Contents
What is a gluten allergy
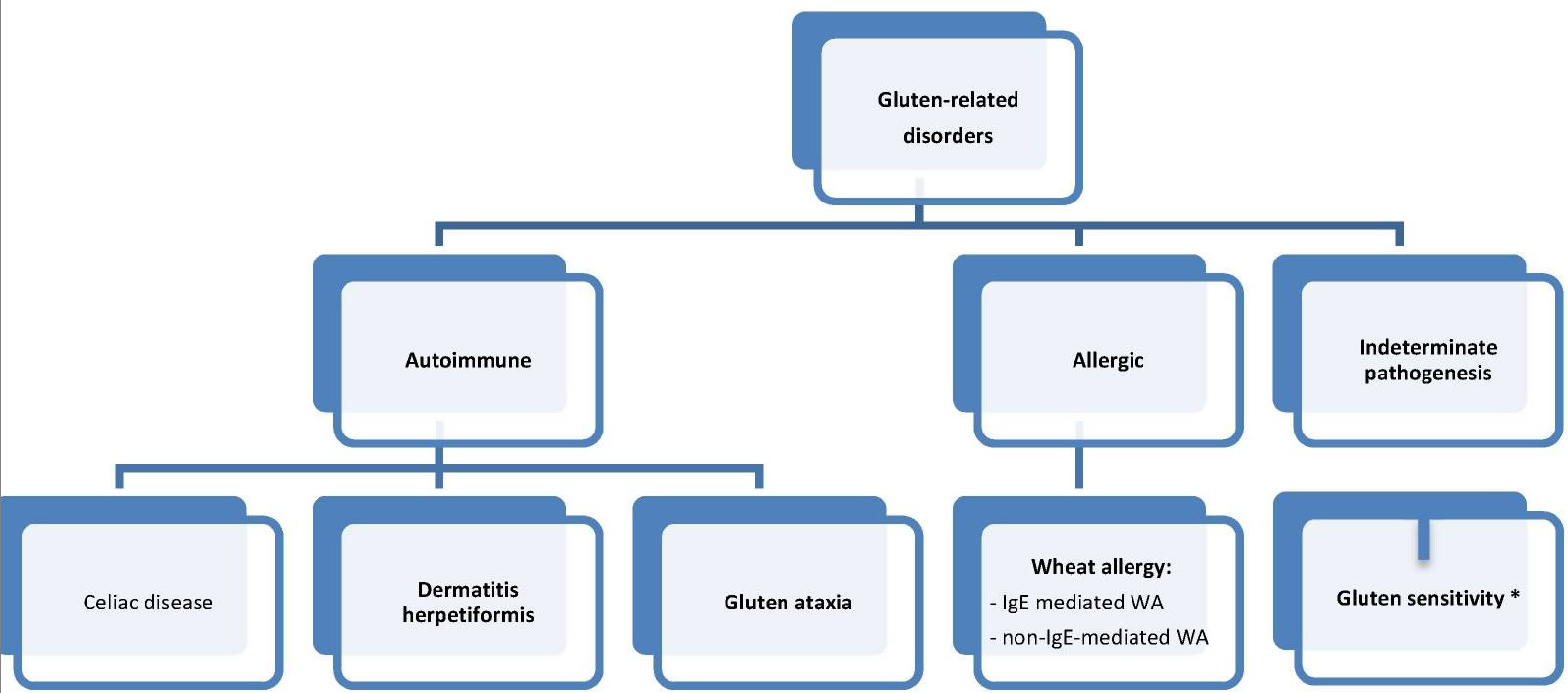
Gluten is a mix of protein (glutenins and gliadins) found in wheat, rye, and barley. It is found mainly in foods but may also be in other products like medicines, vitamins, and supplements. Gluten can cause two distinct immunological diseases: Celiac disease and IgE-mediated gluten allergy (also called wheat allergy) [see Figure 1 below]. In gluten allergy (wheat allergy) it is the cross-linking of immunoglobulin IgE by repeat sequences in gluten peptides (for example, serine-glutamine-glutamine -glutamine-(glutamine-)proline-proline-phenylalanine) that triggers the release of chemical mediators, such as histamine, from basophils and mast cells 1. In contrast, Celiac disease is an autoimmune disorder (your immune system attacks healthy cells in your body by mistake), as demonstrated by specific serologic autoantibodies, most notably serum anti-tissue transglutaminase (tTG) and anti-endomysial antibodies (EMA) 2. There are few cases of gluten allergy reported and little is known about its natural history 3.
