Contents
What is foodborne illness
Foodborne illness, also called food poisoning, is illness caused by eating contaminated food. Infectious organisms — including bacteria, viruses and parasites — or their toxins are the most common causes of foodborne illness. The biggest cause of foodborne illness is Norovirus; whereas nontyphoidal Salmonella spp., norovirus, Campylobacter spp., and Toxoplasma gondii caused the most hospitalizations; and nontyphoidal Salmonella spp., Toxoplasma gondii, Listeria monocytogenes and norovirus caused the most deaths (see Table 1). Scarce data precluded estimates for other known infectious and noninfectious agents, such as chemicals. Foodborne illnesses are also caused by agents not yet recognized as being transmitted in food and by unknown agents 1, 2. Most often, foodborne illness is mild and resolves without treatment. But some people need to go to the hospital.
Infectious organisms or their toxins can contaminate food at any point of processing or production. Contamination can also occur at home if food is incorrectly handled or cooked.
Foodborne illness symptoms may range from mild to severe and may differ depending on the germ you swallowed. Common symptoms of foodborne illnesses, which can start within hours of eating contaminated food, are nausea, vomiting, stomach cramps, and diarrhea. However, symptoms may differ among the different types of foodborne diseases. Symptoms can sometimes be severe and some foodborne illnesses can even be life-threatening. Although anyone can get a foodborne illness, some people are more likely to develop one. Those groups include:
- Pregnant women
- Young children
- Older adults
- People with immune systems weakened from medical conditions, such as diabetes, liver disease, kidney disease, organ transplants, HIV/AIDS, or from receiving chemotherapy or radiation treatment.
Most people with a foodborne illness get better without medical treatment, but people with severe symptoms should see their doctor.
According to the Centers for Disease Control and Prevention (CDC) estimate, each year in the United States, 31 pathogens caused 48 million foodborne illnesses, 128,000 hospitalizations, and 3,000 deaths 3.
The Centers for Disease Control and Prevention (CDC) estimates that 5.5 million (59%) foodborne illnesses were caused by viruses, 3.6 million (39%) by bacteria, and 0.2 million (2%) by parasites.
The pathogens that caused the most illnesses were 4:
- Norovirus (5.5 million, 58%),
- Nontyphoidal Salmonella spp. (1.0 million, 11%),
- Clostridium perfringens (1.0 million, 10%),
- Campylobacter spp. (0.8 million, 9%).
Table 1. Estimated annual number of domestically acquired foodborne hospitalizations and deaths caused by 31 pathogens, United States*
| Pathogen | Estimated annual number of hospitalizations
| Estimated annual number of deaths
|
| Hospitalization rate, %† | Death rate, %† | |
| Bacteria | ||
| Bacillus cereus, foodborne‡ | 0.4 | 0 |
| Brucella spp. | 55 | 0.9 |
| Campylobacter spp. | 17.1 | 0.1 |
| Clostridium botulinum, foodborne‡ | 82.6 | 17.3 |
| Clostridium perfringens, foodborne‡ | 0.6 | <0.1 |
| STEC O157 | 46.2 | 0.5 |
| STEC non-O157 | 12.8 | 0.3 |
| ETEC, foodborne‡ | 0.8 | 0 |
| Diarrheagenic E. coli other than STEC and ETEC | 0.8 | 0 |
| Listeria monocytogenes | 94 | 15.9 |
| Mycobacterium bovis | 55 | 4.7 |
| Salmonella spp., nontyphoidal | 27.2 | 0.5 |
| S. enterica serotype Typhi | 75.7 | 0 |
| Shigella spp. | 20.2 | 0.1 |
| Staphylococcus aureus, foodborne‡ | 6.4 | <0.1 |
| Streptococcus spp. group A, foodborne‡ | 0.2 | 0 |
| Vibrio cholerae, toxigenic | 43.1 | 0 |
| V. vulnificus | 91.3 | 34.8 |
| V. parahaemolyticus | 22.5 | 0.9 |
| Vibrio spp., other | 37.1 | 3.7 |
| Yersinia enterocolitica | 34.4 | 2 |
| Parasites | ||
| Cryptosporidium spp. | 25 | 0.3 |
| Cyclospora cayetanensis | 6.5 | 0 |
| Giardia intestinalis | 8.8 | 0.1 |
| Toxoplasma gondii | 2.6 | 0.2 |
| Trichinella spp. | 24.3 | 0.2 |
| Viruses | ||
| Astrovirus | 0.4 | <0.1 |
| Hepatitis A virus | 31.5 | 2.4 |
| Norovirus | 0.03 | <0.1 |
| Rotavirus | 1.7 | <0.1 |
| Sapovirus | 0.4 | <0.1 |
Footnotes:
*All estimates were based on US population in 2006. STEC = Shiga toxin–producing Escherichia coli; ETEC = enterotoxigenic E. coli.
†For laboratory-confirmed illnesses. Unadjusted hospitalization and death rates are presented. These rates were doubled to adjust for underdiagnosis before being applied to the number of laboratory-confirmed cases to estimate the total number of hospitalizations and deaths. The hospitalization and death rates for astrovirus, norovirus, rotavirus, and sapovirus are the percent of total estimated illness and were not subject to further adjustment.
