Contents
- What is endometrial cancer
- Uterus and endometrium
- Endometrial cancer types
- Grading endometrial cancers
- Endometrial cancer causes
- Endometrial Cancer Prevention
- Endometrial cancer signs and symptoms
- Can Endometrial Cancer Be Found Early?
- Endometrial cancer diagnosis
- Endometrial cancer staging
- Endometrial cancer survival rates
- Endometrial cancer treatment
What is endometrial cancer
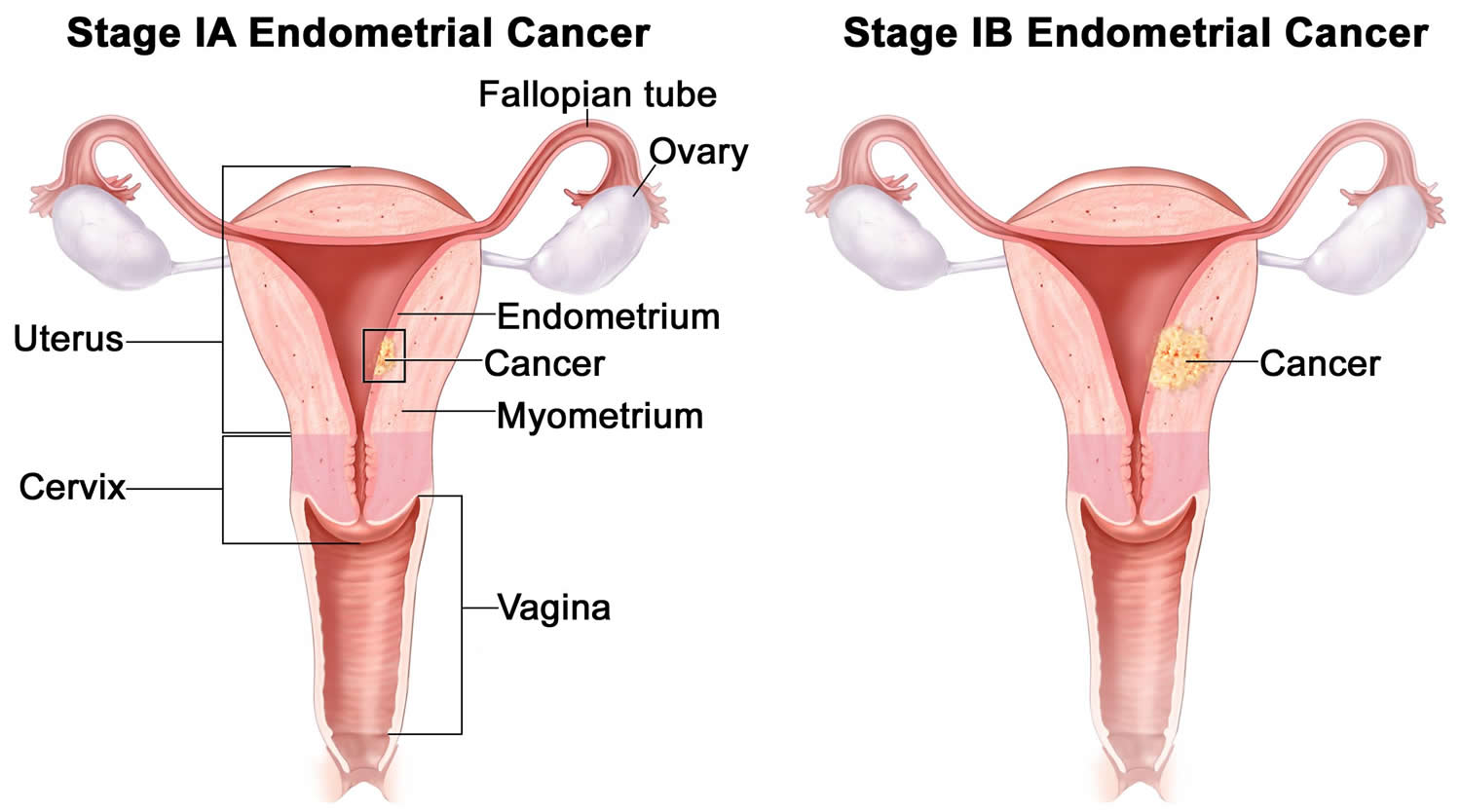
Endometrial cancer begins in the layer of cells that form the lining (the endometrium) of the uterus (see Figures 1 and 3). Endometrial cancer is often detected at an early stage, because it frequently produces abnormal vaginal bleeding, which prompts women to see their health care providers. If endometrial cancer is discovered early, surgically removing the uterus often cures it.
Endometrial cancer is the fourth most common cancer in women in the United States after breast, lung, and colorectal cancers 1.
In the United States, cancer of the endometrium is the most common cancer of the female reproductive organs. The American Cancer Society estimates for cancer of the uterus in the United States for 2018 are 2:
- About 63,230 new cases of cancer of the body of the uterus (uterine body or corpus) will be diagnosed.
- About 11,350 women will die from cancers of the uterine body.
These estimates include both endometrial cancers and uterine sarcomas. Up to 8% of uterine body cancers are sarcomas, so the actual numbers for endometrial cancer cases and deaths are slightly lower than these estimates.
Lifetime chance of getting endometrial cancer
Endometrial cancer affects mainly postmenopausal women. The average age of women diagnosed with endometrial cancer is 60. It is uncommon in women under the age of 45.
This cancer is slightly more common in white women, but black women are more likely to die from it. There are more than 600,000 survivors of endometrial cancer.
Uterus and endometrium
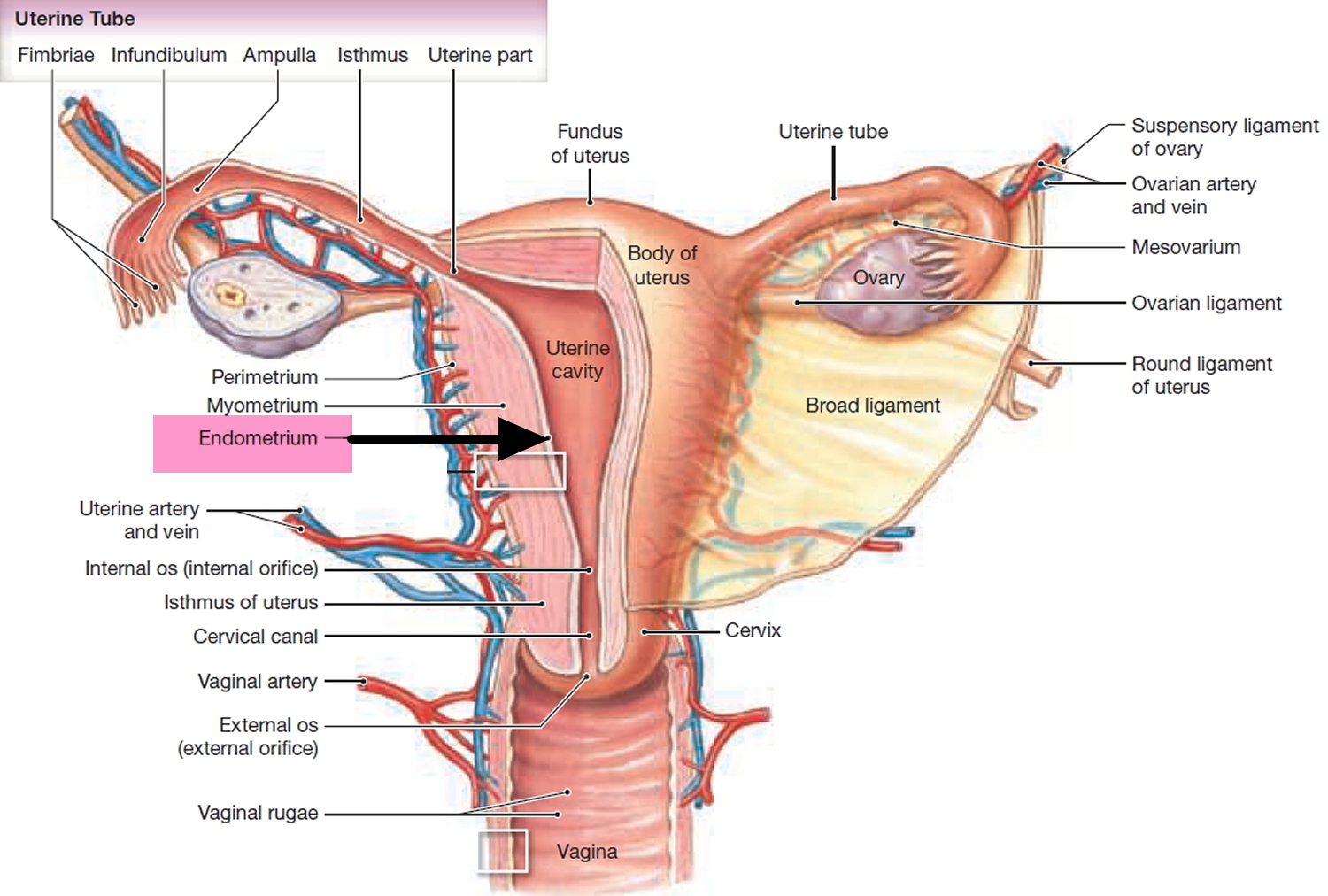
The uterus is a hollow, muscular organ shaped somewhat like an inverted pear. The uterus receives the embryo that develops from an oocyte fertilized in the uterine tube, and sustains its development.
