Contents
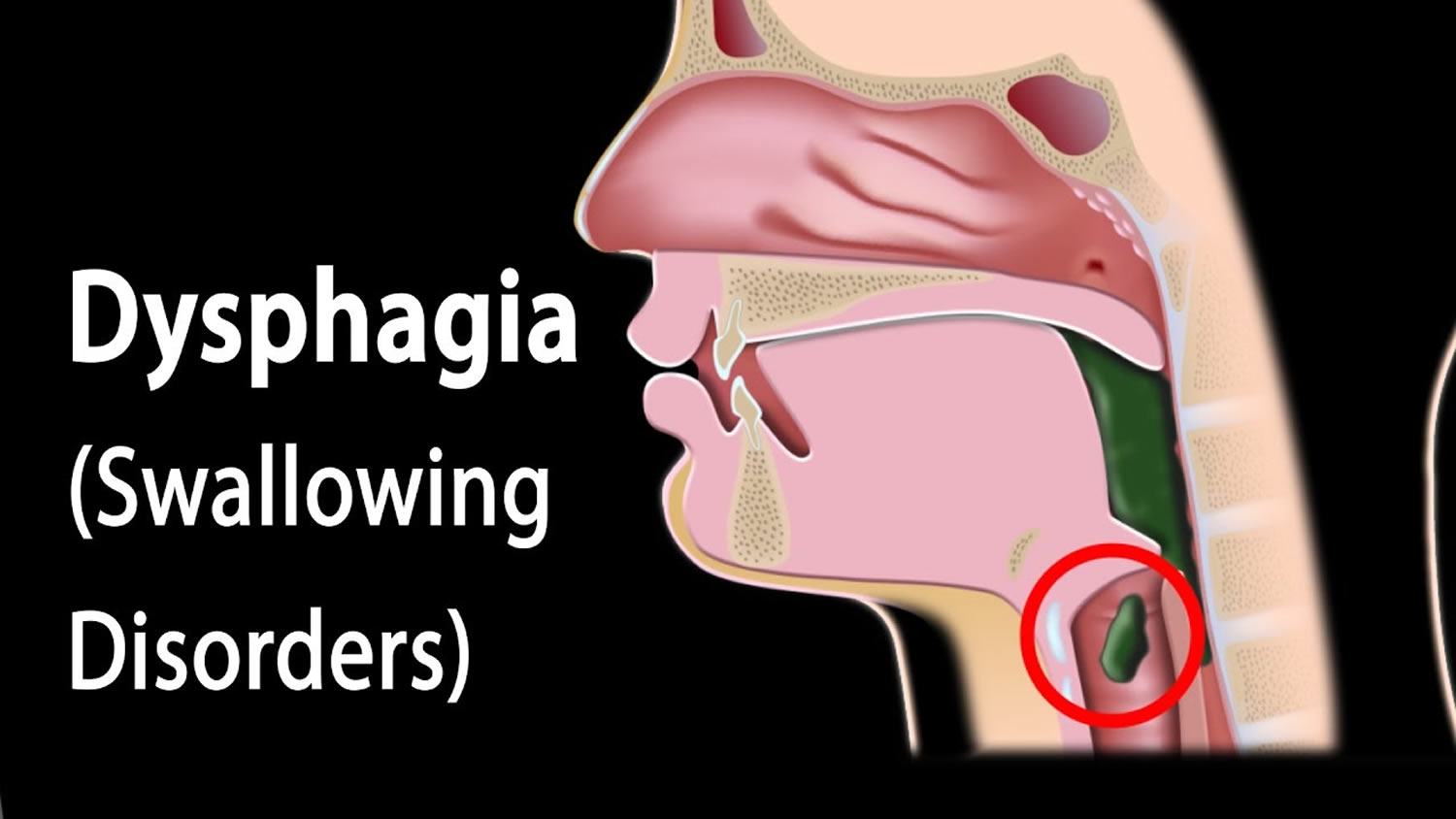
What is dysphagia
Dysphagia is the medical term for swallowing difficulties and may even experience pain while swallowing (odynophagia). Some people with dysphagia have problems swallowing certain foods or liquids, while others can’t swallow at all even their saliva. When that happens, eating becomes a challenge. Often, dysphagia makes it difficult to take in enough calories and fluids to nourish the body and can lead to additional serious medical problems.
Dysphagia can be serious. Someone who cannot swallow safely may not be able to eat enough of the right foods to stay healthy or maintain an ideal weight.