‡Estimates based on the number of foodborne illnesses ascertained in surveillance and therefore assumed to reflect only foodborne transmission.
[Source 4]See your doctor if:
- the diarrhea lasts for more than 2 days in an adult, or for more than 24 hours in a baby
- you get dehydrated
- you also have a fever
- you have severe pain in your abdomen or rectum
- the diarrhea is bloody or black
- your child is very young or small (aged below 6 months or weighs less than 8 kg)
- your child is born preterm, or has other chronic conditions
- your child is passing less than 4 wet nappies/day
- you or your child is passing any blood in the stool
- you or your child is having dark green (bile) vomits
- you or your child vomits blood
- you or your child is having severe abdominal pain
- you or your child less than 3 years old and has a fever more than 101.3 °F (38.5° C)
- you or your child is showing signs of dehydration (very thirsty, cold hands and feet, dry lips and tongue, sunken eyes, sunken fontanelle, sleepy or drowsy)
- you or your child is unable to tolerate any oral intake because of severe vomiting
- you or your child becomes unusually drowsy
- vomiting persists more than two days
- diarrhea persists more than several days
- diarrhea turns bloody
- lightheadedness or fainting occurs with standing
- confusion develops
- worrisome abdominal pain develops
Foodborne illness complications
The most common serious complication of foodborne illness is dehydration — a severe loss of water and essential salts and minerals. If you’re a healthy adult and drink enough to replace fluids you lose from vomiting and diarrhea, dehydration shouldn’t be a problem.
Infants, older adults and people with suppressed immune systems or chronic illnesses may become severely dehydrated when they lose more fluids than they can replace. In that case, they may need to be hospitalized and receive intravenous fluids. In extreme cases, dehydration can be fatal.
Some types of foodborne illness have potentially serious complications for certain people. These include:
- Listeria monocytogenes. Complications of a listeria food poisoning may be most severe for an unborn baby. Early in pregnancy, a listeria infection may lead to miscarriage. Later in pregnancy, a listeria infection may lead to stillbirth, premature birth or a potentially fatal infection in the baby after birth — even if the mother was only mildly ill. Infants who survive a listeria infection may experience long-term neurological damage and delayed development.
- Escherichia coli (E. coli). E. coli is commonly divided into two broad types, Shiga toxin–producing—of which E. coli O157:H7 is the best studied—and non-Shiga toxin–producing, which includes enteropathogenic, enteroinvasive, enteroaggregative, and diffusely adherent E. coli. Certain E. coli strains can cause a serious complication called hemolytic uremic syndrome. This syndrome damages the lining of the tiny blood vessels in the kidneys, sometimes leading to kidney failure. Older adults, children younger than 5 and people with weakened immune systems have a higher risk of developing this complication. If you’re in one of these risk categories, see your doctor at the first sign of profuse or bloody diarrhea.
What causes foodborne illness
Many different disease-causing germs can contaminate foods, so there are many different foodborne infections.
- Researchers have identified more than 250 foodborne diseases.
- Most of them are infections, caused by a variety of bacteria, viruses, and parasites.
- Harmful toxins and chemicals also can contaminate foods and cause foodborne illness.
Contamination of food can happen at any point of production: growing, harvesting, processing, storing, shipping or preparing. Cross-contamination — the transfer of harmful organisms from one surface to another — is often the cause. This is especially troublesome for raw, ready-to-eat foods, such as salads or other produce. Because these foods aren’t cooked, harmful organisms aren’t destroyed before eating and can cause food poisoning.
Many bacterial, viral or parasitic agents cause food poisoning. The following table shows some of the possible contaminants, when you might start to feel symptoms and common ways the organism is spread.
Table 1. Common causes of foodborne illness
| Germs | Onset of symptoms | Typical Signs and Symptoms | Foods affected and means of transmission |
|---|---|---|---|
| Bacillus cereus (food poisoning) | 10 to 16 hours | Abdominal cramps, nausea, watery diarrhea | Gravy, meats, stews, vanilla sauce |
| Campylobacter jejuni (campylobacteriosis) | 2 to 5 days | Diarrhea (often bloody), stomach cramps/pain, fever and vomiting | Meat and poultry. Contamination occurs during processing if animal feces contact meat surfaces. Other sources include unpasteurized milk and contaminated water. |