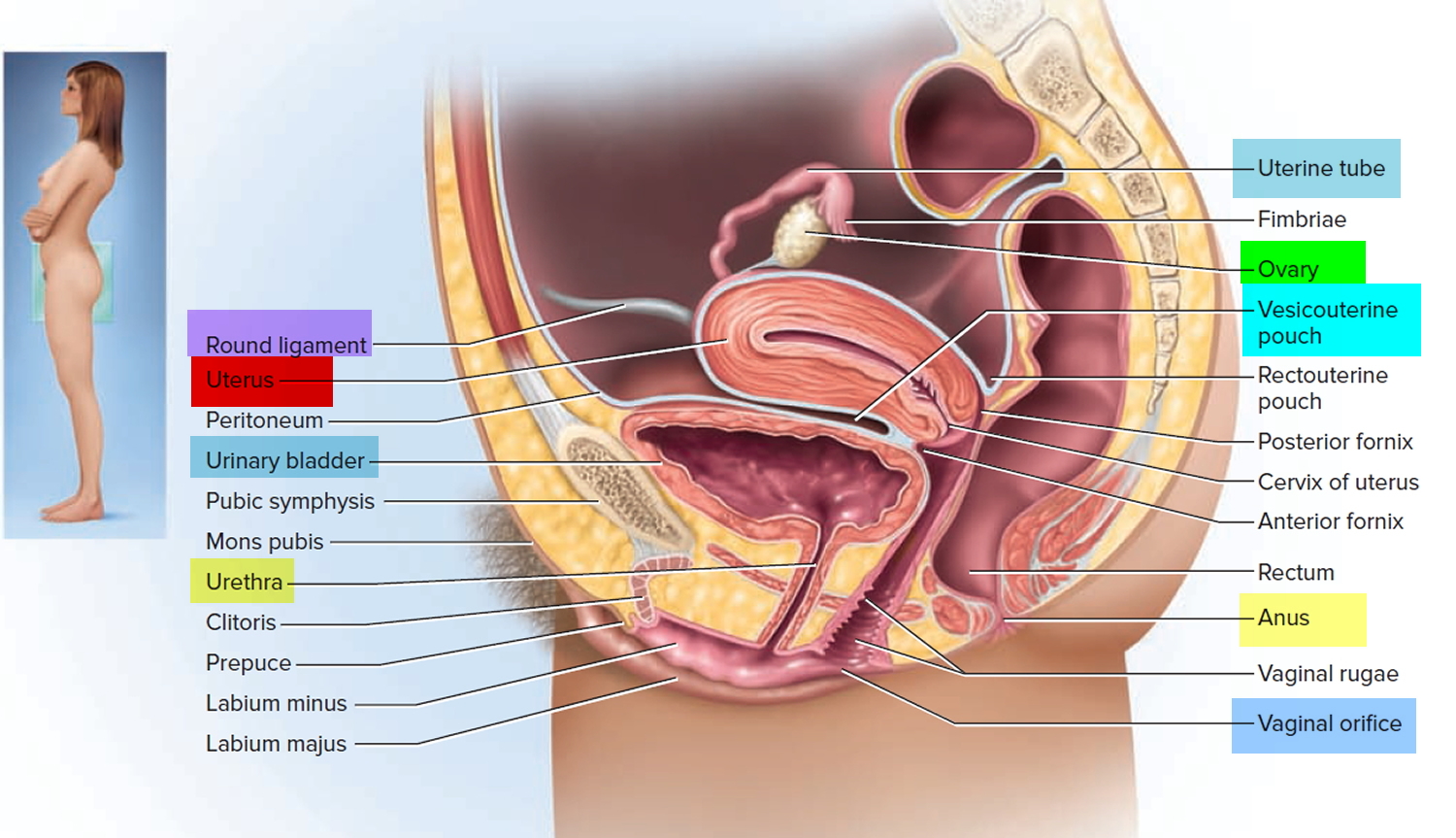
In its nonpregnant, adult state, the uterus is about 7 centimeters long, 5 centimeters wide (at its broadest point), and 2.5 centimeters in diameter. The size of the uterus changes greatly during pregnancy and it is somewhat larger in women who have been pregnant. The uterus is located medially in the anterior part of the pelvic cavity, superior to the vagina, and usually bends forward over the urinary bladder (see Figure 3).
The upper two-thirds or body (corpus), of the uterus has a domeshaped top called the fundus (see Figure 1). The uterine tubes (also called Fallopian tubes) connect at the upper lateral edges of the uterus. The lower third of the uterus is called the cervix. This tubular part extends downward into the upper part of the vagina. The cervix surrounds the opening called the cervical orifice, through which the uterus opens to the vagina.
The uterine wall is thick and has three layers (Figure 1). The endometrium, the inner mucosal layer, is covered with columnar epithelium and contains abundant tubular glands (see Figure 3). The myometrium, a thick, middle, muscular layer, consists largely of bundles of smooth muscle cells. During the monthly female menstrual cycles and during pregnancy, the endometrium and myometrium change extensively. The perimetrium consists of an outer serosal layer, which covers the body of the uterus and part of the cervix.
During a woman’s menstrual cycle, hormones cause the endometrium to change. During the early part of the cycle, before the ovaries release an egg (ovulation), the ovaries produce hormones called estrogens. Estrogen causes the endometrium to thicken so that it could nourish an embryo if pregnancy occurs. If there is no pregnancy, estrogen is produced in lower amounts and more of the hormone called progesterone is made after ovulation. This prepares the innermost layer of the lining to shed. By the end of the cycle, the endometrial lining is shed from the uterus and becomes the menstrual flow (period). This cycle repeats until the woman’s goes through menopause (change of life).
The uterus is supported by the muscular floor of the pelvis and folds of peritoneum that form supportive ligaments around the organ, as they do for the ovary and uterine tube. The broad ligament has two parts: the mesosalpinx mentioned earlier and the mesometrium on each side of the uterus. The cervix and superior part of the vagina are supported by cardinal (lateral cervical) ligaments extending to the pelvic wall. A pair of uterosacral ligaments attaches the posterior side of the uterus to the sacrum, and a pair of round ligaments arises from the anterior surface of the uterus, passes through the inguinal canals, and terminates in the labia majora.
As the peritoneum folds around the various pelvic organs, it creates several dead-end recesses and pouches (extensions of the peritoneal cavity). Two major ones are the vesicouterine pouch, which forms the space between the uterus and urinary bladder, and rectouterine pouch between the uterus and rectum (see Figure 2).
