Contents
What is superior vena cava
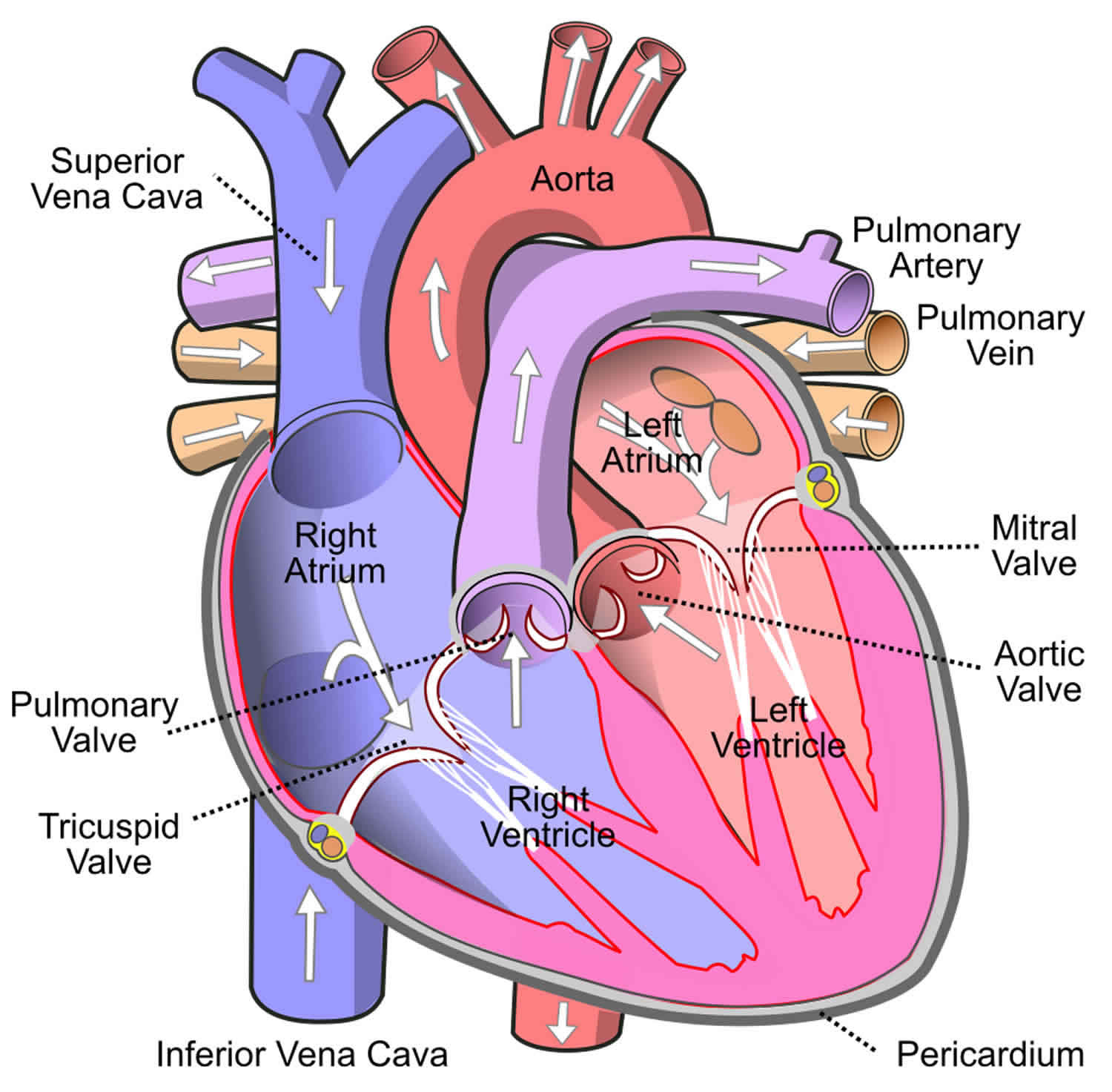
Superior vena cava is formed by the junction of the left and right innominate (brachiocephalic) veins and its function is to return deoxygenated blood from the head, neck, upper extremities and torso back to the right atrium of the heart. Blood coming from body regions superior to the diaphragm (excluding the heart wall) enters the right atrium via the superior vena cava. The superior vena cava is a large-diameter (24 mm), yet short, vein that receives venous return from the upper half of the body, above the diaphragm. Venous return from the lower half, below the diaphragm, flows through the inferior vena cava. The superior vena cava is located in the anterior right superior mediastinum. It is the typical site of central venous access via a central venous catheter or a peripherally inserted central catheter.