| Clostridium botulinum (Botulism) | 18 to 72 hours | Double or blurred vision, drooping eyelids, slurred speech. Difficulty swallowing, breathing and dry mouth. Muscle weakness and paralysis. Symptoms start in the head and move down as severity increases | Home-canned foods with low acidity, improperly canned commercial foods, smoked or salted fish, potatoes baked in aluminum foil, and other foods kept at warm temperatures for too long. |
| Clostridium perfringens (food poisoning) | 6 to 24 hours | Intense abdominal cramps and watery diarrhea. Vomiting and fever are uncommon. Usually begins suddenly and lasts for less than 24 hours | Meats, stews and gravies. Commonly spread when serving dishes don’t keep food hot enough or food is chilled too slowly. |
| Cryptosporidium (cryptosporidiosis) | 2 to 10 days | Abdominal cramps, diarrhea (usually watery), slight fever | Contaminated drinking water, cooked foods that are not reheated after contact with an infected food handler, uncooked foods. |
| Cyclospora cayetanensis (cyclosporiasis) | 1 week | Watery diarrhea, loss of appetite and weight loss. Stomach cramps/pain, bloating, increased gas, nausea, and fatigue. | Raw fruits or vegetables, and herbs |
| Escherichia coli (traveler’s diarrhea) | 1 to 3 days | Abdominal cramps, vomiting, watery diarrhea. | Food or water contaminated with human feces |
| Escherichia coli (E. coli) O157:H7 | 3 to 4 days | Severe stomach cramps, diarrhea (often bloody), and vomiting. Around 5-10% of people diagnosed with this infection develop a life-threatening complication and can cause kidney failure. | Beef contaminated with feces during slaughter. Spread mainly by undercooked ground beef. Other sources include unpasteurized milk and apple cider, alfalfa sprouts, and contaminated water. |
| Giardia lamblia | 1 to 2 weeks | Diarrhea, gas, greasy stools that tend to float, stomach or abdominal cramps, nausea/vomiting | Raw, ready-to-eat produce and contaminated water. Can be spread by an infected food handler. |
| Hepatitis A | 28 days | Fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, diarrhea, clay-colored stools, joint pain, jaundice (yellowing of the skin and eyes) | Raw, ready-to-eat produce and shellfish from contaminated water. Can be spread by an infected food handler. |
| Listeria monocytogenes (listeriosis) | 1 to 4 weeks | Pregnant women typically experience fever and other flu-like symptoms, such as fatigue and muscle aches. Infections during pregnancy can lead to serious illness or even death in newborns. Other people (most often older adults): headache, stiff neck, confusion, loss of balance and convulsions in addition to fever and muscle aches. | Hot dogs, luncheon meats, unpasteurized milk and cheeses, and unwashed raw produce. Can be spread through contaminated soil and water. Queso fresco and other soft cheeses, raw sprouts, melons, hotdogs, pâtés, deli meats, smoked seafood, and raw (unpasteurized) milk. |
| Noroviruses (Norwalk-like viruses) | 12 to 48 hours | Diarrhea, nausea/stomach pain, vomiting | Raw, ready-to-eat produce and shellfish from contaminated water. Can be spread by an infected food handler or by touching contaminated surfaces. |
| Rotavirus | 1 to 3 days | Diarrhea, vomiting, fever, and abdominal pain | Raw, ready-to-eat produce. Can be spread by an infected food handler. |
| Salmonella (salmonellosis) | 12 to 72 hours | Diarrhea, fever, stomach cramps, vomiting | Raw or contaminated meat, poultry, unpasteurized milk or juice, cheese, raw fruits, vegetables and egg yolks. Survives inadequate cooking. Can be spread by knives, cutting surfaces or an infected food handler. |
| Shigella (shigellosis or bacillary dysentery) | 24 to 48 hours | Diarrhea, fever, and stomach cramps | Seafood and raw, ready-to-eat produce. Can be spread by an infected food handler. |
| Staphylococcus aureus | 30 minutes to 6 hours | Nausea, vomiting, and stomach cramps. Most people also have diarrhea. | Meats and prepared salads, cream sauces, and cream-filled pastries. Can be spread by hand contact, coughing and sneezing. |
| Vibrio parahaemolyticus | 4 to 96 hours | Abdominal cramps, fever, nausea, vomiting, watery diarrhea (occasionally bloody) | Undercooked or raw seafood |
| Vibrio vulnificus | 1 to 4 days | Watery diarrhea, nausea. stomach cramps, vomiting, fever, chills | Raw oysters and raw or undercooked mussels, clams, and whole scallops. Can be spread through contaminated seawater. |
Foodborne Pathogens Associated with Fever and Vomiting 5:
- Fever
- Characteristically associated
- Campylobacter jejuni
- Shigella
- Vibrio cholerae non-O1
- Often associated
- Norovirus
- Salmonella
- Vibrio parahaemolyticus
- Characteristically associated
- Vomiting
- Characteristically associated
- Bacillus cereus (emetic syndrome)
- Norovirus
