Contents
What is esophageal varices
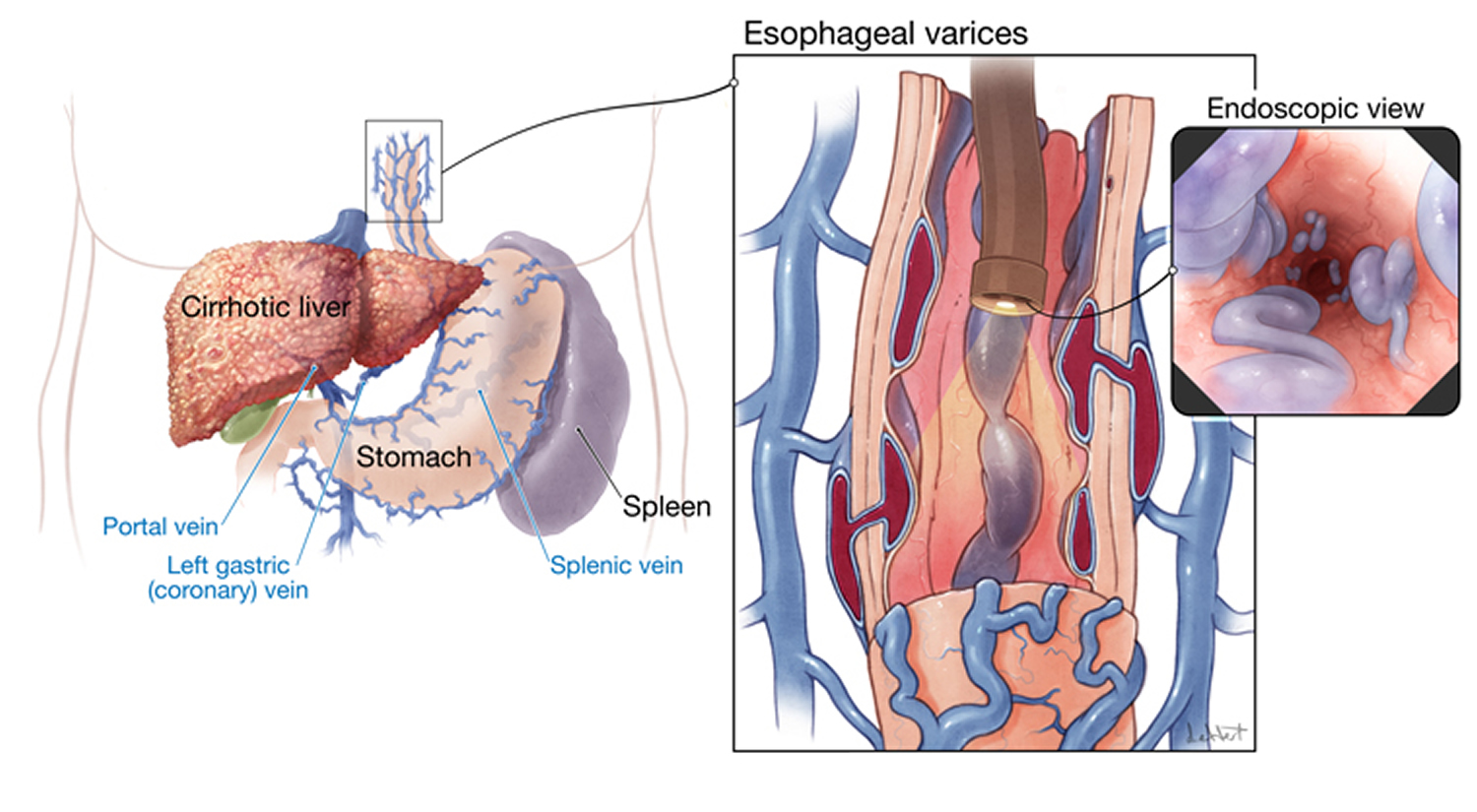
Esophageal varices are abnormal, enlarged veins in the tube that connects the throat and stomach (esophagus). Esophageal varices develop when blood pressure in portal veins becomes greater then 10mmHg so blood gets pushed back through alternative routes in order to reach the heart rather than going through the liver. The normal hepatic venous pressure gradient is typically 1–5 mmHg 1. The risk of developing esophageal varices increases when the hepatic venous pressure gradient reaches a minimum pressure of 10–12 mmHg 2. Portal hypertension, as measured by the hepatic venous pressure gradient, occurs through complex physiological responses resulting in both mechanical and dynamic blockages in the liver 3. The mechanical component of blockage is a result of intrahepatic scar tissue starting at the level of hepatic microcirculation. The scar tissue (fibrosis) develops because of damage to liver cells occurring as a result of alcohol or other liver-damaging processes. Fibroblast and activated hepatic stellate cells appear at the area of injury and deposit collagen. This process leads to connective tissue formation in the periportal and pericentral zones of the liver. These spiderweb-like tissue formations eventually connect the portal triads and central veins of the liver. Also, these areas of fine connective tissue surround small groups of liver cells and, in turn, cause regeneration of the liver cells with resulting nodule formation. This mechanical process causes hardening of the tissue and nodule formation within the liver and initiates the blockage of circulatory pathways 4. This condition occurs most often in people with serious liver diseases.
Esophageal varices develop when normal blood flow to the liver is blocked by a clot or scar tissue in the liver. To go around the blockages, blood flows into smaller blood vessels that aren’t designed to carry large volumes of blood. The vessels can leak blood or even rupture, causing life-threatening bleeding.
Patients with compensated cirrhosis without gastroesophageal varices typically develop varices at a rate of 5 to 10% per year 1. In addition, patients with small esophageal varices progress to large varices at a rate of 8% per year 1. It is important to decrease the risk of variceal hemorrhage, which occurs at a rate of 5 to 15% per year, with the highest rates in those with large esophageal varices, decompensated cirrhosis, or red wale markings on the esophageal varices 1. The term pre-primary prophylaxis refers to prevention of the development of esophageal varices in patients with portal hypertension. Primary prophylaxis is defined as prevention of variceal hemorrhage in patients with known esophageal varices but no history of variceal hemorrhage. Secondary prophylaxis describes variceal hemorrhage prevention measures for patients with a known history of variceal hemorrhage.
For patients with absence of esophageal varices, pre-primary prophylaxis is not recommended to prevent the development of varices. In patients with compensated cirrhosis (i.e. absence of ascites, encephalopathy, jaundice and varices), a large multi-center, placebo-controlled, double-blinded trial showed that nonselective beta-blockers do not prevent the development of varices in the absence of demonstrable effect on hepatic venous pressure gradient and are associated with unwanted side effects 5. Individuals with compensated cirrhosis and absence of varices should undergo screening esophagogastroduodenoscopy every 2 to 3 years.
For patients with esophageal varices the goal of treatment is to reduce portal hypertension. A number of drugs and medical procedures can help prevent and stop bleeding from esophageal varices. By reducing portal pressure there is a concomitant decrease in the probability of esophageal bleeding. Reducing the risk of primary bleeding of esophageal varices can be accomplished by using nonselective ß-blocker (beta-blocker) therapy. This pharmacological intervention works by reducing the hepatic venous pressure gradient 6.
Esophageal varices complications
The most serious complication of esophageal varices is bleeding. Once you have had a bleeding episode, your risk of another bleeding episode greatly increases. If you lose enough blood, you can go into shock, which can lead to death.
