Contents
What is fibrocystic breast disease
Fibrocystic breast disease is a common benign breast disease marked by benign (not cancer) changes in breast tissue. Fibrocystic breast changes is a condition characterized by ‘lumpy’ breasts, associated with pain and tenderness that fluctuate with the menstrual cycle. Many breast lumps are due to fibrocystic changes. The lumps can be caused by a collection of fibrous tissue in an area of the breast. Fibrous tissue is the same tissue that ligaments and scar tissue are made of.
The lumps can also be caused by one or more collections of fluid in an area of the breast. These are called cysts.
Sometimes women have areas of fibrosis and cysts in the same breast.
More than half of women experience fibrocystic breast changes at some point in their lives. Fibrocystic breast changes are most common in women of childbearing age, but they can affect women of any age. Fibrocystic breast changes can happen in different parts of the breast and in both breasts at the same time. Cysts most often occur in women in their 40s.
In fact, medical professionals have stopped using the term “fibrocystic breast disease” and now simply refer to “fibrocystic breasts” or “fibrocystic breast changes” because having fibrocystic breasts isn’t really a disease. Breast changes categorized as fibrocystic are considered normal.
Fibrocystic breast diagnosis often involves exclusion of other significant breast diseases. Usually, fibrocystic breast changes are diagnosed when women go to their doctor with symptoms, such as breast lumps, swelling, and tenderness or pain.
You might have an ultrasound, which usually can clearly show whether the lump is a cyst. If the ultrasound isn’t clear, your doctor or nurse might need to take a small sample of cells called a biopsy.
Fibrocystic breast symptoms
Your breasts might feel lumpy. Some women might have a clear or slightly cloudy discharge from the nipple.
- Breast Cysts
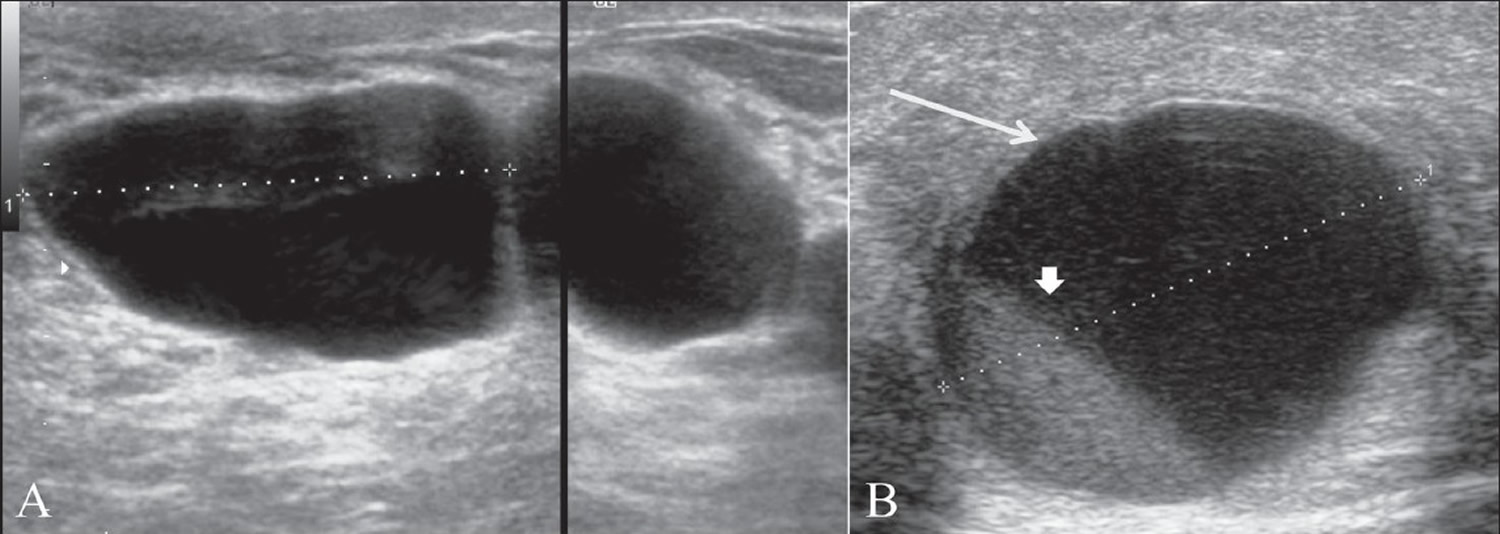
Breast cysts are the commonest cause of breast lumps in women between 35 and 50 years of age 3. A breast cysts occurs when fluid accumulates due to obstruction of the extralobular terminal ducts, either due to fibrosis or because of intraductal epithelial proliferation. A cyst is seen on ultrasound as a well-defined, round or oval, anechoic structure with a thin wall (see Figure 3A below). They may be solitary or multiple (see Figure 3B below).