- Staphylococcus aureus
- Often associated
- Clostridium botulinum
- Vibrio cholerae O1
- Vibrio parahaemolyticus
- Characteristically associated
Risk factors for getting foodborne illness
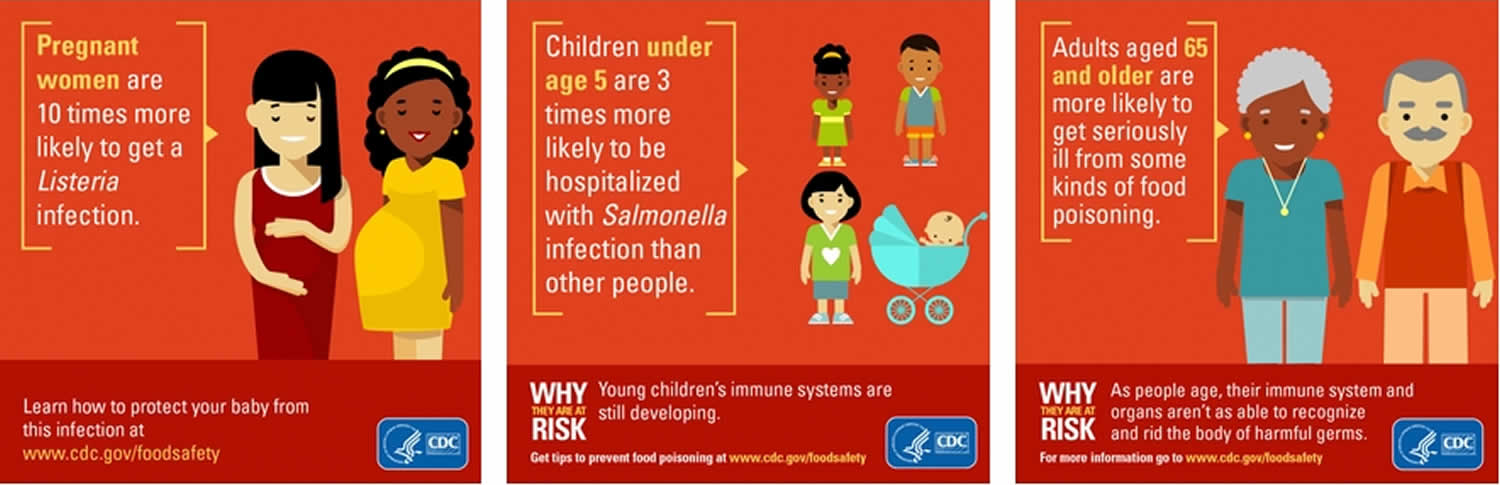
Whether you become ill after eating contaminated food depends on the organism, the amount of exposure, your age and your health. High-risk groups include:
- Older adults. As you get older, your immune system may not respond as quickly and as effectively to infectious organisms as when you were younger. Nearly half of people aged 65 and older who have a lab-confirmed foodborne illness from Salmonella, Campylobacter, Listeria or E. coli are hospitalized.
- Pregnant women. During pregnancy, changes in metabolism and circulation may increase the risk of foodborne illness. Your reaction may be more severe during pregnancy. For example, pregnant women are 10 times more likely to get a Listeria infection. Rarely, your baby may get sick, too.
- Infants and young children. Their immune systems haven’t fully developed, so their body’s ability to fight germs and sickness isn’t as strong. Foodborne illness can be particularly dangerous for them because illness can lead to diarrhea and dehydration. Children younger than 5 are three times more likely to be hospitalized if they get a Salmonella infection. And kidney failure strikes 1 out of 7 children under age 5 who are diagnosed with E. coli O157 infection.
- People with weakened immune systems. Having weakened immune systems — due to diabetes, liver disease or AIDS — or receiving chemotherapy or radiation therapy for cancer reduces your immune response and you cannot fight germs and sickness as effectively. For example, people on dialysis are 50 times more likely to get a Listeria infection.
Foodborne illness is especially serious and potentially life-threatening for young children, pregnant women and their fetuses, older adults, and people with weakened immune systems. These individuals should take extra precautions by avoiding the following foods:
- Raw or rare meat and poultry
- Raw or undercooked fish or shellfish, including oysters, clams, mussels and scallops
- Raw or undercooked eggs or foods that may contain them, such as cookie dough and homemade ice cream
- Raw sprouts, such as alfalfa, bean, clover and radish sprouts
- Unpasteurized juices and ciders
- Unpasteurized milk and milk products
- Soft cheeses, such as feta, Brie and Camembert; blue-veined cheese; and unpasteurized cheese
- Refrigerated pates and meat spreads
- Uncooked hot dogs, luncheon meats and deli meats
Foods linked to foodborne illness
Some foods are more associated with foodborne illnesses and food poisoning than others. They can carry harmful germs that can make you very sick if the food is contaminated.
- Raw foods of animal origin are the most likely to be contaminated, specifically raw or undercooked meat and poultry, raw or lightly cooked eggs, unpasteurized (raw) milk, and raw shellfish.
- Fruits and vegetables also may get contaminated.
- While certain foods are more likely to make you sick, any food can get contaminated in the field, during processing, or during other stages in the food production chain, including through cross-contamination with raw meat in kitchens.
Chicken, Beef, Pork, and Turkey
Raw and undercooked meat and poultry can make you sick. Most raw poultry contains Campylobacter. It also may contain Salmonella, Clostridium perfringens, and other bacteria. Raw meat may contain Salmonella, E. coli, Yersinia, and other bacteria.
- You should not wash raw poultry or meat before cooking it, even though some older recipes may call for this step. Washing raw poultry or meat can spread bacteria to other foods, utensils, and surfaces, and does not prevent illness.
- Thoroughly cooking poultry and meat destroys germs. You can kill bacteria by cooking poultry and meat to a safe internal temperature.
- Use a cooking thermometer to check the temperature. You can’t tell if meat is properly cooked by looking at its color or juices.
- Leftovers should be refrigerated at 40°F (4 °C) or colder within 2 hours after preparation. Large cuts of meat, such as roasts or a whole turkey, should be divided into small quantities for refrigeration so they’ll cool quickly enough to prevent bacteria from growing.
Foodborne illness outbreak
When two or more people get the same illness and investigation shows it came from the same contaminated food or drink, the event is called a foodborne disease outbreak.
In 2017, CDC monitored between 18 and 37 potential food poisoning or related clusters each week, and investigated nearly 200 multistate clusters 6. These investigations identified confirmed or suspected vehicles of transmission. They also led to recalls of foods including soy nut butter, soft raw milk cheeses, and imported papayas.