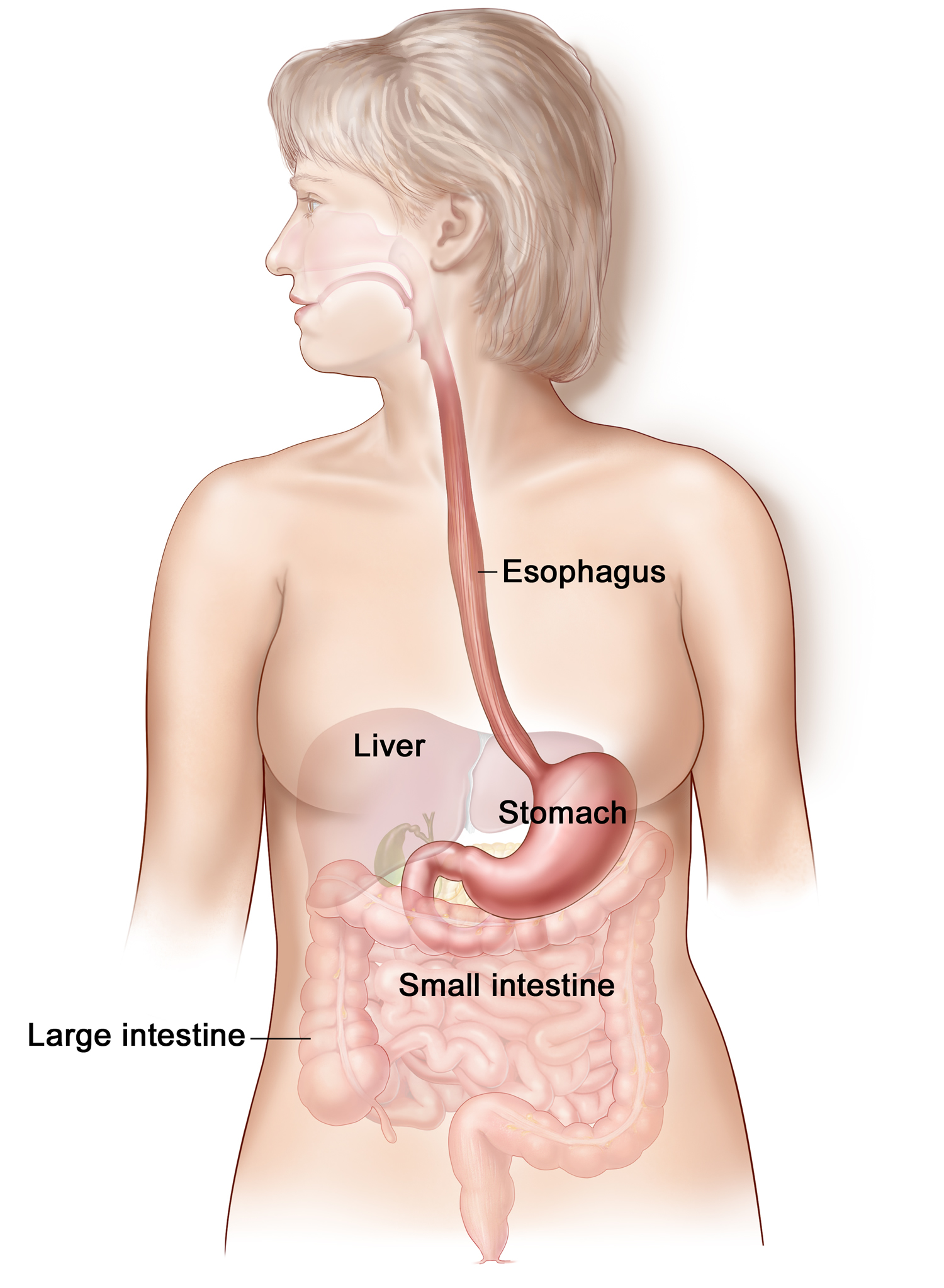
Figure 1. Esophagus
Esophageal varices grading
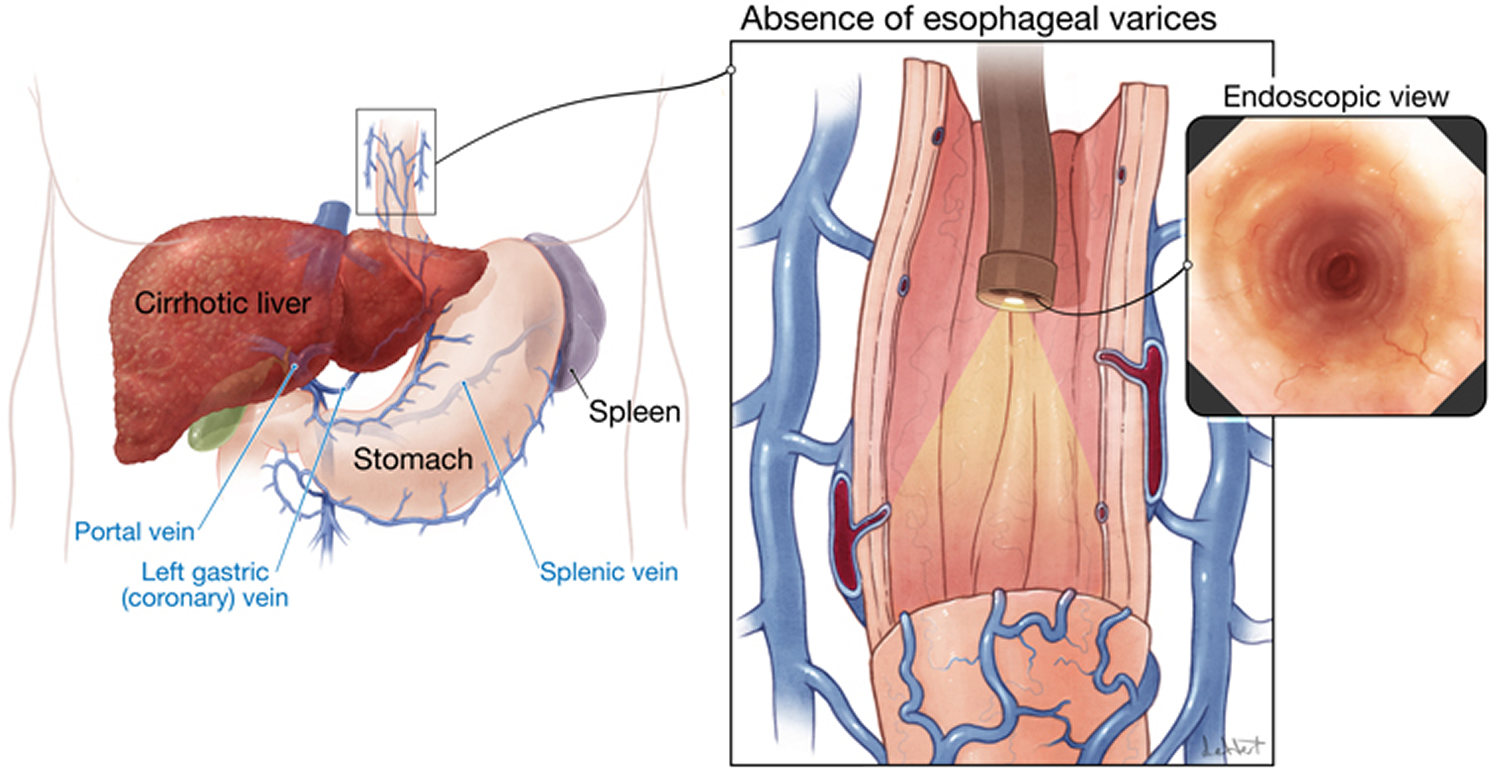
Esophageal varices are present in 30 to 40% of patients with compensated cirrhosis and in 60% of patients with decompensated cirrhosis (at the time of diagnosis of cirrhosis). Upon diagnosis of cirrhosis, screening esophagogastroduodenoscopy is recommended to evaluate for the presence of gastroesophageal varices 7. The esophagogastroduodenoscopy evaluation for esophageal varices will determine whether the patient should receive prophylaxis for variceal bleeding with a nonselective beta-blocker. Less invasive markers for the presence of esophageal varices, such as platelet count, spleen size, and liver stiffness measurement, do not accurately predict the presence of esophageal varices. If no esophageal varices are found (see Figure 3 below), an esophagogastroduodenoscopy should be repeated in 2 to 3 years. If esophageal varices are found (Figure 4), they should be classified into one of two grades: small (less than or equal to 5 mm) or large (greater than 5 mm).
