Contents
- What is folliculitis
- Types of folliculitis
- What causes folliculitis
- Risk factors for developing folliculitis
- Folliculitis prevention
- Folliculitis treatment
What is folliculitis
Folliculitis refers to an infection or inflammation of the hair follicles, the tiny pouches under the skin that hold the hair due to infection, chemical irritation or physical injury. Bacterial folliculitis is the most common form of folliculitis. Folliculitis is quite common and is usually harmless in itself, but can be irritating. Folliculitis is most common on the parts of the body that experience friction, such as the face, scalp, back, and thighs. The friction caused by clothing, shaving, and substances such as sweat, oils, and cosmetics can block and irritate the follicles, allowing bacteria that normally reside on the skin, such as Staphylococcus, to get into these follicles and cause the infection. Once infected, the follicles look like red pimples with a hair in the middle of them.
Folliculitis may be superficial or deep. It can affect anywhere there are hairs, including chest, back, buttocks, arms and legs. Acne and its variants are also types of folliculitis.
At first folliculitis may look like small red bumps or white-headed pimples around hair follicles — the tiny pockets from which each hair grows. These can become itchy or sore, and there may be pus. It can occur anywhere on the body that there is hair. If an infection is more severe or deeper under the skin, you may feel feverish or unwell. The infection can spread and turn into nonhealing, crusty sores. Severe infections can cause permanent hair loss and scarring (folliculitis decalvans).
If you have a mild case, it’ll likely clear in a few days with basic self-care measures. For more serious or recurring folliculitis, you may need to see a doctor for prescription medicine.
Certain types of folliculitis are known as hot tub rash, razor bumps and barber’s itch.
Folliculitis signs and symptoms include:
- Clusters of small red bumps or white-headed pimples that develop around hair follicles
- Pus-filled blisters that break open and crust over
- Itchy, burning skin
- Painful, tender skin
- A large swollen bump or mass
What causes folliculitis?
Folliculitisis is caused by an infection from bacteria, a virus or fungus. It can also be caused by irritation from chemicals or some skin conditions.
