Contents
Femoral artery
The femoral artery is the continuation of the external iliac artery and begins as the external iliac artery passes under the inguinal ligament to enter the femoral triangle on the anterior aspect of the upper thigh.
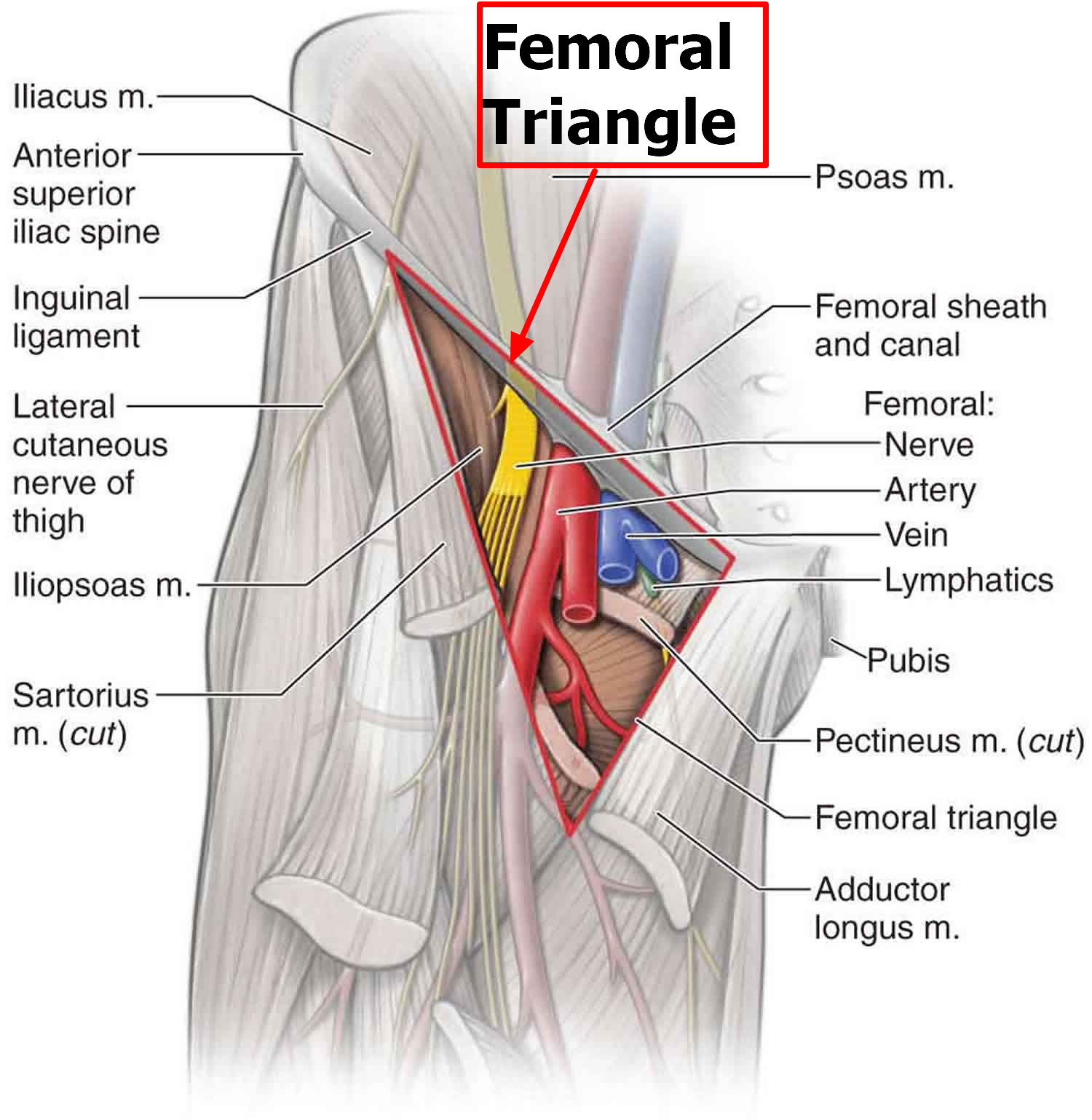
The femoral triangle (Figure 3). The base is formed superiorly by the inguinal ligament, medially by the lateral border of the adductor longus muscle, and laterally by the medial border of the sartorius muscle. The apex is formed by the crossing of the adductor longus by the sartorius muscle. The contents of the femoral triangle, from lateral to medial, are the femoral nerve and its branches, the femoral artery and several of its branches, the femoral vein and its proximal tributaries, and the deep inguinal lymph nodes.
