Contents
What is sinus infection
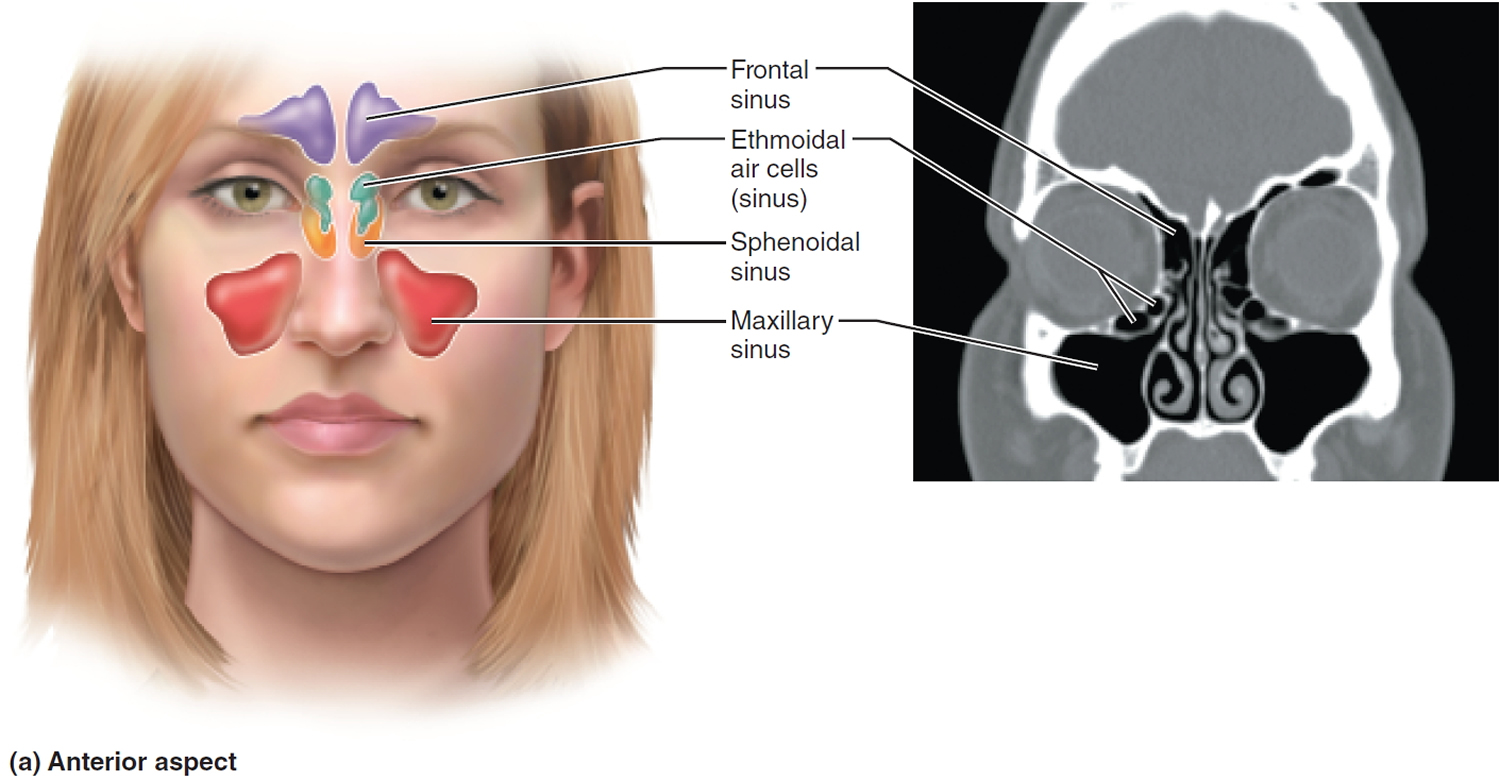
Inflammation or infection of the paransasal sinuses is called sinusitis, however rhinosinusitis is the more accurate term 1. Because sinusitis is often preceded by and almost always accompanied by, inflammation of the nasal mucosa (rhinitis), the term “rhinosinusitis” is used by otolaryngologists (ENT physicians) to replace the term “sinusitis”. The cause can be an infection or another problem. Your sinuses are hollow air spaces within the bones surrounding the nose (see Figure 1). They produce mucus, which drains into the nose. If your nose is swollen, this can block the sinuses and causes facial pain or pressure.
Sinus infection, also called rhinosinusitis, affects about 1 in 8 adults (more than 30 million Americans) annually and generally occurs when viruses or bacteria infect the sinuses (often during a cold) and begin to multiply 2. Rhinosinusitis is the fifth most common diagnosis for which antibiotics are prescribed in the United States 3. Moreover, chronic sinusitis effects approximately 15% of the U.S. population and is one of the most common chronic illnesses in America.
Part of the body’s reaction to the infection causes the sinus lining to swell, blocking the channels that drain the sinuses. This causes mucus and pus to fill up the nose and sinus cavities.
