Contents
- What is esophageal cancer
- The esophagus
- Esophageal cancer types
- Esophageal cancer causes
- Esophageal Cancer Risk Factors
- Esophageal Cancer Prevention
- Esophageal cancer signs and symptoms
- Esophageal cancer complications
- Can Esophageal Cancer Be Found Early?
- Esophageal cancer diagnosis
- Esophageal cancer staging
- Esophageal cancer survival rate
- Esophageal cancer prognosis
- Esophageal cancer treatment
- Living as esophageal cancer survivor
What is esophageal cancer
Esophageal cancer is cancer that occurs in the esophagus — a long, hollow muscular tube that runs from your throat to your stomach. Your esophagus helps move the food you swallow from the back of your throat to your stomach to be digested.
Esophageal cancer usually begins in the cells that line the inside of the esophagus. Esophageal cancer can occur anywhere along the esophagus. More men than women get esophageal cancer.
Esophageal cancer makes up about 1% of all cancers diagnosed in the United States, but it is much more common in some other parts of the world, such as Iran, northern China, India, and southern Africa.
Esophageal cancer is the sixth most common cause of cancer deaths worldwide. Incidence rates vary within different geographic locations. In some regions, higher rates of esophageal cancer cases may be attributed to tobacco and alcohol use or particular nutritional habits and obesity.
The American Cancer Society’s estimates for esophageal cancer in the United States for 2024 are 1, 2:
- New cases: About 22,370 new esophageal cancer cases diagnosed (17,690 in men and 4,680 in women)
- Deaths: About 16,130 deaths from esophageal cancer (12,880 in men and 3,250 in women)
- 5-Year Relative Survival: 21.6%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their esophageal cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
- Esophageal cancer deaths as a percentage of All Cancer Deaths: 2.6%.
- Rate of New Cases and Deaths per 100,000: The rate of new cases of esophageal cancer was 4.2 per 100,000 men and women per year. The death rate was 3.7 per 100,000 men and women per year. These rates are age-adjusted and based on 2017–2021 cases and 2018–2022 deaths.
- Lifetime Risk of Developing Cancer: Approximately 0.5 percent of men and women will be diagnosed with esophageal cancer at some point during their lifetime, based on 2018–2021 data.
- In 2021, there were an estimated 51,185 people living with esophageal cancer in the United States.
Esophageal cancer is more common in men than women, and it is associated with older age, heavy alcohol use and tobacco use 2. The rate of new cases of esophageal cancer was 4.2 per 100,000 men and women per year based on 2017–2021 cases, age-adjusted 2. The lifetime risk of esophageal cancer in the United States is about 1 in 127 in men and about 1 in 434 in women 1. Esophageal cancer is the eleventh leading cause of cancer death in the United States. The death rate was 3.7 per 100,000 men and women per year based on 2018–2022 deaths, age-adjusted.
Overall, the rates of esophageal cancer in the United States have been fairly stable for many years, but over the past decade they have been decreasing slightly 1. Esophageal cancer is most common in whites, but is now almost equally as common in African Americans. American Indian, Alaska Natives, and Hispanics have lower rates of esophageal cancer, followed by Asians and Pacific Islanders.
Adenocarcinoma is the most common type of cancer of the esophagus among whites, while squamous cell carcinomais more common in African Americans.
Esophageal cancer makes up about 1.1% of all cancers diagnosed in the United States, but it is much more common in other parts of the world, such as Iran, northern China, India, and southern Africa.
Many people with esophageal cancer do not have signs or symptoms when the cancer first starts. Later, when the tumor gets larger, symptoms can include:
- Difficulty swallowing (dysphagia)
- Weight loss for no known reason
- Chest pain, pressure or burning
- Worsening indigestion or heartburn
- Hiccups
- Throwing up with streaks of blood
- Coughing or hoarseness
- Streaks of blood in mucus coughed up from the lungs
Although many people with esophageal cancer will go on to die from this cancer, treatment has improved and survival rates are getting better. During the 1960s and 1970s, only about 5% of patients survived at least 5 years after being diagnosed. Now, about 21.6% of patients survive at least 5 years after diagnosis 2. This number includes patients with all stages of esophageal cancer. Survival rates for people with early stage cancer are higher.
Make an appointment with your doctor if you have any persistent signs and symptoms that worry you.
You should see your doctor if you have:
- difficulty swallowing
- symptoms that are unusual for you
- symptoms that don’t go away
Your symptoms are unlikely to be cancer but it is important to get them checked by a doctor.
If you’ve been diagnosed with Barrett’s esophagus, a precancerous condition caused by chronic acid reflux, your risk of esophageal cancer is higher. Ask your doctor what signs and symptoms to watch for that may signal that your condition is worsening.
If you’ve had trouble with heartburn, regurgitation and acid reflux for more than five years, then you should ask your doctor about your risk of Barrett’s esophagus.
Screening for esophageal cancer may be an option for people with Barrett’s esophagus. If you have Barrett’s esophagus, discuss the pros and cons of screening with your doctor.
Seek immediate help if you:
- Have chest pain, which may be a symptom of a heart attack
- Have difficulty swallowing
- Are vomiting red blood or blood that looks like coffee grounds
- Are passing black, tarry or bloody stools
- Are unintentionally losing weight
The esophagus
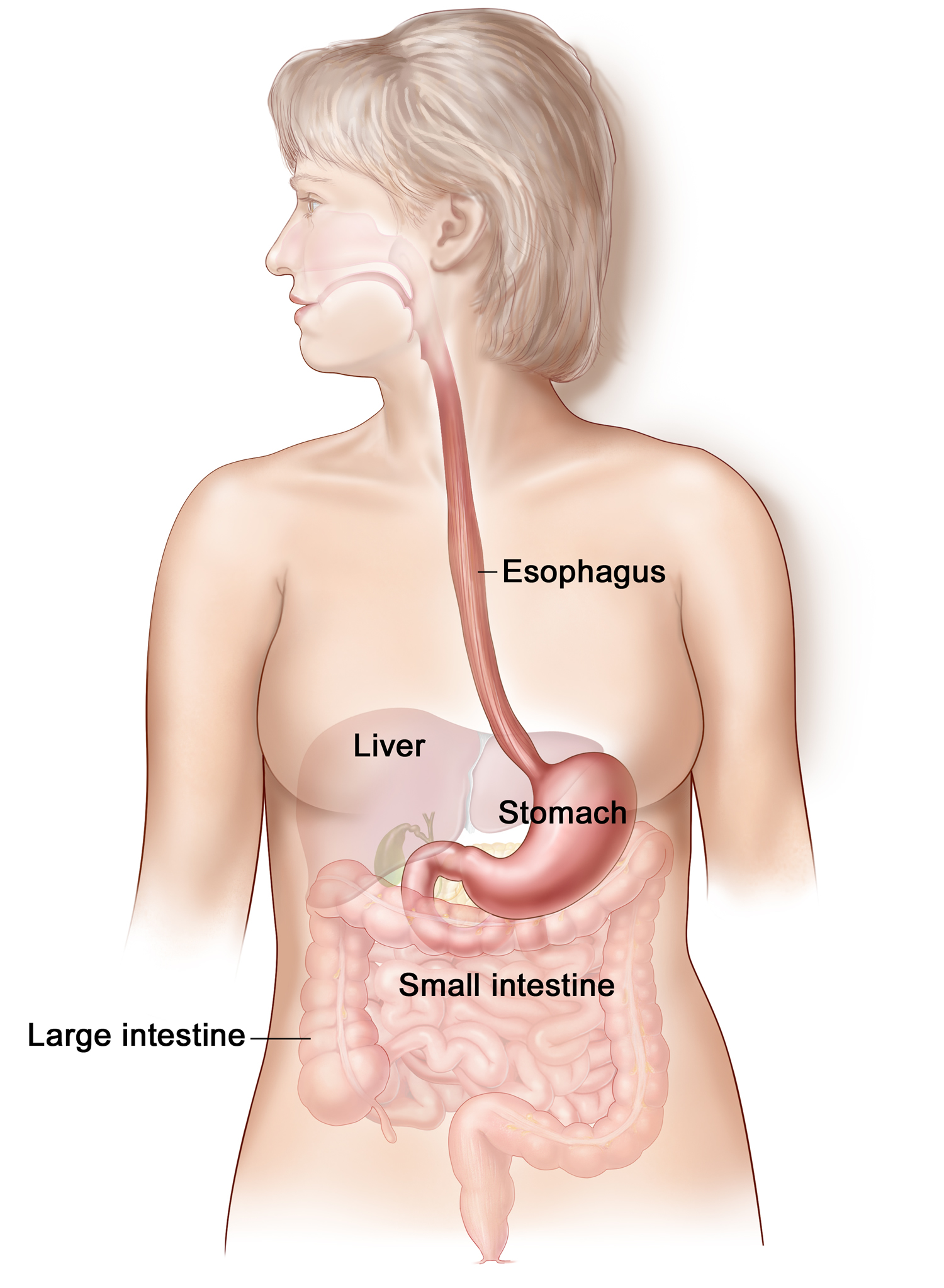
The esophagus, a straight, collapsible muscular tube, about 25 cm (10 in.) long, that lies posterior to the trachea. The esophagus is a food passageway from the pharynx to the stomach (see Figure 1). The esophagus begins at the base of the laryngopharynx and descends posterior to the trachea, passing through the mediastinum. It penetrates the diaphragm through an opening, the esophageal hiatus and is continuous with the stomach on the abdominal side of the diaphragm.
Food and liquids that are swallowed travel through the inside of the esophagus (called the lumen) to reach the stomach.
The upper part of the esophagus has a special ring of muscle at its beginning that relaxes to open the esophagus when it senses food or liquid coming toward it. This muscle is called the upper esophageal sphincter.
The lower part of the esophagus that connects to the stomach is called the gastroesophageal (GE) junction. A special ring of muscle near the gastroesophageal junction, called the lower esophageal sphincter, controls the movement of food from the esophagus into the stomach. Between meals, it closes to keep the stomach’s acid and digestive juices out of the esophagus.
Mucous glands are scattered throughout the submucosa of the esophagus. Their secretions moisten and lubricate the tube’s inner lining.
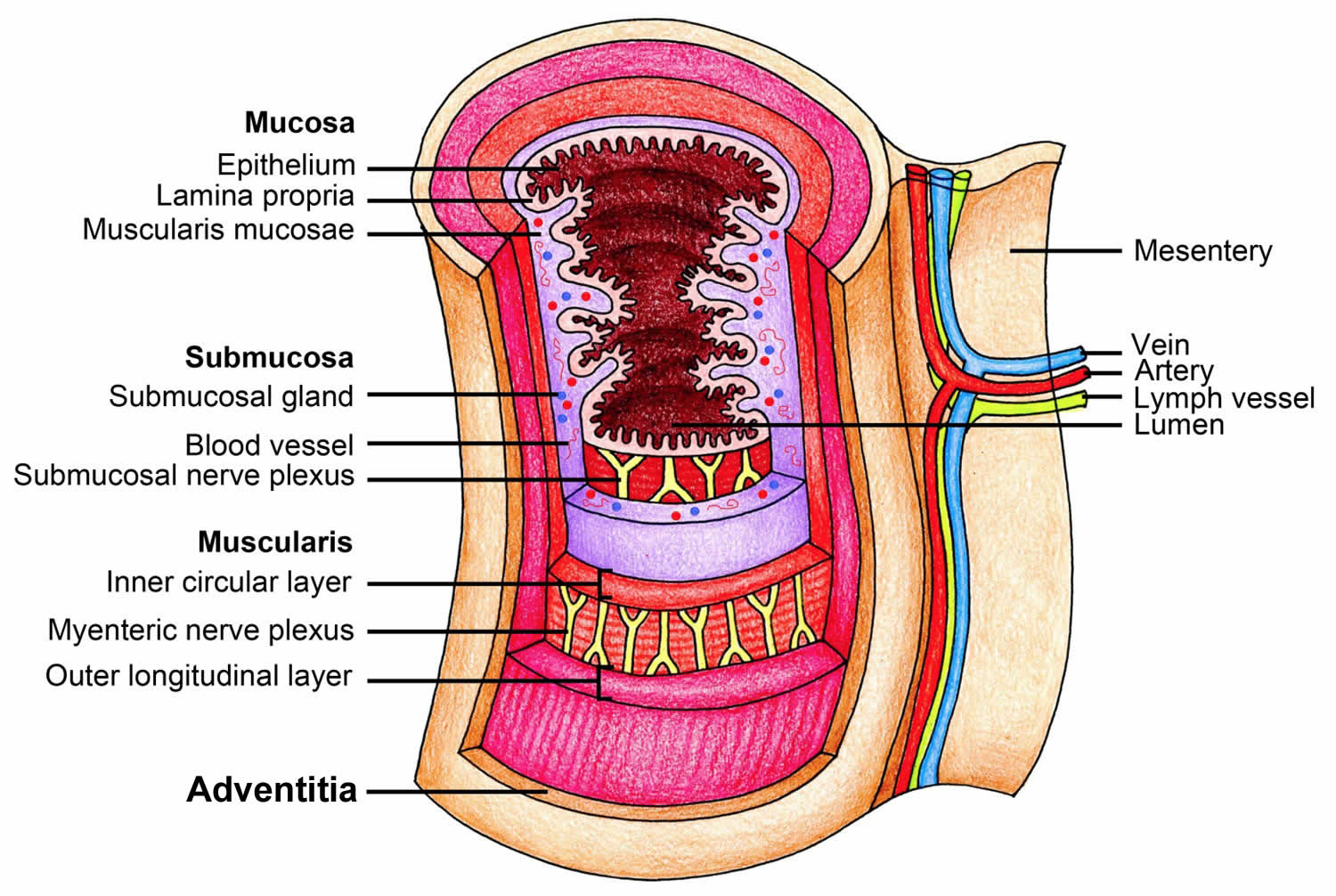
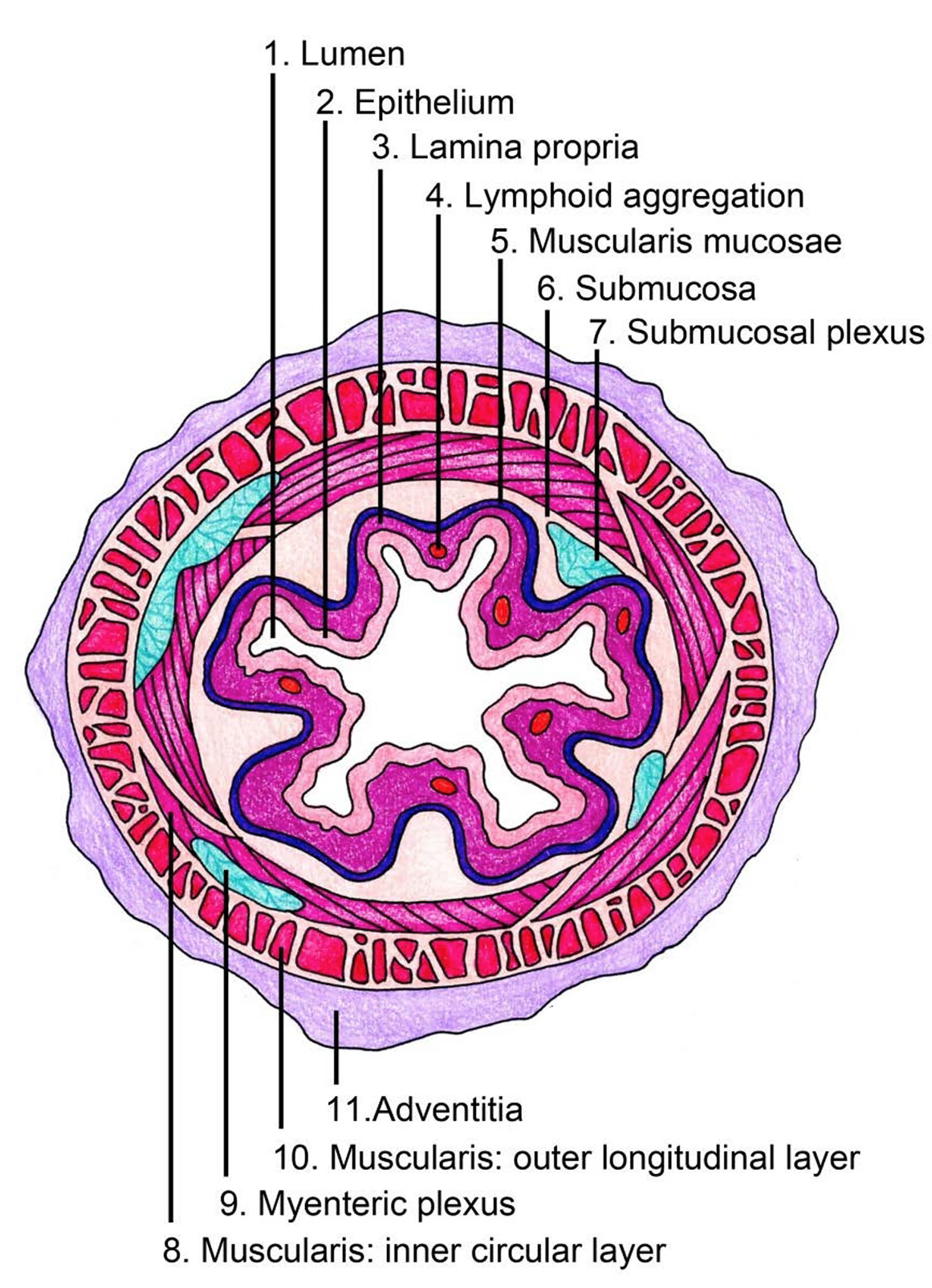
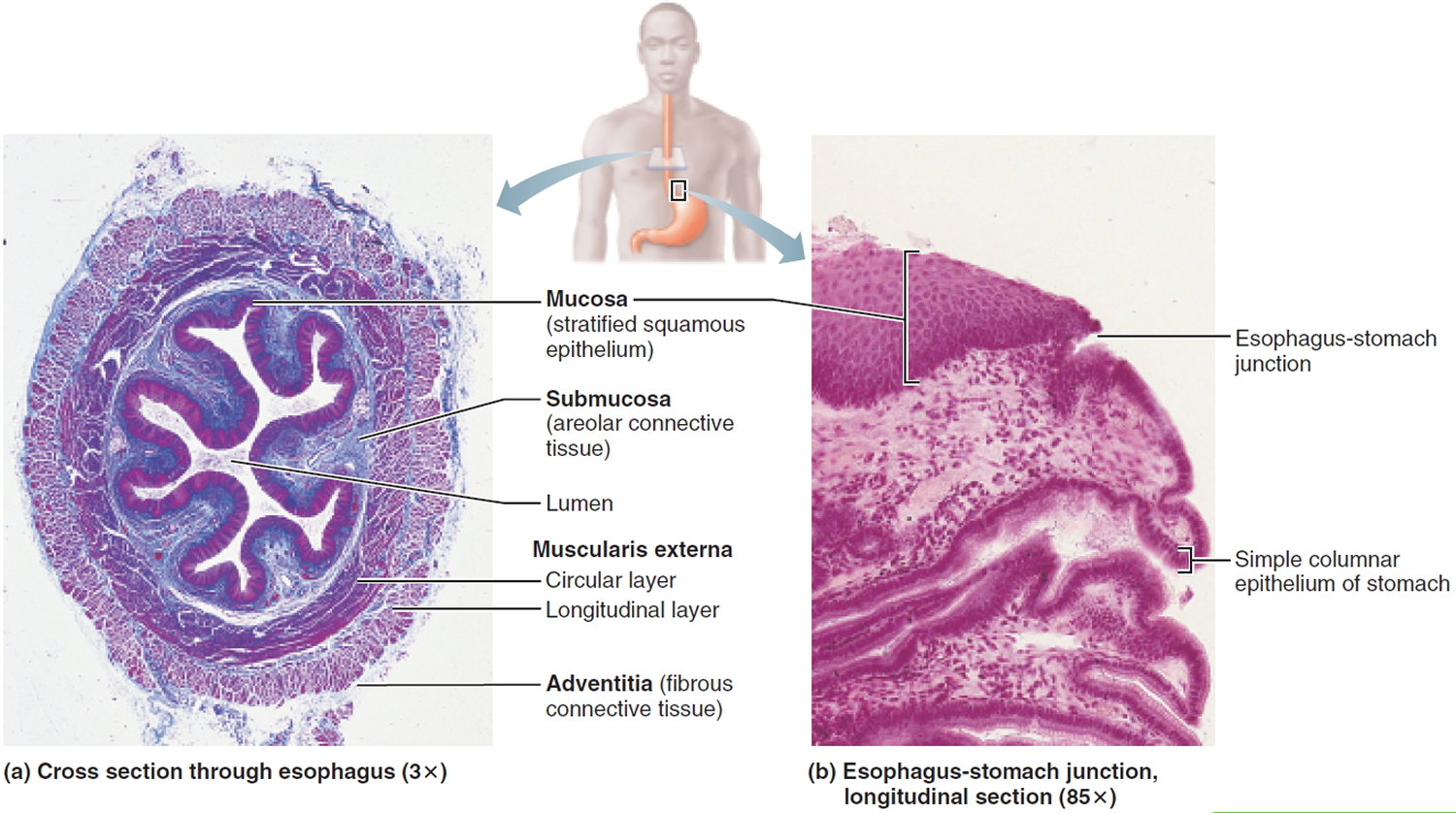
Microscopic Anatomy of the Esophagus
Unlike the mouth and pharynx, the esophagus wall (Figure 2 to 4) contains all four layers of the alimentary canal: mucosa, submucosa, muscularis externa, and adventitia.
The following histological features are of interest:
Mucosa: This layer lines the inside of the esophagus.
The mucosa has 3 parts:
- The mucosal epithelium is the innermost lining of the esophagus and is normally made up of flat, thin cells called squamous cells. At the junction of the esophagus and stomach, this thick, abrasion-resistant layer changes abruptly to the thin simple columnar epithelium of the stomach, which is specialized for secretion (Figure 2). This is where most cancers of the esophagus start.
- The lamina propria is a thin layer of connective tissue right under the epithelium.
- The muscularis mucosa is a very thin layer of muscle under the lamina propria.
Submucosa
- The submucosa of the wall of the esophagus contains mucous glands, primarily compound tubuloalveolar glands, that extend to the lumen. As a bolus passes, it compresses these glands, causing them to secrete a lubricating mucus. This mucus helps the bolus pass through the esophagus.
- When the esophagus is empty, its mucosa and submucosa are thrown into longitudinal folds, but during passage of a bolus, these folds flatten out (Figure 3).
The muscularis externa
- The muscularis externa consists of skeletal muscle in the superior third of the esophagus, a mixture of skeletal and smooth muscle in the middle third, and smooth muscle in the inferior third. This arrangement is easy to remember if the esophagus is viewed as the zone where the skeletal
muscle of the mouth and pharynx gives way to the smooth muscle of the stomach and intestines.
Adventitia
- The most external esophageal layer is an adventitia, not a serosa, because the thoracic segment of the esophagus is not suspended in the peritoneal cavity.
Figure 1. Esophagus
Figure 2. Esophagus anatomy
Figure 3. Cross section view of the esophagus
Esophageal cancer types
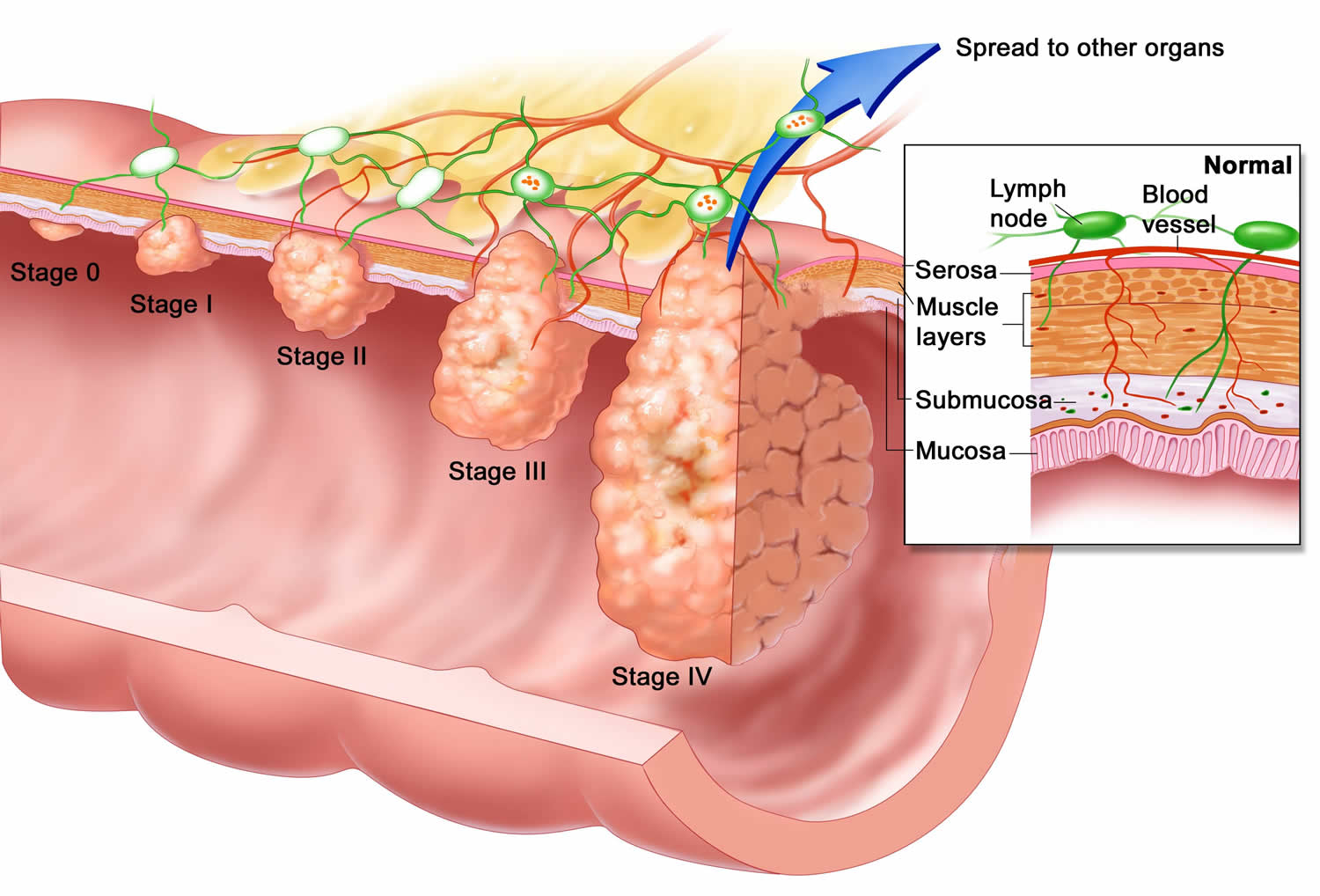
Cancer of the esophagus (also called esophageal cancer) starts in the inner layer (the mucosa) and grows outward (through the submucosa and the muscle layer) (see Figure 4). Since 2 types of cells can line the esophagus, there are 2 main types of esophageal cancer:
Squamous cell carcinoma
The esophagus is normally lined with squamous cells. Cancer starting in these cells is called squamous cell carcinoma. This type of cancer can occur anywhere along the esophagus, but is most common in the portion of the esophagus located in the neck region and in the upper two-thirds of the chest cavity. Squamous cell carcinoma used to be the most common type of esophageal cancer in the United States. This has changed over time, and now it makes up less than half of esophageal cancers in this country.
Adenocarcinoma
Cancers that start in gland cells (cells that make mucus) are called adenocarcinomas. This type of cancer usually occurs in the distal (lower third) part of the esophagus. Before an adenocarcinoma can develop, gland cells must replace an area of squamous cells, which is what happens in Barrett’s esophagus. This occurs mainly in the lower esophagus, which is where most adenocarcinomas start.
Adenocarcinomas that start at the area where the esophagus joins the stomach (the GE junction, which includes about the first 2 inches (5 cm) of the stomach called the cardia), tend to behave like cancers in the esophagus (and are treated like them, as well), so they are grouped with esophagus cancers.
Undifferentiated cancers
Your specialist doctor might not be able to tell which type of esophageal cancer you have. This happens because the cancer cells can look very undeveloped under the microscope.
Undeveloped cancer cells are called undifferentiated cancers. So your doctor might say you have undifferentiated esophageal cancer.
Rare cancers
Other types of cancer can also start in the esophagus, including lymphomas, melanomas, and sarcomas. But these cancers are rare and are not discussed further here.
- Melanoma is a type of skin cancer. Rarely, it can begin in the esophagus.
- Lymphomas are cancers of the lymphatic system. The treatment is different to other esophageal cancers.
- Sarcoma or soft tissue sarcomas are cancers of the supporting cells of the body, such as bone or muscle. Rarely, a type of sarcoma called a gastrointestinal stromal tumour (GIST) can develop in the esophagus.
Esophageal cancer causes
It’s not exactly clear what causes esophageal cancer. However, there are certain risk factors that make getting esophageal cancer more likely.
Factors that cause irritation in the cells of your esophagus and increase your risk of esophageal cancer include:
- Having gastroesophageal reflux disease (GERD)
- Smoking
- Having precancerous changes in the cells of the esophagus (Barrett’s esophagus)
- Being obese
- Drinking alcohol
- Having bile reflux
- Having difficulty swallowing because of an esophageal sphincter that won’t relax (achalasia)
- Having a steady habit of drinking very hot liquids
- Not eating enough fruits and vegetables
- Undergoing radiation treatment to the chest or upper abdomen
Scientists believe that some risk factors, such as the use of tobacco or alcohol, may cause esophageal cancer by damaging the DNA in cells that line the inside of the esophagus. Long-term irritation of the lining of the esophagus, as happens with reflux, Barrett’s esophagus, achalasia, Plummer-Vinson syndrome, or scarring from swallowing lye, may also lead to DNA damage.
DNA is the chemical in each of our cells that makes up your genes – the instructions for how your cells function. You usually look like your parents because they are the source of your DNA. However, DNA affects more than how you look. Some genes control when cells grow, divide into new cells, and die. Genes that help cells grow, divide, and stay alive are called oncogenes. Genes that slow down cell division or make cells die at the right time are called tumor suppressor genes. Cancers can be caused by DNA changes that turn on oncogenes or turn off tumor suppressor genes.
The DNA of esophageal cancer cells often shows changes in many different genes. However, it’s not clear if there are specific gene changes that can be found in all (or most) esophageal cancers.
Some people inherit DNA changes (mutations) from their parents that increase their risk for developing certain cancers. These are called inherited mutations. But esophageal cancer does not seem to run in families, and inherited gene mutations are not thought to be a major cause of this disease. For example:
- Tylosis with esophageal cancer (sometimes called Howel-Evans syndrome) is caused by inherited changes in the RHBDF2 gene. People with changes in this gene are more at risk of developing the squamous cell type of esophageal cancer.
- Bloom syndrome is caused by changes in the BLM gene. The BLM gene is important in making a protein that stabilizes DNA as a cell divides. Without this protein, the DNA can become damaged, which can lead to cancer. People with Bloom syndrome are at a higher risk of developing squamous cell esophageal cancer, as well as AML, ALL, and other cancers involving the lymph system. For this syndrome, an abnormal gene is usually inherited from both parents, not just one.
- Fanconi anemia is a rare syndrome that involves abnormal genes that cannot repair damaged DNA. Mutations (changes) in certain FANC genes can lead to a higher risk of many cancers including AML and squamous cell cancer of the esophagus.
- Familial Barrett’s Esophagus is a syndrome that includes families with Barrett’s esophagus and adenocarcinoma of the esophagus and gastroesophageal (GE) junction. The exact genes associated with this are still being studied.
Special genetic tests can find some of the gene mutations linked to these inherited syndromes. If you have a family history of esophageal cancer or other symptoms linked to these syndromes, you may want to ask your doctor about genetic counseling and genetic testing. The American Cancer Society recommends discussing genetic testing with a qualified cancer genetics professional before any genetic testing is done.
Esophageal Cancer Risk Factors
A risk factor is anything that changes your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed.
Scientists have found several factors that can affect your risk of esophageal cancer. Some are more likely to increase the risk for adenocarcinoma of the esophagus and others for squamous cell carcinoma of the esophagus.
But having a risk factor, or even many, does not mean that you will get esophageal cancer. And some people who get the disease may not have any known risk factors.