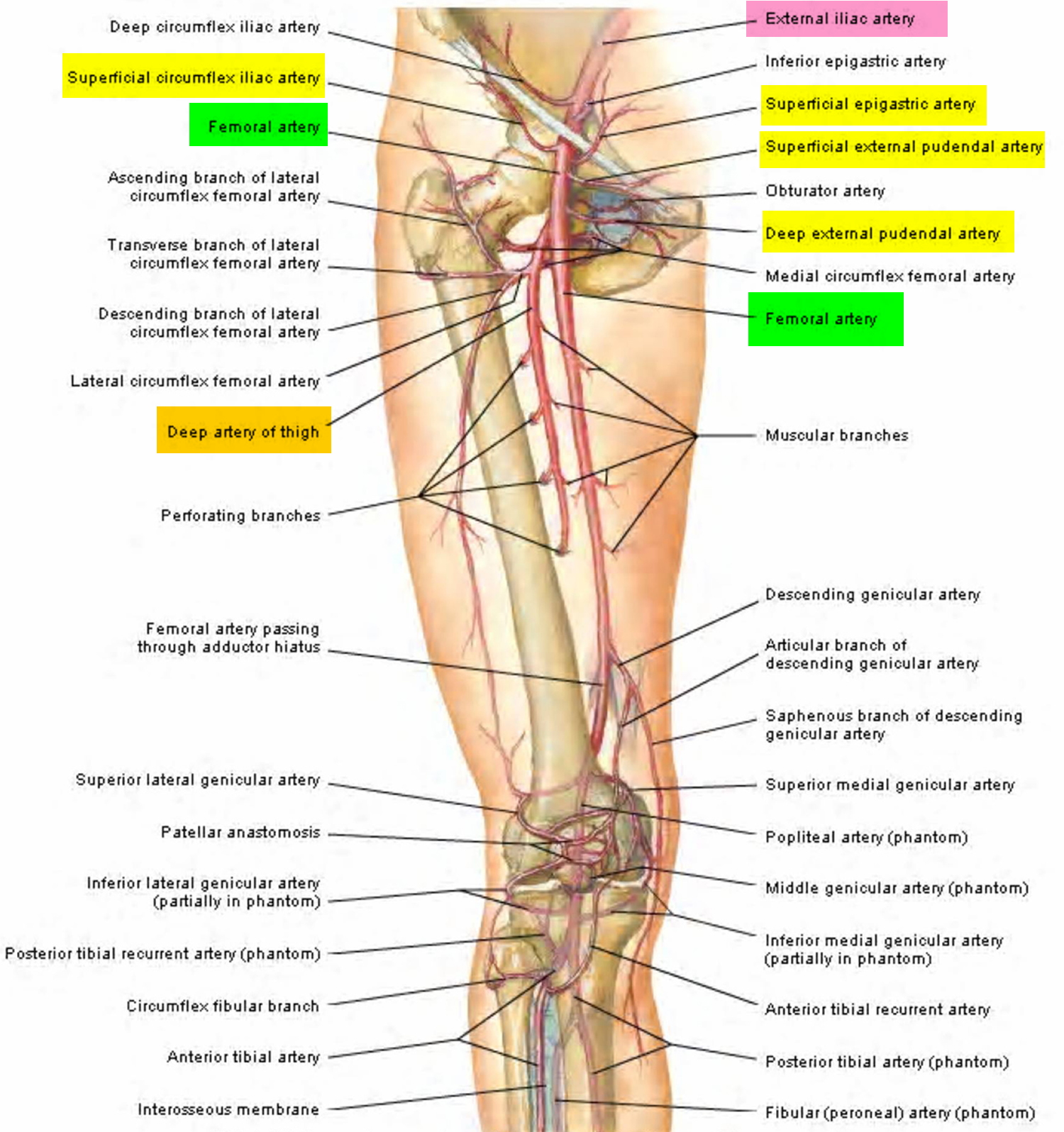
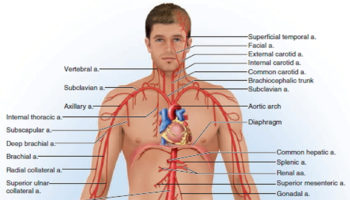
The femoral artery is palpable in the femoral triangle just inferior to the inguinal ligament midway between the anterior superior iliac spine and the pubic symphysis. The femoral artery is easily accessible within the femoral triangle and is the site for insertion of catheters that may extend into the aorta and ultimately into the coronary vessels of the heart. Such catheters are utilized during cardiac catheterization, coronary angiography, and other procedures involving the heart. A cluster of four small branches – superficial epigastric artery, superficial circumflex iliac artery, superficial external pudendal artery, and deep external pudendal artery – originate from the femoral artery in the femoral triangle and supply cutaneous regions of the upper thigh, lower abdomen, and perineum.