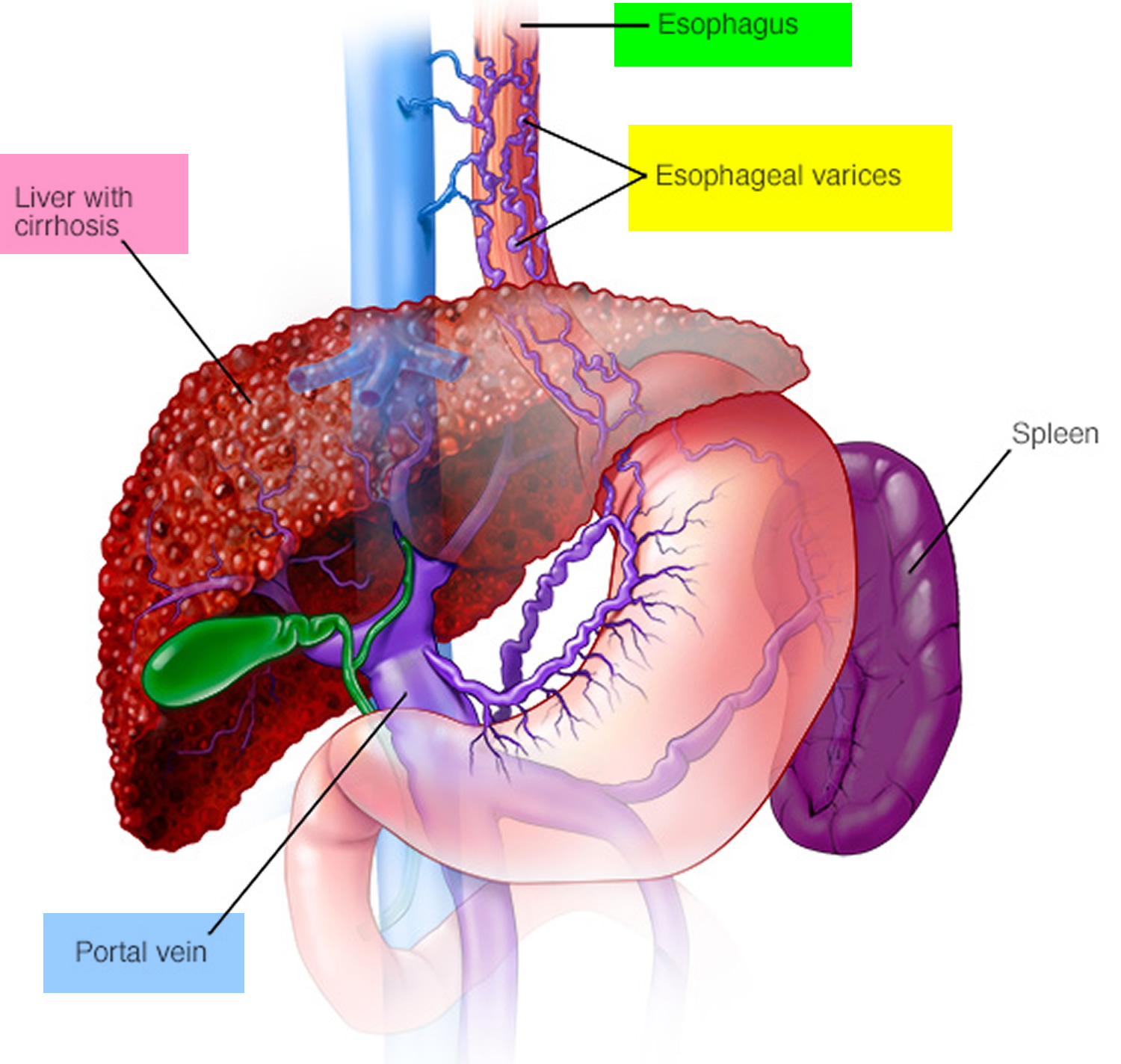
Figure 3. Liver cirrhosis without esophageal varices
Figure 4. Esophageal varices with liver cirrhosis
Small esophageal varices
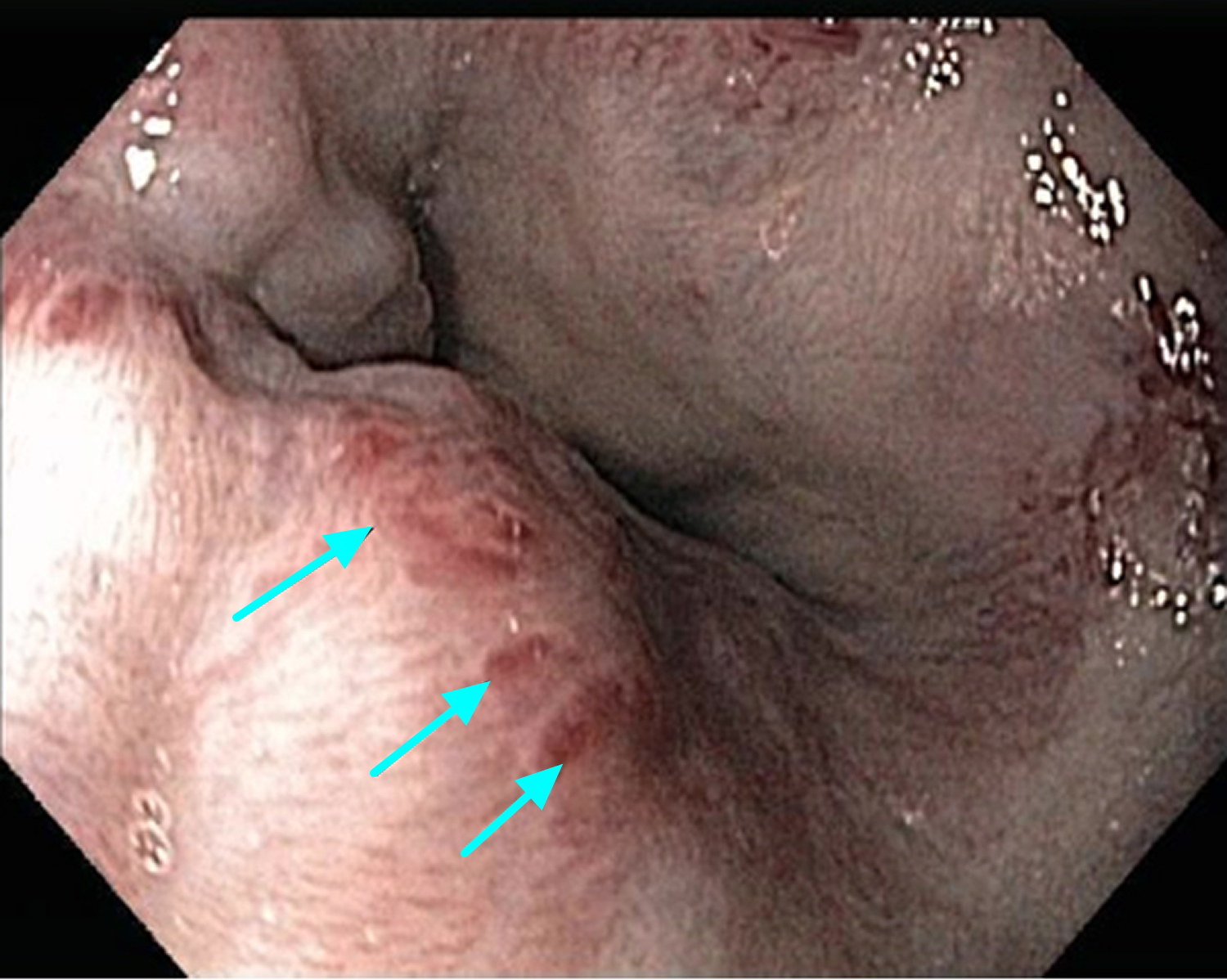
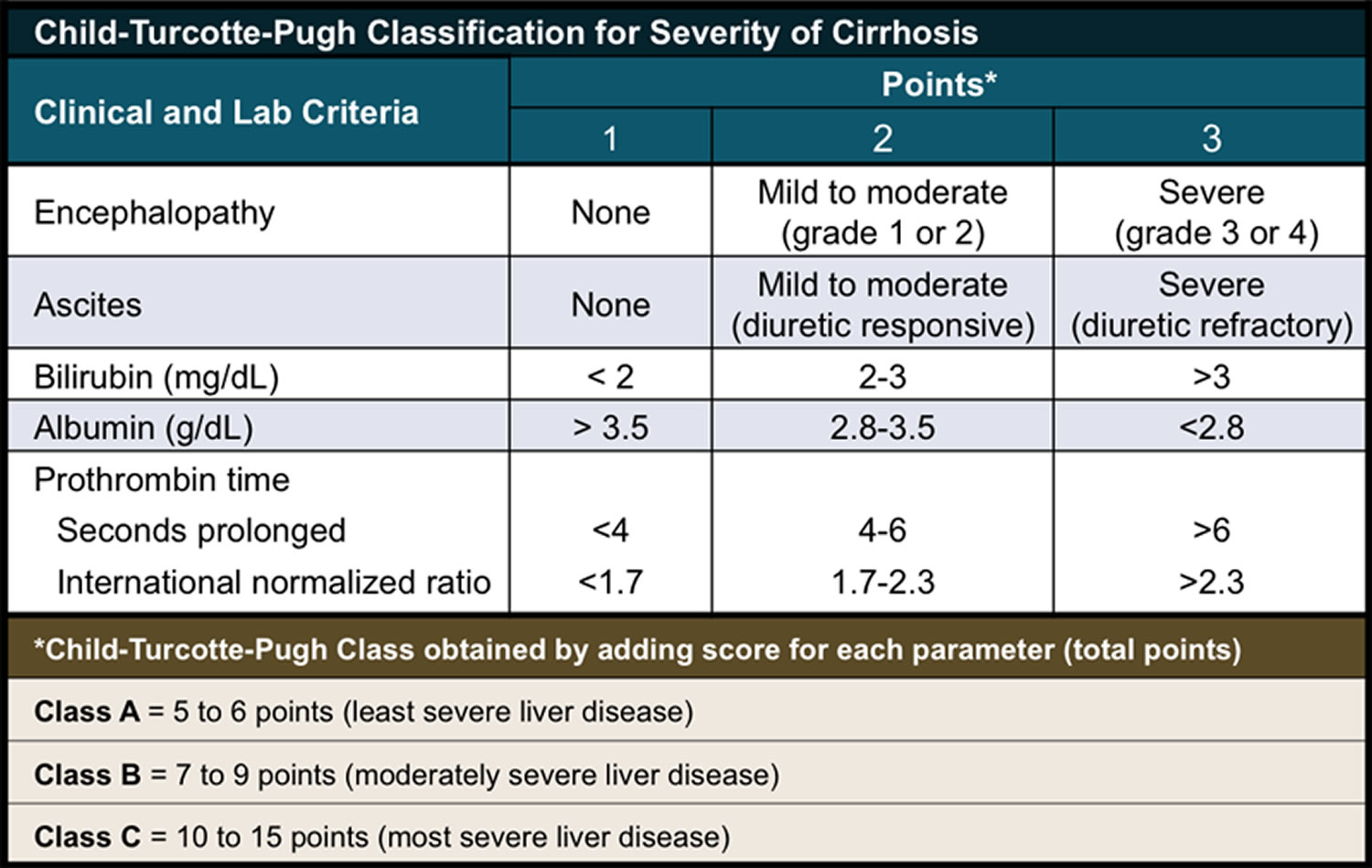
In patients with small esophageal varices (diameter of 5 mm or less) (see Figure 5 below) that have not bled, nonselective beta-blockers may slow down variceal growth, but have not been shown to confer a survival advantage 1. Given the potential for side effects, the use of nonselective beta-blockers for primary prophylaxis in patients with small esophageal varices is generally reserved for those at higher risk of hemorrhage, namely those with red wale marks (red marks or red spots) on esophageal varices (see Figure 6) or Child class B or C cirrhosis (Figure 7) 8. For patients not receiving prophylaxis with a nonselective beta-blocker, esophagogastroduodenoscopy should be repeated in 2 years, or at the time of hepatic decompensation, or annually for those with decompensated liver disease. Patients already taking a nonselective beta-blocker do not need a follow-up esophagogastroduodenoscopy.
