Contents
What is Horner’s syndrome
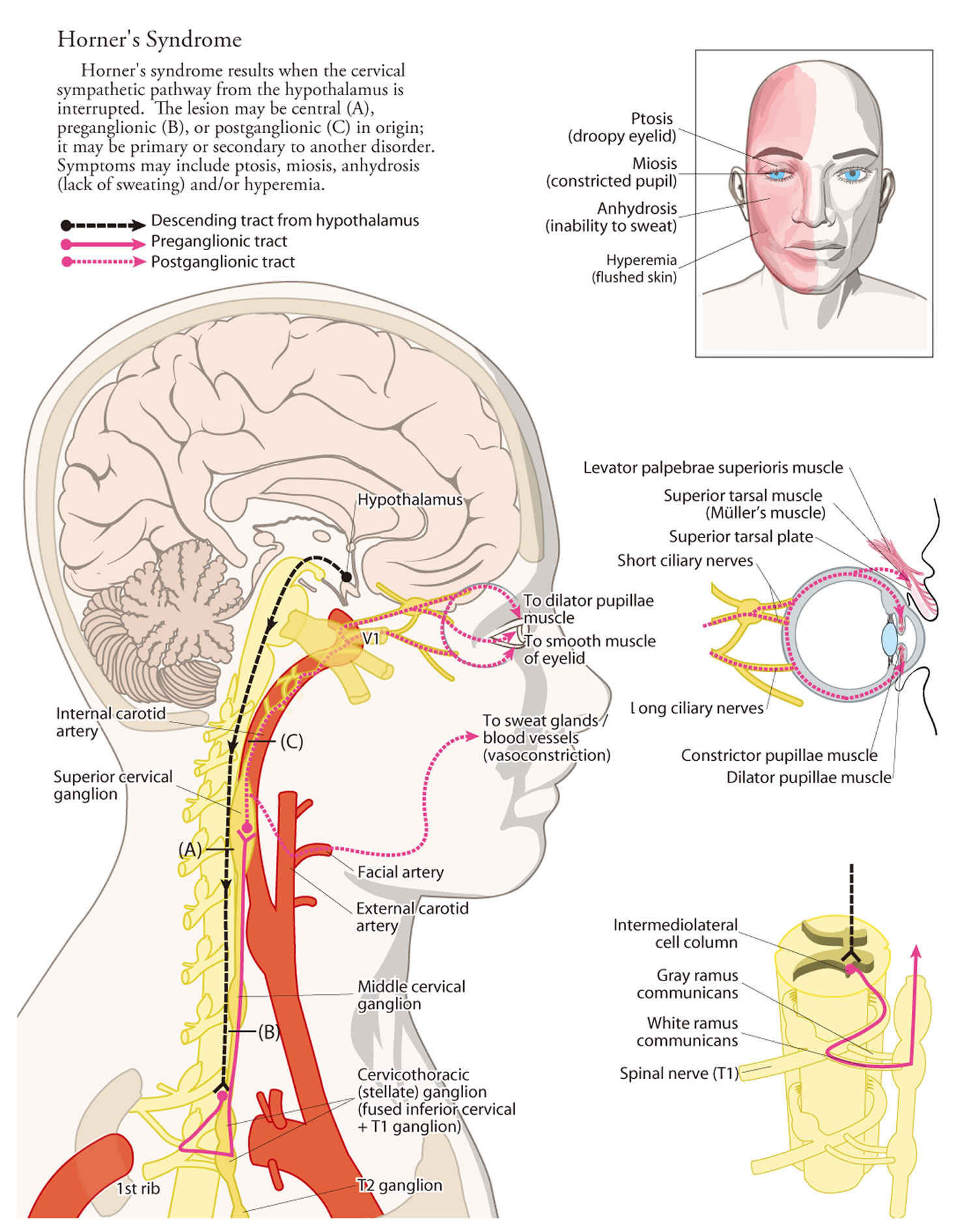
Horner’s syndrome (also called oculosympathetic paresis or Horner syndrome) is a disorder that affects the eye and surrounding tissues on one side of the face and results from paralysis of certain nerves. Horner’s syndrome results from a lesion to the sympathetic pathways that supply the head and neck, including the oculosympathetic fibers (see Figures 1 to 3 below). The significance of Horner’s syndrome lies in the underlying diseases that cause this syndrome, rather than a clinical disease by itself.