The most common bacteria that cause the condition are Staphylococcus aureus, which is commonly found on the skin and Pseudomonas, which can be found in swimming pools or spas if they aren’t well chlorinated.
Other causes include parasites, yeasts infections such as tinea and some viruses like herpes. Skin irritation can also cause folliculitis.
It sometimes happens after shaving. It is also more common in people who have diabetes, are very overweight, take antibiotics long-term, have low immunity or use oily skincare products.
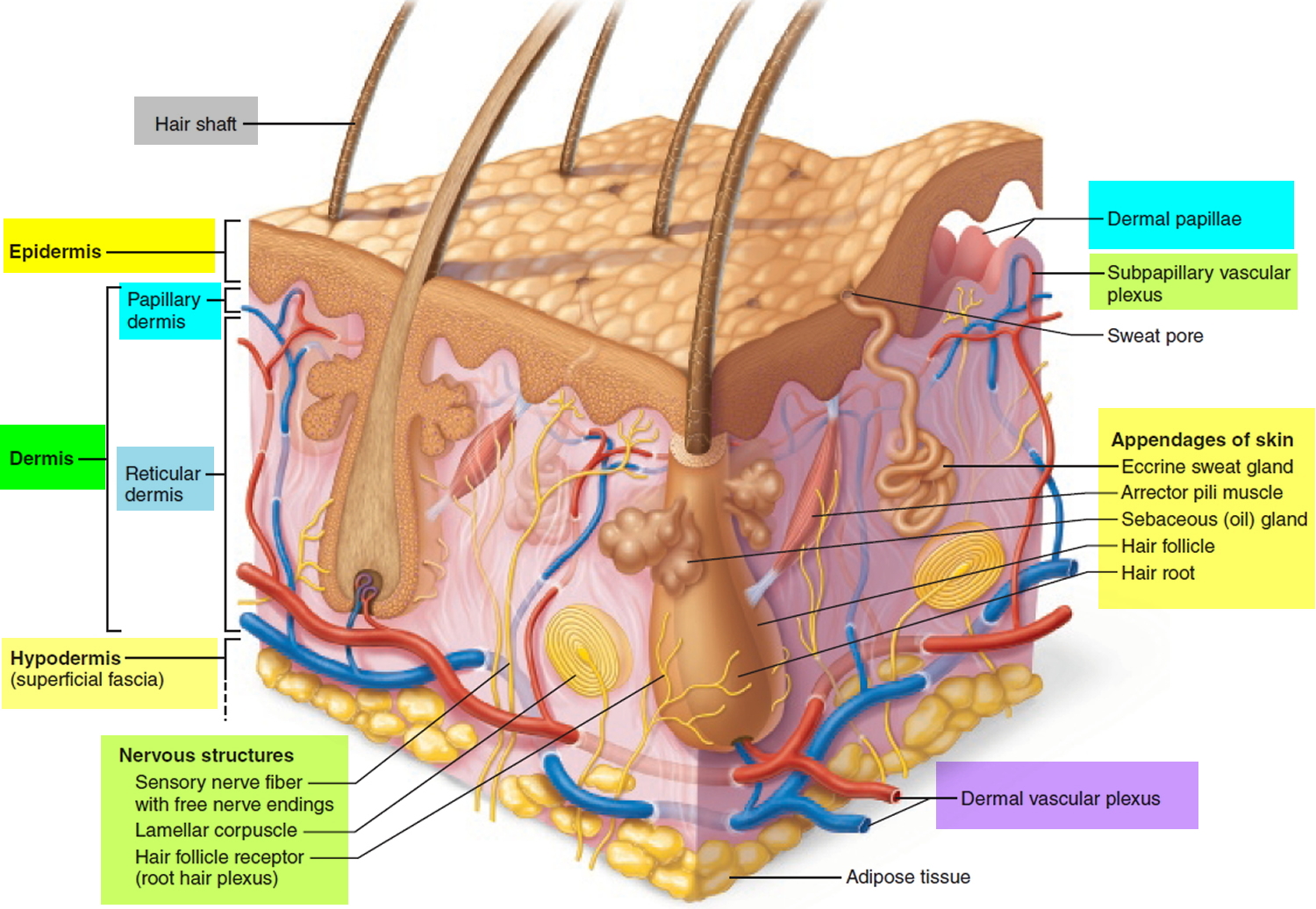
Figure 1. Hair structure
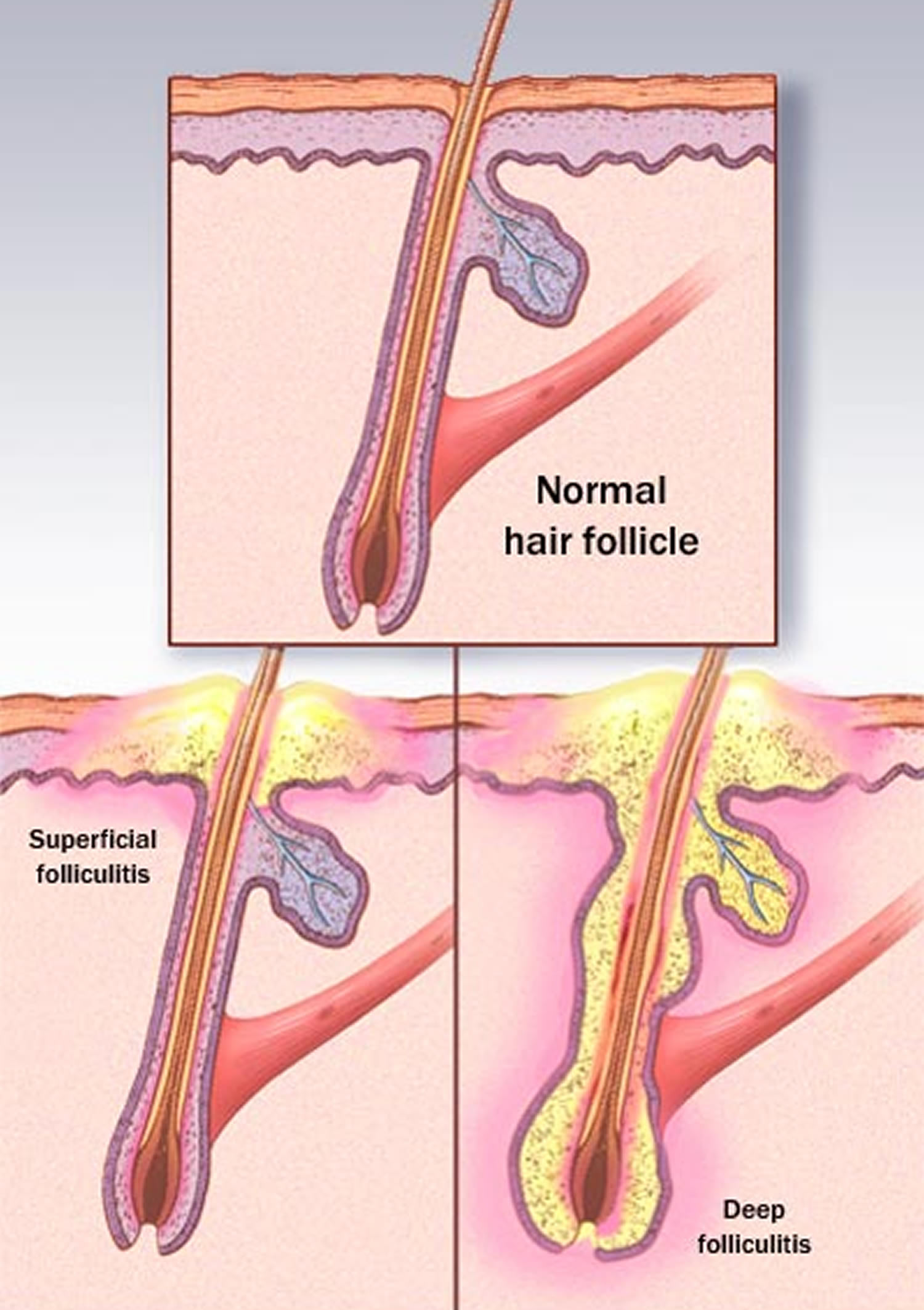
Figure 2. Hair follicle
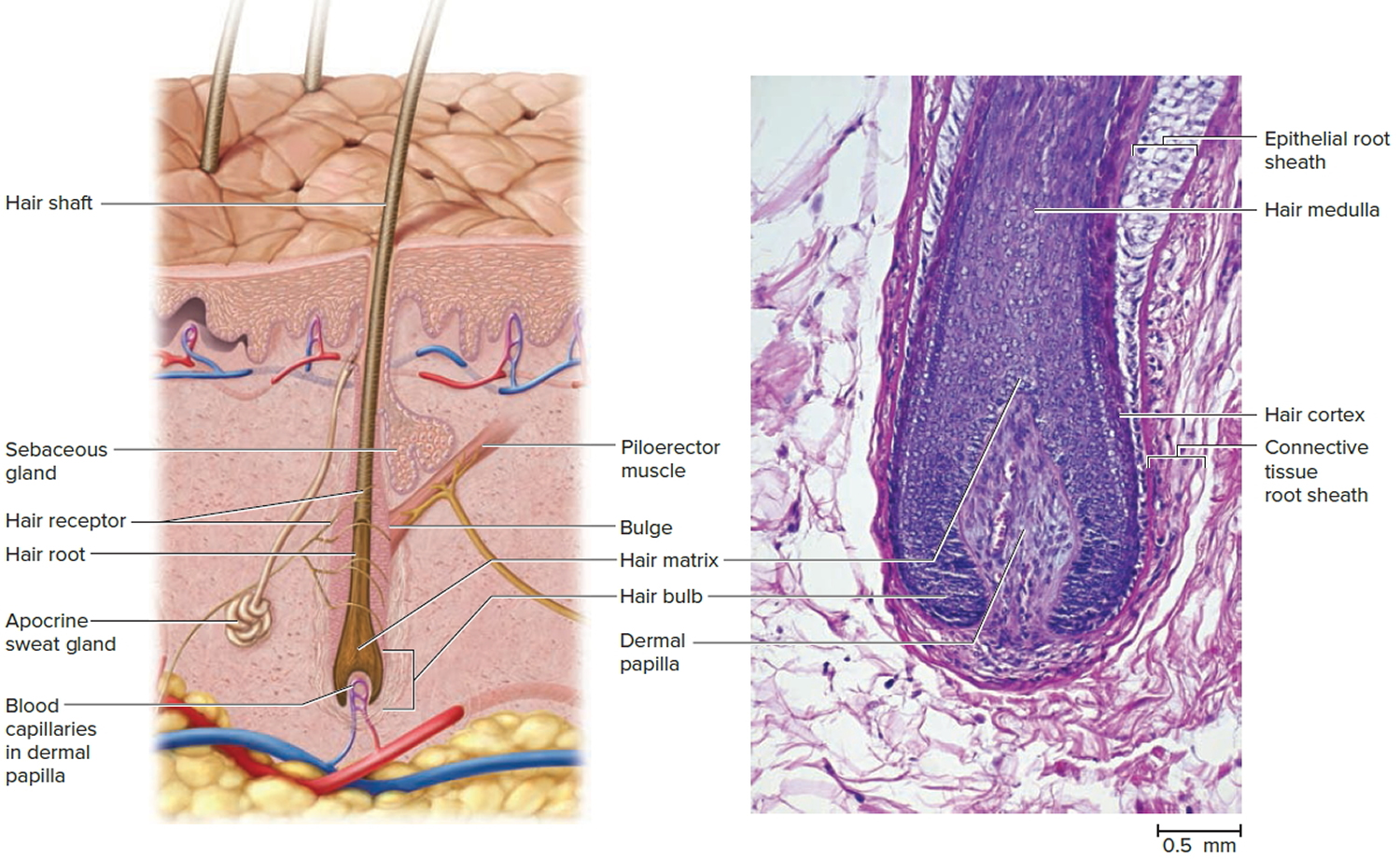 Figure 3. Folliculitis – Superficial folliculitis affects the upper part of the hair follicle and the skin directly next to the follicle. Deep folliculitis affects the deeper portion of the follicle and can involve the entire hair follicle.
Figure 3. Folliculitis – Superficial folliculitis affects the upper part of the hair follicle and the skin directly next to the follicle. Deep folliculitis affects the deeper portion of the follicle and can involve the entire hair follicle.Pityrosporum folliculitis
Pityrosporum folliculitis also called Malassezia folliculitis, is an infection of the hair follicle by the fungus Malassezia furfur, formerly known as Pityrosporum ovale. This condition is often associated with seborrheic dermatitis, which is not surprising since both are caused by Malassezia furfur. Predisposing conditions include hot, humid environments, excessive sweating, immunosuppression, corticosteroid or antibiotic use, adolescence, male gender, and transplantation. Associated diseases include steroid folliculitis, acne, and tinea versicolor.
Pityrosporum folliculitis is characterized by multiple follicular pustules and erythematous papules on the upper back and/or chest and shoulders (Figure 4). Some reports have highlighted facial involvement as being present in more than half of patients. The sides of the face and chin are preferred as opposed to the central face. Some women have noted a flare with their menstrual cycle. The lesions may be intensely itchy.
