’t getting enough oxygen-rich blood circulating throughout your body, your kidneys release a hormone that increases your number of red blood cells, the cells that carry oxygen throughout your body. Having too many red blood cells can reduce the blood flow to other organs and increase your risk of developing blood clots.
- Arrhythmias. Enlargement and thickening of the walls in the heart, along with low oxygen levels, may cause an irregular heart rhythm (arrhythmia). Some types of arrhythmias can cause blood to pool in your heart’s chambers, where it can clot. If the clot travels out of your heart and blocks an artery, you can have a heart attack or stroke.
- Sudden cardiac arrest. If you develop an arrhythmia as a complication of Eisenmenger syndrome, it’s possible the arrhythmia could suddenly stop your heartbeat. Sudden cardiac arrest is the sudden, unexpected loss of heart function, breathing and consciousness. Without immediate medical attention, you can die of sudden cardiac arrest in minutes. You can also go into cardiac arrest during surgical procedures, usually related to changes in blood pressure caused by anesthesia.
- Heart failure. The increased pressure in your heart can cause your heart muscles to weaken, decreasing its pumping effectiveness. Eventually, this can lead to heart failure.
- Coughing up blood (hemoptysis). Increased pressure in the lungs and problems with your blood caused by Eisenmenger syndrome can cause life-threatening bleeding into your lungs and airways, causing you to cough up blood and further lowering your blood oxygen level. Bleeding can also occur in other parts of the body.
- Stroke. Stoke can occur when a blood clot travels from the right to left side of the heart without being filtered out by your lungs. This blood clot may then block a blood vessel in the brain, leading to a stroke. The high levels of red blood cells in Eisenmenger syndrome also increase your risk of blood clots and stroke.
- Kidney problems. Low oxygen levels in your blood may lead to problems with your kidneys. This can also increase your risk of developing gout.
- Pregnancy risks. Due to the demands pregnancy puts on a mother’s heart and lungs, women who have Eisenmenger syndrome shouldn’t become pregnant. Pregnancy for a woman who has Eisenmenger syndrome poses a high risk of death for both the mother and baby.
Eisenmenger syndrome causes
For most people who have Eisenmenger syndrome, the cause of their condition is due to a hole (shunt) between the main blood vessels or chambers of your heart. This shunt is a heart defect you’re born with (congenital). Heart defects that can cause Eisenmenger syndrome include:
- Ventricular septal defect. This shunt in the wall of tissue that divides the right and left sides of your heart’s main pumping chambers (ventricles) is the most common cause of Eisenmenger syndrome.
- Atrial septal defect. An atrial septal defect is a shunt in the wall of tissue that divides the right and left sides of the upper chambers of your heart (atria).
- Patent ductus arteriosus. This heart defect is an opening between the pulmonary artery that carries oxygen-poor blood to the lungs and the artery that carries oxygen-rich blood to the rest of your body (aorta).
- Atrioventricular canal defect. In this heart defect, there’s a large hole in the center of the heart where the walls between the upper chambers (atria) and lower chambers (ventricles) meet. Some of the valves in your heart also may not function properly.
Eisenmenger syndrome results as a complication of certain congenital defects in which there is abnormal connection (communication) between particular heart regions or arteries (e.g., aorta and pulmonary artery). In most cases, this progressive condition occurs secondary to ventricular septal defects (VSDs) in which there is an abnormal opening in the fibrous partition (septum) that normally separates the two lower heart chambers (ventricles). A VSD allows the abnormal passage of blood between the two ventricles: Because there is normally higher pressure in the left ventricle, blood flows from the left to the right ventricle (left-to-right shunt). This increases the amount of blood flow to the lungs and leads to gradually increasing blood pressure (hypertension) in the pulmonary artery, which carries oxygen-poor (deoxygenated) blood to the lungs where the exchange of oxygen and carbon dioxide takes place.
Without early surgical correction of the underlying defect, pulmonary hypertension eventually damages small arteries (e.g., pulmonary arterioles) in lung tissue (pulmonary vascular disease), resulting in abnormal thickening, stiffness, and potential blockage of such blood vessels. These changes lead to increasing resistance to blood flow and elevating pressure in the right ventricle as it works to pump blood to the lungs. Pressure within the right ventricle may eventually equal or surpass that of the left ventricle, reversing the flow of blood through the septal defect from the right to the left ventricle (reversed or right-to-left shunt). As a result, deoxygenated blood that normally is passed on to the lungs to receive oxygen instead is pushed into the left ventricle and through the major artery of the body (aorta) for circulation to the body’s tissues, leading to insufficient oxygen supply to body cells (hypoxia), bluish discoloration of the skin and mucous membranes (cyanosis). Your red blood cell count increases to try to make up for the lack of oxygen.