Horner’s syndrome usually results from a lesion to the sympathetic pathways that supply the head and neck region. The causes of Horner’s syndrome varies with the age of the patient and site of the lesion. Prompt evaluation is necessary to detect and treat life-threatening conditions.
Horner’s syndrome can appear at any time of life; in about 5 percent of affected individuals, the disorder is present from birth (congenital) – congenital Horner’s syndrome. In a population based study of Horner’s syndrome in the pediatric age group, the incidence of Horner’s syndrome was estimated to be 1.42 per 100 000 patients younger than 19 years, with a birth prevalence of 1 in 6250 for those with a congenital onset.
Horner’s syndrome is characterized by these 3 signs:
- Drooping of the upper eyelid (ptosis) on the affected side,
- A constricted pupil in the affected eye (miosis) resulting in unequal pupil size (anisocoria), and
- Absent sweating (anhidrosis) on the affected side of the face.
The pupil is innervated by sympathetic and parasympathetic fibers. Pupillary dilation is mediated by a three- neuron sympathetic pathway that originates in the hypothalamus.
Sinking of the eye into its cavity (enophthalmos) and a bloodshot eye often occur in this disorder. In people with Horner’s syndrome that occurs before the age of 2, the colored part (iris) of the eyes may differ in color (iris heterochromia), with the iris of the affected eye being lighter in color than that of the unaffected eye. Individuals who develop Horner’s syndrome after age 2 do not generally have iris heterochromia.
The abnormalities in the eye area related to Horner’s syndrome do not generally affect vision or health. However, the nerve damage that causes Horner’s syndrome may result from other health problems, some of which can be life-threatening.
A number of factors, some more serious than others, can cause Horner syndrome. It is important to get a prompt and accurate diagnosis.
Get emergency care if signs or symptoms associated with Horner syndrome appear suddenly, appear after a traumatic injury, or are accompanied by other signs or symptoms, such as:
- Impaired vision
- Dizziness
- Muscle weakness or lack of muscle control
- Severe, sudden headache or neck pain
Figure 1. Horner’s syndrome
Oculosympathetic pathway anatomy
It is important to understand the anatomy of sympathetic nerves supplying the eye (see Figures 1 to 3 below).
The sympathetic innervation of the eye and the ocular adnexae is traditionally described as a 3-neuron pathway (Figures 2 and 3). It consists of a central (first-order) neuron located in the posterolateral hypothalamus, which axon descends ipsilaterally and connects to a preganglionic (second-order) neuron in the intermediolateral columns of the spinal cord at level C8 through T2, and a postganglionic (third-order) neuron located in the superior cervical ganglion 1.
Spanning from C8-T4, most fibers from the preganglionic neuron leave through the T1 ventral spinal nerve root, but sudomotor and vasomotor fibers to the face primarily exit at the T2 and T3 level.2 The fibers rejoin in the sympathetic trunk, which ascends adjacent to spinal vertebrae, the apex of the lung, the first rib, and the common carotid artery before synapsing with the postganglionic neuron in the superior cervical ganglion 1. The postganglionic fibers form a nerve plexus in the adventitia of the common carotid artery. Most fibers follow the internal carotid artery through the cavernous sinus, reaching the superior tarsal muscle by the ophthalmic artery, whereas fibers to the iris dilator muscle branch off and follow the nasociliar nerve. The sudomotor and vasomotor fibers, however, follow the external carotid artery to the face 1.
There are 3 group of nerves supplying the sympathetic function of the eyes. The following describes the path of the different nerve fibers:
First order (central) neuron
- The first order (central) neuron descends caudally from the middle of the brain (hypothalamus) to the first synapse in the cervical spinal cord (C8-T2 level-also called the ciliospinal center of Budge). The descending sympathetic tract is in close proximity to other tracts and nuclei in the brainstem.
Second order (preganglionic) neuron
- The second order (preganglionic) neuron destined for the head and neck exits the spinal cord and travels in the cervical sympathetic chain through the brachial plexus, over the pulmonary apex and synapses in the superior cervical ganglion. The superior cervical ganglion is located near the angle of the mandible and bifurcation of the common carotid artery.
