Contents
What is fodmap
FODMAP stands for “Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols“. A diet low in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) – low FODMAP diet. Since ingestion of FODMAPs increases the delivery of readily fermentable substrates and water to the distal small intestine and colon—which results in luminal distention and gas—the reduction of FODMAPs in a patient’s diet may improve functional gastrointestinal symptoms 1.
These fermentable short-chain carbohydrates are prevalent in the diet.
- Oligosaccharides: fructans and galactooligosaccharides (GOS)
- Disaccharides: lactose
- Monosaccharides: fructose
- Polyols: sorbitol and mannitol
Researchers suggest that the small intestine does not absorb FODMAPs very well. They increase the amount of fluid in the bowel. They also create more gas. That’s because bacteria in the colon they are easily fermented by colonic bacteria. The increased fluid and gas in the bowel leads to bloating and changes in the speed with which food is digested. This results in gas, pain and diarrhea. Eating less of these types of carbohydrates should decrease these symptoms.
So far, studies have shown that a low FODMAP diet has a beneficial effect in a majority of patients with Irritable Bowel Syndrome (IBS) symptoms 2. One study even found that 76% of Irritable Bowel Syndrome (IBS) patients following the diet reported improvement with their symptoms. Probiotics also have great potential in the management of Irritable Bowel Syndrome (IBS); however, it is still unclear which strains and doses are the most beneficial. Further research is needed on the effect of different fibers or combinations of fibers, in Irritable Bowel Syndrome (IBS).
What is Irritable bowel syndrome (IBS)
Irritable bowel syndrome (IBS) is a condition that affects the functioning of the bowel. The main symptoms are abdominal pain or discomfort that is often relieved by passing wind or faeces, stomach bloating, and chronic diarrhoea or constipation (or alternating between the two). Irritable bowel syndrome (IBS) sufferers may experience multiple symptoms of diarrhea, constipation, abdominal pain, abdominal distention, excessive flatulence, bloating, a continual urge to defecate, urgency to get to a toilet, incontinence, a sensation of incomplete evacuation, straining with a bowel movement, hard / lumpy stools, or even an inability to have a bowel movement at all.
There are several subtypes of IBS.
- IBS-D: Diarrhea predominant
- IBS-C: Constipation predominant
- IBS-A or IBS-M: Alternating, or mixed, between constipation and diarrhea
- IBS-PI: Post Infectious IBS
- PDV-IBS: Post Diverticulitis IBS
These symptoms can be embarrassing, inconvenient and distressing. Fortunately, IBS does not cause permanent damage to the bowel and it does not cause other serious diseases like bowel cancer.
Irritable Bowel Syndrome is found predominantly in women in a 2:1 ratio versus men.
If you have IBS, then an episode can be triggered by an infection, stress, food intolerance or particular medicines.
The exact cause of IBS is unknown. It’s probably due to many factors, including the nerves in the bowel being more sensitive than usual (allowing the person to feel sensations they wouldn’t normally feel), abnormal contractions in the bowel, chronic inflammation of the bowel and psychological factors.
The main feature of IBS is abdominal pain associated with a change in bowel habits.
Symptoms to look for include:
- recurring episodes of diarrhea or constipation
- symptoms that alternate between diarrhea and constipation
- bloating
- pain or discomfort that is relieved by passing wind or going to the toilet
- symptoms are more common in women and may be worse around menstruation or at times of stress.
IBS does not cause bleeding from the back passage.
Irritable bowel syndrome (IBS) is best defined by what it is NOT!
- IBS is NOT an anatomical or structural defect.
- IBS is NOT an identifiable physical or chemical disorder.
- IBS is NOT a cancer and will not cause cancer.
- IBS will NOT cause other gastrointestinal diseases.
Patients suffering from IBS should not be worried about it leading to other serious diseases. The major problem with IBS is not because it causes death or serious disease, but because it changes the quality of life for the patient.
Irritable bowel syndrome is not associated with serious medical consequences. People with IBS tend to live long and in some studies, somewhat longer than individuals who do not have IBS. IBS is not associated with other serious GI diseases, such as inflammatory bowel disease (Crohn’s disease or ulcerative colitis) or colon cancer. The presence of IBS does not put extra stress on the other organs in the body such as the heart, liver or kidneys. Overall the prognosis for irritable bowel syndrome is excellent.