Age
The chance of getting esophageal cancer increases with age. Less than 15% of cases are found in people younger than age 55.
Gender
Men are more likely than women to get esophageal cancer.
Gastroesophageal reflux disease (GERD)
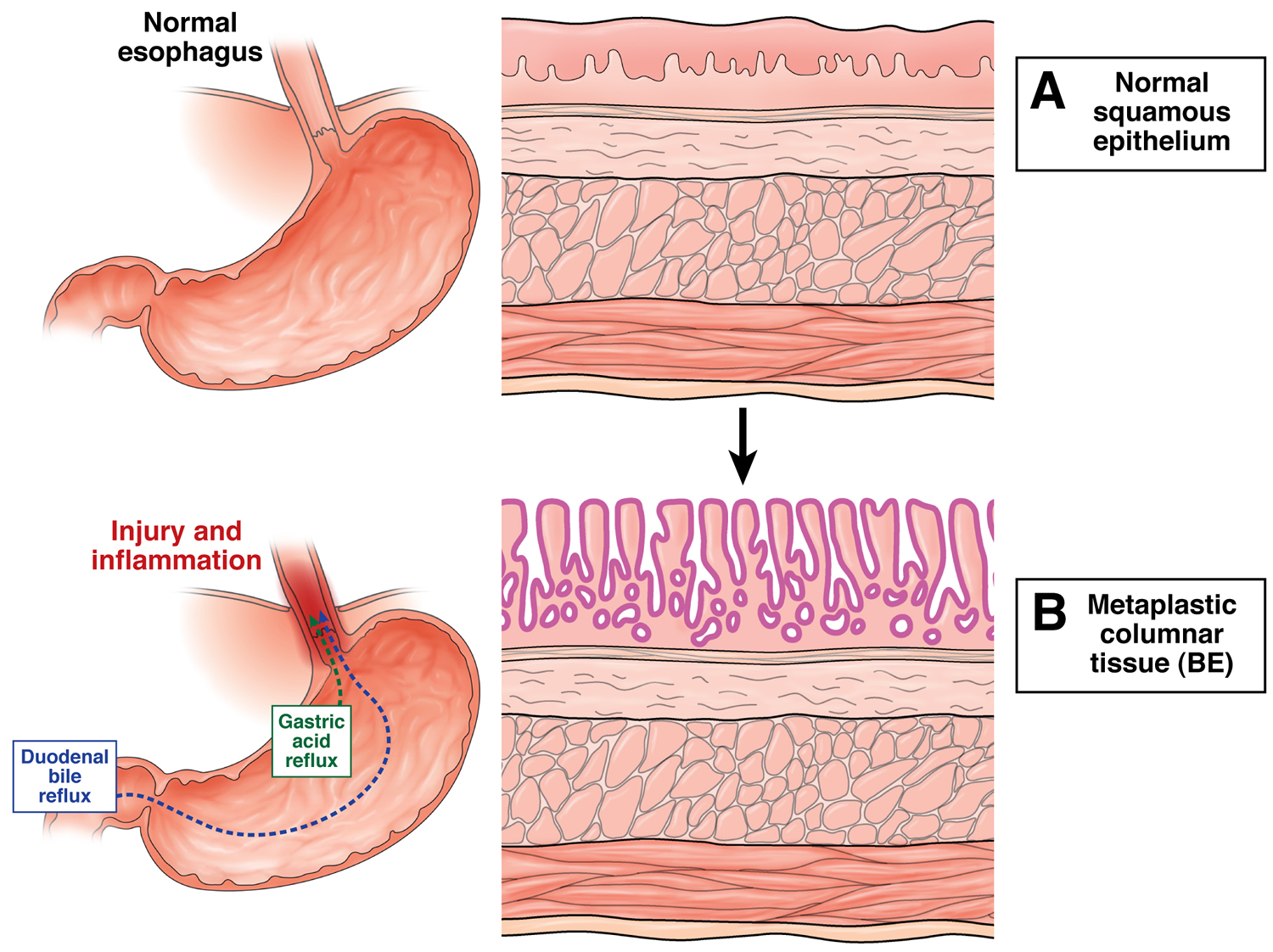
The stomach normally makes strong acid and enzymes to help digest food. In some people, acid can escape from the stomach up into the lower part of the esophagus. The medical term for this is gastroesophageal reflux disease (GERD), or just reflux. In many people, reflux causes symptoms such as heartburn or pain that seem to come from the middle of the chest. In some, though, reflux doesn’t cause any symptoms at all.
People with GERD have a slightly higher risk of getting adenocarcinoma of the esophagus. This risk seems to be higher in people who have more frequent symptoms. But GERD is very common, and most of the people who have it do not go on to develop esophageal cancer. GERD can also cause Barrett’s esophagus (discussed below), which is linked to an even higher risk.
If reflux of stomach acid into the lower esophagus goes on for a long time, it can damage the inner lining of the esophagus. This causes the squamous cells that normally line the esophagus to be replaced with gland cells. These gland cells usually look like the cells that line the stomach and the small intestine, and are more resistant to stomach acid. This condition is known as Barrett’s (or Barrett) esophagus.
The longer someone has reflux, the more likely it is that they will develop Barrett’s esophagus. Most people with Barrett’s esophagus have had symptoms of heartburn, but many have no symptoms at all, a condition often called “silent reflux.”
GERD is an extremely common condition with prevalence rates ranging from 8-40% worldwide. Barrett’s esophagus is found in 1.3 to 1.6% of the general population and 5 to 15% of symptomatic GERD patients undergoing endoscopy 3.
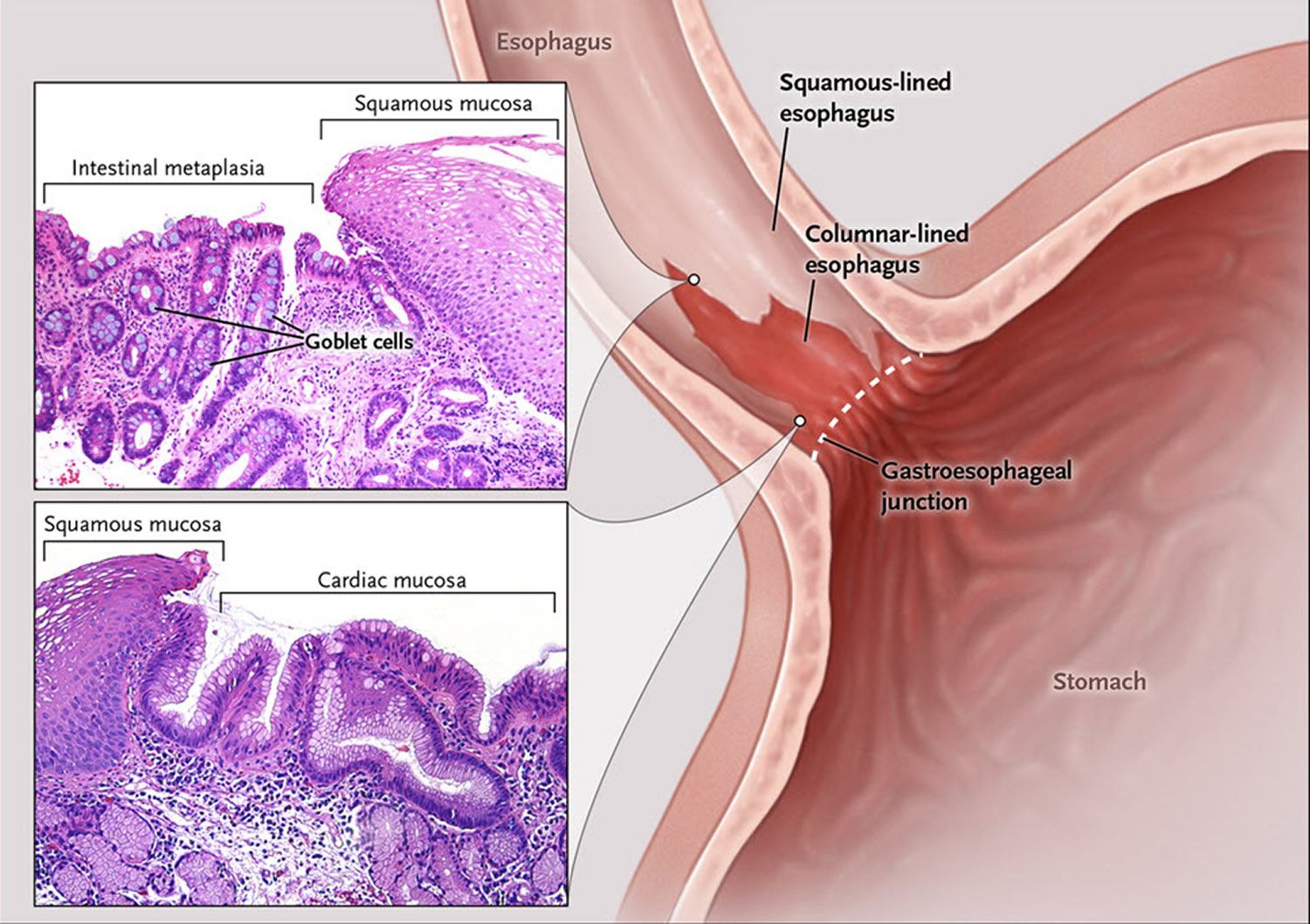
Barrett’s esophagus
Barrett’s esophagus is a condition in which tissue that is similar to the lining of your intestine replaces the tissue lining your esophagus. Doctors call this process intestinal metaplasia. People with Barrett’s esophagus are more likely to develop a rare type of esophageal cancer called esophageal adenocarcinoma 4.
Barrett’s esophagus is defined as the presence of a specialized columnar epithelium with intestinal metaplasia with goblet cells 5. According to the American College of Gastroenterology (ACG) guidelines, Barrett’s esophagus is diagnosed by the presence of intestinal metaplasia on biopsy in addition to the presence of columnar epithelium of at least 1 cm in the esophagus, generally described as “salmon-pink” colored mucosa extending more than 1 cm proximal to the gastroesophageal junction 6. However, the British Society of Gastroenterology 7, as well as the GERD Society Study Committee in Japan 8, do not require the presence of goblet cells to diagnose Barrett’s esophagus and base the diagnosis solely on the presence of columnar metaplasia. Due to the controversy over the significance of goblet cells, another alternative classification has been proposed, which allows the pathologist to state that there is columnar metaplasia and then further specify whether goblet cells are present or are not present. To maximize the possibility of finding Barrett’s esophagus, dysplasia, and/or carcinoma, a minimum of 8 biopsies is recommended by the American College of Gastroenterology. The Prague C & M criteria are recommended for endoscopic grading of Barrett’s esophagus, with the most proximal extent of circumferential columnar mucosa from the gastroesophageal (GE) junction being the C value, and the maximal extent of non-circumferential columnar mucosa above the gastroesophageal (GE) junction being the M value 9.
The development of Barrett’s esophagus is thought to be related to the reflux of gastric acid and bile into the esophagus and the presence of mucosal damage associated with reflux esophagitis 10. In fact, studies using esophageal pH monitoring have reported that acid exposure time in the esophagus is associated with the presence and length of Barrett’s esophagus 11. Furthermore, bilirubin exposure time in the esophagus is associated with the presence and length of Barrett’s esophagus 12. It has also been shown that the combination of gastric and bile acids further increases the risk of developing Barrett’s esophagus 13. However, why Barrett’s esophagus develops in some patients with GERD and not in others remains unclear 3.
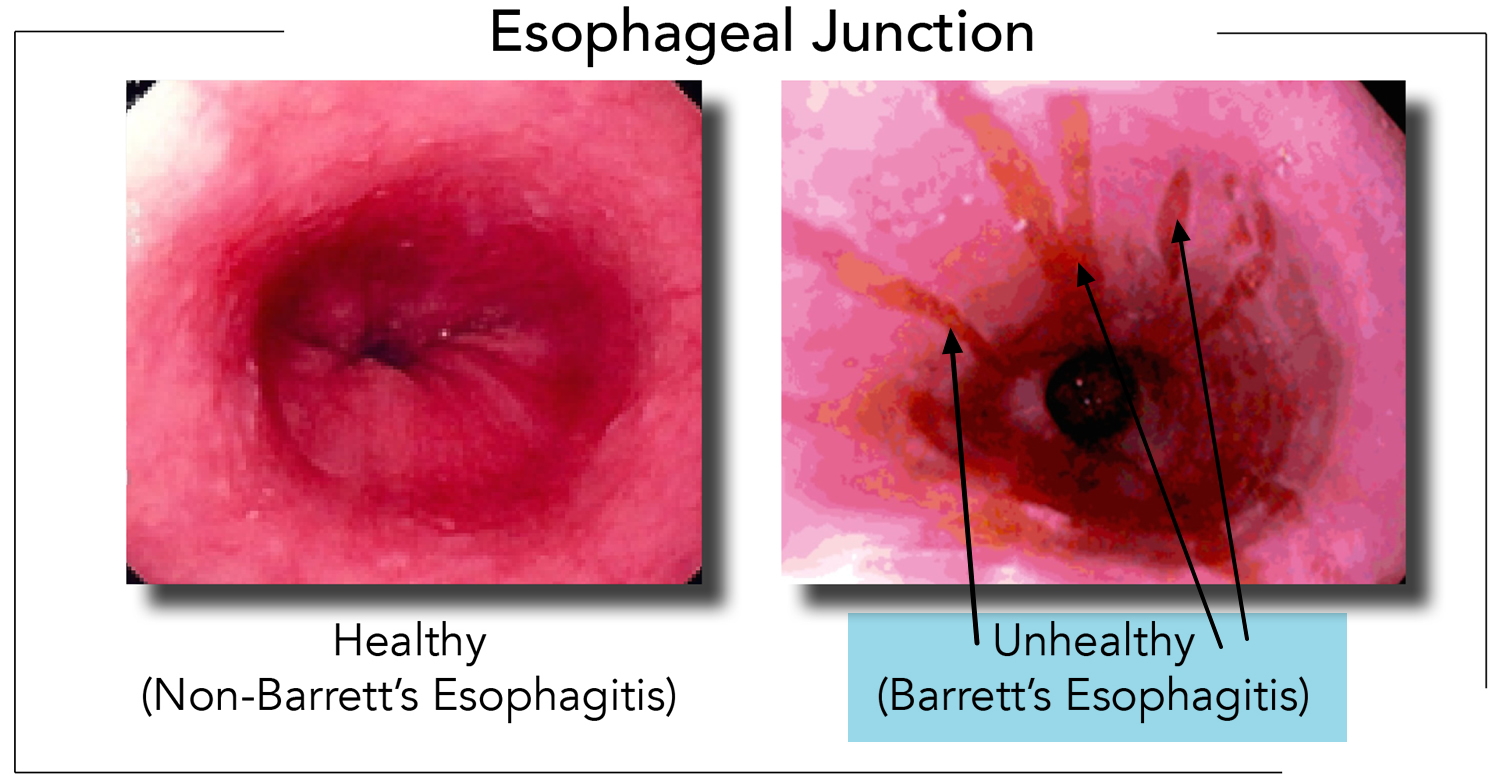
In order to understand Barrett’s esophagus, it is useful to understand the normal appearance of the esophagus. In the normal esophagus, the tissue lining appears pale pink and smooth 14. These flat square cells, called “squamous” (Latin for square) cells, make up the normal lining of the esophagus.
In contrast, Barrett’s esophagus is a salmon-colored lining in the esophagus, made up of cells that are similar to cells found in the small intestine and are called “specialized intestinal metaplasia.”
The reason Barrett’s esophagus is important is because people who have it have a small increased risk of developing esophageal cancer 14. Barrett’s esophagus and heartburn symptoms are associated with a specific type of esophageal cancer called “esophageal adenocarcinoma.” However, cancer is not common 4.
More than 95% of patients with Barrett’s esophagus do not develop cancer. Between 1 and 5 people out of 100 (1–5%) with Barrett’s esophagus will develop esophageal cancer 15. People with Barrett’s esophagus are at a much higher risk than people without this condition to develop adenocarcinoma of the esophagus. Still, most people with Barrett’s esophagus do not get esophageal cancer.
Factors that increase your risk of Barrett’s esophagus include:
- Family history. Your odds of having Barrett’s esophagus increase if you have a family history of Barrett’s esophagus or esophageal cancer.
- Being male. Men are far more likely to develop Barrett’s esophagus.
- Being white. White people have a greater risk of the disease than do people of other races.
- Age. Barrett’s esophagus can occur at any age but is more common in adults over 50.
- Chronic heartburn and acid reflux. Having gastroesophageal reflux disease (GERD) that doesn’t get better when taking medications known as proton pump inhibitors or having GERD that requires regular medication can increase the risk of Barrett’s esophagus.
- Current or past smoking.
- Being overweight. Body fat around your abdomen further increases your risk.
The development of Barrett’s esophagus is most often attributed to long-standing gastroesophageal reflux disease (GERD), which may include these signs and symptoms:
- Frequent heartburn and regurgitation of stomach contents
- Difficulty swallowing food
- Less commonly, chest pain
Curiously, approximately half of the people diagnosed with Barrett’s esophagus report little if any symptoms of acid reflux. So, you should discuss your digestive health with your doctor regarding the possibility of Barrett’s esophagus.
Typically, before esophageal adenocarcinoma develops, precancerous cells appear in the Barrett’s tissue. Doctors call this pre-cancerous condition dysplasia and classify the dysplasia as low grade or high grade. Dysplasia is graded by how abnormal the cells look under the microscope. Low-grade dysplasia looks more like normal cells, while high-grade dysplasia is more abnormal. High-grade dysplasia is linked to the highest risk of cancer.
Studies indicate the absolute annual risk of esophageal adenocarcinoma in nondysplastic Barrett’s esophagus is 0.1 to 0.5% per year, a highly variable 1 to 43% per year for low-grade dysplasia, and 23-60% per year for high-grade dysplasia. A greater extent of dysplasia has a significantly higher risk of cancer as well as the presence of an endoscopic abnormality 16, 17.
In January 2016, the American College of Gastroenterology (ACG) published its new clinical guideline for the diagnosis and management of Barrett’s esophagus 5. The American College of Gastroenterology now recommends screening for Barrett’s esophagus in men with at least five years of chronic GERD symptoms who also have at least two additional risk factors including greater than 50 years of age, history of smoking, white ethnicity, central obesity, or a confirmed family history of Barrett’s esophagus. The current recommendation for surveillance is four-quadrant biopsies every 2 cm (or 1 cm in known or suspected dysplasia) followed by biopsy of mucosal irregularity (nodules, ulcers, or other visible lesions) performed at 3- to 5-year intervals. Due to the extremely low prevalence of esophageal adenocarcinoma in women, this population has no indications for screening except for the presence of multiple risk factors 18, 19.
Figure 5. Barrett’s esophagus
Figure 6. Barrett’s esophagus microscopic view showing changes in the lining of the esophagus
Figure 7. Barrett’s esophagus endoscopic view (as seen by your gut specialist)
Tobacco and alcohol
The use of tobacco products, including cigarettes, cigars, pipes, and chewing tobacco, is a major risk factor for esophageal cancer. The more a person uses tobacco and the longer it is used, the higher the cancer risk. Someone who smokes a pack of cigarettes a day or more has at least twice the chance of getting adenocarcinoma of the esophagus than a nonsmoker, and the risk does not go away if tobacco use stops. The link to squamous cell esophageal cancer is even stronger, but this risk does go down for people who quit tobacco. .
Drinking alcohol also increases the risk of esophageal cancer. The more alcohol someone drinks, the higher their chance of getting esophageal cancer. Alcohol affects the risk of the squamous cell type more than the risk of adenocarcinoma.
Combining smoking and drinking alcohol raises the risk of esophageal cancer much more than using either alone.
Obesity
People who are overweight or obese (very overweight) – obesity means being very overweight with a body mass index (BMI) of 30 or higher — have a higher chance of getting adenocarcinoma of the esophagus. Being overweight or obese is linked to more than 1 in 4 esophageal cancers in men and more than 1 in 10 in women. The more overweight you are the higher the risk. This is in part explained by the fact that people who are obese are more likely to have gastroesophageal reflux.
Diet
Certain substances in the diet may increase esophageal cancer risk. For example, there have been suggestions, as yet not well proven, that a diet high in processed meat may increase the chance of developing esophageal cancer. This may help explain the high rate of this cancer in certain parts of the world.
On the other hand, a diet high in fruits and vegetables is linked to a lower risk of esophageal cancer. The exact reasons for this are not clear, but fruits and vegetables have a number of vitamins and minerals that may help prevent cancer.
Frequently drinking very hot liquids (temperatures of 149° F or 65° C – much hotter than a typical cup of coffee) may increase the risk for the squamous cell type of esophageal cancer. This might be the result of long-term damage to the cells lining the esophagus from the hot liquids.
Achalasia
In this condition, the muscle at the lower end of the esophagus (the lower esophageal sphincter) does not relax properly. Food and liquid that are swallowed have trouble passing into the stomach and tend to collect in the lower esophagus, which becomes stretched out (dilated) over time. The cells lining the esophagus in that area can become irritated from being exposed to foods for longer than normal amounts of time.
People with achalasia have a risk of esophageal cancer that is many times normal. On average, the cancers are found about 15 to 20 years after the achalasia began.
Tylosis
This is a rare, inherited disease that causes excess growth of the top layer of skin on the palms of the hands and soles of the feet. People with this condition also develop small growths (papillomas) in the esophagus and have a very high risk of getting squamous cell cancer of the esophagus.
People with tylosis need to be watched closely to try to find esophageal cancer early. Often this requires regular monitoring with an upper endoscopy.
Plummer-Vinson syndrome
People with this rare syndrome (also called Paterson-Kelly syndrome) have webs in the upper part of the esophagus, typically along with anemia (low red blood cell counts) due to low iron levels, tongue irritation (glossitis), brittle fingernails, and sometimes a large thyroid gland or spleen.
A web is a thin membrane extending out from the inner lining of the esophagus that causes an area of narrowing. Most esophageal webs do not cause any problems, but larger ones can cause food to get stuck in the esophagus, which can lead to problems swallowing and chronic irritation in that area from the trapped food.
About 1 in 10 people with this syndrome eventually develop squamous cell cancer of the esophagus or cancer in the lower part of the throat (hypopharynx).
Workplace exposures
Exposure to chemical fumes in certain workplaces may lead to an increased risk of esophageal cancer. For example, exposure to some of the solvents used for dry cleaning might lead to a greater risk of esophageal cancer. Some studies have found that dry cleaning workers may have a higher rate of esophageal cancer, but not all studies have found this link.
Injury to the esophagus
Lye is a chemical found in strong industrial and household cleaners such as drain cleaners. Lye is a corrosive agent that can burn and destroy cells. Accidentally drinking from a lye-based cleaner bottle can cause a severe chemical burn in the esophagus. As the injury heals, the scar tissue can cause an area of the esophagus to become very narrow (called a stricture). People with these strictures have an increased risk of squamous cell esophageal cancer, which often occurs many years (even decades) later.
History of certain other cancers
People who have had certain other cancers, such as lung cancer, mouth cancer, and throat cancer have a high risk of getting squamous cell carcinoma of the esophagus as well. This may be because these cancers can also be caused by smoking.
Human papilloma virus (HPV) infection
HPV is a group of more than 100 related viruses. They are called papilloma viruses because some of them cause a type of growth called a papilloma (or wart). Infection with certain types of HPV is linked to a number of cancers, including throat cancer, anal cancer, and cervical cancer.
Signs of HPV infection have been found in up to one-third of esophagus cancers from patients in parts of Asia and South Africa. But signs of HPV infection have not been found in esophagus cancers from patients in the other areas, including the US.
Radiotherapy
Radiotherapy for other cancers slightly increases your risk of esophageal cancer, including
- breast cancer
- lung cancer
- oropharynx cancer
- larynx cancer
- Hodgkin lymphoma
Your risk of getting esophageal cancer is still small. You would be at a higher risk from your existing cancer if you didn’t have the radiotherapy your doctor recommends.
Esophageal Cancer Prevention
Not all esophageal cancers can be prevented, but the risk of developing this disease can be greatly reduced by avoiding certain risk factors.
Avoiding tobacco and alcohol
In the United States, the most important lifestyle risk factors for cancer of the esophagus are the use of tobacco and alcohol. Each of these factors alone increases the risk of esophageal cancer many times, and the risk is even greater if they are combined. Avoiding tobacco and alcohol is one of the best ways of limiting your risk of esophageal cancer.
If you smoke, talk to your doctor about strategies for quitting. Medications and counseling are available to help you quit. If you don’t use tobacco, don’t start.
Watching your diet and body weight
Eating a healthy diet and staying at a healthy weight are also important. A diet rich in fruits and vegetables may help protect against esophageal cancer. Obesity has been linked with esophageal cancer, particularly the adenocarcinoma type, so staying at a healthy weight may also help limit the risk of this disease.
Getting treated for gastroesophageal reflux or Barrett’s esophagus
Treating people with reflux may help prevent Barrett’s esophagus and esophageal cancer. Often, reflux is treated using drugs called proton pump inhibitors (PPIs), such as omeprazole (Prilosec®), lansoprazole (Prevacid®), or esomeprazole (Nexium®). Surgery might also be an option for treating reflux if the reflux is not controlled with medical therapy alone.
People at a higher risk for esophageal cancer, such as those with Barrett’s esophagus, are often watched closely by their doctors to look for signs that the cells lining the esophagus have become more abnormal. If dysplasia (a pre-cancerous condition) is found, the doctor may recommend treatments to keep it from developing into esophageal cancer.
For those who have Barrett’s esophagus, daily treatment with a proton pump inhibitor might lower the risk of developing cell changes (dysplasia) that can turn into cancer. If you have chronic heartburn (or reflux), tell your doctor. Treatment can often improve symptoms and might prevent future problems.
Some studies have found that the risk of cancer of the esophagus is lower in people with Barrett’s esophagus who take aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen. However, taking these drugs every day can lead to problems, such as kidney damage and bleeding in the stomach. For this reason, most doctors don’t advise that people take NSAIDs to try to prevent cancer. If you are thinking of taking an NSAID regularly, discuss the potential benefits and risks with your doctor first.
Some studies have also found a lower risk of esophageal cancer in people with Barrett’s esophagus who take drugs called statins, which are used to treat high cholesterol. Examples include atorvastatin (Lipitor®) and rosuvastatin (Crestor®). While taking one of these drugs might help some patients lower esophageal cancer risk, doctors don’t advise taking them just to prevent cancer because they can have serious side effects.
Esophageal cancer signs and symptoms
Early esophageal cancer typically causes no signs or symptoms. Cancers of the esophagus are usually found because of the symptoms they cause. Diagnosis in people without symptoms is rare and usually accidental (because of tests done for other medical problems). Unfortunately, most esophageal cancers do not cause symptoms until they have reached an advanced stage, when they are harder to treat.
The most common symptoms of esophageal cancer are:
- Difficulty swallowing (dysphagia)
- Weight loss without trying
- Chest pain, pressure or burning
- Worsening indigestion or heartburn
- Coughing or hoarseness
- Chronic cough
- Vomiting
- Bone pain (if cancer has spread to the bone)
- Bleeding into the esophagus. This blood then passes through the digestive tract, which may turn the stool black. Over time, this blood loss can lead to anemia (low red blood cell levels), which can make a person feel tired.
Having one or more symptoms does not mean you have esophageal cancer. In fact, many of these symptoms are more likely to be caused by other conditions. Still, if you have any of these symptoms, especially trouble swallowing, it’s important to have them checked by a doctor so that the cause can be found and treated, if needed.
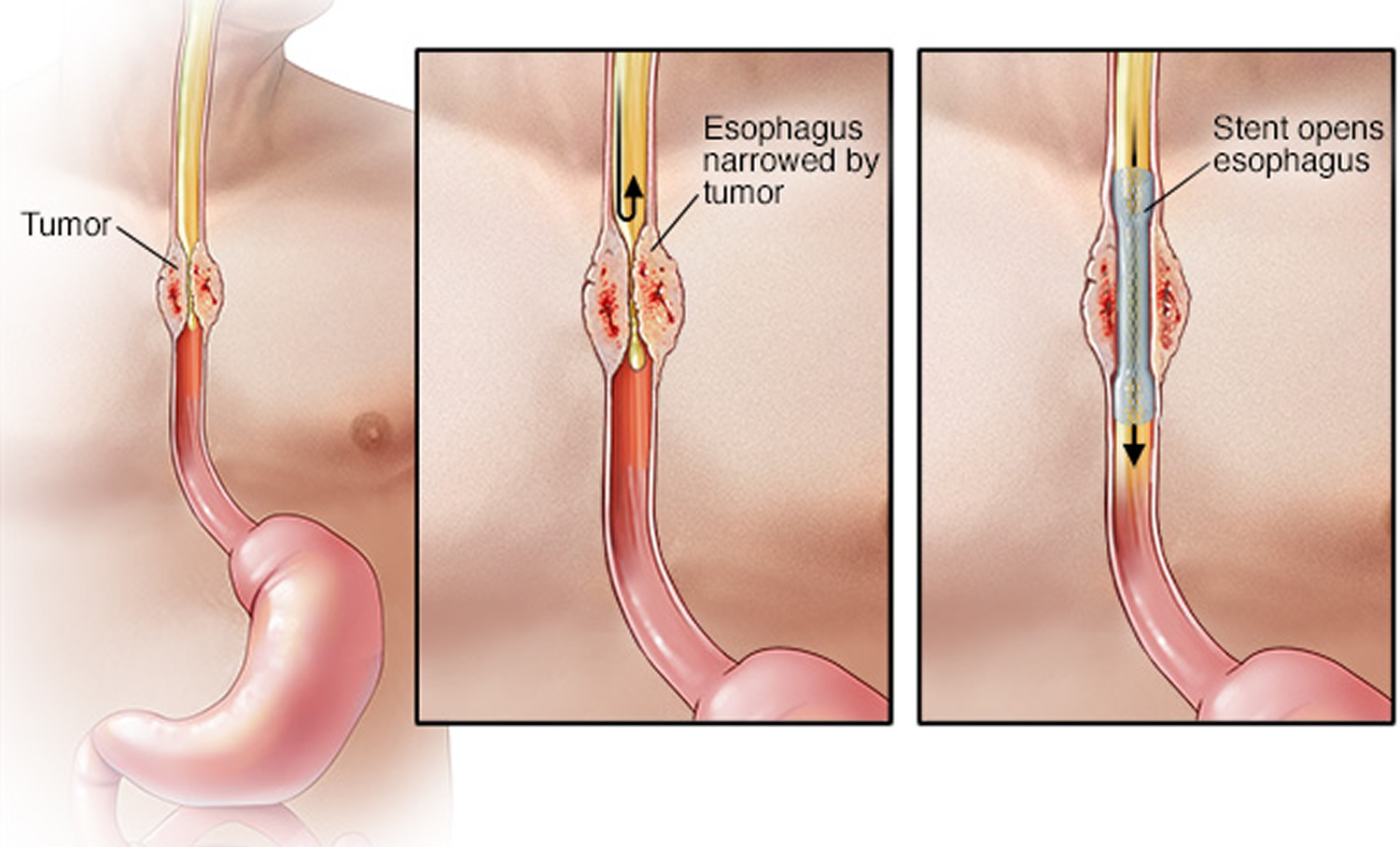
Patients commonly experience difficulty swallowing as the tumor gets larger and the width of the esophagus becomes narrowed. At first, most have trouble swallowing solid foods such as meats, breads or raw vegetables. As the tumor grows, the esophagus becomes more narrowed causing difficulty in swallowing even liquids. Cancer of the esophagus can also cause symptoms of indigestion, heartburn, vomiting and choking. Patients may also have coughing and hoarseness of the voice. Involuntary weight loss is also common.
Trouble swallowing (dysphagia)
The most common symptom of esophageal cancer is a problem swallowing, with a feeling like the food is stuck in the throat or chest, or even choking on food. The medical term for trouble swallowing is dysphagia. This is often mild when it starts, and then gets worse over time as the opening inside the esophagus gets smaller.
When swallowing becomes harder, people often change their diet and eating habits without realizing it. They take smaller bites and chew their food more carefully and slowly. As the cancer grows larger, the problem can get worse. People then might start eating softer foods that can pass through the esophagus more easily. They might avoid bread and meat, since these foods typically get stuck. The swallowing problem may even get bad enough that some people stop eating solid food completely and switch to a liquid diet. If the cancer keeps growing, at some point even liquids might be hard to swallow.