Pityrosporum folliculitis may be misdiagnosed as acne and vice versa. Acne has comedones whereas pityrosporum folliculitis does not. Some patients have developed pityrosporum folliculitis after beginning a tetracycline for acne. Bacterial folliculitis will respond to oral antibiotics. Steroid acne/folliculitis probably represents pityrosporum folliculitis. In the case of pityrosporum folliculitis, Wood’s light may show a yellow-green fluorescence in 2/3 of cases. KOH (potassium hydroxide) may be employed, but caution exercised as Pityrosporum is part of the normal flora.
A punch biopsy with PAS staining to visualize the Pityrosporum species may be needed in difficult cases. A trial of an oral antifungal agent, e.g., itraconazole, which if rapidly effective, may be the easiest way to establish the diagnosis.
Pityrosporum folliculitis treatment
- An oral antifungal agent, e.g., itraconazole, fluconazole.
- Topical antifungal shampoos or creams may help or prevent recurrences.
Oral itraconazole and fluconazole (for 3 weeks) may be given if necessary although rapid relapse is common. Itraconazole 200 mg/day x 7 days-1 month is typical. Fluconazole 400 mg po once may be used. One patient of mine has done well with itraconazole 100 mg once daily for 7 days every 1-2 months.
Selenium sulfide 2.5% or ketoconazole 2% shampoo lathered on the scalp and trunk for 5-10 minutes once daily initially and then tapered is usually effective. You may also use a soap containing 2% zinc pyrithione (ZNP bar). Zinc pyrithione has activity against Malassezia furfur. Topical clotrimazole cream has been employed.
Figure 4. Pityrosporum folliculitis (Malassezia folliculitis)
Hot tub folliculitis
Hot tub folliculitis as the name suggests, is a folliculitis that occurs soon after using a hot tub (see Figure 5). It is caused by the bacteria Pseudomonas, that grows in poorly chlorinated hot tubs and/or whirlpools. Thus, this type of folliculitis is often called hot tub rash. Pseudomonas folliculitis may also occur in patients who use a washcloth, loofah or some type of sponge in the shower or bath. If such an item stays wet between uses, the Pseudomonas can contaminate the item and produce a chronic source of infection of the skin. An outbreak of 35 people who used the same swimming pool was linked to contamination of inflatables by Pseudomonas.
Possible sources:
- Hot tub, Jacuzzi, whirlpool, water slide, or swimming pool
- Bath toys, plug, mat
- Loofah sponge, bath sponges, or nylon towels
- Standing water (e.g., child playing in every day)
- Diving suits
Anyone who uses a contaminated hot tub, whirlpool, or swimming pool can develop hot tub folliculitis.