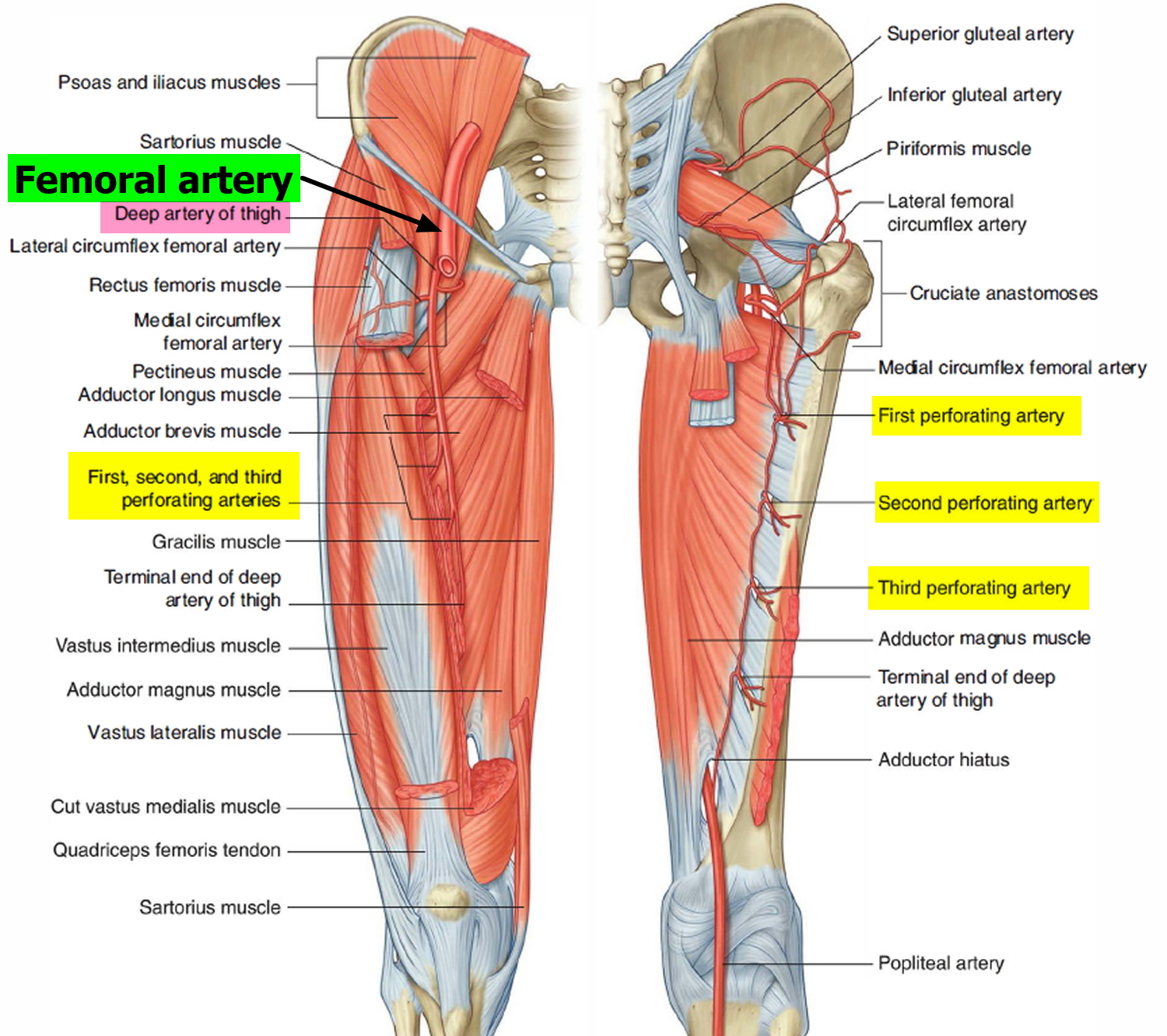
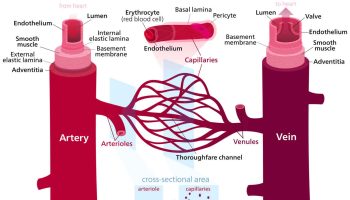
The largest branch of the femoral artery in the thigh is the deep artery of the thigh (profunda femoris artery), which originates from the lateral side of the femoral artery in the femoral triangle and is the major source of blood supply to the thigh (Figure 1). The deep artery of the thigh immediately passes posteriorly between the pectineus and adductor longus muscles and then between the adductor longus and adductor brevis muscles, and then travels inferiorly between the adductor longus and adductor magnus , eventually penetrating through the adductor magnus to connect with branches of the popliteal artery behind the knee. The deep artery of the thigh has lateral and medial circumflex femoral branches and three perforating branches.