To help pass food through the esophagus, the body makes more saliva. This causes some people to complain of bringing up lots of thick mucus or saliva.
A harmless narrowing of the esophagus called a stricture can also make it difficult for you to swallow. It is important to get this symptom checked by your doctor.
Food coming back up
You may regurgitate food – this is when food comes back up soon after you swallow it. It usually starts with food like meat and bread. You may start to bring up soft foods such as mashed potato, drinks and saliva if you don’t have treatment.
Chest pain
Sometimes, people have pain or discomfort in the middle part of their chest. Some people get a feeling of pressure or burning in the chest. These symptoms are more often caused by problems other than cancer, such as heartburn, so they are rarely seen as a signal that a person might have cancer.
You can get indigestion when acid from the stomach goes back up (refluxes) into the esophagus or if the stomach is inflamed or irritated.
The valve between the stomach and esophagus normally stops this from happening. The valve is called the cardiac sphincter. A tumor that develops here can stop the valve working, causing indigestion.
Remember that indigestion is common and it’s not usually caused by cancer. It can be very painful, even when there’s nothing seriously wrong.
See your doctor if you’ve had heartburn most days for 3 weeks or more, even if you’re taking medicine and it seems to help. Heartburn is burning chest pain or discomfort that happens after eating.
Swallowing may become painful if the cancer is large enough to limit the passage of food through the esophagus. Pain may be felt a few seconds after swallowing, as food or liquid reaches the tumor and has trouble getting past it.
Weight loss
About half of people with esophageal cancer lose weight (without trying to). This happens because their swallowing problems keep them from eating enough to maintain their weight. Other factors include a decreased appetite and an increase in metabolism from the cancer.
Other symptoms
Other possible symptoms of cancer of the esophagus can include:
- Hoarseness
- Chronic cough
- Vomiting
- Hiccups
- Bone pain
- Bleeding into the esophagus. This blood then passes through the digestive tract, which may turn the stool black. Over time, this blood loss can lead to anemia (low red blood cell levels), which can make a person feel tired.
Having one or more of the symptoms above does not mean you have esophageal cancer. In fact, many of these symptoms are more likely to be caused by other conditions. Still, if you have any of these symptoms, especially trouble swallowing, it’s important to have them checked by a doctor so that the cause can be found and treated, if needed.
Esophageal cancer complications
As esophageal cancer advances, it can cause complications, such as:
- Obstruction of the esophagus. Cancer may make it difficult or impossible for food and liquid to pass through your esophagus.
- Pain. Advanced esophageal cancer can cause pain.
- Bleeding in the esophagus. Esophageal cancer can cause bleeding. Though bleeding is usually gradual, it can be sudden and severe at times.
Can Esophageal Cancer Be Found Early?
Screening is the process of looking for cancer or pre-cancer in people who have no symptoms of the disease. In the United States, screening the general public for esophageal cancer is not recommended by any professional organization at this time. This is because no screening test has been shown to lower the risk of dying from esophageal cancer in people who are at average risk.
However, people who have a high risk of esophageal cancer, such as those with Barrett’s esophagus, are often followed closely to look for early cancers and pre-cancers.
Testing people at high risk
Barrett’s esophagus
Many experts recommend that people with a high risk of esophageal cancer, such as those with Barrett’s esophagus, have upper endoscopy regularly. For this test, the doctor looks at the inside of the esophagus through a flexible lighted tube called an endoscope. The doctor may remove small samples of tissue (biopsies) from the area with Barrett’s so that they can be checked for dysplasia (pre-cancer cells) or cancer cells.
Doctors aren’t certain how often the test should be repeated, but most recommend testing more often if areas of dysplasia are found. This testing is repeated even more often if there is high-grade dysplasia (the cells appear very abnormal).
If the area of Barrett’s is large and/or there is high-grade dysplasia, treatment of the abnormal area might be advised because of the high risk that an adenocarcinoma is either already present (but was not found) or will develop within a few years. Treatment options for high-grade dysplasia might include surgery to remove part of the esophagus with the abnormal area, endoscopic mucosal resection, photodynamic therapy (PDT), or radiofrequency ablation. The outlook for these patients is relatively good after treatment.
Careful monitoring and treatment (if needed) may help prevent some esophageal cancers from developing. It may also detect some cancers early, when they are more likely to be treated successfully.
Inherited syndromes
People with inherited syndromes (sometimes called hereditary syndromes) that put them at increased risk of developing esophageal cancer, might also need frequent endoscopies to look for cancer or pre-cancer. For example, people with tylosis or Bloom syndrome should consider screening with an upper endoscopy after turning 20 years old. People who have family members with familial (inherited) Barrett’s esophagus should consider screening with an upper endoscopy after 40 years old. If you have one of these inherited syndromes, it is best to speak with your doctor about cancer screening and what is right for you.
Careful monitoring and treatment (if needed) may help prevent some esophageal cancers from developing. It may also detect some cancers early, when they are more likely to be treated successfully.
Esophageal cancer diagnosis
Esophagus cancers are usually found because of signs or symptoms a person is having. If esophagus cancer is suspected, exams and tests will be needed to confirm the diagnosis. If cancer is found, further tests will be done to help determine the extent (stage) of the cancer.
Medical history and physical exam
If you have symptoms that might be caused by esophageal cancer, the doctor will ask about your medical history to check for possible risk factors and to learn more about your symptoms.
Your doctor will also examine you to look for possible signs of esophageal cancer and other health problems. He or she will probably pay special attention to your neck and chest areas.
If the results of the exam are abnormal, your doctor will probably order tests to help find the problem. You may also be referred to a gastroenterologist (a doctor specializing in digestive system diseases) for further tests and treatment.
Imaging tests to look for esophagus cancer
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive substances to create pictures of the inside of your body. Imaging tests might be done for many reasons, such as:
- To help find a suspicious area that might be cancer
- To learn if and how far cancer has spread
- To help determine if the treatment is working
- To look for possible signs of cancer coming back after treatment
Barium swallow
In this test, a thick, chalky liquid called barium is swallowed to coat the walls of the esophagus. When x-rays are then taken, the barium clearly outlines the esophagus. This test can be done by itself, or as a part of a series of x-rays that includes the stomach and part of the intestine, called an upper gastrointestinal (GI) series. A barium swallow test can show any abnormal areas in the normally smooth surface of the inner lining of the esophagus, but it can’t be used to determine how far a cancer may have spread outside of the esophagus.
This is sometimes the first test done to see what is causing a problem with swallowing. Even small, early cancers can often be seen using this test. Early cancers can look like small round bumps or flat, raised areas (called plaques), while advanced cancers look like large irregular areas and can cause narrowing of the inside of the esophagus.
This test can also be used to diagnose one of the more serious complications of esophageal cancer called a tracheo-esophageal fistula. This occurs when the tumor destroys the tissue between the esophagus and the trachea (windpipe) and creates a hole connecting them. Anything that is swallowed can then pass from the esophagus into the windpipe and lungs. This can lead to frequent coughing, gagging, or even pneumonia. This problem can be helped with surgery or an endoscopy procedure.
Computed tomography (CT or CAT) scan
A CT scan uses x-rays to produce detailed cross-sectional images of your body. This test can help tell if esophageal cancer has spread to nearby organs and lymph nodes (bean-sized collections of immune cells to which cancers often spread first) or to distant parts of the body.
Before the test, you may be asked to drink 1 to 2 pints of a liquid called oral contrast. This helps outline the esophagus and intestines. If you are having any trouble swallowing, you need to tell your doctor before the scan.
Magnetic resonance imaging (MRI) scan
Like CT scans, MRI scans provide detailed images of soft tissues in the body. But MRI scans use radio waves and strong magnets instead of x-rays. A contrast material called gadolinium may be injected into a vein before the scan to see details better. MRI can be used to look at abnormal areas in the brain and spinal cord that might be due to cancer spread.
Positron emission tomography (PET) scan
PET scans usually use a form of radioactive sugar (known as fluorodeoxyglucose or FDG) that is injected into the blood. Normal cells use different amounts of the sugar, depending on how fast they are growing. Cancer cells, which grow quickly, are more likely to absorb larger amounts of the radioactive sugar than normal cells. These areas of radioactivity can be seen on a PET scan using a special camera.
The picture from a PET scan is not as detailed as a CT or MRI scan, but it provides helpful information about whether abnormal areas seen on these other tests are likely to be cancer or not.
If you have already been diagnosed with cancer, your doctor may use this test to see if the cancer has spread to lymph nodes or other parts of the body. A PET scan can also be useful if your doctor thinks the cancer may have spread but doesn’t know where.
PET/CT scan: Some machines can do both a PET and CT scan at the same time. This lets the doctor compare areas of higher radioactivity on the PET scan with the more detailed picture of that area on the CT scan.
Endoscopy
An endoscope is a flexible, narrow tube with a tiny video camera and light on the end that is used to look inside the body. Tests that use endoscopes can help diagnose esophageal cancer or determine the extent of its spread.
Upper endoscopy
This is an important test for diagnosing esophageal cancer. During an upper endoscopy, you are sedated (made sleepy) and then the doctor passes an endoscope down yourthroat and into the esophagus and stomach. The camera is connected to a monitor, which lets the doctor see any abnormal areas in the wall of the esophagus clearly.
The doctor can use special instruments through the scope to remove (biopsy) samples from any abnormal areas. These samples are sent to the lab to see if they contain cancer.
If the esophageal cancer is blocking the opening (called the lumen) of the esophagus, certain instruments can be used to help enlarge the opening to help food and liquid pass.
Upper endoscopy can give the doctor important information about the size and spread of the tumor, which can be used to help determine if the tumor can be removed with surgery.
Endoscopic ultrasound
This test is usually done at the same time as the upper endoscopy. For an endoscopic ultrasound, a probe that gives off sound waves is at the end of an endoscope. This allows the probe to get very close to tumors in the esophagus. This test is very useful in determining the size of an esophageal cancer and how far it has grown into nearby areas. It can also help show if nearby lymph nodes might be affected by the cancer. If enlarged lymph nodes are seen on the ultrasound, the doctor can pass a thin, hollow needle through the endoscope to get biopsy samples of them. This helps the doctor decide if the tumor can be removed with surgery.
Bronchoscopy
This exam may be done for cancer in the upper part of the esophagus to see if it has spread to the windpipe (trachea) or the tubes leading from the windpipe into the lungs (bronchi).
Thoracoscopy and laparoscopy
These exams let the doctor see lymph nodes and other organs near the esophagus inside the chest (by thoracoscopy) or the abdomen (by laparoscopy) through a hollow lighted tube.
These procedures are done in an operating room while you are under general anesthesia (in a deep sleep). A small incision (cut) is made in the side of the chest wall (for thoracoscopy) or the abdomen (for laparoscopy). Sometimes more than one cut is made. The doctor then inserts a thin, lighted tube with a small video camera on the end through the incision to view the space around the esophagus. The surgeon can pass thin tools into the space to remove lymph nodes and biopsy samples to see if the cancer has spread. This information is often important in deciding whether a person is likely to benefit from surgery.
Lab tests of biopsy samples
Usually if a suspected esophageal cancer is found on endoscopy or an imaging test, it is biopsied. In a biopsy, the doctor removes a small piece of tissue with a special instrument passed through the scope.
HER2 testing
If esophageal cancer is found but is too advanced for surgery, your biopsy samples may be tested for the HER2 gene or protein. Some people with esophageal cancer have too much of the HER2 protein on the surface of their cancer cells, which helps the cells grow. A drug that targets the HER2 protein called trastuzumab (Herceptin®) may help treat these cancers when used along with chemotherapy. Only cancers that have too much of the HER2 gene or protein are likely to be affected by this drug, which is why doctors may test tumor samples for it.
PD-L1 testing
An esophageal cancer that cannot be treated with surgery or has spread to distant sites may be tested to see if it makes a checkpoint protein called PD-L1. This protein is found in 35% to 45% of esophageal cancers. Tumors that make this protein might be treated with the immunotherapy drug pembrolizumab.
MMR and MSI testing
Esophageal cancer cells might be tested to see if they show high levels of gene changes called microsatellite instability (MSI), or if they have changes in any of the mismatch repair (MMR) genes (MLH1, MSH2, MSH6, and PMS2).
Esophageal cancers that test positive for mismatch repair (MMR) or high microsatellite instability (MSI) and cannot be treated with surgery, have come back after initial treatment, or have spread to other parts of the body might benefit from immunotherapy with the drug pembrolizumab.
Blood tests
Your doctor might order certain blood tests to help determine if you have esophageal cancer.
Complete blood count (CBC): This test measures the different types of cells in your blood. It can show if you have anemia (too few red blood cells). Some people with esophageal cancer become anemic because the tumor has been bleeding.
Liver enzymes: You may also have a blood test to check your liver function, because esophageal cancer can spread to the liver.
Blood tests
Your doctor might order certain blood tests to help determine if you have esophageal cancer.
Complete blood count (CBC): This test measures the different types of cells in your blood. It can show if you have anemia (too few red blood cells). Some people with esophageal cancer become anemic because the tumor has been bleeding.
Liver enzymes: You may also have a blood test to check your liver function, because esophageal cancer can spread to the liver.
Esophageal cancer staging
After someone is diagnosed with esophageal cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how big it is and whether it has spread. It helps determine how serious the cancer is and how best to treat it. Doctors also use a cancer’s stage when talking about survival statistics.
The earliest stage esophageal cancers are called stage 0 (high grade dysplasia). It then ranges from stage I (1) through IV (4). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV, means cancer has spread more. And within a stage, an earlier letter means a lower stage. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
Most esophageal cancers start in the innermost lining of the esophagus (the epithelium) and then grow into deeper layers over time.
How is the esophageal cancer stage determined?
The staging system most often used for esophageal cancer is the American Joint Committee on Cancer (AJCC) TNM system, which is based on 3 key pieces of information:
- The extent (size) of the tumor (T): How far has the cancer grown into the wall of the esophagus? Has the cancer reached nearby structures or organs?
- The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes?
- The spread (metastasis) to distant sites (M): Has the cancer spread to distant lymph nodes or distant organs such as the lungs or liver?
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once a person’s T, N, and M categories have been determined, this information is combined in a process called stage grouping to assign an overall stage.
Staging systems for esophageal cancer
Since esophageal cancer can be treated in different ways, different staging systems have been created for each situation 20:
- Pathological stage also called the surgical stage: Pathological staging means the doctor stages you after examining the tissue that the surgeon removes during an operation. You might see your pathological stage written as pTNM. Your doctors combine your clinical stage results with the surgical results. Pathological staging is generally a more precise way to find out how far your cancer has spread.
- Clinical stage: If surgery might not be possible or will be done after other treatment is given, then the clinical stage is determined based on the results of a physical exam, biopsy, and imaging tests. Clinical staging means the doctor stages you after examining you and looking at test and scan results. You might see your clinical stage written as cTNM. The clinical stage will be used to help plan treatment, but it might not predict outlook as accurately as the pathological stage (surgical stage). This is because sometimes the cancer has spread further than the clinical stage estimates.
- Postneoadjuvant stage: Post neoadjuvant staging means you have had chemotherapy or radiotherapy before surgery (neoadjuvant therapy) and the doctor stages you again after surgery. You might see your post neoadjuvant stage written as ypTNM.
Since most cancers are staged with the pathological stage (surgical stage), we have included that staging system in the tables below. If your cancer has been clinically staged or if you have had neoadjuvant therapy, it is best to talk to your doctor about your specific stage for those situations.
Grade
Another factor that can affect your treatment and your outlook is the grade of your cancer. The grade describes how closely the cancer looks like normal tissue when seen under a microscope.
The scale used for grading esophagus cancers is from 1 to 3.
- GX: The grade cannot be assessed. (The grade is unknown).
- Grade 1 (G1: well differentiated) means the cancer cells look more like normal esophagus tissue. In grade 1, the cancer cells look more like normal cells under a microscope and grow and spread more slowly than grade 2 and 3 cancer cells.
- Grades 2 (G2: moderately differentiated) falls somewhere in between G1 and G3. In grade 2, the cancer cells look more abnormal under a microscope and grow and spread more quickly than grade 1 cancer cells.
- Grade 3 (G3: poorly differentiated, undifferentiated) means the cancer cells look very abnormal. In grade 3, the cancer cells look more abnormal under a microscope and grow and spread more quickly than grade 1 and 2 cancer cells.
The grade is often simplified as either low grade (G1) or high grade (G3).
Low-grade cancers tend to grow and spread more slowly than high-grade cancers. Most of the time, the outlook is better for low-grade cancers than it is for high-grade cancers of the same stage.
Differentiation
Doctors sometimes use the terms well differentiated, moderately differentiated or poorly differentiated to describe the grade of your cancer. As normal cells grow and mature, they become specialised for their role and place in the body. This is called differentiation.
Cancer cells can look very like normal cells and are described as well differentiated or low grade. These cancers are more likely to grow slowly.
If the cancer cells look underdeveloped and nothing like a normal cell, they are known as undifferentiated or high grade. These cancers tend to grow and spread more quickly than low grade cancers.
Location
Some stages of early squamous cell carcinoma also take into account where the tumor is in the esophagus. The location is assigned as either upper, middle, or lower based on where the middle of the tumor is.
Esophageal cancer stage descriptions
The 2 main types of esophageal cancer are squamous cell cancer and adenocarcinoma. Doctors stage esophageal squamous cell cancers in a different way to esophageal adenocarcinomas.
The tables below are simplified versions of the TNM system, based on the most recent American Joint Committee on Cancer (AJCC) systems effective January 2018. They include staging systems for squamous cell carcinoma and adenocarcinoma. It’s important to know that esophageal cancer staging can be complex. If you have any questions about the stage of your cancer or what it means, please ask your doctor to explain it to you in a way you understand.
Table 1. Squamous Cell Carcinoma Stages
| AJCC Stage | Stage description SQUAMOUS CELL CARCINOMA |
|---|---|
| 0 | The cancer is only in the epithelium (the top layer of cells lining the inside of the esophagus). It has not started growing into the deeper layers. This stage is also known as high-grade dysplasia. It has not spread to any lymph nodes or distant organs. The cancer grade does not apply. The cancer can be located anywhere in the esophagus. |
| IA (1A) | The cancer is growing into the lamina propria or muscularis mucosa (the tissue under the epithelium). It has not spread to any lymph nodes or distant organs. The cancer is grade 1 or an unknown grade and located anywhere in the esophagus. |
| IB (1B) | The cancer is growing into the lamina propria, muscularis mucosa (the tissue under the epithelium), submucosa or the thick muscle layer (muscularis propria). It has not spread to nearby lymph nodes or to distant organs. The cancer can be any grade or an unknown grade and located anywhere in the esophagus. |
| IIA (2A) | The cancer is growing into the thick muscle layer (muscularis propria). It has not spread to nearby lymph nodes or to distant organs. The cancer can be grade 2 or 3 or an unknown grade and located anywhere in the esophagus. |
| OR | |
| The cancer is growing into the outer layer of the esophagus (the adventitia). It has not spread to nearby lymph nodes or to distant organs. The cancer can be any of the following:
| |
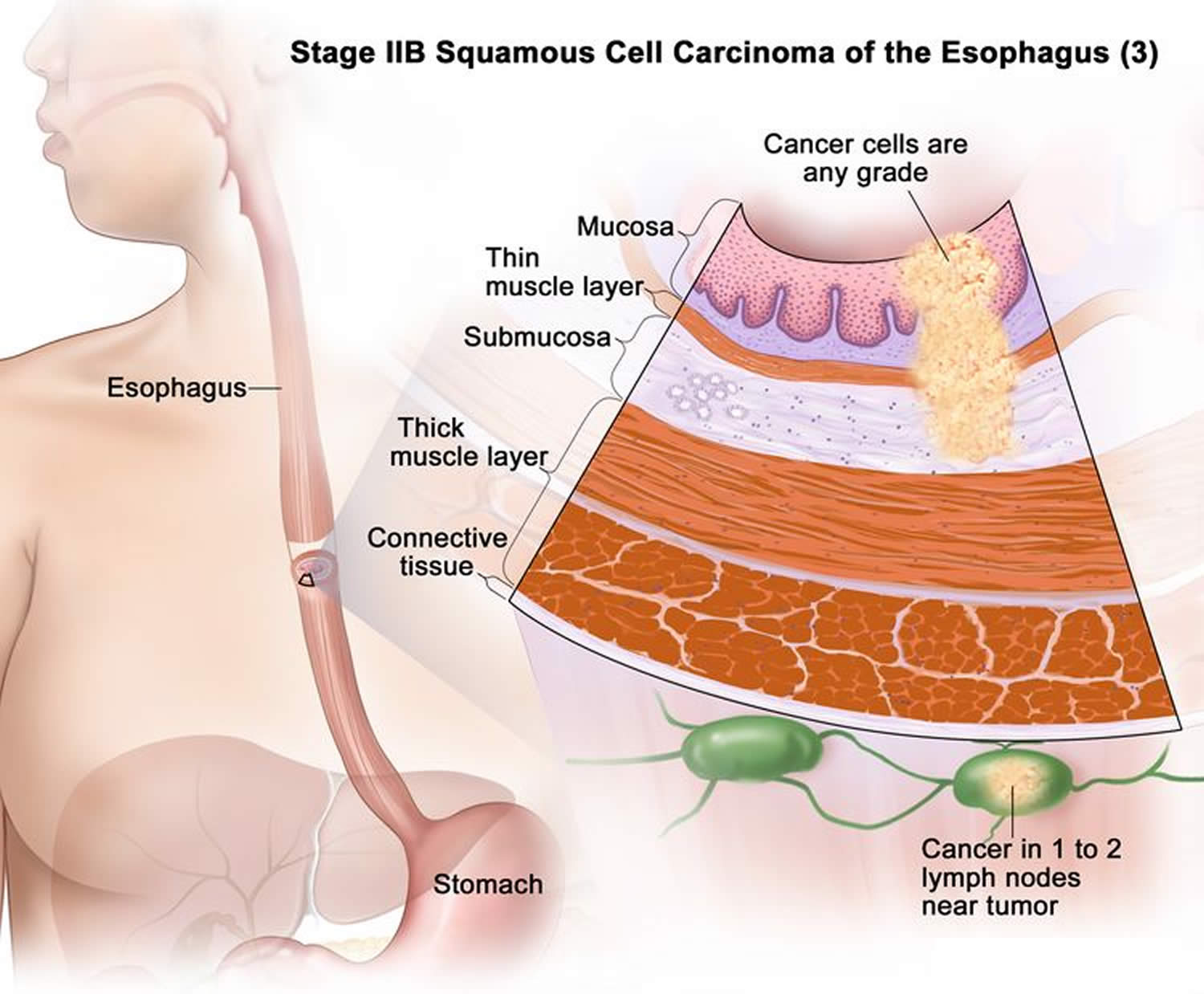
| IIB (2B)
| The cancer is growing into the outer layer of the esophagus (the adventitia). It has not spread to nearby lymph nodes or to distant organs. The cancer can be any of the following:
|
| OR | |
| The cancer is growing into the lamina propria, muscularis mucosa (the tissue under the epithelium) or into the submucosa. It has spread to 1 or 2 nearby lymph nodes. The cancer can be any grade and located anywhere in the esophagus. | |
| IIIA (3A) | The cancer is growing into the lamina propria, muscularis mucosa (the tissue under the epithelium), submucosa or the thick muscle layer (muscularis propria). It has spread to no more than 6 nearby lymph nodes. It has not spread to distant organs. The cancer can be any grade and located anywhere in the esophagus. |
| IIIB (3B) | The cancer is growing into:
It has not spread to distant organs. The cancer can be any grade and located anywhere in the esophagus. |
| IVA (4A) | The cancer is growing into:
It has not spread to distant organs. The cancer can be any grade and located anywhere in the esophagus. |
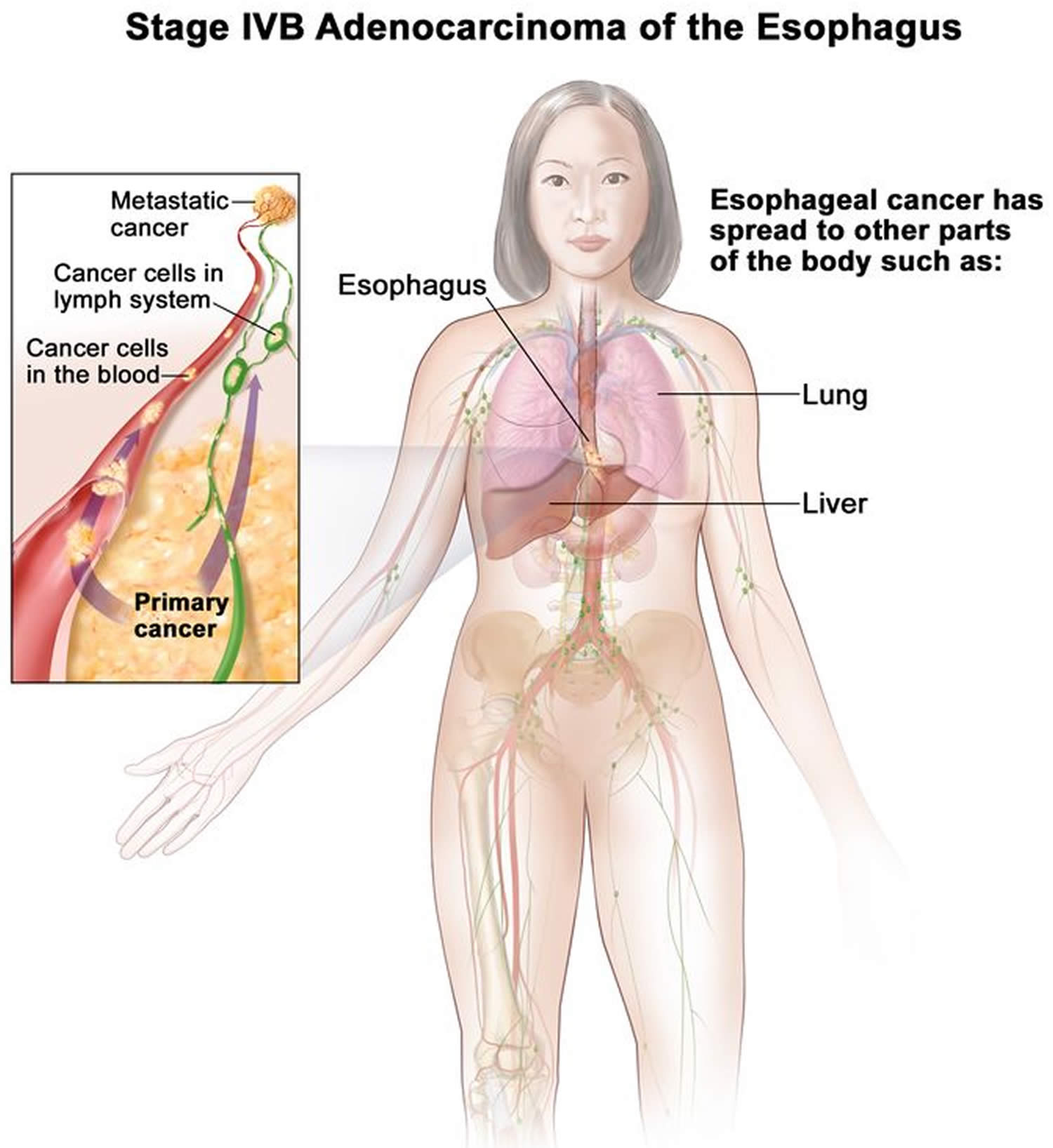
| IVB (4B) | The cancer has spread to distant lymph nodes and/or other organs. such as the liver and lungs. The cancer can be any grade and located anywhere in the esophagus. |
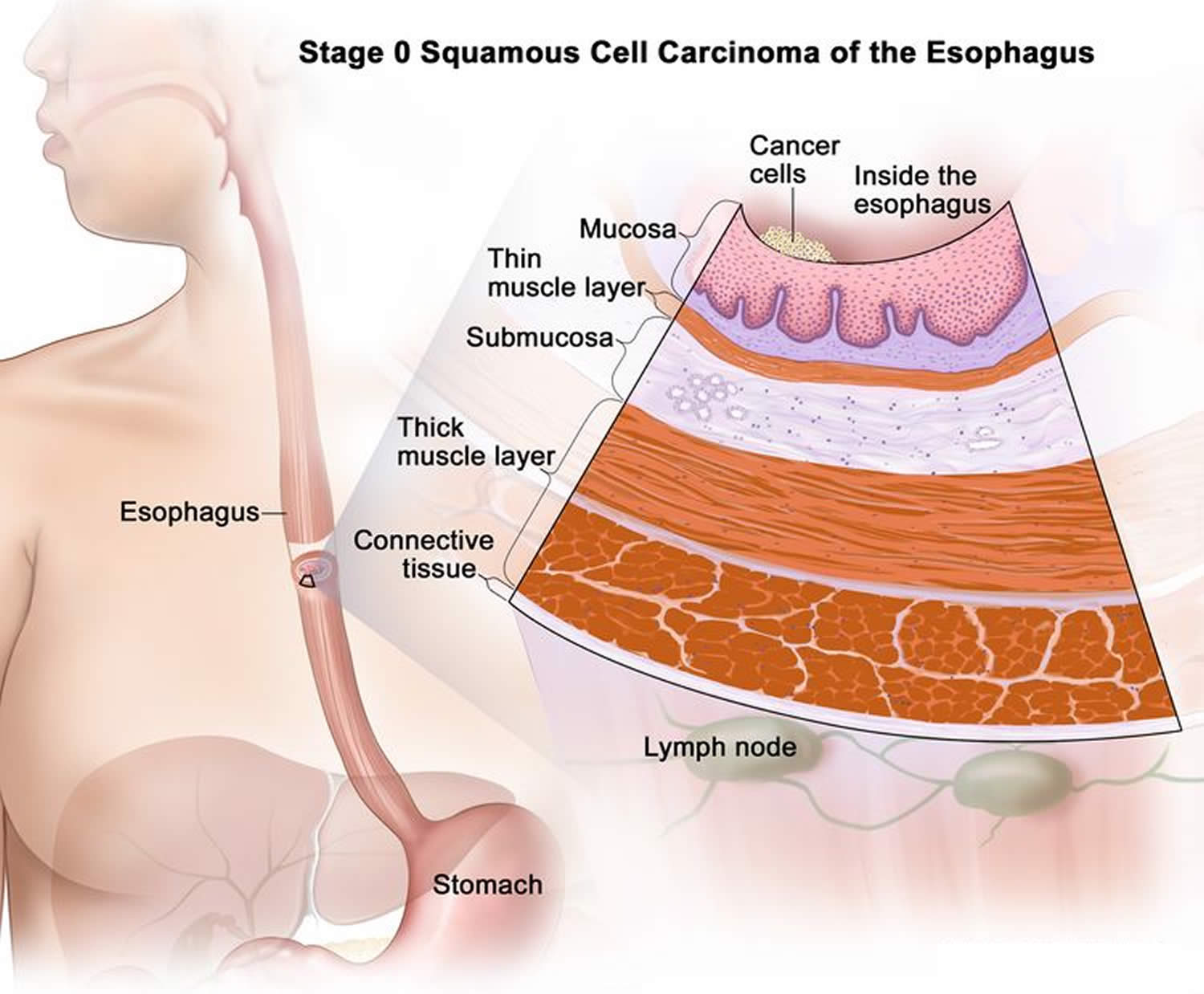
Stage 0 (High-grade Dysplasia) squamous cell carcinoma of the esophagus
In stage 0, cancer has formed in the inner lining of the esophagus wall. Stage 0 is also called high-grade dysplasia.