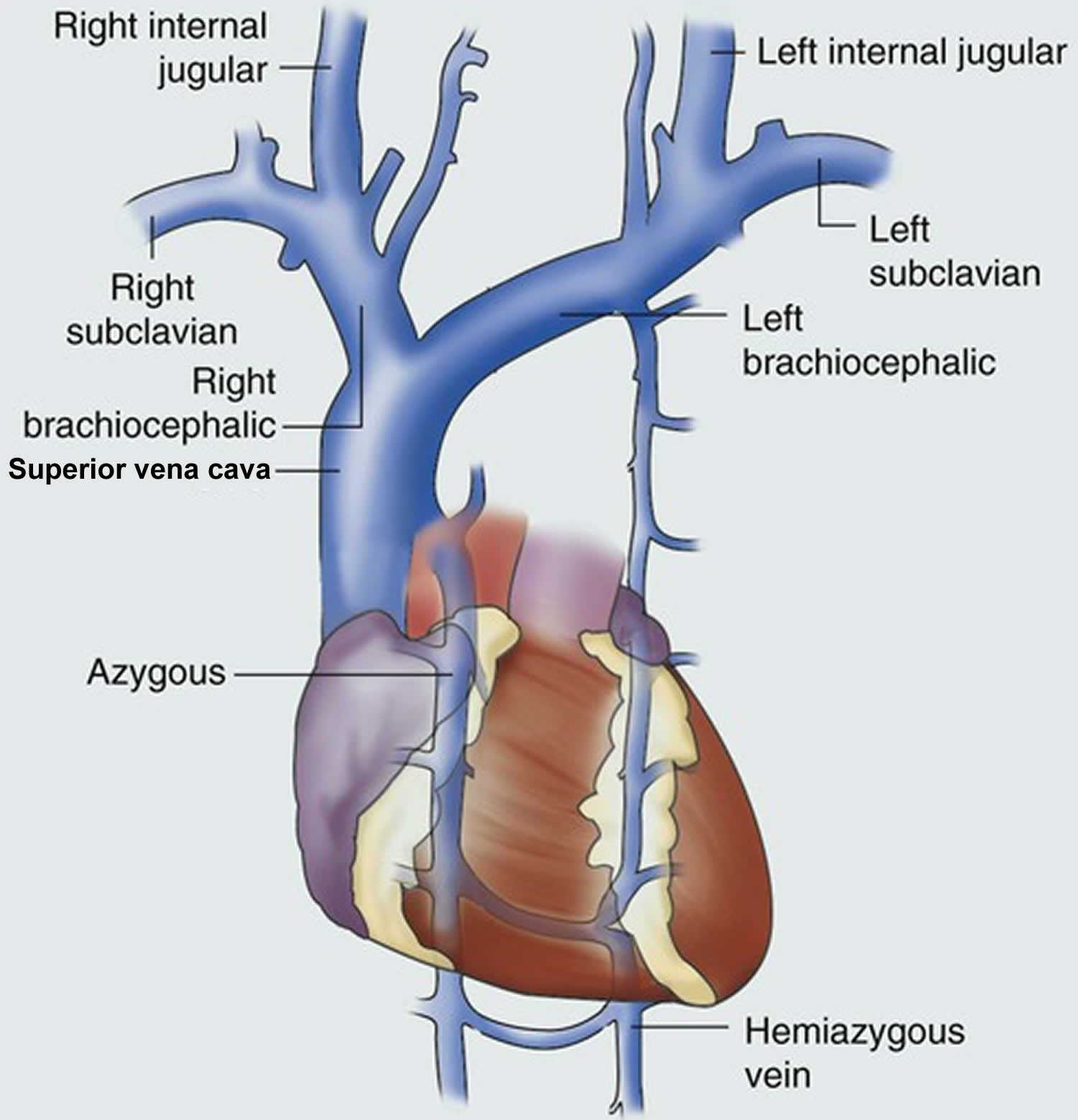
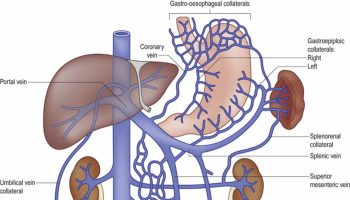
Figure 1. Superior vena cava
Superior vena cava anatomy
Superior vena cava is formed by the left and right brachiocephalic veins (also referred to as the innominate veins), which also receive blood from the upper limbs, eyes and neck, behind the lower border of the first right costal cartilage. Superior vena cava passes vertically downwards behind first intercostal space and receives azygos vein just before it pierces the fibrous pericardium opposite right second costal cartilage and its lower part is intrapericardial. And then, it ends in the upper and posterior part of the sinus venarum of the right atrium, at the upper right front portion of the heart.
No valve divides the superior vena cava from the right atrium. As a result, the (right) atrial and (right) ventricular contractions are conducted up into the internal jugular vein and, through the sternocleidomastoid muscle, can be seen as the jugular venous pressure.
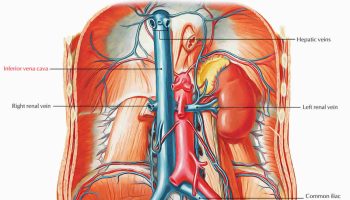
Figure 2. Superior vena cava anatomy
Persistent left superior vena cava
In persistent left superior vena cava, the left brachiocephalic vein does not develop fully and the left upper limb and head & neck drain into the right atrium via the coronary sinus. Persistent left superior vena cava is the most common variation of the thoracic venous system, is prevalent in 0.3% of the population and an embryologic remnant that results from a failure to involute.
The persistent left superior vena cava variation, in isolation, is considered benign, but is very frequently associated with cardiac abnormalities (e.g. ventricular septal defect, atrioventricular septal defect) that have a significant mortality and morbidity. Persistent left superior vena cava is more frequent in patients with congenital heart defects.
What does the superior vena cava do?
Superior vena cava function is to return deoxygenated blood from the head, neck, upper extremities and torso back to the right atrium of the heart.