Public health officials investigate outbreaks to control them, so more people do not get sick, and to learn how to prevent similar outbreaks from happening in the future.
For a list of foodborne outbreaks reported to CDC since 1998, please use NORS Dashboard (https://wwwn.cdc.gov/norsdashboard/), an online data tool from CDC’s National Outbreak Reporting System here (https://wwwn.cdc.gov/norsdashboard/).
Recent Foodborne Illness Outbreak Investigations in 2018
- Raw Chicken Products – Salmonella Infantis
- Ground Beef – Salmonella Newport
- Deli Ham – Listeria monocytogenes
- Ground Beef – E. coli O26
- Gravel Ridge Farms Shell Eggs – Salmonella Enteritidis
- Chicken – Salmonella I 4,[5]],12:i:-
- Raw Turkey Products – Salmonella Infections
- Hy-vee Spring Pasta Salad – Salmonella Sandiego
- Fresh Express Salad Mix Sold at McDonald’s Restaurants – Cyclospora
- Del Monte Fresh Produce Vegetable Trays – Cyclospora
- Imported Fresh Crab Meat – Vibrio parahaemolyticus
- Kellogg’s Honey Smacks Cereal – Salmonella Mbandaka
- Pre-Cut Melon – Salmonella Adelaide
- Shell Eggs – Salmonella Braenderup
- Romaine Lettuce – E. coli O157:H7
- Dried Coconut – Salmonella Typhimurium
- Chicken Salad – Salmonella Typhimurium
- Kratom – Salmonella I 4,[5],12:b:-
- Raw Sprouts – Salmonella Montevideo
- Frozen Shredded Coconut – Salmonella I 4,[5],12:b:- and Salmonella Newport
Table 2. List of Selected Foodborne Illness Outbreak Investigations, by Pathogen
| Escherichia coli (E. coli) | Listeria | Salmonella | Other pathogens |
|
|
|
|
Symptoms of foodborne illness
Foodborne illness can have various presentations, ranging from clinically mild illness that requires only outpatient care to severe illness that requires hospitalization. Most foodborne illnesses are associated with vomiting or diarrhea (more than three loose stools in 24 hours). Other common symptoms include fever, bloody diarrhea, abdominal cramping, headache, dehydration, muscle aches and painful joints 7. Patients may have several symptoms or only one.
The most common symptoms of foodborne illness are:
- Upset stomach
- Stomach cramps
- Nausea
- Vomiting
- Diarrhea
- Fever
After you consume a contaminated food or drink, it may take hours or days before you develop symptoms.
Early onset of vomiting and diarrhea results from ingestion of preformed toxins, most often Staphylococcus aureus or Bacillus cereus. Diarrhea within 24 hours of ingestion is most likely caused by Clostridium perfringens or Bacillus cereus. Diarrhea within 24 to 48 hours of ingestion is most often caused by Campylobacter jejuni in individual cases or Salmonella in outbreaks 7. Foodborne illnesses commonly associated with fever are caused by Vibrio cholerae non-O1, Shigella, and Campylobacter jejuni. Enterotoxins in the small bowel caused by E. coli, Clostridium perfringens, and viruses produce excessive secretions of fluids and electrolytes that overwhelm the large bowel; therefore, they are typically associated with watery diarrhea. Bloody diarrhea with abdominal pain should prompt consideration of inflammatory damage to the intestinal mucosa or an infection (e.g., Campylobacter jejuni, Salmonella enteritidis, enteroinvasive E. coli) affecting the large bowel.
Foodborne illness prevention
You can prevent foodborne illness by:
- Wash your hands, utensils and food surfaces often. Wash your hands well with warm, soapy water before and after handling or preparing food. Use hot, soapy water to wash utensils, cutting boards and other surfaces you use.
- Germs that cause food poisoning can survive in many places and spread around your kitchen.
- Wash hands for 20 seconds with soap and water before, during, and after preparing food and before eating.
- Wash your utensils, cutting boards, and countertops with hot, soapy water.
- Rinse fresh fruits and vegetables under running water.
- Keep raw foods separate from ready-to-eat foods. When shopping, preparing food or storing food, keep raw meat, poultry, fish and shellfish away from other foods. This prevents cross-contamination.
- Raw meat, poultry, seafood, and eggs can spread germs to ready-to-eat foods—unless you keep them separate.
- Use separate cutting boards and plates for raw meat, poultry, and seafood.
- When grocery shopping, keep raw meat, poultry, seafood, and their juices away from other foods.
- Keep raw meat, poultry, seafood, and eggs separate from all other foods in the fridge.
- Cook foods to a safe temperature. Food is safely cooked when the internal temperature gets high enough to kill germs that can make you sick. The only way to tell if food is safely cooked is to use a food thermometer. You can’t tell if food is safely cooked by checking its color and texture. You can kill harmful organisms in most foods by cooking them to the right temperature.
- 145°F (63 °C) for whole cuts of beef, pork, veal, and lamb (then allow the meat to rest for 3 minutes before carving or eating)
- 160°F (71 °C) for ground meats, such as beef and pork
- 165°F (74 °C) for all poultry, including ground chicken and turkey
- 165°F (74 °C) for leftovers and casseroles
- 145°F (63 °C) for fresh ham (raw)
- 145°F (63 °C) for fin fish or cook until flesh is opaque
- Refrigerate or freeze perishable foods promptly — within two hours of purchasing or preparing them. If the room temperature is above 90 °F (32.2 °C), refrigerate perishable foods within one hour. Keep your refrigerator below 40°F (4.4 °C) and know when to throw food out.