Food pieces that are too large for swallowing may enter the throat and block the passage of air. In addition, when foods or liquids enter the airway of someone who has dysphagia, coughing or throat clearing sometimes cannot remove it. Food or liquid that stays in the airway may enter the lungs and allow harmful bacteria to grow, resulting in a lung infection called aspiration pneumonia.
Swallowing disorders may also include the development of a pocket outside the esophagus caused by weakness in the esophageal wall. This abnormal pocket traps some food being swallowed. While lying down or sleeping, someone with this problem may draw undigested food into the throat. The esophagus may also be too narrow, causing food to stick. This food may prevent other food or even liquids from entering the stomach.
Other signs of dysphagia include:
- coughing or choking when eating or drinking
- bringing food back up, sometimes through the nose
- a sensation that food is stuck in your throat or chest
- persistent drooling of saliva
Over time, dysphagia can also cause symptoms such as weight loss and repeated chest infections.
You should see your doctor if you have swallowing difficulties.
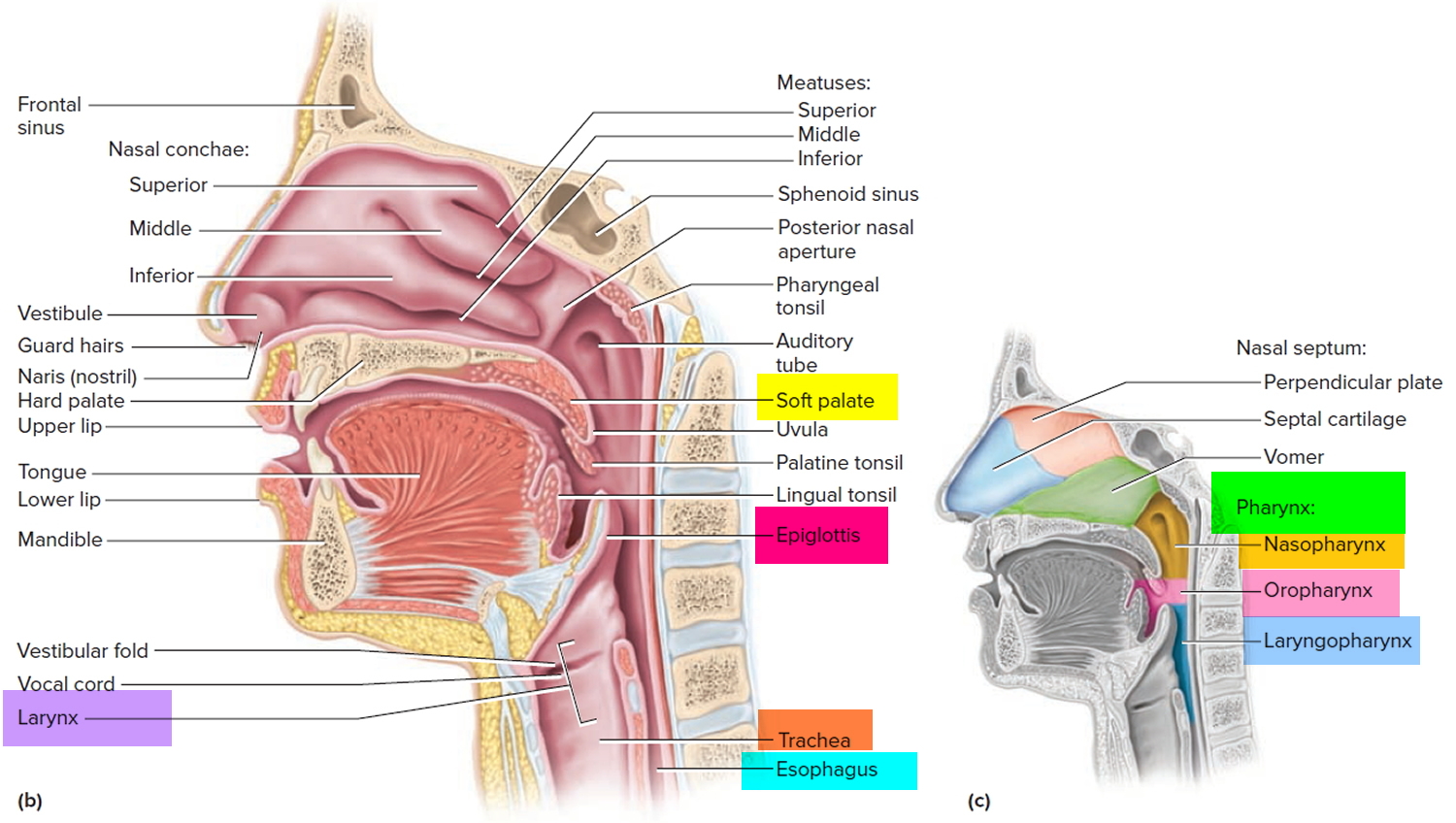
What is the pharynx and the larynx
The pharynx, is a common passageway shared by both the digestive and respiratory systems. The pharynx is a muscular funnel extending about 13 cm (5 in.) from the posterior nasal apertures to the larynx. The pharynx is attached above to the base of the skull and is continuous below, approximately at the level of vertebra CVI (cervical vertebrum C6), with the top of the esophagus. The walls of the pharynx are attached anteriorly to the margins of the nasal cavities, oral cavity, and larynx. Muscles of the pharynx play necessary roles in swallowing and speech.