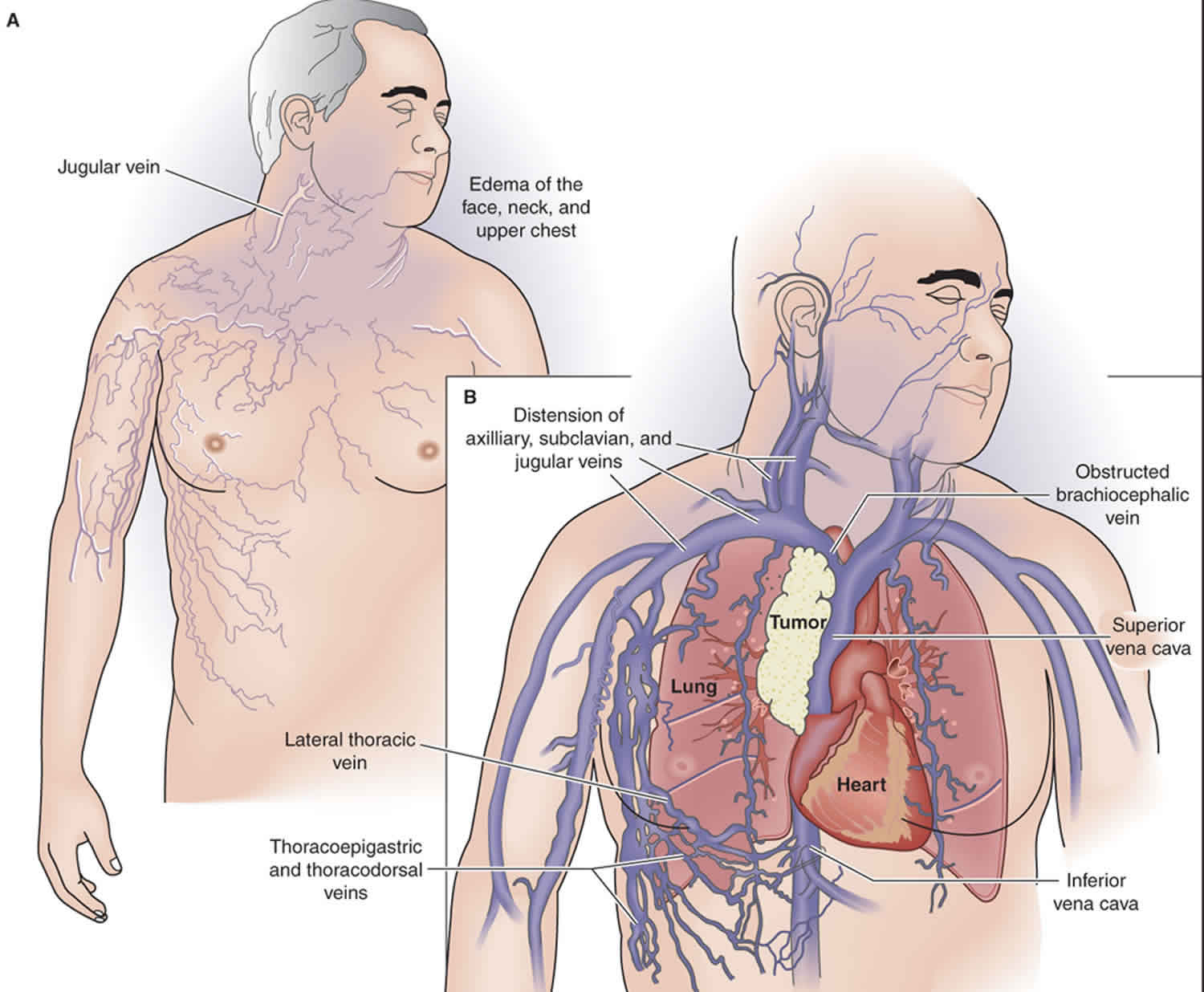
Superior vena cava syndrome
Superior vena cava syndrome (SVCS) also called superior vena cava obstruction (SVCO) is a collection of clinical signs and symptoms resulting from either partial or complete obstruction of blood flow through the superior vena cava (SVC) preventing blood from flowing normally from your head, neck, arms, and chest to your heart 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18. The superior vena cava syndrome (SVCS) is a medical emergency and is most often due to a cancer in your chest. Once diagnosed, the condition needs to be treated. Otherwise, superior vena cava syndrome (SVCS) can lead to brain swelling (cerebral edema) and upper airway fluid build-up (blocked airway). Since the superior vena cava (SVC) traverses the superior mediastinum, it can be obstructed from any number of causes. Superior vena cava obstruction is most commonly a result of blood clot (thrombus) or tumor infiltration of the superior vena cava wall. Today, superior vena cava syndrome (SVCS) is most commonly seen secondary to cancer although there has been a more recent rise in benign (non-cancerous) causes 19. The resulting venous congestion produces a clinical scenario relating to increased upper body venous pressures. The most common signs and symptoms of superior vena cava syndrome (SVCS) include swelling in your face, neck, arms, and upper body, shortness of breath (dyspnea), coughing, bluish skin and dilated chest vein collaterals 20. Moreover, in most cases of superior vena cava syndrome (SVCS), the blood flow through the superior vena cava (SVC) slows down over a few days or even weeks, and the symptoms cause the person to get medical help. In very rare cases, superior vena cava syndrome (SVCS) happens fast and may lead to blockage of the superior vena cava (SVC). This may cause rare but serious upper respiratory problems from fluid build-up (edema). This can make it hard for a person to breathe. Superior vena cava syndrome (SVCS) may be serious when it occurs in adults. But it can be life-threatening in children.
Common causes of superior vena cava syndrome include 21, 22, 23, 24, 25, 26, 27:
- Cancer (>85%)
- Benign (non-cancerous) (3% to 15%)
- Indwelling catheters
- Thymoma
- Cystic hygroma
- Tuberculosis
- Histoplasmosis
- Thyroid goiter
- Aortic aneurysm
While lung cancer is the most common cause of superior vena cava syndrome or superior vena cava obstruction, other causes include non-Hodgkin lymphoma (NHL), aortic aneurysms, mediastinal fibrosis (a rare disease that causes the middle of your chest to become thickened with fibrous or scar tissue), pericarditis, a blood clot that forms in the vein (thrombosis) as a result of venous catheters and infections like histoplasmosis 28. Superior vena cava syndrome (SVCS) is often seen in middle-aged individuals. Radiation therapy is often used as the initial treatment when the diagnosis is uncertain. In the past, surgery was done to reconstruct the superior vena cava (SVC) but today percutaneous angioplasty and stenting offer a better option. With stenting, symptomatic relief is obtained within 24 to 48 hours 29.
An estimated 15,000 cases of superior vena cava syndrome (SVCS) occur each year in the United States, with studies pointing to increasing frequency due to the concomitant rise in the use of semipermanent intravascular catheters 19. The incidence of superior vena cava syndrome reported in the literature range from 1 in 650 to 1 in 3100 patients 19.
Treatment of superior vena cava syndrome (SVCS) depends on the cause of the blockage, the seriousness of your symptoms, and your overall health and preferences. The goal of superior vena cava syndrome (SVCS) treatment is to relieve the blockage. Diuretics (water pills) or steroids (anti-inflammtory drugs) may be used to temporarily relieve swelling. Other treatment options may include radiation or chemotherapy to shrink the tumor, or surgery to remove the tumors. Surgery to bypass the obstruction is rarely performed. Placement of a stent (tube placed inside a blood vessel) to open up the superior vena cava may be performed. If there’s a blood clot (thrombus) in the superior vena cava (SVC) that’s linked to an implanted medical device, medicines will be used to dissolve the clot and the device might be taken out.