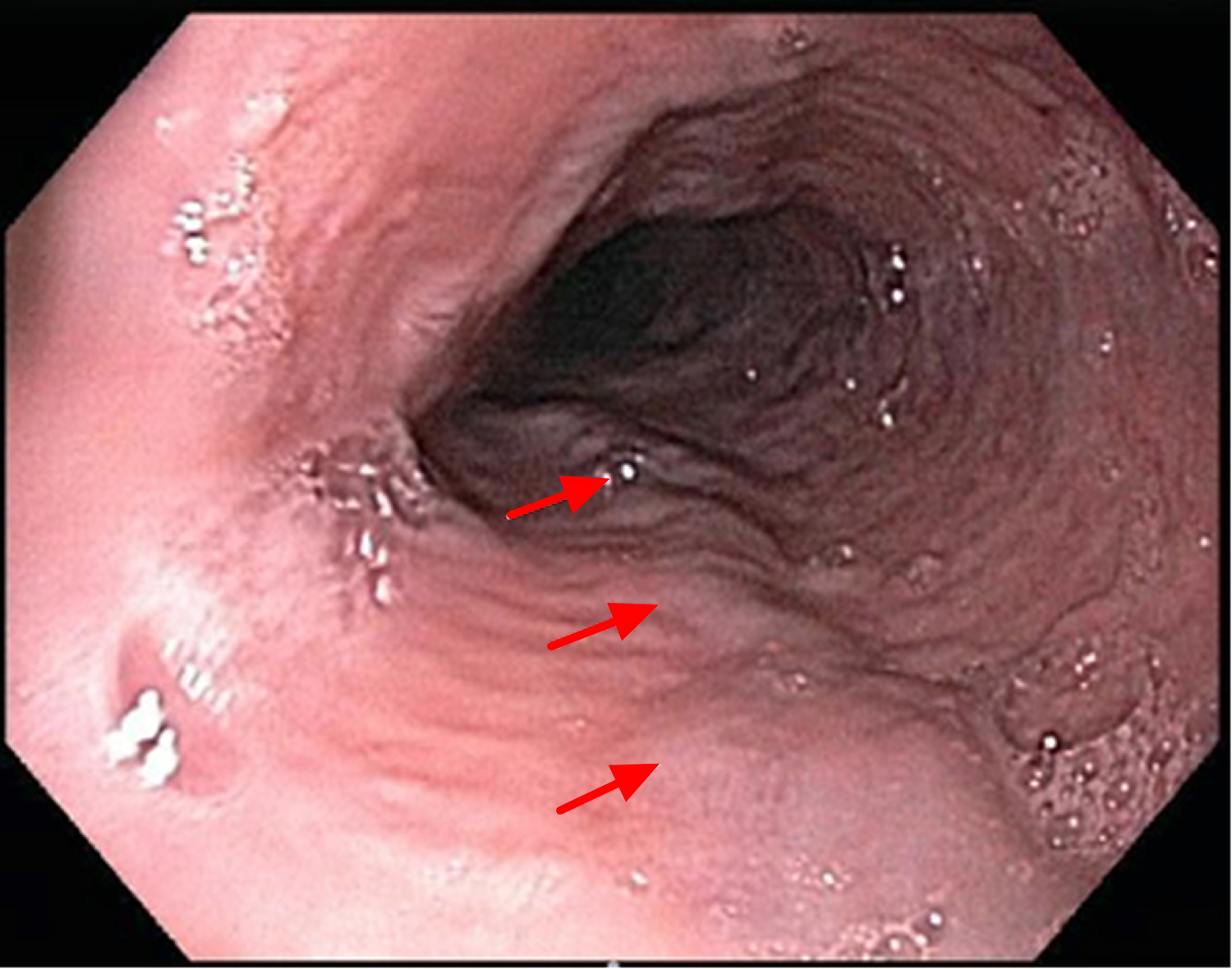
Figure 5. Small Esophageal varices (endoscopic view of the esophagus, looking down into the esophageal lumen. The red arrows are the esophageal varices)
[Source 1]Figure 6. Small Esophageal varices with red wale marks (red marks or red spots) have a higher chance of bleeding
Figure 7. Child-Turcotte-Pugh Classification for Liver Cirrhosis Severity
[Source 8]Large Esophageal Varices
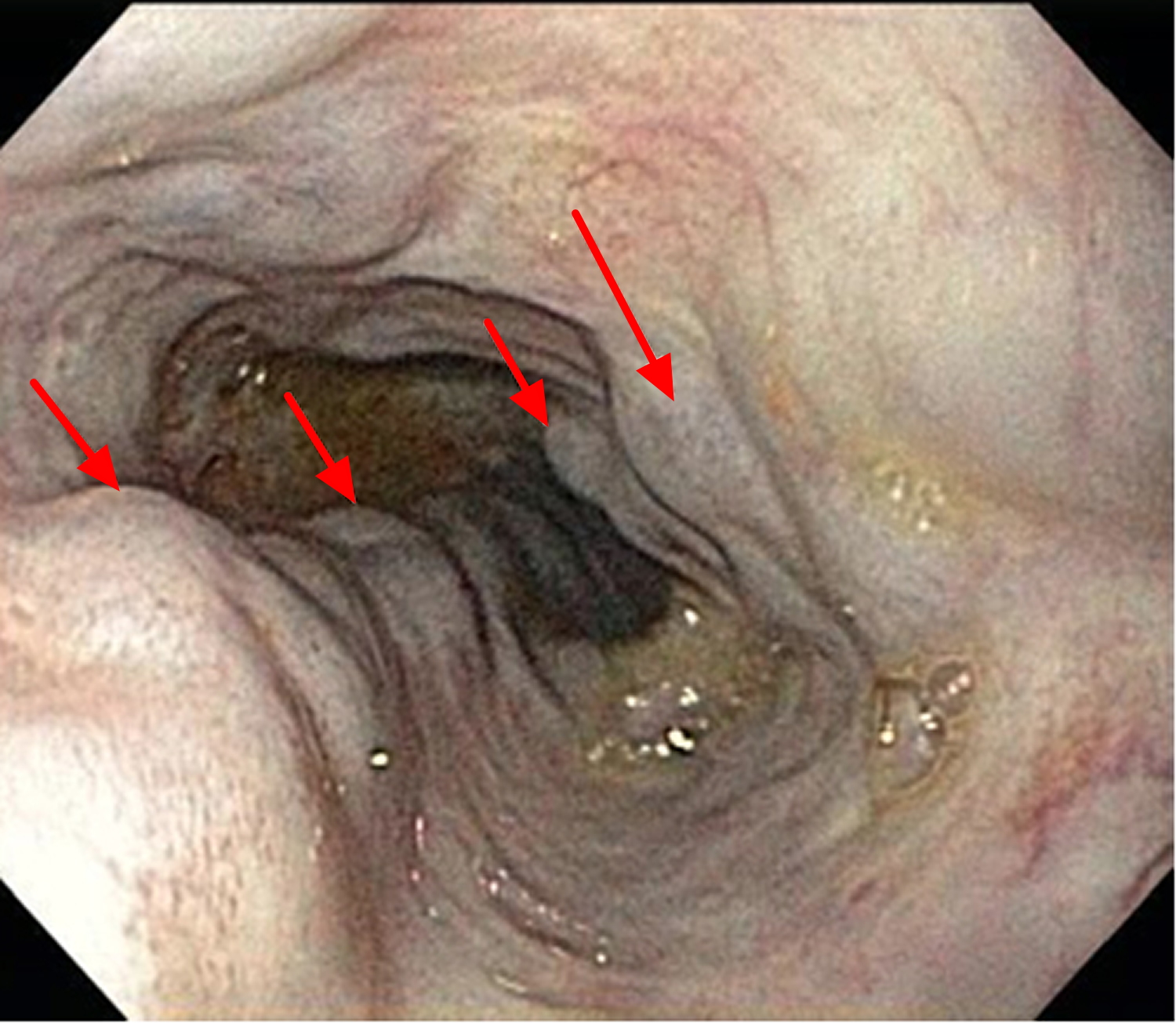
In patients with large esophageal varices (diameter greater than 5 mm) (Figure 8) that have not bled, both nonselective beta-blockers and endoscopic esophageal varices ligation lower the incidence of first variceal hemorrhage. In a meta-analysis, endoscopic esophageal varices ligation reduced risk of bleeding slightly more than nonselective beta-blocker use, but there was no difference in mortality and endoscopic variceal ligation is associated with a risk of procedure-related complications 9.