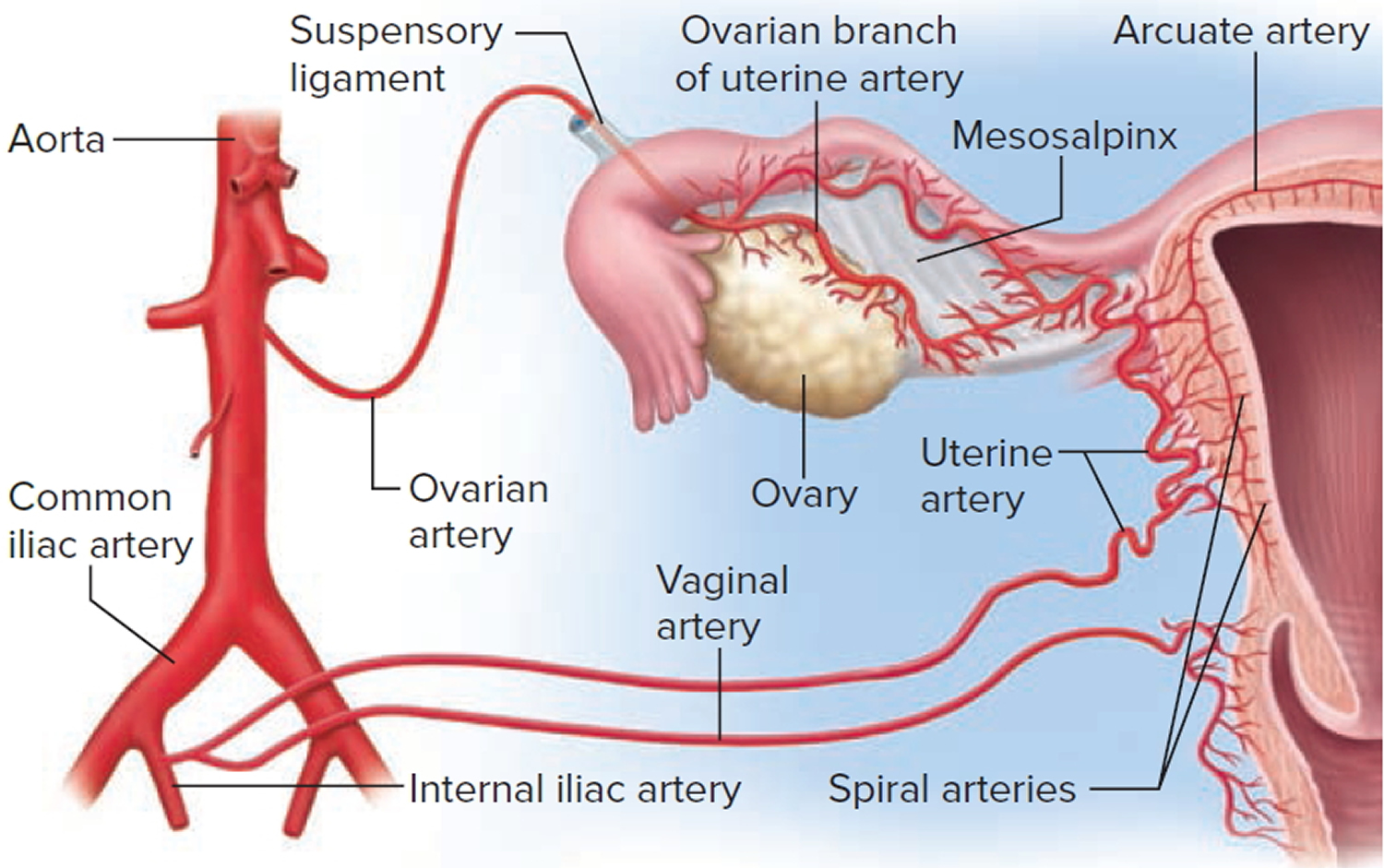
The uterine blood supply to the uterus is particularly important to the menstrual cycle and pregnancy. A uterine artery arises from each internal iliac artery and travels through the broad ligament to the uterus (Figure 4). It gives off several branches that penetrate into the myometrium and lead to arcuate arteries. Each arcuate artery travels in a circle around the uterus and anastomoses with the arcuate artery on the other side. Along its course, it gives rise to smaller arteries that penetrate the rest of the way through the myometrium, into the endometrium, and give off spiral arteries. The spiral arteries wind tortuously between the endometrial glands toward the surface of the mucosa. They rhythmically constrict and dilate, making the mucosa alternately blanch and flush with blood.
Figure 1. Uterus
Figure 2. Uterus location
Figure 3. Endometrium of the uterus and its blood supply
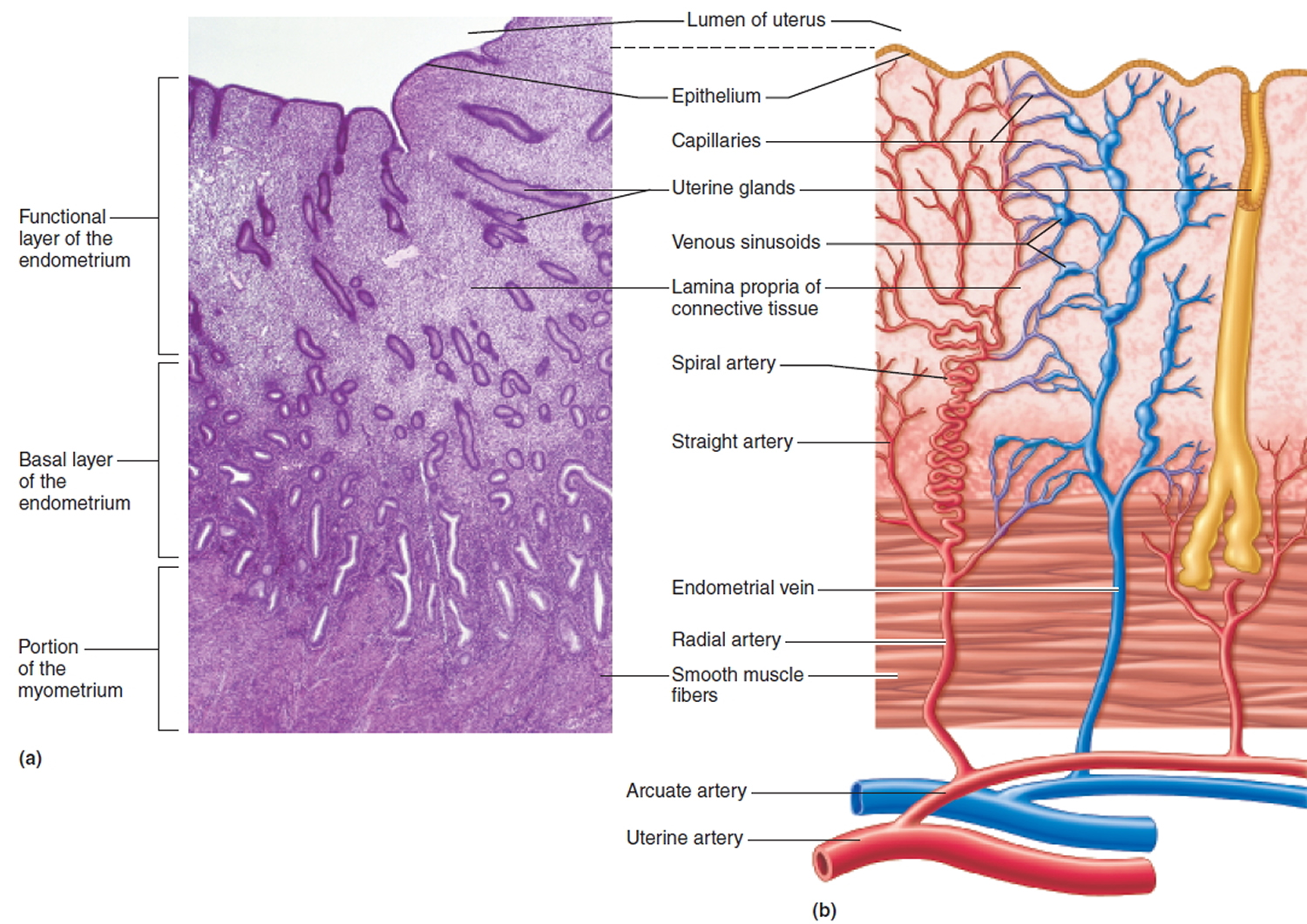 Figure 4. Blood supply to the uterus
Figure 4. Blood supply to the uterus
 Endometrial cancer types
Endometrial cancer types
Endometrial cancer is generally classified into two types 3. Type I is the most common form, representing more than 70% of cases. Type I tumors are associated with unopposed estrogen stimulation and are known as endometrioid adenocarcinoma 4. These tumors are generally low grade. Type II tumors are more likely to be high grade and of papillary serous or clear cell histologic type. They carry a poor prognosis and have a high risk of relapse and metastasis. Type II accounts for only 10% of endometrial cancers, but it is associated with 40% of related deaths 4. Familial tumors are commonly found in association with Lynch syndrome (hereditary nonpolyposis colorectal cancer). Genetic disease represents 10% of cases of endometrial cancer 4.