The typical patient with hot tub folliculitis develops multiple pustules atop urticarial bases scattered on the trunk or buttocks several hours to days after using a hot tub contaminated by Pseudomonas and is most noticeable in areas of the skin that were covered by a bathing suit or clothes at the time of exposure. One typical feature is the significant inflammation surrounding the pustule. Often, the surrounding erythema is 1-2 cm in diameter–larger than that usually seen with Staphylococcal folliculitis. The distribution is typically symmetric and truncal, with a preference for the flanks.
Located around hair follicles, these hot tub folliculitis bumps tend to be itchy or tender.
The most common locations for hot tub folliculitis include:
- Groin and buttocks (“bathing suit” distribution)
- Abdomen or lower back
- Armpits
- Chest or upper back
- Upper arms
- Upper legs
Hot tub folliculitis typically arises within 1–4 days of exposure to the contaminated source. In addition to the rash, symptoms can include mild fever, headache, sore throat, and fatigue. Swollen and tender lymph nodes (glands that help produce antibodies, special proteins that fight off infection) may occur. Breast tenderness occasionally develops in both men and women, as glands in the nipple may become infected.
Some patients may have a chronic infection, e.g., over many months. Hot tub folliculitis is almost invariably associated with repeated exposure to a source. For example, one child suffered from repeated folliculitis of the buttocks from sitting on a bath mat that harbored Pseudomonas. Another child played almost every day in standing water that was the source of exposure.
Hot tub folliculitis treatment
No treatment is needed, as the disease is self-limited. Although hot tub folliculitis usually resolves within 7–14 days without treatment, the rash may leave behind patches of darker (hyperpigmented) skin. These patches are more pronounced in darker-skinned people and may take months to return to normal pigmentation.
If the rash is itchy, an over-the-counter antihistamine may be helpful.
Persistence folliculitis may rarely occur in very sweaty individuals.
In severe cases, your doctor may recommend the following:
- Acetic acid compresses
- Oral antibiotic pills such as ciprofloxacin 500 twice daily
- Topical antibiotic cream such as gentamicin
In order to prevent hot tub rash, proper maintenance and chlorination of pools, spas, and hot tubs is essential. Sponges and loofahs should be completely dried between uses in order to kill any bacteria or better still it should be disposed of.
Figure 5. Hot tub folliculitis
Figure 6. Hot tub folliculitis appears as small (2–10 mm) pink to red bumps, which may be filled with pus or covered with a scab
Folliculitis decalvans
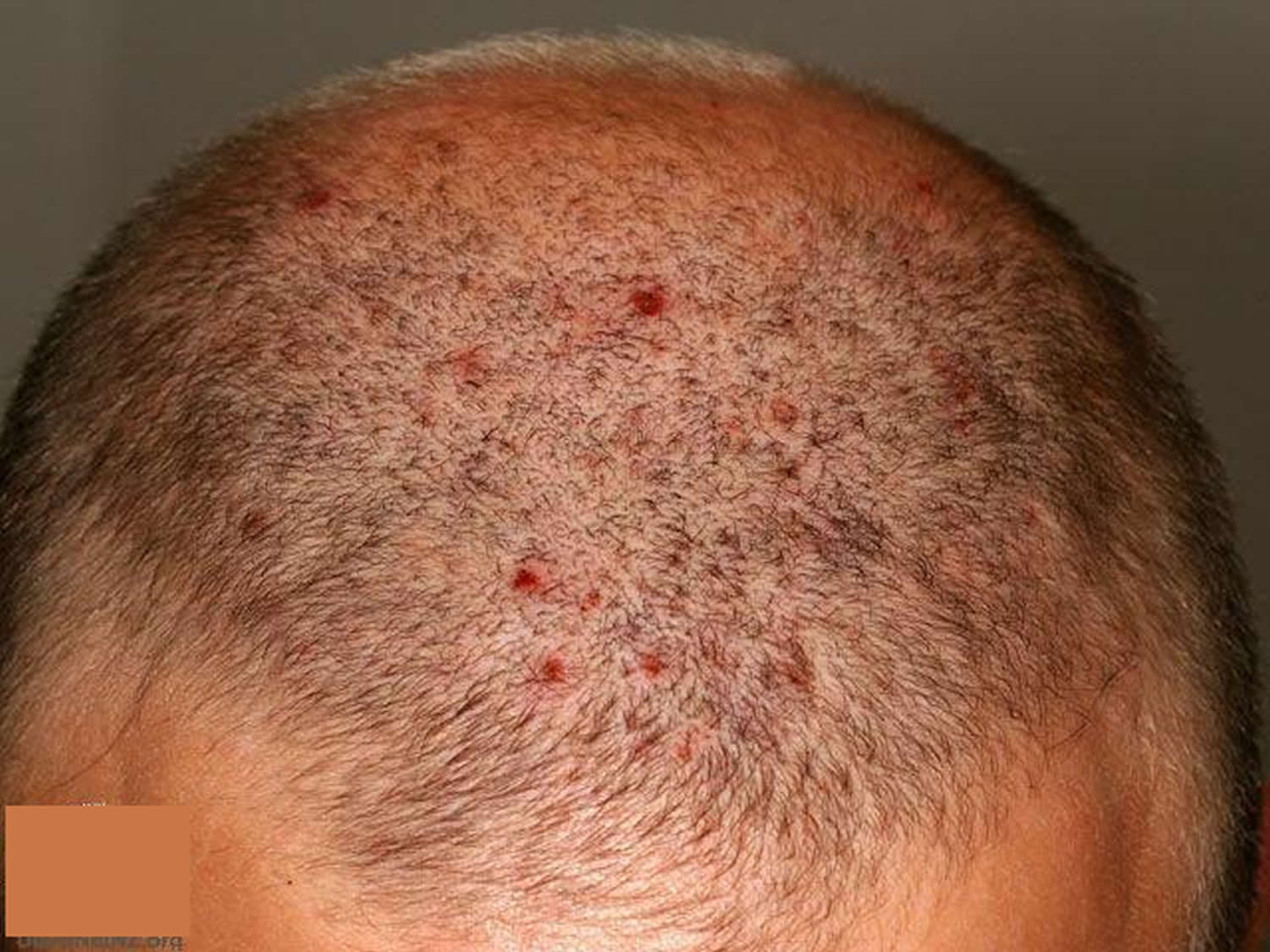
Folliculitis decalvans is a form of alopecia (hair loss) that involves scarring. It is characterized by redness and swelling and pustules around the hair follicle (folliculitis) that leads to destruction of the follicle and consequent permanent hair loss. Folliculitis decalvans is one cause of cicatricial alopecia (baldness with scarring) and is sometimes known as tufted folliculitis.