Third order (postganglionic) neuron
- Third order (postganglionic) neurons travel via the outside of spinal cord near the carotid artery (neck artery that can be felt) to the eye. The third order neuron for the orbit enters the cranium within the adventitia of the internal carotid artery into the cavernous sinus. Here the oculosympathetic fibers exit the internal carotid artery in close proximity to the trigeminal ganglion and the sixth cranial nerve and join the 1st division of the trigeminal nerve to enter the orbit.
The fibers (long ciliary nerve) innervate the dilator muscles of the iris and the Müller’s muscle in the upper and lower lid.
The vasomotor and sudomotor fibers to the face exit the superior cervical ganglion and ascend in the external carotid artery.
Pupillary constriction is produced by parasympathetic (cholinergic) fibers that travel with the third cranial (oculomotor) nerve.
- The last fibers provide innervation to several tissues:
- Muscle that dilates the pupil
- Muscle that raises the eyelid
- Sweat glands of the face, which is responsible for facial sweating
In Horner syndrome, there is disruption to this whole chain of sympathetic nerves. Hence it is important to find out the cause of this. There are many causes of Horner syndrome, but the most sinister one would be a lung cancer sitting on the tip of the lungs, slowing invading the nerve tissue.
Figure 2. Sympathetic division of the autonomic nervous system
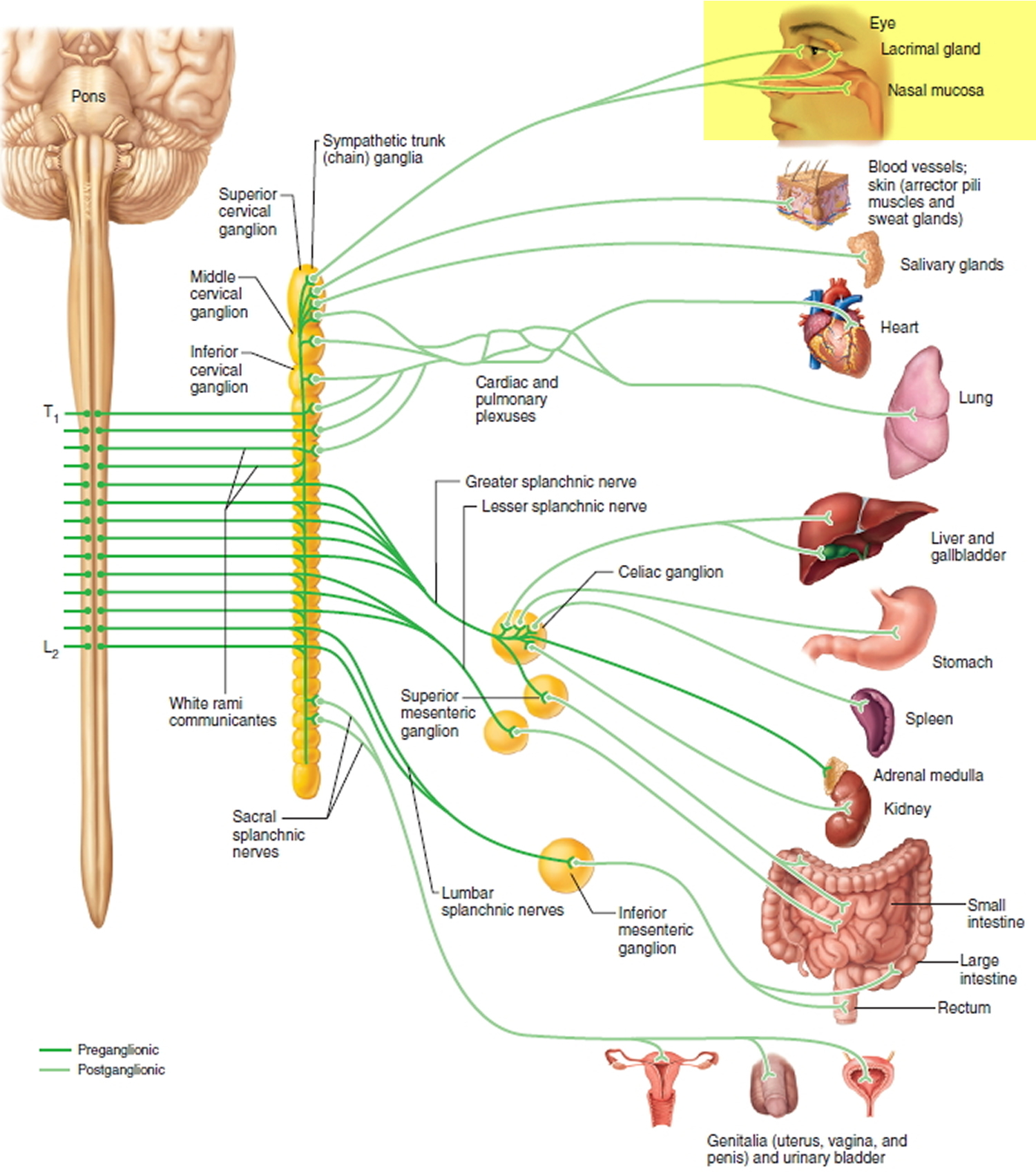 Figure 3. Sympathetic nerves of Horner’s syndrome
Figure 3. Sympathetic nerves of Horner’s syndrome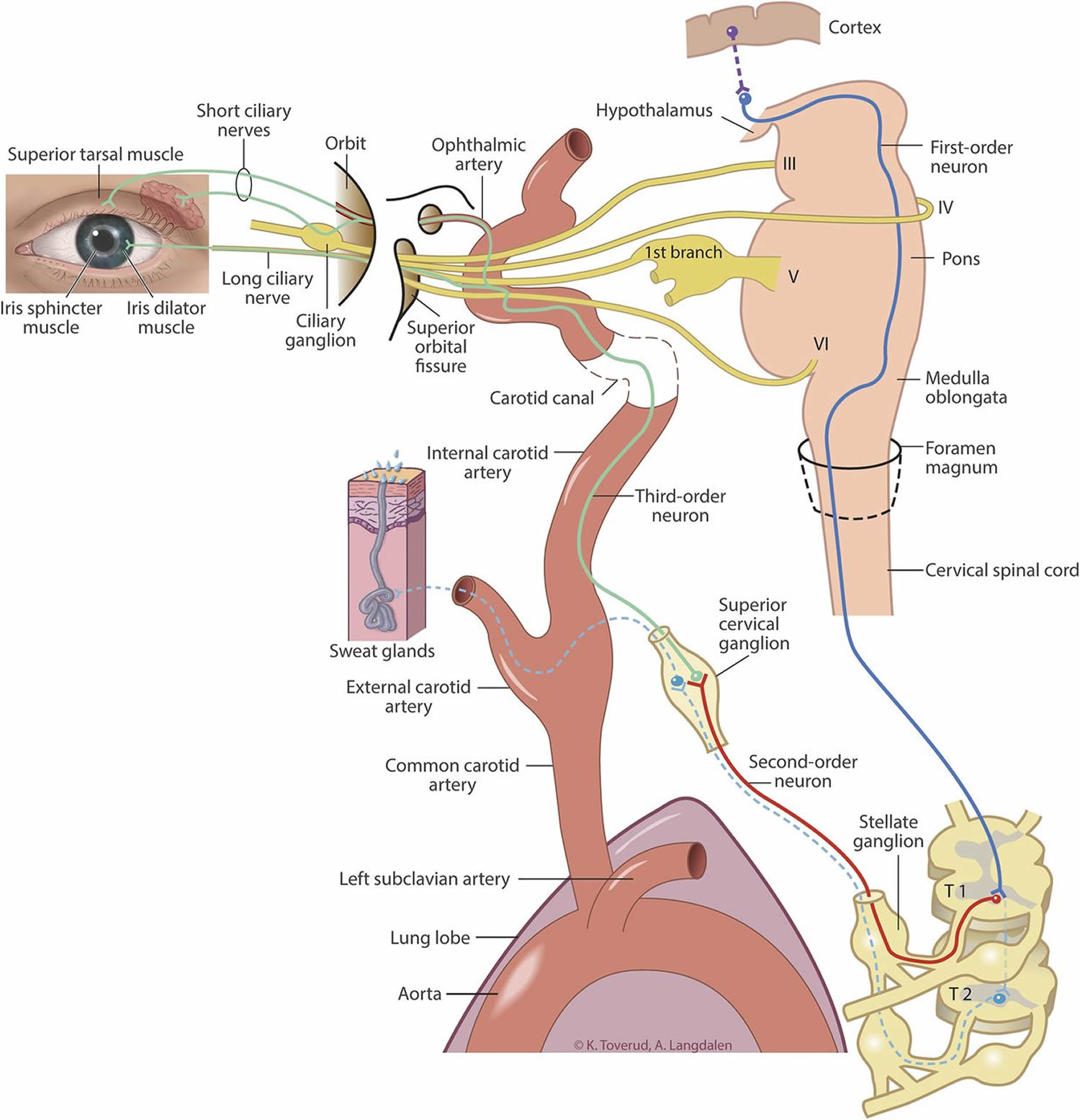
 Horner’s syndrome causes
Horner’s syndrome causes
The cause of Horner’s syndrome varies with the patient age and site of lesion. The cause remains unknown in 35-40% of cases. This is known as idiopathic Horner syndrome.