Endometrial hyperplasia represents a precursor lesion to endometrial cancer. Hyperplasia carries a 1% to 3% risk of progression to cancer. Atypical hyperplasia is associated with greater cancer risk than simple or complex hyperplasia; 30% to 40% of patients with atypical hyperplasia have concomitant adenocarcinoma 3.
Endometrial cancers can be divided into different types based on how the cells look under the microscope (histologic types). These include:
- Adenocarcinoma, (most endometrial cancers are adenocarcinomas)
- Carcinosarcoma (discussed more below)
- Squamous cell carcinoma
- Undifferentiated carcinoma
- Small cell carcinoma
- Transitional carcinoma
The most common type of adenocarcinoma is endometrioid cancer. Endometrioid cancers are made up of cells in glands that look much like the normal uterine lining (endometrium). Some of these cancers have squamous cells (squamous cells are flat, thin cells that can be found on the outer surface of the cervix), as well as glandular cells.
There are many variants (or sub-types) of endometrioid cancers including:
- Adenocarcinoma, (with squamous differentiation)
- Adenoacanthoma
- Adenosquamous (or mixed cell)
- Secretory carcinoma
- Ciliated carcinoma
- Villoglandular adenocarcinoma
Clear-cell carcinoma, mucinous adenocarcinoma, and papillary serous adenocarcinoma are less common types of endometrial adenocarcinomas. These types tend to be more aggressive than most endometrial cancers. They tend to grow quickly and often have spread outside the uterus at the time of diagnosis.
Grading endometrial cancers
The grade of an endometrial cancer is based on how much the cancer forms glands that look similar to those found in normal, healthy endometrium.
In lower-grade cancers (grades 1 and 2), more of the cancerous tissue forms glands.
In higher-grade cancers (grade 3), more of the cancer cells are arranged in a haphazard or disorganized way and do not form glands.
- Grade 1 tumors have 95% or more of the cancerous tissue forming glands.
- Grade 2 tumors have between 50% and 94% of the cancerous tissue forming glands.
- Grade 3 tumors have less than half of the cancerous tissue forming glands. Grade 3 cancers tend to be aggressive and have a poorer outlook than lower-grade cancers.
Grades 1 and 2 endometrioid cancers are type 1 endometrial cancers. Type 1 cancers are usually not very aggressive and do not spread to other tissues quickly. Type 1 endometrial cancers are thought to be caused by excess estrogen. They sometimes develop from atypical hyperplasia, an abnormal overgrowth of cells in the endometrium.
A small number of endometrial cancers are type 2 endometrial cancer. Type 2 cancers are more likely to grow and spread outside the uterus, they have a poorer outlook (than type 1 cancers). Doctors tend to treat these cancers more aggressively. They don’t seem to be caused by too much estrogen. Type 2 cancers include all endometrial carcinomas that aren’t type 1, such as papillary serous carcinoma, clear-cell carcinoma, undifferentiated carcinoma, and grade 3 endometrioid carcinoma. These cancers don’t look at all like normal endometrium and so are called poorly differentiated or high-grade.
Uterine carcinosarcoma starts in the endometrium and has features of both endometrial carcinoma and sarcoma. In the past, carcinosarcoma was considered a type of uterine sarcoma, but doctors now believe that carcinosarcoma is a carcinoma that is abnormal and so no longer looks much like the cells it came from (poorly differentiated).
Uterine carcinosarcoma is considered a type 2 endometrial carcinoma. Carcinosarcoma tumors are also known as malignant mixed mesodermal tumors or malignant mixed mullerian tumors. They make up about 4% of uterine cancers.
Endometrial cancer causes
Scientists do not yet know exactly what causes most cases of endometrial cancer, but they do know certain risk factors, particularly hormone imbalance, for this type of cancer. A great deal of research is going on to learn more about endometrial cancer.
Scientists know that most endometrial cancer cells contain estrogen and/or progesterone receptors on their surfaces. Somehow, interaction of these receptors with their hormones leads to increased growth of the endometrium. This can mark the beginning of cancer. The increased growth can become more and more abnormal until it develops into a cancer.
As noted in the risk factors section below, many of the known endometrial cancer risk factors affect the balance between estrogen and progesterone in the body.
Scientists are learning more about changes in the DNA of certain genes that occur when normal endometrial cells become cancerous.
Endometrial cancer risk factors
A risk factor is anything that affects your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed.
Although certain factors increase a woman’s risk for developing endometrial cancer, they do not always cause the disease. Many women with one or more risk factors never develop endometrial cancer.
Some women with endometrial cancer do not have any known risk factors. Even if a woman with endometrial cancer has one or more risk factors, there is no way to know which, if any, of these factors was responsible for her cancer.
Several factors influence (lowers or increases) the risk of developing endometrial cancer, including:
- Things that affect hormone levels, like taking estrogen after menopause, birth control pills, or tamoxifen; the number of menstrual cycles (over a lifetime), pregnancy, obesity, certain ovarian tumors, and polycystic ovarian syndrome (PCOS)
- Use of an intrauterine device (IUD)
- Age
- Diet and exercise
- Diabetes
- Family history (having close relatives with endometrial or colorectal cancer)
- Having been diagnosed with breast or ovarian cancer in the past
- Having been diagnosed with endometrial hyperplasia in the past
- Treatment with radiation therapy to the pelvis to treat another cancer
Some of these, like pregnancy, birth control pills, and the use of an intrauterine device are linked to a lower risk of endometrial cancer, while many are linked to a higher risk. These factors and how they affect endometrial cancer risk are discussed in more detail below.
Hormone factors
A woman’s hormone balance plays a part in the development of most endometrial cancers. Many of the risk factors for endometrial cancer affect estrogen levels. Before menopause, the ovaries are the major source of the 2 main types of female hormones — estrogen and progesterone.
The balance between these hormones changes during a woman’s menstrual cycle each month. This produces a woman’s monthly periods and keeps the endometrium healthy. A shift in the balance of these hormones toward more estrogen increases a woman’s risk for developing endometrial cancer.
After menopause, the ovaries stop making these hormones, but a small amount of estrogen is still made naturally in fat tissue. Estrogen from fat tissue has a bigger impact after menopause than it does before menopause.
Estrogen therapy
Treating the symptoms of menopause with hormones is known as menopausal hormone therapy (or sometimes hormone replacement therapy). Estrogen is the major part of this treatment. Estrogen treatment can reduce hot flashes, improve vaginal dryness, and help prevent the weakening of the bones (osteoporosis) that can occur with menopause.
Doctors have found, however, that using estrogen alone (without progesterone) can lead to type I endometrial cancer in women who still have a uterus. To lower that risk , a progestin (progesterone or a drug like it) must be given along with estrogen. This approach is called combination hormone therapy.
Women who take progesterone along with estrogen to treat menopausal symptoms do not have an increased risk of endometrial cancer. Still, taking this combination increases a woman’s chance of developing breast cancer and also increases the risk of serious blood clots.