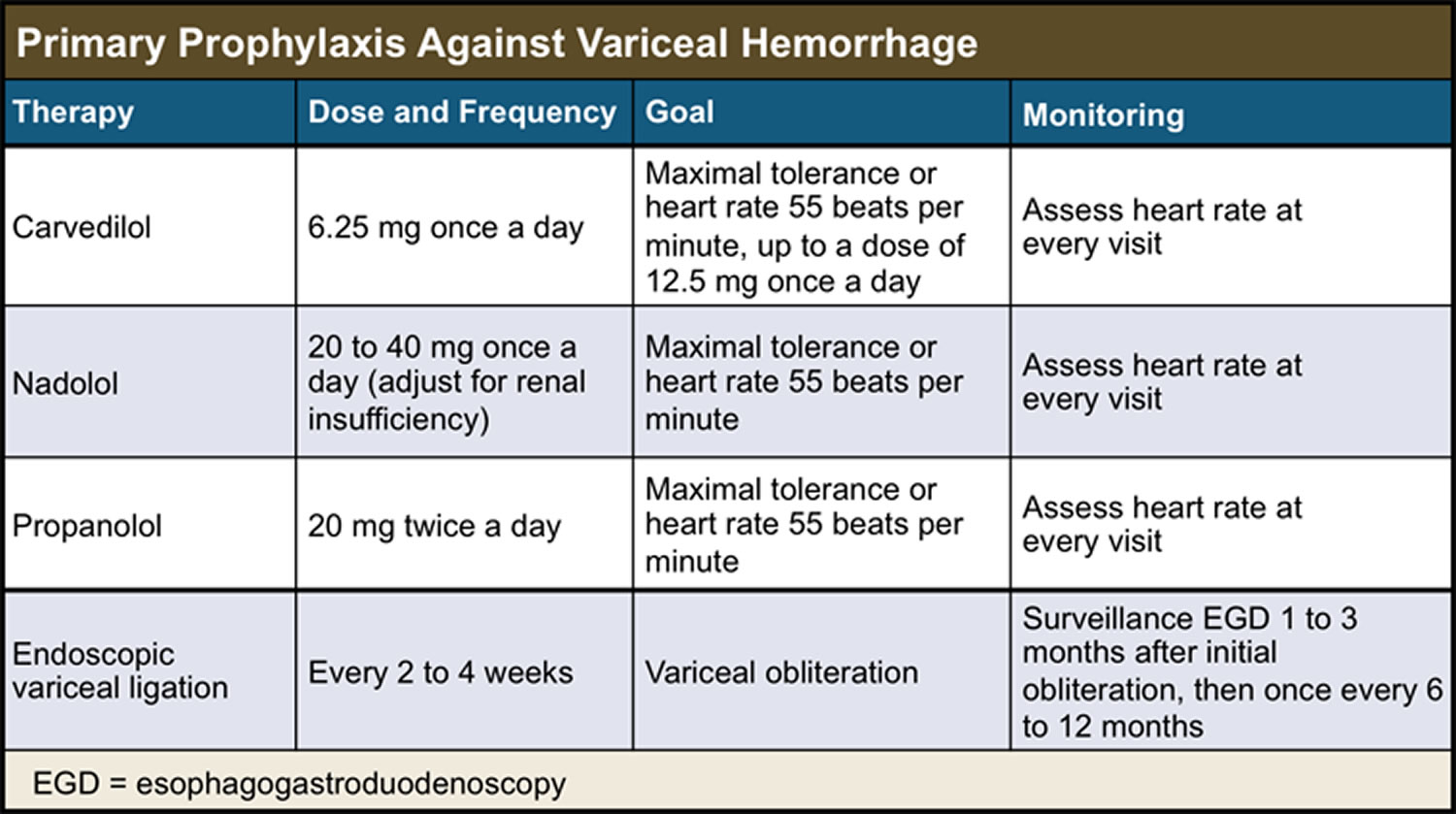
Primary prophylaxis is recommended for patients with large esophageal varices, and for those with small esophageal varices who also have red wale marks on varices or Child class B or C cirrhosis. Primary prophylaxis against variceal hemorrhage includes pharmacologic therapy with nonselective beta-blockers and endoscopic variceal ligation for patients with large esophageal varices who are unable to receive nonselective beta-blockers (Figure 9). The nonselective beta-blockers decrease cardiac output (beta-1 effect) and induce splanchnic vasoconstriction (beta-2 effect), which decreases venous portal blood inflow. In most of the published studies, investigators titrated the nonselective beta-blockers to decrease the heart rate by 25% from baseline, but since the heart rate reduction does not correlate with hepatic venous pressure gradient reduction, most experts recommend increasing to the maximally tolerated dose, or until the heart rate is approximately 55 beats per minute. There is promising data on carvedilol as a possible well-tolerated alternative agent 10. Patients receiving variceal prophylaxis need to continue the nonselective beta-blocker indefinitely, but they do not need follow-up esophagogastroduodenoscopy. For those patients with large varices who have a contraindication to or intolerance of nonselective beta-blockers, endoscopic variceal ligation should be performed every 2 to 4 weeks until the esophageal varices are eradicated. After obliteration is achieved, patients will need to continue with surveillance esophagogastroduodenoscopies every 6 to 12 months indefinitely.