Viruses, bacteria, and nasal allergies are common causes of inflammation 4. The inflamed, swollen mucosa of the nasal and sinus cavities leads to obstruction of the openings of the sinuses, or ostia. Unable to circulate air and eliminate the secretions that are normally produced, the sinuses then become an ideal environment for bacterial infection.
There are several types of sinusitis, including 4:
- Acute, symptoms are present for 4 weeks or less
- Subacute, symptoms are present for more than 4 weeks, but less than 12 weeks
- Chronic, which lasts more than 12 weeks and can continue for months or even years. Chronic sinusitis is usually caused by prolonged inflammation, rather than a longstanding infection. Infection can be a part of chronic sinusitis, especially when it worsens from time to time, but is not usually the main cause.
- Recurrent, 4 or more acute episodes occurring within 1 year, with resolution of symptoms between episodes
- Acute exacerbation of chronic rhinosinusitis – an episode of worsening symptoms in a patient with chronic rhinosinusitis
Acute sinusitis often starts as a cold, which then turns into a bacterial infection. Allergies, nasal problems, and certain diseases can also cause acute and chronic sinusitis.
Symptoms of sinusitis can include fever, weakness, fatigue, cough, and congestion. There may also be mucus drainage in the back of the throat, called postnasal drip. Your health care professional diagnoses sinusitis based on your symptoms and an examination of your nose and face. You may also need imaging tests. Treatments include antibiotics, decongestants, and pain relievers. Using heat pads on the inflamed area, saline nasal sprays, and vaporizers can also help.
Paranasal Sinuses
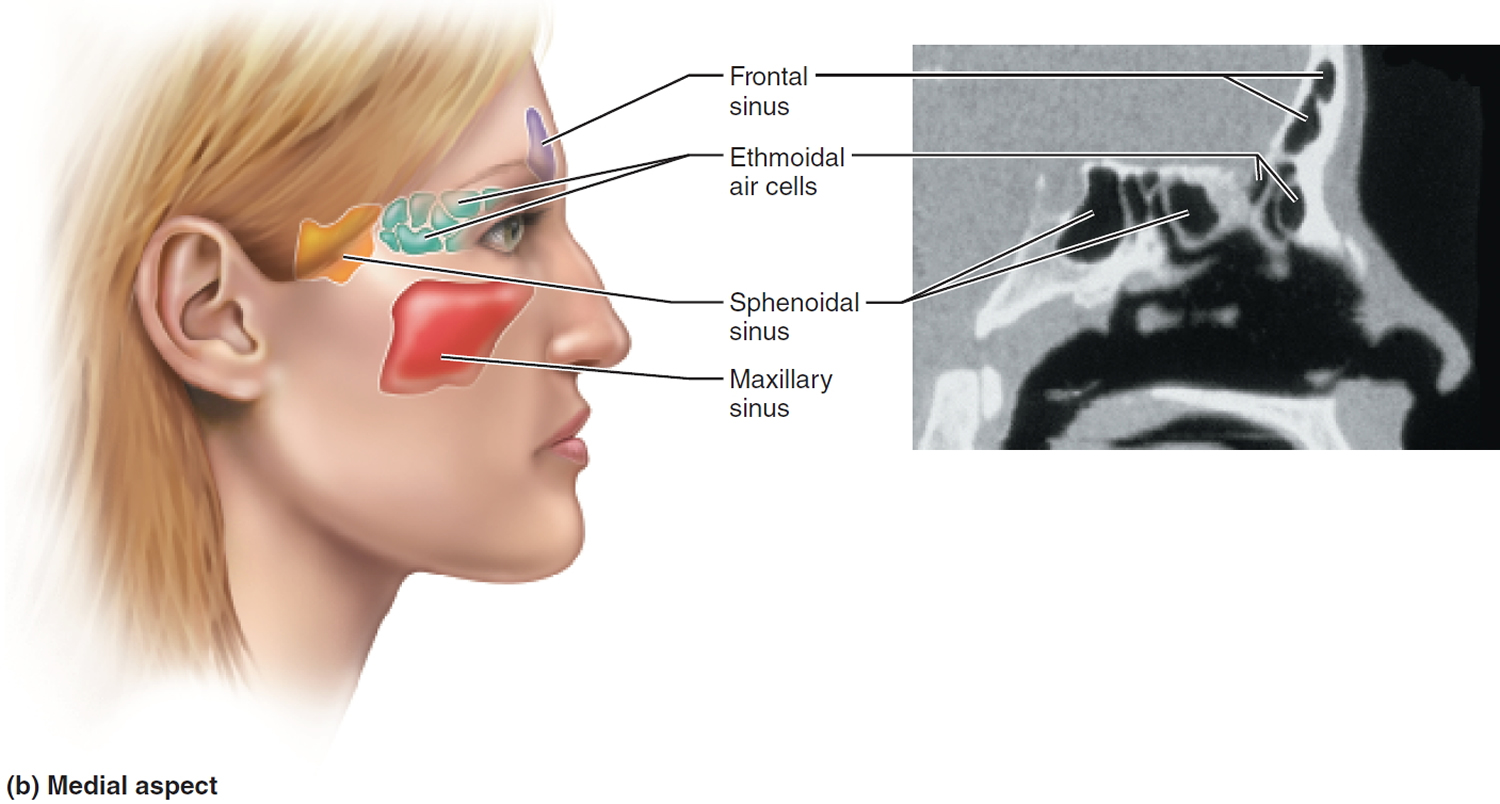
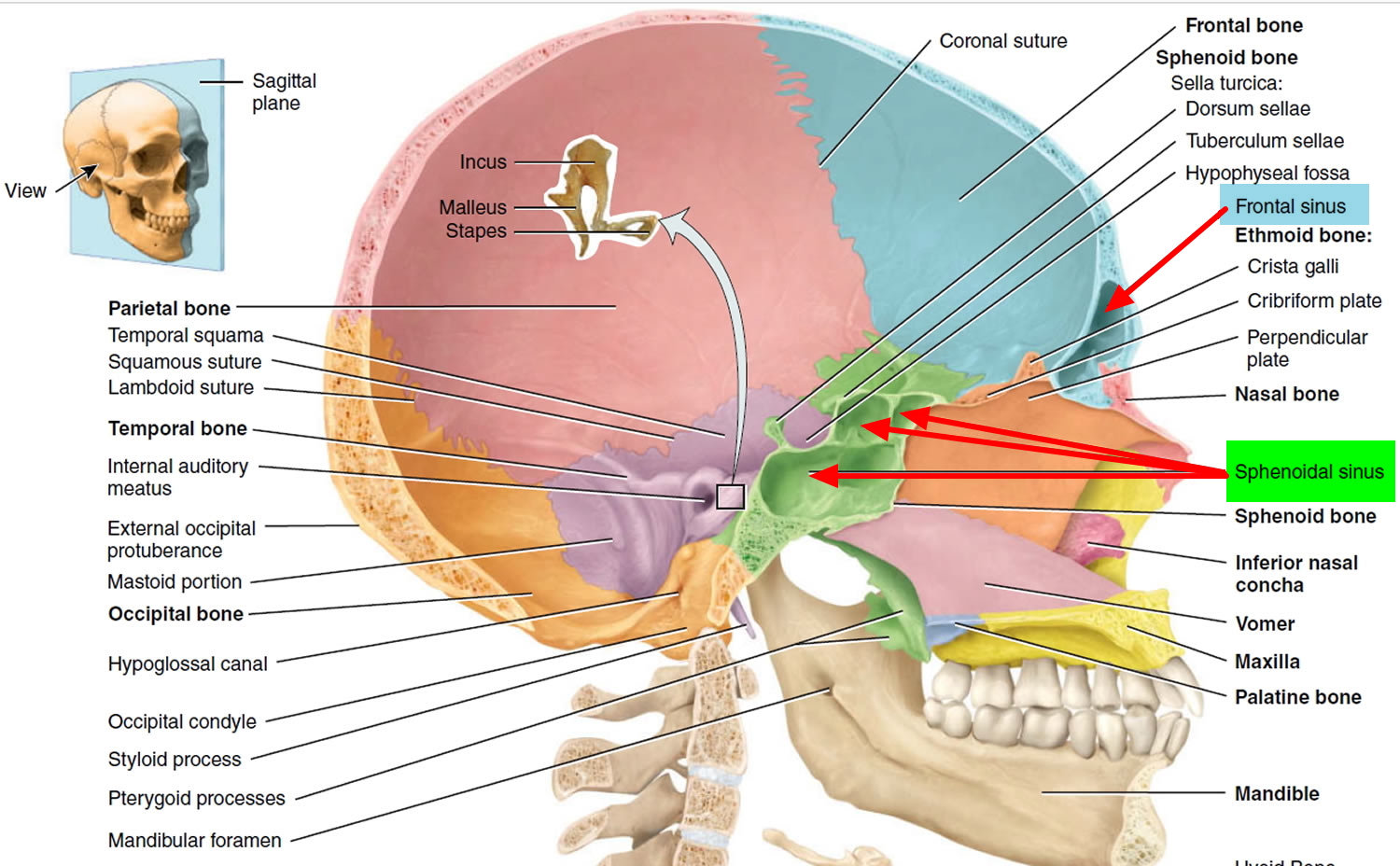
The bones surrounding the nasal cavity—the frontal, ethmoid, sphenoid, and both maxillary bones—contain hollow spaces internally. These air-filled sinuses are called paranasal sinuses because they cluster around the nasal cavity (Figures 1, 2 and 3). There are four paired sinuses, eight in total: 2 maxillary, 2 ethmoid (a honeycomb like structure with multiple smaller air cells within), 2 sphenoid, and 2 frontal sinuses. These sinuses open into the nasal cavity, are lined by the respiratory mucosa and perform the same air-processing functions as the nasal cavity and help warm, moisten, and filter inhaled air. Tiny hairs called cilia remove mucus from your sinuses so it can drain out into the nasal cavities and through your nose. The suctioning effect caused by nose blowing helps to drain them too.
The paranasal sinuses also lighten the skull, giving the bones they occupy a moth-eaten appearance in an X-ray image. These sinuses connect to the nasal cavity through small openings, most of which occur at the meatuses inferior to the conchae.