A subset of Irritable Bowel Syndrome sufferers may have co-morbidities with other digestive health disorders namely; GERD (gastroesophageal reflux disease) / Heartburn, Dyspepsia, Chronic Constipation, Chronic Abdominal Pain, Fibromyalgia, Pelvic pain or perhaps Crohn’s Disease and Ulcerative Colitis, known collectively as Inflammatory Bowel Disease (IBD). For instance, 29% of gastroesophageal reflux disease (GERD) patients have Chronic Constipation. Diagnosis can shift from one motility disorder to another over time; however, co-morbidity in IBS may be due to a general amplification of symptom reporting and physician consultation rather than a direct association. A research study illustrated that patient education in diet, exercise, and stress management showed significant improvement in pain and symptoms at 1 and 6 months of treatment. An educational approach and appropriate use of medications should be components of a physician-based IBS treatment plan.
IBS is usually diagnosed based on your symptoms and your medical history. There is no medical test that can be used to confirm a diagnosis, although tests (such as a blood test or a colonoscopy) may be required to rule out other conditions.
Causes of Irritable Bowel Syndrome
There are many theories about what exactly causes IBS: problems with the nerves or muscles in the gut, an overgrowth of certain bacteria in the small intestine or a change in bacteria in the colon, an inability to digest certain foods, or stomach or bowel inflammation. Some people have symptoms every day, while others experience long symptom-free periods. IBS does not lead to serious disease, but it does significantly affect your quality of life.
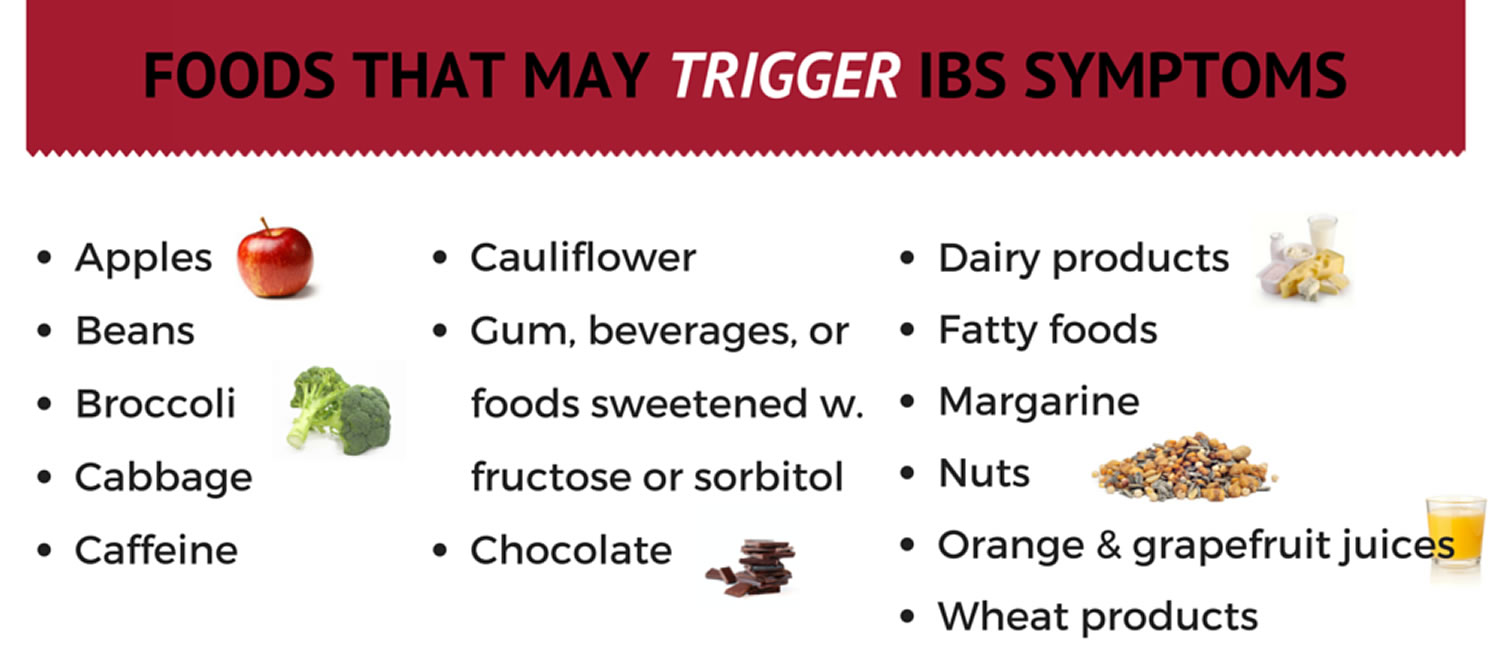
While doctors don’t know what causes IBS, they do know that flare-ups are often triggered by food, caffeine, stress, carbonated drinks, artificial sugars, or infectious diarrhea. The more IBS episodes you have, the more sensitive your gut becomes to triggers.