If you are taking (or plan to take) hormones after menopause, it is important to discuss the possible risks (including cancer, blood clots, heart attacks, and stroke) with your doctor.
Like any other medicine, hormones should be used only at the lowest dose that is needed and for the shortest possible time to control symptoms. As with any other medicine you take for a long time, you’ll need to see your doctor regularly. Experts recommend yearly follow-up pelvic exams. If you have any abnormal bleeding or discharge from the vagina you should see your doctor or other health care provider right away (and not wait for a check-up).
Birth control pills
Using birth control pills (oral contraceptives) lowers the risk of endometrial cancer. The risk is lowest in women who take the pill for a long time, and this protection continues for at least 10 years after a woman stops taking this form of birth control. However, it is important to look at all of the risks and benefits when choosing a contraceptive method; endometrial cancer risk is only one factor to be considered. It’s a good idea to discuss the pros and cons of different types of birth control with your doctor.
Total number of menstrual cycles
Having more menstrual cycles during a woman’s lifetime raises her risk of endometrial cancer. Starting menstrual periods (menarche) before age 12 and/or going through menopause later in life raises the risk. Starting periods early is less a risk factor for women with early menopause. Likewise, late menopause may not lead to a higher risk in women whose periods began later in their teens.
Pregnancy
The hormonal balance shifts toward more progesterone during pregnancy. So having many pregnancies protects against endometrial cancer. Women who have never been pregnant have a higher risk, especially if they were also infertile (unable to become pregnant).
Obesity
A woman’s ovaries produce most of her estrogen, but fat tissue can change some other hormones (called androgens) into estrogens. Having more fat tissue can increase a woman’s estrogen levels, which increases her endometrial cancer risk. In comparison with women who maintain a healthy weight, endometrial cancer is twice as common in overweight women, and more than three times as common in obese women.
Tamoxifen
Tamoxifen is a drug that is used to prevent and treat breast cancer. Tamoxifen acts as an anti-estrogen in breast tissue, but it acts like an estrogen in the uterus. In women who have gone through menopause, it can cause the uterine lining to grow, which increases the risk of endometrial cancer.
The risk of developing endometrial cancer from tamoxifen is low (less than 1% per year). Women taking tamoxifen must balance this risk against the benefits of this drug in treating and preventing breast cancer. This is an issue women should discuss with their doctors. If you are taking tamoxifen, you should have yearly gynecologic exams and should be sure to report any abnormal bleeding, as this could be a sign of endometrial cancer.
Ovarian tumors
A certain type of ovarian tumor, the granulosa cell tumor, often makes estrogen. Estrogen release by one of these tumors is not controlled the way hormone release from the ovaries is, and can sometimes lead to high estrogen levels. The resulting hormone imbalance can stimulate the endometrium and even lead to endometrial cancer. In fact, sometimes vaginal bleeding from endometrial cancer is the first symptom of one of these tumors.
Polycystic ovarian syndrome
Women with a condition called polycystic ovarian syndrome (PCOS) have abnormal hormone levels, such as higher androgen (male hormones) and estrogen levels and lower levels of progesterone. The increase in estrogen relative to progesterone can increase a woman’s chance of getting endometrial cancer. PCOS is also a leading cause of infertility in women.
Using an intrauterine device
Women who used an intrauterine device (IUD) for birth control seem to have a lower risk of getting endometrial cancer. Information about this protective effect is limited to IUDs that do not contain hormones. Researchers have not yet studied whether newer types of IUDs that release progesterone have any effect on endometrial cancer risk. However, these IUDs are sometimes used to treat pre-cancers and early endometrial cancers in women who wish to preserve child-bearing ability.
Age
The risk of endometrial cancer increases as a woman gets older.
Diet and exercise
A high-fat diet can increase the risk of several cancers, including endometrial cancer. Because fatty foods are also high-calorie foods, a high-fat diet can lead to obesity, which is a well-known endometrial cancer risk factor. Many scientists think this is the main way in which a high-fat diet raises endometrial cancer risk. Some scientists think that fatty foods may also have a direct effect on estrogen metabolism, which increases endometrial cancer risk.
Physical activity lowers the risk of endometrial cancer. Several studies found that women who exercised more had a lower risk of endometrial cancer, while in one study women who spent more time sitting had a higher risk.
Diabetes
Endometrial cancer may be as much as 4 times more common in women with diabetes. Diabetes is more common in people who are overweight, but even people with diabetes who are not overweight have a higher risk of endometrial cancer.
Family history
Endometrial cancer tends to run in some families. Some of these families also have an inherited tendency to develop colon cancer. This disorder is called hereditary nonpolyposis colon cancer (HNPCC). Another name for hereditary nonpolyposis colon cancer is Lynch syndrome. In most cases, this disorder is caused by a defect in either the mismatch repair gene MLH1 or the gene MSH2. But at least 5 other genes can cause HNPCC: MLH3, MSH6, TGBR2, PMS1, and PMS2. An abnormal copy of any one of these genes reduces the body’s ability to repair damage to its DNA or regulate cell growth. This results in a very high risk of colon cancer, as well as a high risk of endometrial cancer. Women with this syndrome have a 40% to 60% risk of developing endometrial cancer at some point. The risk of ovarian cancer is also increased.
Some families have a high rate of only endometrial cancer. These families may have a different genetic disorder that hasn’t been discovered yet.
Breast or ovarian cancer
Women who have had breast cancer or ovarian cancer may have an increased risk of developing endometrial cancer, too. Some of the dietary, hormonal, and reproductive risk factors for breast and ovarian cancer also increase endometrial cancer risk.
Endometrial hyperplasia
Endometrial hyperplasia is an increased growth of the endometrium. Mild or simple hyperplasia, the most common type, has a very small risk of becoming cancerous. It may go away on its own or after treatment with hormone therapy. If the hyperplasia is called “atypical,” it has a higher chance of becoming a cancer. Simple atypical hyperplasia turns into cancer in about 8% of cases if it’s not treated. If it’s not treated, complex atypical hyperplasia has a risk of becoming cancerous in up to 29% of cases, and the risk of having an undetected endometrial cancer is even higher. For this reason, complex atypical hyperplasia is usually treated.
Prior pelvic radiation therapy
Radiation used to treat some other cancers can damage the DNA of cells, sometimes increasing the risk of a second type of cancer such as endometrial cancer.
Endometrial Cancer Prevention
Most cases of endometrial cancer cannot be prevented, but there are some things that may lower your risk of developing this disease.
Get to and stay at a healthy weight
One way to lower endometrial cancer risk is to do what you can to change your risk factors whenever possible. For example, women who are overweight or obese have up to 3½ times the risk of getting endometrial cancer compared with women at a healthy weight. Getting to and maintaining a healthy weight is one way to lower the risk of this cancer.
Be physically active
Studies have also linked higher levels of physical activity to lower risks of endometrial cancer, so engaging in regular physical activity (exercise) may also be a way to help lower endometrial cancer risk. An active lifestyle can help you stay at a healthy weight, as well as lower the risk of high blood pressure and diabetes (other risk factors for endometrial cancer.
Discuss pros and cons of hormone therapy with your doctor
Estrogen to treat the symptoms of menopause is available in many different forms like pills, skin patches, shots, creams, and vaginal rings. If you are thinking about using estrogen for menopausal symptoms, ask your doctor about how it will affect your risk of endometrial cancer. Progestins (progesterone-like drugs) can reduce the risk of endometrial cancer in women taking estrogen therapy, but this combination increases the risk of breast cancer. If you still have your uterus and are taking estrogen therapy, discuss this issue with your doctor.
Consider taking birth control pills
Using oral contraceptives for at least one year may reduce endometrial cancer risk. The risk reduction is thought to last for several years after you stop taking oral contraceptives. Oral contraceptives have side effects, though, so discuss the benefits and risks with your doctor.