Figure 8. Stage 0 squamous cell carcinoma of the esophagus
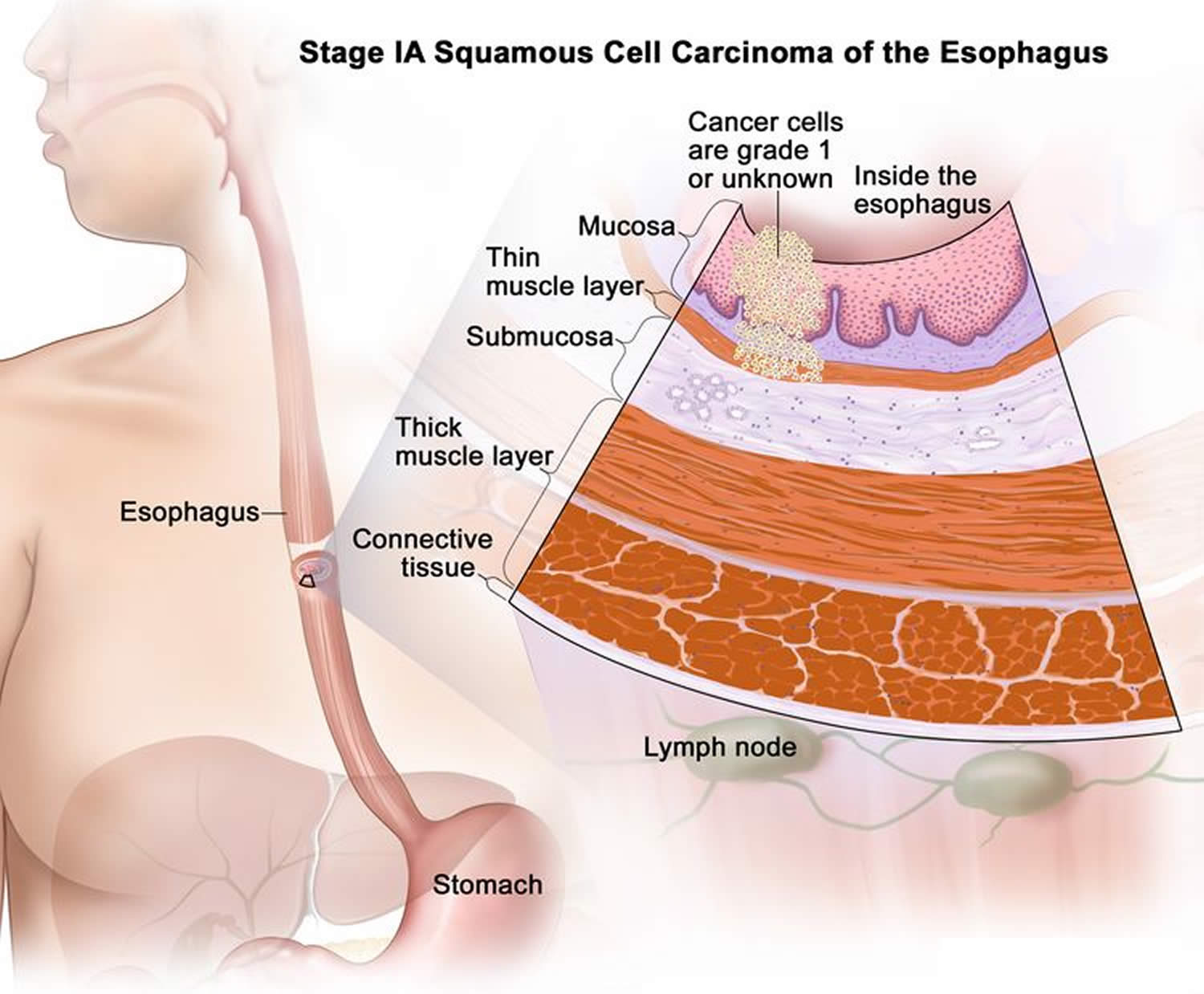
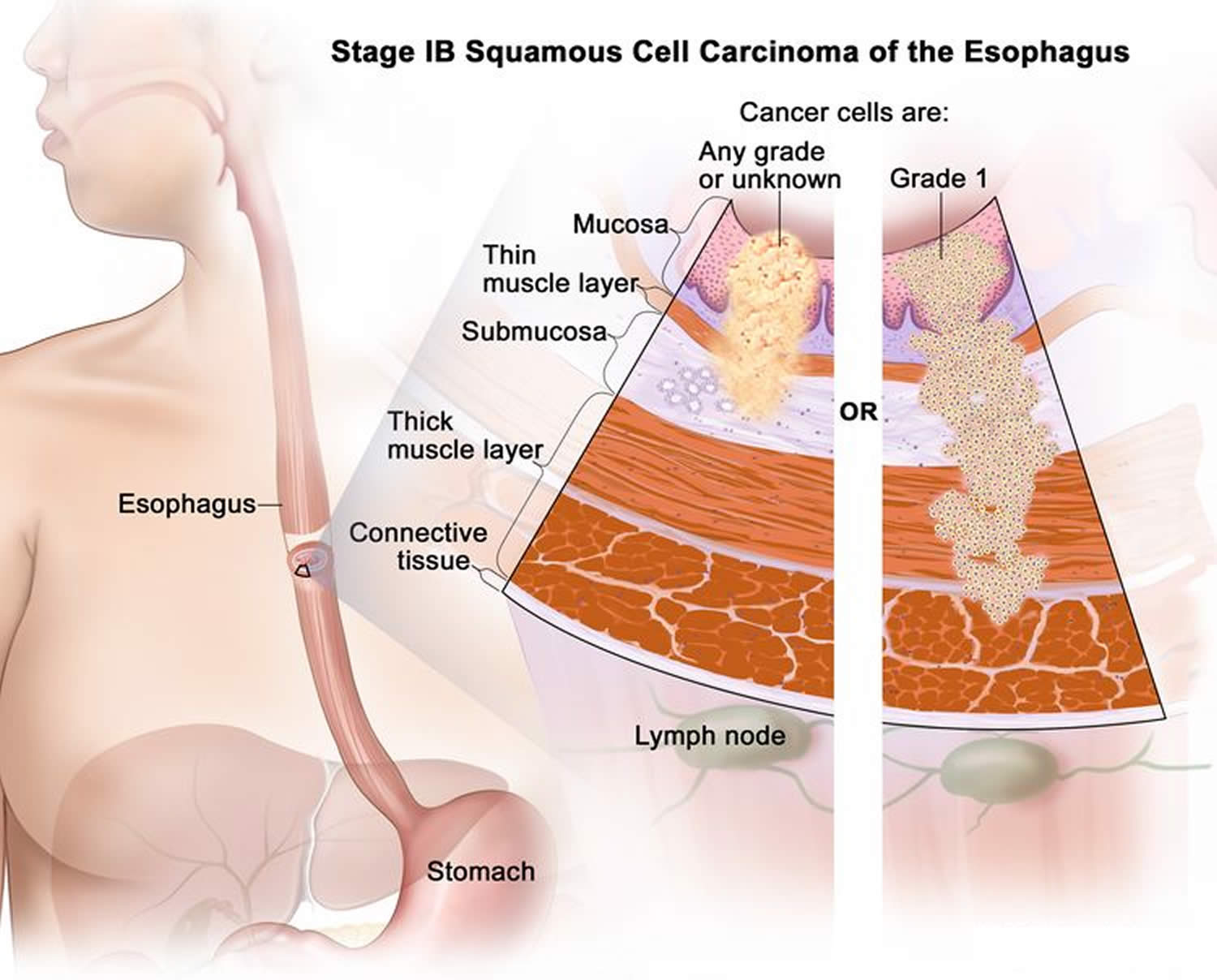
Stage 1 squamous cell carcinoma of the esophagus
Stage 1 squamous cell carcinoma of the esophagus is divided into stages 1A and 1B, depending on where the cancer has spread.
- Stage 1A: Cancer has spread into the mucosa layer or thin muscle layer of the esophagus wall. The cancer cells are grade 1 or the grade is not known.
- Stage 1B: Cancer has spread:
- into the mucosa layer, thin muscle layer, or submucosa layer of the esophagus wall. The cancer cells are any grade or the grade is not known; or
- into the thick muscle layer of the esophagus wall. The cancer cells are grade 1.
Figure 9. Stage 1A squamous cell carcinoma of the esophagus
Figure 10. Stage 1B squamous cell carcinoma of the esophagus
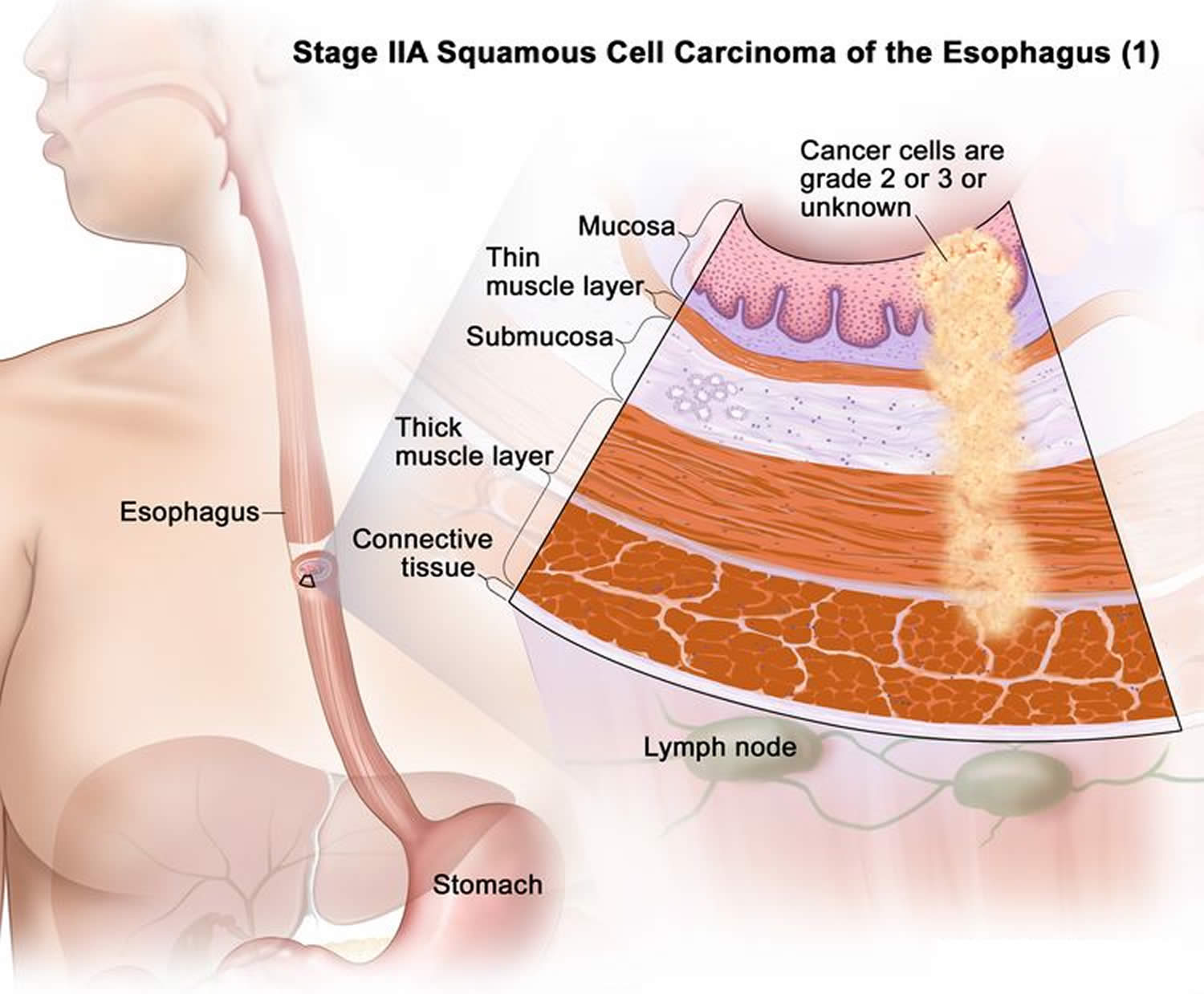
Stage 2 squamous cell carcinoma of the esophagus
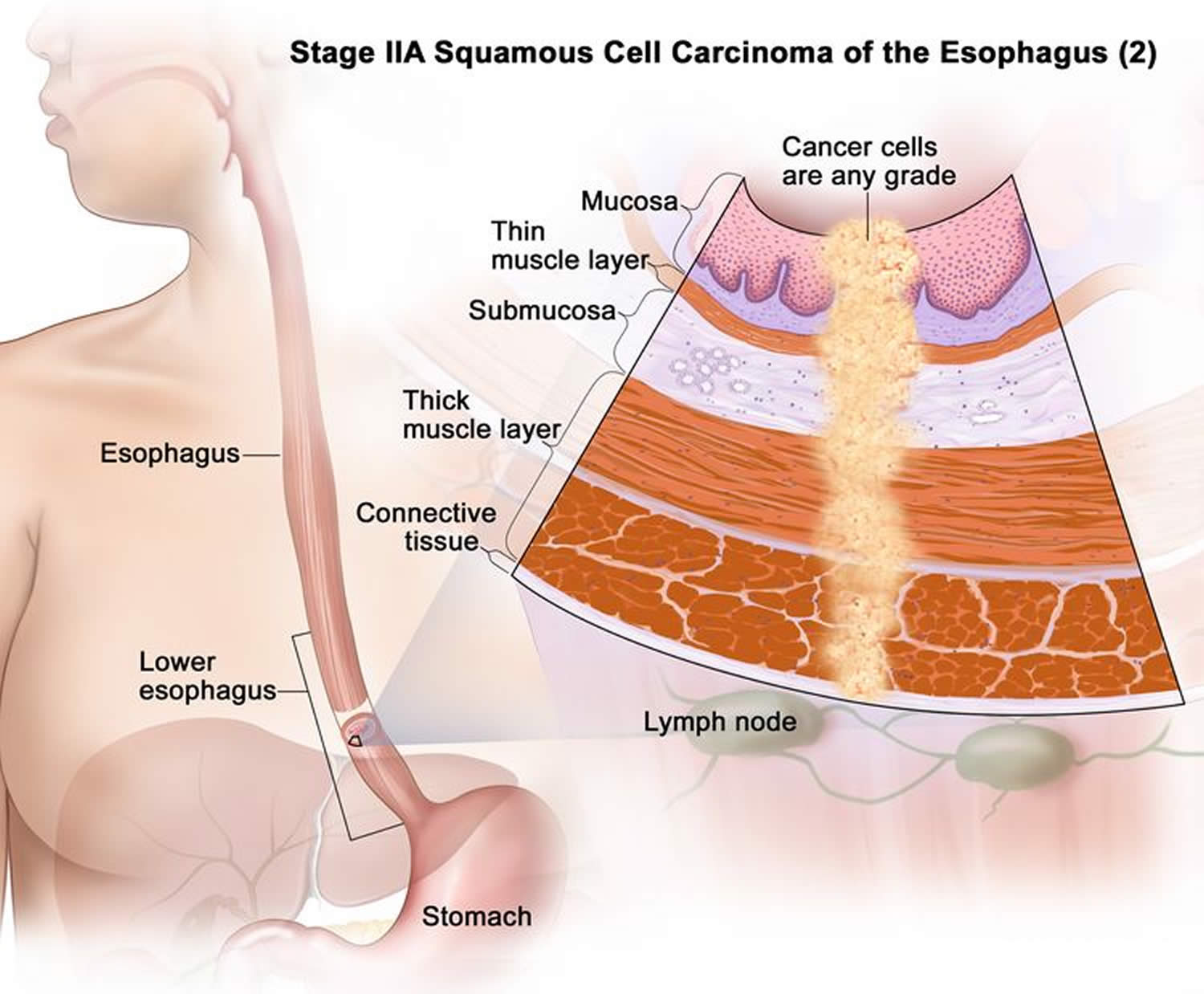
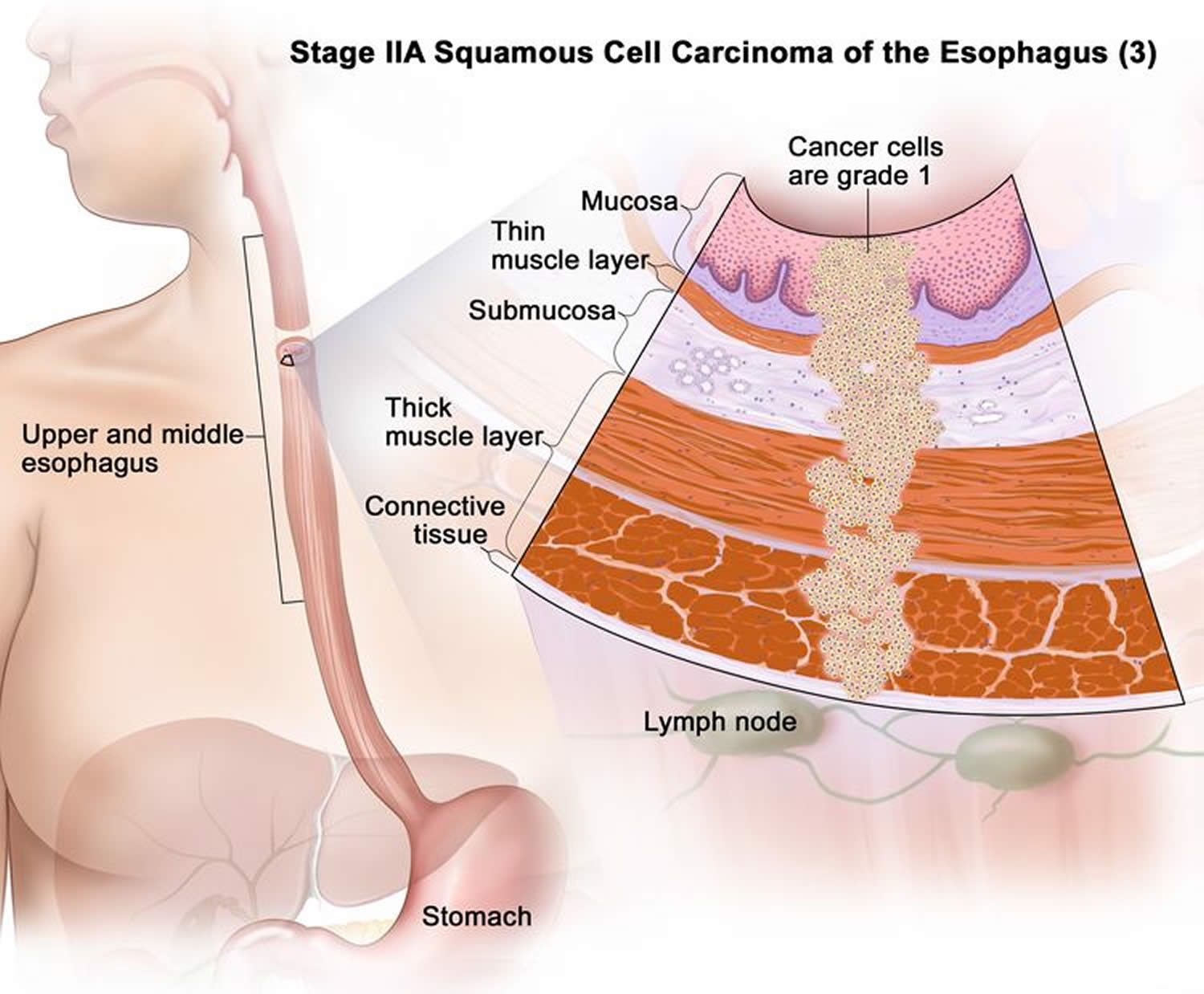
Stage 2 is divided into stages 2A and 2B, depending on where the cancer has spread.
- Stage 2A cancer has spread:
- into the thick muscle layer of the esophagus wall. The cancer cells are grade 2 or 3 or the grade is not known (Figure 11); or
- into the connective tissue layer of the esophagus wall. The tumor is in the lower esophagus (Figure 12); or
- into the connective tissue layer of the esophagus wall. The cancer cells are grade 1. The tumor is in either the upper or middle esophagus (Figure 13).
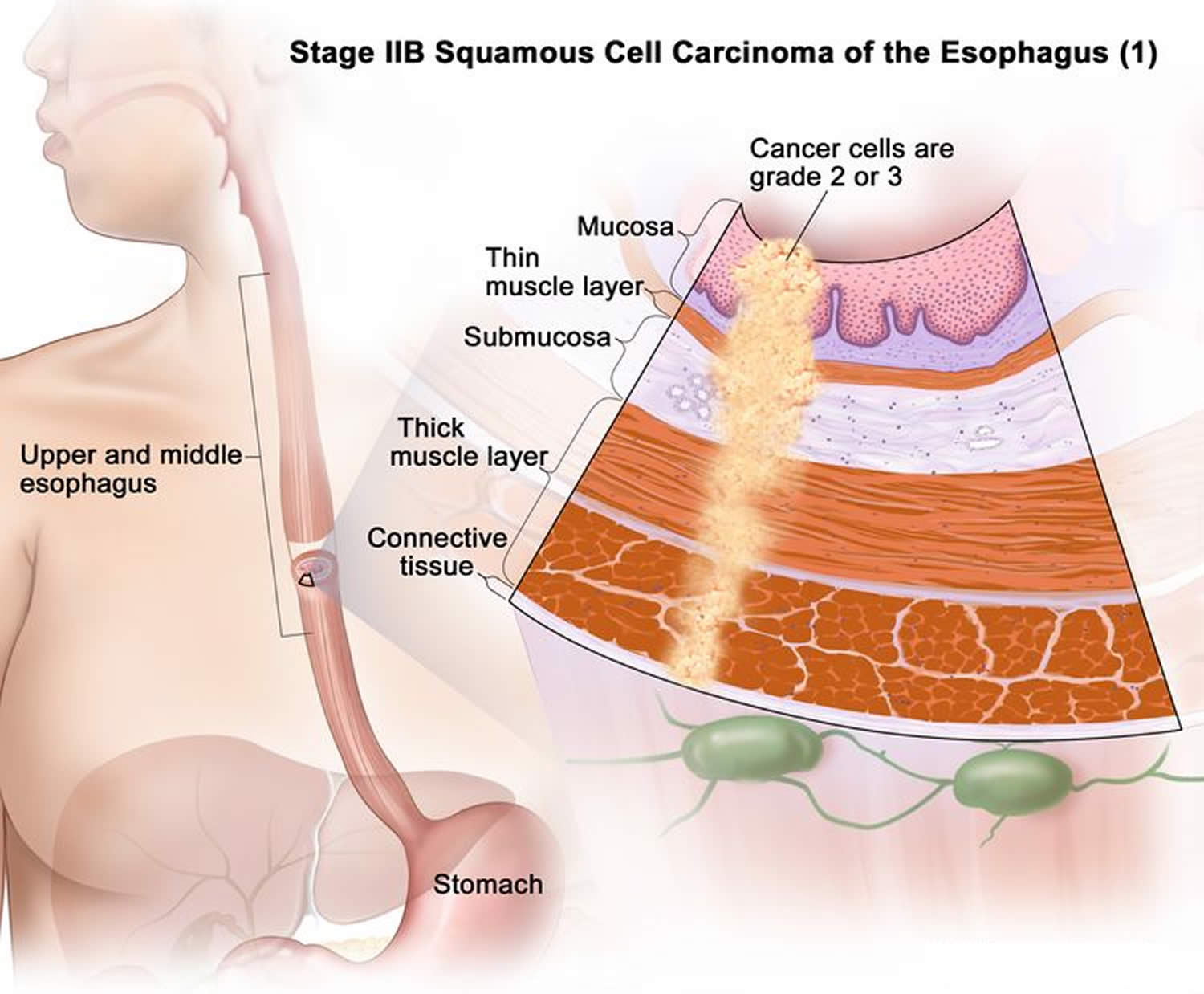
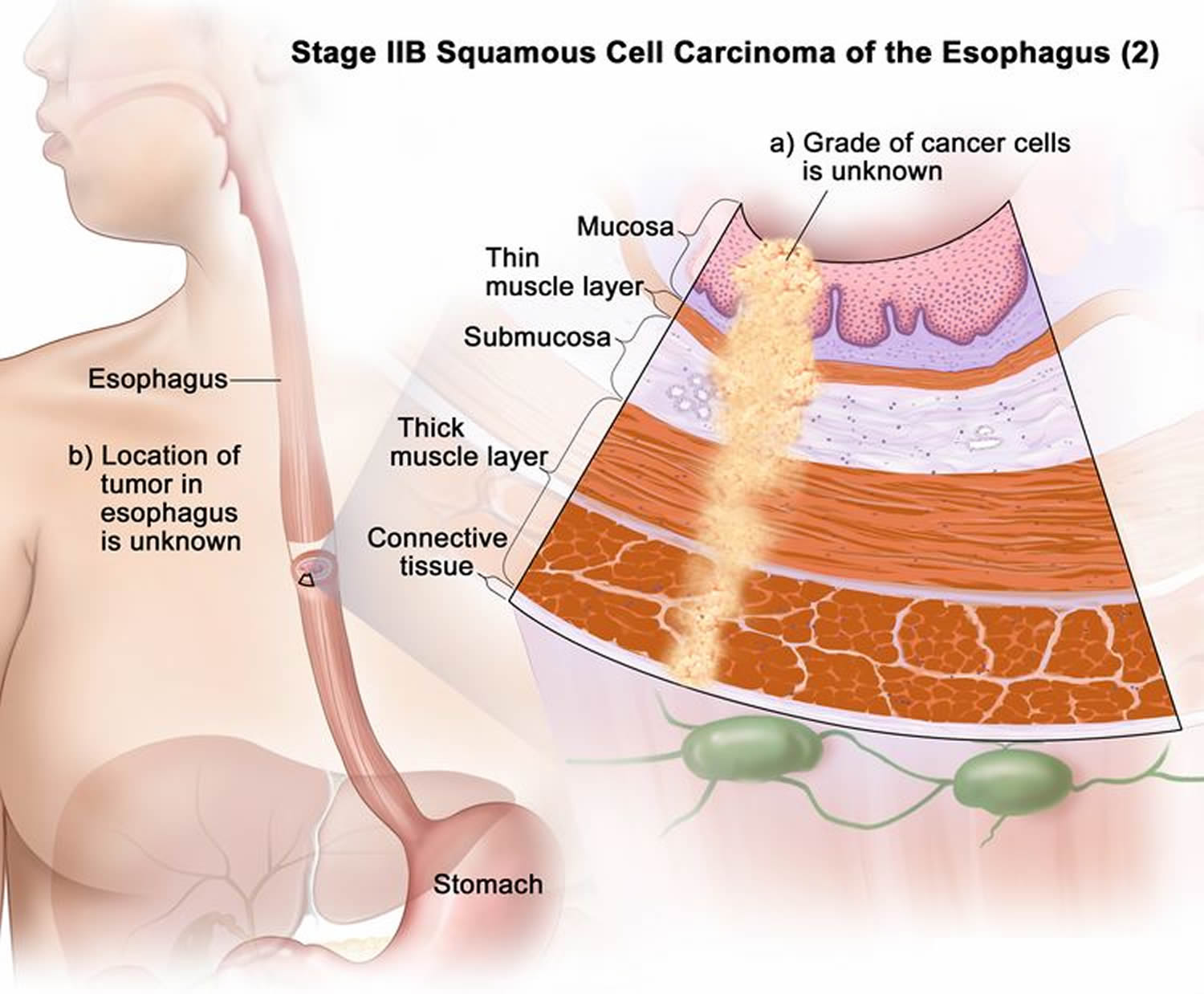
- Stage 2B cancer has spread:
- into the connective tissue layer of the esophagus wall. The cancer cells are grade 2 or 3. The tumor is in either the upper or middle esophagus (Figure 14); or
- into the connective tissue layer of the esophagus wall. The grade of the cancer cells is not known, or it is not known where the tumor has formed in the esophagus (Figure 15); or
- into the mucosa layer, thin muscle layer, or submucosa layer of the esophagus wall. Cancer is found in 1 or 2 lymph nodes near the tumor (Figure 16).
Figure 11. Stage 2A squamous cell carcinoma of the esophagus
Figure 12. Stage 2A squamous cell carcinoma of the esophagus
Figure 13. Stage 2A squamous cell carcinoma of the esophagus
Figure 14. Stage 2B squamous cell carcinoma of the esophagus
Figure 15. Stage 2B squamous cell carcinoma of the esophagus
Figure 16. Stage 2B squamous cell carcinoma of the esophagus
Stage 3 squamous cell carcinoma of the esophagus
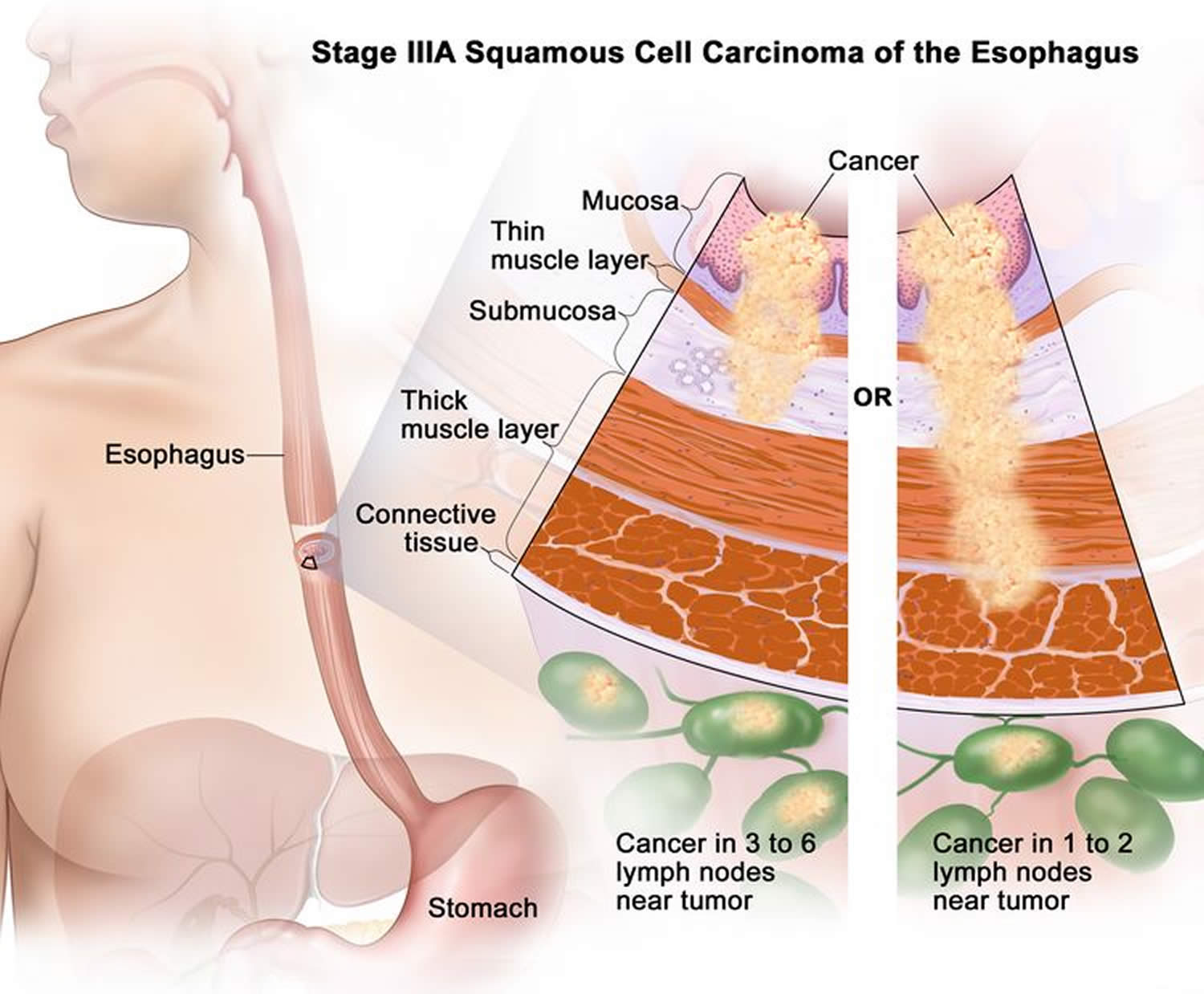
Stage 3 is divided into stages 3A and 3B, depending on where the cancer has spread.
- Stage 3A cancer has spread (Figure 17):
- into the mucosa layer, thin muscle layer, or submucosa layer of the esophagus wall. Cancer is found in 3 to 6 lymph nodes near the tumor; or
- into the thick muscle layer of the esophagus wall. Cancer is found in 1 or 2 lymph nodes near the tumor.