- Defrost food safely. Don’t thaw food at room temperature. The safest way to thaw food is to defrost it in the refrigerator. If you microwave frozen food using the “defrost” or “50 percent power” setting, be sure to cook it immediately.
- Throw it out when in doubt. If you aren’t sure if a food has been prepared, served or stored safely, discard it. Food left at room temperature too long may contain bacteria or toxins that can’t be destroyed by cooking. Don’t taste food that you’re unsure about — just throw it out. Even if it looks and smells fine, it may not be safe to eat.
Safe Minimum Cooking Temperatures
Use this chart and a food thermometer to ensure that meat, poultry, seafood, and other cooked foods reach a safe minimum internal temperature.
Remember, you can’t tell whether meat is safely cooked by looking at it. Any cooked, uncured red meats – including pork – can be pink, even when the meat has reached a safe internal temperature.
Why the Rest Time is Important
After you remove meat from a grill, oven, or other heat source, allow it to rest for the specified amount of time. During the rest time, its temperature remains constant or continues to rise, which destroys harmful germs.
Table 3. Safe Minimum Cooking Temperatures and Rest Time
| Category | Food | Temperature (°F) | Rest Time |
|---|---|---|---|
| Ground Meat & Meat Mixtures | Beef, Pork, Veal, Lamb | 160 | None |
| Turkey, Chicken | 165 | None | |
| Fresh Beef, Veal, Lamb | Steaks, roasts, chops | 145 | 3 minutes |
| Poultry | Chicken & Turkey, whole | 165 | None |
| Poultry breasts, roasts | 165 | None | |
| Poultry thighs, legs, wings | 165 | None | |
| Duck & Goose | 165 | None | |
| Stuffing (cooked alone or in bird) | 165 | None | |
| Pork and Ham | Fresh pork | 145 | 3 minutes |
| Fresh ham (raw) | 145 | 3 minutes | |
| Precooked ham (to reheat) | 140 | None | |
| Eggs & Egg Dishes | Eggs | Cook until yolk and white are firm | None |
| 160 | None | ||
| Leftovers & Casseroles | Leftovers | 165 | None |
| Casseroles | 165 | None | |
| Seafood | Fin Fish | 145 or cook until flesh is opaque and separates easily with a fork. | None |
| Shrimp, lobster, and crabs | Cook until flesh is pearly and opaque. | None | |
| Clams, oysters, and mussels | Cook until shells open during cooking. | None | |
| Scallops | Cook until flesh is milky white or opaque and firm. | None |
Foodborne illness diagnosis
Foodborne illness is often diagnosed based on a detailed history, including how long you’ve been sick, your symptoms and specific foods you’ve eaten. Your doctor will also perform a physical exam, looking for signs of dehydration.
Depending on your symptoms and health history, your doctor may conduct diagnostic tests, such as a blood test, stool culture or examination for parasites, to identify the cause and confirm the diagnosis.
For a stool culture, your doctor will send a sample of your stool to a laboratory, where a technician will try to identify the infectious organism. Newer techniques such as polymerase chain reaction (PCR) testing have become readily available and provide more rapid, reliable determination of specific pathogens. An organism-specific diagnosis can help clinicians to narrow treatment recommendations, aid public health professionals, and prevent unnecessary procedures. If an organism is found, your doctor likely will notify your local health department to determine if the foodborne illness is linked to an outbreak.
Other tests that can be considered include serum chemistry (including albumin levels), C-reactive protein levels, complete blood count, blood cultures, urinalysis, abdominal radiography, anoscopy, and endoscopy, if warranted by the severity and pattern of symptoms 9. In severe cases of infectious diarrhea, toxic megacolon should be considered, which can be identified on plain abdominal radiography 7. Severe inflammatory changes can also be seen on computed tomography. It may be reasonable to obtain blood cultures in patients with fever and diarrhea (with or without blood), because up to 1% of cases of nontyphoidal Salmonella infections are associated with bacteremia 9. Sigmoidoscopy or colonoscopy may be useful in hospitalized patients with bloody diarrhea to obtain tissue and histology, which could aid in the diagnosis.
Stool microscopy is rarely diagnostic, but the presence of red and white blood cells may signal a colonic source 7 Its primary use is identification of ova, cysts, and parasites, although antigen testing is more sensitive and specific for Giardia. Microscopic evaluation for fecal polymorphonuclear leukocytes or lactoferrin measurements may be useful if an inflammatory etiology is suspected. A positive stool culture is more likely when analysis indicates an inflammatory process. Compared with leukocyte examinations, lactoferrin measurements are more sensitive but more expensive, have a higher false-positive rate, and require a fresh-cup sample examined by an experienced microscopist 9.
In some cases, the cause of foodborne illness can’t be identified.
Foodborne illness treatment
Treatment for foodborne illness typically depends on the source of the illness, if known, and the severity of your symptoms. For most people, the illness resolves without treatment within a few days, though some types of food poisoning may last longer.