Horner syndrome is caused by damage to a certain pathway in the sympathetic nervous system. The sympathetic nervous system regulates heart rate, pupil size, perspiration, blood pressure and other functions that enable you to respond quickly to changes in your environment.
The nerve pathway affected in Horner syndrome is divided into three groups of nerve cells (neurons).
Central (first order neuron) Horner’s syndrome
These include lesions of the hypothalamus, brainstem and spinal cord such as stroke (classically the lateral medullary syndrome), demyelination (such as multiple sclerosis), neoplasms (such as glioma) or other processes such as a syrinx (syringomyelia or syringobulbia).
Problems in this region that can disrupt nerve function related to Horner syndrome include:
- Stroke
- Tumor
- Diseases that cause the loss of the protective sheath on neurons (myelin)
- Neck trauma
- Cyst or cavity in the spinal column (syringomyelia or syringobulbia)
Preganglionic (second order neuron) Horner’s syndrome
These include lesions of the thoracic outlet (cervical rib, subclavian artery aneurysm), mediastinum (mediastinal tumors), pulmonary apex (Pancoast’s tumor), neck (thyroid malignancies) or the thoracic spinal cord (trauma) or surgical procedures in this region including radical neck dissection, jugular vein cannulation, thoracoscopy or mediastinoscopy, chest tube placement and other thoracic surgical procedures.
Causes related to nerve damage in this region may include:
- Lung cancer
- Tumor of the myelin sheath (schwannoma)
- Damage to the main blood vessel leading from the heart (aorta)
- Surgery in the chest cavity
- Traumatic injury
Third order neuron or postganglionic lesion
Third order neuron or postganglionic lesion: These include lesions of the superior cervical ganglion (trauma, radical neck dissection or jugular vein ectasia), lesions of the internal carotid artery in the neck and skull base (dissection, thrombosis, invasion by tumors or iatrogenic from endarterectomy or stenting, base of skull malignancies), lesions of internal carotid artery in the cavernous sinus (thrombosis, aneurysm, inflammation or invasive tumors) and lesions of the sellar and parasellar regions (invasive pituitary tumors, metastatic tumors, paratrigeminal tumors). Other causes include cluster headaches.
Nerve damage in this region may be associated with the following:
- Damage to the carotid artery along the side of the neck
- Damage to the jugular vein along the side of the neck
- Tumor or infection near the base of the skull
- Migraines
- Cluster headaches, a disorder that results in cylical patterns of severe headaches
Children
In children, trauma (birth trauma or neck trauma) is the most common cause of Horner’s syndrome.
Other causes of Horner syndrome in children include:
- Defect of the aorta present at birth
- Tumor of the hormonal and nervous systems (neuroblastoma)
Other causes
Other causes include surgical trauma, neuroblastoma, brainstem lesions (such as vascular malformations, glioma and demyelination) and carotid artery thrombosis.
Horner’s syndrome prognosis
Prognosis depends on the etiology of Horner’s syndrome.