The changes associated with this progressive syndrome may also occur as a complication of other congenital defects. These may include an abnormal opening in the septum that separates the upper heart chambers (atrial septal defects), combined atrial and ventricular septal defects (atrioventricular or endocardial cushion defects), or patent ductus arteriosus (PDA). In patent ductus arteriosus, the channel that is present between the aorta and the pulmonary artery during fetal development fails to close after birth. As a result, some of the oxygenated blood that is normally circulated to the body via the aorta is instead returned to the lungs. In those with a large PDA, the defect may lead to increased pulmonary arterial pressure (pulmonary hypertension) and, without early surgical correction, an increased risk of developing pulmonary vascular disease and Eisenmenger syndrome. Changes associated with Eisenmenger syndrome may also occur due to other congenital defects in which there is abnormal communication between the aorta and pulmonary artery.
Eisenmenger syndrome occurs when a congenital heart defect is not detected early enough to be treated before damage to the lung arteries occurs. If you or your child receives a diagnosis of a heart defect, it’s important to start treatment promptly, including having surgeries or procedures to help correct the defect.
A family history of heart defects also increases the risk of a baby developing a congenital heart defect, including the possibility of developing Eisenmenger syndrome. Talk to your doctor about screening other family members for heart defects if you’ve been diagnosed with a heart defect or Eisenmenger syndrome.
Eisenmenger syndrome symptoms
The specific symptoms of Eisenmenger syndrome vary greatly from case to case. Symptoms and signs often do not occur until about the second or third decade of life; however, they may develop more rapidly in some cases. Most symptoms result from insufficient oxygen supply to body cells (hypoxia).
The most notable symptom is often bluish discoloration of the skin and mucous membranes (cyanosis). Individuals with Eisenmenger syndrome typically develop intensification of cyanosis, particularly of the lips, fingernails, and toenails, and elevated levels of the blood cells (red blood cells or erythrocytes) that transport oxygen to body cells (i.e., polycythemia) due to increasingly inadequate oxygen supply to body tissues. Additional signs may include broadening of the tips of the fingers and toes (clubbing), increasing difficulties breathing (dyspnea), fatigue, lethargy, abnormal heart rhythms (arrhythmias); or additional findings. The degree of cyanosis and polycythemia varies, depending upon the duration and severity of hypoxia.
With disease progression, affected individuals develop an impaired ability of the heart to circulate adequate amounts of blood to the lungs and to the rest of the body (heart failure). Additional associated findings may include excessive accumulation of fluid in certain body tissues (edema), causing swelling of the ankles and legs; chest pain (angina pectoris), palpitations; fainting episodes (syncope) due to insufficient oxygen supply to the brain, headaches; coughing up of blood (hemoptysis); and/or other abnormalities, potentially leading to life-threatening complications such as stroke or organ failure.
Additional symptoms that may be associated with Eisenmenger syndrome include low levels of circulating red blood cells due to lack of iron (iron deficiency anemia), an increased risk of developing blood clots, prolonged bleeding, kidney disease and a condition known as tricuspid valve regurgitation. The tricuspid valve connects the right atria to the right ventricle. In this condition, the valve does not close properly allowing blood to seep back into the atria. The symptoms associated with tricuspid valve regurgitation may include weakness, fatigue, generalized swelling especially of the feet, ankles or abdomen, or heart failure.
In some cases, during infancy and early childhood, some affected individuals may have symptoms due to the underlying congenital heart defect. The most common heart defect associated with Eisenmenger syndrome is a ventricular septal defect (VSD), in which an abnormal opening exists in the fibrous partition (septum) that normally separates the two lower heart chambers. Additional associated defects include atrial septal defects (ASD) in which an abnormal opening exists in the septum separating the two upper heart chambers, patent ductus arteriosus, a condition in which the passage (ductus) between the blood vessel that leads to the lungs (pulmonary artery) and the major artery of the body (aorta) fails to close after birth; or other more complicated congenital heart defects.