The pharynx is subdivided into three regions (Figure 1):
- the Nasopharynx,
- the Oropharynx, and
- the Laryngopharynx.
Figure 1. Pharynx and larynx anatomy
The pharynx connects the nose, mouth, and throat. The digestive and respiratory systems share the pharynx. It extends between the posterior nasal apertures and the entrances to the trachea and esophagus. The curving superior and posterior walls are attached to the axial skeleton, but the lateral walls are flexible and muscular.
The Nasopharynx
The posterior apertures (choanae) of the nasal cavities open into the nasopharynx above the soft palate. The nasopharynx receives the auditory (eustachian) tubes from the middle ears and houses the pharyngeal tonsil. The nasopharynx passes only air and is lined by pseudostratified columnar epithelium. Inhaled air turns 90° downward as it passes through the nasopharynx. Relatively large particles (>10 μm) generally cannot make the turn because of their inertia. They collide with the wall of the nasopharynx and stick to the mucosa near the tonsil, which is well positioned to respond to airborne pathogens.
The Oropharynx
The oropharynx extends between the soft palate and the base of the tongue at the level of the hyoid bone. Like the posterior and inferior portions of the nasopharynx, the posterior portion of the oral cavity communicates directly with the oropharynx. The epithelium changes from a pseudostratified ciliated columnar epithelium to a nonkeratinized (mucosal type) stratified squamous epithelium at the boundary between the nasopharynx and oropharynx. The posterior margin of the soft palate supports the dangling uvula and two pairs of muscular pharyngeal arches, the posterior arch and the anterior arch.
The Laryngopharynx
The narrow laryngopharynx includes the region of the pharynx lying between the hyoid bone and the entrance to the esophagus. Like the oropharynx, the laryngopharynx is lined with a stratified squamous epithelium that resists abrasion, chemicals, and pathogens.
How do you swallow?
Swallowing is a complex process. Some 50 pairs of muscles and many nerves work to receive food into the mouth, prepare it, and move it from the mouth to the stomach. This happens in three stages. During the first stage, called the oral phase, the tongue collects the food or liquid, making it ready for swallowing. The tongue and jaw move solid food around in the mouth so it can be chewed. Chewing makes solid food the right size and texture to swallow by mixing the food with saliva. Saliva softens and moistens the food to make swallowing easier. Normally, the only solid we swallow without chewing is in the form of a pill or caplet. Everything else that we swallow is in the form of a liquid, a puree, or a chewed solid.
The second stage begins when the tongue pushes the food or liquid to the back of the mouth. This triggers a swallowing response that passes the food through the pharynx, or throat (see figure). During this phase, called the pharyngeal phase, the larynx (voice box) closes tightly and breathing stops to prevent food or liquid from entering the airway and lungs.
The third stage begins when food or liquid enters the esophagus, the tube that carries food and liquid to the stomach. The passage through the esophagus, called the esophageal phase, usually occurs in about three seconds, depending on the texture or consistency of the food, but can take slightly longer in some cases, such as when swallowing a pill.
How does dysphagia occur?
Dysphagia occurs when there is a problem with the neural control or the structures involved in any part of the swallowing process. Weak tongue or cheek muscles may make it hard to move food around in the mouth for chewing. A stroke or other nervous system disorder may make it difficult to start the swallowing response, a stimulus that allows food and liquids to move safely through the throat. Another difficulty can occur when weak throat muscles, such as after cancer surgery, cannot move all of the food toward the stomach. Dysphagia may also result from disorders of the esophagus.