How is IBS treated ?
It is important to have a doctor who will carefully explain your condition, answer your questions, and work with you to develop a management plan suitable for your individual needs.
Managing IBS may include one or all of the following:
- reassurance that the symptoms are not due to cancer
- changing your lifestyle and diet
- reviewing medication that might aggravate diarrhea or constipation
- a good healthy diet
- dietary fiber.
Some people choose to take medicines to treat their symptoms when they flare up. These may include:
- anti-diarrhoeal medicines
- painkillers
- constipation treatments
- antispasmodics (to ease cramping)
- antidepressants (which are used to treat pain and depression).
Physiotherapy can be helpful in some cases to teach you how to use your muscles to control your bowel function more effectively.
Your doctor will also work with you to discover if psychological issues like anxiety, depression or stress are a problem for you. In some cases it may be beneficial to see a psychologist or counsellor who can teach you strategies for dealing with these issues and for coping with IBS.
Changing your diet
In past years IBS was treated from the perspective that it was a “motility disorder”. The use of fiber supplementation to improve intestinal motility or movement was a common recommendation. While some studies have questioned whether fiber supplementation alone is helpful for the treatment of IBS and its symptoms, there are other good reasons to consume a high fiber diet. High fiber diets are associated with lower blood sugar, lower cholesterol as well as a lower tendency to form diverticula or outpouchings of the colon. Moreover, some patients with IBS report having a good result with a high fiber diet. Certainly every patient should include at least 25 grams of fiber in their diet every day.
There is no ‘one size fits all’ diet for IBS. However, dietary changes can often relieve IBS symptoms.
It may help to keep a food diary so you can identify any foods that make your symptoms worse.
It can also help to modify the amount and type of fiber in your diet:
- If you have IBS with constipation, it can help to eat more soluble fiber and drink more water
- If you have IBS with diarrhea, it can help to cut down on insoluble fiber.
In some cases, avoiding a particular food or food group might help – examples include gluten, caffeine, alcohol, spicy foods, high fat foods or foods that cause excessive bloating such as beans, lentils or certain vegetables.
Australian researchers have recently developed a special diet that may help control IBS symptoms in some people. It’s called the FODMAP diet, and it involves restricting your intake of certain dietary carbohydrates (sugars) that are poorly absorbed by the bowel.
Before making any major changes to your diet it is a good idea to talk to your doctor or a dietitian.