Treatment of food poisoning may include:
- Replacement of lost fluids. Fluids and electrolytes — minerals such as sodium, potassium and calcium that maintain the balance of fluids in your body — lost to persistent diarrhea need to be replaced. Some children and adults with persistent diarrhea or vomiting may need hospitalization, where they can receive salts and fluids through a vein (intravenously), to prevent or treat dehydration.
- Antibiotics. Your doctor may prescribe antibiotics if you have certain kinds of bacterial food poisoning and your symptoms are severe. Food poisoning caused by listeria needs to be treated with intravenous antibiotics during hospitalization. The sooner treatment begins, the better. During pregnancy, prompt antibiotic treatment may help keep the infection from affecting the baby. Antibiotics will not help food poisoning caused by viruses. Antibiotics may actually worsen symptoms in certain kinds of viral or bacterial food poisoning. Talk to your doctor about your options.
Adults with diarrhea that isn’t bloody and who have no fever may get relief from taking the medication loperamide (Imodium A-D) or bismuth subsalicylate (Pepto-Bismol). Ask your doctor about these options.
Antibiotics
Empiric antibiotics
Most cases of acute infectious diarrhea are viral, and improper use of empiric antibiotics is associated with increased morbidity caused by adverse effects and Clostridium difficile colitis. Empiric antibiotics should be considered in cases of suspected foodborne illness only if the patient is febrile and has signs of invasive disease (e.g., gross hematochezia, leukocytes on fecal smear), if symptoms have persisted for more than one week or are severe (i.e., more than eight liquid stools per day), or if hospitalization may be required 10. A fluoroquinolone (or trimethoprim/sulfamethoxazole in children) is generally recommended for empiric antibiotic therapy 9. Stool testing should still be performed.
Empiric antibiotic therapy decreases the duration of symptoms in patients with traveler’s diarrhea 11. Enterotoxigenic E. coli is the most common cause of traveler’s diarrhea worldwide and is generally susceptible to ciprofloxacin, but azithromycin (Zithromax) is equally effective and a better choice in areas where fluoroquinolone-resistant Campylobacter jejuni is present 12. Patients with diarrhea of more than 10 days’ duration that is associated with fatty or foul-smelling stools, cramps, bloating, and weight loss can be treated empirically for Giardia infection 13. Because of an increased risk of hemolytic uremic syndrome, patients receiving empiric antibiotic therapy should be monitored closely if Shiga toxin–producing E. coli infection is suspected 14.
Targeted antibiotics
If empiric treatment has not been initiated, antibiotic therapy may be indicated once stool culture, bacterial toxin, or microscopy results are available. Antibiotic therapy can shorten the duration of symptoms and may prevent bacteremia in older adults, newborns, and immunocompromised patients 7. Recommended treatment regimens for foodborne pathogens are outlined in Table 4. Ciprofloxacin is no longer recommended for treatment of Campylobacter infection; a macrolide, such as erythromycin, is recommended instead 15.
Table 4. Recommended Treatment Regimens for Foodborne Pathogens
| Pathogen | Recommended regimen for adults | Recommended regimen for children | ||
|---|---|---|---|---|
Bacteria | ||||
Campylobacter | Erythromycin, 500 mg 2 times per day for 5 days | Azithromycin, 10 mg per kg per day for 3 to 7 days | ||
or | ||||
Azithromycin (Zithromax), 500 mg on day 1, then 250 mg on days 2 through 5 | ||||
Escherichia coli (non-Shiga toxin–producing) | Ciprofloxacin, 500 mg 2 times per day for 3 days | TMP-SMX, 5/25 mg per kg 2 times per day for 3 days* | ||
or | or | |||
TMP/SMX, 160/800 mg 2 times per day for 3 to 7 days* | Azithromycin, 10 mg per kg per day for 3 to 7 days | |||
or | ||||
Azithromycin, 500 mg on day 1, then 250 mg on days 2 through 5 | ||||
E. coli (Shiga toxin–producing) | Not recommended | Not recommended | ||
Salmonella (nontyphoidal) | Generally not recommended† | Generally not recommended† | ||
If indicated: | If indicated: | |||
Ciprofloxacin, 500 mg 2 times per day for 5 to 7 days | TMP-SMX, 5/25 mg per kg 2 times per day for 5 to 7 days* | |||
or | or | |||
Azithromycin, 500 mg on day 1, then 250 mg on days 2 through 5‡ | Azithromycin, 10 mg per kg per day for 3 to 7 days | |||
or | or | |||
Ceftriaxone, 1 to 2 g per day intramuscularly or intravenously for 5 to 7 days | Ceftriaxone, 50 to 100 mg per kg per day intramuscularly or intravenously for 5 to 7 days | |||
Shigella | Ciprofloxacin, 500 mg 2 times per day for 3 days | TMP-SMX, 5/25 mg per kg 2 times per day for 3 days† | ||
or | or | |||
Azithromycin, 500 mg on day 1, then 250 mg on days 2 through 5 | Azithromycin, 10 mg per kg per day for 3 to 7 days | |||
Parasites | ||||
Cryptosporidium | Generally not recommended§ | Generally not recommended§ | ||
Entamoeba histolytica | Metronidazole (Flagyl), 750 mg 3 times per day for 5 to 10 days | Metronidazole, 30 to 50 mg per kg per day in 3 divided doses for 7 to 10 days | ||
plus | plus | |||
Paromomycin, 500 mg 3 times per day for 7 days, or iodoquinol (Yodoxin), 650 mg 3 times per day for 7 days | Paromomycin, 25 to 35 mg per kg per day in 3 divided doses for 5 to 10 days | |||
Giardia | Metronidazole, 250 to 750 mg 3 times per day for 7 to 10 days | Metronidazole, 30 to 50 mg per kg per day in 3 divided doses for 7 to 10 days | ||
TMP/SMX = trimethoprim/sulfamethoxazole.