Get treated for endometrial problems
Getting proper treatment of pre-cancerous disorders of the endometrium is another way to lower the risk of endometrial cancer. Most endometrial cancers develop over a period of years. Many are known to follow and possibly start from less serious abnormalities of the endometrium called endometrial hyperplasia. Some cases of hyperplasia will go away without treatment, but it sometimes needs to be treated with hormones or even surgery. Treatment with progestins and a dilation and curettage (D&C) or hysterectomy can prevent hyperplasia from becoming cancerous. Abnormal vaginal bleeding is the most common symptom of endometrial pre-cancers and cancers, and it needs to be reported and evaluated right away.
Hereditary nonpolyposis colon cancer
Women with hereditary nonpolyposis colon cancer (HNPCC or Lynch syndrome) have a very high risk of endometrial cancer. A woman with hereditary nonpolyposis colorectal cancer may choose to have her uterus removed (a hysterectomy) after she has finished having children to prevent endometrial cancer. One study found that none of 61 women with hereditary nonpolyposis colon cancer who had prophylactic (preventive) hysterectomies was later found to have endometrial cancer, while 1/3 of the women who didn’t have the surgery were diagnosed with endometrial cancer over the next 7 years.
Endometrial cancer signs and symptoms
There are a few symptoms that may point to endometrial cancer, but some are more common as this cancer becomes advanced.
Unusual vaginal bleeding, spotting, or other discharge
About 90% of women diagnosed with endometrial cancer have abnormal vaginal bleeding, such as a change in their periods or bleeding between periods or after menopause. This symptom can also occur with some non-cancerous conditions, but it is important to have a doctor look into any irregular bleeding right away. If you have gone through menopause already, it’s especially important to report any vaginal bleeding, spotting, or abnormal discharge to your doctor.
Non-bloody vaginal discharge may also be a sign of endometrial cancer. Even if you cannot see blood in the discharge, it does not mean there is no cancer. In about 10% of cases, the discharge associated with endometrial cancer is not bloody. Any abnormal discharge should be checked out by your doctor.
Pelvic pain, a mass, and weight loss
Pain in the pelvis, feeling a mass (tumor), and losing weight without trying can also be symptoms of endometrial cancer. These symptoms are more common in later stages of the disease. Still, any delay in seeking medical help may allow the disease to progress even further. This lowers the odds of treatment being successful.
Although any of these symptoms can be caused by things other than cancer, it’s important to have them checked out by a doctor.
Can Endometrial Cancer Be Found Early?
In most cases, noticing any signs and symptoms of endometrial cancer, such as abnormal vaginal bleeding or discharge (that is increasing in amount, occurring between periods, or occurring after menopause), and reporting them right away to your doctor allows the disease to be diagnosed at an early stage. Early detection improves the chances that your cancer will be treated successfully. But some endometrial cancers may reach an advanced stage before signs and symptoms can be noticed.
Early detection tests (Screening)
Early detection (also called screening) refers to the use of tests to find a disease such as cancer in people who do not have symptoms of that disease.
Women at average endometrial cancer risk
At this time, there are no screening tests or exams to find endometrial cancer early in women who are at average endometrial cancer risk and have no symptoms.
The American Cancer Society recommends that, at menopause, all women should be told about the risks and symptoms of endometrial cancer and strongly encouraged to report any vaginal bleeding, discharge, or spotting to their doctor.
Women should talk to their doctors about getting regular pelvic exams. A pelvic exam can find some cancers, including some advanced uterine cancers, but it is not very effective in finding early endometrial cancers.
The Pap test, which screens women for cervical cancer, can occasionally find some early endometrial cancers, but it’s not a good test for this type of cancer.
Women at increased endometrial cancer risk
The American Cancer Society recommends that most women at increased risk should be informed of their risk and be advised to see their doctor whenever they have any abnormal vaginal bleeding. This includes women whose risk of endometrial cancer is increased due to increasing age, late menopause, never giving birth, infertility, obesity, diabetes, high blood pressure, estrogen treatment, or tamoxifen therapy.
Women who have (or may have) hereditary non-polyposis colon cancer (HNPCC, sometimes called Lynch syndrome) have a very high risk of endometrial cancer. If several family members have had colon or endometrial cancer, you might want to think about having genetic counseling to learn about your family’s risk of having HNPCC.
If you (or a close relative) have genetic testing and are found to have a mutation in one of the genes for HNPCC, you are at high risk of getting endometrial cancer.
The American Cancer Society recommends that women who have (or may have) HNPCC be offered yearly testing for endometrial cancer with endometrial biopsy beginning at age 35. Their doctors should discuss this test with them, including its risks, benefits, and limitations. This applies to women known to carry HNPCC-linked gene mutations, women who are likely to carry such a mutation (those with a mutation known to be present in the family), and women from families with a tendency to get colon cancer where genetic testing has not been done.
Another option for a woman who has (or may have) HNPCC would be to have a hysterectomy once she is done having children.
Endometrial cancer diagnosis
Tests and procedures used to diagnose endometrial cancer include:
Pelvic examination
During a pelvic exam, your doctor carefully inspects the outer portion of your genitals (vulva), and then inserts two fingers of one hand into your vagina and simultaneously presses the other hand on your abdomen to feel your uterus and ovaries. He or she also inserts a device called a speculum into your vagina. The speculum opens your vagina so that your doctor can view your vagina and cervix for abnormalities.
Ultrasound
Ultrasound is often one of the first tests used to look at the uterus, ovaries, and fallopian tubes in women with a possible gynecologic problem. Ultrasound tests use sound waves to take pictures of parts of the body. A small instrument called a transducer or probe gives off sound waves and picks up the echoes as they bounce off the organs. A computer translates the echoes into pictures.
For a pelvic ultrasound, the transducer is placed on the skin of the lower part of the abdomen. Often, to get good pictures of the uterus, ovaries, and fallopian tubes, the bladder needs be full. That is why women getting a pelvic ultrasound are asked to drink lots of water before the exam.
A transvaginal ultrasound (TVUS) is often preferred for looking at the uterus. For this test, the TVUS probe (that works the same way as the ultrasound transducer) is put into the vagina. Images from the TVUS can be used to see if the uterus contains a mass (tumor), or if the endometrium is thicker than usual, which can be a sign of endometrial cancer. It may also help see if a cancer is growing into the muscle layer of the uterus (myometrium).
Salt water (saline) may be put through a small tube into the uterus before the ultrasound so the doctor can see the uterine lining more clearly. This procedure is called a saline infusion sonogram or hysterosonogram. (sonogram is another term for ultrasound.) Sonography may help doctors pinpoint the area they want to biopsy if other procedures didn’t detect a tumor.
Endometrial tissue sampling
To find out whether endometrial hyperplasia or endometrial cancer is present, the doctor must remove some tissue so that it can be looked at with a microscope. Endometrial tissue can be obtained by endometrial biopsy or by dilation and curettage (D&C) with or without a hysteroscopy. A specialist such as a gynecologist usually does these procedures, which are described below.
Endometrial biopsy
An endometrial biopsy is the most commonly performed test for endometrial cancer and is very accurate in postmenopausal women. It can be done in the doctor’s office. In this procedure a very thin flexible tube is inserted into the uterus through the cervix. Then, using suction, a small amount of endometrium is removed through the tube. The suctioning takes about a minute or less. The discomfort is similar to menstrual cramps and can be helped by taking a nonsteroidal anti-inflammatory drug such as ibuprofen before the procedure. Sometimes numbing medicine (local anesthetic) is injected into the cervix just before the procedure to help reduce the pain.
Hysteroscopy
For this technique doctors insert a tiny telescope (about 1/6 inch in diameter) into the uterus through the cervix. To get a better view of the inside of the uterus, the uterus is filled with salt water (saline). This lets the doctor see and biopsy anything abnormal, such as a cancer or a polyp. This is usually done using a local anesthesia (numbing medicine) with the patient awake.
Dilation and curettage (D&C)
If the endometrial biopsy sample doesn’t provide enough tissue, or if the biopsy suggests cancer but the results are uncertain, a D&C must be done. In this outpatient procedure, the opening of the cervix is enlarged (dilated) and a special instrument is used to scrape tissue from inside the uterus. This may be done with or without a hysteroscopy.