The exact cause is unknown. Staphylococcus aureus may be grown from the pustules, however in the vast majority of people who develop a bacterial pustular folliculitis of the scalp it is transient, resolves without antibiotics and heals without scarring, which is not the case in folliculitis decalvans. It may be that staphylococcus aureus, together with a deficient host immune response lead to the development of this condition.
Folliculitis decalvans affects both men and women and may start first during adolescence or at any time in adult life. Men may be affected from adolescence onwards, whereas women tend not to develop this condition until their fourth decade.
Symptoms include itch, pain and tightness. Sometimes no discomfort is felt at all. The disease may remain limited to a few small patches or may progress over time causing extensive hair loss.
Any hairy region may be involved. It is usually confined to the scalp but can involve other sites including the beard, underarm and pubic hair, lower legs, thighs and arms. There are usually round or oval patches of hair loss in which there are pustules surrounding the hair follicles (perifollicular pustules). Characteristically, several or many hairs can be seen coming out of a single follicle, so the scalp looks “tufted” like a toothbrush. Eventually the hairs are shed as the follicle is completely destroyed and leaves behind a scar.
Folliculitis decalvans treatment
There is no permanent cure for the condition but it can be controlled to some degree by using medications.
- Oral antibiotics such as minocycline, tetracycline, rifampicin, clindamycin, fusidic acid, ciprofloxacin and dicloxacillin have all been tried with varying results from patient to patient.
- In some severe forms, addition of an oral corticosteroid may be necessary.
- Oral isotretinoin can result in long-term remissions in some patients.
- Methyl aminolevulinate photodynamic therapy is reported to result in clinical improvement
Figure 7. Folliculitis decalvans
Scalp folliculitis
Scalp folliculitis is an inflammatory disorder of the hair follicles in the scalp. The condition is also known as “acne necrotica miliaris” or “Proprionibacterium folliculitis”.
Scalp folliculitis is characterized by small, very itchy pustules on the scalp, often most troublesome on the frontal hairline. There may be only a small number of lesions or they may be very numerous. They are hard to leave alone because of the itch. They often become sore and crusted.
The cause of scalp folliculitis is not well understood. It is generally considered to be an inflammatory reaction to components of the hair follicle, particularly the micro-organisms. These include:
- Bacteria (especially Cutibacterium acnes, but in severe cases, also Staphylococcus aureus)
- Yeasts (Malassezia species)
- Mites (Demodex folliculorum)
Scalp folliculitis treatment
The scalp affected by folliculitis should be washed with a mild normal shampoo as often as desired. Anti-dandruff shampoos containing antifungal agents such as ketoconazole or ciclopirox are sometimes helpful. Conditioner can be used if desired.
The following medications may be helpful for scalp folliculitis:
- Topical antibiotics eg fusidic acid gel, clindamycin solution, erythromycin solution
- Mild topical steroid lotions or creams
- Oral antihistamines
- Oral antibiotics, particularly long-term tetracycline
- Oral isotretinoin – long-term low dose treatment may be required
Figure 8. Scalp folliculitis
Folliculitis on face
Folliculitis barbae is a type of folliculitis affecting the beard area due to infection with the bacteria Staphylococcus aureus. It occurs in men who shave and in men that do not shave. Deep-seated folliculitis barbae is called sycosis barbae, and leads to scarring and areas of permanent hair loss.
What is pseudofolliculitis barbae?
Pseudofolliculitis barbae is a foreign-body inflammatory reaction surrounding ingrown facial hairs, which results from shaving. It can also occur on any body site where hair is shaved or plucked, including axilla, pubic area, and legs. It is also known as shaving rash or razor bumps.
Folliculitis barbae and pseudofolliculitis barbae can co-exist.
Prevalence of folliculitis barbae and pseudofolliculitis barbae is higher among males of African ancestry than among Caucasian men. Both disorders can also affect women of all races. They are associated with improper shaving practices.
Recent research has confirmed a genetic predisposition to pseudofolliculitis in the African population. A single nucleotide substitution in the hair follicle companion layer-specific keratin (K6hf) is shown to increase the chance of pseudofolliculitis barbae.
Clinical features of pseudofolliculitis and folliculitis barbae
After shaving, patients may experience an acne-like eruption on the area that has been shaved, usually the face and neck of men.
- Pseudofolliculitis barbae presents as ingrown hairs associated with flesh-colored or red follicular papules, which may be itchy or tender.
- Folliculitis barbae presents as painful pustules and can discharge pus.
- Lesions may bleed when they are shaved.
Folliculitis barbae and pseudofolliculitis are aggravated by co-existent eczema/dermatitis.
Pseudofolliculitis barbae causes
Pseudofolliculitis barbae is due to shaving, particularly close shaving—because the cut hair may retract beneath the skin surface. It can also occur in skin folds and scars. It occurs mainly in people with curly hair, because the curl of the hair means that the sharp pointed end of a recently shaved hair comes out from the skin and re-enters the skin close by causing a foreign body inflammatory reaction.
The injured follicles are highly susceptible to become infected, causing folliculitis barbae.
Pseudofolliculitis barbae prevention
To prevent recurrence, follow a proper shaving regimen long term and consider hair removal. Methods may include:
- Eflornithine cream
- Chemical depilatories such as barium sulfide paste and calcium thioglycolate; these can be irritating
- Intense pulsed light (IPL)
- Laser hair removal, especially Nd:YAG and diode lasers, but there is a risk of causing white or dark marks in skin of color.