If there’s no clear cause based on the person’s medical history, tests will be done to look for the cause of superior vena cava syndrome (SVCS). For instance, if scans show a tumor in your chest that’s pressing on the superior vena cava (SVC) and lung cancer is suspected, a sputum test and a biopsy might be done. The results can then help your doctor decide on the best treatment.
Treatment shouldn’t start until your doctor finds the cause of the superior vena cava (SVC) blockage. Unless your airway or windpipe (trachea) is blocked or swelling in your brain, or other symptoms are causing problems, waiting to start treatment is usually not a problem. Superior vena cava syndrome (SVCS) is seldom a life-threatening emergency. This means there’s time to make a definite diagnosis before treatment is started.
Key points about superior vena cava syndrome (SVCS) 30, 31:
- Superior vena cava syndrome (SVCS) is a problem caused by partly blocked blood flow through the superior vena cava (SVC). This is the vein that carries blood away from your head, neck, arms, and upper chest to your heart.
- In most cases, the superior vena cava (SVC) blockage develops slowly. In very rare cases, superior vena cava syndrome (SVCS) happens fast and blocks your airway so you can’t breathe.
- Superior vena cava syndrome (SVCS) is most often seen in people who have cancer, mostly lung cancer or non-Hodgkin lymphoma. Other rare causes include infection or a blood clot in the vein caused by an implanted medical device.
- Superior vena cava syndrome (SVCS) is serious when it occurs in adults. But it can be life-threatening in children.
- Superior vena cava syndrome (SVCS) symptoms include trouble breathing, coughing, and swelling of the face, neck, upper body, and arms.
- Treatment options for superior vena cava syndrome (SVCS) caused by cancer may include radiation therapy, chemotherapy, thrombolysis, and stent placement.
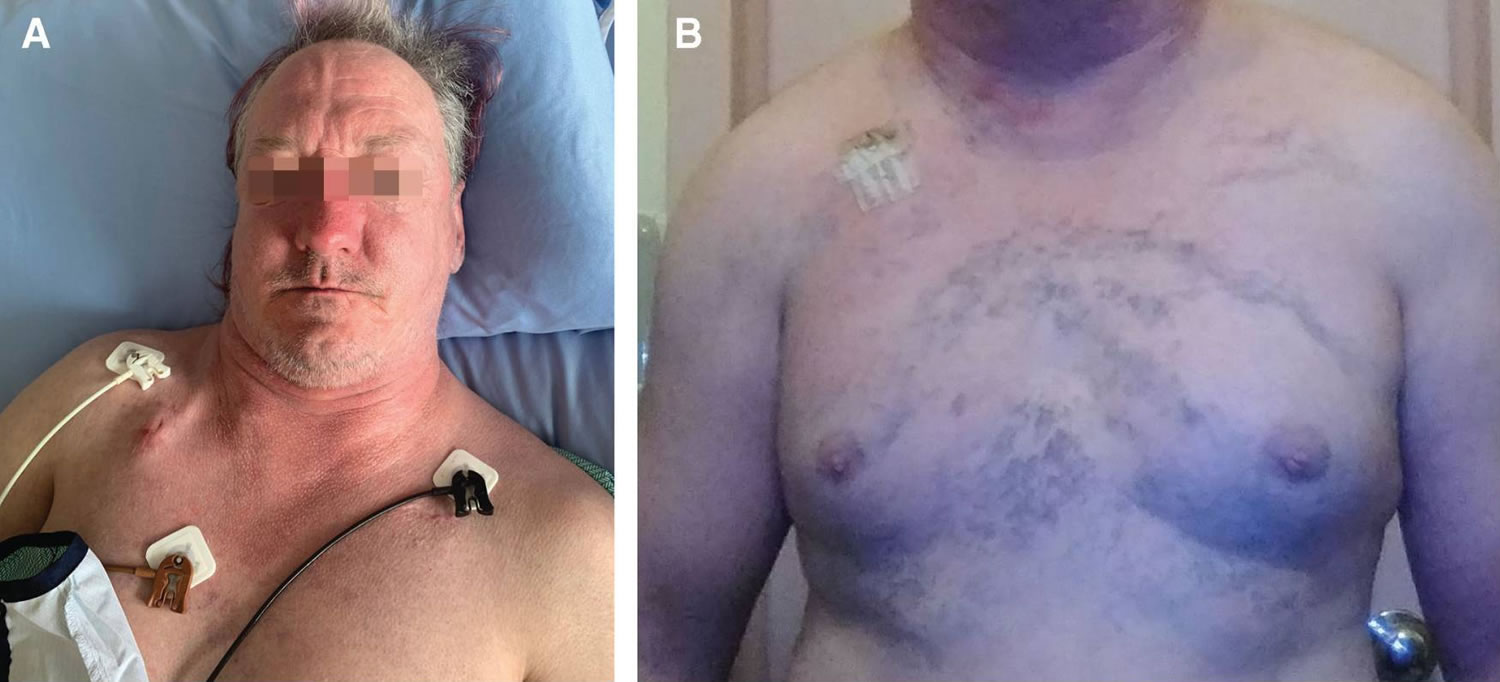
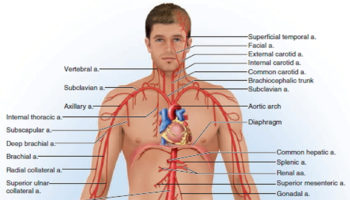
Figure 3. Superior vena cava syndrome
Footnotes: Photographs of the head and upper chest of a 53-year-old man with catheter-associated superior vena cava syndrome (SVCS), showing (A) facial and neck plethora (a symptom of increased blood flow to the face that causes swelling and puffiness) and (B) a prominent superficial venous pattern on the chest.
[Source 1 ]Who is at risk for superior vena cava syndrome?