Breast cysts tend to be round or oval, movable lumps and can be tender to the touch. The cysts might get bigger and become painful and more noticeable just before your period.
Breast cysts start out from fluid building up inside the breast glands. They start as tiny, microscopic cysts (microcysts) that are too small to feel. They can only be seen when breast tissue is looked at under a microscope. Larger cysts are called macrocysts. These are easy to feel and can be up to 1 or 2 inches across. As the cysts grow the breast tissue around them can stretch and be tender or painful.
- Breast Fibrosis
Areas of fibrosis can feel rubbery, firm, or hard to the touch.
Although many women with fibrocystic breasts don’t have symptoms, some women experience breast pain, breast swelling or discomfort, sensitive nipples and itching, tenderness and lumpiness — especially in the upper, outer area of the breasts. Breast symptoms tend to be most bothersome just before menstruation. Fibrocystic breast is rare in women after menopause unless they are taking estrogen. Simple self-care measures can usually relieve discomfort associated with fibrocystic breasts.
Most fibrocystic breast changes are normal. However, make an appointment with your doctor if:
- You find a new breast lump or area of prominent thickening
- You have specific areas of continuous or worsening breast pain
- Breast changes persist after your period
- Your doctor evaluated a breast lump but now it seems to be bigger or otherwise changed
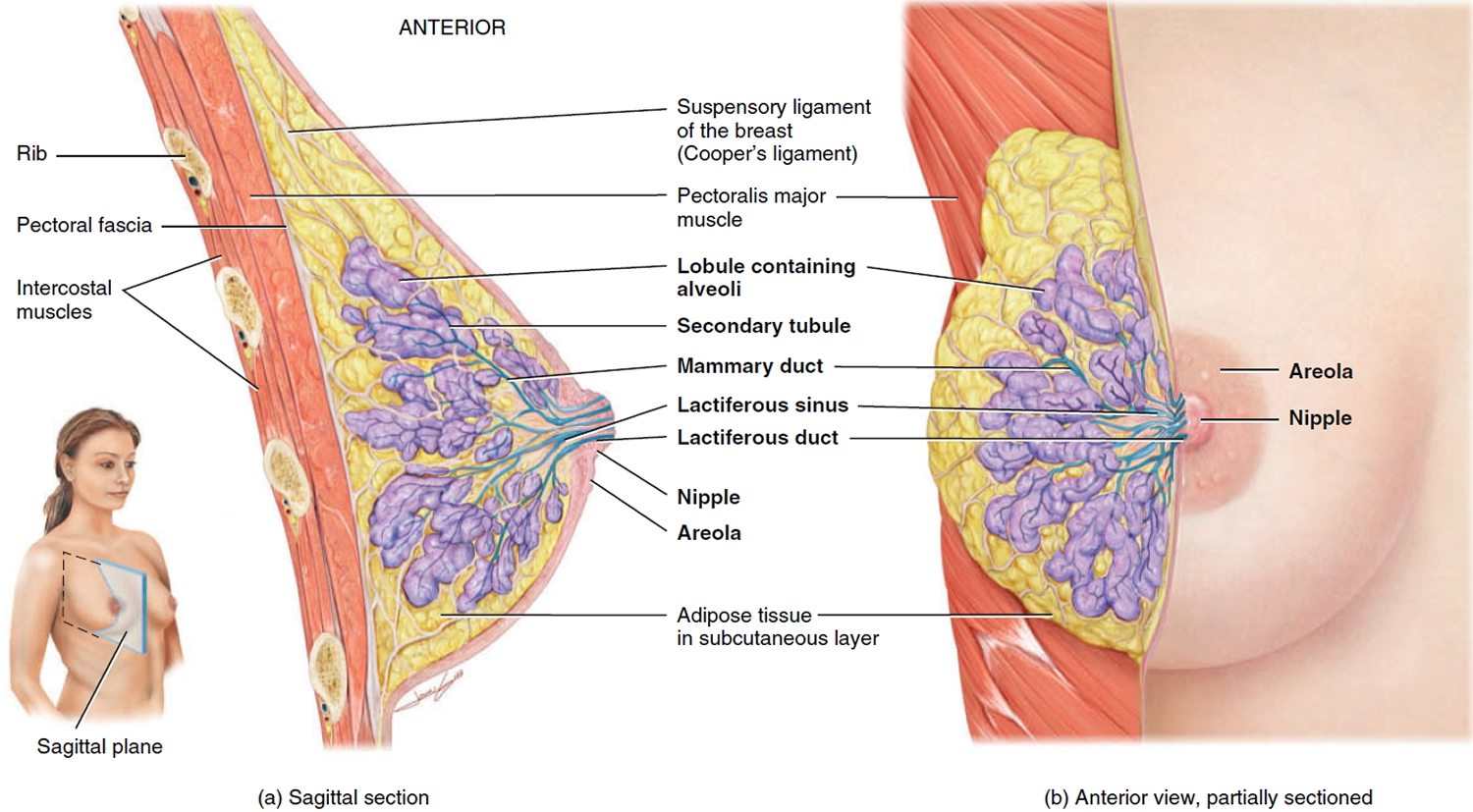
Figure 1. Normal breast (female)
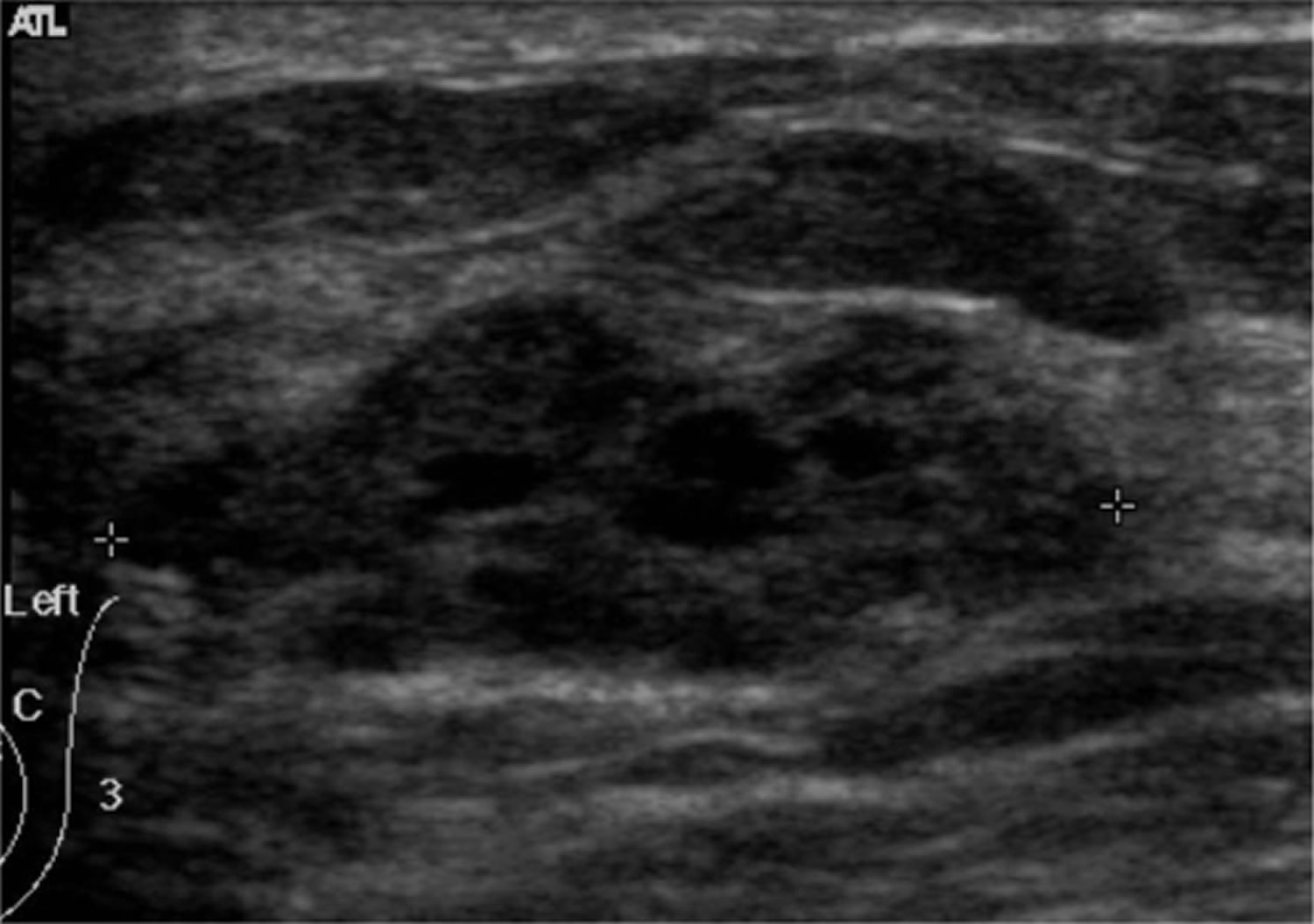
Figure 2. Fibrocystic breast ultrasound
Note: The ultrasound appearance of the breast in this condition is extremely variable since it depends on the stage and extent of morphological changes.
Figure 3. Fibrocystic breast ultrasound (breast cysts)
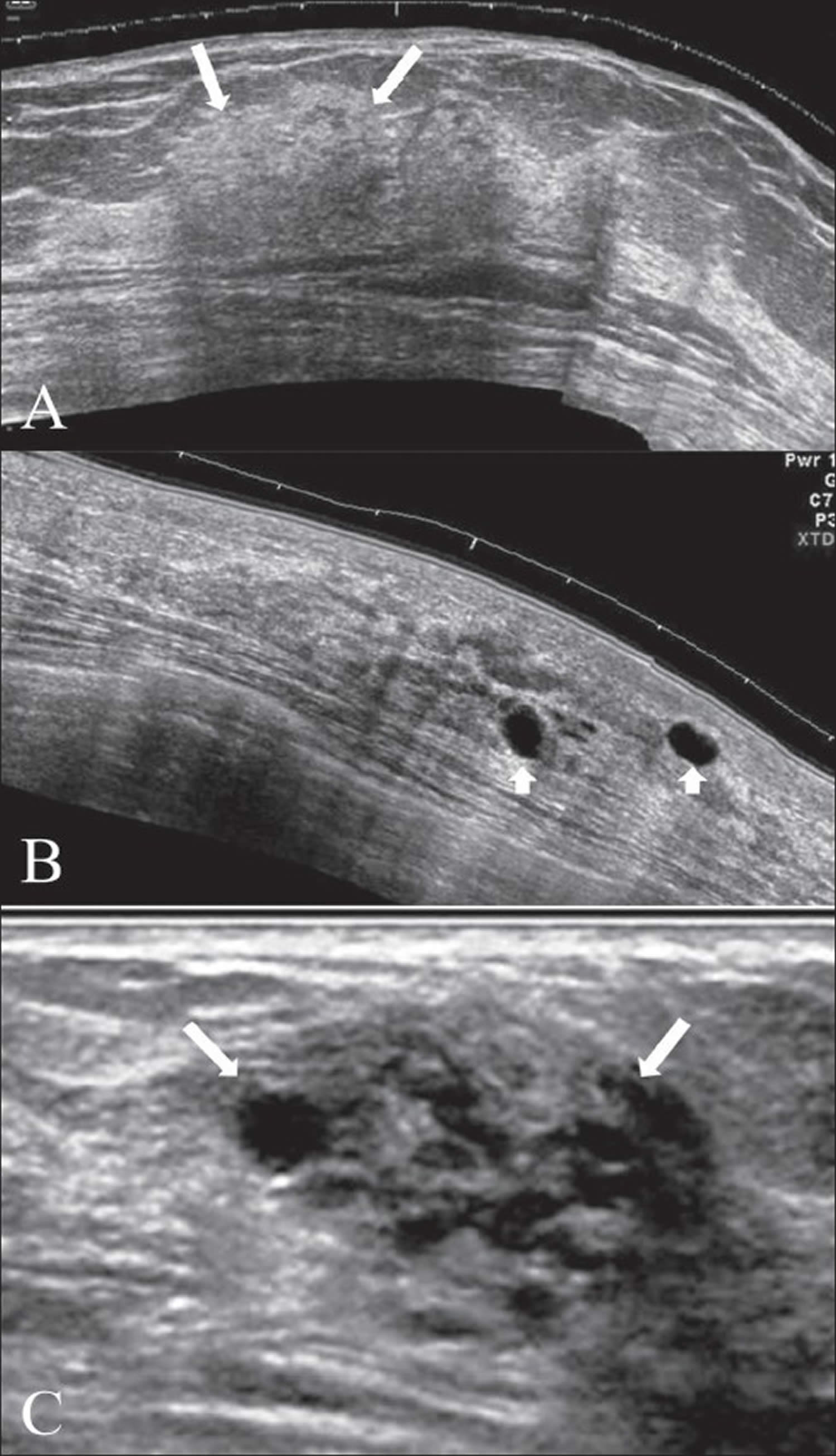
Figure 4. Fibrocystic breast ultrasound
Note: In the early stages, the ultrasound appearance may be normal, even though lumps may be palpable on clinical examination. There may be focal areas of thickening of the parenchyma, with or without patchy increase in echogenicity [A]. Discrete single cysts or clusters of small cysts may be seen in some [B] and [C]. Focal fibrocystic changes may appear as solid masses or thin-walled cysts. About half of these solid masses are usually classified as indeterminate and will eventually require a biopsy 4.
Fibrocystic breast disease causes
The exact cause of fibrocystic breast changes isn’t known, but experts suspect that reproductive hormones — especially estrogen — play a role.