Folliculitis and pseudofolliculitis barbae complications
Complications of folliculitis and pseudofolliculitis barbae include:
- Postinflammatory hyperpigmentation
- Hypertrophic scarring and keloid formation
- Temporary and permanent hair loss
- Sycosis barbae – sinuses, abscesses and spreading infection due to infection and autoinflammatory reaction
Treatment for pseudofolliculitis barbae depends on the severity of the condition. If possible, let the beard grow for 30 days to eliminate ingrown hairs. When ready to shave again, take the following precautions:
- Ensure the skin is well moisturized, for example using a lotion containing glycolic acid to the affected areas. This exfoliates the surface skin cells and reduces the likelihood of new inflamed spots.
- Cleanse the skin using a polyester skin-cleansing pad or a moisturizing shaving foam.
- Aim to have a 5 o’clock shadow immediately after shaving. Shave less frequently, eg every other day.
- Either use a single blade disposable razor, or use electric hair clippers or a razor with an attachment that leaves the cut hairs long.
- Shave in the direction of the follicle, not against it. Do not stretch the skin.
- Sterilize metal hair clippers and electric razors using boiling water, and plastic items should be soaked in antiseptic solution.
Medical treatment of pseudofolliculitis barbae
- Hydrocortisone cream can reduce mild inflammation and itching.
- Topical acne treatments such as benzoyl peroxide and tretinoin are used to suppress follicular hyperkeratosis.
- A combination of tretinoin, low-potency topical corticosteroid, and hydroquinone may be selected to decrease inflammation, hyperkeratosis and pigment production.
- Oral tetracyclines are used to reduce inflammation.
- Photodynamic therapy has been successful.
Folliculitis barbae treatment
As folliculitis barbae and sycosis barbae are due to bacterial infection, they are treated with topical or oral anti-staphylococcal antibiotics.
Folliculitis buttocks
Folliculitis affecting the buttocks is quite common and is often nonspecific, that is no specific cause is found. Buttock folliculitis is equally common in males and females.
Folliculitis of the buttocks is not uncommon in adult women. The patient may or may not have acne elsewhere. Long periods of sitting aggravate the condition. Not showering after working out can trigger as well. An occlusive folliculitis may appear similarly or overlap with this condition. Staphylococcal folliculitis is in the differential. Multiple red follicular papules and pustules scattered on the buttocks may occur in this variant of folliculitis. A bacterial culture should be done to exclude a bacterial folliculitis.
Treatment
- Avoid tight fitting clothing.
- Avoid any creams or moisturizers. If needed, use a lotion that is non-comedogenic.
- Shower off right after sweating, exercise.
- Avoid sitting for prolonged time.
- Topical benzoyl peroxide.
Avoid tight, friction-inducing clothing such as tight jeans and to change out of sweaty gym clothes as soon as possible. Opt for cotton underwear over nylon or Spandex to give the skin a chance to breathe.
Topical benzoyl peroxide is beneficial:
- At bedtime, two or three times a week, apply a small amount of benzoyl peroxide 5% gel (over-the-counter) to the area, avoiding any ‘sensitive’ parts; let it dry completely, then wear white underwear (benzoyl peroxide will bleach fabrics). Shower in the morning. If it gets irritating, take a few days off.”
Your doctor can also prescribe clindamycin topical solution or gel if needed. Aluminum chloride hexahydrate 6.25% (Xerac AC) every night at bedtime has been helpful. Rarely, an oral tetracycline antibiotic may be needed.
- Chronic buttock folliculitis does not often cause significant symptoms but it can be very persistent. Although antiseptics, topical acne treatments, peeling agents such as alphahydroxy acids, long courses of oral antibiotics and isotretinoin can help buttock folliculitis, they are not always effective. Hair removal might be worth trying if the affected area is hairy. As regrowth of hair can make it worse, permanent hair reduction by laser or intense pulsed light (IPL) is best.
Figure 9. Folliculitis buttocks
Figure 10. Folliculitis buttocks (Hookworm folliculitis with complete resolution after a single oral dose of ivermectin)
Folliculitis on legs
It is not uncommon for a woman to get a folliculitis or a pseudofolliculitis in the legs (or pubic area) after shaving. There can be a true folliculitis, e.g. staphylococcus, or ingrown hairs, or irritation or a combination.
Folliculitis on legs is characterized by red follicular papules and at times pustules are seen. Sometimes larger “cystic” lesions may occur and last for weeks. Careful inspection may show ingrown hairs.
Treatment
- Shave in the shower pretreating the area with warm water. Some recommend a minimum of 10 minutes to hydrate the skin.
- You may try exfoliating before with e.g. a pumis stone to release ingrown hairs.
- Then apply a lotion or baby oil.
- With regard to razor, one patient did well with the Schick Quattro For Women Trimstyle Razor & Bikini Trimmer
- Shave with the direction of hair growth and don’t stretch the skin.
- Shave each area only once. Use short strokes.
- After shaving, apply a soothing cream/lotion (e.g. with aloe vera) or hydrocortisone 1% cream/lotion.
- Don’t wax, pluck or pull hairs. This only leads to ingrown hairs.
- Replace the razor heads every few weeks.
- If a breakout is particularly bad, try to let the hair grow out for up to a week.
- Don’t scratch.
The presence of any pustules might prompt a bacterial culture. Topical benzoyl peroxide e.g. 5% several times a week may be helpful, preferably one that you put on and leave on (not a wash). The patient must be careful not to get it on clothes as it will bleach them. One approach is to apply before bedtime every other night and wear white underwear. Alternatively, clindamycin solution/gel/lotion may be prescribed. Also, washing daily in the shower with Hibiclens OTC may reduce the bacterial count.
Ultimately laser hair removal may be the best solution for woman with a chronic problem.
Figure 11. Folliculitis on legs
Types of folliculitis
The two main types of folliculitis are superficial and deep. The superficial type involves part of the follicle, and the deep type involves the entire follicle and is usually more severe.
Forms of superficial folliculitis include:
- Bacterial folliculitis. This common type is marked by itchy, white, pus-filled bumps. It occurs when hair follicles become infected with bacteria, usually Staphylococcus aureus (staph). Staph bacteria live on the skin all the time. But they generally cause problems only when they enter your body through a cut or other wound.