Superior vena cava syndrome (SVCS) is most often seen in people with cancer. Superior vena cava syndrome (SVCS) is most common in people with lung cancer or non-Hodgkin lymphoma. Rarely, superior vena cava syndrome (SVCS) is associated to other causes such as infection or a blood clot in the superior vena cava (SVC) caused by an implanted medical device. The device may be a central catheter, dialysis catheter, or pacemaker wire.
Superior vena cava syndrome causes
Today, the majority of superior vena cava syndromes are the result of mediastinal malignancies, primary among which is small cell bronchogenic carcinoma 15. The second most commonly associated malignancy is non-Hodgkins lymphoma (NHL), followed by metastatic tumors 15. In addition, benign or nonmalignant causes of superior vena cava syndrome now comprise at least 40% of cases 15. Iatrogenic thrombus formation or superior vena cava stenosis is a growing cause due to pacemaker wires and semipermanent intravascular catheters used for hemodialysis, long term antibiotics, or chemotherapy 32, 33.
Other types of cancer that can lead to superior vena cava syndrome include:
- Breast cancer
- Lymphoma
- Metastatic lung cancer (lung cancer that spreads)
- Testicular cancer
- Thyroid cancer
- Thymus tumor
Superior vena cava obstruction can also be caused by noncancerous conditions that cause scarring. These conditions include:
- Histoplasmosis (a type of fungal infection)
- Inflammation of a vein (thrombophlebitis)
- Lung infections (such as tuberculosis)
Other causes of superior vena cava obstruction include:
- Aortic aneurysm (a widening of the artery that leaves the heart)
- Blood clots in the superior vena cava
- Constrictive pericarditis (tightening of the thin lining of the heart)
- Effects of radiation therapy for certain medical conditions
- Enlargement of the thyroid gland (goiter)
Catheters placed in the large veins of the upper arm and neck may cause blood clots in the superior vena cava. A blood clot (thrombosis) that blocks the vein is referred to as deep vein thrombosis (DVT).
The superior vena cava is part of the low-pressure venous system containing thin walls susceptible to damage by a variety of pathologic mechanisms. These mechanisms can be divided into three categories which are compromised vessel anatomy, impaired venous flow, and diminished vessel wall integrity. These mechanisms often coexist in patients presenting with superior vena cava syndrome. Extrinsic compression and obstruction of the superior vena cava by a mass in the mediastinum is the most common cause of superior vena cava syndrome. Most often this is associated with malignancy, however there are a variety of nonmalignant masses as well as dilation of the overlying aorta that can cause compression. A growing proportion of superior vena cava syndromes are now associated with occlusive venous thrombus formation that compromises venous flow back to the heart. The increasing use of indwelling intravascular devices such as catheters as well as pacemakers and implantable cardioverter defibrillator (ICD) leads have played a major role in this growth. Resultant venous wall inflammation, fibrosis, and eventual thrombus leads to stenosis of the vessel itself 34.
Superior vena cava syndrome symptoms
Symptoms occur when something blocks the superior vena cava (SVC) blood from flowing back to your heart. Superior vena cava syndrome (SVCS) symptoms may begin suddenly or gradually, and may worsen when you bend over or lie down.
Early signs of superior vena cava syndrome (SVCS) include 35, 15:
- Swelling or puffiness around your eyes or puffy eyes (also known as periorbital edema)
- Swelling of your face (also known as facial edema)
- Swelling of the whites of your eyes (also known as chemosis)
The swelling will most likely be worse in the early morning hours and go away by mid-morning. Symptoms often get worse when you bend forward or lie down.
The most common superior vena cava syndrome (SVCS) symptoms are shortness of breath (dyspnea), coughing and swelling of your face, neck, upper body, and arms.
Other possible superior vena cava syndrome (SVCS) symptoms include:
- Decreased alertness
- Dizziness, fainting
- Headache
- Lightheadedness
- Reddish face or cheeks
- Swelling of neck or chest veins
- Reddish palms
- Reddish mucous membranes (inside the nose, mouth, and other places)
- Redness changing to blueness later
- Sensation of head or ear fullness
- Vision changes
- Hoarse voice
- Rapid breathing
- Coughing up blood
- Trouble swallowing
In rare superior vena cava syndrome (SVCS) cases, symptoms may include:
- Lips and skin look blue due to a lack of oxygen in the blood This is called cyanosis.
- A group of symptoms called Horner’s syndrome, which is a constricted pupil (miosis), drooping of your upper eyelid (ptosis), and decrease in sweating or lack of sweating on one side of your face (anhidrosis). Horner’s syndrome is caused by damage to the sympathetic nerves that connect your brainstem to your eyes and face. These nerves control involuntary functions, such as sweating (perspiration) and the dilation and constriction of the pupils of your eyes. The underlying causes of nerve damage can vary widely, from a middle ear infection to a carotid artery dissection or apical chest tumor.
How fast the superior vena cava blockage forms and where it is are linked to the seriousness of the superior vena cava syndrome. For instance:
- The faster the superior vena cava (SVC) is blocked, the more severe the symptoms. This is because the other veins don’t have time to widen and adjust to the change in blood flow.
- If the blockage forms above where the superior vena cava (SVC) and inferior vena cava (IVC) meet, symptoms might be harder to notice. The inferior vena cava (IVC) carries blood from the lower part of your body back to your heart. This is because the veins can swell more easily and handle the increased blood flow.
- If the blockage occurs below where the superior vena cava (SVC) and inferior vena cava (IVC) meet, more symptoms are seen. This is because the blood will go back to your heart through the inferior vena cava (IVC) and other veins in the upper belly (abdomen). More pressure is needed to do this.
Superior vena cava syndrome possible complications
If not watched closely or treated, superior vena cava syndrome (SVCS) can lead to serious problems, such as:
- Your throat could become blocked due to swelling of your larynx and pharynx, which can block your airways.
- Increased pressure may develop in your brain (brain swelling or cerebral edema), leading to changed levels of consciousness, nausea, vomiting, or vision changes.
- Blood clots that can break loose and travel to your lungs or brain.