Fluctuating hormone levels during your menstrual cycle can cause breast discomfort and areas of lumpy breast tissue that feel tender, sore and swollen. Fibrocystic breast changes tend to be more bothersome before your menstrual period, and the pain and lumpiness tends to clear up or lessen once your menstrual period begins.
When examined under a microscope, fibrocystic breast tissue includes distinct components such as:
- Fluid-filled round or oval sacs (cysts)
- A prominence of scar-like fibrous tissue (fibrosis)
- Overgrowth of cells (hyperplasia) lining the milk ducts or milk-producing tissues (lobules) of the breast
- Enlarged breast lobules (adenosis)
Risk factors for fibrocystic breast
Having fibrocystic breasts doesn’t increase your risk of breast cancer.
Fibrocystic breast symptoms
Fibrocystic breast disease symptoms
Signs and symptoms of fibrocystic breasts may include:
- Breast lumps or areas of thickening that tend to blend into the surrounding breast tissue
- Generalized breast pain or tenderness
- Breast lumps that fluctuate in size with the menstrual cycle
- Green or dark brown nonbloody nipple discharge that tends to leak without pressure or squeezing
- Breast changes that are similar in both breasts
- Monthly increase in breast pain or lumpiness from midcycle (ovulation) to just before your period
Fibrocystic breast changes occur most often in women in their 20s to 50s. Rarely do postmenopausal women experience fibrocystic breast changes, unless they’re on hormone therapy.
Fibrocystic breast diagnosis
Tests to evaluate your condition may include:
- Clinical breast exam. Your doctor checks for unusual areas by visually and manually examining your breasts and the lymph nodes located in your lower neck and underarm area. If your medical history and the clinical breast exam indicate normal breast changes, you may not need additional tests. If your doctor finds a new lump and suspects fibrocystic changes, you may come back a few weeks later, after your menstrual period, to have another breast exam. If the changes persist, you’ll likely need a mammogram or ultrasound.
- Mammogram. If your doctor detects a breast lump or prominent thickening in your breast tissue, you need a diagnostic mammogram — an X-ray exam that focuses on a specific area of concern in your breast. The radiologist closely examines the area of concern when interpreting the mammogram.
- Ultrasound. An ultrasound uses sound waves to produce images of your breasts and is often performed along with a mammogram. If you’re younger than age 30, you might have an ultrasound instead of a mammogram. Ultrasound is better for evaluating a younger woman’s dense breast tissue — tissue tightly packed with lobules, ducts and connective tissue (stroma). Ultrasound can also help your doctor distinguish between fluid-filled cysts and solid masses.