*—If susceptible.
†—Antibiotic therapy is not recommended except in severe infections, patients younger than 6 months or older than 50 years, immunocompromised patients, and patients with prostheses, valvular heart disease, severe atherosclerosis, malignancy, or decreased renal function.
‡—Alternative dosing regimen for azithromycin in adults with salmonellosis: 1,000 mg on day 1, then 500 mg per day for 2 to 6 days.
§—Treatment for cryptosporidiosis is generally not recommended in immunocompetent patients. For persistent symptoms, some clinicians prescribe nitazoxanide (Alinia), although it has not been approved for this use and has not been proven superior to placebo. Dosing for adults and children 12 years and older is 500 mg orally every 12 hours for 3 days. Dosing for children 4 to 11 years of age is 200 mg of oral suspension every 12 hours for 3 days. Dosing for children 1 to 3 years of age is 100 mg of oral suspension every 12 hours for 3 days.
Home remedies for foodborne illness
Food poisoning often improves without treatment within 48 hours. To help keep yourself more comfortable and prevent dehydration while you recover, try the following:
- Let your stomach settle. Stop eating and drinking for a few hours.
- Try sucking on ice chips or taking small sips of water. You might also try drinking clear soda, clear broth or noncaffeinated sports drinks, such as Gatorade. You’re getting enough fluid when you’re urinating normally and your urine is clear and not dark.
- Ease back into eating. Gradually begin to eat bland, low-fat, easy-to-digest foods, such as soda crackers, toast, gelatin, bananas and rice. Stop eating if your nausea returns.
- Avoid certain foods and substances until you’re feeling better. These include dairy products, caffeine, alcohol, nicotine, and fatty or highly seasoned foods.
- Rest. The illness and dehydration can weaken and tire you.
- Tauxe RV. Emerging foodborne pathogens. Int J Food Microbiol. 2002;78:31–41. https://doi.org/10.1016/S0168-1605(02)00232-5[↩]
- Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM. Foodborne illness acquired in the United States—unspecified agents. Emerg Infect Dis. 2011;17:16–22.[↩]
- Foodborne Illnesses and Germs. https://www.cdc.gov/foodsafety/foodborne-germs.html[↩]
- Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne Illness Acquired in the United States—Major Pathogens. Emerging Infectious Diseases. 2011;17(1):7-15. doi:10.3201/eid1701.p11101[↩][↩]
- Diagnosis and Management of Foodborne Illness. Am Fam Physician. 2015 Sep 1;92(5):358-365. https://www.aafp.org/afp/2015/0901/p358.html[↩][↩]
- List of Selected Multistate Foodborne Outbreak Investigations. https://www.cdc.gov/foodsafety/outbreaks/multistate-outbreaks/outbreaks-list.html[↩]
- Conlon C. Food-borne diarrheal illness. In: Cohen J, ed. Infectious Diseases. 3rd ed. St. Louis, Mo.: Mosby; 2010.[↩][↩][↩][↩][↩]
- Safe Minimum Cooking Temperatures. https://www.foodsafety.gov/keep/charts/mintemp.html[↩]
- Guerrant RL, Van Gilder T, Steiner TS, et al.; Infectious Diseases Society of America. Practice guidelines for the management of infectious diarrhea. Clin Infect Dis. 2001;32(3):331–351.[↩][↩][↩][↩]
- Steffen R. Worldwide efficacy of bismuth subsalicylate in the treatment of travelers’ diarrhea. Rev Infect Dis. 1990;12(suppl 1):S80–S86.[↩]
- Löscher T, Alberer M. Clinical presentation and management of travelers’ diarrhea. In: Keystone JS, ed. Travel Medicine. 3rd ed. Philadelphia, Pa.: Elsevier/Saunders; 2012.[↩]
- Adachi JA, Ericsson CD, Jiang ZD, et al. Azithromycin found to be comparable to levofloxacin for the treatment of US travelers with acute diarrhea acquired in Mexico. Clin Infect Dis. 2003;37(9):1165–1171.[↩]
- DuPont HL; Practice Parameters Committee of the American College of Gastroenterology. Guidelines on acute infectious diarrhea in adults. Am J Gastroenterol. 1997;92(11):1962–1975.[↩]
- Wong CS, Jelacic S, Habeeb RL, Watkins SL, Tarr PI. The risk of the hemolyticuremic syndrome after antibiotic treatment of Escherichia coli O157:H7 infections. N Engl J Med. 2000;342(26):1930–1936[↩]
- Smith KE, Besser JM, Hedberg CW, et al.; Investigation Team. Quinolone-resistant Campylobacter jejuni infections in Minnesota, 1992–1998. N Engl J Med. 1999;340(20):1525–1532.[↩]