Dysphagia causes
Dysphagia has many possible causes and happens most frequently in older adults. Any condition that weakens or damages the muscles and nerves used for swallowing may cause dysphagia. For example, people with diseases of the nervous system, such as cerebral palsy or Parkinson’s disease, often have problems swallowing. Additionally, stroke or head injury may weaken or affect the coordination of the swallowing muscles or limit sensation in the mouth and throat.
People born with abnormalities of the swallowing mechanism may not be able to swallow normally. Infants who are born with an opening in the roof of the mouth (cleft palate) are unable to suck properly, which complicates nursing and drinking from a regular baby bottle.
In addition, cancer of the head, neck, or esophagus may cause swallowing problems. Sometimes the treatment for these types of cancers can cause dysphagia. Injuries of the head, neck, and chest may also create swallowing problems. An infection or irritation can cause narrowing of the esophagus. Finally, for people with dementia, memory loss and cognitive decline may make it difficult to chew and swallow.
As swallowing is a complex process, there are many reasons why dysphagia can develop.
Dysphagia is usually caused by another health condition, such as:
- a condition that affects the nervous system, such as a stroke, head injury, or dementia
- cancer – such as mouth cancer or esophageal cancer
- gastro-esophageal reflux disease (GERD) – where stomach acid leaks back up into the esophagus
Dysphagia can also occur in children as the result of a developmental or learning disability.
Dysphagia can be caused by problems with the:
- mouth or throat, known as oropharyngeal or “high” dysphagia
- esophagus (the tube that carries food from your mouth to your stomach), known as esophageal or “low” dysphagia.
Esophageal dysphagia
Esophageal dysphagia refers to the sensation of food sticking or getting hung up in the base of your throat or in your chest after you’ve started to swallow. Some of the causes of esophageal dysphagia include:
- Achalasia. When your lower esophageal muscle (sphincter) doesn’t relax properly to let food enter your stomach, it may cause you to bring food back up into your throat. Muscles in the wall of your esophagus may be weak as well, a condition that tends to worsen over time.
- Diffuse spasm. This condition produces multiple high-pressure, poorly coordinated contractions of your esophagus, usually after you swallow. Diffuse spasm affects the involuntary muscles in the walls of your lower esophagus.
- Esophageal stricture. A narrowed esophagus (stricture) can trap large pieces of food. Tumors or scar tissue, often caused by gastroesophageal reflux disease (GERD), can cause narrowing.
- Esophageal tumors. Difficulty swallowing tends to get progressively worse when esophageal tumors are present.
- Foreign bodies. Sometimes food or another object can partially block your throat or esophagus. Older adults with dentures and people who have difficulty chewing their food may be more likely to have a piece of food become lodged in the throat or esophagus.
- Esophageal ring. A thin area of narrowing in the lower esophagus can intermittently cause difficulty swallowing solid foods.
- GERD. Damage to esophageal tissues from stomach acid backing up into your esophagus can lead to spasm or scarring and narrowing of your lower esophagus.
- Eosinophilic esophagitis. This condition, which may be related to a food allergy, is caused by an overpopulation of cells called eosinophils in the esophagus.
- Scleroderma. Development of scar-like tissue, causing stiffening and hardening of tissues, can weaken your lower esophageal sphincter, allowing acid to back up into your esophagus and cause frequent heartburn.
- Radiation therapy. This cancer treatment can lead to inflammation and scarring of the esophagus.
Oropharyngeal dysphagia
Certain conditions can weaken your throat muscles, making it difficult to move food from your mouth into your throat and esophagus when you start to swallow. You may choke, gag or cough when you try to swallow or have the sensation of food or fluids going down your windpipe (trachea) or up your nose. This may lead to pneumonia.
Causes of oropharyngeal dysphagia include:
- Neurological disorders. Certain disorders — such as multiple sclerosis, muscular dystrophy and Parkinson’s disease — can cause dysphagia.
- Neurological damage. Sudden neurological damage, such as from a stroke or brain or spinal cord injury, can affect your ability to swallow.
- Pharyngoesophageal diverticulum (Zenker’s diverticulum). A small pouch that forms and collects food particles in your throat, often just above your esophagus, leads to difficulty swallowing, gurgling sounds, bad breath, and repeated throat clearing or coughing.