Figure 1. Gluten related disorders classification (proposed new nomenclature and classification)
Note: Gluten sensitivity (GS) = non-celiac gluten sensitivity (NCGS).
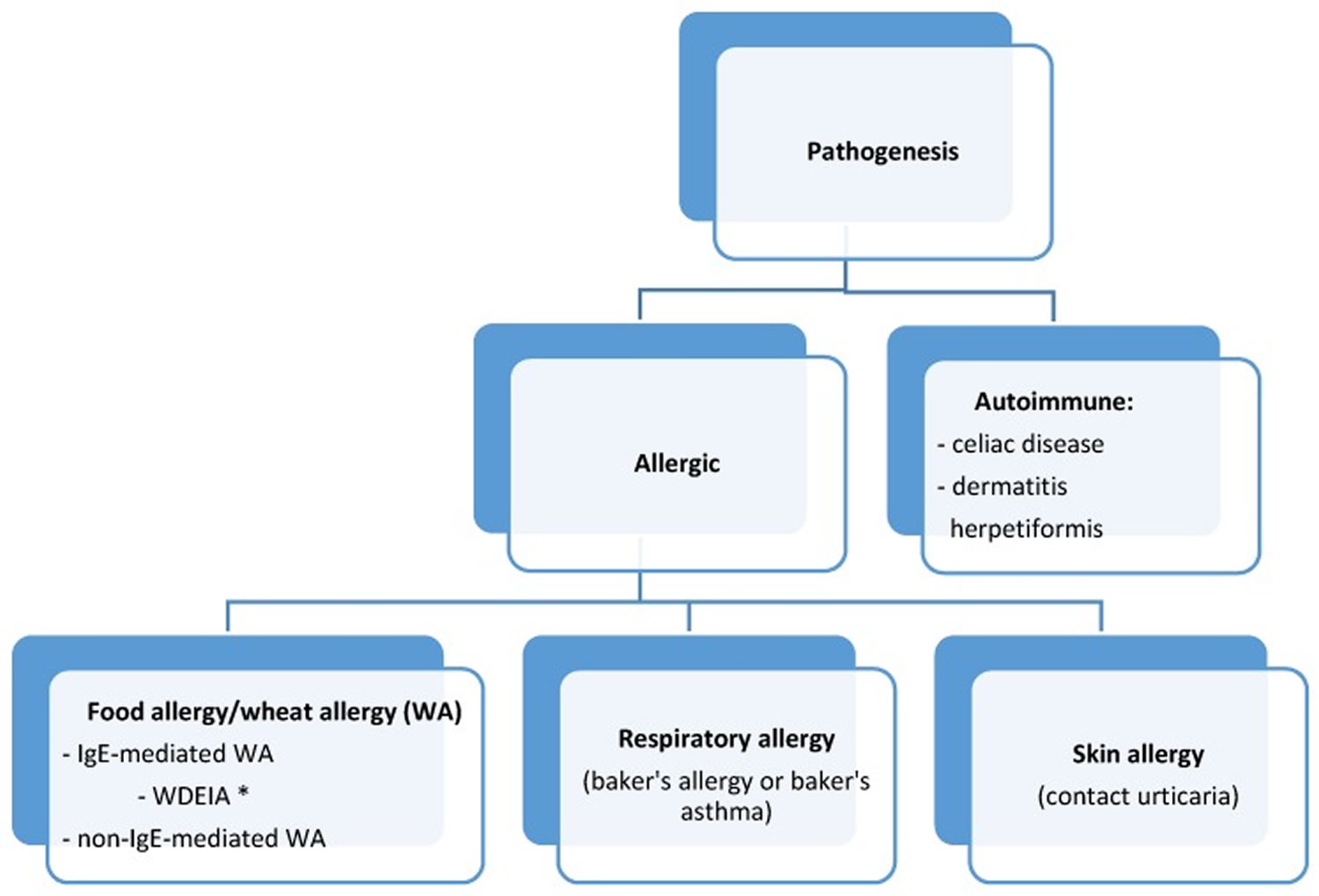
[Source 2]Gluten allergy (wheat allergy) is defined as an adverse immunologic reaction to wheat proteins 2. Depending on the routes of entry, wheat-related allergic disorders are classified into: food allergy affecting the skin, gastrointestinal tract or respiratory tract; wheat-dependent, exercise-induced anaphylaxis; occupational asthma (baker’s asthma) and rhinitis; and contact urticaria (Figure 2) 4. IgE antibodies play a central role in the pathogenesis of these diseases 2.