Low Fodmap Diet
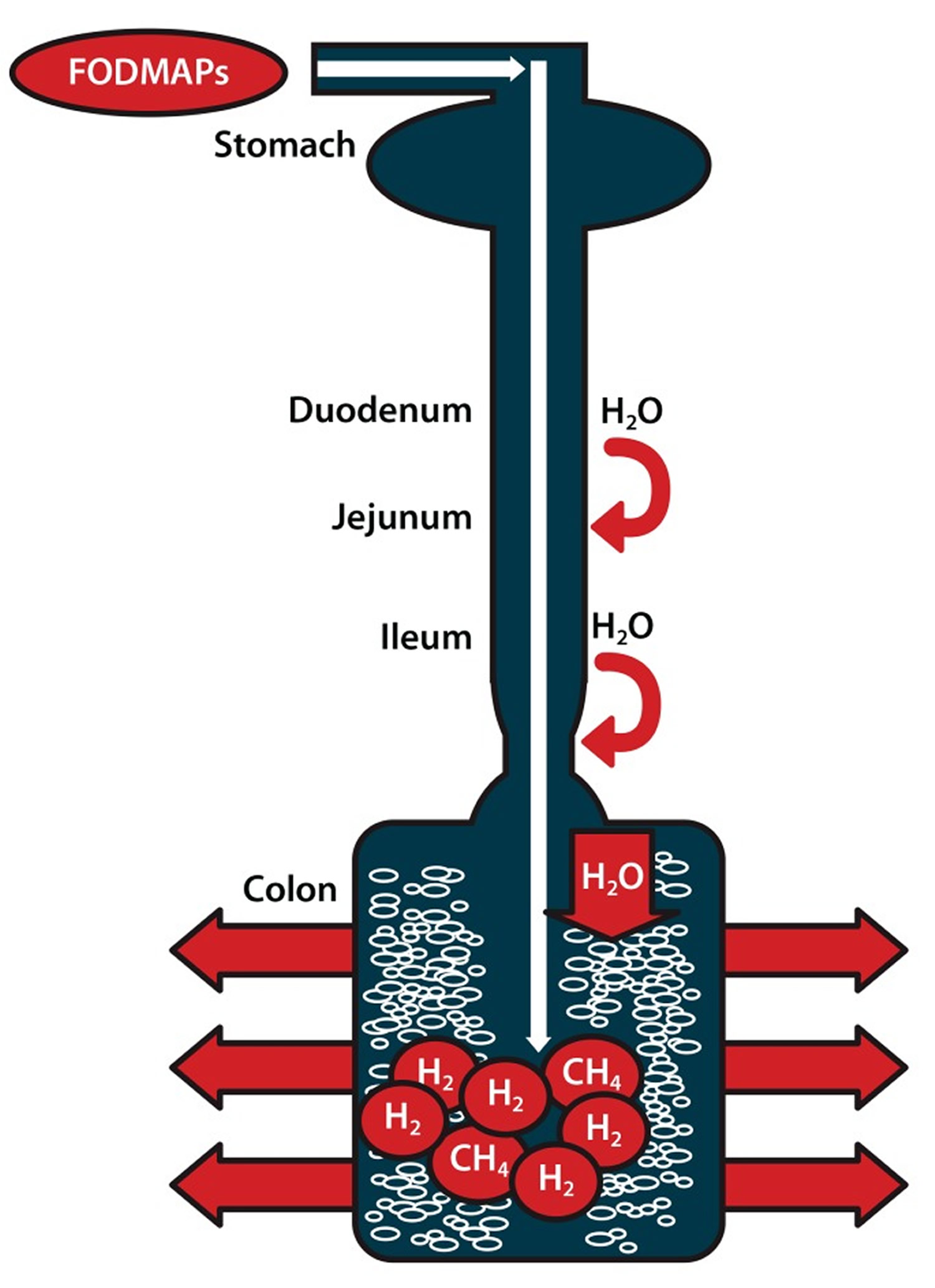
FODMAP stands for Fermentable, Oligo-, Di-, Mono-saccharides And Polyols. FODMAPs are short-chain carbohydrates (sugars) that are highly fermentable (to ferment, is to go through a chemical change that results in alcohol) and poorly absorbed during digestion 3. The acronym FODMAPs was created to describe poorly absorbed, short-chain carbohydrates that can lead to excessive fluid and gas accumulation, resulting in bloating, abdominal pain, and distention (Figure 1).
The Low FODMAP diet was developed by researchers at Monash University more than five years ago, in Australia, by Susan Shepherd and Peter Gibson. This diet eliminates certain foods to improve the symptoms of functional gut disorders (FGD). Irritable bowel syndrome (IBS), a type of FGD, may be helped by this diet. IBS is the most commonly diagnosed gastrointestinal condition and over half of patients with IBS associate a trigger in their symptoms with eating a meal 4. The Monash team, led by Professor Peter Gibson, provided the first evidence that a Low FODMAP diet improves IBS symptoms. Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder affecting one in seven Australian adults and approximately 35 million Americans are impacted by IBS including many in Europe and many in Asian countries. IBS is characterised by chronic and relapsing symptoms; lower abdominal pain and discomfort, bloating, wind, distension and altered bowel habit (ranging from diarrhoea to constipation) but with no abnormal pathology. The diagnosis of IBS should be made by a medical practitioner.