Superior vena cava syndrome diagnosis
The diagnosis of superior vena cava syndrome (SVCS) is made largely based on a patient’s history and physical findings, which often develop over a period of days to weeks. This insidious onset is a result of a collateral vascular network that exists to divert blood to the lower body where it is then returned to the heart through the inferior vena cava (IVC), azygous vein, and the intercostals. The clinical findings in superior vena cava syndrome (SVCS) are closely linked to venous congestion and the resultant elevation in venous pressures seen in the upper body. A careful physical examination is often sufficient to rule out a cardiogenic origin to the patient’s symptoms.
The most common presenting symptoms of superior vena cava syndrome (SVCS) are face, neck swelling, distended neck veins, cough, shortness of breath (dyspnea), shortness of breath that occurs when lying down (orthopnea), upper extremity swelling, distended chest vein collaterals, and redness and swelling of the conjunctiva in the eye (conjunctival suffusion). Other less common symptoms of superior vena cava syndrome (SVCS) include stridor (a harsh vibrating noise when breathing caused by obstruction of the windpipe or larynx), hoarseness, difficulty swallowing (dysphagia), pleural effusion (a buildup of fluid in the pleural space [the cavity between the lungs and chest wall]), head plethora or facial plethora (a symptom of increased blood flow to your face that causes swelling and puffiness), headache, nausea, lightheadedness, fainting (syncope), changes in vision, altered mental status, upper body edema, cyanosis (a bluish discoloration of your skin due to poor circulation or inadequate oxygenation in your blood), papilledema (swelling of both optic discs in your eyes due to increased intracranial pressure), stupor (a state of near-unconsciousness), and coma (prolonged state of deep unconsciousness). Some rare but serious clinical consequences reported in superior vena cava syndrome include brain swelling (cerebral edema) and upper respiratory compromise secondary to edema of larynx and pharynx.
Investigation
If a doctor suspects superior vena cava syndrome (SVCS), tests to look for the type of blockage and where it is in the superior vena cava (SVC) will be needed to be sure. Patients with high clinical suspicion for superior vena cava syndrome (SVCS) should undergo imaging of the upper body and vasculature. If the windpipe (trachea) isn’t blocked and there’s no swelling in your brain, SVCS is seldom a life-threatening emergency. This means there’s time to make a definite diagnosis before treatment is started.
Any of these tests might be used:
- Chest X-ray
- CT scan of the chest
- X-ray imaging of the veins (venography)
- MRI
- Ultrasound
Ultrasound of the jugular, subclavian, and innominate veins can help to identify a blood clot (thrombus) within the vessel lumen. Radiographic imaging and MRI also play a critical role providing additional information as to the location, severity, and etiology of the superior vena cava obstruction. CT of the chest with the presence of collateral vessels is associated with a diagnostic sensitivity of 96% and a specificity of 92%. Venography is widely accepted as the gold standard for visualizing and diagnosing a venous obstruction. This modality should be used concomitantly with endovascular intervention for patients with a severe presentation of superior vena cava syndrome 36.
If lung cancer is suspected, a bronchoscopy may be done. During this procedure, a scope is used to view inside the airways and lungs.
Superior vena cava syndrome treatment
Following a clinical diagnosis, supportive therapy and medical management is commonly initiated. This involves elevation of the patient’s head as a simple maneuver with the goal of decreasing venous pressure. Further management is guided by the patient’s underlying superior vena cava syndrome cause. For patients with blood clot (thrombus) related to an indwelling intravascular device, removal should be considered along with anticoagulation therapy and catheter directed thrombolysis (breaking up blood clots). Multidisciplinary treatment planning for those with obstruction due to cancer is important as tumor type and staging can help to guide appropriate chemotherapy or radiation therapy. Open surgical repair through bypass grafting with spiral saphenous vein, femoral vein, polytetrafluoroethylene graft, or Dacron graft have traditionally been considered to overcome superior vena cava obstruction. However, this is now reserved for cases in which recanalization through endovascular repair is either not possible or has previously failed. With expanding treatment options for both benign and malignant etiology, endovascular therapy is now widely considered as the first-line treatment for superior vena cava syndrome. Less invasive endovascular management can offer patients immediate relief of symptoms. Acute or subacute thrombus can be managed with catheter based thrombolysis or thrombectomy prior to venoplasty and stent placement 37.
The following treatments can be used for cancer-related superior vena cava syndrome (SVCS):
- Radiation therapy. If the blockage of the superior vena cava is caused by a tumor that doesn’t respond or is slow to respond to chemotherapy such as non-small cell lung cancer, radiation therapy may be given. It can quickly shrink tumors and ease symptoms.
- Chemotherapy. This is the treatment of choice for chemo-sensitive tumors, such as lymphoma or small cell lung cancer. Many times, superior vena cava syndrome (SVCS) doesn’t change the treatment plan. Treating the cancer helps clear up the superior vena cava syndrome (SVCS).
- Thrombolysis (breaking up blood clots). Superior vena cava syndrome (SVCS) may happen when a blood clot (thrombus) forms in a partly blocked vein. People who have blood clots may need thrombolysis. This treatment uses medicine to dissolve or remove the blood clot.
- Stent placement. A stent may be used to open up the blocked vein. This can quickly ease superior vena cava syndrome (SVCS) symptoms. A stent is a small metal or plastic tube that’s put into the blocked part of the vein to allow blood to pass through. Some people may also need a blood-thinning medicine (anticoagulant) to help keep more blood clots from forming and blocking the stent.
- Medicines to ease symptoms. Sometimes other medicines can be used to ease symptoms while tests are done to look for the cause of superior vena cava syndrome (SVCS). Steroids can help reduce swelling and inflammation. Water pills (diuretic medicine) can help you pass more urine to get rid of extra fluid in your body.