The femoral artery passes vertically through the femoral triangle and then continues down the thigh in the adductor canal. It leaves the canal by passing through the adductor hiatus in the adductor magnus muscle and becomes the popliteal artery behind the knee. Branches of this artery supply blood to the knee joint and to certain muscles in the thigh and calf. The popliteal artery diverges into the anterior and posterior tibial arteries. The anterior tibial artery passes downward between the tibia and fibula, giving off branches to the skin and muscles in the anterior and lateral regions of the leg. This vessel continues into the foot as the dorsalis pedis artery (dorsal pedis artery), which supplies blood to the foot. The posterior tibial artery, the larger of the two popliteal branches, descends beneath the calf muscles, giving off branches to the skin, muscles, and other tissues of the leg along the way to the foot.
Figure 1. Femoral artery
Figure 2. Femoral Artery and Deep Artery of the Thigh (and its perforating branches)
Figure 3. Femoral Triangle
Femoral artery bypass
Peripheral artery bypass is surgery to reroute the blood supply around a blocked artery in one of your legs. Fatty deposits can build up inside the arteries and block them 1.
Peripheral arterial disease happens when there is a narrowing of the blood vessels outside of your heart 2. The cause of PAD is atherosclerosis. This happens when plaque builds up on the walls of the arteries that supply blood to the arms and legs. Plaque is a substance made up of fat and cholesterol. It causes the arteries to narrow or become blocked. This can reduce or stop blood flow, usually to the legs. If severe enough, blocked blood flow can cause tissue death and can sometimes lead to amputation of the foot or leg.
The main risk factor for peripheral arterial disease is smoking. Other risk factors include older age and diseases like diabetes, high blood cholesterol, high blood pressure, heart disease, and stroke.
Many people who have peripheral arterial disease don’t have any symptoms. If you have symptoms, they may include:
- Pain, numbness, achiness, or heaviness in the leg muscles. This happens when walking or climbing stairs.
- Weak or absent pulses in the legs or feet
- Sores or wounds on the toes, feet, or legs that heal slowly, poorly, or not at all
- A pale or bluish color to the skin
- A lower temperature in one leg than the other leg
- Poor nail growth on the toes and decreased hair growth on the legs
- Erectile dysfunction, especially among men who have diabetes
Peripheral arterial disease can increase your risk of heart attack, stroke, and transient ischemic attack.
Doctors diagnose peripheral arterial disease with a physical exam and heart and imaging tests. Treatments include lifestyle changes, medicines, and sometimes surgery. Lifestyle changes include dietary changes, exercise, and efforts to lower high cholesterol levels and high blood pressure.
Treatment of Peripheral arterial disease
Alternative Names:
- Femoropopliteal bypass;
- Femoral popliteal bypass;
- Aorta-bifemoral bypass;
- Axillo-bifemoral bypass;
- Ilio-bifemoral bypass;
- Femoral-femoral bypass.
A graft is used to replace or bypass the blocked part of the artery. The graft may be a plastic tube, or it may be a blood vessel (vein) taken from your body (most often the opposite leg) during the same surgery.
Peripheral artery bypass surgery can be done in one or more of the following blood vessels:
- Aorta (the main artery that comes from your heart)
- Artery in your hip
- Artery in your thigh
- Artery behind your knee
- Artery in your lower leg
- Artery in your armpit
During bypass surgery of any artery:
- You will receive medicine (anesthesia) so that you do not feel pain. The kind of anesthesia you receive will depend on what artery is being treated.
- Your surgeon will make a cut over the part of the artery that is blocked.
- After moving skin and tissue out of the way, the surgeon will place clamps at each end of the blocked section of artery. The graft is then sewn in place.
- The surgeon will make sure you have good blood flow in your extremity. Then your cut will be closed. You may have an x-ray called an arteriogram to make sure that the graft is working.