- Cancer. Certain cancers and some cancer treatments, such as radiation, can cause difficulty swallowing.
Difficulty swallowing causes
Neurological causes
The nervous system is made up of the brain, nerves and spinal cord. Damage to the nervous system can interfere with the nerves responsible for starting and controlling swallowing. This can lead to dysphagia.
Some neurological causes of dysphagia include:
- a stroke
- neurological conditions that cause damage to the brain and nervous system over time, including Parkinson’s disease, multiple sclerosis, dementia, and
- motor neurone disease (ALS, amyotrophic lateral sclerosis)
- brain tumors
- myasthenia gravis – a rare condition that causes your muscles to become weak
Congenital and developmental conditions
The term “congenital” refers to something you’re born with. Developmental conditions affect the way you develop.
Congenital or developmental conditions that may cause dysphagia include:
- learning disabilities – where learning, understanding, and communicating are difficult
- cerebral palsy – a group of neurological conditions that affect movement and co-ordination
- a cleft lip and palate – a common birth defect that results in a gap or split in the upper lip or roof of the mouth
Obstruction
Conditions that cause an obstruction in the throat or a narrowing of the esophagus (the tube that carries food from your mouth to the stomach) can make swallowing difficult.
Some causes of obstruction and narrowing include:
- mouth cancer or throat cancer, such as laryngeal cancer or esophageal cancer – once these cancers are treated, the obstruction may no longer be an issue
- pharyngeal (throat) pouches, also known as Zenker diverticulum – where a large sac develops in the upper part of the esophagus, which reduces the ability to swallow both liquids and solids; it’s a rare condition that mainly affects older people
- eosinophilic esophagitis – where a type of white blood cell known as an eosinophil builds up in the lining of the esophagus as the result of a reaction to foods, allergens, or acid reflux; the build-up damages the lining of the esophagus and causes swallowing difficulties
- radiotherapy treatment – this can cause scar tissue, which narrows the passageway in your throat and esophagus
- gastro-esophageal reflux disease (GERD) – stomach acid can cause scar tissue to develop, narrowing your esophagus
- infections, such as tuberculosis or thrush – these can lead to inflammation of the esophagus (esophagitis)
Muscular conditions
Any condition that affects the muscles used to push food down the esophagus and into the stomach can cause dysphagia, although such conditions are rare.
Two muscular conditions associated with dysphagia are:
- Scleroderma – where the immune system (the body’s natural defence system) attacks healthy tissue, leading to a stiffening of the throat and esophagus muscles
- Achalasia – where muscles in the esophagus lose their ability to relax and open to allow food or liquid to enter the stomach
Other causes
As you get older, the muscles used for swallowing can become weaker. This may explain why dysphagia is relatively common in elderly people. Treatment is available to help people with age-related dysphagia.
Chronic obstructive pulmonary disease (COPD) is a collection of lung conditions that make it difficult to breathe in and out properly. Breathing difficulties can sometimes affect your ability to swallow.
Dysphagia can also sometimes develop as a complication of head or neck surgery.
Risk factors for developing dysphagia
The following are risk factors for dysphagia:
- Aging. Due to natural aging and normal wear and tear on the esophagus and a greater risk of certain conditions, such as stroke or Parkinson’s disease, older adults are at higher risk of swallowing difficulties. But, dysphagia isn’t considered a normal sign of aging.
- Certain health conditions. People with certain neurological or nervous system disorders are more likely to experience difficulty swallowing.
Dysphagia symptoms
You might have dysphagia if you notice any of these signs and symptoms:
- having pain while swallowing (odynophagia)
- having to cut food into smaller pieces or avoiding certain foods because of trouble swallowing
- food or drink gets stuck in your throat or goes down the wrong way
- eating your meal takes a long time (for example, more than 30 minutes)
- you need to cough or clear your throat during or after eating and drinking
- you have heartburn often
- having food or stomach acid back up into your throat
- you feel short of breath when eating and drinking
- you avoid some foods because you find them hard to swallow
- you often get chest infections for no obvious reason
- drooling
- being hoarse
- bringing food back up (regurgitation)
- unexpectedly losing weight
- coughing or gagging when swallowing
Babies that have difficulty sucking during breast or bottle feeding could have dysphagia.
Dysphagia complications
The main complication of dysphagia is coughing and choking, which can lead to pneumonia.
Coughing and choking
If you have dysphagia, there’s a risk of food, drink or saliva going down the “wrong way”. It can block your airway, making it difficult to breathe and causing you to cough or choke.