Superior vena cava syndrome prognosis
The prognosis (outcome) of superior vena cava syndrome (SVCS) varies, depending on the underlying cause, the amount of blockage and your response to treatment. Superior vena cava obstruction caused by a tumor is a sign that the tumor has spread, and it indicates a poorer long-term outlook (porgnosis). For patients with a benign (non-cancerous) cause of superior vena cava syndrome (SVCS), the life expectancy is not changed, but for cancer cases, there is a significant drop in survival. Individuals who have features of brain and throat swelling can develop life-threatening symptoms and suddenly die. Patients with SVCS as a result of lung cancer usually live less than 24 months. For those who do not respond to radiation treatment, the survival is less than a year 38, 39, 40.
- Morriello F, Brown A, Granton J, Bonta M. Catheter-associated superior vena cava syndrome. CMAJ. 2023 Jan 17;195(2):E72-E75. doi: 10.1503/cmaj.220669[↩][↩]
- Reyhanoglu H, Ozcan K. Left brachiocephalic vein-right atrial bypass in superior vena cava syndrome. Cardiovasc J Afr. 2022 Jan-Feb 23;33(1):33-35. doi: 10.5830/CVJA-2021-025[↩]
- Zhao X, Wang K. Hemorrhagic pericardial tamponade in a hemodialysis patient with catheter-related superior vena cava syndrome: a case report. J Cardiothorac Surg. 2024 Mar 23;19(1):151. doi: 10.1186/s13019-024-02624-y[↩]
- Dragomir L, Marina V, Anghele M, Anghele AD. Clinical or Imaging Diagnosis of the Current Medical Practice for Superior Vena Cava Syndrome? Diagnostics (Basel). 2021 Nov 6;11(11):2058. doi: 10.3390/diagnostics11112058[↩]
- Wei S, Liu J, Li X, Song Z, Dong M, Zhao H, Zhao Q, Chen G, Chen J. A retrospective stenting study on superior vena cava syndrome caused by lung cancer. Thorac Cancer. 2020 Jul;11(7):1835-1839. doi: 10.1111/1759-7714.13461[↩]
- Guerrero-Macías S, Beltrán J, Buitrago R, Beltrán R, Carreño J, Carvajal-Fierro C. Outcomes in patients managed with endovascular stent for malignant superior vena cava syndrome. Surg Open Sci. 2023 Sep 17;16:16-21. doi: 10.1016/j.sopen.2023.09.001[↩]
- Ascione A, Martino G, Di Donato F, Casini B, Covello R, Ascani S. CIC-rearranged sarcoma presenting with superior vena cava syndrome: case report. Pathologica. 2023 Apr;115(2):97-100. doi: 10.32074/1591-951X-784[↩]
- Kanaji N, Watanabe N, Inoue T, Mizoguchi H, Sakamoto K, Komori Y, Kawada K, Kadowaki N. Superior vena cava syndrome induced by lung hyperinflation in chronic obstructive pulmonary disease: a case report. J Med Case Rep. 2023 Dec 1;17(1):497. doi: 10.1186/s13256-023-04256-7[↩]
- Patriarcheas V, Grammoustianou M, Ptohis N, Thanou I, Kostis M, Gkiozos I, Charpidou A, Trontzas I, Syrigos N, Kotteas E, Dimakakos E. Malignant Superior Vena Cava Syndrome: State of the Art. Cureus. 2022 Jan 4;14(1):e20924. doi: 10.7759/cureus.20924[↩]
- Shah RP, Bolaji O, Duhan S, Ariaga AC, Keisham B, Paul T, Aljaroudi W, Alraies MC. Superior Vena Cava Syndrome: An Umbrella Review. Cureus. 2023 Jul 20;15(7):e42227. doi: 10.7759/cureus.42227[↩]
- Sun M, Chen X, Li H, Zhang X, Wang X, Zheng R, Li G, Wang L, Li D. Clinical analysis of 48 cases of malignant superior vena cava syndrome. World J Surg Oncol. 2021 Jun 23;19(1):185. doi: 10.1186/s12957-021-02300-8[↩]
- Ni R, Amr M, Kalla A. Hodgkin Lymphoma-Associated Superior Vena Cava Syndrome: A Case Report and Review of the Literature. Am J Case Rep. 2021 Apr 10;22:e929437. doi: 10.12659/AJCR.929437[↩]
- Zhao QY, Li Q, Cui TL. Risk factors for hypotension in patients with hemodialysis-associated superior vena cava syndrome. J Vasc Surg Venous Lymphat Disord. 2024 Jan;12(1):101682. doi: 10.1016/j.jvsv.2023.08.021[↩]
- Gauden SJ. Superior vena cava syndrome induced by bronchogenic carcinoma: is this an oncological emergency? Australas Radiol. 1993 Nov;37(4):363-6. doi: 10.1111/j.1440-1673.1993.tb00096.x[↩]
- Seligson MT, Surowiec SM. Superior Vena Cava Syndrome. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441981[↩][↩][↩][↩][↩]
- Liu H, Li Y, Wang Y, Yan L, Zhou P, Han X. Percutaneous transluminal stenting for superior vena cava syndrome caused by malignant tumors: a single-center retrospective study. J Cardiothorac Surg. 2021 Mar 20;16(1):39. doi: 10.1186/s13019-021-01418-w[↩]
- Guhlich M, Maag TE, Dröge LH, El Shafie RA, Hille A, Donath S, Schirmer MA, Knaus O, Nauck F, Overbeck TR, Hinterthaner M, Körber W, Andreas S, Rittmeyer A, Leu M, Rieken S. Symptom relief, prognostic factors, and outcome in patients receiving urgent radiation therapy for superior vena cava syndrome : A single-center retrospective analysis of 21 years’ practice. Strahlenther Onkol. 2022 Dec;198(12):1072-1081. doi: 10.1007/s00066-022-01952-z[↩]
- Aung EY, Khan M, Williams N, Raja U, Hamady M. Endovascular Stenting in Superior Vena Cava Syndrome: A Systematic Review and Meta-analysis. Cardiovasc Intervent Radiol. 2022 Sep;45(9):1236-1254. doi: 10.1007/s00270-022-03178-z[↩]