Symptoms due to a VSD may vary greatly, depending on the size of the VSD, pulmonary blood flow and pressure, and other factors. Those with small VSDs may have normal pulmonary arterial pressure and no apparent symptoms (asymptomatic). Small VSDs often close spontaneously. However, some affected infants and children with large VSDs may have multiple symptoms resulting from increased pulmonary blood flow and rising pulmonary blood pressure (pulmonary hypertension). Such findings may include feeding and breathing difficulties, profuse sweating, poor growth; recurrent lung infections, an impaired ability of the heart to pump blood effectively to the lungs and on to the rest of the body (heart failure), enlargement of the heart (cardiomegaly), abnormal heart sounds (heart murmurs) that may be detected by a physician through use of a stethoscope; and/or other findings. With increasing resistance to blood flow within small blood vessels in lung tissue, such symptoms may improve. However, affected children may have decreased stamina and develop relatively mild cyanosis or bluish discoloration of the skin and mucous membranes with exertion.
As noted above, symptoms of Eisenmenger syndrome often do not become apparent until about the second or third decade of life and may be slowly progressive over several years. However, in other cases, symptom onset may be more rapid and severe (fulminant).
Eisenmenger syndrome diagnosis
To diagnose Eisenmenger syndrome, your doctor will discuss your medical history, perform a physical examination and order appropriate diagnostic tests. These tests may include:
- Electrocardiogram (ECG). This test records the electrical activity of the heart through electrodes attached to the skin. This test helps diagnose heart defects that cause Eisenmenger syndrome.
- Chest X-ray. Your doctor may order a chest X-ray to look for heart and pulmonary artery enlargement.
- Echocardiogram. During an echocardiogram (ultrasound of the heart), sound waves create detailed images of your heart. This allows doctors to see the structure of your heart and blood flow through your heart to look for heart defects.
- Blood tests. Blood tests may be done to check your blood cell counts, which are often high in Eisenmenger syndrome. Your kidney and liver function, as well as your iron level, also may be measured with blood tests.
- Computerized tomography (CT) scan. In this test, you’ll lie in a machine that takes images of your lungs so that your doctors can see a cross-section of them. You might also be given dye that makes the images of your lungs show up more clearly.
- Magnetic resonance imaging (MRI). This test, which uses no X-rays, is sometimes used to get images of the blood vessels in your lungs. A computer creates tissue “slices” from data generated by a powerful magnetic field and radio waves.
- Cardiac catheterization. In this test, doctors insert a thin, flexible tube (catheter) into an artery in your groin and guide the catheter to your heart using X-ray imaging. Doctors use cardiac catheterization to measure blood pressure in your blood vessels or heart’s chambers, the size of any septal defect, the pressures across the defect, and the amount of blood in your heart and lungs. If you need to have cardiac catheterization done, make sure you choose a cardiologist who has expertise diagnosing and treating Eisenmenger syndrome.
- Walking test. Your doctor may order a six-minute walking test to check your tolerance to a mild level of exercise.
Eisenmenger syndrome treatment
Eisenmenger syndrome treatment is aimed at controlling your or your child’s symptoms and managing the condition. Although there’s no cure, medications may help you feel better, improve your quality of life and prevent serious complications.
Doctors don’t recommend surgery to repair the hole in your heart once Eisenmenger syndrome has developed, and any surgery may be life-threatening. It’s important that you’re treated by a doctor who has expertise in Eisenmenger syndrome.
Observation and monitoring
You’ll be monitored through regular visits with a congenital heart disease cardiologist. You should have an appointment with your cardiologist at least once a year. A typical evaluation generally includes a thorough review of complaints and symptoms, a physical exam, and blood tests.
Medications
Medications are the primary treatment option for Eisenmenger syndrome. You’ll need to be monitored closely by a doctor when taking medications for any changes in blood pressure, fluid volume or pulse rate.
Medications for Eisenmenger syndrome include:
- Medications to control arrhythmias. If you have an arrhythmia, you may receive medications to control your heart rhythms.
- Iron supplements. Your doctor may prescribe iron supplements if he or she finds your iron level is too low. Don’t start taking iron supplements without talking to your doctor first.