Horner’s syndrome symptoms
Horner syndrome usually affects only one side of the face. Common signs and symptoms include:
- A persistently small pupil (miosis)
- A notable difference in pupil size between the two eyes (anisocoria)
- Little or delayed opening (dilation) of the affected pupil in dim light
- Drooping of the upper eyelid (ptosis)
- Slight elevation of the lower lid, sometimes called upside-down ptosis
- Little or no sweating (anhidrosis) either on the entire side of the face or an isolated patch of skin on the affected side
Signs and symptoms, particularly ptosis and anhidrosis, may be subtle and difficult to detect.
Ocular signs
- Eyelids: patients have a mild (less than 2 mm) ptosis of upper lid and inverse ptosis of the lower lid (lower lid rests at a higher level than normal) which produces a decreased palpebral aperture compared to the fellow eye.
- Pupils: Patients have anisocoria (difference in the pupillary size) with the ptotic eye having the smaller pupil (miosis). The anisocoria is more prominent in the dark indicating pathology of the pupillary dilator. The smaller pupil takes a longer time to dilate when a bright source of light is moved away from the eye. This phenomenon is called dilation lag.
- Iris heterochromia (different colored irides) may be seen in children with congenital Horner’s syndrome.
- Extraocular movements may be affected in lesions of the brainstem or the cavernous sinus.
- Other signs of sympathetic denervation include ipsilateral conjunctival injection, changes in accommodation and lower intraocular pressure.
Neurologic signs
Neurologic signs may be present depending on the site of lesion:
- Brainstem (bulbar) signs: ataxia, diplopia, nystagmus, lateralized weakness or numbness, hoarseness and dysphagia.
- Spinal cord (myelopathic) signs: sensory or motor abnomalities with a level, dysfunction of bowel or bladder movements, erectile dysfunction in men and spasticity.
- Brachial plexopathy: pain and weakness in the arm, or hand; abnormalities can be confirmed by nerve conduction studies and electromyography of the involved extremity.
- Cranial neuropathy (single or multiple cranial nerves) can be produced by lesions in the cavernous sinus or base of skull
Other signs
- Anhidrosis: Variable degree of loss of sweating can be seen depending on the site of lesion. Central or preganglionic lesions tend to produce more noticeable anhidrosis. The sudomotor and vasomotor fibers to most of the face separate out at the superior cervical ganglion and anhidrosis is often not noticeable in postganglionic lesions.
- Harlequin sign: Impaired hemi-facial (or hemi-body) flushing seen in children with sympathetic denervation to the face.
- Cervical or abdominal mass may be seen in children with neuroblastoma.
Non-isolated Horner’s syndrome
Non-isolated Horner’s syndrome may accompany other neurologic or systemic deficits from disease processes listed above.
Isolated Horner’s syndrome
Isolated Horner’s syndrome, the patient, an acquaintance, or a health care provider may notice a difference in the palpebral aperture or pupillary size. Patients may also complain of ocular redness, nasal stuffiness and headache. Children with isolated Horner’s syndrome may present when parents notice a difference in eye color or impaired facial flushing.
Children with Horner’s syndrome
Additional signs and symptoms in children with Horner syndrome may include:
- Lighter iris color in the affected eye of a child under the age of 1
- Lack of redness (flushing) on the affected side of the face that would normally appear from heat, physical exertion or emotional reactions.
Horner’s syndrome diagnosis
Horner’s syndrome is a clinical diagnosis. Horner’s syndrome can be established clinically by an ocular examination.
- Horner’s syndrome is diagnosed clinically by observing ptosis (of upper and lower lids), miosis of the ptotic eye and demonstration of dilation lag in the affected eye.
Pharmacological confirmation tests can be performed in subtle cases. A targeted physical and neurological examination is a must to identify signs that may help localize the lesion and guide appropriate investigations.
Your doctor may administer a type of eyedrop that will cause significant dilation of the healthy eye and little dilation of the affected eye if Horner syndrome is caused by a third-order neuron abnormality — a disruption somewhere in the neck or above.
Pharmacologic tests
Your doctor, often an ophthalmologist, may also confirm a diagnosis by putting a drop in both eyes — either a drop that will dilate the pupil of a healthy eye or a drop that will constrict the pupil in a healthy eye. By comparing the reactions in the healthy eye with that of the suspect eye, your doctor can determine whether nerve damage is the cause of problems in the suspect eye.