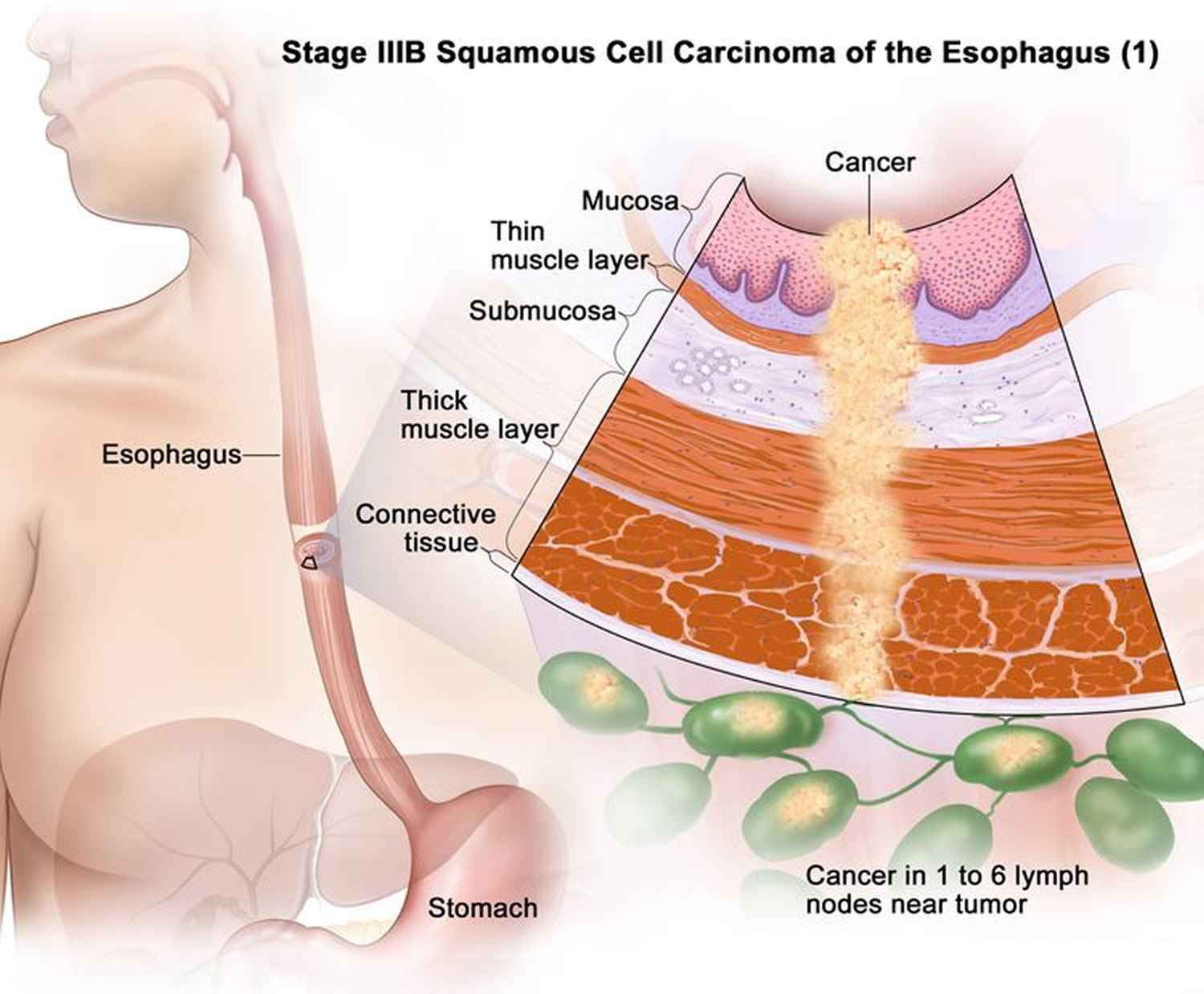
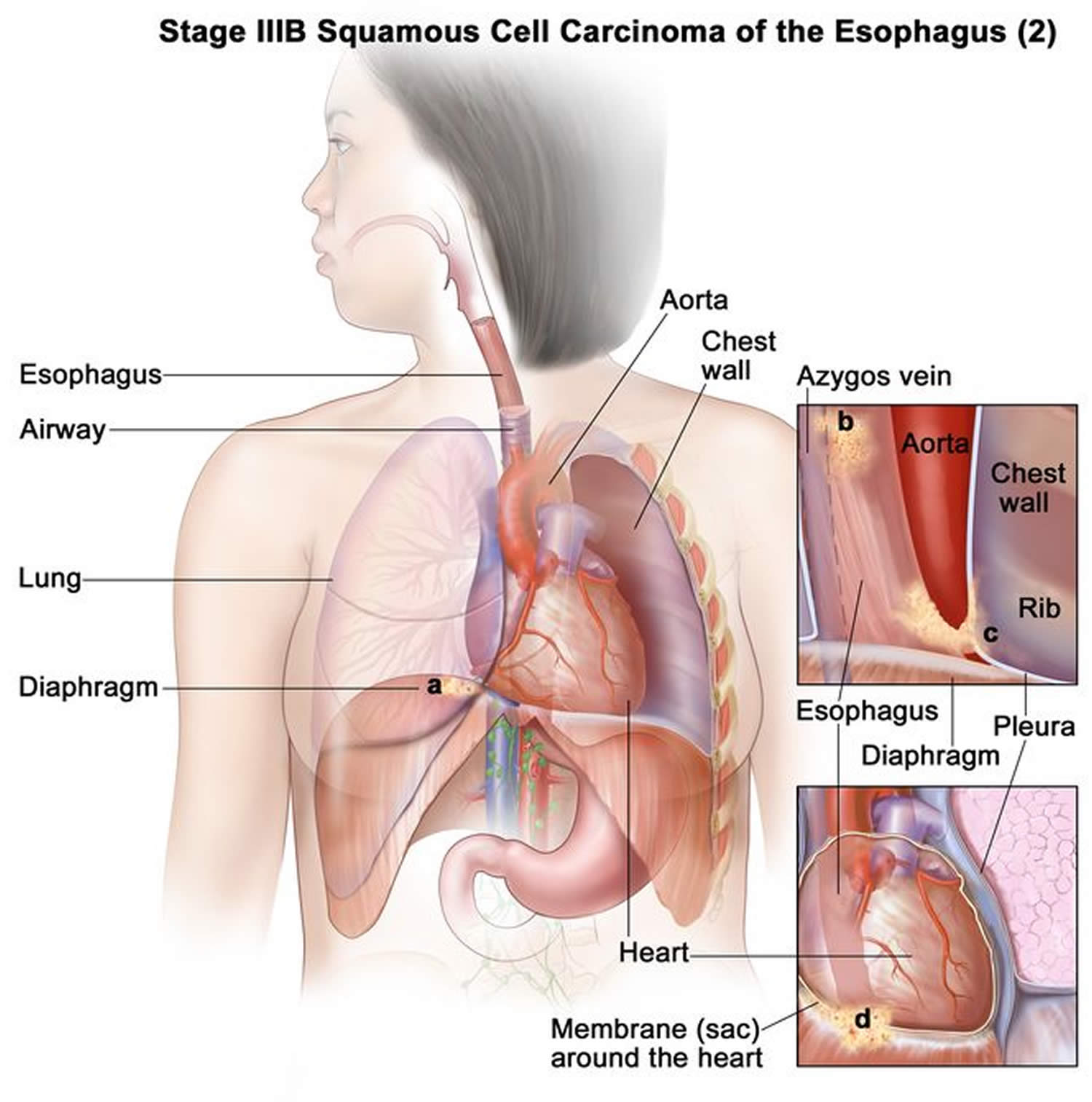
- Stage 3B cancer has spread:
- into the thick muscle layer or the connective tissue layer of the esophagus wall. Cancer is found in 1 to 6 lymph nodes near the tumor (Figure 18); or
- into the diaphragm, azygos vein, pleura, sac around the heart, or peritoneum. Cancer may be found in 0 to 2 lymph nodes near the tumor (Figure 19).
Figure 17. Stage 3A squamous cell carcinoma of the esophagus
Figure 18. Stage 3B squamous cell carcinoma of the esophagus
Figure 19. Stage 3B squamous cell carcinoma of the esophagus
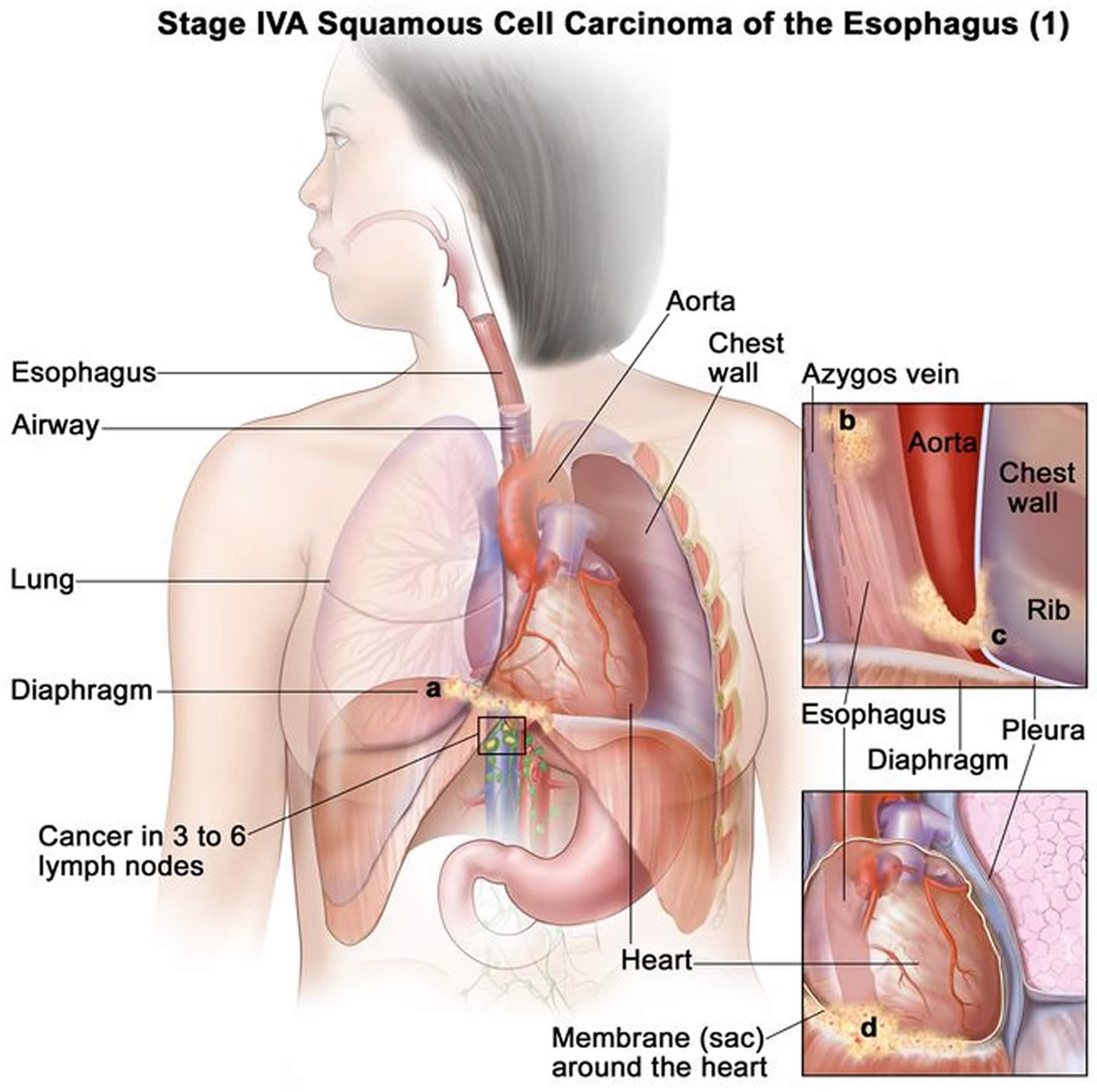
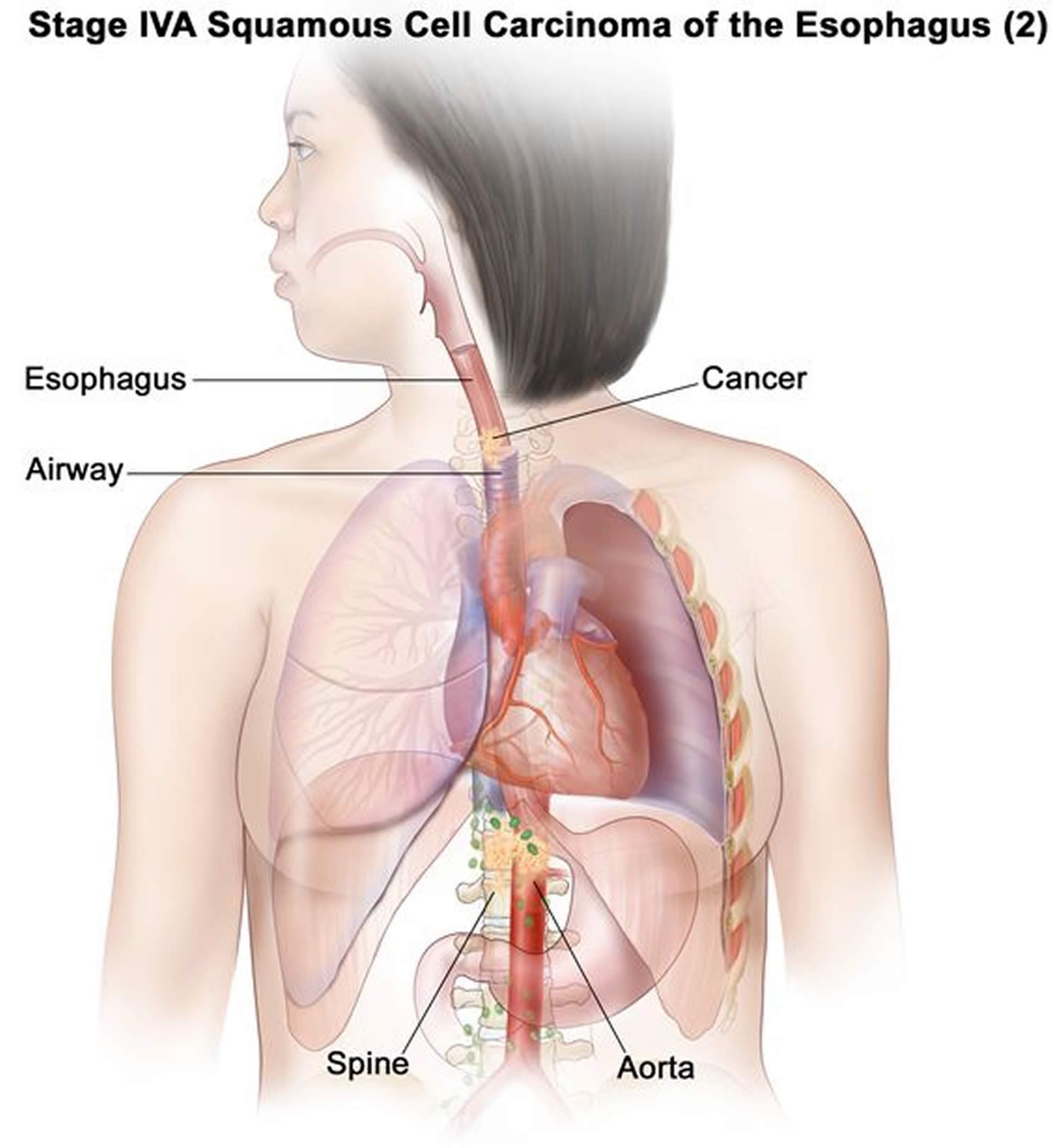
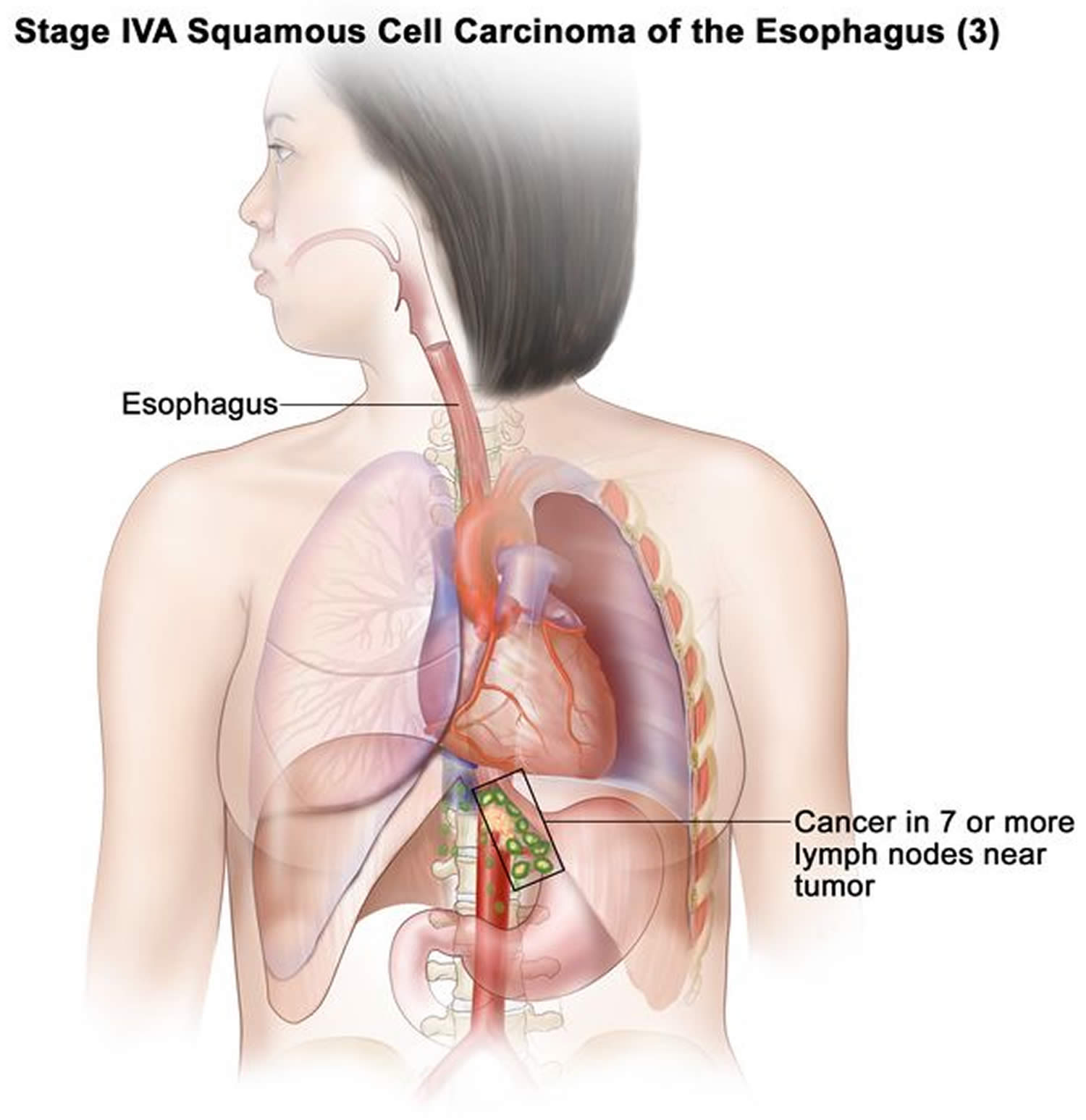
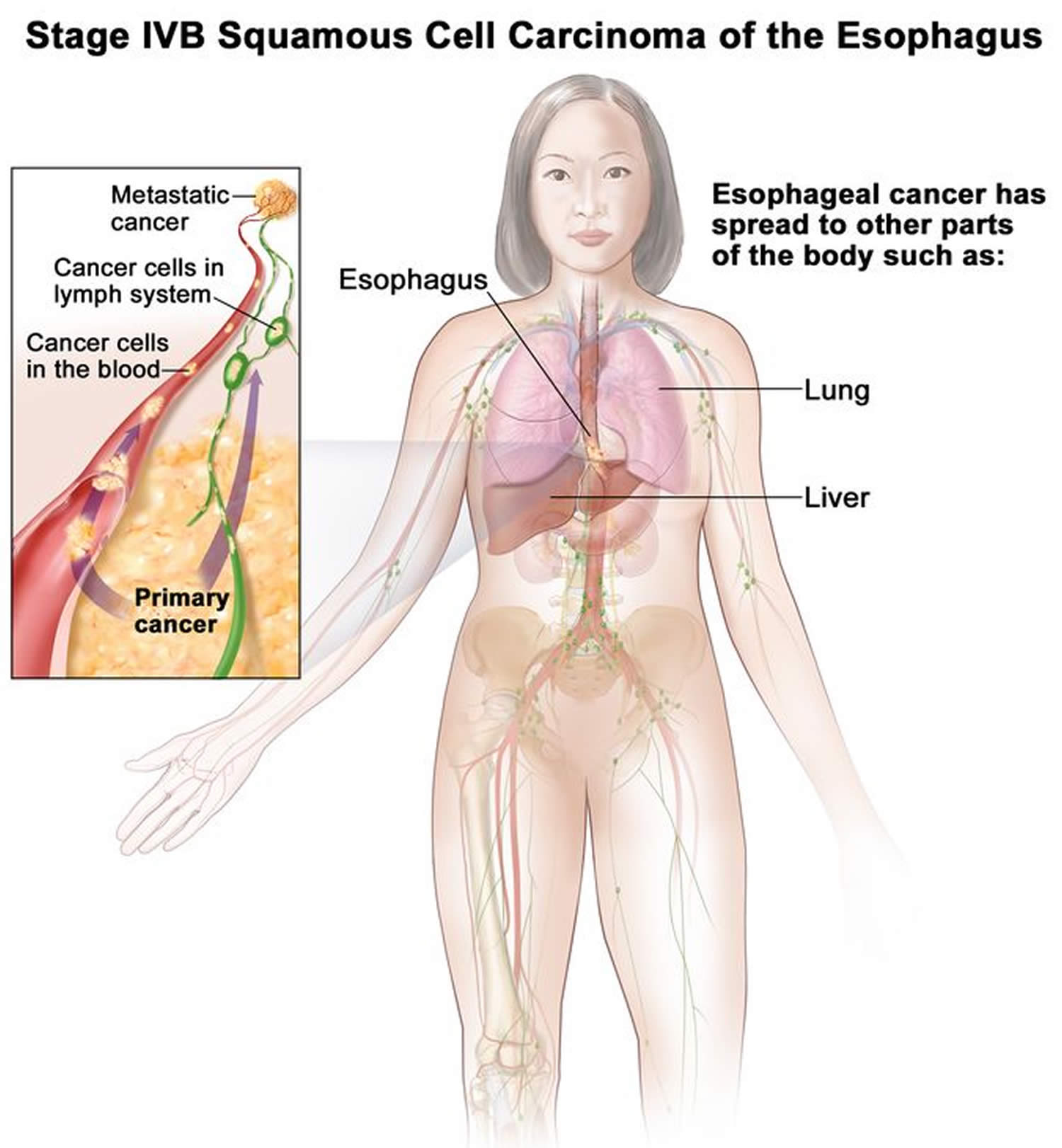
Stage 4 squamous cell carcinoma of the esophagus
Stage 4 is divided into stages 4A and 4B, depending on where the cancer has spread.
- Stage 4A cancer has spread:
- into the diaphragm, azygos vein, pleura, sac around the heart, or peritoneum. Cancer is found in 3 to 6 lymph nodes near the tumor (Figure 20); or
- into nearby structures, such as the aorta, airway, or spine. Cancer may be found in 0 to 6 lymph nodes near the tumor (Figure 21); or
- to 7 or more lymph nodes near the tumor (Figure 22).
- Stage 4B cancer has spread to other parts of the body, such as the liver or lung (Figure 23).
Figure 20. Stage 4A squamous cell carcinoma of the esophagus
Figure 21. Stage 4A squamous cell carcinoma of the esophagus
Figure 22. Stage 4A squamous cell carcinoma of the esophagus
Figure 23. Stage 4B squamous cell carcinoma of the esophagus
Table 2. Adenocarcinoma stages
The location of the cancer in the esophagus does not affect the stage of adenocarcinomas.