- Seligson MT, Surowiec SM. Superior Vena Cava Syndrome. [Updated 2019 Feb 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441981[↩][↩][↩]
- Drouin L, Pistorius MA, Lafforgue A, N’Gohou C, Richard A, Connault J, Espitia O. [Upper-extremity venous thrombosis: A retrospective study about 160 cases]. Rev Med Interne. 2019 Jan;40(1):9-15[↩]
- Nunnelee J.D. Superior vena cava syndrome. J. Vasc. Nurs. 2007;25:2–5. doi: 10.1016/j.jvn.2006.09.004[↩]
- Rice T.W., Rodriguez R.M., Light R.W. The superior vena cava syndrome: Clinical characteristics and evolving etiology. Medicine. 2006;85:37–42. doi: 10.1097/01.md.0000198474.99876.f0[↩]
- Higdon ML, Atkinson CJ, Lawrence KV. Oncologic Emergencies: Recognition and Initial Management. Am Fam Physician. 2018 Jun 1;97(11):741-748. https://www.aafp.org/pubs/afp/issues/2018/0601/p741.html[↩]
- Osawa S., Sakamoto A., Iwasaki H., Mochizuki C., Takagaki K., Horio Y., Furuta T., Kanaoka S., Ikuma M., Hishida A., et al. Superior vena cava syndrome associated with the metastasis of gastric adenocarcinoma to cervical lymph nodes. Dig. Dis. Sci. 2007;52:3343–3345. doi: 10.1007/s10620-007-8101-8[↩]
- Yamaguchi M., Yoshino I., Osoegawa A., Kameyama T., Tagawa T., Fukuyama S., Oda Y., Tsuneyoshi M., Maehara Y. Inflammatory myofibroblastic tumor of the mediastinum presenting as superior vena cava syndrome. J. Thorac. Cardiovasc. Surg. 2003;126:870–872. doi: 10.1016/S0022-5223(03)00611-1[↩]
- Kalra M., Gloviczki P., Andrews J.C., Cherry K.J., Bower T.C., Panneton J.M., Bjarnason H., Noel A., Schleck C., Harmsen W.S., et al. Open surgical and endovascular treatment of superior vena cava syndrome caused by nonmalignant disease. J. Vasc. Surg. 2003;38:215–223. doi: 10.1016/S0741-5214(03)00331-8[↩]
- Krayem H.K., Bowles A., Hanbali A. Mediastinal hematoma with SVC syndrome from a central venous catheter insertion: A case report. Chest. 2003;124:314S. doi: 10.1378/chest.124.4_MeetingAbstracts.314S[↩]
- Rizvi S, Law MA. Anatomy, Thorax, Mediastinum Superior and Great Vessels. [Updated 2019 Jan 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519576[↩]
- Salavitabar A, Flyer JN, Torres AJ, Richmond ME, Crystal MA, Turner ME, Chai P, Zuckerman WA. Transcatheter stenting of superior vena cava obstruction after pediatric heart transplantation: A single-center experience assessing risk factors and outcomes. Pediatr Transplant. 2018 Nov;22(7):e13267[↩]
- Cardiopulmonary Syndromes (PDQ®)–Patient Version. https://www.cancer.gov/about-cancer/treatment/side-effects/cardiopulmonary-pdq[↩]
- Cardiopulmonary Syndromes (PDQ®)–Health Professional Version. https://www.cancer.gov/about-cancer/treatment/side-effects/cardiopulmonary-hp-pdq[↩]
- De Potter B, Huyskens J, Hiddinga B, Spinhoven M, Janssens A, van Meerbeeck JP, Parizel PM, Snoeckx A. Imaging of urgencies and emergencies in the lung cancer patient. Insights Imaging. 2018 Aug;9(4):463-476. doi: 10.1007/s13244-018-0605-6[↩]
- Friedman T, Quencer KB, Kishore SA, Winokur RS, Madoff DC. Malignant Venous Obstruction: Superior Vena Cava Syndrome and Beyond. Semin Intervent Radiol. 2017 Dec;34(4):398-408. doi: 10.1055/s-0037-1608863[↩]
- Labriola L, Seront B, Crott R, Borceux P, Hammer F, Jadoul M. Superior vena cava stenosis in haemodialysis patients with a tunnelled cuffed catheter: prevalence and risk factors. Nephrol. Dial. Transplant. 2018 Dec 01;33(12):2227-2233[↩]
- Straka C, Ying J, Kong FM, Willey CD, Kaminski J, Kim DW. Review of evolving etiologies, implications and treatment strategies for the superior vena cava syndrome. Springerplus. 2016 Feb 29;5:229. doi: 10.1186/s40064-016-1900-7[↩]
- Mansour A, Saadeh SS, Abdel-Razeq N, Khozouz O, Abunasser M, Taqash A. Clinical Course and Complications of Catheter and Non-Catheter-Related Upper Extremity Deep Vein Thrombosis in Patients with Cancer. Clin. Appl. Thromb. Hemost. 2018 Nov;24(8):1234-1240[↩]
- Nossair F, Schoettler P, Starr J, Chan AKC, Kirov I, Paes B, Mahajerin A. Pediatric superior vena cava syndrome: An evidence-based systematic review of the literature. Pediatr Blood Cancer. 2018 Sep;65(9):e27225[↩]
- Lianos GD, Hasemaki N, Tzima E, Vangelis G, Tselios A, Mpailis I, Lekkas E. Superior vena cava syndrome due to central port catheter thrombosis: a real life-threatening condition. G Chir. 2018 Mar-Apr;39(2):101-106.[↩]
- Kuo TT, Chen PL, Shih CC, Chen IM. Endovascular stenting for end-stage lung cancer patients with superior vena cava syndrome post first-line treatments – A single-center experience and literature review. J Chin Med Assoc. 2017 Aug;80(8):482-486. doi: 10.1016/j.jcma.2017.04.005[↩]
- Nakano T, Endo S, Kanai Y, Otani S, Tsubochi H, Yamamoto S, Tetsuka K. Surgical outcomes after superior vena cava reconstruction with expanded polytetrafluoroethylene grafts. Ann Thorac Cardiovasc Surg. 2014;20(4):310-5. doi: 10.5761/atcs.oa.13-00050[↩]