Figure 8. Endoscopic view of Large Esophageal Varices (the red arrows indicate the presence of two columns of large esophageal varices)
Figure 9. Primary prophylaxis against esophageal varices bleeding/hemorrhage
Bleeding esophageal varices
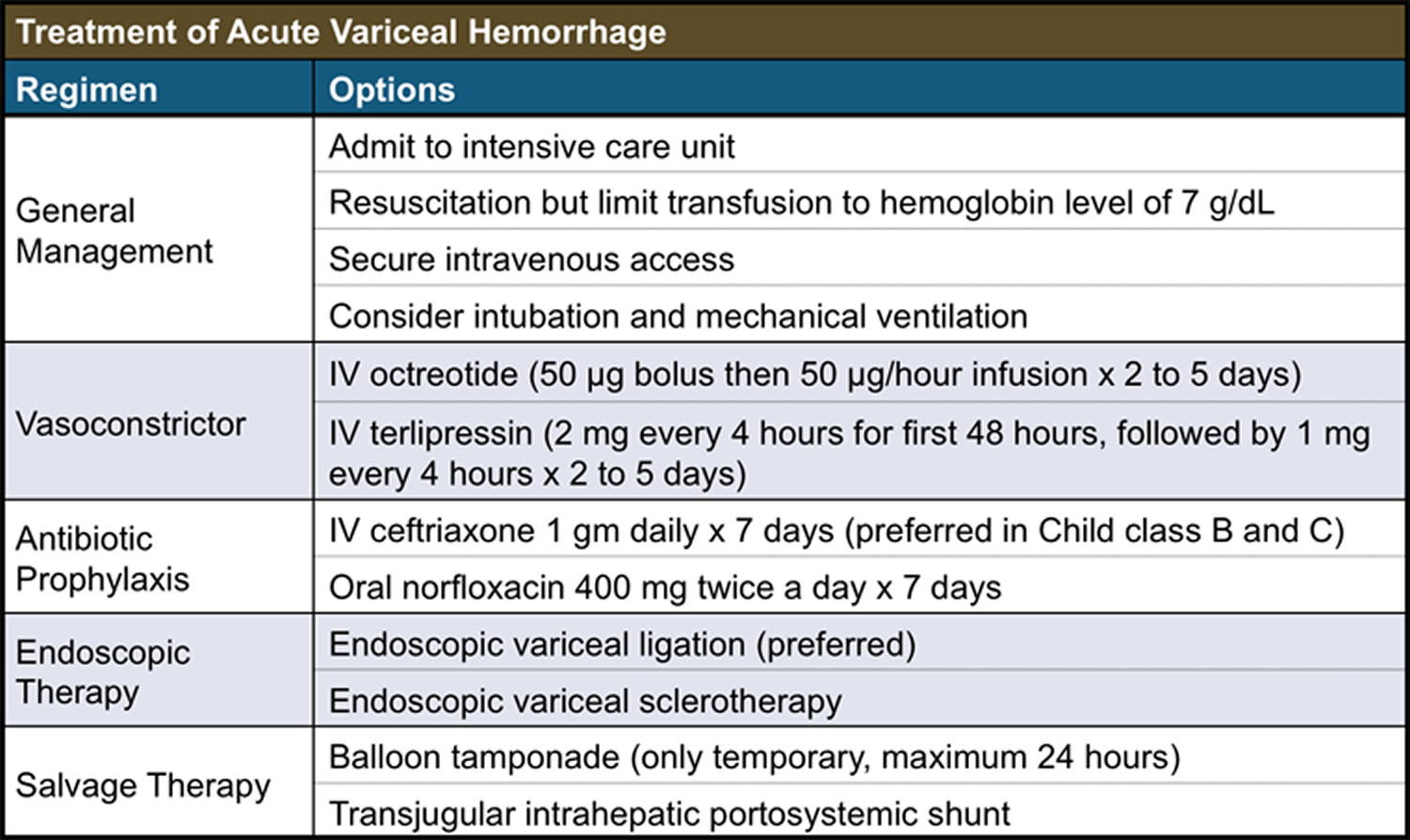
Esophageal varices bleeding accounts for 70% of all cases of upper gastrointestinal bleeding in patients with liver cirrhosis. Esophageal variceal bleeding spontaneously resolves in 40 to 50% of cases, but there is a 30 to 40% chance of early rebleeding in the first 6 weeks. Initial treatment of bleeding esophageal varices is effective in 80 to 90% of cases but mortality remains approximately 15 to 20%, with the majority of deaths due to liver failure, hepatorenal syndrome, and infections, and occurring predominantly in Child class C cirrhotic patients. The management of bleeding esophageal varices requires a multi-pronged approach (Figure 10) 7.
Untreated cirrhotic patients with a history of esophageal varices bleeding have a 60% risk of rebleeding within 1 to 2 years, with a 20% risk of dying with each episode. In the absence of transjugular intrahepatic portosystemic shunt (TIPS), patients should be started on prophylactic therapy with a nonselective beta-blocker prior to discharge from the hospital.
Gastric varices
Gastric varices are present in 20% of patients with portal hypertension, but only account for 5 to 10% of all cases of upper gastrointestinal bleeding in cirrhotic patients. Acute fundal gastric variceal bleeding (1 to 3% of all variceal bleeding episodes) is associated with a higher rate of death than gastroesophageal varices as the bleeding is usually more severe 11. Endoscopic variceal obturation with tissue adhesive (e.g. N-butyl-2-cyanoacrylate, isobutyl-2-cyanoacrylate, or thrombin) is preferred over endoscopic variceal ligation for initial management of bleeding 12. This technique requires special endoscopic expertise, so if it is not available, transjugular intrahepatic portosystemic shunt (TIPS) can also be used to control the bleeding successfully as first-line therapy or in cases of recurrent bleeding 13.
Bleeding esophageal varices symptoms
If there is only a small amount of bleeding, the only symptom may be dark or black streaks in the stools.
If larger amounts of bleeding occur, symptoms may include:
- Black, tarry stools
- Bloody stools
- Lightheadedness
- Paleness
- Symptoms of chronic liver disease
- Vomiting
- Vomiting blood
Figure 10. Treatment of acute esophageal variceal bleeding
Pharmacologic Therapy
A vasoconstrictor agent should be started at the time of admission and continued for 2 to 5 days. Terlipressin, a synthetic vasopressin analogue, has been shown to decrease mortality but is not widely available in the United States. Instead, octreotide (Sandostatin), a somatostatin analogue, is available in the United States 14. Its efficacy is controversial as it is associated with tachyphylaxis, but it may provide some benefit when used in combination with endoscopic therapy 15.
Endoscopic Therapy
Endoscopic therapy, preferably endoscopic variceal ligation, should be performed within 12 hours of admission. Sclerotherapy is an option when endoscopic variceal ligation is not technically feasible.
Infection Prophylaxis
The use of prophylactic antibiotics (norfloxacin or ceftriaxone) decreases the rate of bacterial infection, risk of early rebleeding, and mortality 16.
Rescue Therapy
Rescue therapy is still warranted in 10 to 20% of cases due to failure to control bleeding or recurrent bleeding. Early placement of a transjugular intrahepatic portosystemic shunt (TIPS) within 24 to 48 hours after admission has been shown to improve survival in patients at high risk of rebleeding (hepatic venous pressure gradient greater than or equal to 20 mm Hg or Child class C cirrhosis) 17. Balloon tamponade can assist with temporary control of hemorrhage in patients with difficult to control bleeding awaiting more definitive therapy (e.g. TIPS or endoscopic therapy).
Secondary Prophylaxis of Esophageal Varices Bleeding
Pharmacologic Therapy
Nonselective beta-blockers reduce the variceal rebleeding rate to around 43%. The combination of a nonselective beta-blocker and isosorbide mononitrate may lower the bleeding rate further, but this combination has greater side effects and is poorly tolerated. Thus, most patients use nonselective beta-blockers alone.
Endoscopic Therapy
Endoscopic variceal ligation therapy is superior to sclerotherapy for secondary prophylaxis and decreases the rebleeding rate to around 32%. Sessions are repeated every 7 to 14 days until the esophageal varices are gone and then are repeated every 3 to 6 months for surveillance.
Combination Therapy
The combination of pharmacological and endoscopic therapy is superior over either modality alone in decreasing the rebleeding rate to 14 to 23%, although there is no statistical difference in mortality 18.
Portosystemic Shunt
Placement of a transjugular intrahepatic portosystemic shunt is very effective in preventing rebleeding but has no impact on survival and is associated with an increased risk of hepatic encephalopathy. Similarly, transjugular intrahepatic portosystemic shunt has been shown to be superior to endoscopic therapy and pharmacologic therapy in reducing the risk of rebleeding but with no difference in mortality, an increased risk of hepatic encephalopathy, and increased costs. In general, placement of transjugular intrahepatic portosystemic shunt should be reserved for Child’s class A and B cirrhotic patients who fail the combination of pharmacologic and endoscopic therapy.
Referral for Liver Transplantation Evaluation
Patients who are otherwise liver transplantation candidates should be referred to a transplant center for consideration of an evaluation.
Bleeding esophageal varices survival rate
Esophageal varices are a major concern in patients with cirrhosis. These esophageal varices have a high propensity to bleed because of the fragility of the engorged blood vessels 19. Each episode of esophageal varices bleeding has a 30%–50% mortality risk (risk of dying) 6. Furthermore, after the initial episode of bleeding the incidence of rebleeding is up to 70% and frequently occurs within 6 weeks of the initial hemorrhage 2.
Esophageal varices causes
Esophageal varices sometimes form when blood flow to your liver is blocked, most often by scar tissue in the liver caused by liver disease. The blood flow begins to back up, increasing pressure within the large vein (portal vein) that carries blood to your liver.
This pressure (portal hypertension) forces the blood to seek other pathways through smaller veins, such as those in the lowest part of the esophagus. These thin-walled veins balloon with the added blood. Sometimes the veins can rupture and bleed.
Causes of esophageal varices include:
- Severe liver scarring (cirrhosis). A number of liver diseases — including hepatitis infection, alcoholic liver disease, fatty liver disease and a bile duct disorder called primary biliary cirrhosis — can result in cirrhosis.
- Blood clot (thrombosis). A blood clot in the portal vein or in a vein that feeds into the portal vein (splenic vein) can cause esophageal varices.
- A parasitic infection. Schistosomiasis is a parasitic infection found in parts of Africa, South America, the Caribbean, the Middle East and Southeast Asia. The parasite can damage the liver, as well as the lungs, intestine and bladder
Risk factors for esophageal varices
Although many people with advanced liver disease develop esophageal varices, most won’t have bleeding. Varices are more likely to bleed if you have:
- High portal vein pressure. The risk of bleeding increases with the amount of pressure in the portal vein (portal hypertension).