- Aspirin or other blood-thinning medications. If you have had a stroke, blood clot or certain types of irregular heart rhythms, your doctor may recommend aspirin or other blood thinners such as warfarin (Coumadin, Jantoven). However, people who have Eisenmenger syndrome are also at increased risk of bleeding when taking these medications, so don’t take any blood thinners unless your doctor tells you to do so. Don’t take over-the-counter pain medications, such as ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve, others), without talking to your doctor first.
- Endothelin receptor antagonists. These medications reverse the effect of endothelin, a substance in the walls of blood vessels that causes them to narrow. One of these medications, bosentan (Tracleer), may improve your energy level and symptoms by lowering the resistance in your lung arteries. If you take bosentan, you’ll need monthly liver monitoring because the drug can damage your liver.
- Sildenafil and tadalafil. Sildenafil (Revatio, Viagra) and tadalafil (Cialis, Adcirca) are sometimes used to treat high blood pressure in your pulmonary arteries caused by Eisenmenger syndrome. These drugs work by opening the blood vessels in the lungs to allow blood to flow through more easily. Side effects include upset stomach, dizziness and vision problems.
- Antibiotics. Depending on your condition, you may need to take antibiotics before having certain dental and medical procedures. These procedures may allow bacteria to enter your bloodstream. Antibiotics taken before these procedures can help destroy or control the harmful bacteria that may lead to an infection of your heart’s tissues (endocarditis). Antibiotics are recommended only before certain dental procedures (those that cut your gum tissue or part of the teeth) and procedures involving the respiratory tract, infected skin or tissue that connects muscle to bone.
Blood drawing (phlebotomy)
If your red blood cell count becomes too high and is causing symptoms such as headache, difficulty concentrating or visual disturbances, your doctor may recommend having blood drawn to help decrease your blood cell counts. Phlebotomy should not be done routinely and should only be performed after consultation with a congenital heart disease expert. You should also receive intravenous (IV) fluids when having blood drawn to help replace the lost fluids.
Heart-lung transplantation
Some people who have Eisenmenger syndrome may eventually need a heart and lung transplant or a lung transplant with repair of the hole in the heart if no other treatments prove effective.
Birth control and pregnancy
If you have Eisenmenger syndrome, becoming pregnant poses serious health risks — and can be fatal — for the mother and baby. It’s critical that women who have Eisenmenger syndrome avoid becoming pregnant. It is essential that women affected by Eisenmenger syndrome have a thorough understanding of such risks and receive information, support, and guidance from their physicians and other members of their healthcare team concerning appropriate options to prevent pregnancy.
Your doctor may recommend nonreversible birth control, such as Essure. Essure is a metal coil inserted through the vagina into the fallopian tubes that causes scar tissue to develop. This blocks the fallopian tubes.
Having your fallopian tubes tied (tubal ligation) is less often recommended due to the risks of having even minor surgery.
Birth control pills containing estrogen aren’t recommended for women who have Eisenmenger syndrome. Estrogen increases your risk of developing blood clots that could potentially block an artery to your heart, brain or lungs. Using only barrier methods, such as condoms or diaphragms, isn’t recommended due to the risk of those methods failing.
Home remedies
If you’re diagnosed with Eisenmenger syndrome, you can still lead an active life with proper treatment and precautions.
- Check with your doctor about exercise restrictions. While you shouldn’t perform strenuous exercise or sports, you may be able to do less intense physical activities. Talk to your doctor about what type of physical activity is appropriate for you.
- Avoid high altitudes. Because of the low oxygen levels at high altitudes, the American College of Cardiology and the American Heart Association recommend against living at an altitude of 5,000 feet (1,524 meters) or higher above sea level. Discuss travel by airplane or to high altitudes with your cardiologist for specific recommendations.
- Avoid situations that can excessively lower blood pressure. These include sitting in a hot tub or sauna, steam room or taking long hot baths or showers. These activities lower your blood pressure and cause fainting or even death. You should also avoid activities that cause prolonged straining, such as lifting heavy objects or weights.
- Be cautious with any medications and supplements. Many prescription and over-the-counter medications or supplements may increase or decrease blood pressure, increase risk of bleeding or blood clots, or affect kidney function in patients who have Eisenmenger syndrome. Talk to your doctor before taking any supplements or medications.
- Avoid secondhand smoke and quit using tobacco products. Cigarette smoke and other tobacco products can cause further damage to your lungs’ arteries and increase your risk of developing complications.