Figure 1. Paranasal sinuses (frontal view)
Figure 2. Paranasal sinuses (lateral view)
Figure 3. Paranasal sinuses lateral view
What causes sinus infection ?
The central event in sinusitis is blockage of the sinus openings, or ostia as a result of inflammation. Causes of sinonasal inflammation include:
- Viruses
- Bacteria
- Fungus
- Nasal allergy
- Reactive airway disease, such as Asthma and Samter’s triad
- Impaired ciliary motility: smoking, cystic fibrosis, Kartagener syndrome, immotile cilia syndrome
- Inflammatory diseases, such as Sarcoidosis and Wegener’s Granulomatosis
- Mucosal edema: preceding viral upper respiratory infection, allergic rhinitis, vasomotor rhinitis
- Immunodeficiencies, such as human immunodeficiency virus infection (HIV), AIDS and immunoglobulin deficiencies
- Previous surgery, resulting in scar tissue formation
- Mechanical obstruction: deviated nasal septum, nasal polyps, hypertrophic middle turbinates, tumor, trauma, foreign body, Wegener granulomatosis
- Growths called polyps. These can block your sinus passages.
- Trauma, resulting in facial fractures
- Changes in temperature or air pressure.
Certain factors increase your risk of sinusitis. These include:
- Having a cold
- Allergies
- Using decongestant nasal sprays too much
- Smoking
- Swimming or diving
- Dental infections and procedures
- Iatrogenic causes: sinus surgery, nasogastric tubes, nasal packing, mechanical ventilation.
Unable to circulate air and eliminate the secretions that are produced, obstructed sinuses become an ideal environment for bacterial infection.
Many different types of bacteria can infect the sinuses. The bacteria most often identified in acute sinusitis are:
- Streptococcus pneumoniae
- Hemophilus pneumoniae
- Moraxella catarrhalis
In chronic rhinosinusitis, it is not uncommon to find multiple bacteria present in a single culture sample. In addition, these organisms may demonstrate drug resistance, responding to only select antibiotics. Bacteria commonly cultured in chronic rhinosinusitis include:
- Staphylococcus aureus
- Gram negative organisms, such as Pseudomonas aeriginosa
How is sinus infection diagnosed ?
The diagnosis of sinusitis is made based on the subjective symptoms that a patient experiences combined with objective findings identified on examination or testing.
Your otolaryngologist will ask questions to determine exactly what symptoms you are experiencing and for how long.
Diagnostic symptoms include:
- Nasal drainage that is thick and discolored, or purulent
- Facial pain, pressure, or fullness, that often affects the cheeks, teeth, or area around the eyes
- Nasal congestion or obstruction
- Decreased sense of smell
During your visit your otolaryngologist will perform a head and neck examination and may recommend a procedure called nasal endoscopy. Nasal endoscopy is an examination of the nasal cavity that is performed with a small, lighted telescope. It is an office-based procedure that is typically performed after applying a nasal decongestant and anesthetic spray. Nasal endoscopy provides a more detailed and extensive examination of the nasal cavity that may be necessary to identify the objective inflammatory findings needed to make a diagnosis of sinusitis. If chronic sinusitis is suspected, but not clearly demonstrated on nasal endoscopy, your otolaryngologist may recommend a CT scan of sinuses to confirm the diagnosis.
In the first three to four days of illness, viral rhinosinusitis cannot be differentiated from early acute bacterial rhinosinusitis 5. A pattern of initial improvement followed by a worsening of symptoms—called double sickening—between days 5 and 10 of the illness is consistent with acute bacterial rhinosinusitis 6. Diagnosis of acute bacterial rhinosinusits is indicated when signs or symptoms of acute rhinosinusitis persist without evidence of improvement for at least 10 days beyond the onset of upper respiratory symptoms. After 10 days of upper respiratory symptoms, the probability of bacterial rhinosinusitis is 60% 7.
Symptoms of sinus infection
The symptoms of sinusitis include:
- Pain or pressure in your cheeks, forehead, and nose, or between your eyes
- Headache
- Nasal congestion
- Post nasal drip
- Ear pain, pressure, or fullness
- Fever
- Coughing, which may be worse at night
- drainage in your throat
- reduced sense of smell and taste
- Bad breath (called halitosis)
- Weakness
- Toothache
- Fatigue.
How is sinus infection treated ?
Much like the common cold, acute viral sinusitis resolves without treatment. Because viruses do not respond to antibiotic therapy, viral sinusitis is primarily managed with supportive care such as nasal saline rinses, rest and hydration. Medications, such as decongestants, mucolytics and pain relievers, may be offered by your physician to help decrease the severity of your symptoms.