The allergy classifications also consider Celiac disease as a wheat-related allergic disorder. However, Celiac disease is, rather, an autoimmune disease and in most countries it is treated according to gastroenterological protocols. Food allergies triggered by wheat consumption are divided to IgE-dependent wheat allergy and IgE-non-dependent wheat allergy 4. One of the wheat allergy syndromes is also wheat-dependent exercise-induced anaphylaxis. In the latest European Academy of Allergy and Clinical Immunology classification it has been recognized as an independent form of wheat allergy 4.
Gluten allergy (wheat allergy) is also one of the gluten-related disorders, the classification of which was published in 2012 (see Figure 1 above) 2. It is important to note that although wheat allergy belongs to this group, all of its forms stem solely from the adverse effect of wheat proteins (including gluten proteins). Therefore, the treatment is based on the elimination of wheat grains only. The allergy induced by proteins contained in other gluten grains is less common and has not been included in the classification discussed herein.
Figure 2. Classification of gluten/wheat-related allergic diseases
Note: WDEIA = wheat-dependent exercise-induced anaphylaxis
[Source 5]Prevalence of IgE-Mediated Gluten (Wheat) Allergy
Wheat is one of the five most common foods that trigger allergic reactions in children. In Germany, Japan, and Finland it has been reported as the third most common allergen, after milk and egg 6. Wheat allergy prevalence, both in children and adults, is usually approximately 1% (0.4%–4%), depending on age and region 6, 7, 8, 9. In people with food allergies, wheat allergy is diagnosed in 11%–20% of children and in 25% of adults 10. Taking into account all gluten-related disorders, it has been estimated that about 3% of the human population suffers from wheat intolerance (1% WA, 1% celiac disease, 1% non-celiac gluten sensitivity) 11.
Figure 1. Gluten allergy rash
Gluten allergy signs and symptoms
Wheat allergy prevails chiefly in children with a family history of atopy. Almost all of the juvenile wheat allergy patients are diagnosed with allergies to other foods and other allergic disorders, most commonly atopic dermatitis (78%–87%). Half of people suffer from asthma (48%–67%) and/or allergic rhinitis (34%–62%) 12. The majority of children are allergic to cow’s milk (80%), chicken egg white (56%–72%), fish (28%), soya (24%–50%), and peanuts (29%–50%) 12.
The wheat allergy clinical picture depends on age 12. Symptoms develop within minutes to 1–2 h after the ingestion of wheat. In young children gastroenterological symptoms prevail, such as vomiting, diarrhea or rarely, abdomen pains. In about 40% of children skin symptoms are observed in a form of urticaria, erythema, angioedema, pruritus, or worsening atopic dermatitis 13. Intestinal symptoms recede with age; therefore, older children suffer mostly from dermatitis, which is accompanied by respiratory disorders (wheeze, stridor, persistent cough, hoarse voice, respiratory distress, nasal congestion) and, in the most severe cases, anaphylaxis. In teenagers and adults the most severe forms of allergy prevail, such as anaphylaxis symptoms (in 45%–50%), which is typical of wheat allergy. Intestinal and skin symptoms are less common in these age groups 12.
Wheat allergy is usually diagnosed in young children, but it is rarely seen in infants, despite the fact that wheat proteins pass into breast milk, which wheat allergys proven by Linn et al. in 1996 14. In another study on 50 children with wheat allergy, the disease was diagnosed in 32% of infants 5. Three of them were fed exclusively on their mother’s milk 12. In 1981, Rudd et al. 15 described a case of an infant with anaphylactic shock after consuming semolina pudding.
Wheat allergy can be accompanied by allergies to other cereals, most often to rye and/or corn 16.
A child or adult with wheat allergy is likely to develop symptoms within minutes to hours after eating something containing wheat. Wheat allergy symptoms include:
- Swelling, itching or irritation of the mouth or throat
- Hives, itchy rash or swelling of the skin
- Nasal congestion
- Headache
- Itchy, watery eyes
- Difficulty breathing
- Cramps, nausea or vomiting
- Diarrhea
- Anaphylaxis
Most young children with wheat allergy outgrow it by ages 3 to 5.