FODMAPs are found in a wide variety of foods, including those containing lactose, fructose in excess of glucose, fructans, galacto-oligosaccharides, and polyols (sorbitol, mannitol, xylitol, and maltitol). All FODMAPs have poor absorption and rapid fermentation, and they are comprised of small, osmotically active molecules. FODMAPs are poorly absorbed for a number of reasons, including the absence of luminal enzymes capable of hydrolyzing the glycosidic bonds contained in carbohydrates, the absence or low activity of brush border enzymes (eg, lactase), or the presence of low-capacity epithelial transporters (fructose, glucose transporter 2 [GLUT-2], and glucose transporter 5 [GLUT-5]). Fructose, which is an important FODMAP in the Western diet, is absorbed across villous epithelium through low-capacity, carrier-mediated diffusion involving GLUT-5. The absorption of free fructose is markedly enhanced in the presence of glucose via GLUT-2. Therefore, if fructose is present in excess of glucose, the risk of fructose malabsorption is increased. In addition, some molecules, such as polyols, are too large for simple diffusion. The fermentation rate is determined by the chain length of the carbohydrate 5.
For example, oligosaccharides are rapidly fermented, compared to polysaccharides. Fermentation results in the production of carbon dioxide, hydrogen, and/or methane gas. Finally, small, osmotically active molecules draw more water and other liquid into the small bowel. Given these properties, a diet low in FODMAPs has become a potential therapy for IBS patients.
When FODMAPs reach the colon (large intestine), bacteria ferment these sugars, turning them into gas and chemicals. This stretches the walls of the colon, causing abdominal bloating, distension, and pain or cramping in many people. Other symptoms, such as diarrhea, constipation, and nausea, are also common side effects of FODMAP carbohydrates. Not everyone has the same reaction to FODMAPs. Ethnicity, genetics, and environmental factors (such as an individual’s microbiome, motility, immune system, and sensory system) may play a part in your body’s ability to tolerate these carbohydrates.
Figure 1. FODMAPs in your gut
Note: Ingested fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) are poorly absorbed in the small intestine. Their small molecular size results in an osmotic effect, drawing water (H20) through to the large intestine. FODMAPs are then fermented by colonic microflora, producing hydrogen (H2) and/or methane gas (CH4). The increase in fluid and gas leads to diarrhea, bloating, flatulence, abdominal pain, and distension.
[Source 1]What symptoms may be associated with FODMAPS ?
As FODMAPs are poorly absorbed during the digestive process, they may pass to the large intestine (colon), where they are rapidly fermented by the bacteria that normally live in the colon. This makes chemicals called short chain fatty acids, as well as gas. This, in turn, leads to changes in the acidity and types of bacteria in the colon. The colon expands, which can lead to pain, bloating, and changes in bowel habits.
Diets rich in FODMAPs may increase symptoms in patients with functional gut disorders (FGD) or irritable bowel syndrome (IBS). However, the FODMAPs themselves are not the root of the problem. For that reason, patients may need to include other options to treat their symptoms. This may include medicine, exercise, meditation, hypnotherapy, etc.
When is a Low-FODMAP diet recommended ?
Despite limited data, implementation of a low-FODMAP diet should be considered in patients with IBS, particularly those in whom food is a trigger for symptoms.
Eliminating or restricting FODMAPs from the diet may greatly improve symptoms of functional gut disorders (FGD). In Australia, a Low-FODMAP diet is the main treatment for irritable bowel syndrome (IBS). It was adopted by their National Therapeutic Guidelines. The Low-FODMAP diet can be adjusted to meet personal food and lifestyle preferences. Following a personally developed Low-FODMAP plan does not cure IBS, but it may lead to drug-free management of symptoms and better quality of life. As with any diet, it is important to discuss with your doctor and working with a gastrointestinal trained dietician is also useful.