- Fine-needle aspiration. For a breast lump that feels a lot like a cyst, your doctor may try fine-needle aspiration to see if fluid can be withdrawn from the lump. This helpful procedure can be done in the office. A fine-needle aspiration may collapse the cyst and resolve discomfort.
- Breast biopsy. If a diagnostic mammogram and ultrasound are normal, but your doctor still has concerns about a breast lump, you may be referred to a breast surgeon to determine whether you need a surgical breast biopsy. A breast biopsy is a procedure to remove a small sample of breast tissue for microscopic analysis. If a suspicious area is detected during an imaging exam, your radiologist may recommend an ultrasound-guided breast biopsy or a sterotactic biopsy, which uses mammography to pinpoint the exact location for the biopsy.
Fibrocystic breast disease treatment
You might not need any treatment for fibrocystic breast disease. But you might have appointments every now and again with a doctor or nurse to check the lumps. Cysts can go away on their own after a while.
If it isn’t clear what the lump is or if it is causing soreness or pain, your doctor or nurse might put a thin needle into it to drain fluid. This can get rid of a cyst and also get rid of the soreness.
Rarely, surgery may be needed to remove a persistent cyst-like lump that doesn’t resolve after repeated aspiration and careful monitoring or has features that concern your doctor during a clinical exam.
If you have mild soreness due to fibrosis, you might find that it helps to:
- Wear well-fitted, supportive bras
- Apply gentle heat to the area
- Take mild painkillers such as acetaminophen (Tylenol, others) or nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others) or prescription medication.
- Oral contraceptives, which lower the levels of cycle-related hormones linked to fibrocystic breast changes.
Fibrocystic breast disease diet
Some women have said that their breast symptoms improve if they avoid caffeine found in coffee, tea, chocolate, and some soft drinks. There is no scientific evidence that caffeine causes the symptoms, but it might be worth trying.
Fibrocystic breast home remedies
You might find relief from symptoms of fibrocystic breasts through one of these home remedies:
- Wear a firm support bra, fitted by a professional, if possible.
- Wear a sports bra during exercise and while sleeping, especially when your breasts are extra sensitive.
- Limit or avoid caffeine, a dietary change many women report as helpful, although medical studies of caffeine’s effect on breast pain and other premenstrual symptoms have been inconclusive.
- Decrease the fat in your diet, which may decrease breast pain or discomfort associated with fibrocystic breasts.
- Reduce or stop taking hormone therapy if you’re postmenopausal — but be sure to talk to your doctor before making any change in your prescription medications.
- Use a heating pad or warm water bottle to relieve your discomfort.
Alternative medicine
Vitamins and dietary supplements may lessen breast pain symptoms and severity for some women. Ask your doctor if one of these might help you — and ask about doses and any possible side effects:
- Evening primrose oil. This supplement may change the balance of fatty acids in your cells, which may reduce breast pain.
- Vitamin E. Early studies showed a possible beneficial effect of vitamin E on breast pain in premenstrual women who experience breast pain that fluctuates during the menstrual cycle. In one study, 200 international units (IU) of vitamin E taken twice daily for two months improved symptoms in women with cyclic breast pain. There was no additional benefit after four months. For adults older than 18 years, pregnant women and breast-feeding women, the maximum dose of vitamin E is 1,000 milligrams daily (or 1,500 IU).
If you try a supplement for breast pain, stop taking it if you don’t notice any improvement in your breast pain after a few months. Try just one supplement at a time so that you can clearly determine which one helps alleviate the pain — or not.
- Santen RJ, Mansel R. Benign breast disorders. N Engl J Med. 2005;353:275-285. http://www.nejm.org/doi/full/10.1056/NEJMra035692[↩]
- Marchant DJ. Benign breast disease. Obstet Gynecol Clin North Am. 2002;29:1-20. https://www.ncbi.nlm.nih.gov/pubmed/11892859[↩]
- Howlett DC, Marchbank NDP, Allan SM. Sonographic assessment of symptomatic breast – a pictorial review. J Diagnostic Radiography & Imaging 2003;5:3-12.[↩]
- Shetty MK, Shah Y. Sonographic Findings in Focal Fibrocystic Changes of the Breast. Ultrasound Quarterly 2002;18;35-40.[↩]