- Hot tub folliculitis (pseudomonas folliculitis). With this type you may develop a rash of red, round, itchy bumps one to two days after exposure to the bacteria that causes it. Hot tub folliculitis is caused by pseudomonas bacteria, which is found in many places, including hot tubs and heated pools in which the chlorine and pH levels aren’t well-regulated.
- Razor bumps (pseudofolliculitis barbae). This is a skin irritation caused by ingrown hairs. It mainly affects men with curly hair who shave too close and is most noticeable on the face and neck. People who get bikini waxes may develop barber’s itch in the groin area. This condition may leave dark raised scars (keloids).
- Pityrosporum folliculitis. This type produces chronic, red, itchy pustules on the back and chest and sometimes on the neck, shoulders, upper arms and face. This type is caused by a yeast infection.
Forms of deep folliculitis include:
- Sycosis barbae. This type affects males who have begun to shave.
- Gram-negative folliculitis. This type sometimes develops if you’re receiving long-term antibiotic therapy for acne.
- Boils (furuncles) and carbuncles. These occur when hair follicles become deeply infected with staph bacteria. A boil usually appears suddenly as a painful pink or red bump. A carbuncle is a cluster of boils.
- Eosinophilic folliculitis. This type mainly affects people with HIV/AIDS. Signs and symptoms include intense itching and recurring patches of bumps and pimples that form near hair follicles of the face and upper body. Once healed, the affected skin may be darker than your skin was previously (hyperpigmented). The cause of eosinophilic folliculitis isn’t known.
What causes folliculitis
Folliculitis can be due to infection, occlusion (blockage), irritation and various skin diseases.
Folliculitis due to infection
To determine if folliculitis is due to an infection, swabs should be taken from the pustules for cytology and culture in the laboratory.
Bacteria
Bacterial folliculitis is commonly due to Staphylococcus aureus. If the infection involves the deep part of the follicle, it results in a painful boil. Recommended treatment includes careful hygiene, antiseptic cleanser or cream, antibiotic ointment, and/or oral antibiotics.
Spa pool folliculitis is due to infection with Pseudomonas aeruginosa, which thrives in inadequately chlorinated warm water. Gram negative folliculitis is a pustular facial eruption also due to infection with Pseudomonas aeruginosa or other similar organisms. When it appears, it usually follows tetracycline treatment of acne, but is quite rare.
Yeasts
The most common yeast to cause a folliculitis is Pityrosporum ovale, also known as Malassezia. Malassezia folliculitis (Pityrosporum folliculitis) is an itchy acne-like condition usually affecting the upper trunk of a young adult. Treatment includes avoiding moisturisers, stopping any antibiotics and topical antifungal or oral antifungal medication for several weeks.
Candida albicans can also provoke a folliculitis in skin folds (intertrigo) or in the beard area. It is treated with topical or oral antifungal agents.
Fungi
Ringworm of the scalp (tinea capitis) usually results in scaling and hair loss, but sometimes results in folliculitis. Cat ringworm (Microsporum canis) is the commonest organism causing scalp fungal infection. Other fungi such as Trichophyton tonsurans are increasingly reported. Treatment is with oral antifungal agents for several months.
Viral infections
Folliculitis may caused by herpes simplex virus. This tends to be tender, and resolves without treatment in around 10 days. Severe recurrent attacks may be treated with aciclovir and other antiviral agents.
Herpes zoster (the cause of shingles) may also present as folliculitis with painful pustules and crusted spots within a dermatome (an area of skin supplied by a single nerve). It is treated with hihg-dose aciclovir.
Molluscum contagiosum, common in young children, may also cause follicular umbilicated papules, usually clustered in and around a body fold. Molluscum may provoke dermatitis.
Parasitic infection
Folliculitis on the face or scalp of older or immunosuppressed adults may be due to colonisation by hair follicle mites (demodex). This is known as demodicosis.
The human infestation, scabies, often provokes folliculitis, as well as non-follicular papules, vesicles and pustules.
Folliculitis due to irritation from regrowing hairs
Folliculitis may arise as hairs regrow after shaving, waxing, electrolysis or plucking. Swabs taken from the pustules are sterile ie there is no growth of bacteria or other organisms. In the beard area irritant folliculitis is known as pseudofolliculitis barbae.
Irritant folliculitis is also common on the lower legs of women (shaving rash). It is frequently very itchy. Treatment is by stopping hair removal, and not beginning again for about three months after the folliculitis has settled. To prevent reoccurring irritant folliculitis, use a gentle hair removal method, such as a lady’s electric razor. Avoid soap and apply plenty of shaving gel, if using a blade shaver.
Folliculitis due to contact reactions
Occlusion
Paraffin-based ointments, moisturizers, and adhesive plasters may all result in a sterile folliculitis. If a moisturizer is needed, choose an oil-free product, as it is less likely to cause occlusion.
Chemicals
Coal tar, cutting oils and other chemicals may cause an irritant folliculitis. Avoid contact with the causative product.
Topical steroids
Overuse of topical steroids may produce a folliculitis. Perioral dermatitis is a facial folliculitis provoked by moisturisers and topical steroids. Perioral dermatitis is treated with tetracycline antibiotics for six weeks or so.
Folliculitis due to immunosuppression
Eosinophilic folliculitis is a specific type of folliculitis that may arise in some immune suppressed individuals such as those infected by human immunodeficiency virus (HIV) or those who have cancer.
Folliculitis due to drugs
Folliculitis may be due to drugs, particularly corticosteroids (steroid acne), androgens (male hormones), ACTH, lithium, isoniazid (INH), phenytoin and B-complex vitamins. Protein kinase inhibitors (epidermal growth factor receptor inhibitors) and targeted therapy for metastatic melanoma (vemurafenib, dabrafenib) nearly always result in folliculitis.
Folliculitis due to inflammatory skin diseases
Certain uncommon inflammatory skin diseases may cause permanent hair loss and scarring because of deep seated sterile folliculitis. These include:
- Lichen planus
- Discoid lupus erythematosus
- Folliculitis decalvans
- Folliculitis keloidalis
Treatment depends on the underlying condition and its severity. A skin biopsy is often necessary to establish the diagnosis.