A number of studies suggest that limiting FODMAPs in the diet leads to improved symptoms in one-half to two-thirds of patients who follow this diet. Many patients see improvement in 1-2 weeks, though some may need to wait up to 4 weeks. Bloating and abdominal pain are the most likely symptoms to improve. Diarrhea is more likely to improve than constipation. If there is no improvement after 4 weeks, it is likely not worth continuing this diet.
A Low-FODMAP diet is not recommended for people without gastrointestinal symptoms. Also, if your IBS symptoms improve on the Low-FODMAP diet, you should eventually re-introduce FODMAPs, one at a time, to identify foods that trigger symptoms and those that do not. This will allow a more diverse diet. Keeping a personal food diary may help simplify this process
Implementation of a low-FODMAP diet is best done with the help of a dietician during a one-to-one consultation so that the dietician can understand the patient’s symptoms; this process also ensures that any diet modifications are individualized and still provide a balanced diet. A diet history should be taken to determine the composition of FODMAPs in an individuals diet. Education can then be tailored appropriately rather than focusing on FODMAPs that may never be consumed. Lists of food substitutions can help patients understand what they can and cannot eat (Table 1) 6. For good symptom control, individuals should restrict their total FODMAP load for 6-8 weeks. After this time, the diet may be modified to be less restrictive based on symptom response.
However, there are also several limitations to low-FODMAP diets. Most foods do not list their FODMAP content. In addition, the cutoff levels for FODMAP content are not clearly defined. When this diet was first examined, cutoff values were proposed based on foods that patients identified to be triggers for their symptoms. Foods and beverages with the following amounts of FODMAPs were considered to have risk for inducing symptoms: more than 0.5 g of fructose in excess of glucose per 100 g, more than 3 g of fructose in an average serving quantity regardless of glucose amount, and more than 0.2 g of fructans per serving 6. Although a low-FODMAP diet has been shown to be helpful in patients with IBS or other functional bowel disorders, further randomized controlled trials should be conducted.
Table 1. Foods High in Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols (FODMAPs) and Suitable Alternatives
| FODMAP | Foods high in FODMAPs | Suitable alternatives low in FODMAPs |
|---|---|---|
| Excess fructose | Fruits: apple, clingstone peach, mango, nashi pear, pear, sugar snap pea, tinned fruit in natural juice, watermelon | Fruits: banana, blueberry, cantaloupe, carambola, durian, grape, grapefruit, honeydew melon, kiwi, lemon, lime, orange, passion fruit, pawpaw, raspberry, strawberry, tangelo |
| Honey sweeteners: fructose, high-fructose corn syrup | Honey substitutes: golden syrup, maple syrup | |
| Large total fructose dose: concentrated fruit sources, large servings of fruit, dried fruit, fruit juice | Sweeteners: any sweeteners except polyols | |
| Lactose | Milk: regular and low-fat cow, goat, and sheep milk; ice cream | Milk: lactose-free milk, rice milk Ice cream substitutes: gelato, sorbet |
| Yogurts: regular and low-fat yogurts | Yogurts: lactose-free yogurts | |
| Cheeses: soft and fresh cheeses | Cheeses: hard cheeses | |
| Oligosaccharides (fructans and/or galactans) | Vegetables: artichoke, asparagus, beetroot, broccoli, Brussels sprout, cabbage, fennel, garlic, leek, okra, onion, pea, shallot | Vegetables: bamboo shoot, bok choy, capsicum, carrot, celery, chives, choko, choy sum, corn, eggplant, green bean, lettuce, parsnip, pumpkin, silverbeet, spring onion (green part only) |
| Cereals: rye and wheat cereals when eaten in large amounts (eg, biscuit, bread, couscous, cracker, pasta) | Onion/garlic substitutes: garlic-infused oil | |
| Legumes: baked bean, chickpea, lentil, red kidney bean | Cereals: gluten-free and spelt bread/cereal products | |