| AJCC Stage | Stage description ADENOCARCINOMA |
|---|---|
| 0 | The cancer is only in the epithelium (the top layer of cells lining the inside of the esophagus). It has not started growing into the deeper layers. This stage is also known as high-grade dysplasia. It has not spread to any lymph nodes or distant organs. The cancer grade does not apply. |
| IA (1A) | The cancer is growing into the lamina propria or muscularis mucosa (the tissue under the epithelium). It has not spread to any lymph nodes or distant organs. The cancer is grade 1 or an unknown grade. |
| IB (1B) | The cancer is growing into the lamina propria, muscularis mucosa (the tissue under the epithelium), or the submucosa. It has not spread to nearby lymph nodes or to distant organs. The cancer can be grade 1 or 2 or an unknown grade. |
| IC (1C) | The cancer is growing into the lamina propria, muscularis mucosa (the tissue under the epithelium), submucosa or the thick muscle layer (muscularis propria). It has not spread to nearby lymph nodes or to distant organs. The cancer can be grade 1, 2 or 3. |
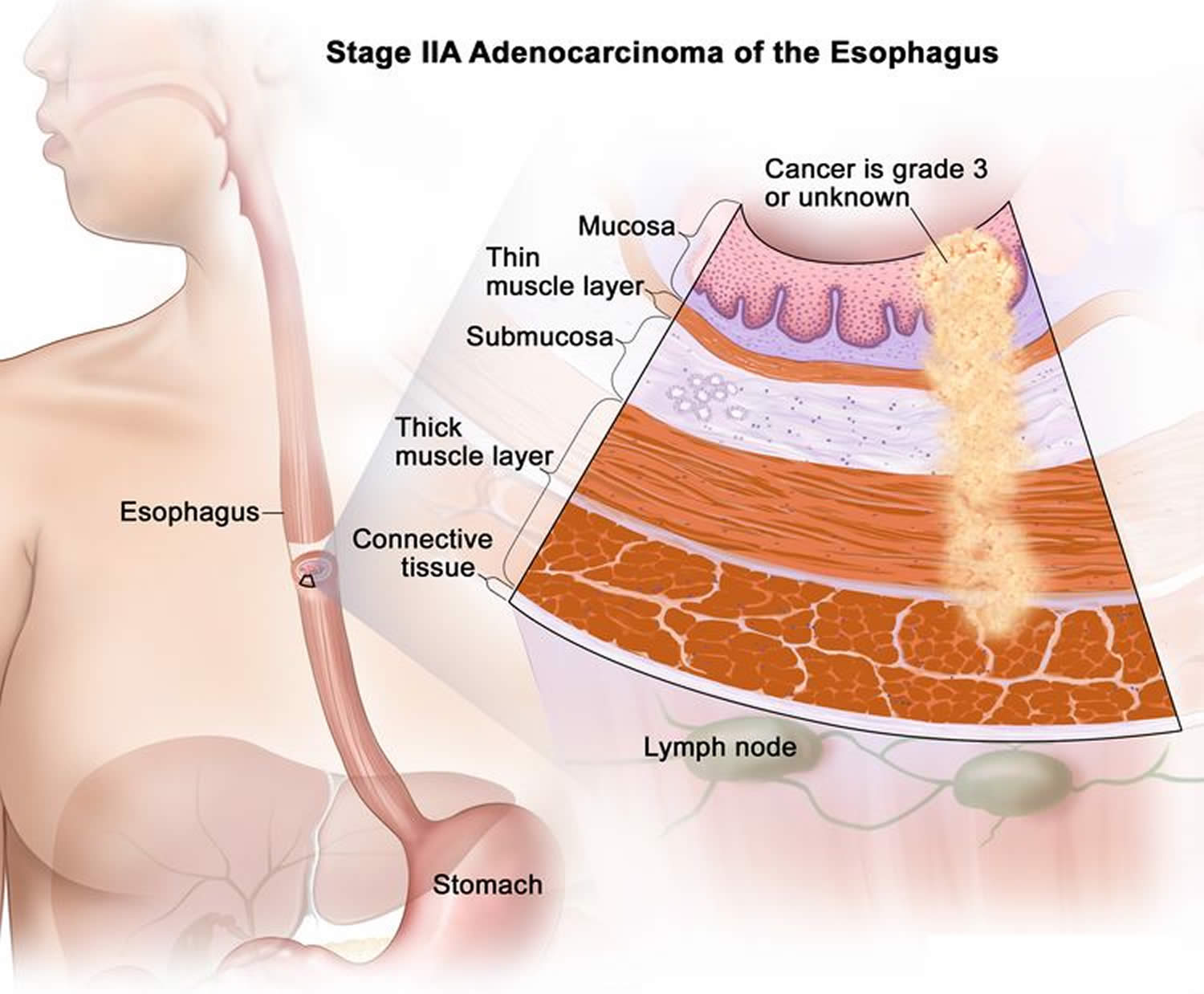
| IIA (2A) | The cancer is growing into the thick muscle layer (muscularis propria). It has not spread to nearby lymph nodes or to distant organs. The cancer can be grade 3 or an unknown grade. |
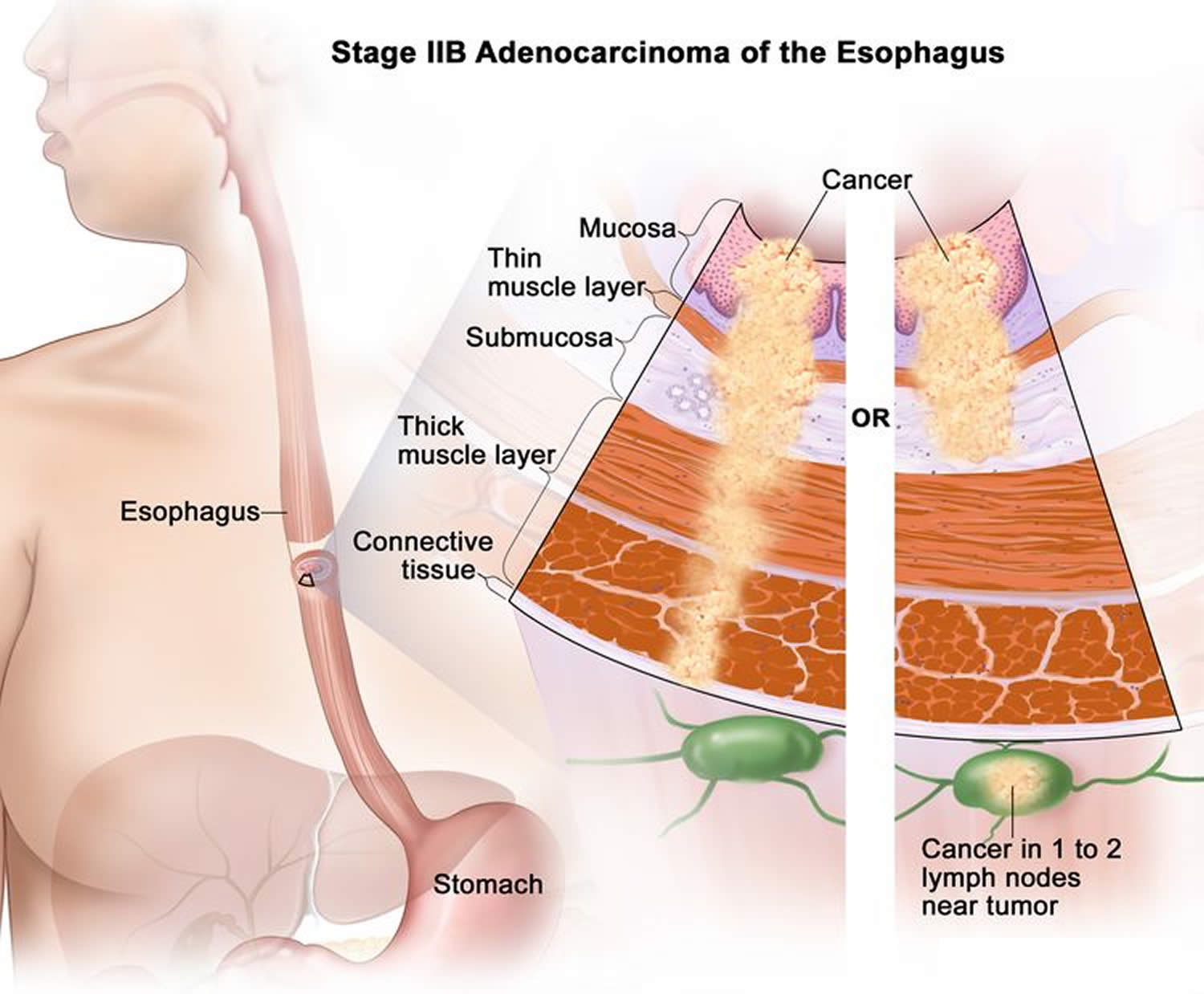
| IIB (2B)
| The cancer is growing into the lamina propria, muscularis mucosa (the tissue under the epithelium), or the submucosa. It has spread to 1 or 2 nearby lymph nodes. It has not spread to distant organs. The cancer can be any grade. |
| OR | |
| The cancer is growing into the outer layer of the esophagus (the adventitia). It has not spread nearby lymph nodes. The cancer can be any grade. | |
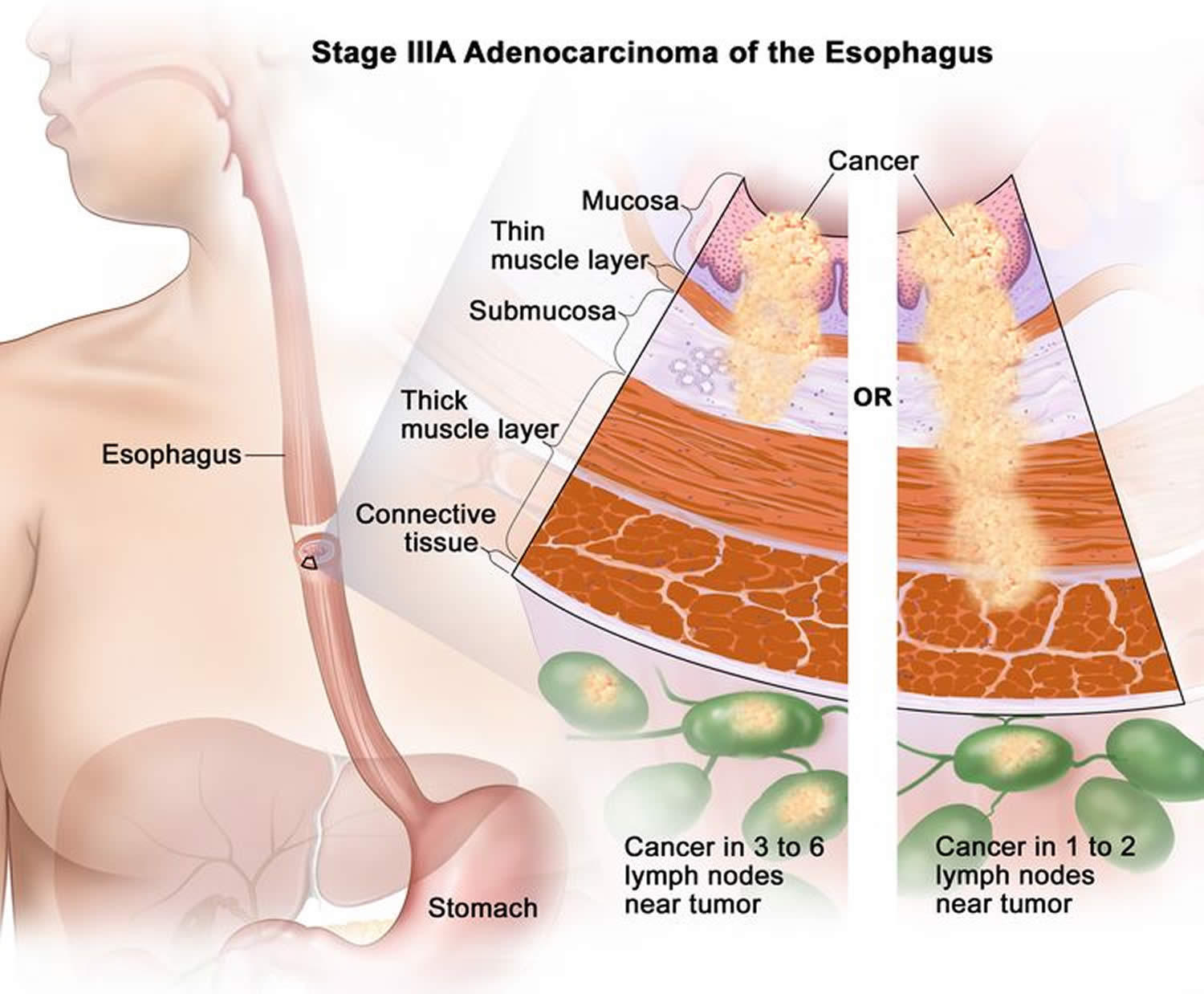
| IIIA (3A) | The cancer is growing into the lamina propria, muscularis mucosa (the tissue under the epithelium), the submucosa, or the thick muscle layer (muscularis propria). It has spread to no more than 6 nearby lymph nodes. It has not spread to distant organs. The cancer can be any grade. |
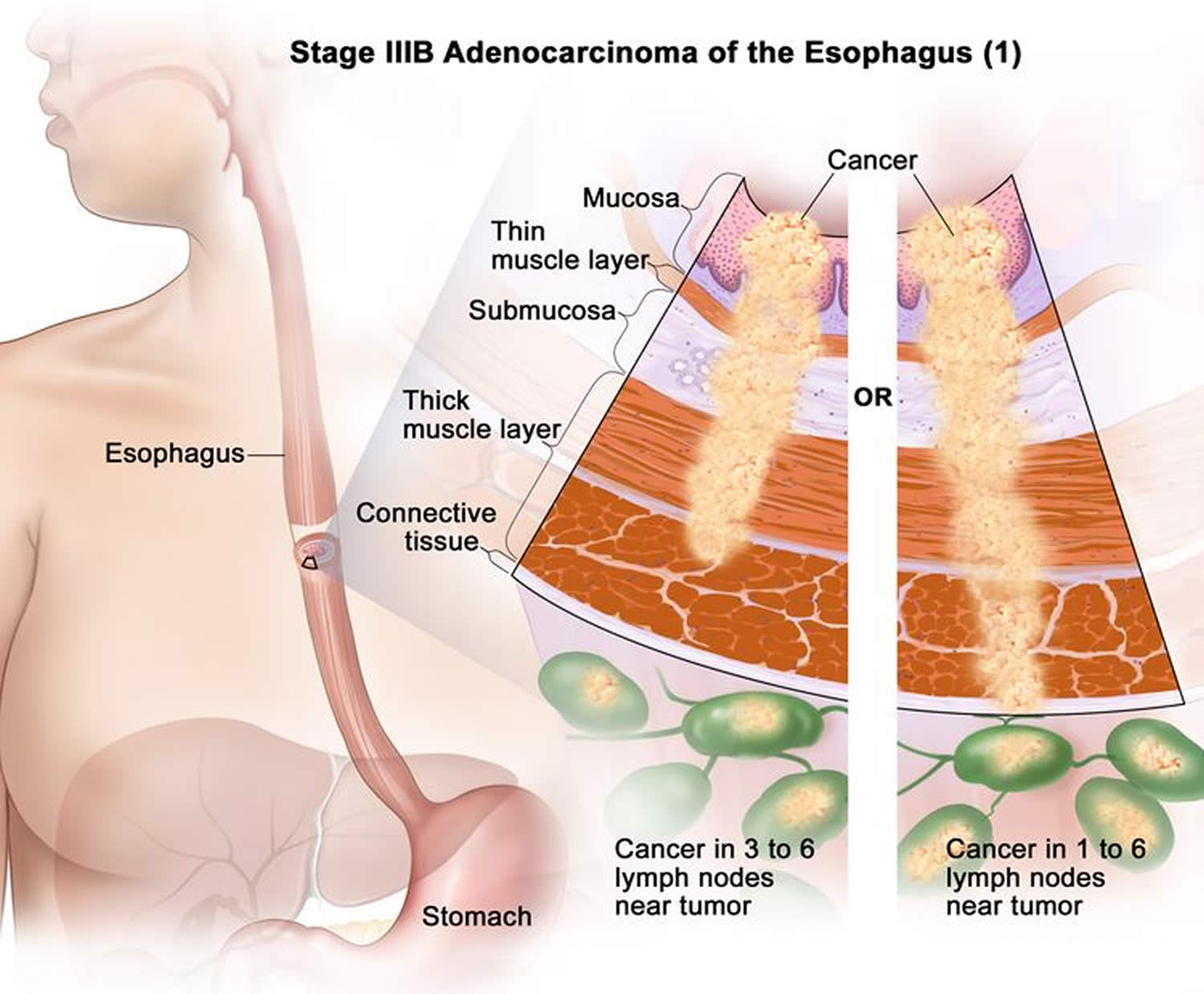
| IIIB (3B) | The cancer is growing into:
It has not spread to distant organs. The cancer can be any grade. |
| IVA (4A) | The cancer is growing into:
It has not spread to distant organs. The cancer can be any grade. |
| IVB (4A) | The cancer has spread to distant lymph nodes and/or other organs. such as the liver and lungs. The cancer can be any grade. |
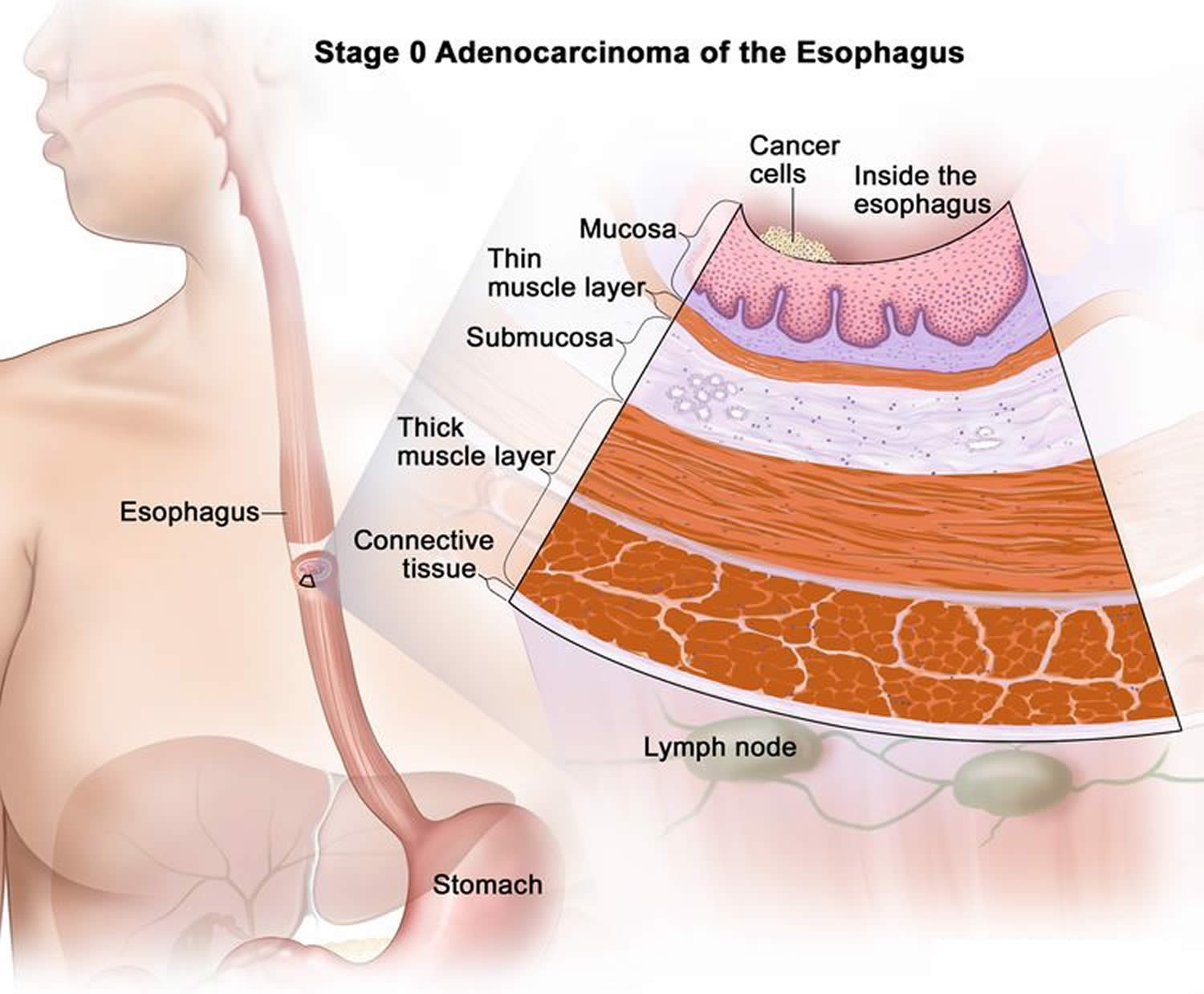
Stage 0 (High-grade Dysplasia) adenocarcinoma of the esophagus
In stage 0, cancer has formed in the inner lining of the esophagus wall. Stage 0 is also called high-grade dysplasia.
Figure 24. Stage 0 adenocarcinoma of the esophagus
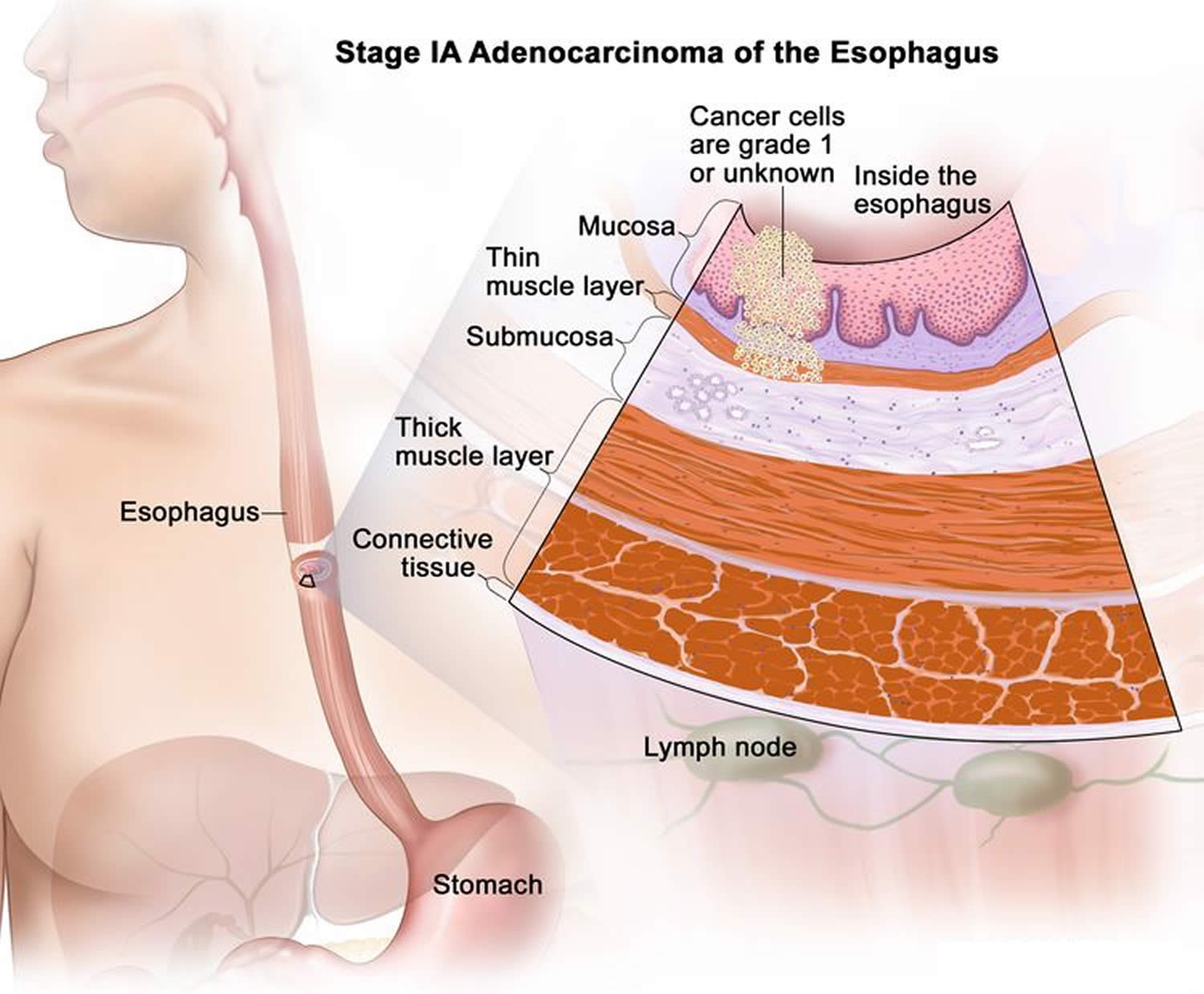
Stage 1 adenocarcinoma of the esophagus
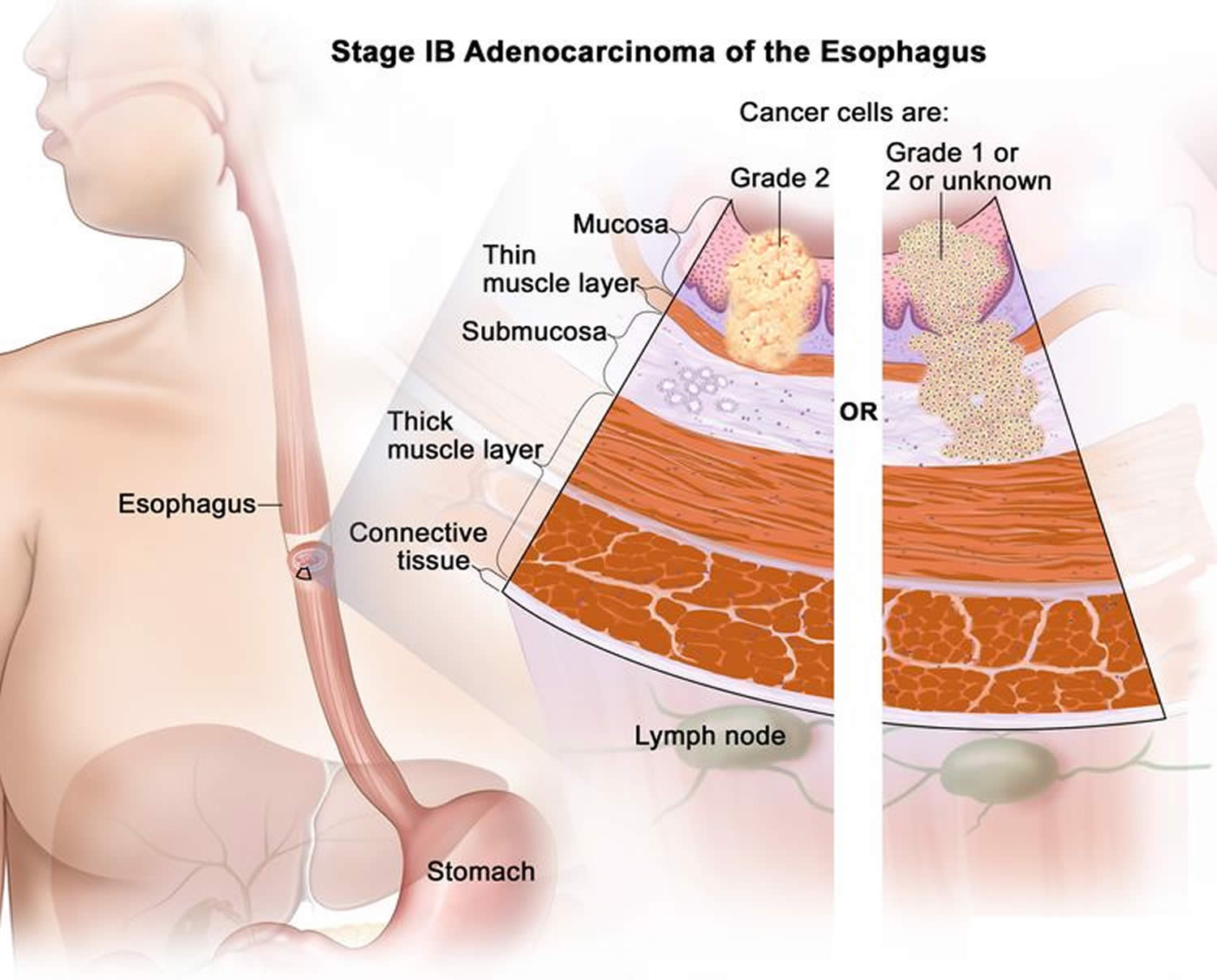
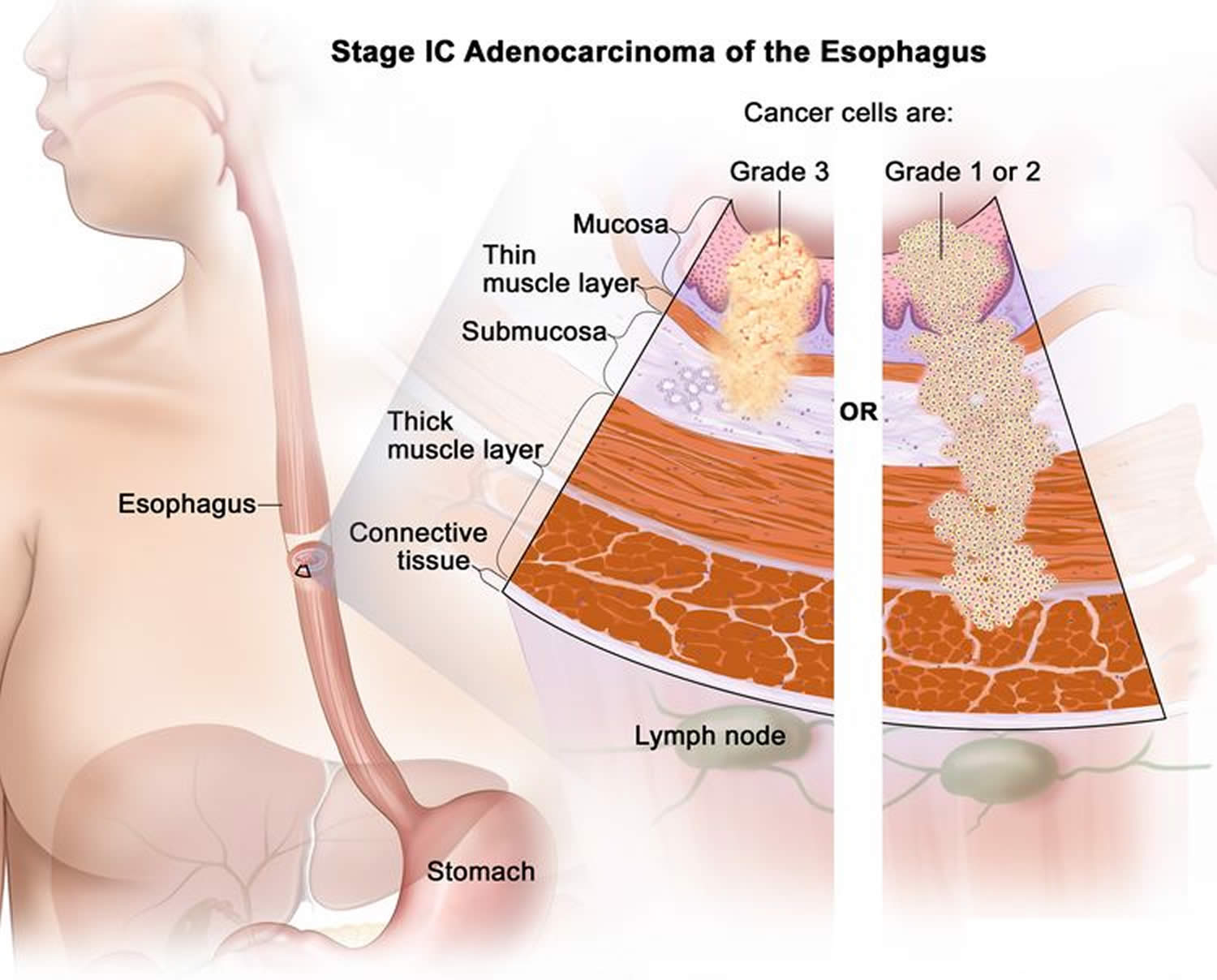
Stage 1 is divided into stages 1A, 1B, and 1C, depending on where the cancer has spread.
- Stage 1A cancer has spread into the mucosa layer or thin muscle layer of the esophagus wall (Figure 25). The cancer cells are grade 1 or the grade is not known.
- Stage 1B cancer has spread (Figure 26):
- into the mucosa layer or thin muscle layer of the esophagus wall. The cancer cells are grade 2; or
- into the submucosa layer of the esophagus wall. The cancer cells are grade 1 or 2 or the grade is not known.
- Stage 1C cancer has spread (Figure 27):
- into the mucosa layer, thin muscle layer, or submucosa layer of the esophagus wall. The cancer cells are grade 3; or
- into the thick muscle layer of the esophagus wall. The cancer cells are grade 1 or 2.
Figure 25. Stage 1A adenocarcinoma of the esophagus
Figure 26. Stage 1B adenocarcinoma of the esophagus
Figure 27. Stage 1C adenocarcinoma of the esophagus
Stage 2 adenocarcinoma of the esophagus
Stage 2 is divided into stages 2A and 2B, depending on where the cancer has spread.
- Stage 2A cancer has spread into the thick muscle layer of the esophagus wall. The cancer cells are grade 3 or the grade is not known (Figure 28).
- Stage 2B cancer has spread (Figure 29):
- into the connective tissue layer of the esophagus wall; or
- into the mucosa layer, thin muscle layer, or submucosa layer of the esophagus wall. Cancer is found in 1 or 2 lymph nodes near the tumor.
Figure 28. Stage 2A adenocarcinoma of the esophagus
Figure 29. Stage 2B adenocarcinoma of the esophagus
Stage 3 adenocarcinoma of the esophagus
Stage 3 is divided into stages 3A and 3B, depending on where the cancer has spread.
- Stage 3A cancer has spread (Figure 30):
- into the mucosa layer, thin muscle layer, or submucosa layer of the esophagus wall. Cancer is found in 3 to 6 lymph nodes near the tumor; or
- into the thick muscle layer of the esophagus wall. Cancer is found in 1 or 2 lymph nodes near the tumor.
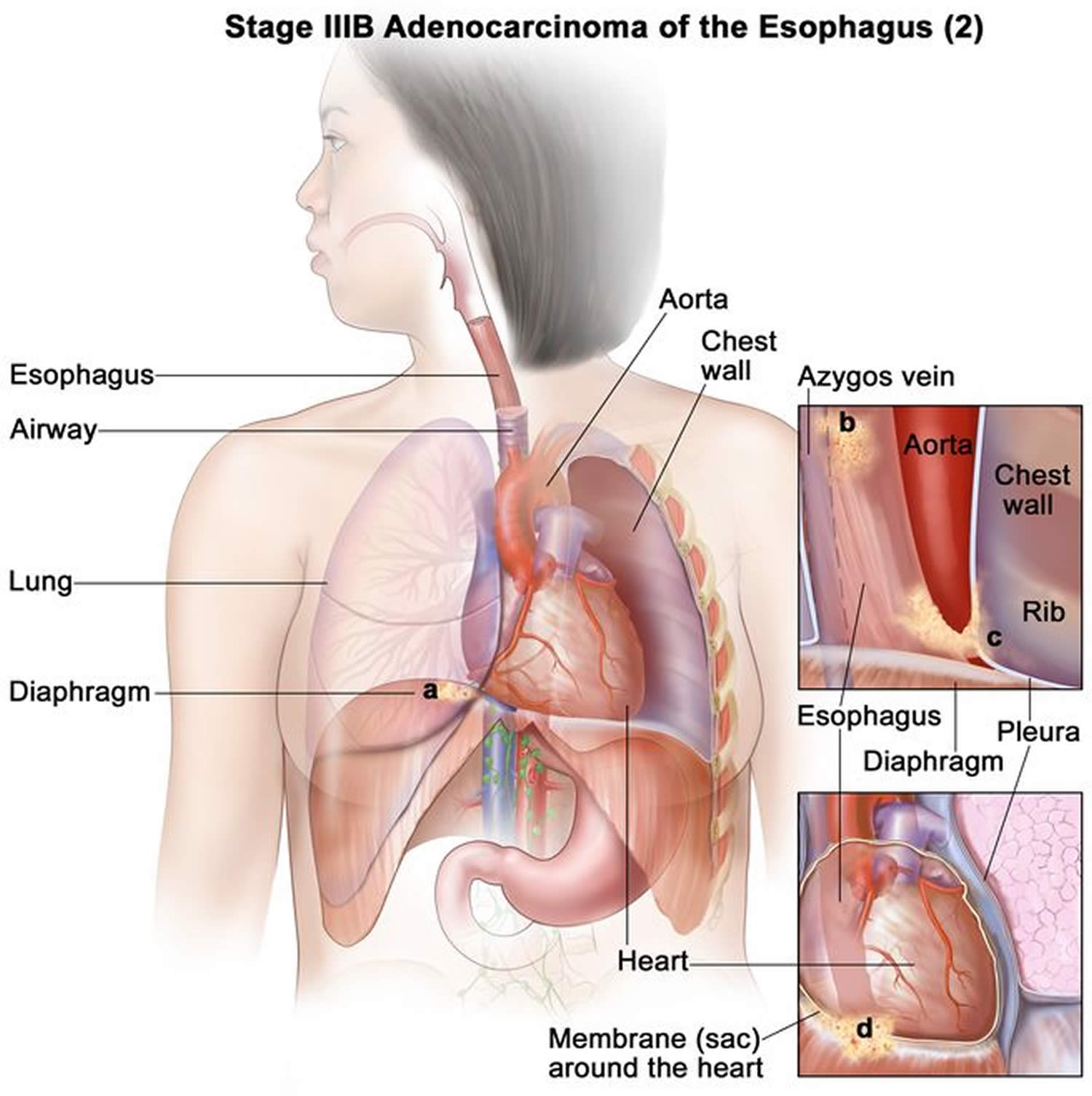
- Stage 3B cancer has spread:
- into the thick muscle layer of the esophagus wall. Cancer is found in 3 to 6 lymph nodes near the tumor; or
- into the connective tissue layer of the esophagus wall. Cancer is found in 1 to 6 lymph nodes near the tumor (Figure 31); or
- into the diaphragm, azygos vein, pleura, sac around the heart, or peritoneum. Cancer may be found in 0 to 2 lymph nodes near the tumor (Figure 32).
Figure 30. Stage 3A adenocarcinoma of the esophagus
Figure 31. Stage 3B adenocarcinoma of the esophagus
Figure 32. Stage 3B adenocarcinoma of the esophagus
Stage 4 adenocarcinoma of the esophagus
Stage 4 is divided into stages 4A and 4B, depending on where the cancer has spread.