Anaphylaxis
Symptoms of severe allergy (anaphylaxis) may include:
- trouble breathing or noisy breathing
- difficulty talking more than a few words and/or hoarse voice
- wheeze
- cough
- swelling and tightness of the throat
- collapse
- light-headedness or dizziness
- diarrhea
- tingling in the hands, feet, lips or scalp
- swelling of tongue
- pale and floppy (in young children)
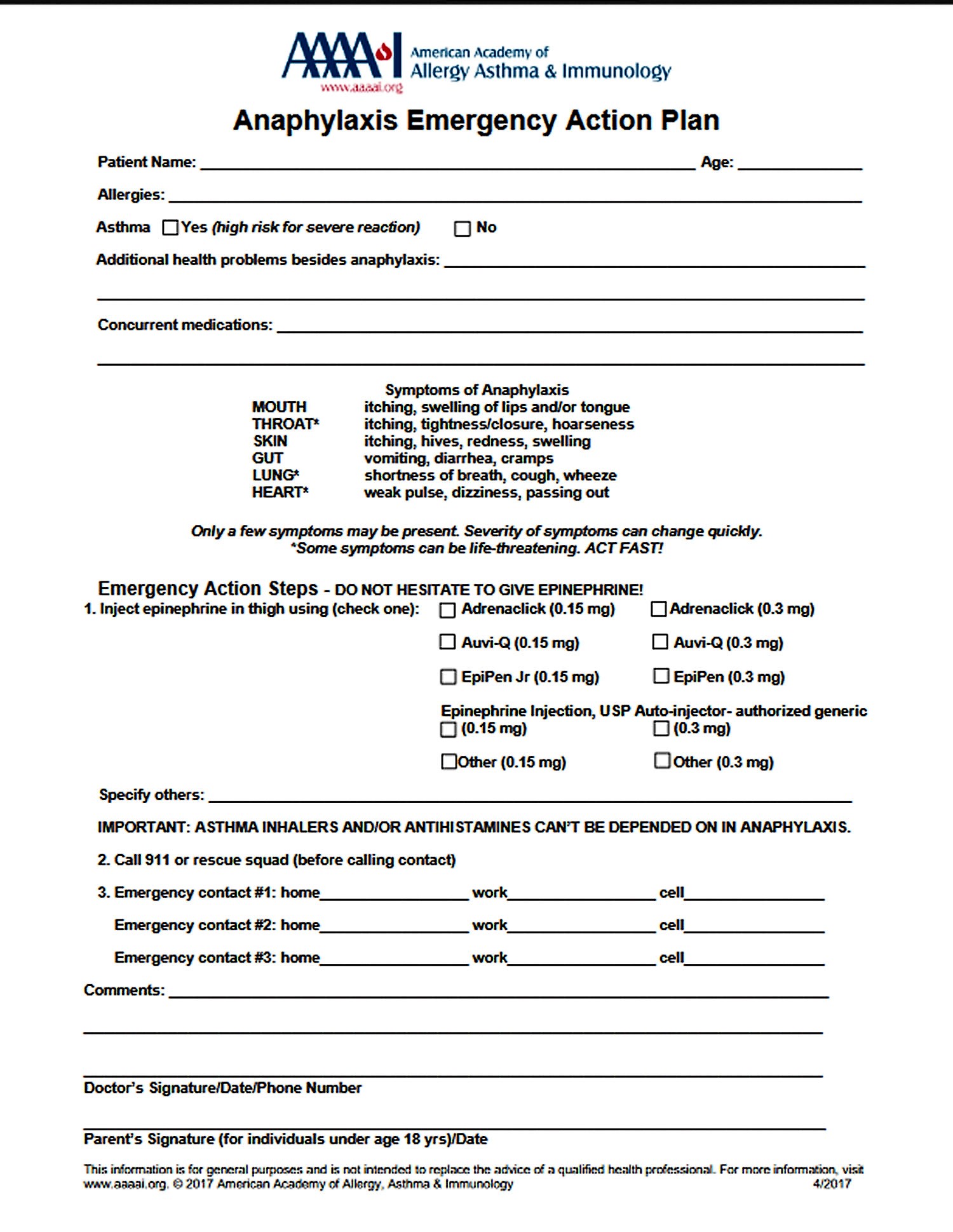
A severe allergic reaction (anaphylaxis) is a medical emergency. Call your local emergency immediately. Lay the person down. If they have an adrenaline injector and you are able to administer it, do so.