The mainstay of treatment for acute bacterial sinusitis is an appropriate antibiotic, although some physicians and patients may prefer watchful waiting, as most acute bacterial infections will resolve without antibiotics. Your physician will base the choice of antibiotics on many factors, including:
- The most likely type of bacteria causing the infection
- Potential resistance of the bacteria to certain antibiotics
- Any medication allergies that you may have
- Other medications that you are taking
- Other medical conditions that you are being treated for
- Previous treatments that you have undergone
The duration of treatment is typically between 10-14 days. Pain relief should also be provided with either over the counter or prescription medications. As with acute viral sinusitis, additional medications, such as steroids, decongestants and mucolytics may be offered by your physician to help decrease the severity and duration of your symptoms. Nasal saline rinses are also often recommended.
Because of the vast number of underlying, often multiple, causes, the treatment of chronic sinusitis becomes more complicated. In general, however, chronic sinusitis requires more prolonged durations of medical therapy. Antibiotics, when required, are often based on the results of sinus cultures and are prescribed for 3-4 weeks time. A culture is a test that uses a sample of a patient’s mucous to determine which bacteria are present.
Watchful Waiting
Watchful waiting is appropriate in place of antibiotics for seven to 10 days after upper respiratory symptoms appear when there is assurance of follow-up 8. Antibiotic therapy should be considered if the patient’s condition does not improve by seven to 10 days after initial presentation or if symptoms worsen at any time 9. Symptomatic therapies should be offered to patients who are under observation. Physicians may also provide these patients with a safety net antibiotic prescription (also called a delayed prescription), with instructions describing when to fill the prescription. Watchful waiting is supported by four meta-analyses that were published after the 2007 American Academy of Otolaryngology–Head and Neck Surgery clinical practice guideline was released 10. These studies did not provide evidence confirming or disproving the American Academy of Otolaryngology–Head and Neck Surgery position that patients with more severe acute bacterial rhinosinusitis should initially be treated with antibiotics.
A Cochrane review showed that the symptoms of bacterial rhinosinusitis had resolved in 47% of all patients after seven days with or without antibiotic therapy 11. In addition, approximately 70% of patients improved within two weeks without antibiotics 12. Antibiotic therapy did increase cure rates for patients between seven and 15 days compared with placebo; however, the clinical benefit was small, with only 5% of patients having a faster cure 12. Moreover, analysis of individual patient data found that it was not possible to identify which patients with rhinosinusitis would benefit from antibiotics based on the presence of common clinical signs and symptoms 8. The number needed to treat was estimated to be 11 to 15 12. Adverse effects occurred more often with antibiotics than with placebo (number needed to harm = 8). The risk of harm outweighs the potential benefit of antibiotic therapy. As a result of this research, the 2015 American Academy of Otolaryngology–Head and Neck Surgery guideline recommends offering watchful waiting to patients regardless of illness severity.
Antibiotic Therapy
Antibiotics for the treatment of acute bacterial rhinosinusitis are outlined in Table 1 9. Most guidelines recommend amoxicillin with or without clavulanate as a first-line antibiotic for adults because of its safety, effectiveness, low cost, and narrow microbiologic spectrum 13. Amoxicillin/clavulanate (Augmentin) should be used in patients who are at high risk of bacterial resistance or who have comorbid conditions, as well as in those with moderate to severe infection 2. No significant differences in acute bacterial rhinosinusitis cure rates are noted between different antibiotic classes 3.
Respiratory fluoroquinolones are not recommended as first-line antibiotics because they conferred no benefit over beta-lactam antibiotics and are associated with a variety of adverse effects. According to a recent U.S. Food and Drug Administration safety alert, fluoroquinolones should be reserved for patients who do not have other treatment options 14. Macrolides, including azithromycin (Zithromax), trimethoprim/sulfamethoxazole, and second- or third-generation cephalosporins, are no longer recommended as initial therapy for acute bacterial rhinosinusitis because of high rates of resistance in S. pneumoniae and H. influenzae.
The recommended duration of therapy for uncomplicated acute bacterial rhinosinusitis is five to 10 days for most adults 3. This recommendation is based primarily on findings from a meta-analysis of 12 randomized controlled trials 15. A shorter treatment course (median of five days) may be just as effective as a longer course of treatment (median of 10 days) and is associated with fewer adverse effects. Regardless, clinicians should assess disease and symptom response before stopping antibiotic therapy prematurely, especially in older adults and in patients with underlying disease.
Treatment failure occurs when a patient’s symptoms do not improve by seven days after diagnosis or when they worsen at any time, with or without antibiotic therapy.1 If treatment failure occurs following initial antibiotic therapy, an alternative antibiotic with a broader spectrum is required. High-dose amoxicillin/clavulanate, a respiratory fluoroquinolone, or the combination of clindamycin plus a third-generation oral cephalosporin may be considered.