This procedure takes about an hour and may require general anesthesia (where you are asleep) or conscious sedation (given medicine into a vein to make you drowsy) either with local anesthesia injected into the cervix or a spinal (or epidural). A D&C is usually done in an outpatient surgery area of a clinic or hospital. Most women have little discomfort after this procedure.
Testing endometrial tissue samples
Endometrial tissue samples removed by biopsy or D&C are looked at with a microscope to see whether cancer is present. If cancer is found, the lab report will state what type of endometrial cancer it is (like endometrioid or clear cell) and what grade it is.
Endometrial cancer is graded on a scale of 1 to 3 based on how much it looks like normal endometrium. Women with lower grade cancers are less likely to have advanced disease or recurrences.
If the doctor suspects hereditary non-polyposis colon cancer (HNPCC) as an underlying cause of the endometrial cancer, the tumor tissue can be tested for protein changes (such as having fewer mismatch repair proteins) or DNA changes (called microsatellite instability, or MSI) that can happen when one of the genes that causes HNPCC is faulty. If these protein or DNA changes are present, the doctor may recommend that you consider genetic testing for the genes that cause HNPCC. Testing for low mismatch repair protein levels or for MSI is most often ordered in women diagnosed with endometrial cancer at a younger than usual age or who have a family history of endometrial or colon cancer.
Tests to look for cancer spread
If the doctor suspects that your cancer is advanced, you will probably have to have other tests to look for cancer spread.
Chest x-ray
A plain x-ray of your chest may be done to see if cancer has spread to your lungs.
Computed tomography (CT)
The CT scan is an x-ray procedure that creates detailed, cross-sectional images of your body. For a CT scan, you lie on a table while an X-ray takes pictures. Instead of taking one picture, like a standard x-ray, a CT scanner takes many pictures as the camera rotates around you. A computer then combines these pictures into an image of a slice of your body. The machine will take pictures of many slices of the part of your body that is being studied.
CT scans are not used to diagnose endometrial cancer. However, they may be helpful to see whether the cancer has spread to other organs and to see if the cancer has come back after treatment.
Magnetic resonance imaging (MRI)
MRI scans use radio waves and strong magnets instead of x-rays. The energy from the radio waves is absorbed and then released in a pattern formed by the type of tissue and by certain diseases. A computer translates the pattern of radio waves given off by the tissues into a very detailed image of parts of the body. This creates cross sectional slices of the body like a CT scanner and it also produces slices that are parallel with the length of your body.
MRI scans are particularly helpful in looking at the brain and spinal cord. Some doctors also think MRI is a good way to tell whether, and how far, the endometrial cancer has grown into the body of the uterus. MRI scans may also help find enlarged lymph nodes with a special technique that uses very tiny particles of iron oxide. These are given into a vein and settle into lymph nodes where they can be spotted by MRI.
Positron emission tomography (PET)
In this test radioactive glucose (sugar) is given to look for cancer cells. Because cancers use glucose (sugar) at a higher rate than normal tissues, the radioactivity will tend to concentrate in the cancer. A scanner can spot the radioactive deposits. This test can be helpful for spotting small collections of cancer cells. Special scanners combine a PET scan with a CT to more precisely locate areas of cancer spread. PET scans are not a routine part of the work-up of early endometrial cancer, but may be used for more advanced cases.
Cystoscopy and proctoscopy
If a woman has problems that suggest the cancer has spread to the bladder or rectum, the inside of these organs will probably be looked at through a lighted tube. In cystoscopy the tube is placed into the bladder through the urethra. In proctoscopy the tube is placed in the rectum. These exams allow the doctor to look for possible cancers. Small tissue samples can also be removed during these procedures for pathologic (microscopic) testing. They can be done using a local anesthetic but some patients may require general anesthesia. Your doctor will let you know what to expect before and after the procedure. These procedures were used more often in the past, but now are rarely part of the work up for endometrial cancer.
Blood tests
Complete blood count
The complete blood count (CBC) is a test that measures the different cells in the blood, such as the red blood cells, the white blood cells, and the platelets. Endometrial cancer can cause bleeding, which can lead to low red blood cell counts ( anemia).
CA-125 blood test
CA-125 is a substance released into the bloodstream by many, but not all, endometrial and ovarian cancers. If a woman has endometrial cancer, a very high blood CA-125 level suggests that the cancer has probably spread beyond the uterus. Some doctors check CA-125 levels before surgery or other treatment. If they are elevated, they can be checked again to find out how well the treatment is working (for example, levels will drop after surgery if all the cancer is removed).
CA-125 levels are not needed to diagnose endometrial cancer, and so this test isn’t ordered on all patients.
Endometrial cancer staging
After a woman is diagnosed with endometrial cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes the amount of cancer in the body. It helps determine how serious the cancer is and how best to treat it. The stage is one of the most important factors in deciding how to treat the cancer and determining how successful the treatment might be.
Endometrial cancer stages range from stage I (1) through IV (4). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV, means cancer has spread more. And within a stage, an earlier letter means a lower stage. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
How is the stage determined?
The 2 systems used for staging endometrial cancer, the FIGO (International Federation of Gynecology and Obstetrics) system and the American Joint Committee on Cancer TNM staging system are basically the same.
They both stage (classify) this cancer based on 3 factors:
- The extent (size) of the tumor (T): How far has the cancer grown into the uterus? Has the cancer reached nearby structures or organs?
- The spread to nearby lymph nodes (N): Has the cancer spread to the lymph nodes in the pelvis or around the aorta (the main artery that runs from the heart down along the back of the abdomen and pelvis). Also called para-aortic lymph nodes.
- The spread (metastasis) to distant sites (M): Has the cancer spread to distant lymph nodes or distant organs?
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once a person’s T, N, and M categories have been determined, this information is combined in a process called stage grouping to assign an overall stage.
The staging system in the table below uses the pathologic stage (also called the surgical stage). It is determined by examining tissue removed during an operation. This is also known as surgical staging. Sometimes, if surgery is not possible right away, the cancer will be given a clinical stage instead. This is based on the results of a physical exam, biopsy, and imaging tests done before surgery. For more information see Cancer Staging.
The system described below is the most recent AJCC system. It went into effect January 2018.
Endometrial cancer staging can be complex, so ask your doctor to explain it to you in a way you understand.
Table 1. Endometrial cancer staging
| Stage | Stage grouping | FIGO Stage | Stage description* |
| I | T1 N0 M0 | I | The cancer is growing within the body of the uterus. It may also be growing into the glands of the cervix, but not into the supporting connective tissue of the cervix (T1). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| IA | T1a N0 M0 | IA | The cancer is in the endometrium (inner lining of the uterus) and may have grown less than halfway through the underlying muscle layer of the uterus (the myometrium) (T1a). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| IB | T1b N0 M0
| IB | The cancer has grown from the endometrium into the myometrium. It has grown more than halfway through the myometrium but has not spread beyond the body of the uterus (T1b). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| II
| T2 N0 M0 | II | The cancer has spread from the body of the uterus and is growing forward into the supporting connective tissue of the cervix (called the cervical stroma). The cancer has not spread outside the uterus (T2). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| III | T3 N0 M0 | III | The cancer has spread outside the uterus, but has not spread to the inner lining of the rectum or urinary bladder (T3). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| IIIA | T3a N0 M0 | IIIA | The cancer has spread to the outer surface of the uterus (called the serosa) and/or to the fallopian tubes or ovaries (the adnexa) (T3a). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| IIIB | T3b N0 M0 | IIIB | The cancer has spread to the vagina or to the tissues around the uterus (the parametrium) (T3b). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| IIIC1 | T1-T3 N1, N1mi or N1a M0 | IIIC1 | The cancer is growing in the body of the uterus. It may have spread to some nearby tissues, but is not growing into the inside of the bladder or rectum (T1 to T3). The cancer has spread to pelvic lymph nodes (N1, N1mi, or N1a), but not to lymph nodes around the aorta or distant sites (M0). |
| IIIC2 | T1-T3 N2, N2mi or N2a M0 | IIIC2 | The cancer is growing in the body of the uterus. It may have spread to some nearby tissues, but is not growing into the inside of the bladder or rectum (T1 to T3). The cancer has spread to lymph nodes around the aorta (para-aortic lymph nodes) (N2, N2mi, or N2a) but not to distant sites (M0). |
| IVA | T4 Any N M0 | The cancer has spread to the inner lining of the rectum or urinary bladder (called the mucosa) (T4). It may or may not have spread to nearby lymph nodes (Any N) but has not spread to distant sites (M0). | |
| IVB | Any T Any N M1 | IVB | The cancer has spread to inguinal (groin) lymph nodes, the upper abdomen, the omentum, or to organs away from the uterus, such as the lungs, liver, or bones (M1). The cancer can be any size (Any T) and it might or might not have spread to other lymph nodes (Any N). |
*The following additional categories are not listed on the table above:
- TX: Main tumor cannot be assessed due to lack of information.