Figure 3. Anaphylaxis Emergency Action Plan
Causes of wheat allergy
If you have wheat allergy, exposure to a wheat protein primes your immune system for an allergic reaction. You can develop an allergy to any of the four classes of wheat proteins — albumin, globulin, gliadin and gluten.
Wheat Grain Proteins
All of the wheat-induced diseases are caused by wheat proteins which constitute 10%–18% of the grain mass, depending on the strain. The main component (70%) of the wheat grain is starch.
Depending on their dissolving agent, the wheat grain proteins are categorized into four main fractions: albumins (15%), globulins (7%), gliadins (33%), and glutenins (45%). Albumins are soluble in water; globulins, in salt solutions; gliadins, in alcohol; and while glutenins, in dilute acid and alkali. Albumins and globulins are structural proteins that contain many enzymes. Gliadins and glutenins are prolamins and are referred to as gluten. They are storage proteins.
The wheat proteins that are regarded today as the WA major allergens will be discussed in detail in the next chapter. Wheat proteins triggering CD symptoms belong to gliadins. Wheat proteins responsible for non-celiac-gluten sensitivity have not been identified yet. One of the proteins under the researchers’ examination is a group of amylase-trypsin inhibitors that do not belong to glutens 17.
Sources of wheat proteins
Some sources of wheat proteins are obvious, such as bread, but all wheat proteins — and gluten in particular — can be found in many prepared foods and even in some cosmetics, bath products and play dough. Foods that may include wheat proteins include:
- Breads and bread crumbs
- Cakes and muffins
- Cookies
- Breakfast cereals
- Pasta
- Couscous
- Farina
- Semolina
- Spelt
- Crackers
- Beer
- Hydrolyzed vegetable protein
- Soy sauce
- Some condiments, such as ketchup
- Meat products, such as hot dogs or cold cuts
- Dairy products, such as ice cream
- Natural flavorings
- Gelatinized starch
- Modified food starch
- Vegetable gum
- Licorice
- Jelly beans
- Hard candies
If you have a wheat allergy, you might also be allergic to barley, oats and rye — but the chance is slim. If you’re not allergic to grains other than wheat, a wheat-free diet is less restrictive than a gluten-free diet.
Wheat-dependent, exercise-induced anaphylaxis
Some people with a wheat allergy develop symptoms only if they exercise within a few hours after eating wheat. Exercise-induced changes in your body either trigger an allergic reaction or worsen an immune system response to a wheat protein. This condition usually results in life-threatening anaphylaxis.
Risk factors for wheat allergy
Certain factors may put you at greater risk of developing a wheat allergy:
- Family history. You’re at increased risk of allergy to wheat or other foods if your parents have food allergies or other allergies, such as hay fever.
- Age. Wheat allergy is most common in babies and toddlers, who have immature immune and digestive systems. Most children outgrow wheat allergy, but adults can develop it, often as a cross-sensitivity to grass pollen.
Diagnosis of gluten (wheat) allergy
Gluten allergy test
The wheat allergy diagnosis is difficult because not all of the major wheat grain allergens are recognized. Similarly, to any other allergy, the gold standard of wheat allergy diagnosis remains the oral food challenge. It is usually performed in its open form, as the majority of the observed adverse reactions is of the objective nature. The patient is given whole wheat starting from small doses of wheat-specific protein (1–50 mg) followed by increasingly larger hourly doses (digestion of wheat can be slower than egg or milk), ending with a cumulative dose of up to 0.5–1 g of wheat protein 4. Additionally, double-blind placebo-controlled protocols of wheat allergy have been published both for children 18 and adults 19. Wheat allergy is diagnosed when the challenge test results are positive and the symptoms appear up to two hours after ingestion.