Table 1. Oral Antibiotics for the Treatment of Acute Bacterial Rhinosinusitis
| Antibiotic | Clinical effectiveness (%) | Dosage | Cost* | ||
|---|---|---|---|---|---|
First line for most patients | |||||
Amoxicillin (regular dose) | 83 to 88 | 500 mg every eight hours for five to 10 days | $15 (500-mg tablets) | ||
or | $11† (500-mg capsules) | ||||
875 mg every 12 hours for five to 10 days | $17 (875-mg tablets) | ||||
First line for coverage of beta lactamase–producing Haemophilus influenzae and Moraxella (Branhamella) catarrhalis | |||||
Amoxicillin/clavulanate (Augmentin; regular dose) | 90 to 92 | 500 mg/125 mg every eight hours for five to 10 days | $114 (500-mg/125-mg tablets) | ||
or | |||||
875 mg/125 mg every 12 hours for five to10 days | $101 (875-mg/125-mg tablets) | ||||
For possible Streptococcus pneumoniae resistance (e.g., child in household who attends day care) | |||||
Amoxicillin (high dose) | 83 to 88 | 1 g every eight hours for five to 10 days | $30 (500-mg tablets) | ||
or | $23† (500-mg capsules) | ||||
1 g four times per day for five to 10 days | $40 (500-mg tablets) | ||||
$30 (500-mg capsules) | |||||
For moderate to severe disease, high risk of resistance, recent antibiotic use, or treatment failure | |||||
Amoxicillin/clavulanate, extended release (Augmentin XR) | 90 to 92 | 2,000 mg/125 mg twice per day for 10 days | $1,608 (1,000-mg/62.5-mg tablets) | ||
For patients with penicillin allergy or as second-line antibiotic | |||||
Doxycycline | 77 to 81 | 100 mg twice per day or 200 mg once per day for five to 10 days | $123 (100-mg capsules) | ||
Levofloxacin (Levaquin)‡ | 90 to 92 | 500 mg per day for 10 to 14 days | $193 (500-mg tablets) | ||
or | |||||
750 mg every day for five days | $180 (750-mg tablets) | ||||
Moxifloxacin (Avelox)‡ | 90 to 92 | 400 mg per day for 10 days | $272 (400-mg tablets) | ||
Non–type I penicillin allergy or second-line antibiotic | |||||
Clindamycin | 77 to 81 | 300 mg three times per day for five to10 days | $112 (300-mg capsules) | ||
plus | |||||
Cefixime (Suprax) | 83 to 88 | 400 mg per day for 10 days | $277 (400-mg tablets) | ||
or | |||||
Cefpodoxime | 83 to 88 | 200 mg twice per day for 10 days | $169 (200-mg tablets) | ||
*—Estimated retail price of 10-day treatment course based on information obtained at http://online.lexi.com.
†—May be available at discounted prices at one or more national retail chains.
‡—Fluoroquinolones should be reserved for those who do not have alternative treatment options.
Symptomatic Treatment
Current guidelines consider analgesics, intranasal corticosteroids, and saline nasal irrigation to be options for the management of rhinosinusitis symptoms. They are recommended for use within the first 10 days but may be continued if antibiotics are initiated. Selection of interventions should be based on shared decision making. Decongestants, antihistamines, and guaifenesin are not recommended for patients with acute bacterial rhinosinusitis because of their unproven effectiveness, potential adverse effects, and cost. Table 2 summarizes adjunctive therapies for acute rhinosinusitis.
A 2013 Cochrane review found that patients receiving intranasal corticosteroids were more likely to experience symptom improvement after 15 to 21 days compared with those receiving placebo (73% vs. 66.4%; number needed to treat = 15) 17. Higher doses of intranasal corticosteroids had a greater effect on symptom relief than lower doses. Even though their benefits are only marginal,3 intranasal corticosteroids are often used as an adjunct to antibiotic therapy in the symptomatic treatment of acute bacterial sinusitis. They are likely most beneficial in patients with concurrent allergic rhinitis 3.
Saline Nasal Irrigation. Intranasal irrigations with either physiologic or hypertonic saline have been shown to improve mucociliary clearance and may be beneficial for the treatment of acute rhinosinusitis 18. One randomized controlled trial of 76 patients with frequent sinusitis found that daily hypertonic saline nasal irrigation decreases nasal symptoms and medication use 19. A Cochrane review concluded that saline nasal irrigation may relieve symptoms of upper respiratory infection 20. Despite limited evidence regarding effectiveness, saline nasal irrigation can be a safe and inexpensive adjunctive therapy for symptom relief in acute rhinosinusitis. It is important to inform patients to prepare irrigations using distilled, boiled, or filtered water because there have been reports of amebic encephalitis due to contaminated tap water rinses 21.
Decongestants. Oral decongestants have been shown to be modestly effective for short-term relief of symptoms in adults with the common cold by reducing nasal airway resistance 22. However, the effect of decongestants in the nasal cavity does not extend to the paranasal sinuses 23. There are currently no randomized controlled trials evaluating the effectiveness of decongestants in patients with sinusitis. Oral decongestants should be used with caution in patients with hypertension or cardiovascular disease. Topical decongestants should not be used for longer than 72 hours, owing to the potential for rebound congestion (rhinitis medicamentosa).
Antihistamines. Antihistamines are often used to relieve symptoms of excessive secretions and sneezing. However, there are no studies to support the effectiveness of antihistamine in acute rhinosinusitis 2. Antihistamines may also worsen congestion by overdrying the nasal mucosa. Current guidelines do not recommend antihistamines as an adjunctive therapy for acute bacterial rhinosinusitis, except in patients with a history of allergy 24.