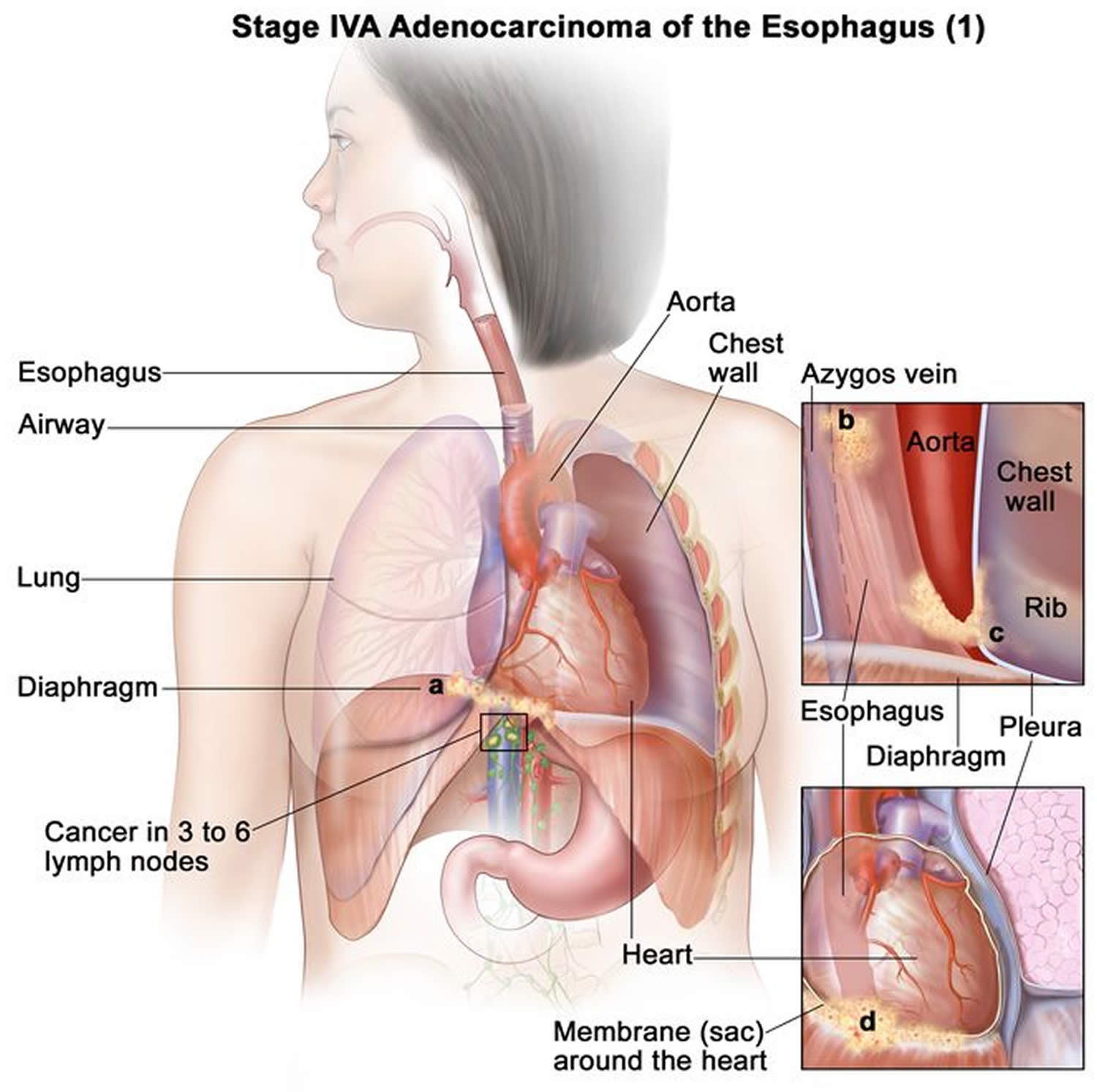
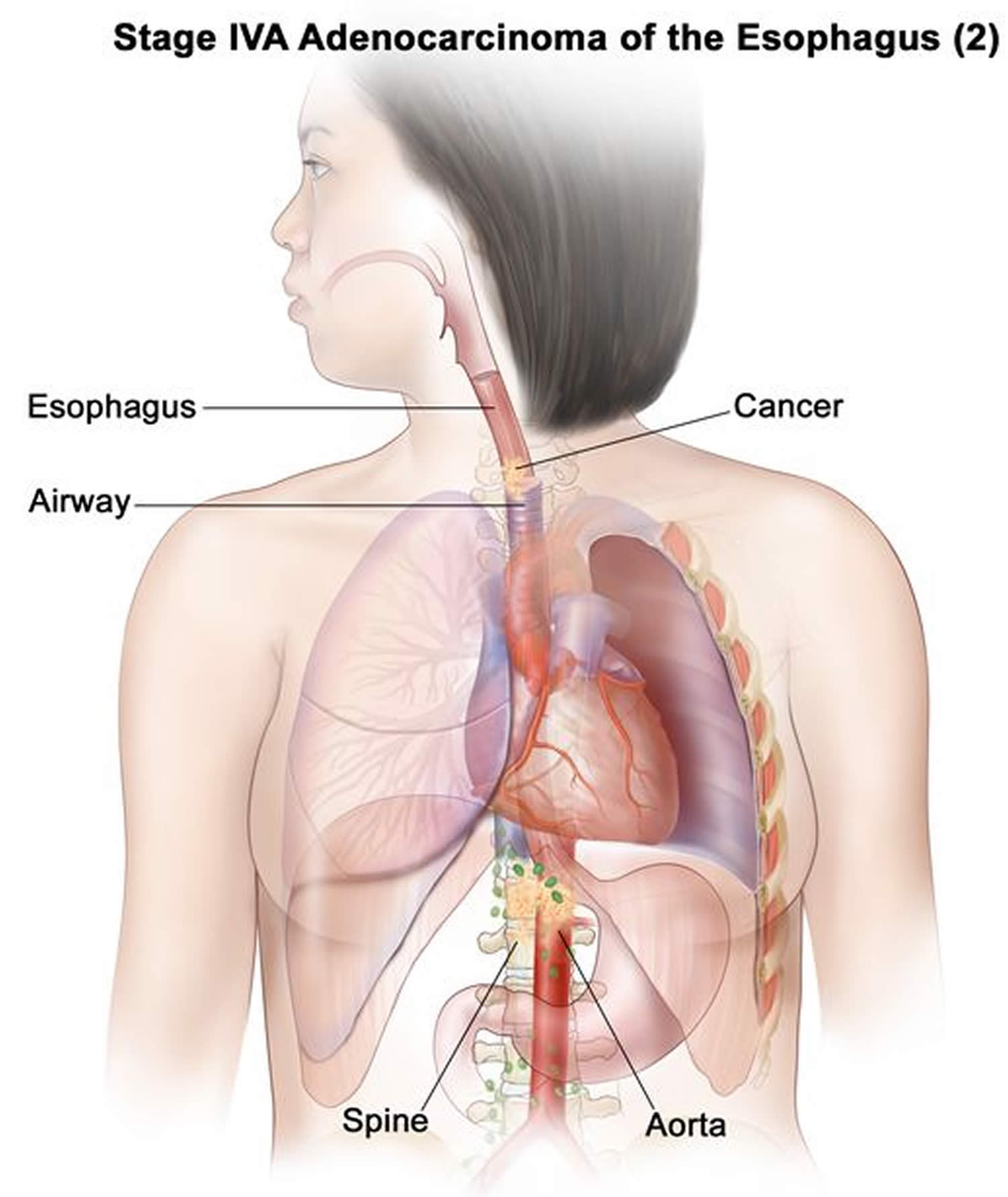
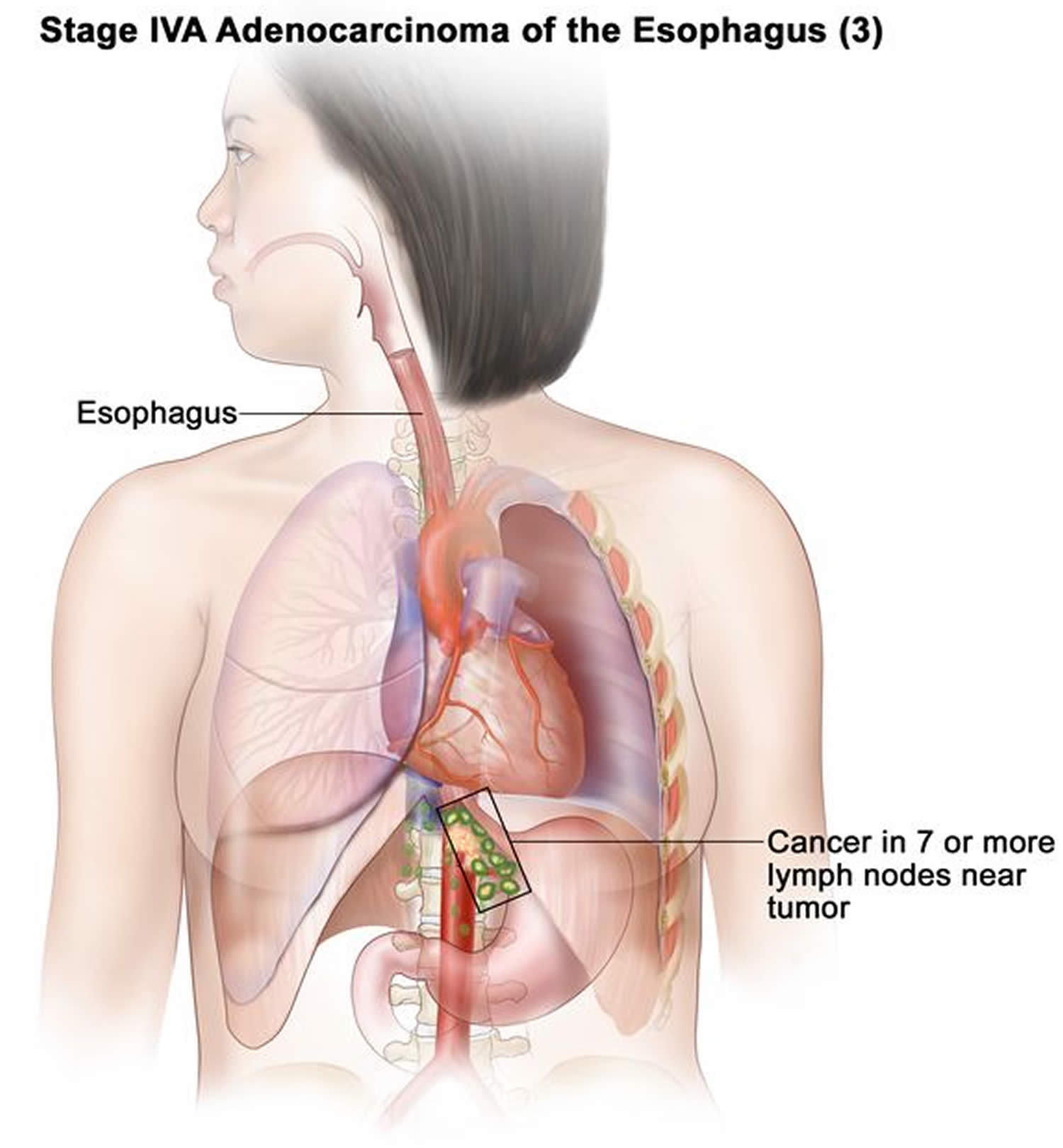
- Stage 4A cancer has spread:
- into the diaphragm, azygos vein, pleura, sac around the heart, or peritoneum. Cancer is found in 3 to 6 lymph nodes near the tumor (Figure 33); or
- into nearby structures, such as the aorta, airway, or spine. Cancer may be found in 0 to 6 lymph nodes near the tumor (Figure 34); or
- to 7 or more lymph nodes near the tumor (Figure 35).
- Stage 4B cancer has spread to other parts of the body, such as the liver or lung (Figure 36).
Figure 33. Stage 4A adenocarcinoma of the esophagus
Figure 34. Stage 4A adenocarcinoma of the esophagus
Figure 35. Stage 4A adenocarcinoma of the esophagus
Figure 36. Stage 4B adenocarcinoma of the esophagus
Resectable versus Unresectable cancer
The American Joint Committee on Cancer (AJCC) staging system provides a detailed summary of how far an esophagus cancer has spread. But for treatment purposes, doctors are often more concerned about whether the cancer can be removed completely with surgery (resected). If, based on where the cancer is located and how far it has spread, it could be removed completely by surgery, it is considered potentially resectable. If the cancer has spread too far to be removed completely, it is considered unresectable.
As a general rule, all stage 0, I (1) and II (2) esophageal cancers are potentially resectable. Most stage III (3) cancers are potentially resectable also, even when they have spread to nearby lymph nodes, as long as the cancer has not grown into the trachea (windpipe), the aorta (the large blood vessel coming from the heart), the spine, or other nearby important structures. Unfortunately, many people whose cancer is potentially resectable might not be able to have surgery to remove their cancers because they aren’t healthy enough.
If you have localized esophageal cancer, it is often recommended that your case be discussed at a multidisciplinary meeting. In this meeting, your medical information is reviewed at one time with doctors from different specialties (for example, medical oncology, pathology, surgery, radiation oncology) who, as a group, recommend a treatment plan for you.
Cancers that have grown into nearby structures or that have spread to distant lymph nodes or to other organs are considered unresectable, so treatments other than surgery are usually the best option.
Esophageal cancer survival rate
Statistics on the outlook for a certain type and stage of cancer are often given as 5-year survival rates, but many people live longer than 5 years. The 5-year survival rate is the percentage of people who live at least 5 years after being diagnosed with cancer.
But remember, the 5-year relative survival rates are estimates – your outlook can vary based on many factors specific to you.
Cancer survival rates don’t tell the whole story
Survival rates are often based on previous outcomes of large numbers of people who had the disease, but they can’t predict what will happen in any particular person’s case. There are a number of limitations to remember:
- The numbers below are among the most current available. But to get 5-year survival rates, doctors must look at people who were treated at least 5 years ago.
- As treatments are improving over time, people who are now being diagnosed with esophageal cancer may have a better outlook than these statistics show.
- These statistics are based on the stage of the cancer when it was first diagnosed. They do not apply to cancers that later come back or spread, for example.
- The outlook for people with esophageal cancer varies by the stage (extent) of the cancer – in general, the survival rates are better for people with earlier stage cancers. But many other factors can affect a person’s outlook, such as age and overall health, and how well the cancer responds to treatment. The outlook for each person is specific to his or her circumstances.
Your doctor can tell you how these numbers may apply to you, as he or she is familiar with your situation.
The numbers below come from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) database, looking at people diagnosed with esophageal cancer between 2013 and 2019. The SEER database doesn’t divide survival rates by AJCC TNM stage. Instead, it divides cancers into 3 larger, summary stages:
- Localized means that the cancer is only growing in the esophagus. It includes AJCC stage I and some stage II tumors (such as those that are T1, T2, or T3, N0, M0). Stage 0 cancers are not included in these statistics.
- Regional means that the cancer has spread to nearby lymph nodes or tissues. This includes T4 tumors and cancers with lymph node spread (N1, N2, or N3).
- Distant means that the cancer has spread to organs or lymph nodes away from the tumor, and includes all M1 (stage IV) cancers.
These survival rates for esophageal cancer do not separate squamous cell carcinomas from adenocarcinomas, although people with adenocarcinomas are generally thought to have a slightly better prognosis (outlook) overall.
Survival rates are often based on previous outcomes of large numbers of people who had the disease, but they can’t predict what will happen with any specific person. Knowing the type and the stage of a person’s cancer is important in estimating their outlook. But many other factors are also important, such as the treatment received, how well the cancer responds to treatment, and a person’s overall health. Even when taking these other factors into account, survival rates are at best rough estimates. Your doctor can tell you how well these numbers may apply to you, as he or she knows your situation best.
Table 3. Esophageal cancer life expectancy
| Stage | 5-Year Relative Survival Rate |
|---|---|
| Localized | 48.1% |
| Regional | 28.1% |
| Distant | 5.3% |
| All SEER* stages combined | 21.6% |
Footnotes:
- People now being diagnosed with esophageal cancer may have a better outlook than these numbers show. Treatments improve over time, and these numbers are based on people who were diagnosed and treated at least five years earlier.
- These numbers apply only to the stage of the cancer when it is first diagnosed. They do not apply later on if the cancer grows, spreads, or comes back after treatment.
- These numbers don’t take everything into account. Survival rates are grouped based on how far the cancer has spread, but your age, overall health, how well the cancer responds to treatment, and other factors will also affect your outlook.
Esophageal cancer prognosis
For both adenocarcinoma and squamous cell esophageal cancer, the prognosis depends on the stage. In general, the survival rates per stage are similar for both cancers.
Once a patient has positive lymph nodes, the survival is decreased. Less than 20% of patients with esophageal cancer are alive at 5 years, with stage 4 having the worst prognosis 22.
Surgery has slightly increased survival rates but the postoperative complications are often serious, and the quality of life is poor 23, 24.
Esophageal cancer treatment
What treatments you receive for esophageal cancer are based on the type of cells involved in your cancer, your cancer’s stage, your overall health and your preferences for treatment.
If you’ve been diagnosed with esophageal cancer, your cancer care team will discuss your treatment options with you. It’s important that you think carefully about each of your choices. You will want to weigh the benefits of each treatment option against the possible risks and side effects.
Which treatments are used for esophageal cancer?
There are several ways to treat esophageal cancer, depending on its type and stage.
Local treatments: Some treatments are called local therapies, meaning they treat the tumor in a specific location, without affecting the rest of the body. Types of local therapy used for esophageal cancer include:
- Surgery
- Radiation therapy
- Endoscopic treatments
These treatments are more likely to be useful for earlier stage (less advanced) cancers, although they might also be used in some other situations.
Systemic treatments: Esophageal cancer can also be treated using drugs, which can be given by mouth or directly into the bloodstream. These are called systemic therapies because they travel through your whole system, allowing them to reach cancer cells almost anywhere in the body. Depending on the type of esophageal cancer, several different types of drugs might be used, including:
- Chemotherapy
- Combined chemotherapy and radiation is called chemoradiotherapy or chemoradiation. You might have chemoradiotherapy before surgery. Or you might have it on its own as your main treatment.
- Targeted drug therapy
- Immunotherapy
Depending on the stage of the cancer and other factors, different types of treatment may be combined at the same time or used after one another.
Esophageal cancer surgery
For some earlier stage cancers, surgery can be used to try to remove the cancer and some of the normal surrounding tissue. In some cases, it might be combined with other treatments, such as chemotherapy and/or radiation therapy.
Surgery used to treat esophageal cancer include:
- an esophagectomy – your surgeon removes the part of the esophagus containing the cancer
- a total esophagectomy – your surgeon removes your whole esophagus
- an esophago-gastrectomy – your surgeon removes the top of your stomach and the part of the esophagus containing cancer
Your surgeon also removes some of the nearby lymph nodes. This is called a lymphadenectomy or lymph node dissection. It helps to reduce the risk of cancer coming back.
Esophagectomy
Surgery to remove some or most of the esophagus is called an esophagectomy. Often a small part of the stomach is removed as well. The upper part of the esophagus is then connected to the remaining part of the stomach. Part of the stomach is pulled up into the chest or neck to become the new esophagus. How much of the esophagus is removed depends upon the stage of the tumor and where it’s located:
- If the cancer is in the lower part of the esophagus (near the stomach) or at the place where the esophagus and stomach meet (the gastroesophageal or GE junction), the surgeon will remove part of the stomach, the part of the esophagus containing the cancer and about 3 to 4 inches (about 7.6 to 10 cm) of normal esophagus above this (this procedure is also known as esophagogastrectomy). Then the stomach is connected to what is left of the esophagus either high in the chest or in the neck. If necessary, part of your colon is used to help join the two.
- If the tumor is in the upper or middle part of the esophagus, most of the esophagus will need to be removed to be sure to get enough tissue above the cancer. The stomach will then be brought up and connected to the esophagus in the neck. If for some reason the stomach can’t be pulled up to attach it to the remaining part of the esophagus, the surgeon may use a piece of the intestine to bridge the gap between the two. When a piece of intestine is used, it must be moved without damaging its blood vessels. If the vessels are damaged, not enough blood will get to that piece of intestine, and the tissue will die.
Esophagectomy techniques
Open esophagectomy: In the standard, open technique, the surgeon operates through one or more large incisions (cuts) in the neck, chest, or abdomen (belly). Many different approaches can be used to remove part of the esophagus.
- For a transthoracic esophagectomy, the esophagus is removed with the main incisions in the abdomen and the chest.
- If the main incisions are in the abdomen and neck, it is called a transhiatal esophagectomy.
- Some procedures are done through incisions in the neck, chest, and abdomen.
You and your surgeon should discuss in detail the operation planned for you and what you can expect.
Minimally invasive esophagectomy (also known as keyhole surgery or thoracoscopically assisted esophagectomy): For some early (small) cancers, the esophagus can be removed through several small incisions instead of large incisions. The surgeon puts a scope (like a tiny telescope) through one of the incisions to see everything during the operation. Then the surgical instruments go in through other small incisions. To do this type of procedure well, the surgeon needs to be highly skilled and have a great deal of experience removing the esophagus this way. Because it uses smaller incisions, minimally invasive esophagectomy may allow the patient to leave the hospital sooner and recover faster.
No matter which approach is used, esophagectomy is not a simple operation, and it may require a long hospital stay. It is very important to have it done at a center that has a lot of experience treating these cancers and performing these procedures.
If the cancer has not yet spread far beyond the esophagus, removing the esophagus (and nearby lymph nodes) may cure the cancer. Unfortunately, most esophageal cancers are not found early enough for doctors to cure them with surgery.
Lymph node removal
For either type of esophagectomy, nearby lymph nodes are also removed during the operation as well. These are then checked in the lab to see if they contain cancer cells. If the cancer has spread to lymph nodes, the outlook is not as good, and the doctor may recommend other treatments (like chemotherapy and/or radiation) after surgery.
Possible risks of esophagectomy
Like most serious operations, surgery of the esophagus has some risks.
- Short-term risks include reactions to anesthesia, excess bleeding, blood clots in the lungs or elsewhere, and infections. Most people will have at least some pain after the operation, which can usually be helped with pain medicines.
- Lung complications are common. Pneumonia may develop, leading to a longer hospital stay, and sometimes even death.
- Some people might have voice changes after the surgery.
- There may be a leak at the place where the stomach (or intestine) is connected to the esophagus, which might require another operation to fix. This is not as common as it used to be because of improvements in surgical techniques.
- Strictures (narrowing) can form where the esophagus is surgically connected to the stomach, which can cause problems swallowing for some patients. To relieve this symptom, these strictures can be expanded during an upper endoscopy procedure.
- After surgery, the stomach may empty too slowly because the nerves that control its contractions can be affected by surgery. This can sometimes lead to frequent nausea and vomiting.
- After surgery, bile and stomach contents can back up into the esophagus because the ring-shaped muscle that normally controls this (the lower esophageal sphincter) is often removed or changed by the surgery. This can cause symptoms such as heartburn. Sometimes antacids or motility drugs can help relieve these symptoms.
Some complications from this surgery can be life threatening. The risk of dying from this operation is related to the doctor’s experience with these procedures. In general, the best outcomes are achieved with surgeons and hospitals that have the most experience. This is why patients should ask the surgeon about his or her experience: how often they operate on the esophagus, how many times they have done this procedure, and what percentage of their patients have died after this surgery. The hospital where the surgery is done is also important, and any hospital that you consider should be willing to show you their survival statistics.
Surgery for palliative care
Sometimes minor types of surgery are used to help prevent or relieve problems caused by the cancer, instead of trying to cure it. For example, minor surgery can be used to place a feeding tube directly into the stomach or small intestine in people who need help getting enough nutrition.
Endoscopic Treatments for Esophageal Cancer
Several types of treatment for esophageal cancer can be done by passing an endoscope (a long, flexible tube) down the throat and into the esophagus. Some of these treatments may be used to try to cure very early stage cancers, or even to prevent them from developing by treating Barrett’s esophagus or dysplasia. Other treatments are used mainly to help relieve symptoms from more advanced esophageal cancers that can’t be removed.
Endoscopic mucosal resection
Endoscopic mucosal resection (EMR) can be used for dysplasia (pre-cancer) and some small, very early-stage cancers of the esophagus.
In this technique, a piece of the inner lining of the esophagus is removed with instruments passed down the endoscope. After the abnormal tissue is removed, patients take drugs called proton pump inhibitors to suppress acid production in the stomach. This can help keep the disease from returning.
The most common side effect of endoscopic mucosal resection is bleeding in the esophagus, which is usually not serious. Less common but more serious side effects can include esophageal strictures (areas of narrowing) that might need to be treated by with dilation, and puncture (perforation) of the wall of the esophagus.
Photodynamic therapy
Photodynamic therapy (PDT) can be used to treat Barrett’s esophagus, esophageal pre-cancers (dysplasia), and some very early stage esophageal cancers. It is also often used to treat large cancers that are blocking the esophagus. In this situation, photodynamic therapy is not meant to destroy all the cancer, but to kill enough of the cancer to improve a person’s ability to swallow.
For this technique, a light-activated drug called porfimer sodium (Photofrin®) is injected into a vein. Over the next couple of days, the drug is more likely to collect in cancer cells than in normal cells. A special type of laser light is then focused on the cancer through an endoscope. This light changes the drug into a new chemical that can kill the cancer cells. The dead cells may then be removed a few days later during an upper endoscopy. This process can be repeated if needed.
The advantage of photodynamic therapy is that it can kill cancer cells with very little harm to normal cells. But because the chemical must be activated by light, it can only kill cancer cells near the inner surface of the esophagus – those that can be reached by the light. This light cannot reach cancers that have spread deeper into the esophagus or to other organs.
Photodynamic therapy can cause swelling in the esophagus for a few days, which may lead to some problems swallowing. Strictures (areas of extreme narrowing) can also happen. These often need to be treated by with dilation. Other possible side effects include bleeding or holes in the esophagus.
Some of this drug also collects in normal cells in the body, such as skin and eye cells. This can make you very sensitive to sunlight or strong indoor lights. Too much exposure can cause serious skin reactions, which is why doctors recommend staying out of any strong light for 4 to 6 weeks after the injection.
This treatment can cure some very early esophageal cancers that have not spread to deeper tissues. But this procedure destroys the tissue, so it can be hard to be certain that the cancer hasn’t spread into deeper layers of the esophagus. Since the light used in photodynamic therapy can only reach those cancer cells near the surface of the esophagus, cells of deeper cancers could be left behind, and grow into a new tumor. People getting this treatment need to have follow-up endoscopies to make sure the cancer hasn’t grown back. They also need to stay on a drug called a proton pump inhibitor to stop stomach acid production.
Radiofrequency ablation (RFA)
Radiofrequency ablation (RFA) can be used to treat dysplasia in areas of Barrett’s esophagus. It may lower the chance of cancer developing in that area.
A balloon containing many small electrodes is passed into an area of Barrett’s esophagus through an endoscope. The balloon is then inflated so that the electrodes are in contact with the inner lining of the esophagus. Then an electrical current is passed through it, which kills the cells in the lining by heating them.
Over time, normal cells will grow in to replace the Barrett’s cells. People getting this treatment need to stay on drugs to block stomach acid production after the procedure. Endoscopy (with biopsies) is then done periodically to watch for any further changes in the lining of the esophagus. Rarely, radiofrequency ablation (RFA) can cause strictures (narrowing) or bleeding in the esophagus.
Treatments to help keep the esophagus open
Laser ablation
This technique can be used to help open the esophagus when it is blocked by an advanced cancer. This can help improve problems swallowing.
A laser beam is aimed at the cancer through the tip of an endoscope to destroy the cancerous tissue. The laser is called a neodymium: yttrium-aluminum-garnet (Nd:YAG) laser. Laser endoscopy can be helpful, but the cancer often grows back, so the procedure may need to be repeated every month or two.
Argon plasma coagulation
This technique is like laser ablation, but it uses argon gas and a high-voltage spark delivered through the tip of an endoscope. The spark causes the gas to reach very high temperatures, which can then be aimed at the tumor. This approach is used to help unblock the esophagus for people who have trouble swallowing.
Electrocoagulation (electrofulguration)
For this treatment, a probe is passed down into the esophagus through an endoscope to burn the tumor off with electric current. In some cases, this treatment can help relieve esophageal blockage.
Esophageal stent
A stent is a device that, once in place, self-expands (opens up) to become a tube that helps hold the esophagus open. Stents are made of mesh material. Most often stents are made of metal, but they can also be made of plastic. Using endoscopy, a stent can be placed into the esophagus across the length of the tumor.
How well the stent works depends on the type that is used and where it is placed. Stents will relieve trouble swallowing for most people. They are often used after other endoscopic treatments to help keep the esophagus open.
Figure 37. Esophageal stent
Chemotherapy
Chemotherapy is drug treatment that uses chemicals to kill cancer cells. Chemotherapy drugs are typically used before (neoadjuvant chemotherapy) or after (adjuvant chemotherapy ) surgery in people with esophageal cancer. Chemotherapy can also be combined with radiation therapy. In people with advanced cancer that has spread beyond the esophagus, chemotherapy may be used alone to help relieve signs and symptoms caused by the cancer.
The chemotherapy side effects that you experience depend on which chemotherapy drugs you receive.
Some common drugs and drug combinations used to treat esophageal cancer include those below which can be given along with radiation or without:
- Carboplatin and paclitaxel (Taxol)
- Oxaliplatin and either 5-FU or capecitabine
- Cisplatin and either 5-fluorouracil (5-FU) or capecitabine
- Cisplatin and Irinotecan (Camptosar)
- Paclitaxel (Taxol) and either 5-FU or capecitabine
Other common drugs and drug combinations that can be used to treat esophageal cancer but are usually not given with radiation include:
- ECF: epirubicin (Ellence), cisplatin, and 5-FU (especially for gastroesophageal junction tumors)
- DCF: docetaxel (Taxotere), cisplatin, and 5-FU
- Trifluridine and tipiracil (Lonsurf), a combination drug in pill form
For some esophageal cancers, chemo may be used along with the targeted drug trastuzumab (Herceptin) or ramucirumab (Cyramza).
Chemo drugs for esophageal cancer are typically given into a vein (IV), either as an injection over a few minutes or as an infusion over a longer period of time. Some drugs you take by mouth. All of these drugs enter your bloodstream and reach most areas of your body. These drugs can be given in a doctor’s office, infusion center, or in a hospital.
Often, a slightly larger and sturdier IV called a central venus catheter (CVC) is needed to administer chemo. It might also be called a central venous access device (CVAD), or central line. Once put in place, a CVC can stay in as long as you’re getting treatment so you won’t need to be stuck with a needle in the arms or hands each time to put in an IV catheter. It can be used to put medicines, blood products, nutrients, or fluids right into your blood. It can also be used to take out blood for testing. There are many different kinds of CVCs. The most common types are the port and the PICC line.
Chemo is given in cycles, followed by a rest period to give you time to recover from the effects of the drugs. Cycles are most often 2 or 3 weeks long. The schedule varies depending on the drugs used. For example, with some drugs, the chemo is given only on the first day of the cycle. With others, it is given for a few days in a row, or once a week. Then, at the end of the cycle, the chemo schedule repeats to start the next cycle.
Adjuvant or neoadjuvant chemo is often given for a total of 3 to 6 months, depending on the drugs used. The length of treatment for advanced esophageal cancer depends on how well it is working and what side effects you might have.
Chemotherapy side effects
Chemo drugs can cause side effects. These depend on the type and dose of drugs given, and the length of treatment. Some of the most common side effects of chemo include:
- Nausea and vomiting
- Loss of appetite
- Hair loss
- Mouth sores
- Diarrhea or constipation
Chemo can also affect the blood-forming cells of the bone marrow, which can lead to:
- Increased chance of infection (from having too few white blood cells)
- Easy bleeding or bruising (from having too few blood platelets)
- Fatigue (from having too few red blood cells and other reasons)
Other side effects are also possible. Some of these are more common with certain chemo drugs. For example:
- Hand-foot syndrome. During treatment with capecitabine or 5-FU (when given as an infusion), this can start out as redness in the hands and feet, and then progress to pain and sensitivity in the palms and soles. If it worsens, blistering or skin peeling can occur, sometimes leading to painful sores. It’s important to tell your doctor right away about any early symptoms, such as redness or sensitivity, so that steps can be taken to keep things from getting worse.
- Neuropathy (nerve damage). This is a common side effect of oxaliplatin, cisplatin, docetaxel, and paclitaxel. Symptoms include numbness, tingling, and even pain in the hands and feet. Oxaliplatin can also cause intense sensitivity to cold in the throat and esophagus (the tube connecting the throat to the stomach) and the palms of the hands. This can cause problems swallowing liquids or holding a cold glass. If you will be getting oxaliplatin, talk with your doctor about side effects, and let them know right away if you develop numbness and tingling or other side effects.
- Allergic or sensitivity reactions. Some people can have reactions while getting the drug oxaliplatin. Symptoms can include skin rash, chest tightness and trouble breathing, back pain, or feeling dizzy, lightheaded, or weak. Be sure to tell your nurse right away if you notice any of these symptoms while you are getting chemo.
- Diarrhea. This is a common side effect with many of these drugs, but can be particularly bad with irinotecan. It needs to be treated right away — at the first loose stool — to prevent severe dehydration. This often means taking drugs like loperamide (Imodium). If you are on a chemo drug that is likely to cause diarrhea, your doctor will give you instructions on what drugs to take and how often to take them to control this symptom.
- Weight loss. People with esophageal cancer often have already lost weight before the cancer was found. Treatments such as chemo, radiation, or both can make it hard to eat well enough to get good nutrition, making weight loss worse. Depending on your situation, the cancer care team might recommend placement of a feeding tube to keep up your nutrition and weight during treatment. This feeding tube may be used short-term (during treatment and a bit afterwards) or it may be permanent depending on your cancer.
Most of these side effects tend to go away after treatment is finished. Some, such as hand and foot numbness, may last for a long time. There are often ways to lessen these side effects. For example, you can be given drugs to help prevent or reduce nausea and vomiting.