In the next stage, allergological tests should be performed to confirm the elevated levels of wheat allergen-specific IgE. The first are skin tests to wheat flour. Generally, commercial wheat extract is used, the specificity of which is very low 4 Some allergologists prepare an in-house wheat flour solution, but its specificity is also very low. It can be improved by additional testing to ω-5 gliadin or other gliadins, but these solutions are not routinely available and are mainly used in scientific research. In skin test, tiny drops of purified allergen extracts — including extracts for wheat proteins — are pricked onto your skin’s surface, either on your forearm or upper back. After 15 minutes, your doctor or nurse looks for signs of allergic reactions. If you develop a red, itchy bump where the wheat protein extract was pricked onto your skin, you may be allergic to wheat. The most common side effect of these skin tests is itching and redness.
Another step is the determination of serum concentrations of allergen-specific IgE to whole wheat extract. They are commercially available but their specificity is low despite high sensitivity 4.
Solutions used for skin tests to wheat flour and for the assessment of allergen-specific IgE to whole wheat extract consist of the mixture of grain albumins and globulins and, thus, do not contain the insoluble major wheat allergens, i.e., prolamins. This is why the utility of these tests in wheat allergy diagnosis is lower than in allergies to other foods, such as milk, egg, or peanuts 20. Moreover, their concentration is not correlated with the severity of clinical reactions after wheat ingestion.
Gluten-specific IgE can also be assessed. Since the commercial test contains wheat gluten proteins, it is positive only in the case of a wheat allergy and negative in the case of allergies to other gluten-containing cereals. It is not known if it includes major wheat allergens. Gluten-specific IgE assays are positive in two thirds of children with wheat allergy 12.
Currently, there are commercial tests for the IgE specific to two known allergenic molecules of wheat: Tri a 14 non-specific lipid transfer protein and Tri a 19 rω-5-gliadin.
It is characteristic of children who had wheat allergy, and have developed a tolerance to wheat, that in most of them (approximately 80%) skin tests to wheat continue to be positive and IgE specific to whole wheat extract and gluten-specific IgE remain elevated, which is rare in other food allergies 12. For the majority of food allergens, tolerance development is accompanied by negative skin tests and normalized specific IgE levels. In our studies, at the time of tolerance development, the levels of IgE specific to whole wheat extract ranged between 0.35–23.9 kU/L (median: 3.0 kU/L) 12. In that group of people, at the time of wheat allergy diagnosis, the levels of IgE specific to whole wheat extract had been between 2.2 kU/L and 39.3 kU/L (median: 8.42 kU/L). This is why the size of skin test and the levels of IgE specific to whole wheat extract are not useful in differentiating between the periods of allergy and tolerance. It should be stressed, however, that in individual children who have developed tolerance to wheat the skin test values and IgE specific to whole wheat extract and gluten are lower than when wheat allergy was diagnosed.
Gluten allergy management
Avoiding wheat proteins is the best treatment for wheat allergy. Because wheat proteins appear in so many prepared foods, read product labels carefully. It is believed that different species of wheat have the same allergenicity, therefore, it is not recommended for the patients with severe wheat allergy to try different forms of wheat.
The research literature has provided the first report on the oral immunotherapy administered to older children with anaphylaxis triggered by wheat ingestion. After two years, the therapy resulted in the desensitization in 61% of the patients 21. Further studies are necessary to evaluate the effectiveness of this type of wheat allergy treatment.
In the USA the rω-5 gliadin-free variety of wheat has been produced 22.
It is worth emphasizing that even though IgE-mediated wheat allergy belongs to gluten-dependent disorders, it is induced solely by wheat proteins, thus being treated by a wheat-free diet. The remaining gluten cereals, such as rye, barley, and oats are well tolerated by most patients and should not be eliminated from their diet 5. In wheat allergy children, oat allergy is very rare. Rye and barley allergies are slightly more common.
Drugs
Antihistamines may reduce signs and symptoms of wheat allergies. These drugs can be taken after exposure to wheat to control your reaction and help relieve discomfort. Ask your doctor if a prescription or over-the-counter allergy drug is appropriate for you.
Epinephrine is an emergency treatment for anaphylaxis. If you’re at risk of having a severe reaction to wheat, you may need to carry two injectable doses of epinephrine (EpiPen, Auvi-Q, others) with you at all times. A second pen is recommended for people at high risk of life-threatening anaphylaxis in case anaphylactic symptoms return before emergency care is available.
Home remedies
You can take steps to avoid exposure to wheat proteins and ensure prompt treatment when you’re accidentally exposed to wheat.