Table 2. Adjunctive Therapies for Acute Rhinosinusitis
| Treatment | Evidence summary | Comment |
|---|---|---|
Intranasal corticosteroids | Two systematic reviews of randomized controlled trials showed minimal benefit and symptom relief occurred late (at 15 to 21 days) | Some agents available over the counter |
Saline nasal irrigation | One small randomized controlled trial found hypertonic saline decreased nasal symptoms | Available in a low-pressure method using a spray or squeeze bottle or a gravity-flow method using a vessel with a nasal spout |
Another study found no significant difference between groups receiving no treatment vs. those treated with saline nasal solutions, topical decongestants, and intranasal corticosteroids | ||
Oral decongestants | No clinical trial evidence for patients with acute sinusitis | Significant adverse effects; phenylephrine is similar in effectiveness to placebo for nasal congestion due to seasonal allergic rhinitis |
Topical decongestants | One comparative trial found no significant difference in improvement among groups receiving no treatment vs. those treated with saline nasal solutions, topical decongestants, and intranasal corticosteroids | May cause rebound congestion when used for prolonged periods |
Is chronic sinusitis treated differently than acute sinusitis ?
Because chronic sinusitis is caused more by inflammation than infection, the treatments for chronic sinusitis are meant to control the inflammation. Salt water nasal irrigation and/or nasal steroid sprays are the main treatments for the symptoms of chronic sinusitis. It may help to look for other factors that can go along with chronic sinusitis and possibly make the problem worse, and have them treated too. Some of these factors are allergies, nasal polyps, asthma, and problems with the body’s ability to fight infections.
When is surgery needed for sinus infection ?
Sinus surgery is reserved for patients with chronic sinusitis who have persistent symptoms despite medical therapy.
It must be remembered that sinusitis is an inflammatory process that needs to be treated aggressively with medication before considering surgery. Even after successful sinus surgery, most patients with chronic sinusitis will continue to require medication to control the underlying cause(s) of inflammation and prevent the return of symptoms.
For patients who fail to improve with appropriate medical treatment, sinus surgery is an excellent option. Today, sinus surgery is typically performed through the nose, endoscopically (endoscopic sinus surgery), with the use of a nasal endoscope to visualize the nasal cavity and sinuses, thus avoiding the need for incisions through the skin. The primary goal of endoscopic sinus surgery is to widen the natural drainage pathways between the sinuses and the nose, allowing mucus to get out of the sinuses and air to get in. Medications that are delivered to the surface of the nose and sinuses, like sprays and irrigations, can get into the sinuses better after surgery as well.
During the procedure, the surgeon locates and enlarges the small natural drainage passageways of the sinuses.
Very rarely patients with acute bacterial sinusitis will develop a complication when the infection spreads to adjacent structures such as the eye or the brain. Such complications are considered medical emergencies, requiring immediate treatment. Typically, surgery is also required in these patients in order to drain the collection of infection and enlarge the ostia of the responsible sinuses.
Home remedies for sinus infection
You can use a saline nasal spray. This will clean out your nasal passages and help clear congestion. Your doctor may suggest a decongestant nasal spray to treat swelling. Do not use this for more than 3 days. It can worsen the swelling in your sinuses once you stop using the medicine.
Decongestant medicines relieve sinus pain and pressure. In general, you should only use them short-term. Over-the-counter pain relievers can relieve pain and aches as well. Talk with your doctor before using an over-the-counter cold medicine. Some can make your symptoms worse or have other side effects.
Your doctor can prescribe allergy medicine to treat conditions caused by allergies. Severe cases caused by bacteria may require an antibiotic. Your doctor will instruct you to take this for 10 to 14 days. However, you often will start to feel better after taking it a few days. Make sure you finish all the medicine your doctor prescribes.
A process called nasal irrigation can provide relief. A saline solution through a device called a neti pot (which looks like a small teapot with a long spout) can flush out your sinuses and help loosen thick mucus. It is important to use distilled or sterile water, or tap water that has been boiled for 3 to 5 minutes and cooled. Regular tap water is not safe to use because it has not been properly filtered or treated. Some tap water contains organisms that can cause serious infections in your nasal passages.
There are many over-the-counter saline solutions available, but patients can make their own saline solution at home:
- 1 quart (4 cups) boiled or distilled water
- 1 teaspoon baking soda
- 1 teaspoon non-iodized salt
Sinusitis often goes away with treatment. There are things you can do at home to help.
- Get plenty of rest. Lying on your back can make your sinuses feel more blocked. Try lying on your side instead. This helps you breathe better. Or you can try propping yourself up with a pillow.
- Drink plenty of fluids. Sipping hot liquids can help soothe your throat.
- Apply heat. Try holding a warm, wet towel against your face. Or you can breathe in steam through a hot cloth or towel. This can relieve sinus pressure and help open your sinus passages.
- Avoid alcohol. It can worsen the swelling in your sinuses.
Analgesics. An over-the-counter analgesic, such as acetaminophen or a nonsteroidal anti-inflammatory drug, is often sufficient to relieve pain or fever in acute rhinosinusitis. Narcotics are not recommended because of potential adverse effects.