Acne variants
Acne and acne-like or acneform disorders are also forms of folliculitis. These include:
- Acne vulgaris
- Nodulocystic acne
- Rosacea
- Scalp folliculitis
- Chloracne
The follicular occlusion syndrome refers to:
- Hidradenitis suppurativa (acne inversa)
- Acne conglobata (a severe form of nodulocystic acne)
- Dissecting cellulitis (perifolliculitis capitis abscedens et suffodiens)
- Pilonidal sinus.
Treatment of the acne variants may include topical therapy as well as long courses of tetracycline antibiotics, isotretinoin (vitamin-A derivative) and in women, antiandrogenic therapy.
Risk factors for developing folliculitis
Anyone can develop folliculitis. But certain factors make you more susceptible to the condition, including:
- Having a medical condition that reduces your resistance to infection, such as diabetes, chronic leukemia and HIV/AIDS
- Having acne or dermatitis
- Taking some medications, such as steroid creams or long-term antibiotic therapy for acne
- Being a male with curly hair who shaves
- Regularly wearing clothing that traps heat and sweat, such as rubber gloves or high boots
- Soaking in a hot tub that’s not maintained well
- Causing damage to hair follicles by shaving, waxing or wearing tight clothing
Folliculitis prevention
Keeping your skin clean and dry can help prevent folliculitis. Avoid irritating the skin. Choose skin products that do not clog the pores. Wear breathable clothing and change wet or sweaty clothes promptly.
You can try to prevent folliculitis from coming back with these tips:
- Avoid tight clothes. It helps to reduce friction between your skin and clothing.
- Dry out your rubber gloves between uses. If you wear rubber gloves regularly, after each use turn them inside out, rinse with soap and water, and dry thoroughly.
- Avoid shaving, if possible. For men with razor bumps (pseudofolliculitis), growing a beard may be a good option if you don’t need a clean-shaven face.
- Shave with care. If you shave, adopt habits such as the following to help control symptoms by reducing the closeness of the shave and the risk of damaging your skin:
- Shaving less frequently
- Washing your skin with warm water and antibacterial soap before shaving
- Using a washcloth or cleansing pad in a gentle circular motion to raise embedded hairs before shaving
- Applying a good amount of shaving lotion before shaving
- Shaving in the direction of hair growth, though one study found that men who shaved against the grain had fewer skin bumps. See what works best for you.
- Avoiding shaving too close by using an electric razor or guarded blade and by not stretching the skin
- Using a sharp blade and rinsing it with warm water after each stroke
- Applying moisturizing lotion after you shave
- Avoiding the sharing of razors, towels and washcloths
- Considering hair-removing products (depilatories) or other methods of hair removal. Though they, too, may irritate the skin.
- Use only clean hot tubs and heated pools. And if you own a hot tub or a heated pool, clean it regularly and add chlorine as recommended.
- Talk with your doctor. Depending on your situation and frequency of recurrences, your doctor may suggest controlling bacterial growth in your nose with a five-day regimen of antibacterial ointment and using a body wash with chlorhexidine (Hibiclens, Hibistat). Further study is needed to prove the effectiveness of these steps.
Folliculitis treatment
If you think you might have folliculitis, consult a doctor for advice on what treatments to try.
Treatment depends on the cause, whether bacterial, fungal, parasitic or irritation.
Mild folliculitis often settles down with an antiseptic wash. More severe folliculitis might need antibiotic ointments or tablets. If the infection has progressed into a large boil, this may need draining by a doctor.
If you have folliculitis from shaving, taking break from shaving can help it settle down. Use plenty of gel (not soap) when shaving and avoid shaving against the grain.
If initial treatments don’t clear up your infection, your doctor may use a swab to take a sample of your infected skin or hair. This is sent to a laboratory to help determine what’s causing the infection. Rarely, a skin biopsy may be done to rule out other conditions.
Medications
- Creams or pills to control infection. For mild infections, your doctor may prescribe an antibiotic cream, lotion or gel. Oral antibiotics aren’t routinely used for folliculitis. But for a severe or recurrent infection, your doctor may prescribe them.
- Creams, shampoos or pills to fight fungal infections. Antifungals are for infections caused by yeast rather than bacteria. Antibiotics aren’t helpful in treating this type.
- Creams or pills to reduce inflammation. If you have mild eosinophilic folliculitis, your doctor may suggest you try a steroid cream to ease the itching. If you have HIV/AIDS, you may see improvement in your eosinophilic folliculitis symptoms after antiretroviral therapy.
Other interventions
- Minor surgery. If you have a large boil or carbuncle, your doctor may make a small incision in it to drain the pus. This may relieve pain, speed recovery and lessen scarring. Your doctor may then cover the area with sterile gauze in case pus continues to drain.
- Laser hair removal. If other treatments fail, long-term hair removal with laser therapy may clear up the infection. This method is expensive and often requires several treatments. It permanently removes hair follicles, thus reducing the density of the hair in the treated area. Other possible side effects include discolored skin, scarring and blistering.
Folliculitis home remedy
Mild cases of folliculitis often improve with home care. The following approaches may help relieve discomfort, speed healing and prevent an infection from spreading:
- Apply a warm, moist washcloth or compress. Do this several times a day to relieve discomfort and help the area drain, if needed. Moisten the compress with a saltwater solution (1 teaspoon of table salt in 2 cups of water).
- Apply over-the-counter antibiotics. Try various nonprescription infection-fighting gels, creams and washes.
- Apply soothing lotions. Try relieving itchy skin with a soothing lotion or an over-the-counter hydrocortisone cream.
- Clean the affected skin. Gently wash the infected skin twice a day with antibacterial soap. Use a clean washcloth and towel each time and don’t share your towels or washcloths. Use hot, soapy water to wash these items. And wash clothing that has touched the affected area.
- Protect the skin. If possible, stop shaving, as most cases of barber’s itch clear up a few weeks after you stop shaving.