Be sure to discuss any questions about side effects with your cancer care team. Report any side effects or changes you notice while getting chemo right away so that they can be treated promptly. In some cases, the doses of the chemo drugs may need to be reduced or treatment may need to be delayed or stopped to prevent the effects from getting worse.
Radiation therapy
Radiation therapy uses high-powered X-ray beams to kill cancer cells. Radiation typically will come from a machine outside your body that aims the beams at your cancer (external-beam radiation therapy [EBRT]). Or, less commonly, radiation can be placed inside your body near the cancer (brachytherapy).
Radiation therapy may be used:
- As part of the main treatment of esophageal cancer in some patients, typically along with chemo (chemoradiation). This is often used for people who can’t have surgery due to poor health or for people who don’t want surgery.
- Before surgery (and along with chemo when possible), to try to shrink the cancer and make it easier to remove. This is called neoadjuvant therapy.
- After surgery (and along with chemo when possible), to try to kill any cancer cells that may have been left behind but are too small to see. This is known as adjuvant therapy.
- To ease the symptoms of advanced esophageal cancer such as pain, bleeding, or trouble swallowing. This is called palliative therapy.
Radiation therapy is most often combined with chemotherapy in people with esophageal cancer. It’s typically used before surgery (neoadjuvant therapy) or occasionally after surgery (adjuvant therapy). Radiation therapy is also used to relieve complications of advanced esophageal cancer, such as when a tumor grows large enough to stop food from passing to your stomach. Treatment can last from two to six weeks of daily radiation treatments.
If you are going to get radiation therapy, it’s important to ask your doctor beforehand about the possible side effects so you know what to expect.
Possible Side effects of external radiation therapy can include:
- Skin changes in areas getting radiation, such as redness, blistering and peeling
- Nausea and vomiting
- Diarrhea
- Fatigue
- Painful sores in the mouth and throat
- Dry mouth or thick saliva (spit)
- Pain with swallowing
These side effects are often worse if chemotherapy is given at the same time as radiation.
Most side effects of radiation are temporary, but some less common side effects can be permanent. For example, in some cases radiation can cause a stricture (narrowing) in the esophagus, which might require more treatment. Radiation to the chest can cause lung damage, which may lead to problems breathing and shortness of breath.
If you notice any side effects, talk to your doctor right away so steps can be taken to lessen them.
Combined chemotherapy and radiation
Combining chemotherapy and radiation therapy may enhance the effectiveness of each treatment. Combined chemotherapy and radiation may be the only treatment you receive, or combined therapy can be used before surgery. But combining chemotherapy and radiation treatments increases the likelihood and severity of side effects.
- Chemoradiotherapy as your main treatment. You might have chemoradiotherapy instead of surgery if you have a squamous cell esophageal cancer that hasn’t spread. The doctors keep a close eye on you after the treatment. This is called active surveillance.
- Chemoradiotherapy before surgery also called neoadjuvant chemoradiotherapy. You might have chemoradiotherapy before surgery if you have adenocarcinoma or squamous cell esophageal cancer which hasn’t spread to other parts of your body. It shrinks the cancer and makes it easier to remove.
- Chemoradiotherapy instead of surgery. You might have other health conditions that mean you’re not well enough to have surgery. Or you might not be able to have surgery because the cancer has grown into nearby tissues. The doctor might offer you chemoradiotherapy instead.
Targeted drug therapy
Cancer cells are different to normal cells. These differences help them to grow and survive. There are medicines that can target those changes. These drugs are called targeted cancer drugs.
Targeted drugs work differently from standard chemotherapy drugs. They sometimes work when standard chemo drugs don’t, and they often have different side effects. They can be used either along with chemo or by themselves.
Drugs that target HER2
Some esophagus cancers have too much of the HER2 protein on the surface of their cells, which can help cancer cells grow. Having too much of this protein is caused by having too many copies of the HER2 gene. Cancers with increased levels of HER2 are called HER2-positive. Drugs that target the HER2 protein can often be helpful in treating HER2-positive cancers.
Trastuzumab (Herceptin, others)
Trastuzumab is a monoclonal antibody, a man-made version of an immune system protein, which targets HER2. It can be used to help treat some HER2-positive cancers of the gastroesophageal (GE) junction (the place where the esophagus and stomach meet).
If you have a gastroesophageal (GE) junction cancer and can’t have surgery, your doctor may have your tumor tested for the HER2 protein or gene. People whose cancers have normal amounts of HER2 are very unlikely to be helped by this drug.
Trastuzumab is given into a vein (IV), typically once every 3 weeks, along with chemo.
Herceptin was the original brand name for trastuzumab, but several similar versions (called biosimilars) are now available as well, including Ogivri, Herzuma, Ontruzant, Trazimera, and Kanjinti.
Possible side effects of trastuzumab
Most of the side effects of trastuzumab are relatively mild and can include fever and chills, cough, and headache. These occur less often after the first dose.
Trastuzumab can also sometimes cause heart damage, leading to the heart muscle becoming weak. Trastuzumab is not given with certain chemo drugs called anthracyclines, such as epirubicin (Ellence) or doxorubicin (Adriamycin), because it can further increase the risk of heart damage if they are given together. Before starting treatment with trastuzumab, your doctor may test your heart function with an echocardiogram or a MUGA scan.
Fam-trastuzumab deruxtecan (Enhertu)
This is an antibody-drug conjugate, which is a monoclonal antibody linked to a chemotherapy drug. In this case, the anti-HER2 antibody acts like a homing signal by attaching to the HER2 protein on cancer cells, bringing the chemo directly to them.
This antibody-drug conjugate can be used by itself to treat advanced HER2-positive GE junction cancers, typically after treatment with trastuzumab has been tried.
Fam-trastuzumab deruxtecan (Enhertu) is infused into a vein (IV). It is typically given once every 3 weeks.
Side effects of fam-trastuzumab deruxtecan
- Fam-trastuzumab deruxtecan (Enhertu) can cause low blood cell counts, which can increase a person’s risk of infections and bleeding. Other common side effects can include nausea, vomiting, diarrhea or constipation, loss of appetite, fever, feeling tired, and hair loss.
- Fam-trastuzumab deruxtecan (Enhertu) can cause serious lung disease in some people, which might even be life threatening. It’s very important to let your doctor or nurse know right away if you’re having symptoms such as coughing, wheezing, trouble breathing, or fever.
- Fam-trastuzumab deruxtecan (Enhertu) can also rarely cause heart damage. Before starting treatment with this drug, your doctor may test your heart function with an echocardiogram or a MUGA scan.
Ramucirumab
For cancers to grow and spread, they need to make new blood vessels so that the tumors get blood and nutrients. One of the proteins that tells the body to make new blood vessels is called vascular endothelial growth factor (VEGF). To start this process, VEGF attaches to other proteins on the outside of the cancer cell called receptors.
Ramucirumab (Cyramza) is a monoclonal antibody that blocks the process of making new blood vessels. Ramucirumab joins to the VEGF receptor, which blocks VEGF and stops the signal to the body to make more blood vessels. This can help slow or stop the growth of the cancer.
Ramucirumab is used to treat cancers that start at the gastroesophageal (GE) junction when they are advanced. It is most often used after another drug stops working. It can be used alone or in combination with the chemo drug paclitaxel.
Ramucirumab is given as infusion into a vein (IV) every 2 weeks.
Possible side effects of ramucirumab
The most common side effects of this drug are high blood pressure, swelling of the arms or legs, protein in the urine, and fatigue. Rare but possibly serious side effects include blood clots, severe bleeding, holes forming in the stomach or intestines (called perforations), and problems with wound healing. If a hole forms in the stomach or intestine it can lead to severe infection and may require surgery to correct.
Entrectinib and larotrectinib
In some cancers, the cells have genes that join together. The fusion of one of these genes, called NTRK, with another gene can lead to abnormal cell growth.
Drugs that target cells with this abnormal gene fusion, called TRK inhibitors, include entrectinib (Rozlytrek) and larotrectinib (Vitrakvi). One of these drugs might be used to treat esophageal cancer with an NTRK gene fusion if the cancer cannot be removed with surgery or has spread to other parts of the body, and if it has grown despite other treatments.
Entrectinib and larotrectinib are given as pills daily.
Possible side effects of entrectinib and larotrectinib
The most common side effects are fatigue, nausea, vomiting, dizziness, cough, diarrhea, and constipation. Other more serious, but less common, side effects include liver problems and confusion.
Immunotherapy
Immunotherapy is the use of medicines that help a person’s own immune system find and destroy cancer cells more effectively. It can be used to treat some people with esophagus cancer.
An important part of the immune system is its ability to keep itself from attacking normal cells in the body. To do this, it uses “checkpoint” proteins on immune cells, which act like switches that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to avoid being attacked by the immune system.
Drugs called immune checkpoint inhibitors target these checkpoint proteins, which can help restore the immune response against esophagus cancer cells.
Possible side effects of immune checkpoint inhibitors
Common side effects of these drugs can include fatigue, cough, nausea, skin rash, poor appetite, constipation, muscle or joint pain, itching, fever, and diarrhea.
Other, more serious side effects happen less often. These can include:
- Infusion reactions: Some people might have an infusion reaction while getting one of these drugs. This is like an allergic reaction, and can include fever, chills, flushing of the face, rash, itchy skin, feeling dizzy, wheezing, and trouble breathing. It’s important to tell your doctor or nurse right away if you have any of these symptoms while getting one of these drugs.
- Autoimmune reactions: These drugs work by basically removing one of the safeguards on the body’s immune system. Sometimes the immune system starts attacking other parts of the body, which can cause serious or even life-threatening problems in the lungs, intestines, liver, hormone-making glands, kidneys, skin, or other organs.
It’s very important to report any new side effects to your health care team promptly. If serious side effects do occur, treatment may need to be stopped and you may get high doses of corticosteroids to suppress your immune system.
PD-1 inhibitors
Pembrolizumab (Keytruda) and nivolumab (Opdivo) are drugs that target PD-1, a protein on T cells (a type of immune system cell). The PD-1 protein normally helps keep T cells from attacking other cells in the body. By blocking PD-1, these drugs boost the immune response against cancer cells. This can shrink some tumors or slow their growth.
Pembrolizumab can be used to treat some advanced cancers of the esophagus or gastroesophageal junction (GEJ), typically when treatments such as surgery and chemoradiation (chemotherapy plus radiation therapy) can’t be done. Pembrolizumab might be given by itself or along with chemotherapy, depending on the situation.
In certain cases when no other treatment options are available, this drug can be used for people whose cancer has tested positive for specific gene changes, such as a high level of microsatellite instability (MSI-H), or changes in one of the mismatch repair (MMR) genes.
Pembrolizumab can also be used with chemotherapy, and the targeted drug, trastuzumab, as the first treatment in people with advanced GEJ cancers that test positive for HER2.
Pembrolizumab is given as an intravenous (IV) infusion, typically every 3 or 6 weeks.
Nivolumab (Opdivo) can be used in different situations:
- Nivolumab can be used in people with cancer of the esophagus or gastroesophageal junction (GEJ) who got chemotherapy and radiation (chemoradiation) before surgery, if lab tests after surgery show that some cancer may have been left behind.
- Nivolumab can be used by itself in people with advanced squamous cell cancer of the esophagus, typically after chemotherapy has been tried.
- Nivolumab can be used along with chemotherapy as a first treatment in people with advanced squamous cell cancer of the esophagus. When given this way, it can help some people live longer.
- Nivolumab can be used along with ipilimumab as a first treatment in people with advanced squamous cell cancer of the esophagus. When given this way, it can help some people live longer.
- Nivolumab can be used along with chemo in people with advanced adenocarcinoma of the esophagus or with advanced cancer of the gastroesophageal junction (GEJ).
Nivolumab is given as an intravenous (IV) infusion, usually once every 2, 3, or 4 weeks.
CTLA-4 inhibitor
Ipilimumab (Yervoy) is another drug that boosts the immune response, but it has a different target. It blocks CTLA-4, another protein on T cells that normally helps keep them in check.
It can be used along with nivolumab as the first option to treat advanced squamous cell cancer of the esophagus that can’t be removed by surgery or that has spread to other parts of the body.
Ipilimumab (Yervoy) is given as an intravenous (IV) infusion, usually once every 6 weeks when given in combination with nivolumab.
Treatments for complications
Treatments for esophageal obstruction and difficulty swallowing (dysphagia) can include:
- Relieving esophageal obstruction. If your esophageal cancer has narrowed your esophagus, a surgeon may do esophageal dilation to stretch out an area of the esophagus that is narrowed or blocked to allow better swallowing. A small balloon-like device or a device shaped like a pipe is passed down the throat and pushed through the narrowed area to stretch it out. This can be repeated if needed. Before the procedure, your doctor may give you a sedative to help you relax and may numb your throat by spraying it with a local anesthetic. There is a small risk of bleeding or tearing a hole in the esophagus (called a perforation) with this procedure, which could require surgery or other treatments to fix. The esophagus typically stays open only a few weeks after dilation, so this is often followed by other treatments (such as placing an expandable stent) to help keep the esophagus open. Other endoscopic procedures that can be used to help keep the esophagus open in people who are having trouble swallowing include:
- Esophageal stent placement
- Photodynamic therapy
- Electrocoagulation
- Laser ablation
- Argon plasma coagulation
- Providing nutrition. Your doctor may recommend a feeding tube if you’re having trouble swallowing or if you’re having esophagus surgery. A feeding tube allows nutrition to be delivered directly to your stomach or small intestine, giving your esophagus time to heal after cancer treatment. Some people with esophageal cancer may need to have a feeding tube, usually called a jejunostomy tube (or J-tube), put in place before treatment. This is done through a small hole in the skin over the abdomen during a minor operation. A J-tube lets liquid nutrition be put directly into the small intestine to prevent further weight loss and improve nutrition. This can make treatment easier to tolerate. Less often, the tube is placed into the stomach instead. This is known as a gastrostomy tube (G-tube). A feeding tube can easily be removed when it’s no longer needed.
Coping and support
Coping with the shock, fear and sadness that come with a cancer diagnosis can take time. You may feel overwhelmed just when you need to make crucial decisions. With time, each person finds a way of coping and coming to terms with the diagnosis.
Until you find what brings you the most comfort, consider trying to:
- Find out enough about esophageal cancer to make decisions about your care. Ask your doctor for the specifics about your cancer, such as its type and stage. And ask for recommended sources of information where you can learn more about your treatment options. The National Cancer Institute (https://www.cancer.gov) and the American Cancer Society (https://www.cancer.org) are good places to start.
- Stay connected to friends and family. Your friends and family can provide a crucial support network for you during your cancer treatment. As you begin telling people about your esophageal cancer diagnosis, you’ll likely get offers for help. Think ahead about things you may like help with, whether it’s having someone to talk to if you’re feeling low or getting help preparing meals.
- Find someone to talk to. You might have a close friend or family member who’s a good listener. Or talk to a counselor, medical social worker, or pastoral or religious counselor.
Consider joining a support group for people with cancer. You may find strength and encouragement in being with people who are facing the same challenges you are. Ask your doctor, nurse or social worker about groups in your area. Or try online message boards, such as those available through the American Cancer Society 25.
Alternative medicine
Complementary and alternative therapies may help you cope with the side effects of cancer and cancer treatment. For instance, people with esophageal cancer may experience pain caused by cancer treatment or by a growing tumor. Your doctor can work to control your pain by treating the cause or with medications. Still, pain may persist, and complementary and alternative therapies may help you cope.
Options include:
- Acupuncture
- Guided imagery
- Massage
- Relaxation techniques
Ask your doctor whether these options are safe for you.
Treating esophageal cancer by stage
The type of treatment(s) your doctor recommends will depend on the stage of the cancer and on your overall health. This section sums up the options usually considered for each stage of esophageal cancer.
Stage 0 esophagus cancer treatment
A stage 0 tumor contains abnormal cells called high-grade dysplasia and is a type of pre-cancer. The abnormal cells look like cancer cells, but they are only found in the inner layer of cells lining the esophagus (the epithelium). They have not grown into deeper layers of the esophagus. This stage is often diagnosed when someone with Barrett’s esophagus has a routine biopsy.
Options for treatment typically include endoscopic treatments such as photodynamic therapy (PDT), radiofrequency ablation (RFA), or endoscopic mucosal resection (EMR). Long-term follow-up with frequent upper endoscopy is very important after endoscopic treatment to continue to look for pre-cancer (or cancer) cells in the esophagus.
Another option is to have the abnormal part of the esophagus removed with an esophagectomy. This is a major operation, but one advantage of this approach is that it doesn’t require lifelong follow-up with endoscopy.
Stage 1 esophagus cancer treatment
In this stage the cancer has grown into some of the deeper layers of the esophagus wall (past the innermost layer of cells) but has not reached the lymph nodes or other organs.
- T1 cancers: Some very early stage I cancers that are only in a small area of the mucosa and haven’t grown into the submucosa (T1a tumors) can be treated with endoscopic mucosal resection, sometimes followed by another type of endoscopic procedure, like ablation, to destroy any remaining abnormal areas in the esophagus lining. Other times, ablation alone is enough treatment. But most patients with T1 cancers who are healthy enough will have surgery (esophagectomy) to remove the part of their esophagus that contains the cancer. Chemotherapy and radiation therapy given at the same time (chemoradiation) may be recommended after surgery if there are signs that all of the cancer may not have been removed.
- T2 cancers: For patients with cancers that have invaded the muscularis propia (T2 tumors), treatment with chemoradiation is often given before surgery. Surgery alone may be an option for smaller tumors (less than 2 cm). If the cancer is in the part of the esophagus near the stomach, chemo without radiation may be given before surgery. If the cancer is in the upper part of the esophagus (in the neck), chemoradiation may be recommended as the main treatment instead of surgery. For some patients, this may cure the cancer. Close follow-up with endoscopy is very important in looking for possible signs of cancer returning.
People with stage 1 cancers who can’t have surgery because they have other serious health problems, or who don’t want surgery, may be treated with endoscopic mucosal resection and endoscopic ablation, chemo, radiation therapy, or both together (chemoradiation).
Stages 2 and 3 esophageal cancer treatment
Your treatment depends on whether you have squamous cell cancer or adenocarcinoma.
Stage 2 includes cancers that have grown into the main muscle layer of the esophagus or into the connective tissue on the outside of the esophagus. This stage also includes some cancers that have spread to 1 or 2 nearby lymph nodes.
Stage 3 includes some cancers that have grown through the wall of the esophagus to the outer layer, as well as cancers that have grown into nearby organs or tissues. It also includes most cancers that have spread to nearby lymph nodes.
For squamous cell cancer you usually have chemoradiotherapy. And then you either have:
- surgery to remove part or all of your oesophagus
- no further treatment and the doctors keep a close eye on you – this is called active surveillance
For adenocarcinoma you either have:
- chemotherapy before surgery
- chemotherapy before and after surgery
- chemoradiotherapy before surgery
For people who are healthy enough, treatment for these cancers is most often chemoradiation (chemotherapy plus radiation therapy) followed by surgery. Patients with adenocarcinoma at the place where the stomach and esophagus meet (the gastroesophageal junction) are sometimes treated with chemo (without radiation) followed by surgery. Surgery alone may be an option for some small tumors.
If surgery is the first treatment, chemoradiation may be recommended afterward, especially if the cancer is an adenocarcinoma or if there are signs that some cancer may have been left behind.
In some instances (especially for cancers in the upper part of the esophagus), chemoradiation may be recommended as the main treatment instead of surgery. Patients who do not have surgery need close follow-up with endoscopy to look for possible signs of remaining cancer. Unfortunately, even when cancer cannot be seen, it can still be present below the inner lining of the esophagus, so close follow-up is very important.
People who cannot have surgery because they have other serious health problems or the cancer is too large to remove are usually treated with chemoradiation. If chemoradiation isn’t an option, chemotherapy, immunotherapy, or a combination of the two might be used. Sometimes, two immunotherapy drugs might be used together. For people with gastroesophageal junction cancers that are HER2 positive, immunotherapy with pembrolizumab, plus chemotherapy, plus the targeted drug, trastuzumab, might be used as the first treatment.
Stage 4 esophageal cancer treatment
Stage 4 esophageal cancer has spread to distant lymph nodes or to other distant organs.
In general, these cancers are very hard to get rid of completely, so surgery to try to cure the cancer is usually not a good option. Treatment is used mainly to help keep the cancer under control for as long as possible and to relieve any symptoms it is causing.
Some stage 4 esophageal cancers haven’t spread to distant body parts, such as the lungs or liver. You might be able to have:
- chemoradiotherapy on its own or before surgery
- chemotherapy and surgery
Some stage 4 esophageal cancers have spread further and you can’t have surgery. Treatment aims to control the cancer and maintain a good quality of life. You might have:
- chemotherapy
- radiotherapy
- targeted cancer drugs or immunotherapy
- symptom control, such as treatment to help you swallow food
Chemo may be given (possibly along with targeted drug therapy or immunotherapy) to try to help patients feel better and live longer. Sometimes, two immunotherapy drugs might be used together. Radiation therapy or other treatments may be used to help with pain or trouble swallowing. Another option at some point might be treatment with immunotherapy by itself. If the cancer cells have certain gene changes, a targeted drug such as larotrectinib (Vitrakvi) or entrectinib (Rozlytrek) might be an option.
For cancers that started at the gastroesophageal (GE) junction, treatment with the targeted drug ramucirumab (Cyramza) may be an option at some point. It can be given by itself or combined with chemo. Other options at some point might include treatment with an immunotherapy drug (possibly along with chemo), or the chemotherapy combination pill trifluridine–tipiracil (Lonsurf). If the cancer is HER2-positive, treatment with the targeted drug trastuzumab, plus the immunotherapy drug pembrolizumab, plus chemotherapy, can be given as the first treatment. The targeted drug fam-trastuzumab deruxtecan (Enhertu) might be an option at some point.
Recurrent esophageal cancer treatment
Recurrent means the cancer has come back after treatment. The recurrence may be local (near the area of the initial tumor), or it may be in distant organs. Treatment of esophageal cancer that comes back (recurs) after initial treatment depends on where it recurs and what treatments have been used, as well as a person’s health and wishes for further treatment.
Local recurrence
If the cancer was initially treated endoscopically (such as with endoscopic mucosal resection or photodynamic therapy), it most often comes back in the esophagus. This type of recurrence is often treated with surgery to remove the esophagus. If the patient isn’t healthy enough for surgery, the cancer may be treated with chemotherapy, radiation, or both.
If cancer recurs locally (such as in nearby lymph nodes), radiation and/or chemotherapy may be used after the esophagus has been removed. Radiation may not be an option if it was already given as part of the initial treatment. If chemotherapy was given before, it is usually still possible to give more chemotherapy. Sometimes the same drugs that were used before are given again, but often other drugs are used. Other treatment options for local recurrence after surgery might include more surgery or other treatments to help prevent or relieve symptoms.
If the cancer recurs locally after chemoradiation (without surgery), esophagectomy might be an option if the person is healthy enough. If surgery is not possible, treatment options might include chemotherapy or other treatments to help prevent or relieve symptoms.
Distant recurrence
Esophageal cancer that recurs in distant parts of the body is treated like a stage IV cancer.
Your options depend on which, if any, drugs you received before the cancer came back and how long ago you received them, as well as on your health. Radiation therapy may be an option to relieve symptoms as well.
Recurrent cancers can often be hard to treat, so you might also want to ask your doctor if you might be eligible for clinical trials involving newer treatments.
Managing symptoms of recurrent esophageal cancer
Some people prefer not to have treatments that have serious side effects and choose to receive only treatments that will help keep them comfortable and add to their quality of life.
Living as esophageal cancer survivor
For some people with esophagus cancer, treatment can remove or destroy the cancer. For other people, the esophagus cancer might never go away completely.
Talk with your doctor about developing a survivorship care plan for you. This plan might include:
- A suggested schedule for follow-up exams and tests
- A schedule for other tests you might need to look for long-term health effects from your cancer or its treatment
- A list of possible late- or long-term side effects from your treatment, including what to watch for and when you should contact your doctor
- Suggestions for things you can do that might improve your health and possibly lower your chances of the cancer coming back (such diet changes and increasing physical activity).
- Reminders to keep your appointments with your primary care provider, who will monitor your general health care
Supportive treatments are aimed at helping to relieve the symptoms of esophagus cancer. In some cases they are used along with other treatments that focus on curing the cancer, but are often used in people with advanced cancer to help improve their quality of life.
Trouble swallowing
Cancer of the esophagus often causes trouble swallowing, which can lead to weight loss and weakness due to poor nutrition. A team of doctors and nutritionists can work with you to provide nutritional supplements and information about your individual nutritional needs during and after treatment. Certain surgeries to treat esophageal cancer can also affect your eating habits and may make gaining weight difficult. Your cancer care team can give you suggestions such as eating small frequent meals, using nutritional supplements, and other advice to help you maintain your weight and nutritional intake.
Some people with esophageal cancer treated with surgery or radiation therapy to the esophagus may have later problems with an esophageal stricture (narrowing of the esophagus). This can be helped with procedures to open this area such as placing an esophageal stent or sometimes using esophageal dilatation.
Pain
There are many ways to control pain caused by cancer of the esophagus and its treatment. If you have pain, tell your cancer care team right away, so they can give you quick and effective pain management.
Nutrition
Eating right can be hard for anyone, but it can get even tougher during and after cancer treatment. This is especially true for cancers of the esophagus. The cancer or its treatment may affect how you swallow or cause other problems. Nausea can be a problem from some treatments. You may not feel like eating and lose weight when you don’t want to.
- During treatment: Many people lose weight or have taste problems during treatment. If this happens to you, do the best you can. Eat whatever appeals to you. Eat what you can, when you can. Now is not the time to restrict your diet. You may find it helps to eat small portions every 2 to 3 hours. Try to keep in mind that these problems usually improve over time. You may want to ask your cancer team about seeing a dietitian, an expert in nutrition who can give you ideas on how to optimize your weight and diet during treatment. Some patients may benefit from having a feeding tube put in temporarily while they get treatment.
- After treatment: If the stomach was used to replace all or part of the esophagus, the stomach might not be able to hold food for digestion like it did before. Swallowed food passes quickly into the intestine, which can cause diarrhea, sweating, and flushing after eating. This is called dumping syndrome. This may mean you have to change your diet and how you eat. For example, you may need to eat smaller amounts of food more often. Your health care team can help you adjust your diet if you are having problems eating.
- Key Statistics for Esophageal Cancer. https://www.cancer.org/cancer/types/esophagus-cancer/about/key-statistics.html[↩][↩][↩]
- Esophageal Cancer — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/esoph.html[↩][↩][↩][↩][↩]
- Khieu M, Mukherjee S. Barrett Esophagus. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430979[↩][↩]
- Barrett esophagus. Medline Plus. https://medlineplus.gov/ency/article/001143.htm[↩][↩]
- Clermont M, Falk GW. Clinical Guidelines Update on the Diagnosis and Management of Barrett’s Esophagus. Dig Dis Sci. 2018 Aug;63(8):2122-2128. doi: 10.1007/s10620-018-5070-z[↩][↩]
- Shaheen NJ, Falk GW, Iyer PG, Gerson LB; American College of Gastroenterology. ACG Clinical Guideline: Diagnosis and Management of Barrett’s Esophagus. Am J Gastroenterol. 2016 Jan;111(1):30-50; quiz 51. doi: 10.1038/ajg.2015.322. Epub 2015 Nov 3. Erratum in: Am J Gastroenterol. 2016 Jul;111(7):1077.[↩]
- Beg S, Ragunath K, Wyman A, Banks M, Trudgill N, Pritchard DM, Riley S, Anderson J, Griffiths H, Bhandari P, Kaye P, Veitch A. Quality standards in upper gastrointestinal endoscopy: a position statement of the British Society of Gastroenterology (BSG) and Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland (AUGIS). Gut. 2017 Nov;66(11):1886-1899. doi: 10.1136/gutjnl-2017-314109. Epub 2017 Aug 18. Erratum in: Gut. 2017 Dec;66(12 ):2188.[↩]
- Japan Esophageal Society. Japanese Classification of Esophageal Cancer, 11th Edition: part I. Esophagus. 2017;14(1):1-36. doi: 10.1007/s10388-016-0551-7[↩]
- Akın H, Aydın Y. How should we describe, diagnose and observe the Barrett’s esophagus? Turk J Gastroenterol. 2017 Dec;28(Suppl 1):S26-S30. doi: 10.5152/tjg.2017.08[↩]
- Koike T, Saito M, Ohara Y, Hatta W, Masamune A. Current status of surveillance for Barrett’s esophagus in Japan and the West. DEN Open. 2022 Feb 13;2(1):e94. doi: 10.1002/deo2.94[↩]
- Fass R, Hell RW, Garewal HS, Martinez P, Pulliam G, Wendel C, Sampliner RE. Correlation of oesophageal acid exposure with Barrett’s oesophagus length. Gut. 2001 Mar;48(3):310-3. doi: 10.1136/gut.48.3.310[↩]
- Koek GH, Sifrim D, Lerut T, Janssens J, Tack J. Multivariate analysis of the association of acid and duodeno-gastro-oesophageal reflux exposure with the presence of oesophagitis, the severity of oesophagitis and Barrett’s oesophagus. Gut. 2008 Aug;57(8):1056-64. doi: 10.1136/gut.2006.119206[↩]
- Champion G, Richter JE, Vaezi MF, Singh S, Alexander R. Duodenogastroesophageal reflux: relationship to pH and importance in Barrett’s esophagus. Gastroenterology. 1994 Sep;107(3):747-54. doi: 10.1016/0016-5085(94)90123-6[↩]
- Barrett’s Esophagus. American College of Gastroenterology. http://patients.gi.org/topics/barretts-esophagus/[↩][↩]
- Desai TK, Krishnan K, Samala N, Singh J, Cluley J, Perla S, Howden CW. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett’s oesophagus: a meta-analysis. Gut. 2012 Jul;61(7):970-6. doi: 10.1136/gutjnl-2011-300730[↩]
- Erőss B, Farkas N, Vincze Á, Tinusz B, Szapáry L, Garami A, Balaskó M, Sarlós P, Czopf L, Alizadeh H, Rakonczay Z Jr, Habon T, Hegyi P. Helicobacter pylori infection reduces the risk of Barrett’s esophagus: A meta-analysis and systematic review. Helicobacter. 2018 Aug;23(4):e12504. doi: 10.1111/hel.12504[↩]
- Thrift AP. Barrett’s Esophagus and Esophageal Adenocarcinoma: How Common Are They Really? Dig Dis Sci. 2018 Aug;63(8):1988-1996. doi: 10.1007/s10620-018-5068-6[↩]
- Michopoulos S. Critical appraisal of guidelines for screening and surveillance of Barrett’s esophagus. Ann Transl Med. 2018 Jul;6(13):259. doi: 10.21037/atm.2018.05.09[↩]
- Bellizzi AM, Hafezi-Bakhtiari S, Westerhoff M, Marginean EC, Riddell RH. Gastrointestinal pathologists’ perspective on managing risk in the distal esophagus: convergence on a pragmatic approach. Ann N Y Acad Sci. 2018 Dec;1434(1):35-45. doi: 10.1111/nyas.13680[↩]
- Esophageal Cancer Stages. https://www.cancer.org/cancer/types/esophagus-cancer/detection-diagnosis-staging/staging.html[↩]
- Survival Rates for Esophageal Cancer. https://www.cancer.org/cancer/types/esophagus-cancer/detection-diagnosis-staging/survival-rates.html[↩]
- Mukkamalla SKR, Recio-Boiles A, Babiker HM. Esophageal Cancer. [Updated 2022 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459267[↩]
- Zhao X, Ren Y, Hu Y, Cui N, Wang X, Cui Y. Neoadjuvant chemotherapy versus neoadjuvant chemoradiotherapy for cancer of the esophagus or the gastroesophageal junction: A meta-analysis based on clinical trials. PLoS One. 2018 Aug 23;13(8):e0202185. doi: 10.1371/journal.pone.0202185[↩]
- Tramontano AC, Nipp R, Mercaldo ND, Kong CY, Schrag D, Hur C. Survival Disparities by Race and Ethnicity in Early Esophageal Cancer. Dig Dis Sci. 2018 Nov;63(11):2880-2888. doi: 10.1007/s10620-018-5238-6[↩]
- American Cancer Society. https://www.cancer.org/[↩]