Contact your doctor if you:
- still have symptoms after 12 weeks
- get the condition several times in one year.
Sinus infection complications
Complications, such as orbital cellulitis, subperiosteal abscess, intraorbital abscess, altered mental status, meningitis, cavernous sinus thrombosis, intracranial abscess, Pott puffy tumor (osteomyelitis of frontal bone).
- Sinusitis. Medline Plus. https://medlineplus.gov/sinusitis.html[↩]
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 suppl):S1–S39.[↩][↩][↩]
- Chow AW, Benninger MS, Brook I, et al.; Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):e72–e112.[↩][↩][↩][↩]
- Sinusitis Q&A. American Rhinologic Society. http://care.american-rhinologic.org/sinusitis_q_a[↩][↩]
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152 (2 suppl):S10.[↩]
- Hwang PH. A 51-year-old woman with acute onset of facial pressure, rhinorrhea, and tooth pain: review of acute rhinosinusitis. JAMA. 2009;301(17):1798–1807.[↩]
- van den Broek MF, Gudden C, Kluijfhout WP, et al. No evidence for distinguishing bacterial from viral acute rhinosinusitis using symptom duration and purulent rhinorrhea: a systematic review of the evidence base. Otolaryngol Head Neck Surg. 2014;150(4):533–537.[↩]
- Young J, De Sutter A, Merenstein D, et al. Antibiotics for adults with clinically diagnosed acute rhinosinusitis: a meta-analysis of individual patient data. Lancet. 2008;371(9616):908–914.[↩][↩]
- Desrosiers M, Evans GA, Keith PK, et al. Canadian clinical practice guidelines for acute and chronic rhinosinusitis. J Otolaryngol Head Neck Surg. 2011;40(suppl 2):S99–S193.[↩][↩]
- Rosenfeld RM, Singer M, Jones S. Systematic review of antimicrobial therapy in patients with acute rhinosinusitis. Otolaryngol Head Neck Surg. 2007;137(3 suppl):S32–S45.[↩]
- [↩]
- Lemiengre MB, van Driel ML, Merenstein D, Young J, De Sutter AI. Antibiotics for clinically diagnosed acute rhinosinusitis in adults. Cochrane Database Syst Rev. 2012;(10):CD006089.[↩][↩][↩]
- Anon JB, Jacobs MR, Poole MD, et al.; Sinus And Allergy Health Partnership. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis [published correction appears in Otolaryngol Head Neck Surg. 2004; 130(6):794–796]. Otolaryngol Head Neck Surg. 2004;130(1 suppl):1–45.[↩]
- U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA advises restricting fluoroquinolone antibiotic use for certain uncomplicated infections; warns about disabling side effects that can occur together. http://www.fda.gov/Drugs/DrugSafety/ucm500143.htm[↩]
- Falagas ME, Karageorgopoulos DE, Grammatikos AP, Matthaiou DK. Effectiveness and safety of short vs. long duration of antibiotic therapy for acute bacterial sinusitis: a meta-analysis of randomized trials. Br J Clin Pharmacol. 2009;67(2):161–171.[↩]
- Current Concepts in Adult Acute Rhinosinusitis. Am Fam Physician. 2016 Jul 15;94(2):97-105. http://www.aafp.org/afp/2016/0715/p97.html#afp20160715p97-b1[↩][↩]
- Zalmanovici Trestioreanu A, Yaphe J. Intranasal steroids for acute sinusitis. Cochrane Database Syst Rev. 2013;(12):CD005149.[↩]
- Hauptman G, Ryan MW. The effect of saline solutions on nasal patency and mucociliary clearance in rhinosinusitis patients. Otolaryngol Head Neck Surg. 2007;137(5):815–821.[↩]
- Rabago D, Zgierska A, Mundt M, Barrett B, Bobula J, Maberry R. Efficacy of daily hypertonic saline nasal irrigation among patients with sinusitis: a randomized controlled trial. J Fam Pract. 2002;51(12):1049–1055.[↩]
- King D, Mitchell B, Williams CP, Spurling GK. Saline nasal irrigation for acute upper respiratory tract infections. Cochrane Database Syst Rev. 2015;(4):CD006821.[↩]
- Yoder JS, Straif-Bourgeois S, Roy SL, et al. Primary amebic meningoencephalitis deaths associated with sinus irrigation using contaminated tap water. Clin Infect Dis. 2012;55(9):e79–e85.[↩]
- Taverner D, Danz C, Economos D. The effects of oral pseudoephedrine on nasal patency in the common cold: a double-blind single-dose placebo-controlled trial. Clin Otolaryngol Allied Sci. 1999;24(1):47–51.[↩]
- Caenen M, Hamels K, Deron P, Clement P. Comparison of decongestive capacity of xylometazoline and pseudoephedrine with rhinomanometry and MRI. Rhinology. 2005;43(3):205–209.[↩]
- Braun JJ, Alabert JP, Michel FB, et al. Adjunct effect of loratadine in the treatment of acute sinusitis in patients with allergic rhinitis. Allergy. 1997;52(6):650–655.[↩]