- Keep others informed. If your child has wheat allergy, make sure that anyone who takes care of your child, including the principal, teachers and nurse at school, know about the allergy and the signs of wheat exposure. If your child carries epinephrine, make sure school personnel know how to use the pen, if necessary, and that they need to contact emergency care immediately. Inform friends, relatives and co-workers of your own food allergy.
- Wear a bracelet. A medical identification bracelet that describes the allergy and need for emergency care can help if you experience anaphylaxis and can’t communicate.
- Always read labels. Don’t trust that a product is free of what you can’t eat until you read the label. Wheat proteins, especially gluten, are used as food thickeners, and they appear in many unexpected places. Also, don’t assume that once you’ve used a certain brand of a product, that it’s always safe. Ingredients change.
- Shop for gluten-free foods. Some specialty stores and supermarkets offer gluten-free foods, which are safe for people with wheat allergies. However, they may also be free of grains that you can eat, so sticking to gluten-free foods may limit your diet for no reason.
- Consult wheat-free cookbooks. Cookbooks specializing in recipes without wheat can help you cook safely and enable you to enjoy baked goods and other foods made with substitutes for wheat.
- Dine out cautiously. Tell restaurant staff about your allergy and how serious it can be if you eat anything with wheat. Order simple dishes prepared with fresh foods. Avoid foods that may have hidden sources of wheat proteins, such as sauces, or deep-fried foods that may be cooked with other foods containing wheat.
- Tanabe S. Analysis of food allergen structures and development of foods for allergic patients. Biosci Biotechnol Biochem. 2008;72:649–659. doi: 10.1271/bbb.70708. https://www.jstage.jst.go.jp/article/bbb/72/3/72_70708/_pdf/-char/en[↩]
- Sapone A, Bai JC, Ciacci C, et al. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Medicine. 2012;10:13. doi:10.1186/1741-7015-10-13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3292448/[↩][↩][↩][↩][↩]
- Barrosa Maia E, Chaves LC, Lemos S, Pinheiro JA. P98 – Gluten allergy. Clinical and Translational Allergy. 2014;4(Suppl 1):P153. doi:10.1186/2045-7022-4-S1-P153. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4082129/[↩]
- Mäkelä M. Wheat allergy. In: Matricardi P.M., Kleine-Tebbe J., Hoffmann H., Rudolf V., Ollert M., editors. EAACI Molecular Allergology User’s Guide. 1st ed. European Academy of Allergy and Clinical Immunology; Viena, Austria: 2016. pp. 213–223.[↩][↩][↩][↩][↩][↩]
- Czaja-Bulsa G, Bulsa M. What Do We Know Now about IgE-Mediated Wheat Allergy in Children? Nutrients. 2017;9(1):35. doi:10.3390/nu9010035. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5295079/[↩][↩][↩]
- Longo G., Berti I., Burks A.W., Krauss B., Brabie E. IgE-mediated food allergy in children. Lancet. 2013;382:1656–1664. doi: 10.1016/S0140-6736(13)60309-8. https://www.ncbi.nlm.nih.gov/pubmed/23845860[↩][↩]
- Nwaru B.I., Hickstein L., Panesar S.S., Roberts G., Muraro A., Sheikh A. on behalf of The EAACI Food Allergy and Anaphyllaxis Guidelines Group. Prevelence of common food allergies in Europe. In: Muraro A., Roberts G., editors. Food Allergy and Anaphylaxis Guidelines. 1st ed. European Academy of Allergy and Clinical Immunology (EAACI); Zurich, Switzerland: 2014. pp. 23–45. https://www.ncbi.nlm.nih.gov/pubmed/24816523[↩]
- Zuidmeer L., Goldhahn K., Rona R.J., Gislason D., Madsen C., Summers C., Sodergren E., Dahlstrom J., Lindner T., Sigurdardottir S.T., et al. The prevalence of plant food allergies: A systematic review. J. Allergy Clin. Immunol. 2008;121:1210–1218. doi: 10.1016/j.jaci.2008.02.019. https://www.ncbi.nlm.nih.gov/pubmed/18378288[↩]