- Topical Cocaine may be used to confirm Horner’s syndrome in subtle cases. Cocaine blocks reuptake of the neurotransmitter norepinephrine from the synaptic cleft and will cause dilation of the pupil with intact sympathetic innervation. One hour after instillation of two drops of 10% cocaine, the normal pupil dilates more than the Horner’s pupil, thus increasing the degree of anisocoria. It is becoming increasingly difficult to obtain cocaine eye drops due to increased regulations.
- Topical Apraclonidine is an alternative to topical cocaine to confirm Horner’s syndrome. Apraclonidine is an alpha adrenergic agonist. It causes pupillary dilation in the Horner’s pupil due to denervation supersensitivity while producing a mild pupillary constriction in the normal pupil presumably by down-regulating the norepinephrine release at the synaptic cleft. A reversal of anisocoria after instilling two drops of 0.5% apraclonidine is suggestive of Horner’s syndrome.
- Topical Hydroxyamphetamine is used to differentiate pre and postganglioninc Horner’s. Hydroxyamphetamine causes a release of norepinephrine from intact adrenergic nerve endings causing pupillary dilation. One hour after instillation of 1% hydroxyamphetamine eye drops dilation of both pupils indicate a lesion of the 1st or 2nd order neuron. If the smaller pupil fails to dilate it indicates a lesion of the 3rd order or postganglionic neuron.
Tests to identify the site of nerve damage
The prominence or nature of certain symptoms may help your doctor narrow the search for the cause of Horner syndrome. Your doctor may also conduct additional tests or order imaging tests to locate the lesion or abnormality disrupting the nerve pathway.
Your doctor may order one or more of the following imaging tests to locate the site of a probable abnormality causing Horner syndrome:
- Magnetic resonance imaging (MRI), a technology that uses radio waves and a magnetic field to produce detailed images
- Computerized tomography (CT), a specialized X-ray technology
- X-ray imaging
For children with Horner syndrome, a doctor may order blood and urine tests that are used to diagnose a tumor of the hormonal and nervous systems (neuroblastoma).
Horner’s syndrome treatment
Acute onset of painful Horner’s should be considered a neurological emergency and subject should be evaluated for dissection of the internal carotid artery as described below. These patients are at increased risk for cerebral infarction.
The first step in the management of a patient with Horner’s syndrome is to perform appropriate studies to identify the cause. Imaging is often indicated in new onset Horner’s syndrome unless it occurs in the setting of trauma or surgical manipulation. High-yield sites of imaging can be identified based on accompanying signs and symptoms. These may include amongst others radiologic evaluation of brain, cervical spinal cord, cerebral vasculature, head, neck and thorax.
Treatment depends on the etiology of Horner’s syndrome.
- Carotid artery dissection: Appropriate imaging modalities should be obtained emergently and may include MRI and MR angiography or CT angiography of the neck. Conventional angiogram remains the gold standard. Patients should be treated promptly by anticoagulation under the supervision of a neurologist.
- Neuroblastoma: Children with new Horner’s syndrome without obvious cause such as trauma should be evaluated for systemic malignancy particularly neuroblastoma with the help of the pediatrician. They should be evaluated for neck and abdominal masses and tested for urinary catecholamine metabolites. Appropriate radiological evaluation of head, neck and chest should be obtained in consultation with the pediatrician.
- Brainstem or myelopathic lesions: Patients with brainstem or myelopathic signs require imaging of the brain and the spinal cord typically by MR imaging. Appropriate sequences should be ordered based on the suspected etiology. Cavernous sinus and sellar region should be evaluated in patients with Horner’s syndrome with ophthalmoparesis especially isolated sixth cranial nerve palsy. These patients should be under the care of a neurologist or neurosurgeon for treatment of the underlying causes.
- Thoracic malignancy: Isolated spontaneous onset Horner without additional neurologic signs should prompt imaging of the neck and thorax for lesions of the pulmonary apex or the paravertebral area. Contrasted CT or MR scans should be obtained based on the suspected etiology.
- Blepharoptosis: Once life-threatening conditions have been ruled out and the patient is stable, visually symptomatic ptosis can be managed surgically. The surgical approach varies on surgeon preference. Since characteristically the levator palpebrae function is normal in Horner’s syndrome, surgery typically involves strengthening the action of the levator muscle. The approach may include either aponeurotic advancement or Müller’s muscle- conjunctival resection.