If you are having bypass surgery to treat your aorta and iliac artery or your aorta and both femoral arteries (aortobifemoral):
You will probably have general anesthesia. This will make you unconscious and unable to feel pain. Or, you may have epidural or spinal anesthesia instead. The doctor will inject your spine with medicine to make you numb from your waist down.
Your surgeon will make a surgical cut in the middle of the abdomen to reach the aorta and iliac arteries.
If you are having bypass surgery to treat your lower leg (femoral popliteal):
- You may have general anesthesia. You will be unconscious and unable to feel pain. You may instead have an epidural or spinal anesthesia. The doctor will inject your spine with medicine to make you numb from your waist down. Some people have local anesthesia and a medicine to relax them. Local anesthesia numbs just the area being worked on.
- Your surgeon will make a cut in your leg between your groin and knee. It will be near the blockage in your artery.
Why the Procedure is Performed
Symptoms of a blocked peripheral artery are pain, achiness, or heaviness in your leg that starts or gets worse when you walk.
You may not need bypass surgery if these problems happen only when you walk and then go away when you rest. You may not need this surgery if you can still do most of your everyday activities. Your doctor can try medicines and other treatments first.
Reasons for having arterial bypass surgery of the leg are:
- You have symptoms that keep you from doing your everyday tasks.
- Your symptoms do not get better with other treatment.
- You have skin ulcers (sores) or wounds on your leg that do not heal.
- You have an infection or gangrene in your leg.
- You have pain in your leg from your narrowed arteries, even when you are resting or at night.
Before having surgery, your doctor will do special tests to see the extent of the blockage.
Risks of Artery Bypass Surgery
Risks for any anesthesia and surgery are:
- Allergic reactions to medicines
- Breathing problems
- Blood clots in the legs that may travel to the lungs
- Breathing problems
- Heart attack or stroke
Risks for this surgery are:
- Bypass does not work
- Damage to a nerve that causes pain or numbness in your leg
- Damage to nearby organs in the body
- Damage to the bowel during aortic surgery
- Excess bleeding
- Infection in the surgical cut
- Injury to nearby nerves
- Sexual problems caused by damage to a nerve during aortofemoral or aortoiliac bypass surgery
- Surgical cut that opens up
- Need for a second bypass surgery or a leg amputation
- Heart attack
- Death
Before the Procedure
You will have a physical exam and many medical tests.
- Most people need to get their heart and lungs checked before they have peripheral artery bypass.
- If you have diabetes, you will need to see your health care provider to have it checked.
Always tell your provider what medicines you are taking, even drugs, supplements, or herbs you bought without a prescription.
During the 2 weeks before your surgery:
- You may be asked to stop taking drugs that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), clopidogrel (Plavix), naprosyn (Aleve, Naproxen), and other similar drugs.
- Ask your provider which drugs you should still take on the day of your surgery.
- If you smoke, you need to stop. Ask your provider for help.
- Always let your provider know about any cold, flu, fever, herpes breakout, or other illness you may have before your surgery.
DO NOT drink anything after midnight the night before your surgery, including water.
On the day of your surgery:
- Take the medicines your provider told you to take with a small sip of water.
- Your provider will tell you when to arrive at the hospital.
After the Procedure
Right after surgery, you will go to the recovery room, where nurses will watch you closely. After that you will go either to the intensive care unit (ICU) or a regular hospital room.
- You may need to spend 1 or 2 days in bed if the surgery involves the large artery in your abdomen called the aorta.
- Most people stay in the hospital for 4 to 7 days.
- After femoral popliteal bypass, you will spend less time or no time in the ICU.
When your provider says it is ok, you will be allowed to get out of bed. You will slowly increase how far you can walk. When you are sitting in a chair, keep your legs raised on a stool or another chair.
Your pulses will be checked regularly after your surgery. The strength of your pulse will show how well your new bypass graft is working. While you are in the hospital, tell your provider right away if the leg that had surgery feels cool, looks pale or pink, feels numb, or if you have any other new symptoms.
You will receive pain medicine if you need it.
Outlook (Prognosis) of Artery Bypass Surgery
Bypass surgery improves blood flow in the arteries for most people. You may not have symptoms anymore, even when you walk. If you still have symptoms, you should be able to walk much farther before they start.
If you have blockages in many arteries, your symptoms may not improve as much. The prognosis is better if other medical conditions such as diabetes are well controlled. If you smoke, it is very important to quit.