- Large esophageal varices. The larger the esophageal varices, the more likely they are to bleed.
- Red marks on the esophageal varices. When viewed through an endoscope passed down your throat, some esophageal varices show long, red streaks or red spots. These marks indicate a high risk of bleeding.
- Severe cirrhosis or liver failure. Most often, the more severe your liver disease, the more likely varices are to bleed.
- Continued alcohol use. Your risk of variceal bleeding is far greater if you continue to drink than if you stop, especially if your disease is alcohol related.
Esophageal varices prevention
Currently, no treatment can prevent the development of esophageal varices in people with cirrhosis. While beta blocker drugs are effective in preventing bleeding in many people who have esophageal varices, they do not prevent esophageal varices from forming.
If you’ve been diagnosed with liver disease, ask your doctor about strategies to avoid liver disease complications. To keep your liver healthy:
- Don’t drink alcohol. People with liver disease are often advised to stop drinking alcohol, since the liver processes alcohol. Drinking alcohol may stress an already vulnerable liver.
- Eat a healthy diet. Choose a plant-based diet that’s full of fruits and vegetables. Select whole grains and lean sources of protein. Reduce the amount of fatty and fried foods you eat.
- Maintain a healthy weight. An excess amount of body fat can damage your liver. Obesity is associated with a greater risk of complications of cirrhosis. Lose weight if you are obese or overweight.
- Use chemicals sparingly and carefully. Follow the directions on household chemicals, such as cleaning supplies and insect sprays. If you work around chemicals, follow all safety precautions. Your liver removes toxins from your body, so give it a break by limiting the amount of toxins it must process.
- Reduce your risk of hepatitis. Sharing needles and having unprotected sex can increase your risk of hepatitis B and C. Protect yourself by abstaining from sex or using a condom if you choose to have sex. Ask your doctor whether you should be vaccinated for hepatitis B and hepatitis A.
Esophageal varices symptoms
Esophageal varices usually don’t cause signs and symptoms unless they bleed.
Signs and symptoms of bleeding esophageal varices include:
- Vomiting and seeing significant amounts of blood in your vomit
- Black, tarry or bloody stools
- Lightheadedness
- Loss of consciousness (in severe case)
Your doctor might suspect esophageal varices if you have signs of liver disease, including:
- Yellow coloration of your skin and eyes (jaundice)
- Easy bleeding or bruising
- Fluid buildup in your abdomen (ascites)
Esophageal varices diagnosis
If you have cirrhosis, your doctor should screen you for esophageal varices when you’re diagnosed. How often you’ll undergo screening tests depends on your condition. Main tests used to diagnose esophageal varices are:
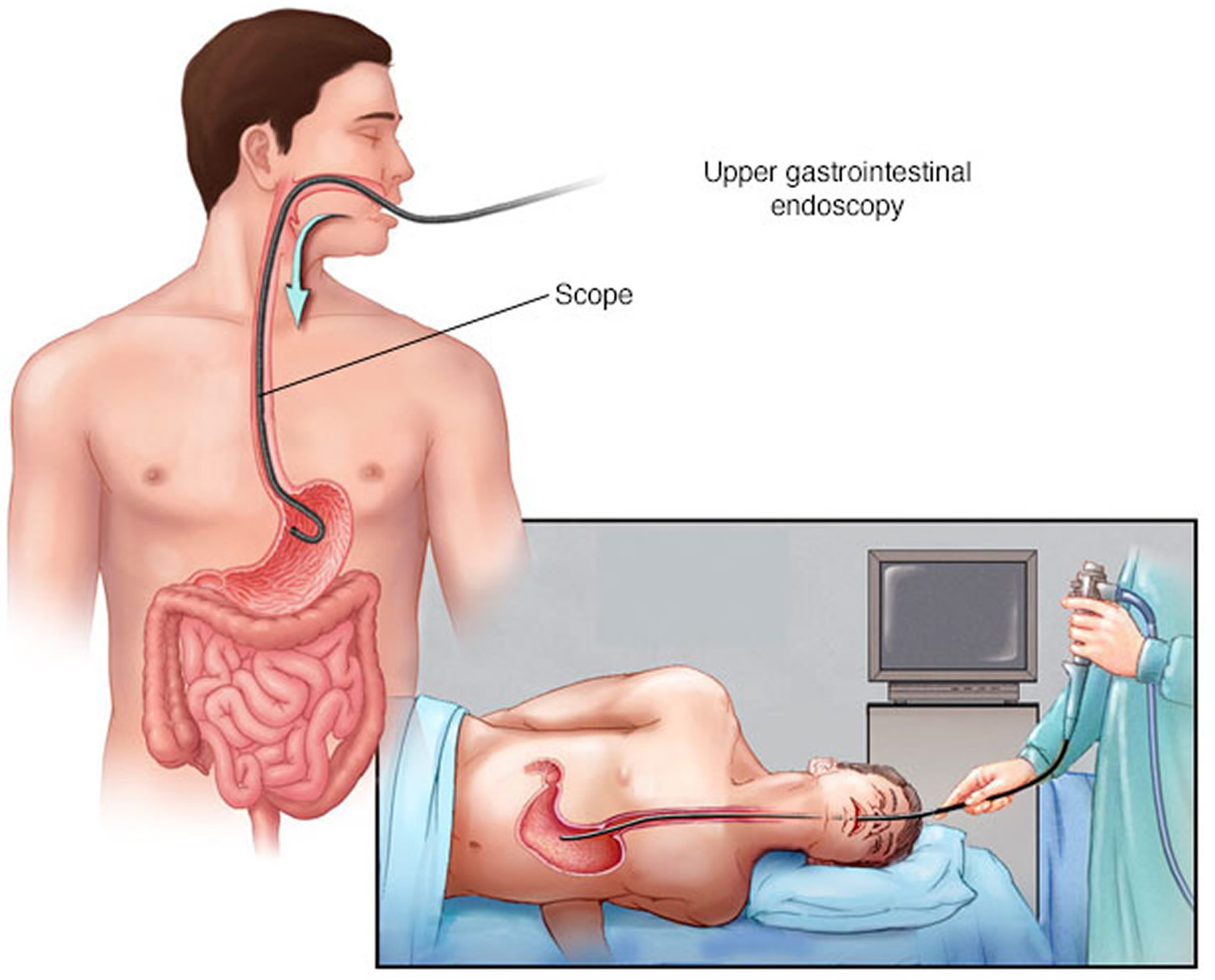
- Endoscope exam. A procedure called upper gastrointestinal endoscopy is the preferred method of screening for varices. Your doctor inserts a thin, flexible, lighted tube (endoscope) through your mouth and into your esophagus, stomach and the beginning of your small intestine (duodenum). The doctor will look for dilated veins, measure them, if found, and check for red streaks and red spots, which usually indicate a significant risk of bleeding. Treatment can be performed during the exam.
- Imaging tests. Both abdominal CT scans and Doppler ultrasounds of the splenic and portal veins can suggest the presence of esophageal varices.
- Capsule endoscopy. In this test, you swallow a vitamin-sized capsule containing a tiny camera, which takes pictures of the esophagus as it goes through your digestive tract. This might be an option for people who are unable or unwilling to have an endoscope exam. This technology is more expensive than regular endoscopy and not as available.
Figure 11. Esophagogastroduodenoscopy (endoscopy)
Esophageal varices treatment
The primary aim in treating esophageal varices is to prevent bleeding. Bleeding esophageal varices are life-threatening. If bleeding occurs, treatments are available to try to stop the bleeding.