Coping and support
Whether you or your child has been diagnosed with Eisenmenger syndrome, it’s natural to worry about health concerns, even after treatment. Although treatments can help your symptoms and improve your prognosis, you may feel stressed or nervous about your condition.
Here are a few things to keep in mind to help you cope with an Eisenmenger syndrome diagnosis and treatment:
- Emotional difficulties. Being diagnosed with Eisenmenger syndrome is life-changing. You may need to alter your plans to have a family, and you may find yourself nervous that your condition will worsen. If your child has been diagnosed with Eisenmenger syndrome, he or she may feel insecure and may have emotional difficulties as he or she reaches school age. Talk to your doctor or your child’s doctor about ways you can cope with these problems, which may include support groups, or a visit to a therapist or psychologist.
- Developmental difficulties for children. Because some children who have congenital heart defects and Eisenmenger syndrome may have had a long recovery time from surgeries or procedures, they may developmentally lag behind other children their age. Some children’s difficulties may last into their school years, and they may have difficulties learning to read or write, as well. Talk to your child’s doctor about ways to help your child through his or her developmental difficulties.
- Support groups. A serious medical problem for you or your child isn’t easy and, depending on the severity of your condition, may be very difficult and frightening. You may find that talking with others who’ve been through the same situation brings you comfort and encouragement. Ask your doctor or your child’s doctor if there are any local support groups.
- Eisenmenger V. Die angeborenen Defecte der Kammerscheide-wand des Herzens. Z Klin Med. 1897;32:1–28.[↩][↩]
- Pulmonary arterial hypertension in congenital heart disease: an epidemiologic perspective from a Dutch registry. Duffels MG, Engelfriet PM, Berger RM, van Loon RL, Hoendermis E, Vriend JW, van der Velde ET, Bresser P, Mulder BJ. Int J Cardiol. 2007 Aug 21; 120(2):198-204. https://www.ncbi.nlm.nih.gov/pubmed/17182132/[↩]
- Baumgartner H, Bonhoeffer P, De Groot NM, et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J 31: 2915-2957, 2010. https://www.ncbi.nlm.nih.gov/pubmed/20801927[↩][↩]
- Diller GP, Kempny A, Alonso-Gonzalez R, et al. Survival prospects and circumstances of death in contemporary adult congenital heart disease patients under follow-up at a large tertiary centre. Circulation 132: 2118-2125, 2015. http://circ.ahajournals.org/content/132/22/2118.long[↩]
- Wood P. The Eisenmenger syndrome or pulmonary hypertension with reversed central shunt. I. Br Med J 2: 701-709, 1958. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2026671/pdf/brmedj03069-0015.pdf[↩]
- Kaemmerer H, Mebus S, Schulze-Neick I, et al. The Adult Patient with Eisenmenger Syndrome: A Medical Update After Dana Point Part I: Epidemiology, Clinical Aspects and Diagnostic Options. Current Cardiology Reviews. 2010;6(4):343-355. doi:10.2174/157340310793566154.[↩]
- Wood P. The Eisenmenger syndrome or pulmonary hypertension with reversed central shunt. I. Br Med J. 1958;2(5098):701–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2026671/pdf/brmedj03069-0015.pdf[↩]
- Hopkins WE, Ochoa LL, Richardson GW, Trulock EP. Comparison of the hemodynamics and survival of adults with severe primary pulmonary hypertension or Eisenmenger syndrome. J Heart Lung Transplant. 1996;15(1 Pt 1):100–5. https://www.ncbi.nlm.nih.gov/pubmed/8820089[↩]
- Hopkins WE. The remarkable right ventricle of patients with Eisenmenger syndrome. Coron Artery Dis. 2005;16(1):19–25. https://www.ncbi.nlm.nih.gov/pubmed/15654195[↩]
- Kidd L, Driscoll DJ, Gersony WM, et al. Second natural history study of congenital heart defects. Results of treatment of patients with ventricular septal defects. Circulation. 1993;87(2 Suppl):I38–51. https://www.ncbi.nlm.nih.gov/pubmed/8425321[↩]
- Vongpatanasin W, Brickner ME, Hillis LD, Lange RA. The Eisenmenger syndrome in adults. Ann Intern Med. 1998;128(9):745–55. https://www.ncbi.nlm.nih.gov/pubmed/9556469[↩]