- T0: No evidence of a primary tumor.
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Endometrial cancer survival rates
Survival rates tell you what percentage of people with the same type and stage of cancer are still alive a certain length of time (usually 5 years) after they were diagnosed. These numbers can’t tell you how long you will live, but they may help give you a better understanding about how likely it is that your treatment will be successful.
Statistics on the outlook for a certain type and stage of cancer are often given as 5-year survival rates, but many people live longer – often much longer – than 5 years. The 5-year survival rate is the percentage of people who live at least 5 years after being diagnosed with cancer.
Survival rates are estimates – your outlook can vary based on a number of factors specific to you.
Survival rates don’t tell the whole story
Survival rates are often based on previous outcomes of large numbers of people who had the disease, but they can’t predict what will happen in any particular person’s case. Your doctor can tell you how the numbers below may apply to you, as he or she is familiar with the aspects of your particular situation.
The survival rates below are based on the stage of the cancer at the time it was diagnosed. These rates do not apply to cancers that have come back after treatment or have spread after treatment starts.
The numbers below come from the National Cancer Data Base as published in the AJCC Staging Manual in 2017, and are based on people diagnosed between 2000 and 2002.
Endometrial cancer survival rates
- The 5-year survival rate for women with stage 0 endometrial cancer is 90%*
- The 5-year survival rate for women with stage IA endometrial cancer is 88%
- The 5-year survival rate for women with stage IB endometrial cancer is 75%
- The 5-year survival rate for women with stage II endometrial cancer is 69%
- The 5-year survival rate for women with stage IIIA endometrial cancer is 58%
- The 5-year survival rate for women with stage IIIB endometrial cancer is 50%
- The 5-year survival rate for women with stage IIIC endometrial cancer is 47%
- The 5-year survival rate for women with stage IVA endometrial cancer is 17%
- The 5-year survival rate for women with stage IVB endometrial cancer is 15%
*The new staging system that went into effect January 2018 no longer includes Stage 0 cancers.
Endometrial cancer treatment
If you’ve been diagnosed with endometrial cancer, your cancer care team will discuss your treatment options with you. It’s important that you think carefully about your choices. You will want to weigh the benefits of each treatment option against the possible risks and side effects.
Your options for treating your endometrial cancer will depend on the characteristics of your cancer, such as the stage, your general health and your preferences.
Treatments for endometrial cancer
After all of the test results have been reviewed, your doctor will recommend one or more treatment options. The four basic types of treatment for women with endometrial cancer are:
- Surgery
- Radiation therapy
- Hormonal therapy
- Chemotherapy
Surgery is the main treatment for most women with this cancer. But in certain situations, a combination of these treatments may be used. The choice of treatment depends largely on the type of cancer and stage of the disease when it is found. Other factors could play a part in choosing the best treatment plan. These might include your age, your overall state of health, whether you plan to have children, and other personal considerations.
Surgery
Surgery to remove the uterus is recommended for most women with endometrial cancer. Most women with endometrial cancer undergo a procedure to remove the uterus (hysterectomy), as well as to remove the fallopian tubes and ovaries (salpingo-oophorectomy). A hysterectomy makes it impossible for you to have children in the future. Also, once your ovaries are removed, you’ll experience menopause, if you haven’t already.
During surgery, your surgeon will also inspect the areas around your uterus to look for signs that cancer has spread. Your surgeon may also remove lymph nodes for testing. This helps determine your cancer’s stage.
Radiation
Radiation therapy uses powerful energy beams, such as X-rays and protons, to kill cancer cells. In some instances, your doctor may recommend radiation to reduce your risk of a cancer recurrence after surgery. In certain situations, radiation therapy may also be recommended before surgery, to shrink a tumor and make it easier to remove.
If you aren’t healthy enough to undergo surgery, you may opt for radiation therapy only. In women with advanced endometrial cancer, radiation therapy may help control cancer-related pain.
Radiation therapy can involve:
- Radiation from a machine outside your body. During external beam radiation, you lie on a table while a machine directs radiation to specific points on your body.
- Radiation placed inside your body. Internal radiation (brachytherapy) involves placing a radiation-filled device, such as small seeds, wires or a cylinder, inside your vagina for a short period of time.
Hormone therapy
Hormone therapy involves taking medications that affect hormone levels in the body. Hormone therapy may be an option if you have advanced endometrial cancer that has spread beyond the uterus.
Options include:
- Medications to increase the amount of progesterone in your body. Synthetic progestin, a form of the hormone progesterone, may help stop endometrial cancer cells from growing.
- Medications to reduce the amount of estrogen in your body. Hormone therapy drugs can help lower the levels of estrogen in your body or make it difficult for your body to use the available estrogen. Endometrial cancer cells that rely on estrogen to help them grow may die in response to these medications.
Chemotherapy
Chemotherapy uses chemicals to kill cancer cells. You may receive one chemotherapy drug, or two or more drugs can be used in combination. You may receive chemotherapy drugs by pill (orally) or through your veins (intravenously). Chemotherapy may be recommended for women with advanced or recurrent endometrial cancer that has spread beyond the uterus. These drugs enter your bloodstream and then travel through your body, killing cancer cells.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing other aggressive treatments, such as surgery, chemotherapy or radiation therapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
Coping and support
Coping with the shock, fear and sadness that come with a cancer diagnosis can take time. You may feel overwhelmed just when you need to make crucial decisions. With time, each person finds a way of coping and coming to terms with the diagnosis.
Until you find what brings you the most comfort, consider trying to:
- Find out enough about endometrial cancer to make decisions about your care. Ask your doctor for the specifics about your cancer, such as its type and stage. And ask for recommended sources of information where you can learn more about your treatment options. The National Cancer Institute 5 and the American Cancer Society 6 are good places to start.
- Stay connected to friends and family. Your friends and family can provide a crucial support network for you during your cancer treatment. As you begin telling people about your endometrial cancer diagnosis, you’ll likely get offers for help. Think ahead about things you may like help with, whether it’s having someone to talk to if you’re feeling low or getting help preparing meals.
- Find someone to talk to. You might have a close friend or family member who’s a good listener. Or talk to a counselor, medical social worker, or pastoral or religious counselor.
Consider joining a support group for people with cancer. You may find strength and encouragement in being with people who are facing the same challenges you are. Ask your doctor, nurse or social worker about groups in your area. Or try online message boards, such as those available through the American Cancer Society 6.
- Diagnosis and Management of Endometrial Cancer. Am Fam Physician. 2016 Mar 15;93(6):468-474. https://www.aafp.org/afp/2016/0315/p468.html[↩]
- American Cancer Society. https://cancerstatisticscenter.cancer.org/#!/[↩]
- Sorosky JI. Endometrial cancer. Obstet Gynecol. 2012;120(2 pt 1):383–397.[↩][↩]
- Practice Bulletin No. 149: Endometrial cancer. Obstet Gynecol. 2015;125(4):1006–1026.[↩][↩][↩]
- National Cancer Institute. https://www.cancer.gov/[↩]
- American Cancer Society. https://www.cancer.org/[↩][↩]