| Fruits: custard apple, persimmon, rambutan, watermelon, white peach | Fruit: tomato | |
| Polyols | Fruits: apple, apricot, avocado, cherry, longon, lychee, nashi pear, nectarine, peach, pear, plum, prune, watermelon | Fruits: banana, blueberry, cantaloupe, carambola, durian, grape, grapefruit, honeydew melon, kiwi, lemon, lime, orange, passion fruit, pawpaw, raspberry |
| Vegetables: cauliflower, mushroom, snow pea | ||
| Sweeteners: isomalt, maltitol, mannitol, sorbitol, xylitol, and other sweeteners ending in “-ol” | Sweeteners: glucose, sugar (sucrose), other artificial sweeteners not ending in “-ol” |
FODMAP Food List
Table 2. FODMAP Food List
Food | Avoid | Suitable |
| Lactose | Dairy whey and high-lactose containing milks such as cow, goat, sheep, chocolate, buttermilk, and condensed milk, and whipped cream. Ice cream, cow’s milk-based yogurt, brie, cottage cheese, ricotta, and sour cream. | Gelato or sorbet (though watch fructose content) and lactose-free yogurts. Aged hard cheeses tend to be easier to tolerate. Cheddar, Colby, parmesan, and mozzarella. Greek yogurt. Limit: Butter, margarine, sour cream, half and half, cream cheese, Swiss cheese, goat cheese, feta cheese, cheddar, parmesan, and mozzarella contain lactose, although at lower amounts. |
| Non-Dairy Milk Alternatives | Soy milk contains galactans and should be avoided as well, coconut milk, soy products, hummus, beans, and lentils. | Lactose- free or lactaid milk, rice milk, almond milk, almond butter, and cashew milk. |
| Fructose / Sweeteners | Honey, agave, apples, cherries, dates, guava, honeydew melon, lychee, mandarin oranges, mangoes, peaches, pears, persimmons, star fruit, canned fruit in natural juices, dried fruits and less ripe fruits, corn syrup, high fructose sweeteners, coconut milk, fruit pastes (i.e. chutney, plum sauce, barbeque sauce, ketchup), rosé wine, port, and sherry | Maple syrup, jams, marmalades, vegemite, table sugar, bananas, blackberries, blueberries, boysenberries, cranberries, grapefruit, kiwis, kumquats, lemons, limes, passion fruit, raspberries, and strawberries. Limit: grapes, oranges, papaya, pineapple, and watermelon. |
| Fructans | ||
| Starches | Bread, pasta, semolina, flour tortillas, wheat-based bread and breadcrumbs. Wheat-based cereals, crackers, cookies, cakes, pasta, and pastries. Beer. | Corn breads, gluten- free breads, pastas, cereals, as well as corn flakes, oatmeal, potato-based breads, rice-based noodles and breads, and wheat-free rye bread. |
| Fruit | Grapes, mangoes, peaches, persimmon, pineapple, watermelon, and bananas. | Grapefruit, lemons, limes, papaya, raspberries, strawberries, and blueberries. |
| Vegetables | Artichokes, asparagus, beets, broccoli, Brussel sprouts, cabbage, chicory, garlic, leeks, lettuce, okra, onions, radicchio, scallions, shallots, snow peas, and zucchini. | Bean sprouts, bell peppers, bok choy, carrots, celery, chives, cucumber, eggplant, potatoes, pumpkin, radishes, spinach, tomatoes, turnips, winter squash, and garlic-infused oil. |
| Galactans | Plant based proteins such as beans, black-eyed peas, chick peas, kidney beans, lentils, lima beans, pinto beans, soy products, broccoli, Brussel sprouts, cabbage, green beans, and yellow beans. | Eggs, nuts, quinoa, seeds, bean sprouts, bell peppers, bok choy, carrots, celery, chives, cucumbers, eggplant, potatoes, pumpkin, radish, spinach, and tomatoes. |
| Artificial Sweeteners | Sorbitol, mannitol, isomaltose, malitol, xylitol, polydextrose, hydrogenated starch | Aspartame, sucralose, saccharin. Commonly found in various gum and candy as well. |
| Polyols | ||
| Fruit | Apples, apricots, avocados, cherries, lychee, nectarines, peaches, pears, plums, and watermelon. | Bananas, blueberries, grapefruit, kiwi, lemons, limes, passion fruit, raspberries, cantaloupe, honeydew, and strawberries |