If you have dysphagia, you may also develop a fear of choking. However, it’s very important you don’t avoid eating and drinking, as it could cause dehydration and malnutrition.
If you often choke on your food because of dysphagia, you may also be at an increased risk of developing a condition called aspiration pneumonia.
Aspiration pneumonia
Aspiration pneumonia is a chest infection that can develop after accidentally inhaling something, such as a small piece of food. It causes irritation in the lungs, or damages them. Older people are particularly at risk of developing aspiration pneumonia.
The symptoms of aspiration pneumonia include:
- a cough – this may be a dry cough, or you may produce phlegm that’s yellow, green, brown, or bloodstained
- a high temperature of 38 °C (100.4 °F) or over
- chest pain
- difficulty breathing – your breathing may be rapid and shallow and you may feel breathless, even at rest.
Symptoms of aspiration pneumonia can range from mild to severe, and it is usually treated with antibiotics. Severe cases will require hospital admission and treatment with intravenous antibiotics (through a drip). Read more about treating pneumonia.
In particularly old or frail people, there’s a chance the infection could lead to their lungs becoming filled with fluid, preventing them working properly. This is known as acute respiratory distress syndrome (ARDS).
Your chances of developing pneumonia as a result of dysphagia are higher if you have a weakened immune system, chronic obstructive pulmonary disease (COPD), or if your oral and dental hygiene is poor.
Dysphagia in children
If children with long-term dysphagia aren’t eating enough, they may not get the essential nutrients they need for physical and mental development.
Children who have difficulty eating may also find meal times stressful, which may lead to behavioral problems.
Dysphagia diagnosis
See your doctor if you’re having any difficulty swallowing. They’ll carry out an initial assessment and may refer you for further tests and treatment.
Tests will help determine whether your dysphagia is the result of a problem with your mouth or throat (oropharyngeal, or “high” dysphagia), or your esophagus, the tube that carries food from the mouth to the stomach (esophageal, or “low” dysphagia).
Diagnosing the specific type of dysphagia can make treatment more effective and reduce your chances of developing complications of dysphagia, such as choking or pneumonia.
Your doctor will want to know:
- how long you’ve had dysphagia
- whether your symptoms come and go, or are getting worse
- whether dysphagia has affected your ability to swallow solids, liquids, or both
- whether you’ve lost weight
Depending on the suspected cause, you may be referred for further tests with:
- an ear, nose and throat (ENT) specialist
- a speech and language therapist
- a neurologist – a specialist in conditions that affect the brain, nerves, and spinal cord
- a gastroenterologist – a specialist in treating conditions of the gullet, stomach, and intestines
- a geriatrician – a specialist in the care of elderly people
Your doctor will ask you about your symptoms, examine you and might also refer you for tests such as:
- a barium swallow – swallowing a non-toxic substance called barium shows your upper digestive system on an x-ray
- endoscopy – to view inside the oesophagus
- muscle testing – to see if your oesophagus is working properly
- CT scan
- MRI scan
The types of tests you might need are explained below.
Water swallow test
A water swallow test is usually carried out by a speech and language therapist, and can give a good initial assessment of your swallowing abilities. You’ll be given 150ml of water and asked to swallow it as quickly as possible.
The time it takes you to drink all of the water and the number of swallows required will be recorded. You may also be asked to swallow a soft piece of pudding or fruit.
Videofluoroscopy
A videofluoroscopy, or modified barium swallow, is one of the most effective ways of assessing your swallowing ability and finding exactly where the problem is.
An X-ray machine records a continuous moving X-ray on to video, allowing your swallowing problems to be studied in detail.
You’ll be asked to swallow different types of food and drink of different consistencies, mixed with a non-toxic liquid called barium that shows up on X-rays.
A videofluoroscopy usually takes about 30 minutes. You may feel sick after the test, and the barium may cause constipation. Your stools may also be white for a few days as the barium passes through your system.
Nasoendoscopy
A nasendoscopy, sometimes also known as fibreoptic endoscopic evaluation of swallowing, is a procedure that allows the nose and upper airways to be closely examined using a very small flexible tube known as an endoscope.
The endoscope is inserted into your nose so the specialist can look down on to your throat and upper airways. It has a light and camera at the end so images of the throat can be viewed on a television screen. This allows any blockages or problem areas to be identified.
Fibreoptic endoscopic evaluation of swallowing can also be used to test for oropharyngeal dysphagia after you’re asked to swallow a small amount of test liquid (usually colored water or milk).