Figure 12. Treatment consists of pharmacologic therapy to decrease portal pressure, endoscopic treatment of varices (band ligation or sclerotherapy) to treat variceal bleeding, and creation of a transjugular intrahepatic portosystemic shunt (TIPS) to reduce portal pressure if drug therapy and endoscopic treatment fail.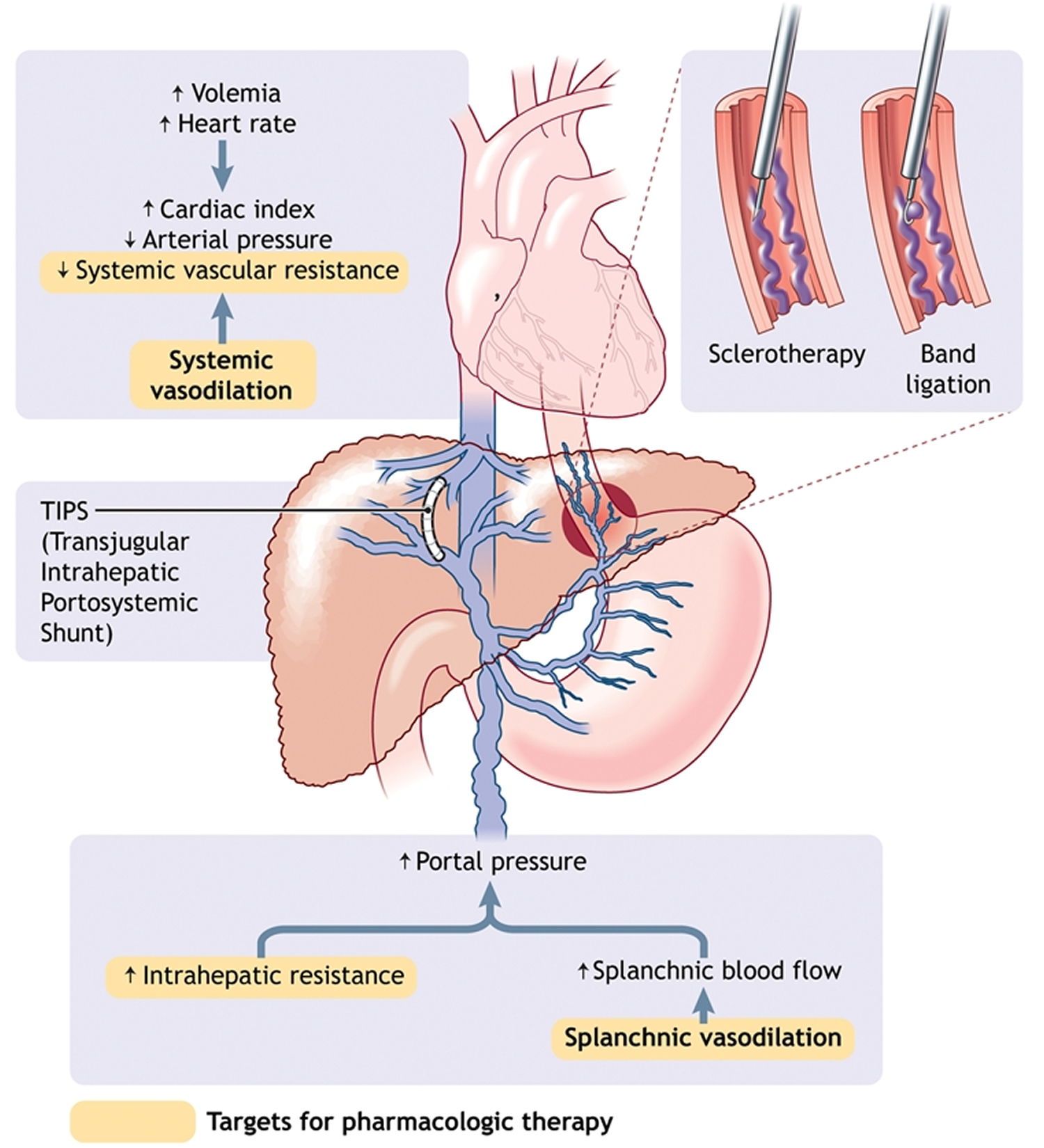
Treatment to prevent bleeding
Treatments to lower blood pressure in the portal vein may reduce the risk of bleeding esophageal varices. Treatments may include:
- Medications to reduce pressure in the portal vein. A type of blood pressure drug called a beta blocker may help reduce blood pressure in your portal vein, decreasing the likelihood of bleeding. These medications include propranolol (Inderal, Innopran) and nadolol (Corgard).
- Using elastic bands to tie off bleeding veins. If your esophageal varices appear to have a high risk of bleeding, your doctor might recommend a procedure called band ligation. Using an endoscope, the doctor snares the varices and wraps them with an elastic band, which essentially “strangles” the veins so they can’t bleed. Esophageal band ligation carries a small risk of complications, such as scarring of the esophagus.
Treatment if you’re bleeding
Bleeding varices are life-threatening, and immediate treatment is essential. Treatments used to stop bleeding and reverse the effects of blood loss include:
- Using elastic bands to tie off bleeding veins.
- Medications to slow blood flow into the portal vein. A drug called octreotide (Sandostatin) is often used with endoscopic therapy to slow the flow of blood from internal organs to the portal vein. The drug is usually continued for five days after a bleeding episode.
- Diverting blood flow away from the portal vein. Your doctor might recommend a procedure called transjugular intrahepatic portosystemic shunt (TIPS) to place a shunt. The shunt is a small tube that is placed between the portal vein and the hepatic vein, which carries blood from your liver to your heart. The shunt reduces pressure in the portal vein and often stops bleeding from esophageal varices. But transjugular intrahepatic portosystemic shunt (TIPS) can cause serious complications, including liver failure and mental confusion, which can develop when toxins that the liver normally would filter are passed through the shunt directly into the bloodstream. TIPS is mainly used when all other treatments have failed or as a temporary measure in people awaiting a liver transplant.
- Restoring blood volume. You might be given a transfusion to replace lost blood and clotting factor to stop bleeding.
- Preventing infection. There is an increased risk of infection with bleeding, so you’ll likely be given an antibiotic to prevent infection.
- Replacing the diseased liver with a healthy one. Liver transplant is an option for people with severe liver disease or those who experience recurrent bleeding of esophageal varices. Although liver transplantation is often successful, the number of people awaiting transplants far outnumbers the available organs.
Rebleeding
Bleeding will recur in most people who have bleeding from esophageal varices. Beta blockers and esophageal band ligation are the recommended treatments to help prevent rebleeding.
- Screening for Varices and Prevention of Bleeding. https://www.hepatitisc.uw.edu/go/management-cirrhosis-related-complications/varices-screening-prevention-bleeding/core-concept/all[↩][↩][↩][↩][↩][↩][↩]
- Portal hypertension and variceal hemorrhage. Toubia N, Sanyal AJ. Med Clin North Am. 2008 May; 92(3):551-74, viii. https://www.ncbi.nlm.nih.gov/pubmed/18387376/[↩][↩]
- Current management of the complications of portal hypertension: variceal bleeding and ascites. Dib N, Oberti F, Calès P. CMAJ. 2006 May 9; 174(10):1433-43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1455434/[↩]
- Kasper D, Braunwald E, Fauci A, Hauser S, Longo D, Jameson J. Harrison’s principles of internal medicine. 16th ed. New York: McGraw-Hill; 2005.[↩]
- Groszmann RJ, Garcia-Tsao G, Bosch J, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005;353:2254-61.[↩]
- Tursi T. Use of ß-blocker therapy to prevent primary bleeding of esophageal varices. Journal of the American Academy of Nurse Practitioners. 2010;22(12):640-647. doi:10.1111/j.1745-7599.2010.00567.x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3017746/[↩][↩]
- Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38.[↩][↩]
- de Franchis R; Baveno V Faculty. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53:762-8.[↩][↩]
- Gluud LL, Krag A. Banding ligation versus beta-blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012;8:CD004544.[↩]
- Li T, Ke W, Sun P, et al. Carvedilol for portal hypertension in cirrhosis: systematic review with meta-analysis. BMJ Open. 2016;6:e010902.[↩]
- Ryan BM, Stockbrugger RW, Ryan JM. A pathophysiologic, gastroenterologic, and radiologic approach to the management of gastric varices. Gastroenterology. 2004;126:1175-89.[↩]
- Tan PC, Hou MC, Lin HC, Liu TT, Lee FY, Chang FY, Lee SD. A randomized trial of endoscopic treatment of acute gastric variceal hemorrhage: N-butyl-2-cyanoacrylate injection versus band ligation. Hepatology. 2006;43:690-7.[↩]
- Chau TN, Patch D, Chan YW, Nagral A, Dick R, Burroughs AK. “Salvage” transjugular intrahepatic portosystemic shunts: gastric fundal compared with esophageal variceal bleeding. Gastroenterology. 1998;114:981-7.[↩]
- Ioannou G, Douse J, Rockey DC. Terlipressin for acute variceal hemorrhage. Cochrane Database Syst Rev 2003;(1):CD002147.[↩]
- Bañares R, Albillos A, Rincón D, et al. Endoscopic treatment versus endoscopic plus pharmacologic treatment for acute variceal bleeding: a meta-analysis. Hepatology. 2002;35:609-15.[↩]
- Fernández J, Ruiz del Arbol L, Gomez C, et al. Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Gastroenterology. 2006;131:1049-56.[↩]
- García-Pagán JC, Caca K, Bureau C, et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362:2370-9.[↩]
- Gonzalez R, Zamora J, Gomez-Camarero J, Molinero LM, Bañares R, Albillos A. Meta-analysis: Combination endoscopic and drug therapy to prevent variceal rebleeding in cirrhosis. Ann Intern Med. 2008;149:109-22.[↩]
- Pathophysiology of portal hypertension. Cichoz-Lach H, Celiński K, Słomka M, Kasztelan-Szczerbińska B. J Physiol Pharmacol. 2008 Aug; 59 Suppl 2():231-8. https://www.ncbi.nlm.nih.gov/pubmed/18812641/[↩]