| Vegetables | Artichoke, asparagus, brussel sprouts, cabbage, cauliflower, green beans mushrooms, snow peas sprouts, and summer squash. | Bean sprouts, bell peppers, bok choy, carrots, celery, chives, cucumbers, eggplant, kale, lettuce, potatoes, pumpkin, radishes, spinach, tomatoes, winter squash, yams, and zucchini. |
Eat Less Of These Foods
Lactose
- Cow’s milk, yogurt, pudding, custard, ice cream, cottage cheese, ricotta cheese and mascarpone
Fructose
- Fruits, such as apples, pears, peaches, cherries, mangoes, pears and watermelon
- Sweeteners, such as honey and agave nectar
- Products with high fructose corn syrup
Fructans
- Vegetables, such as artichokes, asparagus, Brussels sprouts, broccoli, beetroot, garlic and onions
- Grains such as wheat and rye
- Added fiber, such as inulin
Oligosaccharides (fructans and/or galactans)
- Chickpeas, lentils, kidney beans and soy products
- Vegetables, such as broccoli
Polyols
- Fruits, such as apples, apricots, blackberries, cherries, nectarines, pears, peaches, plums and watermelon
- Vegetables, such as cauliflower, mushrooms and snow peas
- Sweeteners, such as sorbitol, mannitol, xylitol, maltitol and isomalt found in sugar-free gum and mints, and cough medicines and drops
Eat More Of These Foods
- Dairy: Lactose-free milk, rice milk, almond milk, coconut milk, lactose-free yogurt; hard cheeses such as feta and brie
- Fruit: Bananas, blueberries, cantaloupe, grapefruit, honeydew, kiwi, lemon, lime, oranges and strawberries
- Vegetables: Bamboo shoots, bean sprouts, bok choy, carrots, chives, cucumbers, eggplant, ginger, lettuce, olives, parsnips, potatoes, spring onions and turnips
- Protein: Beef, pork, chicken, fish, eggs and tofu
- Nuts/seeds (limit to 10-15 each): Almonds, macadamia, peanuts, pine nuts and walnuts
- Grain: Oat, oat bran, rice bran, gluten-free pasta, such as rice, corn, quinoa, white rice, corn flour and quinoa
The idea behind the low FODMAPs diet is to only limit the problematic foods in a category — not all of them. (After all, they do have health benefits.) You may tolerate some foods better than others.
Meet with a registered dietician if you are considering this diet. It’s important to make sure your eating plan is safe and healthy. He or she will have you eliminate FODMAPs from your diet. Then you gradually add the carbohydrates back in one at a time and monitor your symptoms. A food diary and symptom chart may be helpful tools.
Summary
A low-FODMAP diet appears to be effective for treatment of at least a subset of patients with IBS. FODMAPs likely induce symptoms in IBS patients due to luminal distention and visceral hypersensitivity. Some health professionals believe it’s too restrictive. Proponents of the diet report that people stick with it because of how it improves their quality of life. Whenever possible, implementation of a low-FODMAP diet should be done with the help of an experienced dietician.
However, more research is needed to determine which patients can benefit from a low-FODMAP diet and to quantify the FODMAP content of various foods, which will help patients follow this diet effectively.
- Magge S, Lembo A. Low-FODMAP Diet for Treatment of Irritable Bowel Syndrome. Gastroenterology & Hepatology. 2012;8(11):739-745. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3966170/[↩][↩]
- Irritable bowel syndrome and diet: where are we in 2018 ? Current Opinion in Clinical Nutrition & Metabolic Care: November 2017 – Volume 20 – Issue 6 – p 456–463. http://journals.lww.com/co-clinicalnutrition/Abstract/2017/11000/Irritable_bowel_syndrome_and_diet___where_are_we.6.aspx[↩]
- Low-FODMAP Diet. American College of Gastroenterology. http://patients.gi.org/topics/low-fodmap-diet/[↩]
- Low FODMAP diet for Irritable Bowel Syndrome. Monash University. https://www.monash.edu/medicine/ccs/gastroenterology/fodmap[↩]
- Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. Gibson PR, Shepherd SJ. J Gastroenterol Hepatol. 2010 Feb; 25(2):252-8. https://www.ncbi.nlm.nih.gov/pubmed/20136989/[↩]
- Gibson PR, Barrett JS. Clinical ramifications of malabsorption of fructose and other short-chain carbohydrates. Practical Gastroenterology. 2007;31:51–65.[↩][↩][↩]