- Ostblom E., Lilja G., Pershagen G., van Hage M., Wickman M. Phenotypes of food hypersensitivity and development of allergic diseases during the first 8 years of life. Clin. Exp. Allergy. 2008;38:1325–1332. doi: 10.1111/j.1365-2222.2008.03010.x. https://www.ncbi.nlm.nih.gov/pubmed/18477012[↩]
- Sicherer S.H., Morrow E.H., Sampson H.A. Dose-response in double-blind, placebo-controlled oral food challenges in children with atopic dermatitis. J. Allergy Clin. Immunol. 2004;114:144–149. doi: 10.1067/mai.2000.104941. https://www.ncbi.nlm.nih.gov/pubmed/10719311[↩]
- Catassi C., Gatti S., Fasano A. The new epidemiology of celiac disease. J. Pediatr. Gastroenterol. Nutr. 2014;59:S7–S9. doi: 10.1097/01.mpg.0000450393.23156.59. https://www.ncbi.nlm.nih.gov/pubmed/24979197[↩]
- Czaja-Bulsa G., Bulsa M. The natural history of IgE mediated wheat allergy in children with dominant gastrointestinal symptoms. Allergy Asthma Clin. Immunol. 2014;10:12. doi: 10.1186/1710-1492-10-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3939402/[↩][↩][↩][↩][↩][↩][↩][↩]
- Christensen M.J., Eller E., Mortz C.H., Bindslev-Jensen C. Patterns of suspected wheat-related allergy: A retrospective single-centre case note review in 156 patients. Clin. Transl. Allergy. 2014;4:39. doi: 10.1186/2045-7022-4-39. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4405838/[↩]
- Linna O. Specific IgE antibodies to uningested cereals. Allergy. 1996;51:849–850. doi: 10.1111/j.1398-9995.1996.tb00034.x. https://www.ncbi.nlm.nih.gov/pubmed/8947346[↩]
- Rudd P., Manuel P., Walker-Smith J. Anaphylactic shock in an infant after feeding with a wheat rusk. A transient phenomenon. Postgrad Med. J. 1981;57:794–795. doi: 10.1136/pgmj.57.674.794. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2426275/pdf/postmedj00228-0054.pdf[↩]
- Mansouri M., Pourpak Z., Mozafari H., Abdollah Gorji F., Shokouhi Shoormasti R. Follow-up of the wheat allergy in children; consequences and outgrowing the allergy. Iran. J. Allergy Asthma Immunol. 2012;11:157–163. https://www.ncbi.nlm.nih.gov/pubmed/22761189[↩]
- Junker Y., Zeissinq S., Kim S.J., Barisani D., Wieser H., Leffler D.A., Zevallos V., Libermann T.A., Dillon S., Freitaq T.L., et al. Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J. Exp. Med. 2012;209:2395–2408. doi: 10.1084/jem.20102660. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3526354/[↩]
- Ito K., Futamura M., Borres M.P., Takaoka Y., Dahlstrom J., Sakamoto T., Tanaka A., Kohno K., Matsuo H., Morita E. IgE antibodies to ω-5 gliadin associate with immediate symptoms on oral wheat challenge in Japanese children. Allergy. 2008;63:1536–1542. doi: 10.1111/j.1398-9995.2008.01753.x. https://www.ncbi.nlm.nih.gov/pubmed/18925890[↩]
- Scibilia J., Pastorello E.A., Zisa G., Ottolenghi A., Bindslev-Jensen C., Pravettoni V., Scovena E., Robino A., Ortolani C. Wheat allergy: A double-blind, placebo-controlled study in adults. J. Allergy Clin. Immunol. 2006;117:433–439. doi: 10.1016/j.jaci.2005.10.014. https://www.ncbi.nlm.nih.gov/pubmed/16461145[↩]
- Sampson H.A. Utility of food-specific IgE concentrations in predicting symptomatic food allergy. J. Allergy Clin. Immunol. 2001;107:891–896. doi: 10.1067/mai.2001.114708. https://www.ncbi.nlm.nih.gov/pubmed/11344358[↩]
- Sato S., Utsunomiya T., Imai T., Yanagida N. Wheat oral immunotherapy for wheat-induced anaphylaxis. J. Allergy Clin. Immunol. 2015;4:1131–1133. doi: 10.1016/j.jaci.2015.07.019. https://www.ncbi.nlm.nih.gov/pubmed/26319801[↩]
- Altenbach S.B., Allen P.V. Transformation of the US bread wheat ‘Butte 86’ and silencing of omega-5 gliadin genes. GM Crops. 2011;2:66–73. doi: 10.4161/gmcr.2.1.15884. https://www.ncbi.nlm.nih.gov/pubmed/21844700[↩]