Before the procedure, you may have local anesthetic spray into your nose, but because the camera doesn’t go as far as your throat, it doesn’t cause retching. The procedure is safe and usually only takes a few minutes.
Manometry and 24-hour pH study
Manometry is a procedure to assess the function of your esophagus. It involves passing a small tube (catheter) with pressure sensors through your nose and into your esophagus to monitor its function.
The test measures the pressures within your esophagus when you swallow, which determines how well it’s working.
The 24-hour pH study involves inserting a tube into your esophagus through your nose to measure the amount of acid that flows back from your stomach. This can help determine the cause of any swallowing difficulties.
Diagnostic gastroscopy
Diagnostic gastroscopy, also known as diagnostic endoscopy of the stomach, or oesophagogastroduodenoscopy (OGD), is an internal examination using an endoscope.
The endoscope is passed down your throat and into your esophagus, and images of the inside of your body are transmitted to a television screen. It can often detect cancerous growths or scar tissue.
Nutritional assessment
If dysphagia has affected your ability to eat, you may need a nutritional assessment to check that you’re not lacking nutrients (malnourished). This could involve:
- measuring your weight
- calculating your body mass index (BMI) to check whether you’re a healthy weight for your height
- carrying out blood tests.
Dysphagia treatment
Most swallowing problems can be treated, although the treatment you receive will depend on the type of dysphagia you have.
Treatment will depend on whether your swallowing problem is in the mouth or throat (oropharyngeal, or “high” dysphagia), or in the esophagus (esophageal, or “low” dysphagia).
The cause of dysphagia is also considered when deciding on treatment. In some cases, treating the underlying cause, such as mouth cancer or esophageal cancer, can help relieve swallowing problems.
Treatment for dysphagia may be managed by a group of specialists known as a multidisciplinary team. Your multidisciplinary team may include a speech and language therapist (speech and language pathologist), a surgeon, and a dietitian.
High (oropharyngeal) dysphagia
High dysphagia is swallowing difficulties caused by problems with the mouth or throat.
It can be difficult to treat if it’s caused by a condition that affects the nervous system. This is because these problems can’t usually be corrected using medication or surgery.
There are three main treatments for high dysphagia:
- swallowing therapy
- dietary changes
- feeding tubes
Swallowing therapy
You may be referred to a speech and language therapist (speech and language pathologist) for swallowing therapy if you have high dysphagia.
An speech and language pathologist is a healthcare professional trained to work with people with feeding or swallowing difficulties.
speech and language pathologists use a range of techniques that can be tailored for your specific problem, such as teaching you swallowing exercises.
Dysphagia diet
You may be referred to a dietitian (specialist in nutrition) for advice about changes to your diet to make sure you receive a healthy, balanced diet.
An speech and language pathologist can give you advice about softer foods and thickened fluids that you may find easier to swallow. They may also try to ensure you’re getting the support you need at meal times.
Feeding tubes
Feeding tubes can be used to provide nutrition while you’re recovering your ability to swallow. They may also be required in severe cases of dysphagia that put you at risk of malnutrition and dehydration.
A feeding tube can also make it easier for you to take the medication you may need for other conditions.
There are two types of feeding tubes:
- a nasogastric tube – a tube that is passed down your nose and into your stomach
- a percutaneous endoscopic gastrostomy (PEG) tube – a tube that is implanted directly into your stomach
Nasogastric tubes are designed for short-term use. The tube will need to be replaced and swapped to the other nostril after about a month. PEG tubes are designed for long-term use and last several months before they need to be replaced.
Most people with dysphagia prefer to use a percutaneous endoscopic gastrostomy (PEG) tube because it can be hidden under clothing. However, they carry a greater risk of complications compared with nasogastric tubes.
Minor complications of PEG tubes include tube displacement, skin infection, and a blocked or leaking tube. Two major complications of percutaneous endoscopic gastrostomy (PEG) tubes are infection and internal bleeding.
Resuming normal feeding may be more difficult with a percutaneous endoscopic gastrostomy (PEG) tube compared with using a nasogastric tube. The convenience of percutaneous endoscopic gastrostomy (PEG) tubes can make people less willing to carry out swallowing exercises and dietary changes than those who use nasogastric tubes.
You should discuss the pros and cons of both types of feeding tubes with your treatment team.
Low (oesophageal) dysphagia
Low dysphagia is swallowing difficulties caused by problems with the esophagus.
Medication
Depending on the cause of low dysphagia, it may be possible to treat it with medication. For example, proton pump inhibitors (PPIs) used to treat indigestion may improve symptoms caused by narrowing or scarring of the esophagus.
Botulinum toxin
Botulinum toxin can sometimes be used to treat achalasia. This is a condition where the muscles in the esophagus become too stiff to allow food and liquid to enter the stomach.
It can be used to paralyze the tightened muscles that prevent food from reaching the stomach. However, the effects only last for around six months.
Surgery
Other cases of low dysphagia can usually be treated with surgery.
Surgery may be recommended to relieve swallowing problems caused by throat narrowing or blockages, including bony outgrowths, vocal cord paralysis, pharyngoesophageal diverticulum, GERD and achalasia, or to treat esophageal cancer. Speech and swallowing therapy is usually helpful after surgery.
The type of surgical treatment depends on the cause for dysphagia. Some examples are:
- Laparoscopic Heller myotomy, which is used to cut the muscle at the lower end of the esophagus (sphincter) when it fails to open and release food into the stomach in people who have achalasia.
- Esophageal dilation. Your doctor inserts a lighted tube (endoscope) into your esophagus and inflates an attached balloon to gently stretch and expand its width (dilation). This treatment is used for a tight sphincter muscle at the end of the esophagus (achalasia), a narrowing of the esophagus (esophageal stricture), an abnormal ring of tissue located at the junction of the esophagus and stomach (Schatzki’s ring) or a motility disorder. Alternatively, your doctor may pass a flexible tube or tubes of different diameters instead of a balloon.
- Stent placement. The doctor can also insert a metal or plastic tube (stent) to prop open a narrowing or blockage in your esophagus. Some stents are permanent, such as those for people with esophageal cancer, while others are temporary and are removed later.
Endoscopic dilatation
Endoscopic dilation is widely used to treat dysphagia caused by obstruction. It can also be used to stretch your esophagus if it’s scarred.
Endoscopic dilatation will be carried out during an internal examination of your esophagus (gastroscopy) using an endoscopy.
An endoscope is passed down your throat and into your esophagus, and images of the inside of your body are transmitted to a television screen.
Using the image as guidance, a small balloon or a bougie (a thin, flexible medical instrument) is passed through the narrowed part of your esophagus to widen it. If a balloon is used, it will be gradually inflated to widen your esophagus before being deflated and removed.
You may be given a mild sedative before the procedure to relax you. There’s a small risk that the procedure could cause a tear or perforate your esophagus.
Inserting a stent
If you have esophageal cancer that can’t be removed, it’s usually recommended that you have a stent inserted instead of endoscopic dilatation. This is because, if you have cancer, there’s a higher risk of perforating your esophagus if it’s stretched.
A stent (usually a metal mesh tube) is inserted into your esophagus during an endoscopy or under X-ray guidance.
The stent then gradually expands to create a passage wide enough to allow food to pass through. You’ll need to follow a particular diet to keep the stent open without having blockages.
Congenital dysphagia
If your baby is born with difficulty swallowing (congenital dysphagia), their treatment will depend on the cause.
Cerebral palsy
Dysphagia caused by cerebral palsy can be treated with speech and language therapy. Your child will be taught how to swallow, how to adjust the type of food they eat, and how to use feeding tubes.
Cleft lip and palate
Cleft lip and palate is a facial birth defect that can cause dysphagia. It’s usually treated with surgery.
Narrowing of the esophagus
Narrowing of the esophagus may be treated with a type of surgery called dilatation to widen the esophagus.
Gastro-esophageal reflux disease (GERD)
Dysphagia caused by gastro-esophageal reflux disease (GERD) can be treated using special thickened feeds instead of your usual breast or formula milk. Sometimes medication may also be used.
Lifestyle and home remedies
If you have trouble swallowing, be sure to see a doctor and follow his or her advice. Also, some things you can try to help ease your symptoms include:
- Changing your eating habits. Try eating smaller, more-frequent meals. Be sure to cut your food into smaller pieces, chew food thoroughly and eat more slowly.
- Trying foods with different textures to see if some cause you more trouble. Thin liquids, such as coffee and juice, are a problem for some people, and sticky foods, such as peanut butter or caramel, can make swallowing difficult. Avoid foods that cause you trouble.
- Avoiding alcohol, tobacco and caffeine. These can make heartburn worse.